- 1Department of Urology, The Affiliated Hospital of Yangzhou University, Yangzhou University, Yangzhou, China
- 2Department of Paediatrics, Yantai Yuhuangding Hospital, Yantai, China
- 3Department of Endocrinology, Yantai Yuhuangding Hospital, Yantai, China
Background: The desmopressin combined with anticholinergic agents for the treatment of nocturnal enuresis (NE) remains controversial. This meta-analysis assesses the efficacy and safety of desmopressin compared with desmopressin plus anticholinergic agents for the treatment of NE.
Methods: We searched MEDLINE, Embase, and Cochrane Controlled Trials Register databases for RCTs published for the treatment of NE. Systematic review was carried out using the Preferred Reporting Items for Systematic Reviews and Meta-analyses. This meta-analysis used RevMan v.5.1.0 to analyze data.
Results: Eight studies involving 600 patients (293 in the combination group and 307 in the desmopressin group) contained meaningful data. The results were as follows: after one month of treatment, compared with the desmopressin monotherapy group, the combination group was significantly better in treating NE in FR (full responders, P = 0.003), FR + PR (partial responders) (P < 0.0001), and the mean number of wet nights (P = 0.004); also, the combination group had a better effect in FR (P < 0.00001), FR + PR (P = 0.02) and the mean number of wet nights (P = 0.04) after 3 months' treatment. For side effects, combination therapy does not cause more adverse events in treating NE (P = 0.42).
Conclusions: This study elucidates that desmopressin combined with the anticholinergic agent was demonstrated to be more effective in treating NE than desmopressin monotherapy, and the anticholinergic agent does not increase the risk of adverse events (AEs).
Introduction
The International Children's Continence Society (ICCS) defines nocturnal enuresis (NE) as intermittent incontinence of urine or bed wetting during sleep in children aged >5 years (1, 2). According to the characteristics of NE, it can be categorized into primary and secondary enuresis. Primary enuresis is diagnosed when the symptoms of enuresis have persisted since infancy, while secondary enuresis is defined as a return to bedwetting after the patient has been consistently dry for at least 6 months at night. Moreover, based on the presence of daytime lower urinary tract symptoms (LUTS), enuresis can be categorized into monosymptomatic (MNE) or non-monosymptomatic (NMNE) (3). NE affects approximately 15%–20% of 5-year-old children, 5% of 10-year-olds, 1%–2% of individuals aged 15 years, and up to 2% of young adults (4, 5). It has brought a significant influence and considerable distress to the patients and their family. It would seriously affect the everyday life. The etiology and pathogenesis of NE are still unknown. However, in view of the present research, the primary etiology includes the following aspects: nocturnal low bladder capacity, nocturnal polyuria, and arousal disorder (6). At present, NE is not considered a self-healing disease, and it necessitates appropriate diagnostic and therapeutic work-up by humans. In principle, NE treatment can be divided into drug and non-drug treatment. The medication for NE includes desmopressin, anticholinergic drugs (tolterodine and solifenacin), and others (imipramine). Non-drug therapy includes bedwetting alarms and limitations of fluid intake (7).
Desmopressin, a naturally produced vasopressin analog, can increase the water permeability of collecting ducts and reduce urination frequency and nocturia (excessive urination at night) (8). At present, desmopressin is used as a first-line therapy for NE. It has been approved to cure NE (9). It has an immediate effect on NE and can be administered intranasally or orally. Compared with intranasal administration, oral administration has fewer side effects and is more convenient. The recommended dosage of desmopressin is 0.2 mg daily (taken orally). Faraj et al. (10) reported that desmopressin resulted in 85% dry nights after 3 months of treating MNE. However, research shows that approximately 20% of patients experience poor effects after drug therapy for 3 months, which is known as desmopressin-resistant NE (11). Moreover, functional bladder capacity decreases because of detrusor overactivity, the major cause of NE (12). However, in the clinical course of treatment, using a single drug (desmopressin monotherapy) cannot produce satisfactory results for patients with NE. Therefore, combination drug therapy was gradually used in clinical treatment and was proven efficient. Anticholinergic agents, such as tolterodine and solifenacin, may improve the function of the bladder and allow it to store more urine (13). Some studies show that the combined use of anticholinergic agents and desmopressin plays an important role in treating desmopressin-resistant NE, reducing the mean number of wet nights in patients with NE (14, 15). However, desmopressin combined with anticholinergic agents for treating NE remains controversial.
We performed a systematic review and meta-analysis of randomized controlled trials (RCTs) to assess the efficacy and safety of desmopressin compared with anticholinergic agents for treating NE.
Materials and methods
Search strategy
We searched the MEDLINE, Embase, and Cochrane Controlled Trials Register databases for RCTs published before January 2023 using the following search criteria: NE, desmopressin, anticholinergic agent, and RCT. We confined our search to published studies in English only and obtained certain essential information directly from the authors. We also screened the relevant references of the included studies.
