- 1Department of Physical Medicine and Rehabilitation, Chang Gung Memorial Hospital, Taoyuan, Taiwan
- 2Department of Physical Medicine and Rehabiltiation, New Taipei City Municipal Tucheng Hospital, Chang Gung Memorial Hospital, Tucheng branch, New Taipei City, Taiwan
Introduction: To assess the association between a three-month interruption of language intervention programs and the language performance of children with language delay during the COVID-19 pandemic, and to identify which children are more vulnerable to such interruptions.
Materials and methods: This is a retrospective study involving 33 children with language delay who experienced a three-month suspension of language interventions due to the COVID-19 pandemic. We collected their demographic data and language performance scores from the Comprehensive Developmental Inventory for Infants and Toddlers—Diagnostic test (CDIIT-DT) at four different time points. The scores were analyzed using a Wilcoxon Signed Ranks test.
Results: The median scores of language comprehension and overall language ability showed a decreasing trend during the interruption period. However, resuming interventions post-interruption showed a statistically significant increase in all language domains. Children in the borderline delay group (CDIIT-DT DQ scores between 71 and 85) were more likely to experience a decline in their language abilities during the interruption.
Discussion: This is the first study to reveal a decreasing trend in language performance during interruption periods, and highlighting the significance of post-interruption language interventions in facilitating improvements. Furthermore, our study brings attention to the heightened vulnerability of children exhibiting borderline language delay in overall language ability tests when faced with interruptions in language interventions.
1. Introduction
Language delay, a condition in which children fail to meet the expected developmental milestones for their age group in terms of language comprehension and/or expression (1, 2), is common in young children, affecting approximately 5% to 12% of those between the ages of 2 and 5 (3, 4). Early identification and intervention can prevent language delay from interfering with formal education and behavioral adjustment (5). There have been numerous studies conducted to identify risk factors, predictors, and prevalence of language disorders in children (3, 6–10). Additionally, there is a considerable body of research focused on interventions for children with language delay (11–13). Some studies have reported outcome predictors specifically related to children with delayed expressive language (14, 15). However, it is worth noting that there are currently no studies investigating the influence of interrupting interventions on these children. Ethical considerations have made it impractical to interrupt interventions for children with language delay for research purposes. During the COVID-19 pandemic, Taiwan suspended non-emergency medical treatments, including language interventions for three months. This event provided a unique opportunity to study this topic. Our study aimed to explore the relationship between intervention interruptions and language performance in young children with language delay, and to identify which groups of children are more vulnerable to such interruptions.
2. Materials and methods
2.1. Patient inclusion
This retrospective study analyzed 33 children who were diagnosed with language delay or borderline language delay using the Comprehensive Developmental Inventory for Infants and Toddlers—Diagnostic test (CDIIT-DT) (16–20) and underwent language intervention programs at New Taipei City Hospital Tu Cheng Branch between June 2020 and August 2022. All these children experienced a three-month interruption of the program from April 2021 to July 2021 due to a sharp surge in Covid-19 cases in Taiwan.
2.2. Data collection
We collected general data from each study child with language delay, including date of birth, gender, gestational age, birth weight, medical history, family history, multilingual speaking, parents' education level, main caregiver, siblings' condition, early childhood education condition, and other developmental delay conditions. We used the CDIIT-DT to evaluate the language performance of each study child. Raw scores were collected from three subdomains (language comprehension, language expression, and overall language ability) at four different time points: T1—the first assessment before interventions, T2—the last assessment before the three-month interruption, T3—the first assessment after the three-month interruption, and T4—the last assessment obtained from patients' medical records.
2.3. Comprehensive developmental inventory for infants and toddlers (CDIIT)
The CDIIT was created by a multidisciplinary team in Taiwan in 1995 to evaluate the developmental levels of infants and toddlers between 3 and 71 months old, encompassing seven age groups. The CDIIT includes both a diagnostic test (CDIIT-DT) and a screening test (CDIIT-ST). These components are used to assess five developmental areas: motor skills, language skills, cognition, social skills, and self-care skills.
The CDIIT utilizes age-related norms established for the Taiwan population, with a mean score of 100 and a standard deviation of 15. It has been shown to exhibit good reliability and validity in previous studies. The CDIIT is generally supported as a norm-referenced test for evaluating developmental changes of children with developmental delay and outcome measures of pediatric intervention programs (16–19).
