- 1Department of Pediatric Surgery, Yijishan Hospital of Wannan Medical College, Wannan Medical College, Wuhu, China
- 2Clinical Medicine School of Wannan Medical College, Wannan Medical College, Wuhu, China
- 3Department of Medical Biology of Wannan Medical College, Wannan Medical College, Wuhu, China
- 4Department of Pediatric Surgery, Maternal and Child Health Hospital of Hubei, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
- 5Department of General Surgery, Qingdao Women and Children’s Hospital, Qingdao, China
- 6Institute of Digital Medicine and Computer-Assisted Surgery of Qingdao University, Qingdao University, Qingdao, China
- 7Shandong Provincial Key Laboratory of Digital Medicine and Computer-Assisted Surgery, Qingdao, China
Objective: The aim of this study was to evaluate the clinical efficacy of single-incision laparoscopy appendectomy (SILA) and traditional three-hole laparoscopy appendectomy (THLA) for the treatment of acute appendicitis in children.
Methods: The clinical data of children (<14 years old) who underwent laparoscopic appendectomy at Yijishan Hospital of Wannan Medical College, Hubei Provincial Maternal Health Hospital and Qingdao Women and Children's Medical Center from January 2019 to June 2022 were retrospectively analyzed. According to the operation method, the patients were assigned to the SILA group or the THLA group. The clinical data, including the efficacy, and the surgical details, including the complications, of the two surgical methods were compared. The personal information of the children and the time of disease onset were recorded.
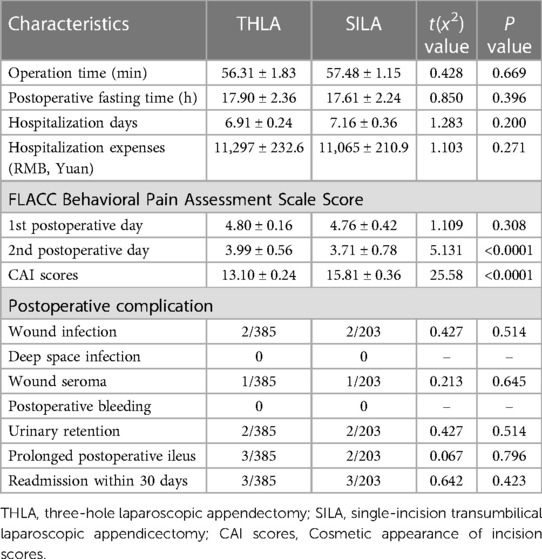
Results: In this study, the data of 588 patients, including 385 patients in the THLA group and 203 patients in the SILA group were collected. The baseline characteristics between the two groups of patients before surgery were comparable. There was no significant difference in the average operation time between the THLA group and the SILA group (56.31 ± 1.83 min vs. 57.48 ± 1.15 min, P > 0.05). There was also no significant difference in the average length of hospital stay between the THLA group and the SILA group (6.91 ± 0.24 days vs. 7.16 ± 0.36 days, P > 0.05). However, the FLACC scores of the SILA group (3.71 ± 0.78) were significantly lower than those of the THLA group (3.99 ± 0.56) on the second postoperative day, and the difference was significant (P < 0.05). The score of the questionnaire evaluating cosmetic appearance of the postoperative abdomen was significantly higher in the SILA group (15.81 ± 0.36) than in the THLA group (13.10 ± 0.24) (P < 0.05). There was no significant difference in the incidence of postoperative complications between the two groups (P > 0.05).
Conclusion: SILA is more advantageous in terms of postoperative FLACC scores and cosmetic appearance in children than THLA. There was no significant difference in the incidence of complications or other aspects between the two surgical methods.
Introduction
Acute appendicitis is highly prevalent in children with an acute abdomen, and appendectomy is still the main method of treatment for this disease (1). With the development of minimally invasive technology, laparoscopic technology has been increasingly used in pediatric surgery (2). The standard treatments for acute appendicitis are early open surgery and laparoscopic surgery. Semm reported laparoscopic appendectomy for the first time in 1983 (3, 4). Compared with traditional open surgery, laparoscopic appendectomy significantly reduces trauma and has been widely used. At present, traditional three-hole laparoscopic appendectomy (THLA) is a common appendectomy technique. However, THLA has a negative impact on quality of life and aesthetics because it requires three surgical incisions. On the contrary, in single-incision transumbilical laparoscopic appendicectomy (SILA), the incision is made around the umbilicus. Because the surgical incision is made around the umbilicus, it is very concealed and could be perceived as a natural scar, thereby achieving good cosmetic results. Although SILA has been increasingly performed in adult and pediatric surgeries, it still has not achieved the expected results (5). Some scholars believe that this technology can not only reduce the appearance of surgical scars but also reduce surgical trauma, relieve postoperative discomfort, and enable patients to move ahead of schedule (6). However, other studies have found that SILA is not superior to THLA in terms of cosmetic outcomes (7, 8).
