- 1Department of Pediatric Gastroenterology, School of Medicine, Ankara University, Ankara, Turkey
- 2Clinic of Pediatric Gastroenterology, Istanbul Sisli Hamidiye Etfal Training and Research Hospital, Istanbul, Turkey
- 3Department of Pediatrics, Afyonkarahisar Health Sciences University, Afyonkarahisar, Turkey
- 4Clinic of Pediatric Gastroenterology, Istanbul Kanuni Sultan Suleyman Training and Research Hospital, Istanbul, Turkey
- 5Clinic of Pediatric Gastroenterology, Adana City Training and Research Hospital, Adana, Turkey
- 6Department of Pediatric Allergy and Immunology, Faculty of Medicine, Istinye University, Istanbul, Turkey
- 7Department of Pediatric Gastroenterology, Faculty of Medicine, Firat University, Elazig, Turkey
- 8Department of Pediatric Allergy, Faculty of Medicine, Hacettepe University, Ankara, Turkey
- 9Department of Pediatric Immunology and Allergy, Faculty of Medicine, Zonguldak Bulent Ecevit University, Zonguldak, Turkey
- 10Clinic of Pediatric Immunology and Allergy, Health Sciences University Dr. Sami Ulus Gynecology, Obstetrics and Child Health and Diseases Training and Research Hospital, Ankara, Turkey
- 11Clinic of Pediatric Gastroenterology, Istanbul Umraniye Training and Research Hospital, Istanbul, Turkey
- 12Department of Pediatric Gastroenterology, Faculty of Medicine, Gazi University, Ankara, Turkey
- 13Clinic of Pediatric Gastroenterology, Istanbul Bakirkoy Dr. Sadi Konuk Training and Research Hospital, Istanbul, Turkey
- 14Department of Pediatric Gastroenterology, Faculty of Medicine, Gaziantep University, Gaziantep, Turkey
- 15Clinic of Pediatric Gastroenterology, Samsun Training and Research Hospital, Samsun, Turkey
- 16Department of Pediatric Gastroenterology, Faculty of Medicine, Kirikkale University, Kirikkale, Turkey
- 17Abbott Nutrition, Abbott Laboratories, Istanbul, Turkey
Objective: To evaluate growth, tolerance and safety outcomes with use of an extensively hydrolyzed casein-based formula (eHCF) in infants with cow’s milk protein allergy (CMPA).
Methods: A total of 226 infants (mean ± SD age: 106.5 ± 39.5 days, 52.7% were girls) with CMPA who received eHCF comprising at least half of the daily dietary intake were included. Data on anthropometrics [weight for age (WFA), length for age (LFA) and weight for length (WFL) z-scores] were recorded at baseline (visit 1), while data on infant feeding and stool records, anthropometrics and Infant Feeding and Stool Patterns and Formula Satisfaction Questionnaires were recorded at visit 2 (on Days 15 ± 5) and visit 3 (on Days 30 ± 5).
Results: From baseline to visit 2 and visit 3, WFA z-scores (from −0.60 ± 1.13 to −0.54 ± 1.09 at visit 2, and to −0.44 ± 1.05 at visit 3, p < 0.001) and WFL z-scores (from −0.80 ± 1.30 to −0.71 ± 1.22 at visit 2, and to −0.64 ± 1.13 at visit 3, p = 0.002) were significantly increased. At least half of infants never experienced irritability or feeding refusal (55.7%) and spit-up after feeding (50.2%). The majority of mothers were satisfied with the study formula (93.2%), and wished to continue using it (92.2%).
Conclusions: In conclusion, eHCF was well-accepted and tolerated by an intended use population of infants ≤ 6 months of age with CMPA and enabled adequate volume consumption and improved growth indices within 30 days of utilization alongside a favorable gastrointestinal tolerance and a high level of parental satisfaction.
Introduction
Cow’s milk protein allergy (CMPA), a reproducible clinically abnormal reaction to cow’s milk protein (CMP), is a common food allergy in the pediatric age (1, 2). CMPA usually presents within the first six months of life with gastrointestinal, cutaneous, and/or respiratory manifestations or anaphylaxis (1–3).
The principles of CMPA treatment include avoidance of CMP in the mothers of breastfed infants and the provision of substitute formulae adapted to CMPA dietary management in terms of allergic and nutritional safety in formula-fed infants (2–7). Extensively-hydrolyzed casein-based infant formulas (eHCF) with demonstrated hypoallergenicity and favorable tolerance are therefore recommended by guidelines as a first line treatment for infants and children with confirmed CMPA (4–8).
The safety and efficacy of extensively hydrolyzed formula (eHFs) compared to other treatment formulas has been emphasized particularly in terms of the decreased incidence of CMPA-related symptoms and better tolerance (9, 10). However, CMPA may also result in growth retardation due to several factors including the impact of the allergic manifestations on nutritional status, increased metabolic needs, disrupted sleep patterns, gut inflammation causing impaired nutrient bioavailability, and a restricted diet (5, 11–15).
In this regard, eHFs should also be investigated for their growth adequacy in children with CMPA, since children with CMPA are considered to be at increased risk of poor growth (5, 11, 14, 15). Indeed, the assessment of growth and development with eHFs is considered to be a critical safety parameter, given the likelihood of slower weight and length growth with eHFs compared to the amino acid-based formula in the setting of CMPA (16–18).
However, while the efficacy and tolerability of eHCF in the management of infants and children with CMPA have been demonstrated, its suitability for growth in infants with CMPA has not been sufficiently investigated (11, 17, 19–21).
This prospective observational multicenter study aimed to evaluate the utility of an eHCF in an intended-use population of infants with CMPA in terms of the growth indices, gastrointestinal intolerance and safety as well as the parent’s assessment of infant feeding and stool patterns and formula satisfaction.
Material and methods
Study population
A total of 226 infants (mean ± SD age: 106.5 ± 39.5 days, 52.7% were girls) with CMPA who received eHCF comprising at least half of the daily dietary intake were included in this non-randomized, single-arm, multicenter clinical trial conducted at 35 pediatric gastroenterology and allergy centers across Turkey. The study sample was composed of infants (aged 0–180 days) with newly diagnosed CMPA where an eHCF was deemed appropriate by the healthcare professional for at least 50% of their feeding with breastfeeding comprising the other half, as confirmed by parents’ records on daily frequency of feeding. None of the infants were on the complementary feeding. Although 320 infants were initially enrolled, the final study population was composed of 226 infants with the exclusion of 94 infants due to protocol violation and/or loss to follow up (n = 72), discontinuation of the formula due to dissatisfaction (n = 13), consent withdrawal (n = 3), adverse event development (n = 1) and other reasons (n = 5).