2.4. Language intervention programs in Taiwan
In Taiwan, young children are taken to pediatric rehabilitation clinics when there is a suspicion of developmental delay. Caregivers or kindergarten teachers usually notice these delays. If a physician clinically assesses children and identifies a language delay, they are referred to a speech-language pathologist for diagnostic tests. Once the reports confirm a language developmental delay, language intervention programs begin for them once per week.
In the Physical Medicine and Rehabilitation Department of New Taipei City Hospital Tu Cheng Hospital, a single pediatric speech-language pathologist utilized CDIIT-DT to track the language performance of children with language delay during intervention programs every three to six months. The intervention programs were discontinued when the CDIIT-DT indicated that the language delay was no longer present. Subsequently, every six months to a year, the speech-language pathologist utilized CDIIT-ST to track the language development of this children until they reached the age of six.
2.5. Statistical analysis
In this study, we transformed the raw scores into developmental quotient (DQ) scores and utilized the Wilcoxon Signed Ranks test (significance level: p < 0.05) to analyze the differences between various time points. The “W” test statistic in the Wilcoxon Signed Ranks test represents the sum of ranks computed from the absolute differences between paired observations, facilitating the assessment of significant variations between these paired measurements.
To further investigate the CDIIT score regression following intervention interruption, we segregated the children into two groups based on this specific criterion. To examine the potential correlations between each variable and CDIIT score regression, univariate logistic regression and multivariate logistic regression were employed (significance level: p < 0.05). Moreover, for the construction of a prediction model, we applied machine learning algorithms, including KNN, decision tree, and random forest. All analyses were conducted using Python 3, capitalizing on its extensive libraries, and figures were generated using both Python 3 and Prism 9 software.
With regard to ethical considerations, the study was reviewed and approved by the Institutional Review Board of Chang Gung Memorial Hospital, with a waiver of informed consent granted for the use of de-identified data from routine clinical care, ensuring ethical compliance. This study followed the STROBE reporting guideline.
3. Results
3.1. Findings on language comprehension, expression, and overall language ability
Of all the children studied, 19 were male and 14 were female. Characteristics of Study Participants were presented in the Table 1. The median scores of language comprehension, language expression, and overall language ability at different time points are presented in Table 2. Our findings showed that the scores for language comprehension were consistently higher than those for language expression across all time points. Compared with T3, there were statistically significant increases of scores at T4 among all three domains: language comprehension (W = 315, p = 0.0001), language expression (W = 140, p = 0.04), and overall language ability (W = 228, p = 0.001).

Table 1. Characteristics of study participants and comparison of Two groups based on regression Status after intervention interruption.
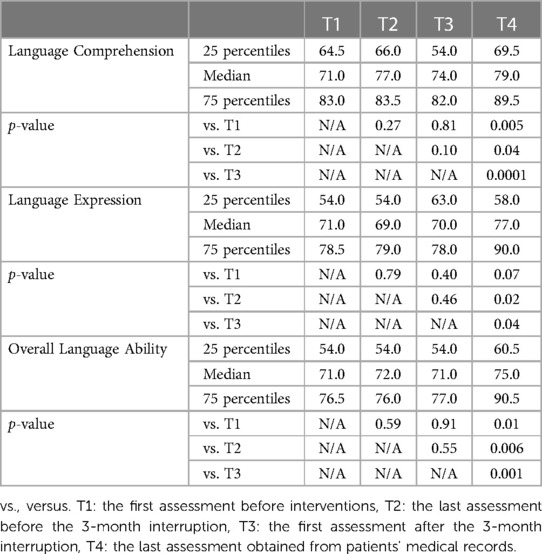
Table 2. Median CDIIT-DT scores and significance levels at different timepoints across language comprehension, expression, and ability domains.
3.2. Trends in CDIIT-DT DQ scores and the impact of intervention interruption
Figure 1 illustrates the trends in CDIIT-DT DQ scores over time for the domains of language comprehension, language expression, and overall language ability. Comprising the three line charts, the trend of language comprehension aligns consistently and synchronously with the overall language ability. The median scores of the two domains, language comprehension and overall language ability, showed a decreasing trend during the interruption. Moreover, resuming the intervention after the interruption showed a statistically significant increase in all language domains.