There is no “golden triangle” operating field in conventional laparoscopy, and the operating instruments create a serious “chopstick” effect in single-site laparoscopy, especially in suturing and knotting operations (9). Therefore, surgeons who are accustomed to conventional laparoscopic operations need to master the “learning curve” of modified laparoscopic techniques (10). The abdominal cavity of children is small, and the operating space is limited, so minimally invasive operations are challenging in such a small space. SILA is infrequently performed in children because it is difficult to coordinate movements with the operation instruments. In fact, whether SILA has obvious advantages over traditional THLA in the diagnosis and treatment of acute appendicitis in children has been controversial. In this study, we retrospectively analyzed the clinical data of children with acute appendicitis in Yijishan Hospital of Wannan Medical College, Hubei Maternal Health Hospital, and Qingdao Women and Children's Medical Center and compared the results with those of traditional THLA. We compared the advantages and disadvantages of THLA and SILA, providing a reference for the clinical treatment of acute appendicitis in children.
Materials and methods
Patients and clinical parameters
We retrospectively analyzed the clinical data of children who underwent laparoscopic appendectomy at Yijishan Hospital of Wannan Medical College, Hubei Women's Health Hospital, and Qingdao Women and Children's Medical Center from January 2019 to June 2022 (<14 years). All operations were performed by two senior pediatric surgeons, each of whom had rich experience in performing laparoscopic appendectomy. The surgeon in charge informed the patients about the possible advantages and limitations of the two surgical methods before the operation, and the parents themselves decided the surgical method. We collected the clinical data of the children, including personal information, time of disease onset, surgery details, and complications. Patients with periappendix abscesses, chronic appendicitis or other diseases found during surgery were not included in this study. In this study, acute purulent appendicitis was defined to include both cases of acute purulent appendicitis and acute suppurative appendicitis with perforated appendicitis. Similarly, acute gangrenous appendicitis was defined to include cases of acute gangrene appendicitis and acute gangrene with perforated appendicitis. This study was approved by the Ethics Committee of Yijishan Hospital, Wannan Medical College (No. 2023-LSYD-24), and written consent was obtained from the parents of the children.
Surgical methods
SILA
The children in the SILA group emptied their bladder before the operation and were given general anesthesia. After the anesthesia was satisfactory, the child was placed in the supine position, the operative field was routinely disinfected, and sterile towels were spread. A transverse incision of approximately 5 mm was made in the lower edge of the umbilicus. A CO2 pneumoperitoneum was established with a pneumoperitoneum needle, the intra-abdominal pressure was set to 8–12 mmHg, and a 5 mm trocar was placed through the puncture. The abdominal cavity was routinely explored through trocars placed on the left and right sides of the umbilical ring. The 5 mm and 12 mm trocars were punctured to search for the appendix. The patient was changed from the left-lying position to the Trendelenburg position, with the head down and feet up. The pus in the rectal fossa was drained, the ileocecal part was exposed, the appendix was lifted with grasping forceps, the mesappendix at the root of the appendix was bluntly separated with blood vessel forceps to expose the root of the appendix. Hem-o-lok clips were used to ligate the mesentery of the appendix, and the mesentery was disconnected with an electric hook before undergoing electrocoagulation to stop bleeding. Hem-o-lok clips were used to ligate the root of the appendix twice, and then the appendix was cut off before being removed through a puncture hole in the outer edge of the right umbilical region. The pus that had accumulated in the abdominal pelvic cavity and intestinal space was drained; no active bleeding in the abdominal cavity was observed. Finally, the peritoneum and muscle layers of each puncture hole were sutured with 4-0 absorbable sutures, and the surgical incision was sutured with 5-0 absorbable sutures (Figure 1).
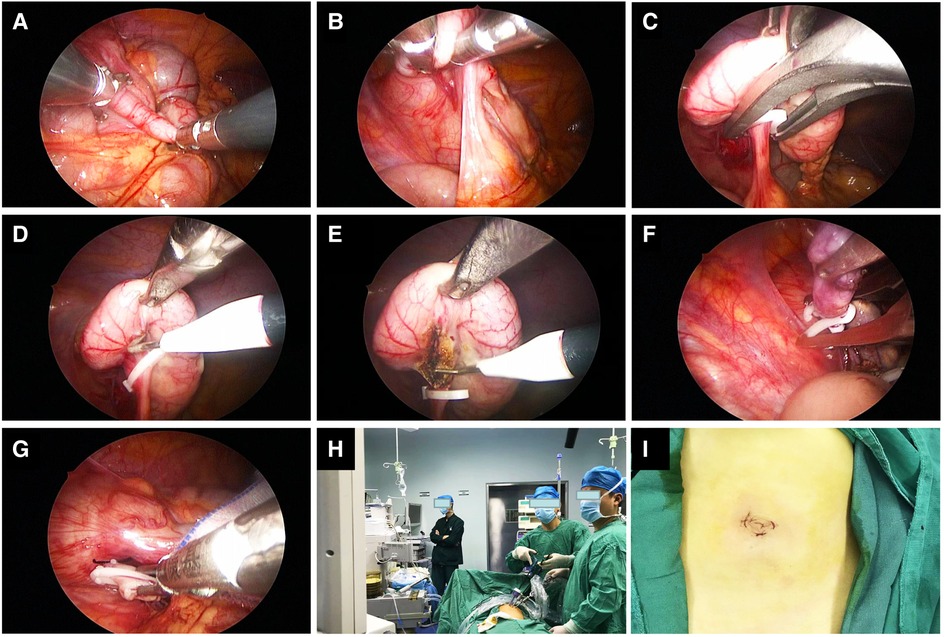
Figure 1. Intraoperative photos and screenshots of single-site laparoscopic appendectomy. (A–E) Separate and ligate the mesentery of the appendix. (F,G) Ligate the base of the appendix. (H) The positions of the surgeon and the first assistant surgeon. (I) Photos of the postoperative umbilical incision.