Written informed consent was obtained from the parent/legal guardian of each subject following a detailed explanation of the objectives and protocol of the study, which was conducted in accordance with the ethical principles stated in the “Declaration of Helsinki” and approved by the Ankara University Faculty of Medicine Clinical Research Ethics Committee (Date of Approval: 24/07/2017; Reference number/Protocol No: 12-703-17).
Maternal diet
Mothers followed a CMP-free diet by avoiding all milk and milk products like cheese, yogurt and butter as well as the foods that may contain traces of milk, from the maternal diet and received calcium supplements in accordance with the qualified dietary counseling.
Assessments
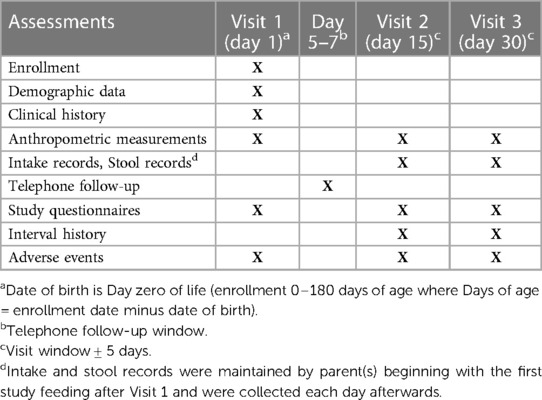
Data on demographics, clinical history and anthropometrics [z-scores for weight for age (WFA), length for age (LFA) and weight for length (WFL)] were recorded at baseline (visit 1). The infant feeding, spit-up (mild vomiting or regurgitation of milk, formula and saliva in small amounts) or vomiting (throwing up of the stomach contents with force and muscle contractions) and stool records, anthropometrics and study questionnaires (Infant Feeding and Stool Patterns and Formula Satisfaction Questionnaires) as well as safety (adverse events) were evaluated at visit 2 (on days 15 ± 5) and visit 3 (on days 30 ± 5). Outcome measures included infant growth, gastrointestinal tolerance, safety and parental satisfaction with eHCF in the overall study population, as well as in the subgroups of exclusively formula-fed and mixed-fed infants (Table 1).
Infant growth was assessed based on the maintenance of anthropometric z-scores (using WHO reference data) during the study (22). Formula intake and stool records were requested to be kept by the mother beginning with the first study formula feeding after Visit 1 and were collected daily thereafter. Gastrointestinal tolerance and compliance of the study product were also assessed along with parental satisfaction via responses to the Infant Feeding and Stool Patterns and Formula Satisfaction Questionnaires.
Growth indices
Anthropometric measurements included body weight (kg) and length (cm) along with the calculation of mean z-scores for WFA, LFA and WFL. At each study visit, body weight was measured using the same digital baby weight scale (10 g precision) and height measurement was performed using a 1-m length measuring tape (0.1 cm precision), while the use of an infant stadiometer was at the discretion of the physician.
Statistical analysis
Statistical analysis was made using IBM SPSS Statistics for Windows, Version 23.0 (IBM Corp., Armonk, NY). Chi-square (χ2) test was used for the comparison of categorical data, while numerical data were analyzed using the Friedman test. Change over time for continuous data was evaluated by Wilcoxon signed rank test or paired t-test. Change over time for categorical data was analyzed using McNemar’s test or Bowker’s test. Data were expressed as mean ± SD (standard deviation), median (minimum-maximum) and percent (%) where appropriate. A p-value <0.05 was considered statistically significant.
Results
Baseline characteristics
Mean ± SD age of infants was 106.5 ± 39.5 days, and 52.7% were girls.
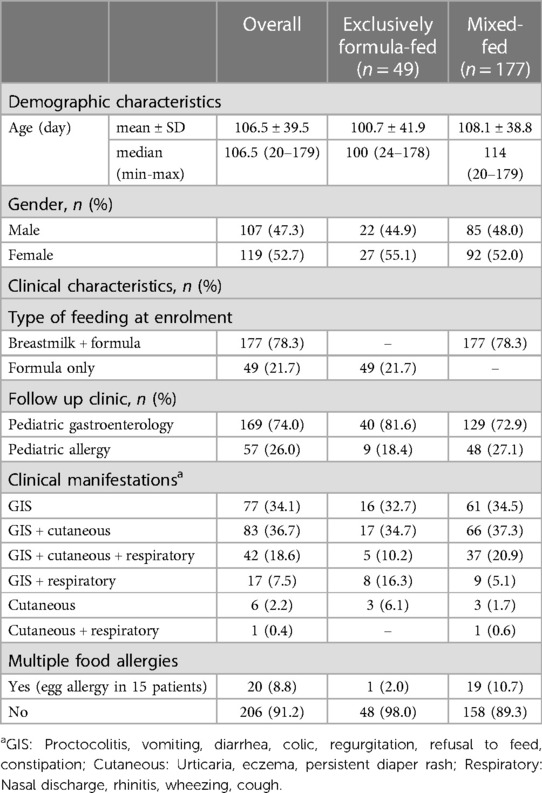
At the time of enrolment, 78.3% of infants were fed by breast milk (with avoidance of CMP in the mothers) + eHCF (mixed-fed group), while 21.7% were exclusively fed by eHCF (exclusively formula-fed group) (Table 2).
Overall, most of infants presented with gastrointestinal manifestations either alone (34.1%) or together with cutaneous (36.7%) complaints, regardless of the feeding subgroup (exclusively formula-fed or mixed-fed) (Table 2).
Respiratory complaints were more likely to accompany the gastrointestinal + cutaneous complaints in the mixed-fed group (20.9% vs. 10.2%) and the gastrointestinal complaints (16.3% vs. 5.1%) in the exclusively-fed group (Table 2).
Multiple food allergies (≥2 food groups) were evident in 20 (8.8%) infants overall (egg allergy in most cases), which was more likely in the mixed-fed vs. exclusively formula-fed group (10.7% vs. 2.0%) (Table 2).