Figure 1. Trends in CDIIT-DT DQ scores over time. T1: the first assessment before interventions, T2: the last assessment before the 3-month interruption, T3: the first assessment after the 3-month interruption, T4: the last assessment obtained from patients’ medical records. The plot shows the median and interquartile range of CDIIT-DT DQ scores at each timepoint.
3.3. Analysis of individual variable contributions to CDIIT-DT DQ score regression in children with language delay following intervention interruption
To identify key variables that might contribute to CDIIT score regression following intervention interruption, we conducted both univariate logistic regression and multivariate logistic regression analyses. However, none of the variables exhibited statistical significance. The p-values obtained from the univariate logistic regression analysis are detailed in Table 1.
3.4. Identifying vulnerable groups: language ability scores and therapy interruption
To identify which group were more vulnerable to speech therapy interruption, we divided studied children based on their CDIIT-DT DQ scores at T2. We used 15 points as an interval to group these children. We observed a group of children with overall language ability scores ranging from 71 to 85 (borderline delay) at T2. Out of the 15 children in this group, 10 showed a decline in scores between T2 and T3, while 2 maintained stable scores (Figure 2).
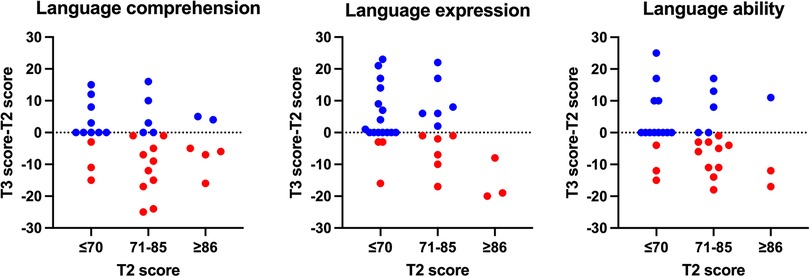
Figure 2. Scatter plot of CDIIT-DT DQ scores and T3-T2 score differences. X-axis: CDIIT-DT DQ score (interval: 10 points), Y-axis: T3-T2 score difference, T2 score: score evaluated at last assessment before the 3-month interruption, T3 score: score evaluated at first assessment after the 3-month of interruption. The red dots represent cases where the CDIIT-DT DQ score at T3 is lower than the score at T2, while the blue dots indicate cases where the CDIIT-DT DQ score at T3 is higher than or equal to the score at T2.
3.5. Constructing a prediction model for CDIIT-DT DQ score regression following intervention interruption
While no key variable was identified as contributing to CDIIT score regression after intervention interruption, we endeavored to construct a prediction model utilizing all available variables. By employing machine learning algorithms such as KNN, decision tree, and random forest, we sought to find the most effective predictive approach. The random forest algorithm emerged as the most accurate, achieving a 70% accuracy rate and an area under the ROC curve of 0.720 (Figure 3).
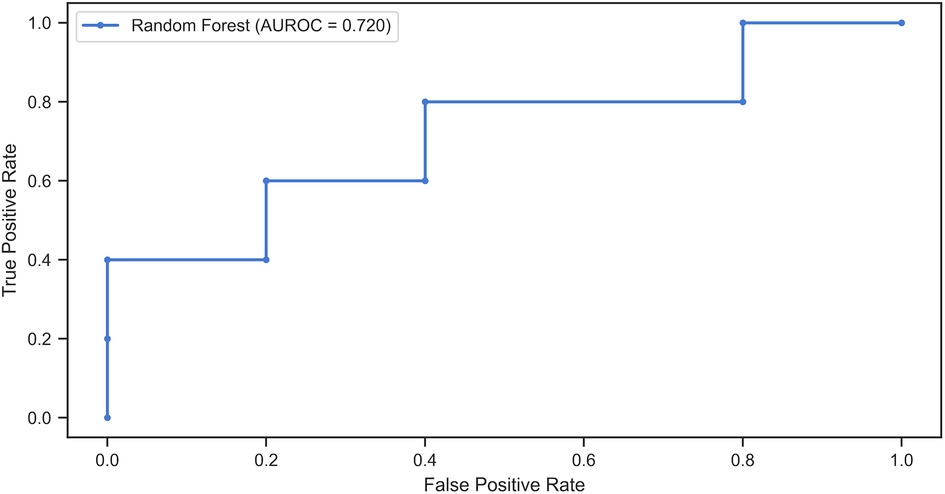
Figure 3. Receiver operating characteristic (ROC) curve of random forest algorithm for predicting CDIIT-DT score regression after intervention interruption. The ROC curve illustrates the performance of the Random Forest algorithm in predicting CDIIT-DT score regression after intervention interruption. The Area Under the ROC Curve (AUROC) was calculated to be 0.720, indicating a moderate level of predictive accuracy.