THLA
After satisfactory anesthesia in the traditional group, a 5 mm trocar was inserted into the lower umbilical border, and an observation lens was placed. In addition, 5 mm and 12 mm trocars were placed at the anti-Mc Burney's point and the outer edge of the right upper abdominal rectus abdominis, respectively, and the appendix removal procedure was the same as that of the single-site group. In order to minimize postoperative pain, all children were administered local analgesic injections of ropivacaine at a concentration of 0.25% in the surgical incision area.
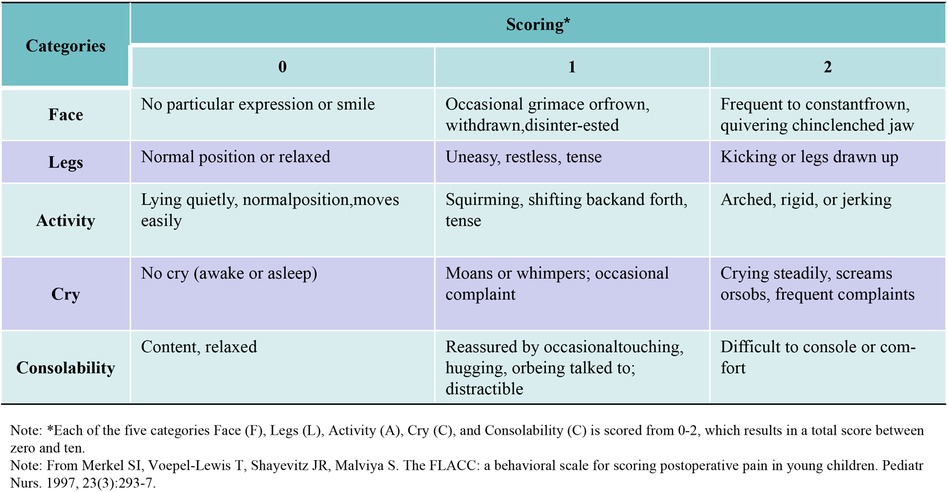
The postoperative pain scores were evaluated using the FLACC Behavioral Pain Assessment Scale (11, 12). See Figure 2 for detailed scoring rules.
Follow-up
Patients were followed up as outpatients or via telephone for 6 months. The parents of the patient completed a questionnaire to assess their perception of the Cosmetic appearance of their child's incision, scores ranged from 0 to 20 (13). The patients were followed up until February 2023.
Statistical analysis
All statistical analyses in this study were processed using SPSS 23.0 software. The measurement data were expressed as x ± s, and the Mann‒Whitney test was performed on the count data by t-test. A P value < 0.05 indicated that the difference was statistically significant.
Results
General information
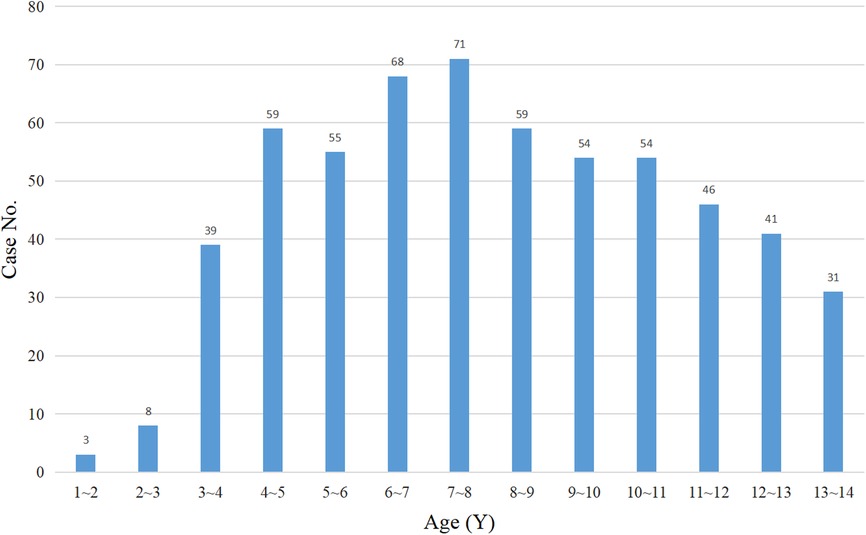
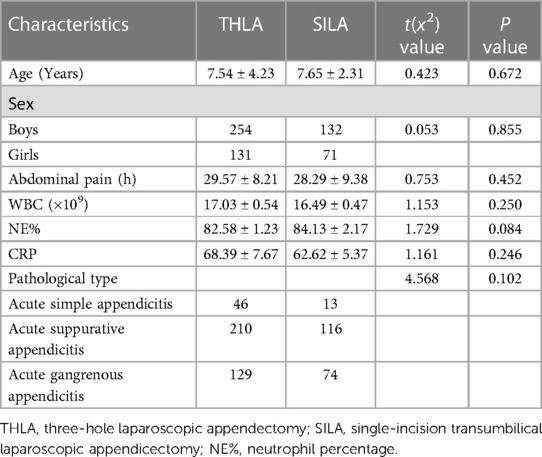
In this study, the data of 607 patients who underwent laparoscopic appendectomy in three children's surgical centers were collected. Of these 607 children, 11 children did not come to the hospital for re-examination for various reasons and were lost to follow-up. The patients were transferred back to the local hospital for treatment on the second day after the operation. Five hundred eighty-eight patients were finally enrolled in this study, with 385 patients in the THLA group and 203 patients in the SILA group (Figure 3). Laparoscopic appendectomy was successfully performed in all the patients and there was no need for conversion to open surgery. All patients were followed up for 6–24 months after the operation, and the median follow-up time was 10.5 months. The THLA group consisted of 254 boys and 131 girls with a mean age of 7.54 ± 4.23 years. The SILA group included 132 boys and 71 girls, and the mean age was 7.65 ± 2.31 years. The results of the statistical analysis showed that there was no significant difference in sex or age between the two groups (P > 0.05) (Table 1). The age distribution of children in this study was analyzed and a histogram was produced (Figure 4). The average duration of abdominal pain in the THLA group was 29.57 ± 8.21 h and that in the SILA group was 28.29 ± 9.38 h. There was no significant difference between the two groups (P > 0.05). In the THLA group and the SILA group, the average number of white blood cells in blood tests at admission were 17.03 ± 0.54 × 109 and 16.49 ± 0.47 × 109, the percentages of neutrophils were 82.58% ± 1.23% and 84.13% ± 2.17%, and the CRP levels were 68.39 ± 7.67 mg/dl and 62.62 ± 5.37 mg/dl, respectively. There was no significant