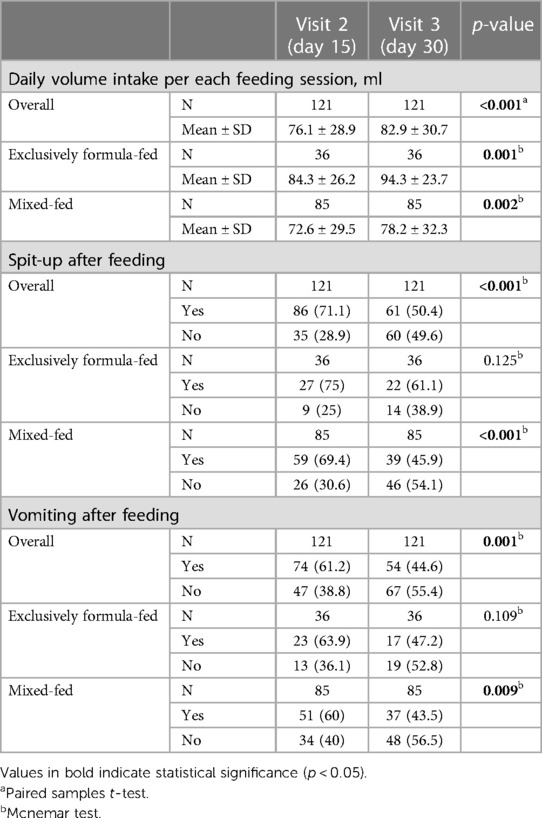
Daily volume intake per each feeding session and spit-up or vomiting after feeding
Daily volume intake per each feeding significantly increased from visit 2 to visit 3 in the overall study population (76.1 ± 28.9 vs. 82.9 ± 30.7 ml/per feeding/per day, p < 0.001), and in both exclusively formula-fed (84.3 ± 26.2 vs. 94.3 ± 23.7 ml/per feeding/per day, p = 0.001) and mixed-fed (72.6 ± 29.5 vs. 78.2 ± 32.3 ml/per feeding/per day, p = 0.002) groups (Table 3).
Overall, the frequency of spit-up after feeding (71.1% to 50.4%, p < 0.001) and vomiting after feeding (61.2% to 44.6%, p = 0.001) were significantly decreased from visit 2 to visit 3, particularly in the mixed-fed group (p < 0.001 and p = 0.009, respectively) (Table 3).
Anthropometrics
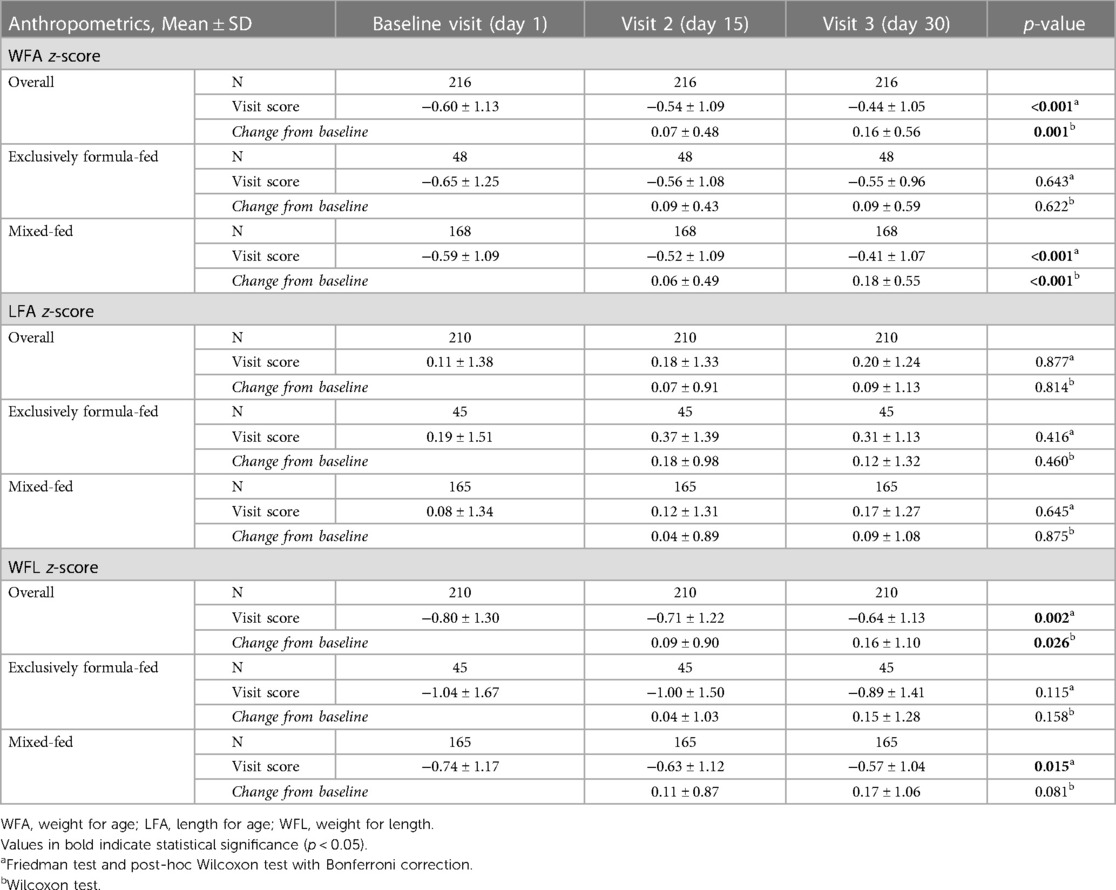
Overall, WFA z-scores were significantly increased from baseline to visit 2 and visit 3 (from −0.60 ± 1.13 to −0.54 ± 1.09 at visit 2, and to −0.44 ± 1.05 at visit 3, p < 0.001). Mean ± SD WFA z-scores (p < 0.05) and change from baseline (0.16 ± 0.56 vs. 0.07 ± 0.48, p = 0.001) were also significantly higher at visit 3 vs. visit 2 (Table 4, Figure 1).

Figure 1. Weight for age (WFA) Z-scores from baseline to visit 3, *p < 0.001 compared to baseline visit.
In the mixed-fed group, mean ± SD WFA z-scores were significantly increased from baseline (−0.59 ± 1.09) to visit 2 (−0.52 ± 1.09, p < 0.001) and visit 3 (−0.41 ± 1.072, p < 0.001), as well as from visit 2 to visit 3 (p < 0.05). In the exclusively formula-fed group baseline mean ± SD WFA z-scores (−0.65 ± 1.25) were maintained at visit 2 (−0.56 ± 1.08) and visit 3 (−0.55 ± 0.96) (p = 0.643) (Table 4).