Inclusion criteria
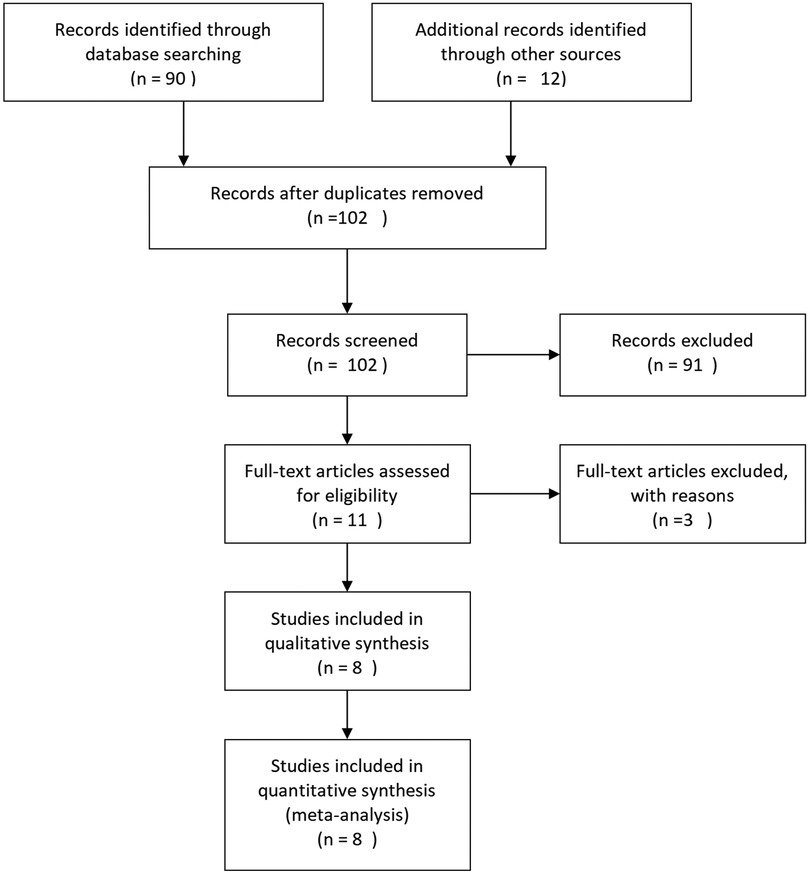
All of the included RCTs meet the following criteria: (1) involved the use of desmopressin and anticholinergic agents for the treatment of NE, (2) had full useful RCT texts, and (3) provided accurate data for analysis, including the total number of subjects and the values of each indicator. The exclusion criteria include (1) data incompleteness in articles and (2) article types of abstract, review, case–control, comment, cohort studies, and others. We included the most recently published study only if it described identical experiments. However, each study would be included if different indicators were evaluated. As shown in Figure 1, we used a flowchart to show the selection process of the study.
Quality assessment
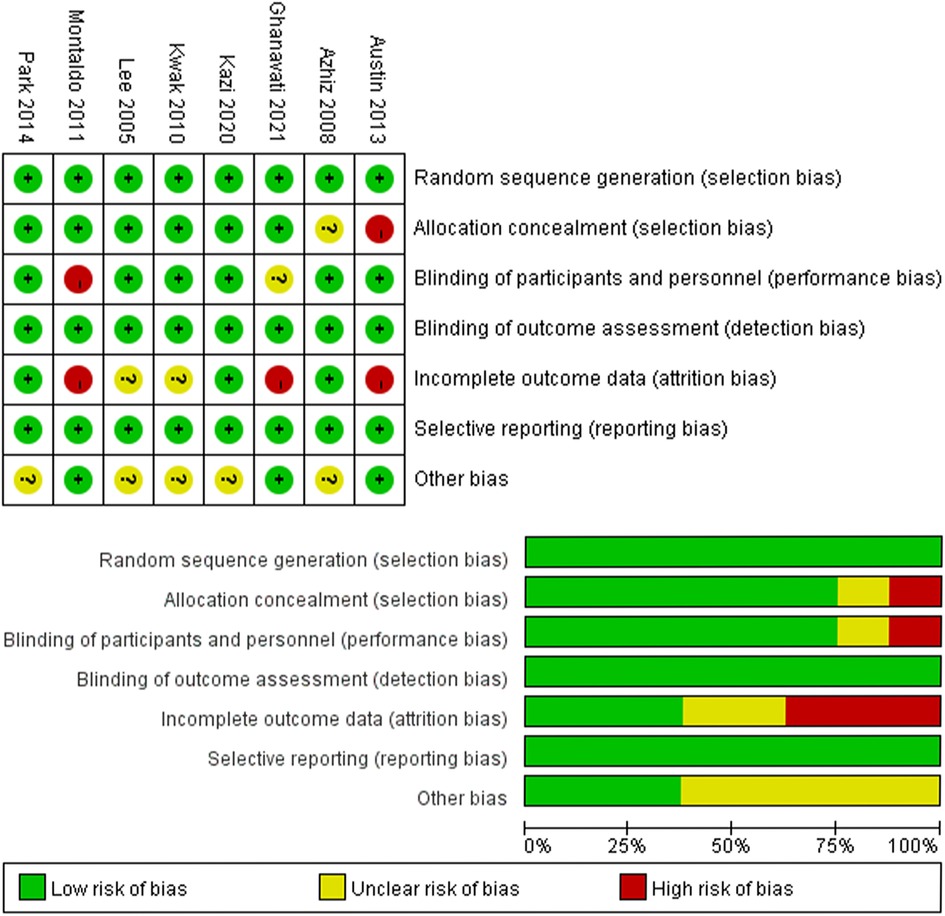
The Cochrane risk of bias tool was used to determine the quality of the retrieved RCTs. The quality items were selective outcome reporting, blinding, allocation concealment, incomplete outcome data, random sequence generation, and other sources of bias. According to the discussions among the authors, a graph summarizing the risk of bias was generated, as shown in Figure 2. Meanwhile, according to the guidelines published in the Cochrane Handbook for Systematic Reviews of Interventions v.5.3.0, the studies were classified qualitatively (16). All authors participated in the quality assessment of all RCTs and agreed with the results. Moreover, any differences between each RCT were resolved through discussion among authors. All authors participated in the RCTs’ quality assessment and agreed on the final results.