difference between the two groups (P > 0.05). The postoperative pathology report in the THLA group showed 46 cases of acute simple appendicitis, 210 cases of acute suppurative appendicitis, and 129 cases of acute gangrenous appendicitis. In the SILA group, 13 cases of acute simple appendicitis, 116 cases of acute suppurative appendicitis, and 74 cases of acute gangrenous appendicitis were shown in the postoperative pathology report. There was no significant difference in the pathological characteristics between the two groups (P > 0.05). The preoperative clinical characteristics of the two groups are compared in Table 1.
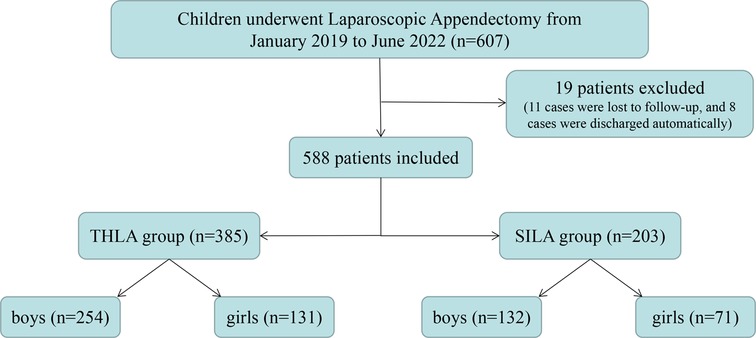
Figure 3. Flow chart of all the patients. THLA, three-hole laparoscopy appendectomy; SILA, single-incision laparoscopy appendectomy.
Surgery-related information
To study the advantages and limitations of the two surgical procedures, we calculated the operation time of the two surgical methods. The results showed that the average operation time of the THLA group was 56.31 ± 1.83 min, while that of the SILA group was 57.48 ± 1.15 min. There was no significant difference in the operation time between the two groups (P > 0.05). The average postoperative fasting time of the THLA group was 17.90 ± 2.36 h and that of the SILA group was 17.61 ± 2.24 h. There was no significant difference in the postoperative fasting time between the two groups (P > 0.05). The average hospitalization days of the THLA group was 6.91 ± 0.24 days, and the average hospitalization expenses (RMB) was 11,297 ± 232.6 yuan; however, the average hospitalization days in the SILA group was 7.16 ± 0.36 days, and the average hospitalization expenses (RMB) was 11,065 ± 210.9 yuan. There was no significant difference between the two groups in terms of total hospitalization days and hospitalization expenses (P > 0.05). To compare the severity of postoperative incision pain in the children, we collected the FLACC Behavioral Pain Assessment Scale scores from the children's medical records. In this study, only the FLACC scores on the first and second days after surgery were collected because some medical staff did not complete the records on the third day after surgery, and some data were missing. The statistical results showed that there was no significant difference in the FLACC scores on the first postoperative day between the THLA group (4.80 ± 0.16) and the SILA group (4.76 ± 0.42), but the FLACC scores on the second postoperative day were significantly different between the two groups (3.71 ± 0.78). The FLACC scores were lower in the SILA group than in the THLA group (3.99 ± 0.56), and the difference was significant (P < 0.05). To further evaluate the patient's satisfaction with their abdominal appearance 6 months after surgery, we administered a survey to parents to assess their perception of the cosmetic appearance of their child's abdomen and found that the cosmetic scores in the SILA group (15.81 ± 0.36) were significantly higher than those in the THLA group (13.10 ± 0.24). The scores were significantly different between the two groups (P < 0.05). The results of the analysis are shown in Figure 5 and Table 2.