Overall, WFL z-scores were significantly increased from baseline to visit 2 and visit 3 (from −0.80 ± 1.30 to −0.71 ± 1.22 at visit 2, and to −0.64 ± 1.13 at visit 3, p = 0.002). Mean ± SD change from baseline (0.16 ± 1.10 vs. 0.09 ± 0.90, p = 0.026) was also significantly higher at visit 3 vs. visit 2 (Table 4, Figure 2).
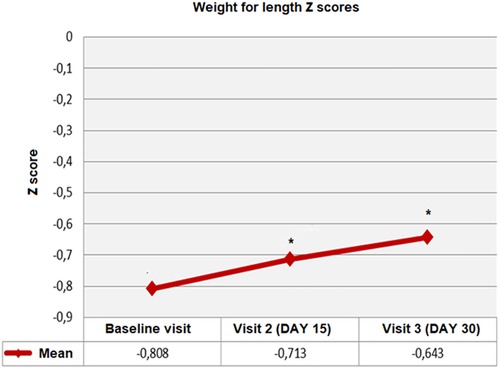
Figure 2. Weight for length (WFL) Z-scores from baseline to visit 3, *p < 0.01 compared to baseline visit.
In the mixed-fed group, mean ± SD WFL z-scores were significantly increased from baseline to follow-up visits (from −0.74 ± 1.173 at baseline to −0.63 ± 1.12 and −0.57 ± 1.04 at visit 2 and 3 respectively; p = 0.015). In the exclusively formula-fed group, baseline WFL z-scores were maintained at visit 2 and visit 3 (−1.04 ± 1.67 at baseline and −1.00 ± 1.50 and −0.89 ± 1.41 at follow-up visits, respectively; p = 0.115) (Table 4).
No significant change was noted in LFA z-scores from baseline to follow-up visits overall or in mixed-fed and exclusively formula-fed groups (Table 4).
Perianal problems, infant feeding and stool patterns
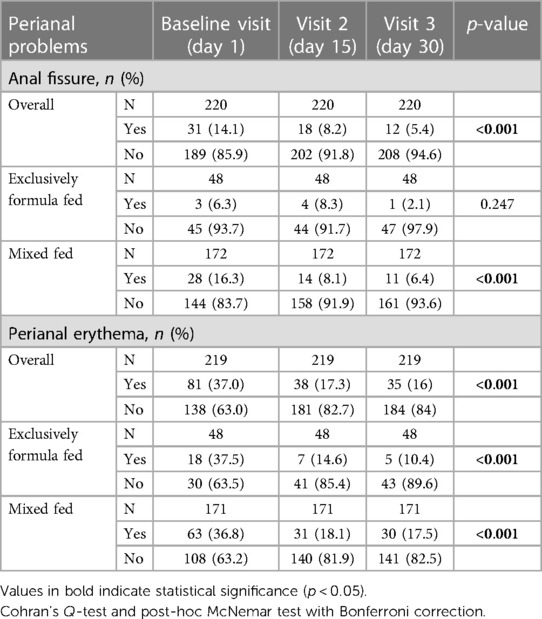
When compared to baseline, the percentage of infants with anal fissure (14.1% vs. 8.2% and 5.4%, respectively, p < 0.001) and perianal erythema (37.0% vs. 17.3% and 16.0%, respectively, p < 0.001) significantly decreased at visit 2 and visit 3 (Table 5).
The amelioration of perianal erythema at follow-up visits was significant in both exclusively formula-fed (p < 0.001) and mixed-fed (p < 0.001) groups, whereas the significant decrease in anal fissure during follow-up visits was only evident in the mixed-fed group (p < 0.001) (Table 5).
Visit 3 data on “Infant Feeding and Stool Patterns” related to compliance and gastrointestinal tolerance revealed that at least half of parents perceived that their infants never fussed or resisted the bottle while being fed the formula (55.7%) and never spit-up after feeding (50.2%) along with presence of normal stool consistency always in 54.7%. No significant change was noted between visit 2 and visit 3 in terms of these compliance and gastrointestinal tolerance characteristics in formula-fed and mixed-fed groups (Table 6).
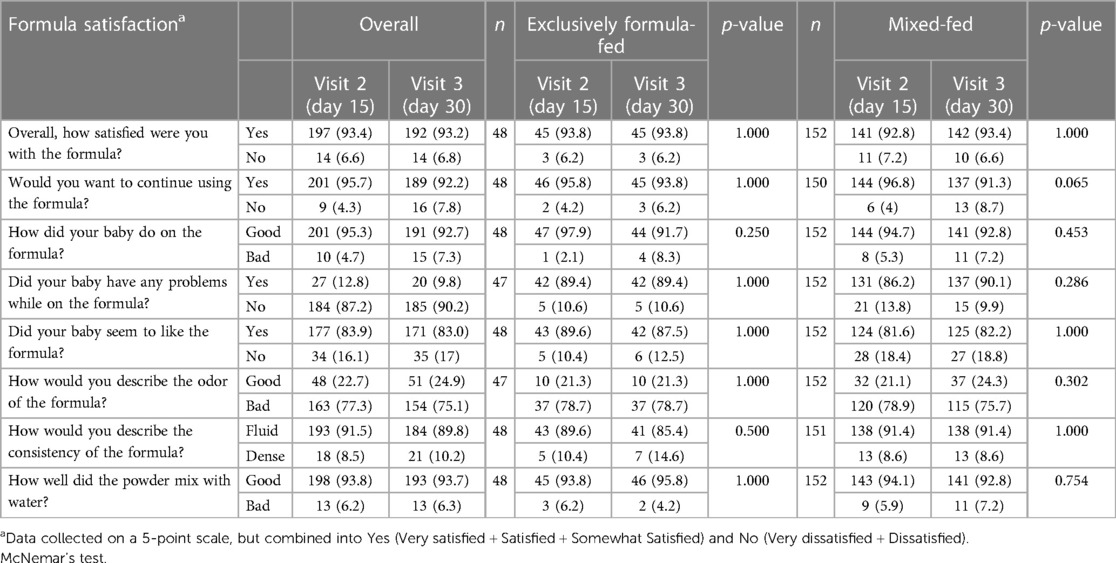
Formula satisfaction
According to “Formula Satisfaction Questionnaire”, the majority of parents were satisfied with the study formula (93.2%), and reported their infants did well or very well on the formula (92.7%) with no problems encountered during formula feeding (90.2%), and wished to continue using it (92.2%). No significant change was noted between visit 2 and visit 3 in terms of formula satisfaction in formula-fed and mixed-fed groups (Table 7).