Data extraction
We recorded the following information from the studies: (1) general data of RCTs, (2) name of the first author, (3) design of the study and size of the sample, (4) published time, and (5) changes of efficacious data at 1 and 3 months for the parameters full responders (FR: ≥90% reduction in the number of wet nights), FR plus partial responders (PR: 50%–89% reduction in the number of wet nights), mean number of wet nights, and side effects. Finally, another author checked the data extracted from the text. Meanwhile, our team crosschecked the references and data for each included study to ensure no overlapping data and maintain the integrity of the meta-analysis.
Statistical analysis and meta-analysis
This meta-analysis used RevMan v.5.1.0 (Cochrane Collaboration, Oxford, UK) to analyze the data (17). The odds ratio (OR) with 95% confidence interval (CI) was applied to analyze the dichotomous data, and the mean difference (MD) with 95% CI was utilized to analyze the continuous data among the groups. The chi-squared test based on Q statistic was performed to check the heterogeneity among the studies, and the result was recognized as significant at P < 0.05. The fixed-effects model was used and considered homogeneous if the result has a P-value of >0.05. We utilized the I2 statistic to analyze inconsistent results, which can reflect the proportion of heterogeneity across trials. When I2 < 50%, indicating that there was no significant heterogeneity, the fixed-effects model (Mantel–Haenszel method) would be used. We performed the random-effects model (DerSimonian and Laird method) when the heterogeneity of the data could not be explained (P < 0.05, I2 > 50%). In this meta-analysis, it is not necessary to have ethical approval and patient consent because all data were acquired from articles that have already been published.
Results
Characteristics of the individual studies
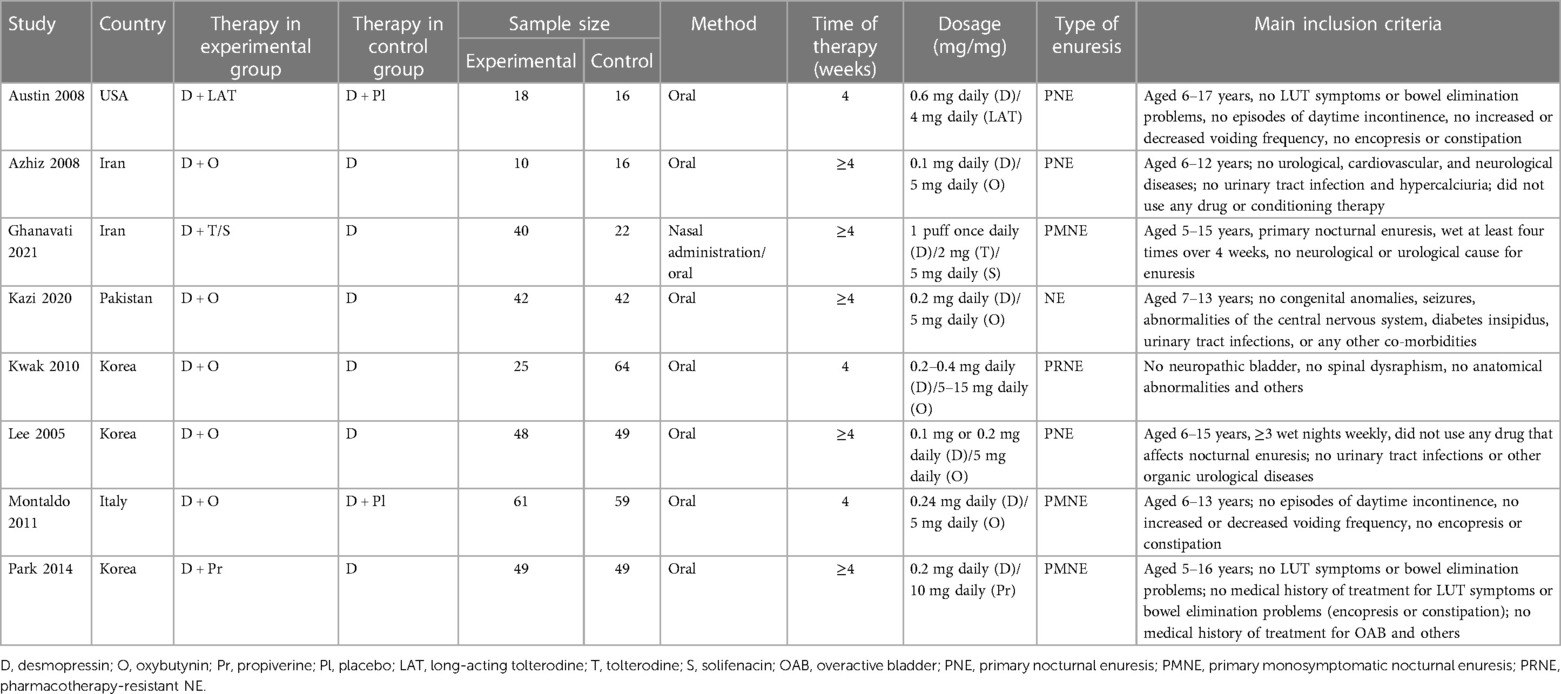
We identified 102 studies in all databases. According to the inclusion and exclusion criteria described above, our research removed 91 studies after reviewing the titles and abstracts of the articles. Three studies were excluded for lack of valuable data. A total of 26 studies were ruled out for lack of useful data. Finally, eight RCTs (18–25) involving 600 patients were included in our analysis. Figure 1 presents a detailed flowchart showing the selection process. Table 1 shows the baseline characteristics of the studies.