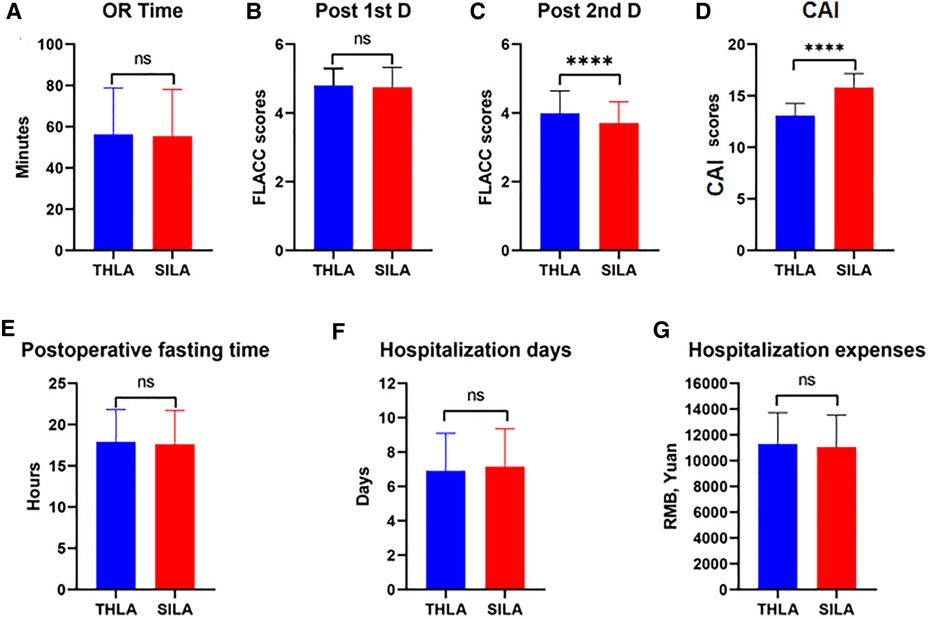
Figure 5. Comparative analysis of three-port laparoscopic appendectomy and single-port laparoscopic appendectomy in this study. ns, not significant; ****P < 0.0001. (A) The comparison results between the two groups of Operation time. (B, C) Comparison of results between two groups of FLACC Behavioral Pain Assessment Scale Scores on the first and second postoperative days. (D) Comparative results of Cosmetic appearance of incidence scores between the two groups. (E) Comparative results of Postoperative fasting time between the two groups. (F) Comparative results of Hospitalization days between the two groups. (G) Comparative results of Hospitalization expenses between the two groups.
To compare the two groups with the same pathological type of appendicitis, we analyzed the operation time. The findings revealed that the average operation time for acute simple appendicitis was 45.00 ± 18.07 min and 52.68 ± 18.88 min in the THLA and SILA groups, respectively. However, there was no significant statistical difference between the two groups (P > 0.05). Similarly, for acute suppurative appendicitis, the mean operation time was 54.50 ± 20.38 min and 55.07 ± 22.18 min in the THLA and SILA groups, respectively. Again, there was no statistically significant difference between the two groups (P > 0.05). The mean operation time for acute gangrene appendicitis was 63.49 ± 24.83 min and 64.90 ± 27.07 min in the THLA and SILA groups, respectively, and there was no statistically significant difference between the two groups (P > 0.05). The results of the detailed statistical analysis are shown in Table 3.
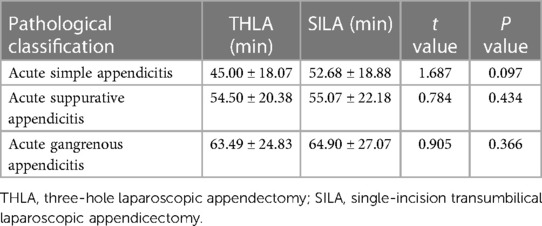
Table 3. Comparative analysis of operation time between two groups based on pathological classification.