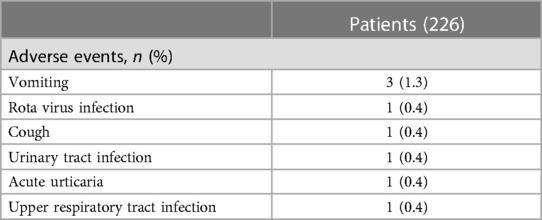
Adverse events
Adverse events were reported in 8 infants including vomiting in 3 of them (Table 8).
Discussion
Our findings revealed that the use of eHCF in infants with CMPA during the first 6 months of life was associated with a normal growth profile, improved WFA and WFL z-scores, favorable GI tolerance and a high level of parental satisfaction. There was an increase in daily frequency and amount of formula consumption over time, without a concomitant increase in the rate of spit-up and/or vomiting. At least half of the infants never experienced irritability or feeding refusal and spit-up after feeding and had normal stool consistency, while the majority of mothers considered the study formula to be satisfactory. Considering the outcomes in exclusively formula-fed and mixed-fed groups, both feeding patterns were associated with an increase in daily volume intake per each feeding, amelioration of perianal erythema, improved compliance and gastrointestinal tolerance, and high parental satisfaction with the formula. Nonetheless, the mixed-fed group seemed to be more advantageous particularly in terms of improvement in WFA and WFL z-scores, a decrease in frequencies of spit-up and vomiting after feeding, and a decrease in anal fissure.
Similarly, in a prospective multicenter trial in 30 infants (aged <12 months) with CMPA who received a thickened eHCF for four months, the authors reported that eHCF was tolerated by more than 90% of infants and was associated with significantly increased WFA, LFA and WFL z-scores during the study period (11). The authors also noted a significant increase in the percentage of infants having normal stool consistency (from 66.7% at inclusion to 90.0%) and a decrease in the rate of vomiting by 50% after 14 days of feeding along with no adverse event related to the eHCF (19). Hence, the thickened eHCF is considered to be a hypoallergenic, efficient and safe alternative in children with CMPA as associated with improvement of growth indices and absence of related adverse events (11).
The association of eHCF feeding with an improvement in growth indices was reported in other studies in infants with CMPA, and eHCF feeding was considered to enable growth normalization in line with WHO standards (19, 20, 21). Demonstrating growth in line with WHO standards for infants consuming eHCF is important given that CMPA is frequently associated with a growth deficit due to reduced bioavailability or loss of nutrients in the gastrointestinal tract, increased metabolic needs as well as the inadequate elimination diet (5, 11, 14, 15, 20, 23).
Also, in a 12-month growth and accession of tolerance study in 116 infants with CMPA, the authors reported that eHF was associated with significantly improved WFA z-score, while the growth improvement was more likely in infants with one symptom at diagnosis, those who had a gastrointestinal symptom, and those with an allergy to only CMP (19). This seems notable given the predominance of gastrointestinal manifestations either alone or together with other complaints and the presence of allergy to only CMP in a majority of infants in the present cohort.
In the current study, eHCF-based growth improvement was evident for WFA and WFL z-scores with no significant change from baseline to day 30 for LFA scores, supporting that weight gain occurs more rapidly and earlier than linear growth after nutritional interventions with alternative formulae (19, 24).
Bitter taste and poor digestive comfort including regurgitations are the two problems frequently encountered with use of eHF (11, 25–28). In the current study, >80% of parents reported that infants liked the formula, and at least half of infants never experienced feeding refusal and spit-up after feeding, along with the increase in daily amount of formula consumption over time. Hence, our findings support the previously reported high parent satisfaction rates with eHCF, particularly in terms of their child’s acceptance of the formula’s taste (11).
Moreover, in addition to enabling normal stool consistency with no bloating or flatulence in at least half of infants, eHCF also revealed feelings of satiety, normal feeding time and soft and formed stools and no difficulty in defecating in the majority of our study population along with a significant decrease in the rate of anal fissure and perianal erythema. Notably, the mixed-fed group had certain advantages over the exclusively formula-fed group in terms of improvement in WFA and WFL z-scores, decrease in the frequency of spit-up and/or vomiting after feeding and amelioration of anal fissure over time, despite the higher likelihood of having multiple food allergies and gastrointestinal + cutaneous + respiratory manifestations at the initial presentation.
Data from small case series indicated up to 10% of children with CMPA could react adversely to eHCF (29, 30). Our findings indicate adverse events in 8(3.5%) of infants with vomiting as the leading event (3 of 8 patients), while parents reported no additional problems during feeding in 87.2% and 90.2% of infants on day 15 and day 30 of eHCF intervention, respectively. In a study among infants with CMPA receiving eHCF, 33 AEs were reported in 24 patients including respiratory infections (48.5%) and gastroenteritis (30.0%), while none were related to the tested formula nor led to feeding discontinuation of the tested formula (19). Likewise, in a study with 220 children with CMPA who received eHCF or eHCF plus LGG, authors reported no adverse reactions to any of the study formulas (31).
In a systematic review of 15 RCTs in 1,285 children with CMPA on the use of a formula containing eHF (whey and/or casein) or any other formula for CMPA management, the authors concluded that eHF products appear to be well-tolerated by most children with CMPA (32). However, they also noted that there are numerous methodological issues preventing to reach a conclusion regarding the benefit of one formula over another formula, such as the differences in outcome measures and their definitions, lack of pre-specified protocols and/or trial registration, and poor reporting of adverse events (32). Hence, the authors emphasized the need for standardized treatment protocols and a standardized set of outcomes to be measured and reported in clinical trials addressing the utility of specialized milk formula for the management of CMA (32).
The major strength of this observational study seems to be the nationwide inclusion of infants with CMPA from 35 pediatric gastroenterology and allergy centers across Turkey which enables our findings to be likely to be generalizable with a representative sample of the overall CMPA population. In addition, the current study provides evidence on the management of infants with CMPA via a comprehensive assessment including not only the gastrointestinal tolerance and safety of the eHCF but also the infant growth, infant feeding and stool patterns and the parental satisfaction with the formula, both in exclusively formula-fed and mixed-fed infants. However, certain limitations to this study should be considered. First, single-arm design with no control group is an important limitation. Second, the short duration of follow up is another limitation. Third, while not included within the scope of the current study, data on changes in individual presenting symptoms over the course of feeding with eHCF might extend the knowledge achieved in the current study.