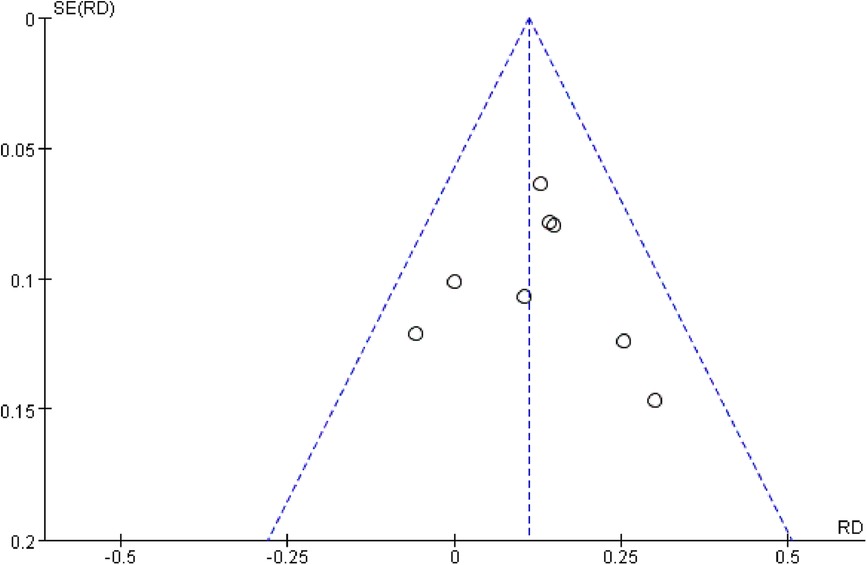
Quality of the individual studies
All eight studies were RCTs and double-blind. Figure 2 presents a graphical summary of the risk bias. Meanwhile, we also found that their randomization process had been elaborated in all the papers. All the included RCTs calculated the efficiency and determined the best sample size. The funnel plot displayed the conclusion of a qualitative estimation of the publication bias of each RCT (Figure 3). Table 2 shows the specific inclusion and exclusion criteria.
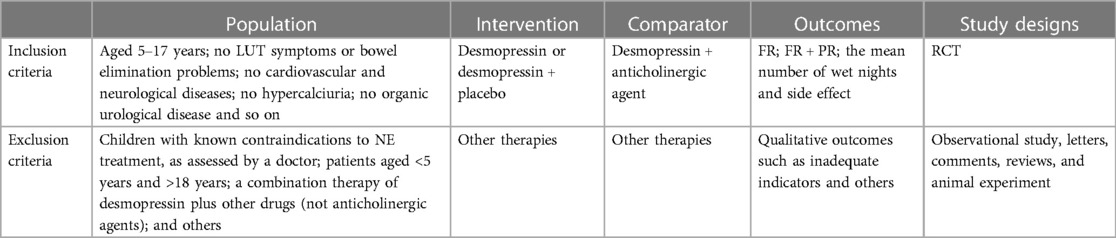
Table 2. Criteria for considering studies for the review based on the Population, Intervention, Comparator, Outcomes, and Study Designs (PICOS) structure.
Efficacy
One month
FR
Eight studies involving 600 patients (293 in the combination group and 307 in the desmopressin group) contained meaningful data. A fixed-effects model was used to evaluate changes between the two groups, which showed an OR of 1.81, 95% CI: −1.22 to 2.69, P = 0.003. The result of the research proves that the combination group showed more significant improvement in FR compared with the desmopressin group (Figure 4A).
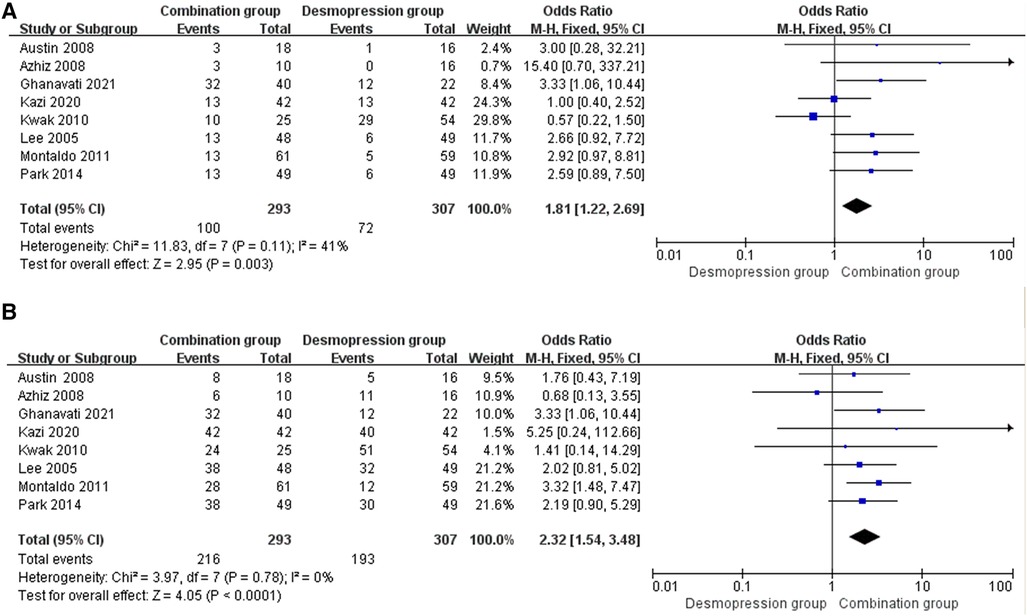
Figure 4. Forest plots showing changes between two groups in (A) FR at 1 month and (B) FR+PR at 1 month.