Complications
Last, we studied the complications related to the two surgical procedures. Incision infection occurred in 2 patients in the THLA group and in 2 patients in the SILA group, but the difference in the infection incision rates (0.52% vs. 0.99%) was not significant between the two groups (P > 0.05). Incision infection was effectively controlled in all children and healed after changing the dressing. Wound seroma occurred in one patient in the THLA group and in 1 patient in the SILA group, and the difference in the wound seroma rate (0.26% vs. 0.49%) was not significant between the two groups (P > 0.05). Two children in the THLA group and 2 children in the SILA group developed postoperative urinary retention, and the difference in the postoperative urinary retention rate (0.52% vs. 0.99%) was not significant between the two groups (P > 0.05). Children with urinary retention successfully released urine after symptomatic treatment. In the THLA group, 3 children were readmitted due to intestinal obstruction within 30 days after the operation and were cured and discharged after conservative treatment. In the SILA group, 2 children with intestinal obstruction were readmitted within 30 days, and another child with an incision infection was readmitted to the hospital for anti-infection treatment and a dressing change within 30 days. There was no significant difference in the incidence of intestinal obstruction (0.78% vs. 0.99%) or the incidence of readmission within 30 days (0.78% vs. 1.48%) between the two groups (P > 0.05). The results are shown in Table 2.
Discussion
Acute appendicitis is the most common acute abdominal disease in children who are older than 6 years (14). However, in this study, 3 children were 1 year old, indicating that pediatric surgeons should be aware that this disease can present in younger children. The three children's centers involved in this study are renowned for their expertise in treating complex and challenging cases. Typically, local municipal or county-level hospitals prefer to perform appendicitis surgery on older children, while younger children are often referred to the three major medical institutions in this study. As a result, the average age of children in this study was relatively low. Studies have found that the incidence of acute appendicitis in children is gradually increasing. Since the symptoms of appendicitis in children are generally atypical, the disease progresses more rapidly than in adults, and the incidence of perforation is much higher in children than in adults (15). Early surgery is the most important treatment for this disease. Compared with open appendectomy, laparoscopic appendectomy has significant advantages, including a shorter surgical time, a faster postoperative recovery, fewer postoperative complications, and a shorter hospital stay. It may be more suitable for elderly and pediatric patients. With the development of laparoscopic technology, transumbilical single-site, single-port laparoscopic surgery has been increasingly performed in pediatric appendectomy, but whether this technique has more obvious advantages than traditional three-port laparoscopy is still unknown (16). Because single-port laparoscopy requires special operating instruments, which significantly increases medical expenses, its application in primary hospitals in China has been significantly restricted (17). The majority of pediatric surgeons may be more likely to perform SILA instead of THLA. This was a multicenter retrospective study involving three children's medical centers in China and we found that compared with THLA, SILA had better FLACC scores and cosmetic outcomes in children on the second day after surgery. However, there was no significant difference in intraoperative surgery time, hospital stay, total medical costs, or postoperative complications between the two surgical methods.
Laparoscopic appendectomy allows the appendix to be found under direct vision, abdominal exploration and ascites removal, with less trauma, faster postoperative recovery and better cosmetic outcomes (18). It has gradually become the first choice for the treatment of appendicitis. In transumbilical laparoscopic surgery, the navel, a natural biological channel, is the site of entry, thus allowing the postoperative incision to be concealed, which has become the goal of the surgery. Although the abdominal wall is thin, the colon is relatively free, and the umbilicus and root of the appendix are close in children, the incision from the umbilicus is still preferred so that the appendix can be pulled through the umbilical incision with grasping forceps or a homemade copper wire hook. In doing so, appendectomy is completed in vitro. However, this technique is only suitable for those with mild appendicitis symptoms, no obvious adhesions to the surrounding structures and a free appendix; this operation significantly increases the risk of an incision infection (19). Using the traditional method, the dissociation of the mesentery of the appendix and the treatment of the root of the appendix are completed under the laparoscope. The appendix is removed through a trocar and placed in a specimen bag. Since the appendix does not touch the wound, the risk of an incision infection is low. Some scholars have suggested that all trocars be placed in the umbilicus and that the appendix should be freed and removed under the laparoscope, which not only ensures a highly concealed incision but also avoids the high risk of an incision infection. The mirror technique is a concern for surgeons (20). Unfortunately, to date, SILA has not been widely recognized for the treatment of acute appendicitis in children (21). Compared with THLA, SILA requires that the spatial relationship between the operating forceps and the observation lens be considered, and the single-incision approach affects the surgeon's and assistant's range of motion, thereby complicating and prolonging the surgery (22). To date, there is no consensus on SILA having more advantages than traditional laparoscopic approaches.