4. Discussion
This study is the first to examine the effects of interrupting language intervention programs on children with language delay, which occurred during the COVID-19 outbreak in Taiwan in 2021. The unique circumstances presented by the pandemic provided an opportunity to investigate this topic. While it is unlikely that similar situations will arise in the future, the findings of this study remain valuable in understanding the consequences of unexpected disruptions in healthcare services. Despite the numerous studies conducted during the global COVID-19 pandemic focusing on strategies and alternative language intervention methods, such as telepractice speech therapy (21–23), little is known about the specific impact of pandemic-induced intervention interruption on children with language delays. Hackenberg et al. reported a high psychosocial burden experienced by parents of children with speech and language disorders due to therapy pause during the Covid-19 pandemic; however, the effects on their children's speech and language abilities were not addressed (24).
Regarding the relationship between intervention interruption and language performance in children with language delays, our findings indicated a decreasing trend during the interruption period, while post-interruption language interventions were significantly associated with performance improvements. These findings can provide clinicians and parents with an overview of language performance trends following rehabilitation interruption and encourage them to pursue post-interruption interventions. In addition, Hackenberg el. reported parents of children with speech and language disorders had more fears and worries about their children's development (24). In a clinical setting, our study can alleviate parents' psychosocial burden and increase parental compliance and confidence in resuming intervention post-interruption.
Children with developmental delay typically demonstrate stronger language comprehension abilities relative to their language expression skills (25). This observation aligns with our results, which showed that the mean CDIIT-DT scores for language comprehension consistently exceeded those for language expression at all evaluated time points. More notably, language comprehension scores exhibited greater sensitivity to the impact of continuity and discontinuity in rehabilitation programs compared to language expression scores. In our study, the slopes in the line chart depicting language abilities closely paralleled those for language comprehension (Figure 1). These results reinforce the substantial role that language comprehension plays in the speech and language abilities of children. Earlier studies have likewise reported that language comprehension could serve as a reliable predictor of language expression outcomes (3). Therefore, assessing language comprehension is not just crucial for differential diagnosis, but also invaluable for evaluating outcomes in children with speech and language disorders.
To further enhance language comprehension in children with developmental delay, several strategies can be employed (26). These include Enhanced Milieu Teaching (EMT), a conversation-based therapy technique that uses the child's interests as opportunities to model and prompt language use in everyday contexts. Parent-based Video Home Training, where parents are trained in attachment, referencing, relevance, and connectivity of language, can also be beneficial. Techniques such as pausing and expanding in shared book reading and in everyday situations can be used to encourage children to choose or initiate a topic of interest to them. Interactive book reading with expository books and language facilitation strategies can also be employed to focus children's attention on the expository structure and help them construct responses to questions. It is possible that tailoring post-interruption intervention strategies to enhance comprehension could expedite improvements in expressive abilities in overall language abilities.
Our study is also the first to identify which groups of children are more vulnerable to interruptions in language interventions. Our results revealed that among the children with overall language ability scores ranging from 71 to 85 at T2, 10 out of the 15 children in this group exhibited a decline in scores between T2 and T3. Similar results were observed in the language comprehension test (Figure 2). In clinical practice, parents often assume that their child is approaching age-appropriate milestones, overlooking the importance of language intervention during the borderline delay phase. However, our study highlights the particular importance of maintaining ongoing language intervention during this phase, as discontinuation poses a high risk of score regression. Further research is necessary to corroborate this finding, which would provide clinicians and parents with a better understanding of the optimal timing for ceasing interventions.
Although this study is the only one examining young children with language delay who experience interruptions in language intervention programs, there were some limitations to this study. The most notable constraint is the small sample size, which may have curtailed the statistical power of our analyses and led to an absence of statistically significant findings in both univariate and multivariate logistic regression. This small sample size could explain our inability to detect meaningful differences. Nevertheless, our application of a machine learning algorithm enabled us to predict CDIIT score regression after intervention interruption with an accuracy of 70%. We anticipate that expanding the database for model training could enhance this accuracy further. It is essential to note that our findings are preliminary and derived from a small, heterogeneous sample. These initial results emphasize the need for larger and more diverse studies to corroborate and solidify our conclusions.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Institutional Review Board of Chang Gung Memorial Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The Ethics Committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because The use of de-identified data from routine clinical care, ensuring ethical compliance.