FR+PR
Eight studies involving 600 patients (293 in the combination group and 307 in the desmopressin group) contained meaningful data. A fixed-effects model was used to evaluate changes between the two groups, which showed an OR of 2.32, 95% CI: 1.54–3.48, P < 0.0001. The research results proved that the combination group showed greater improvement in FR+PR compared with the desmopressin group (Figure 4B).
Three months
FR
Five studies involving 367 patients (189 in the combination group and 178 in the desmopressin group) contained meaningful data. A fixed-effects model was used to evaluate changes between the two groups, which showed an OR of 3.18, 95% CI: 1.91–5.28, P < 0.00001. The result of the research proved that the combination group showed greater improvement in FR compared with the desmopressin group (Figure 5A).

Figure 5. Forest plots showing changes between two groups in (A) FR at 3 months and (B) FR+PR at 3 months.
FR+PR
Eight studies involving 367 patients (189 in the combination group and 178 in the desmopressin group) contained meaningful data. A fixed-effects model was used to evaluate changes between the two groups, which showed an OR of 2.39, 95% CI: 1.18–4.83, P = 0.02. The research results prove that the combination group showed greater improvement in FR+PR compared with the desmopressin group (Figure 5B).
The mean number of wet nights
One month
Five RCTs involving 317 patients (165 in the combination group and 152 in the desmopressin group) recorded changes in impact in the mean number of wet nights (Figure 6A). A fixed-effects model showed an MD of −4.57, 95% CI: −7.65 to −1.48, P = 0.004. The results suggest that the combination group showed statistical differences in the impact on the mean number of wet nights compared with the desmopressin group.
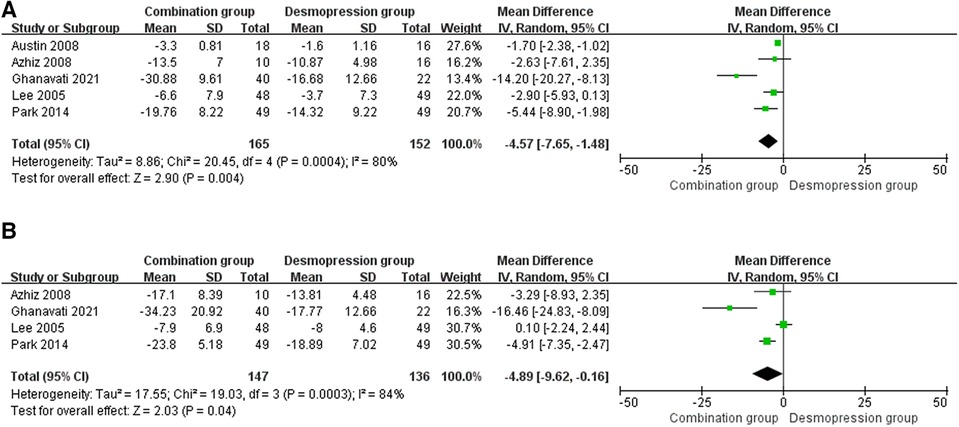
Figure 6. Forest plots showing changes between two groups in (A) the mean number of wet nights at 1 month and (B) the mean number of wet nights at 3 months. IV, inverse variance.
Three months
Four RCTs involving 283 patients (147 in the combination group and 136 in the desmopressin group) recorded the changes in impact in the mean number of wet nights (Figure 6B). A random-effects model showed an MD of −4.89, 95% CI: −9.62 to 0.16, P = 0.04. In addition, there were differences in the mean number of wet nights between the two groups.
Safety
Side effect
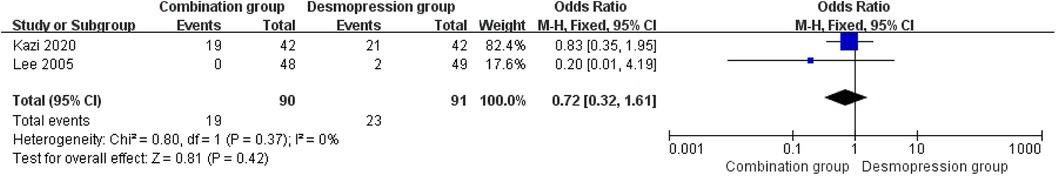
Two RCTs, including 181 participants (90 in the combination group and 91 in the desmopressin group), were involved in the research for side effect. The study of the OR was 0.72, and the 95% CI was 0.32–1.61 (P = 0.42). These results indicate that there is no significant difference between the two groups in terms of side effect (Figure 7).