Zhao et al. (23) conducted a meta-analysis of 12 pediatric appendectomy procedures and found that compared with THLA, SILA significantly shortened the hospitalization time, but there was no significant difference in surgical time or other aspects. A meta-analysis conducted by Köhler et al. (24) included a total of 20 studies, and the results showed that extracorporeal SILA seemed to have the advantage of a shorter surgical time, while in vitro/in vivo SILA showed no significant difference in safety compared to THLA. Aly (25) found that traditional laparoscopic appendectomy is significantly better than SILA in terms of surgical time and intraoperative conversion rate. In addition, some studies suggest that the abdominal wall nearest to the umbilical cord is thin and very close to the cecum. It is possible to slightly expand the umbilical incision and then resect and lift the appendix through the incision under direct vision (26, 27). Lee et al. (28) reported for the first time that in patients undergoing laparoscopic appendectomy, patients with a narrow and deep umbilicus have a significantly increased risk of a postoperative incision infection, while extending the umbilicus incision during surgery seems to reduce the risk of postoperative incision infection. However, in practical practice, pediatric surgeons have found that this method is more commonly used for simple appendicitis, but for complex appendicitis patients with special locations or heavy adhesions, it is very difficult to remove the appendix through an umbilical incision (29).
Some scholars believe that because all operation instruments are used at the same site, the traditional “triangular operation” method cannot be applied smoothly, and there are certain deficiencies in visual field exposure and operational accuracy (30). This viewpoint may greatly limit the development of this technology. In fact, there are certain techniques for placing the three trocars for SILA. The trocar with the lens should be placed as shallow as possible, preferably with the mirror just entering the abdominal cavity, while the trocar with the auxiliary forceps should be placed as deep as possible to minimize the “chopstick effect” and ensure that the surgical operation is completed under direct endoscopy. There are various methods for dissecting the mesentery of the appendix, such as wire ligation, biological clamp closure, and single bipolar electrocoagulation. However, it is difficult to ligate or clamp the root of the mesentery under endoscopy, so an ultrasound knife can be used to directly detach the appendix mesentery. The operation is simple and hemostasis is fast, so there is less intraoperative bleeding and no risk of major bleeding after surgery. In fact, separating the mesentery of the appendix is the most time-consuming process in appendectomy. This study found that the surgical time of SILA was not significantly longer than that of THLA. We consider that this may be related to the fact that most of the laparoscopic appendectomies that were performed at the three pediatric surgical centers included in this study were performed by senior doctors with rich surgical experience who are very familiar with the anatomical structure of the appendix. Therefore, there is no significant difference in the surgical time between traditional laparoscopic surgery and SILA. There are various methods for the treatment of laparoscopic appendiceal stumps, among which the commonly used methods include suture insertion and ligation, biological clamping, and snare thread ligation. These treatment measures are the same for single-site laparoscopic appendectomy and traditional three-hole laparoscopic appendectomy. In addition, this study found that although there was no significant difference in FLACC scores between the two groups on the first day after surgery, the scores of the single site group were significantly lower than those of the traditional group on the second day after surgery, which differed from Que et al.'s (31) study. We believe that the FLACC scoring standard used in this study is more suitable for children. All scores are evaluated and recorded by specialized pediatric surgical staff, and single-site surgical incisions are mainly concentrated in the umbilical region, with no excessive wounds in other areas, which can reduce postoperative pain in children.
This study also has some limitations. First, this was a retrospective study. The specific surgical method was chosen by the family members of the patient before surgery, and all preoperative conversations were initiated by the surgeon. Whether the surgeon's preferred surgery caused any bias remains unknown. Second, although all the surgeries were performed by advanced pediatric surgeons, there may have been some differences in personal skills. Third, The three medical centers involved in this study utilized a single-site laparoscopic appendectomy procedure around the umbilicus due to the high cost of single-port surgical instruments. This is a major consideration for parents and surgeons in developing countries where medical costs can be a limiting factor. The medical staff and parents of the children treated in this study preferred to use the most cost-effective medical equipment to achieve the best surgical outcomes. As China's medical insurance system continues to evolve, the cost of medical devices is expected to decrease, which will enable the use of single-port instruments for more minimally invasive laparoscopic surgeries in future research. Finally, the hospitalization fees are comparable among all three medical centers despite the three medical centers included in this study being in three different provinces in China (Anhui, Hubei, and Shandong). However, there may be slight differences in the charging standards between each province. To avoid these limitations and reduce bias in the future, we will include larger samples and more centers.
Conclusions
In summary, this study found that SILA has significant advantages over THLA in terms of postoperative FLACC scores and aesthetic outcomes in children. However, there was no significant difference in operation time, length of hospital stay, total medical costs, or incidence of postoperative complications between the two surgical methods.