Author contributions
Conceptualization, Methodology, Data curation, Formal analysis, Investigation, Writing – original draft, Visualization: S-CH. Supervision: AM-KW. All author contributed to the article and approved the submitted version.
Acknowledgments
The authors gratefully acknowledge the valuable contributions of Heng-An Yeh and Guan-Ting Huang in data extraction. Heng-An Yeh and Guan-Ting Huang, both holding degrees in SLP, are affiliated with the Department of Physical Medicine and Rehabiltiation, New Taipei City Municipal Tucheng Hospital, Chang Gung Memorial Hospital, Tucheng branch, New Taipei City, Taiwan.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Khan I, Leventhal BL. Developmental delay. In: Khan I, Leventhal BL, editors. Statpearls. Treasure Island, FL: StatPearls Publishing (2023).
2. Definitions of Communication Disorders and Variations. American Speech-Language-Hearing Association. (1993). https://www.asha.org/policy/RP1993-00208/ (Accessed December 28, 2022).
3. Sunderajan T, Kanhere SV. Speech and language delay in children: prevalence and risk factors. J Family Med Prim Care. (2019) 8(5):1642–6. doi: 10.4103/jfmpc.jfmpc_162_19
4. Wallace IF, Berkman ND, Watson LR, Coyne-Beasley T, Wood CT, Cullen K, et al. Screening for speech and language delay in children 5 years old and younger: a systematic review. Pediatrics. (2015) 136(2):e448–62. PMID: 26152671. doi: 10.1542/peds.2014-3889
5. Jullien S. Screening for language and speech delay in children under five years. BMC Pediatr. (2021) 21(Suppl 1):362. doi: 10.1186/s12887-021-02817-7
6. Sansavini A, Favilla ME, Guasti MT, Marini A, Millepiedi S, Di Martino MV, et al. Developmental language disorder: early predictors, age for the diagnosis, and diagnostic tools. A scoping review. Brain Sci. (2021) 11(5):654. doi: 10.3390/brainsci11050654
7. Kumar A, Zubair M, Gulraiz A, Kalla S, Khan S, Patel S, et al. An assessment of risk factors of delayed speech and language in children: a cross-sectional study. Cureus. (2022) 14(9):e29623. doi: 10.7759/cureus.29623
8. St Clair MC, Forrest CL, Yew SGK, Gibson JL. Early risk factors and emotional difficulties in children at risk of developmental language disorder: a population cohort study. J Speech Lang Hear Res. (2019) 62(8):2750–71. doi: 10.1044/2018_JSLHR-L-18-0061
9. Yanuarti HP, Rusmil K, Effendi SH. Environment as a risk factor in delayed development in premature, low-birthweight and mild asphyxia children. Pediatr Int. (2014) 56(5):720–5. doi: 10.1111/ped.12333
10. Korrel H, Mueller KL, Silk T, Anderson V, Sciberras E. Research review: language problems in children with attention-deficit hyperactivity disorder—a systematic meta-analytic review. J Child Psychol Psychiatry. (2017) 58(6):640–54. doi: 10.1111/jcpp.12688
11. Law J, Dennis JA, Charlton JJ. Speech and language therapy interventions for children with primary speech and/or language disorders. Cochrane Database Syst Rev. (2017) 2017(1):CD012490. doi: 10.1002/14651858.CD012490
12. Carson L, Baker E, Munro N. A systematic review of interventions for late talkers: intervention approaches, elements, and vocabulary outcomes. Am J Speech Lang Pathol. (2022) 31(6):2861–74. doi: 10.1044/2022_AJSLP-21-00168
13. Roberts MY, Kaiser AP. Early intervention for toddlers with language delays: a randomized controlled trial. Pediatrics. (2015) 135(4):686–93. doi: 10.1542/peds.2014-2134
14. Fisher EL. A systematic review and meta-analysis of predictors of expressive-language outcomes among late talkers. J Speech Lang Hear Res. (2017) 60(10):2935–48. doi: 10.1044/2017_JSLHR-L-16-0310
15. Hawa VV, Spanoudis G. Toddlers with delayed expressive language: an overview of the characteristics, risk factors and language outcomes. Res Dev Disabil. (2014) 35(2):400–7. doi: 10.1016/j.ridd.2013.10.027