Discussion
NE, also known as enuresis, is a common problem for children. The prevalence of NE is falling by approximately 15% a year, and the incidence rate for boys is higher than that for girls (26). A great lot of evidence sustains that NE is a heterogeneous disease. Several important etiological factors can explain this disease. The genetic determinant is one of the important mechanisms that cause NE. Children had a 44% and 77% increased risk of having the disease if one or both of their parents suffered from NE (27). Nevertheless, no specific gene that appeared to be involved in NE had been discovered until now (27). Disturbed and delayed maturation plays an important part in the pathogenesis of NE (28). Although desmopressin is the first choice for treating NE, the treatment alone is not satisfactory sometimes. Anticholinergic therapy has been proven to be an effective solution for children who no longer respond or have partial responses to desmopressin monotherapy.
The systematic review and quantitative meta-analysis showed evidence from RCTs regarding the efficacy and safety of desmopressin compared with anticholinergic agents for NE. For the study, the inclusion criteria included patients aged between 5 and 17 years, no neurological or urological cause for enuresis, and no LUTS or bowel elimination problems. In a 1-month-long study, compared with the desmopressin group, the combination group showed statistical difference in FR (P = 0.003) and FR+PR (P < 0.0001) for NE. During the 6-month study, the combination group also showed statistical difference in FR (P < 0.00001) and FR+PR (P = 0.02) compared with the desmopressin group for NE. Meanwhile, for the change in the mean number of wet nights, the combination group showed statistical differences compared with the desmopressin group for NE at 1 (P = 0.004) or 3 (P = 0.04) months. To sum up, the effect of combined medication is more effective, which is superior to the alone group.
Desmopressin monotherapy is often considered the first-line treatment for NE. It can reduce urine production in the nighttime (29). Desmopressin is relatively safe and effective; reports have claimed that the effective rate is between 60% and 70%. Approximately 30% of patients are FR, and 40% partially responded to the treatment (30, 31). Meanwhile, patients with oral desmopressin should limit water intake in the evening because of its side effects (water intoxication and hyponatremia). As mentioned earlier, using a single drug has failed to achieve satisfactory treatment outcomes. Therefore, anticholinergics combined with desmopressin in treating NE was regarded as second-line therapy for patients who failed to respond to desmopressin monotherapy (23, 32). It has been confirmed that anticholinergic treatment can reduce the frequency and severity of urge incontinence in children with non-organic lower urinary tract (LUT) dysfunction (33). Meanwhile, studies have pointed out that anticholinergic agents may play an essential role in improving the vesical volume and thickness of the bladder wall for patients with NE (24). In our study, the alleviation of symptoms is much better in the combination therapy than the desmopressin monotherapy. Thus, the success of combination therapy ultimately depends on two pivotal regulatory factors: (1) desmopressin can decrease the production or secretion of nocturnal urine (34, 35) and (2) anticholinergic agents can increase bladder capacity and reduce detrusor overactivity (36). It is noteworthy that the anticholinergics monotherapy is not currently recommended (37).
Only two studies reported on the results of adverse events (AEs). Significantly, the incidence of adverse reactions between the two groups (P < 0.42), such as headache, nausea, and decreased appetite, was not significantly different. Therefore, these results demonstrate the safety of desmopressin in conjunction with anticholinergics in treating NE. Also, note that the study excluded children with constipation; the anticholinergic treatment may worsen the symptoms of constipation, and the rate of this side effect is 0.2%–2.3% (38). In addition, the potential mechanisms of combination therapy are currently unclear and need further studies.
In a word, this meta-analysis included eight RCTs and concentrated on the efficacy and safety of desmopressin in combination with anticholinergic agents for treating NE. This study had advantages compared with previous studies. The data of this meta-analysis were derived from randomized, double-blind, controlled trials. Thus, the results of this analysis can provide a basis for guiding clinical applications. However, this study also has some limitations. The doses of desmopressin and the types of anticholinergic agents were not completely the same in this article, which may affect our meta-analysis quality. Therefore, our research will need more appropriate high-quality randomized trials to improve the accuracy of results.
Conclusions
In summary, this meta-analysis elucidates that desmopressin combined with anticholinergic agents is more effective in treating NE than desmopressin monotherapy. Both methods are noted to be safe, and the anticholinergic agent does not increase the risk of AEs.
Data availability statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding authors.
Author contributions
TC performed the conceptualization. YY performed the data curation. TC and WS performed the funding acquisition. PL worked on the methodology. TC and YY performed the writing—original draft. WS and PL performed the writing—review and editing. All authors contributed to the article and approved the submitted version.