Conclusion
In conclusion, our findings indicate that eHCF was well-accepted and tolerated by an intended-use population of infants with CMPA during the first 6 months of life and enabled adequate volume consumption and improved growth indices even within 30 days of utilization alongside favorable gastrointestinal tolerance and a high level of parental satisfaction. Future longer-term and larger-scale studies are warranted to assess the utility of eHCF in infants with CMPA in terms of growth indices, development of tolerance and amelioration of gastrointestinal and allergy symptoms.
Data availability statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Ankara University Faculty of Medicine Clinical Research Ethics Committee (Date of Approval: 24/07/2017; Reference number/Protocol No: 12-703-17). Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
All authors contributed to data analysis, drafting, or revising the article, gave final approval for the version to be published, agreed to the submitted journal, and agreed to be accountable for all aspects of the work. All authors contributed to the article and approved the submitted version.
ISPAT Study Group
Ankara University School of Medicine, Ankara; Aydan Kansu (Pediatric Gastroenterology), Ceyda Tuna Kırsaclioglu (Pediatric Gastroenterology), Adana State Training and Research Hospital, Adana; Didem Gulcu Taskin (Pediatric Gastroenterology), Afyonkarahisar Health Sciences University Faculty of Medicine, Afyonkarahisar; Aysegul Bukulmez (Pediatric Gastroenterology), Lutfi Molon (Pediatrics), Akdeniz Univesity Faculty of Medicine, Antalya; Reha Artan (Pediatric Gastroenterology), Aysen Bingol (Pediatric Immunology and Allergy), Arzu Aras (Pediatric Gastroenterology), Dilara Kocacik Uygun (Pediatric Immunology and Allergy), Aygen Yilmaz (Pediatric Gastroenterology), Ankara Diskapi Children’s Hospital, Ankara; Arzu Meltem Demir (Pediatric Gastroenterology), Burcu Berberoglu Ates (Pediatric Gastroenterology), Ankara Sami Ulus Maternity and Child Health and Diseases Training and Research Hospital, Ankara; Ilknur Bostanci (Pediatric Immunology and Allergy), Aysegul Ertugrul (Pediatric Immunology and Allergy), Ezgi Ulusoy Severcan (Pediatric Immunology and Allergy), Ankara Training and Research Hospital, Ankara; Emine Vezir (Pediatric Gastroenterology), Hayriye Hizarcioglu Gulsen (Pediatric Gastroenterology), Ankara Yildirim Beyazit University Faculty of Medicine, Ankara; Samil Hizli (Pediatric Gastroenterology), Balikesir University Faculty of Medicine, Balikesir; Sezin Akman (Pediatric Gastroenterology), Gulce Baranli (Pediatric Gastroenterology), Baskent University Hospital, Konya; Bahar Gokturk (Pediatric Immunology and Allergy), Erzurum Regional Training and Research Hospital, Erzurum; Asuman Nur Karhan (Pediatric Gastroenterology), Firat University Faculty of Medicine, Elazig; Yasar Dogan (Pediatric Gastroenterology), Hatice Altug Demirol (Pediatric Gastroenterology), Gazi University Faculty of Medicine, Ankara; Buket Dalgic (Pediatric Gastroenterology), Hakan Ozturk (Pediatric Gastroenterology), Gaziantep University Faculty of Medicine, Gaziantep; Ahmet Basturk (Pediatric Gastroenterology), Hacettepe University Faculty of Medicine, Ankara, Hasan Ozen (Pediatric Gastroenterology), Bulent Enis Sekerel (Pediatric Allergy), Betul Buyuktiryaki (Pediatric Allergy), Ersin Gümüş (Pediatric Gastroenterology), Health Sciences University Bursa Yuksek Ihtisas Training and Research Hospital, Bursa; Kaan Demiroren (Pediatric Gastroenterology), Havva Hasret Cagan (Pediatric Gastroenterology), Inonu University Faculty of Medicine, Malatya Fatma Ilknur Varol (Pediatric Gastroenterology), Senay Kenc (Pediatric Gastroenterology), Istanbul Atakent Acibadem Hospital, Istanbul; Vildan Ertekin (Pediatric Gastroenterology), Istanbul Bakirkoy Sadi Konuk Training and Research Hospital, Istanbul; Hasret Ayyildiz (Pediatric Gastroenterology), Lida Bülbül (Pediatric Gastroenterology), Istanbul Esenler Maternity and Child Health and Diseases Hospital; Istanbul; Mahmut Caner Us, Erkan Akkuş, Istanbul Goztepe Training and Research Hospital, Istanbul; Mustafa Arga (Pediatric Allergy), Ozlem Cavkaytar (Pediatric Allergy), Istanbul Okmeydani Training and Research Hospital, Istanbul; Birol Ozturk (Pediatric Gastroenterology), Istanbul Sisli Hamidiye Etfal Training and Research Hospital, Istanbul; Aysenur Kaya (Pediatric Immunology and Allergy), Nafiye Urganci (Pediatric Gastroenterology), A. Merve Usta (Pediatric Gastroenterology), Lutfiye Sahin Keskin (Pediatric Gastroenterology), Gokce Kuru (Pediatric Gastroenterology), Istanbul Umraniye Training and Research Hospital, Istanbul; Nelgin Gerenli (Pediatric Gastroenterology), Esra Polat (Pediatric Gastroenterology), Istanbul University Cerrahpasa Faculty of Medicine, Istanbul; Tufan Kutlu (Pediatric Gastroenterology), Hasan Karakas (Pediatric Gastroenterology), Kanuni Sultan Suleyman Training and Research Hospital, Istanbul; Gunsel Kutluk (Pediatric Gastroenterology), Karadeniz Teknik University Faculty of Medicine, Trabzon Murat Cakir (Pediatric Gastroenterology), Elif Sag (Pediatric Gastroenterology), Kirikkale University Faculty of Medicine, Kirikkale; Hacer Fulya Gulerman (Pediatric Gastroenterology), Zeynep Arslan (Pediatric Gastroenterology), Dilek Azkur (Pediatric Gastroenterology), Kocaeli University Faculty of Medicine, Kocaeli; Aysen Uncuoglu Aydogan (Pediatric Gastroenterology), Nihal Uyar Aksu (Pediatric Gastroenterology), Konya Necmettin Erbakan University Meram Faculty of Medicine, Konya; Sukru Nail Guner (Pediatric Allergy), Hasan Kapakli (Pediatric Allergy), Konya Selcuk University Faculty of Medicine, Konya; Halil Haldun Emiroglu (Pediatric Gastroenterology), Mehmet Akif Agir (Pediatric Gastroenterology), Meltem Gumus (Pediatric Gastroenterology), Alaaddin Yorulmaz (Pediatric Gastroenterology), Pamukkale University Faculty of Medicine, Denizli; Halil Kocamaz (Pediatric Gastroenterology), Ebru Arik Yilmaz (Pediatric Immunology and Allergy), Eda Didem Kayakiran (Pediatric Gastroenterology), Samsun Training and Research Hospital, Samsun; Mahir Igde (Pediatric Immunology and Allergy), Ozlem Yuce Kirmemiş (Pediatric Immunology and Allergy), Trabzon Kanuni Training and Research Hospital, Trabzon Aysegul Akan (Pediatric Immunology and Allergy), Zonguldak Bulent Ecevit University Faculty of Medicine, Zonguldak; Mutlu Yuksek (Pediatric Immunology and Allergy), Aysugul Alptekin Sarioglu, Simge Erdogan, Abbott Nutrition, Abbott Laboratories.