16. Liao HF, Pan YL. Test-retest and inter-rater reliability for the comprehensive developmental inventory for infants and toddlers diagnostic and screening tests. Early Hum Dev. (2005) 81(11):927–37. doi: 10.1016/j.earlhumdev.2005.07.008
17. Liao HF, Wang TM, Yao G, Lee WT. Concurrent validity of the comprehensive developmental inventory for infants and toddlers with the bayley scales of infant development-II in preterm infants. J Formos Med Assoc. (2005) 104(10):731–7.16385375
18. Hwang AW, Weng LJ, Liao HF. Construct validity of the comprehensive developmental inventory for infants and toddlers. Pediatr Int. (2010) 52(4):598–606. doi: 10.1111/j.1442-200X.2010.03102.x
19. Tsai YP, Tung LC, Lee YC, Wang YL, Yen YS, Chen KL. Selecting score types for longitudinal evaluations: the responsiveness of the comprehensive developmental inventory for infants and toddlers in children with developmental disabilities. Neuropsychiatr Dis Treat. (2016) 12:1103–9. doi: 10.2147/NDT.S99171
20. Yu TY, Chou W, Chow JC, Lin CH, Tung LC, Chen KL. IQ Discrepancy differentiates levels of fine motor skills and their relationship in children with autism spectrum disorders. Neuropsychiatr Dis Treat. (2018) 14:597–605. doi: 10.2147/NDT.S153102
21. Palomares-Aguilera M, Inostroza-Allende F, Solar LR. Speech pathology telepractice intervention during the COVID-19 pandemic for Spanish-speaking children with cleft palate: a systematic review. Int J Pediatr Otorhinolaryngol. (2021) 144:110700. doi: 10.1016/j.ijporl.2021.110700
22. Tohidast SA, Mansuri B, Bagheri R, Azimi H. Provision of speech-language pathology services for the treatment of speech and language disorders in children during the COVID-19 pandemic: problems, concerns, and solutions. Int J Pediatr Otorhinolaryngol. (2020) 138:110262. doi: 10.1016/j.ijporl.2020.110262
23. Tenforde AS, Borgstrom H, Polich G, Steere H, Davis IS, Cotton K, et al. Outpatient physical, occupational, and speech therapy synchronous telemedicine: a survey study of patient satisfaction with virtual visits during the COVID-19 pandemic. Am J Phys Med Rehabil. (2020) 99(11):977–81. doi: 10.1097/PHM.0000000000001571
24. Hackenberg B, Büttner M, Große L, Martin E, Cordier D, Matthias C, et al. Auswirkungen der COVID-19-Pandemie auf die logopädische Therapie von Kindern mit einer Sprachentwicklungsstörung [Impact of the COVID-19 pandemic on speech therapy for children with Speech and Language Disorders]. Laryngorhinootologie. (2021) German. PMID: 34507370. doi: 10.1055/a-1613-5747 [Epub ahead of print].
25. Fisher EL, Sevcik RA, Romski M. Language comprehension in toddlers with significant developmental delays: an IRT approach. J Commun Disord. (2022) 96:106195. doi: 10.1016/j.jcomdis.2022.106195
Keywords: developmental language delay, language therapy, disruption of language intervention, language ability, COVID-19
Citation: Hsu S-C and Wong AM-K (2023) Association between interruption of intervention and language performance in young children with language delay—a cohort study during COVID-19 pandemic. Front. Pediatr. 11:1240354. doi: 10.3389/fped.2023.1240354
Received: 14 June 2023; Accepted: 17 August 2023;
Published: 15 September 2023.
Edited by:
Daniel Holzinger, Hospitaller Brothers of Saint John of God Linz, AustriaReviewed by:
J. Carolyn Graff, University of Tennessee Health Science Center (UTHSC), United StatesMaria Fernanda Lara-Diaz, National University of Colombia, Colombia
© 2023 Hsu and Wong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alice May-Kuen Wong d2FsaWNlQGNnbWgub3JnLnR3
 Shao-Chih Hsu
Shao-Chih Hsu Alice May-Kuen Wong1,2*
Alice May-Kuen Wong1,2*