Funding
The study was funded by the Postgraduate Research & Practice Innovation Program of Jiangsu Province (SJCX22_1814).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bayne AP, Skoog SJ. Nocturnal enuresis: an approach to assessment and treatment. Pediatr Rev. (2014) 35(8):327–35. doi: 10.1542/pir.35-8-327
2. Park SJ, Park JM, Pai KS, Ha TS, Lee SD, Baek M, et al. Desmopressin alone versus desmopressin and an anticholinergic in the first-line treatment of primary monosymptomatic nocturnal enuresis: a multicenter study. Pediatr Nephrol. (2014) 29(7):1195–200. doi: 10.1007/s00467-014-2751-5
3. Butler R, Heron J, Team AS. Exploring the differences between mono- and polysymptomatic nocturnal enuresis. Scand J Urol Nephrol. (2006) 40(4):313–9. doi: 10.1080/00365590600750144
4. Triantafyllidis A, Charalambous S, Papatsoris AG, Papathanasiou A, Kalaitzis C, Rombis V, et al. Management of nocturnal enuresis in Greek children. Pediatr Nephrol. (2005) 20(9):1343–5. doi: 10.1007/s00467-005-1921-x
5. Robson WL. Clinical practice. Evaluation and management of enuresis. N Engl J Med. (2009) 360(14):1429–36. doi: 10.1056/NEJMcp0808009
6. Nevéus T. Pathogenesis of enuresis: towards a new understanding. Int J Urol. (2017) 24(3):174–82. doi: 10.1111/iju.13310
8. Van Herzeele C, Evans J, Eggert P, Lottmann H, Norgaard JP, Vande Walle J. Predictive parameters of response to desmopressin in primary nocturnal enuresis. J Pediatr Urol. (2015) 11(200):e1–8. doi: 10.1016/j.jpurol.2015.03.007
9. Ferrara P, Sannicandro V, Ianniello F, Quattrocchi E, Sbordone A, Petitti T, et al. Attention-deficit/hyperactivity disorder and enuresis: a study about effectiveness of treatment with methylphenidate or desmopressin in a pediatric population. Minerva Pediatr. (2019) 71(2):135–8. doi: 10.23736/S0026-4946.17.04680-1
10. Faraj G, Cochat P, Cavailles ML, Chevallier C. Treatment of isolated nocturnal enuresis: alarm or desmopressin? Arch Pediatr. (1999) 6(3):271–4. doi: 10.1016/s0929-693x(99)80263-2
11. Walle JV, Rittig S, Bauer S, Eggert P, Marschall-Kehrel D, Tekgul S. Practical consensus guidelines for the management of enuresis. Eur J Pediatr. (2012) 171(6):971–83. doi: 10.1007/s00431-012-1687-7
12. Neveus T. Oxybutynin, desmopressin and enuresis. J Urol. (2001) 166:2459–62. doi: 10.1016/S0022-5347(05)65616-9
13. Franco I. Overactive bladder in children. Part 1: pathophysiology. J Urol. (2007) 178(3 Pt 1):761–8; discussion 768. doi: 10.1016/j.juro.2007.05.014
14. Chimenz R, Spinuzza A, Cannavò L, Di Benedetto V, Scuderi MG, Concolino D, et al. Monosymptomatic enuresis: the therapeutic weapons. J Biol Regul Homeost Agents. (2019) 33(5 Suppl. 1):45–51. 31630713.31630713
15. Fagundes SN, Lebl AS, Azevedo Soster L, Sousa E, Silva GJ, Silvares EF, et al. Monosymptomatic nocturnal enuresis in pediatric patients: multidisciplinary assessment and effects of therapeutic intervention. Pediatr Nephrol. (2017) 32(5):843–51. doi: 10.1007/s00467-016-3510-6
16. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. (1986) 7(3):177–88. doi: 10.1016/0197-2456(86)90046-2
17. Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. Wiley-Blackwell (2008). doi: 10.1002/9780470712184.ch1
18. Austin PF, Ferguson G, Yan Y, Campigotto MJ, Royer ME, Coplen DE. Combination therapy with desmopressin and an anticholinergic medication for nonresponders to desmopressin for monosymptomatic nocturnal enuresis: a randomized, double-blind, placebo-controlled trial. Pediatrics. (2008) 122(5):1027–32. doi: 10.1542/peds.2007-3691
19. Azhir A, Gheissari A, Fragzadegan Z, Adebi A. New treatment protocol for primary nocturnal enuresis in children according to ultrasound bladder measurements. Saudi Med J. (2008) 29(10):1475–9. 18946576.18946576
20. Ghanavati PM, Khazaeli D, Amjadzadeh M. A comparison of the efficacy and tolerability of treating primary nocturnal enuresis with solifenacin plus desmopressin, tolterodine plus desmopressin, and desmopressin alone: a randomized controlled clinical trial. Int Braz J Urol. (2021) 47(1):73–81. doi: 10.1590/S1677-5538.IBJU.2019.0448
21. Kazi A, Moorani KN, Zehra S, Zaidi IH. Comparative response of desmopressin versus combination therapy (desmopressin+oxybutynin) in children with nocturnal enuresis. Pak J Med Sci. (2020) 36(6):1263–9. doi: 10.12669/pjms.36.6.1957
22. Kwak KW, Park KH, Baek M. The efficacy of enuresis alarm treatment in pharmacotherapy-resistant nocturnal enuresis. Urology. (2011) 77(1):200–4. doi: 10.1016/j.urology.2010.06.050