Funding
This work was supported by Abbott Nutrition Turkey.
Conflict of interest
AS and SE are Abbott employees.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Lifschitz C, Szajewska H. Cow’s milk allergy: evidence-based diagnosis and management for the practitioner. Eur J Pediatr. (2015) 174(2):141–50. doi: 10.1007/s00431-014-2422-3
2. Kansu A, Yüce A, Dalgıç B, Şekerel BE, Çullu-Çokuğraş F, Çokuğraş H. Consensus statement on diagnosis, treatment and follow-up of cow’s milk protein allergy among infants and children in Turkey. Turk J Pediatr. (2016) 58(1):1–11. doi: 10.24953/turkjped.2016.01.001
3. Boyce JA, Assa’ad A, Burks AW, Jones SM, Sampson HA, Wood RA, et al. Guidelines for the diagnosis and management of food allergy in the United States: summary of the NIAID-sponsored expert panel report. J Allergy Clin Immunol. (2010) 126(6):1105–18. doi: 10.1016/j.jaci.2010.10.008
4. Koletzko S, Niggemann B, Arato A, Dias JA, Heuschkel R, Husby S, et al. Diagnostic approach and management of cow’s-milk protein allergy in infants and children: eSPGHAN GI committee practical guidelines. J Pediatr Gastroenterol Nutr. (2012) 55(2):221–9. doi: 10.1097/MPG.0b013e31825c9482
5. Fiocchi A, Brozek J, Schünemann H, Bahna SL, von Berg A, Beyer K, et al. World allergy organization (WAO) diagnosis and rationale for action against cow’s milk allergy (DRACMA) guidelines. World Allergy Organ J. (2010) 3(4):57–161. doi: 10.1097/WOX.0b013e3181defeb9
6. Vandenplas Y, Abuabat A, Al-Hammadi S, Aly GS, Miqdady MS, Shaaban SY, et al. Middle east consensus statement on the prevention, diagnosis, and management of cow’s milk protein allergy. Pediatr Gastroenterol Hepatol Nutr. (2014) 17(2):61–73. doi: 10.5223/pghn.2014.17.2.61
7. Sackesen C, Altintas DU, Bingol A, Bingol G, Buyuktiryaki B, Demir E, et al. Current trends in tolerance induction in cow’s milk allergy: from passive to proactive strategies. Front Pediatr. (2019) 7:372. doi: 10.3389/fped.2019.00372
8. Sekerel BE, Seyhun O. Expert panel on practice patterns in the management of cow’s milk protein allergy and associated economic burden of disease on health service in Turkey. J Med Econ. (2017) 20(9):923–30. doi: 10.1080/13696998.2017.1342171
9. Wilsey MJ, Florio J, Beacker J, Lamos L, Baran JV, Oliveros L, et al. Extensively hydrolyzed formula improves allergic symptoms in the short term in infants with suspected cow’s milk protein allergy. Nutrients. (2023) 15(7):1677. doi: 10.3390/nu15071677
10. Niggemann B, von Berg A, Bollrath C, Berdel D, Schauer U, Rieger C, et al. Safety and efficacy of a new extensively hydrolyzed formula for infants with cow’s milk protein allergy. Pediatr Allergy Immunol. (2008) 19:348–54. doi: 10.1111/j.1399-3038.2007.00653.x
11. Dupont C, Bradatan E, Soulaines P, Nocerino R, Berni-Canani R. Tolerance and growth in children with cow’s milk allergy fed a thickened extensively hydrolyzed casein-based formula. BMC Pediatr. (2016) 16:96. doi: 10.1186/s12887-016-0637-3
12. Laitinen K, Kalliomaki M, Poussa T, Lagstrom H, Isolauri E. Evaluation of diet and growth in children with and without atopic eczema: follow-up study from birth to 4 years. Br J Nutr. (2005) 94(4):565–74. doi: 10.1079/bjn20051503
13. Dupont C, Chouraqui JP, de Boissieu D, Bocquet A, Bresson JL, Briend A, et al. Dietary treatment of cows’ milk protein allergy in childhood: a commentary by the committee on nutrition of the French society of paediatrics. Br J Nutr. (2012) 107(3):325–38. doi: 10.1017/S0007114511004831
14. Giovannini M, D’Auria E, Caffarelli C, Verduci E, Barberi S, Indinnimeo L, et al. Nutritional management and follow up of infants and children with food allergy: Italian society of pediatric nutrition/Italian society of pediatric allergy and immunology task force position statement. Ital J Pediatr. (2014) 40:1. doi: 10.1186/1824-7288-40-1
15. Meyer R, Venter C, Fox AT, Shah N. Practical dietary management of protein energy malnutrition in young children with cow’s milk protein allergy. Pediatr Allergy Immunol. (2012) 23(4):307–14. doi: 10.1111/j.1399-3038.2012.01265.x
16. Isolauri E, Sutas Y, Makinen-Kiljunen S, Oja SS, Isosomppi R, Turjanmaa K. Efficacy and safety of hydrolyzed cow milk and amino acid-derived formulas in infants with cow milk allergy. J Pediatr. (1995) 127:550–7. doi: 10.1016/S0022-3476(95)70111-7
17. Scalabrin D, Harris C, Johnston WH, Berseth CL. Long-term safety assessment in children who received hydrolyzed protein formulas with Lactobacillus rhamnosus GG: a 5-year follow-up. Eur J Pediatr. (2017) 176(2):217–24. doi: 10.1007/s00431-016-2825-4
18. Szajewska H, Chmielewska A. Growth of infants fed formula supplemented with Bifidobacterium lactis Bb12 or Lactobacillus GG: a systematic review of randomized controlled trials. BMC Pediatr. (2013) 13:185. doi: 10.1186/1471-2431-13-185