23. Lee T, Suh HJ, Lee HJ, Lee JE. Comparison of effects of treatment of primary nocturnal enuresis with oxybutynin plus desmopressin, desmopressin alone or imipramine alone: a randomized controlled clinical trial. J Urol. (2005) 174(3):1084–7. doi: 10.1097/01.ju.0000169160.84418.15
24. Montaldo P, Tafuro L, Rea M, Narciso V, Iossa AC, Del Gado R. Desmopressin and oxybutynin in monosymptomatic nocturnal enuresis: a randomized, double-blind, placebo-controlled trial and an assessment of predictive factors. BJU Int. (2012) 110(8 Pt B):E381–6. doi: 10.1111/j.1464-410X.2011.10918.x
25. Park SJ, Park JM, Pai KS, Ha TS, Lee SD, Baek M, et al. Desmopressin alone versus desmopressin and an anticholinergic in the first-line treatment of primary monosymptomatic nocturnal enuresis: a multicenter study. Pediatr Nephrol. (2014) 29(7):1195–200. doi: 10.1007/s00467-014-2751-5
26. Nevéus T. Nocturnal enuresis-theoretic background and practical guidelines. Pediatr Nephrol. (2011) 26(8):1207–14. doi: 10.1007/s00467-011-1762-8
27. von Gontard A, Eiberg H, Hollmann E, Rittig S, Lehmkuhl G. Molecular genetics of nocturnal enuresis: clinical and genetic heterogeneity. Acta Paediatr. (1998) 87(5):571–8. doi: 10.1080/08035259850158317
28. Nevéus T. Enuretic sleep: deep, disturbed or just wet? Pediatr Nephrol. (2008) 23(8):1201–2. doi: 10.1007/s00467-008-0859-1
29. Tauris LH, Andersen RF, Kamperis K, Hagstroem S, Rittig S. Reduced anti-diuretic response to desmopressin during wet nights in patients with monosymptomatic nocturnal enuresis. J Pediatr Urol. (2012) 8(3):285–90. doi: 10.1016/j.jpurol.2011.03.018
30. Neveus T, Eggert P, Evans J, Macedo A, Rittig S, Tekgül S, et al. Evaluation of and treatment for monosymptomatic enuresis: a standardization document from the International Children’s Continence Society. J Urol. (2010) 183(2):441–7. doi: 10.1016/j.juro.2009.10.043
31. Hjalmas K, Arnold T, Bower W, Caione P, Chiozza LM, von Gontard A, et al. Nocturnal enuresis: an international evidence based management strategy. J Urol. (2004) 171(6 Pt 2):2545–61. doi: 10.1097/01.ju.0000111504.85822.b2
32. Hodges SJ, Atala A. A randomized, double-blind, placebo-controlled trial of anticholinergic medication for nonresponders to desmopressin for monosymptomatic nocturnal enuresis. Curr Urol Rep. (2011) 12(1):1–2. doi: 10.1007/s11934-010-0150-4
33. Maternik M, Krzeminska K, Zurowska A. The management of childhood urinary incontinence. Pediatr Nephrol. (2015) 30(1):41–50. doi: 10.1007/s00467-014-2791-x
34. Alloussi SH, Mürtz G, Lang C, Madersbacher H, Strugala G, Seibold J, et al. Desmopressin treatment regimens in monosymptomatic and nonmonosymptomatic enuresis: a review from a clinical perspective. J Pediatr Urol. (2011) 7(1):10–20. doi: 10.1016/j.jpurol.2010.04.014
35. Zaffanello M, Giacomello L, Brugnara M, Fanos V. Therapeutic options in childhood nocturnal enuresis. Minerva Urol Nefrol. (2007) 59(2):199–205. 17571056.17571056
36. Madersbacher H, Mürtz G. Efficacy, tolerability and safety profile of propiverine in the treatment of the overactive bladder (non-neurogenic and neurogenic). World J Urol. (2001) 19(5):324–35. doi: 10.1007/s003450100223
37. Deshpande AV, Caldwell PH, Sureshkumar P. Drugs for nocturnal enuresis in children (other than desmopressin and tricyclics). Cochrane Database Syst Rev. (2012) 12(12):CD002238. doi: 10.1002/14651858.CD002238.pub2
38. Alloussi S, Mürtz G, Braun R, Gerhardt U, Heinrich M, Hellmis E, et al. Efficacy, tolerability and safety of propiverine hydrochloride in comparison to oxybutynin in children with urge incontinence due to overactive bladder: results of a multicentre observational cohort study. BJU Int. (2010) 106(4):550–6. doi: 10.1111/j.1464-410X.2009.09129.x
Keywords: nocturnal enuresis (NE), desmopressin, anticholinergic agent, randomized controlled trials, meta-analysis
Citation: Cai T, Yao Y, Sun W and Lei P (2023) Desmopressin in combination with anticholinergic agents in the treatment of nocturnal enuresis: a systematic review and meta-analysis. Front. Pediatr. 11:1242777. doi: 10.3389/fped.2023.1242777
Received: 19 June 2023; Accepted: 21 September 2023;
Published: 19 October 2023.
Edited by:
Stephen Shei-dei Yang, Taipei Tzu Chi Hospital, TaiwanReviewed by:
Maria Grazia Scuderi, University of Catania, ItalyEliane Garcez Fonseca, Rio de Janeiro State University, Brazil
© 2023 Cai, Yao, Sun and Lei. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Weigui Sun c3Vud2VpZ3VpMjAyMUAxNjMuY29t Peipei Lei eWFudGFpbGVpcGVpcGVpQDE2My5jb20=
†These authors have contributed equally to this work and share first authorship
 Tong Cai
Tong Cai Yi Yao2,†
Yi Yao2,†