19. Trakulpark C, Densupsoontorn N. Twelve-month growth and accession of tolerance in infants with cow’s milk protein allergy compared among those fed with breast milk or alternative formulae. Asian Pac J Allergy Immunol. (2021). doi: 10.12932/AP-300720-0933. [Epub ahead of print].33638631
20. Dupont C, Hol J, Nieuwenhuis EE, Cow’s Milk Allergy Modified by Elimination and Lactobacilli study group. An extensively hydrolysed casein-based formula for infants with cows’ milk protein allergy: tolerance/hypo-allergenicity and growth catch-up. Br J Nutr. (2015) 113(7):1102–12. doi: 10.1017/S000711451500015X
21. Agostoni C, Fiocchi A, Riva E, Terracciano L, Sarratud T, Martelli A, et al. Growth of infants with IgE-mediated cow’s milk allergy fed different formulas in the complementary feeding period. Pediatr Allergy Immunol. (2007) 18(7):599–606. doi: 10.1111/j.1399-3038.2007.00566.x
22. WHO Multicentre Growth Reference Study Group. WHO Child growth standards based on length/height, weight and age. Acta Paediatr Suppl. (2006) 450:76–85. doi: 10.1111/j.1651-2227.2006.tb02378.x
23. Isolauri E, Sütas Y, Salo MK, Isosomppi R, Kaila M. Elimination diet in cow’s milk allergy: risk for impaired growth in young children. J Pediatr. (1998) 132(6):1004–9. doi: 10.1016/s0022-3476(98)70399-3
24. American Academy of Pediatrics Committee on Nutrition. Failure to thrive. In: Kleinman RE, Greer FR, editors. Pediatric nutrition. 7th edn. Elk Grove Village, IL: American Academy of Pediatrics (2014). p. 663–700.
25. de Jong NW, Sprikkelman AB, Oude Elberink HN, Arends NJ, Vlieg-Boerstra BJ. Blinded sensory evaluation of extensively hydrolyzed formulas and amino acid formulas. Ann Allergy Asthma Immunol. (2014) 113(2):235–6. doi: 10.1016/j.anai.2014.05.027
26. Del Giudice M, D’Auria E, Peroni D, Palazzo S, Radaelli G, Comberiati P, et al. Flavor, relative palatability and components of cow’s milk hydrolysed formulas and amino acid-based formula. Ital J Pediatr. (2015) 41:42. doi: 10.1186/s13052-015-0141-7
27. Pedrosa M, Pascual CY, Larco JI, Esteban MM. Palatability of hydrolysates and other substitution formulas for cow’s milk-allergic children: a comparative study of taste, smell, and texture evaluated by healthy volunteers. J Investig Allergol Clin Immunol. (2006) 16(6):351–6.17153882
28. Jirapinyo P, Densupsoontorn N, Kangwanpornsiri C, Wongarn R. Chicken-based formula is better tolerated than extensively hydrolyzed casein formula for the management of cow milk protein allergy in infants. Asia Pac J Clin Nutr. (2012) 21(2):209–14.22507606
29. Caffarelli C, Plebani A, Poiesi C, Petroccione T, Spattini A, Cavagni G. Determination of allergenicity to three cow’s milk hydrolysates and an amino acid-derived formula in children with cow’s milk allergy. Clin Exp Allergy. (2002) 32(1):74–9. doi: 10.1046/j.0022-0477.2001.01262.x
30. Ragno V, Giampietro PG, Bruno G, Businco L. Allergenicity of milk protein hydrolysate formulae in children with cow’s milk allergy. Eur J Pediatr. (1993) 152(9):760–2. doi: 10.1007/BF01953996
31. Canani RB, Di Costanzo M, Bedogni G, Amoroso A, Cosenza L, Di Scala C, et al. Extensively hydrolyzed casein formula containing Lactobacillus rhamnosus GG reduces the occurrence of other allergic manifestations in children with cow’s milk allergy: 3-year randomized controlled trial. J Allergy Clin Immunol. (2017) 139(6):1906–13. doi: 10.1016/j.jaci.2016.10.050
Keywords: cow’s milk protein allergy, extensively hydrolyzed casein-based formula, growth indices, gastrointestinal intolerance, stool patterns, parental satisfaction
Citation: Kansu A, Urganci N, Bukulmez A, Kutluk G, Gulcu Taskin D, Sahin Keskin L, Igde M, Molon L, Dogan Y, Sekerel BE, Yuksek M, Bostanci I, Gerenli N, Polat E, Dalgic B, Ayyildiz H, Usta M, Basturk A, Yuce Kirmemis O, Tuna Kirsaclioglu C, Gulerman HF, Alptekin Sarioglu A and Erdogan S (2023) Growth, tolerance and safety outcomes with use of an extensively hydrolyzed casein-based formula in infants with cow’s milk protein allergy. Front. Pediatr. 11:1230905. doi: 10.3389/fped.2023.1230905
Received: 29 May 2023; Accepted: 18 July 2023;
Published: 31 July 2023.
Edited by:
Alexandra Papadopoulou, Children’s Hospital Hagia Sophia, GreeceReviewed by:
Tudor Lucian Pop, University of Medicine and Pharmacy Iuliu Hatieganu, RomaniaAntigoni Mavroudi, Aristotle University of Thessaloniki, Greece
© 2023 Kansu, Urganci, Bukulmez, Kutluk, Gulcu Taskin, Sahin Keskin, Igde, Molon, Dogan, Sekerel, Yuksek, Bostanci, Gerenli, Polat, Dalgic, Ayyildiz, Usta, Basturk, Yuce Kirmemis, Tuna Kirsaclioglu, Gulerman, Alptekin Sarioglu and Erdogan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Aydan Kansu YXlkYW5rYW5zdUBnbWFpbC5jb20=
†ISPAT Study Group
 Aydan Kansu
Aydan Kansu Nafiye Urganci
Nafiye Urganci Aysegul Bukulmez3
Aysegul Bukulmez3 Mahir Igde
Mahir Igde Bulent Enis Sekerel
Bulent Enis Sekerel Buket Dalgic
Buket Dalgic Hasret Ayyildiz
Hasret Ayyildiz Aysugul Alptekin Sarioglu
Aysugul Alptekin Sarioglu Simge Erdogan
Simge Erdogan