Data availability statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving human participants were reviewed and approved by This study was approved by the Ethics Committee of Yijishan Hospital, Wannan Medical College (No. 2023-LSYD-24), and written consent was obtained from the parents of the children. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
All authors have approved the final version of the manuscript. JL, GC and XM contributed equally to this paper. JL, AL and GD designed the research, analyzed the data, and wrote the manuscript; ZJ, NJ, and JL analyzed and interpreted the data; JL, NX, AL and GD designed the research, analyzed the data, and corrected the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was funded by the Research project of Hubei Maternal and Child Health Hospital (Grant No. 2021SFYM024), the Talent Introduction Fund of Yijishan Hospital of Wannan Medical College (Grant No. YR202203), the Scientific Research Project of Wannan Medical College (Grant No. WK2022ZF08), the Teaching quality and teaching reform project of Wannan Medical College (Grant No. 2022xnfz09), Anhui Provincial Department of Education offers blended online and offline courses (Grant No. 2022xsxx243), Wannan Medical College Yijishan Hospital Management and Service Innovation Project (Grant No. CX2023005). The funders had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Acknowledgments
We thank all the researchers who participated in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. de Almeida LR, Seo DJ, Gomez-Eslava B, Hossain S, Lesegretain A, de Souza AV, et al. Nonoperative vs operative management of uncomplicated acute appendicitis: a systematic review and meta-analysis. JAMA Surg. (2022) 157:828–34. doi: 10.1001/jamasurg.2022.2937
2. Bai S, Hu S, Zhang Y, Guo S, Zhu R, Zeng J. The value of the alvarado score for the diagnosis of acute appendicitis in children: a systematic review and meta-analysis. J Pediatr Surg. (2023): S0022-3468(23)00181-1. doi: 10.1016/j.jpedsurg.2023.02.060
4. Markar SR, Karthikesalingam A, Di Franco F, Harris AM. Systematic review and meta-analysis of single-incision versus conventional multiport appendicectomy. Br J Surg. (2013) 100:1709–18. doi: 10.1002/bjs.9296
5. Kang SI, Woo IT, Bae SU, Yang CS. Single-incision versus conventional laparoscopic appendectomy: a multi-center randomized controlled trial (SCAR trial). Int J Surg Protoc. (2021) 25:201–8. doi: 10.29337/ijsp.159
6. Li C, Liu Y, Jiang Y, Xu Y, Wang Z. Single-incision compared with conventional laparoscopy for appendectomy in acute appendicitis: a systematic review and meta-analysis. Int J Colorectal Dis. (2022) 37:1925–35. doi: 10.1007/s00384-022-04231-6
7. Jin SG, Cho SH, Kim KY, Ahn SK, Cho J, Jung BW, et al. Transumbilical single-incision laparoscopic-assisted appendectomy (TULAA) is useful in adults and young adolescents: comparison with multi-port laparoscopic appendectomy. Medicina (Kaunas). (2019) 55:248. doi: 10.3390/medicina55060248
8. Deng L, Xiong J, Xia Q. Single-incision versus conventional three-incision laparoscopic appendectomy: a meta-analysis of randomized controlled trials. J Evid Based Med. (2017) 10:196–206. doi: 10.1111/jebm.12238
9. Sekioka A, Takahashi T, Yamoto M, Miyake H, Fukumoto K, Nakaya K, et al. Outcomes of transumbilical laparoscopic-assisted appendectomy and conventional laparoscopic appendectomy for acute pediatric appendicitis in a single institution. J Laparoendosc Adv Surg Tech A. (2018) 28:1548–52. doi: 10.1089/lap.2018.0306
10. Vellei S, Borri A. Single-incision versus three-port laparoscopic appendectomy: short- and long-term outcomes. J Laparoendosc Adv Surg Tech A. (2017) 27:804–11. doi: 10.1089/lap.2016.0406
11. Willis MH, Merkel SI, Voepel-Lewis T, Malviya S. FLACC behavioral pain assessment scale: a comparison with the child’s self-report. Pediatr Nurs. (2003) 29:195–8.12836995
12. Merkel SI, Voepel-Lewis T, Shayevitz JR, Malviya S. The FLACC: a behavioral scale for scoring postoperative pain in young children. Pediatr Nurs. (1997) 23:293–7.9220806
13. Carter JT, Kaplan JA, Nguyen JN, Lin MY, Rogers SJ, Harris HW. A prospective, randomized controlled trial of single-incision laparoscopic vs conventional 3-port laparoscopic appendectomy for treatment of acute appendicitis. J Am Coll Surg. (2014) 218:950–9. doi: 10.1016/j.jamcollsurg.2013.12.052
14. Lounis Y, Hugo J, Demarche M, Seghaye MC. Influence of age on clinical presentation, diagnosis delay and outcome in pre-school children with acute appendicitis. BMC Pediatr. (2020) 20:151. doi: 10.1186/s12887-020-02053-5
15. Feng W, Zhao XF, Li MM, Cui HL. A clinical prediction model for complicated appendicitis in children younger than five years of age. BMC Pediatr. (2020) 20:401. doi: 10.1186/s12887-020-02286-4
16. Carrillo Montenegro AF, Aristizabal Rojas S, Pulido Segura JA, Pedraza M, Padilla L, Lozada-Martinez ID, et al. Single incision laparoscopic appendectomy with surgical-glove port is cost-effective and reliable in complicated acute appendicitis: a casecontrol multicenter study in Colombia. Heliyon. (2023) 9:e12972–8. doi: 10.1016/j.heliyon.2023.e12972
17. Zaman S, Mohamedahmed A, Srinivasan A, Stonelake S, Sillah AK, Hajibandeh S, et al. Single-port laparoscopic appendicectomy versus conventional three-port approach for acute appendicitis: a systematic review, meta-analysis and trial sequential analysis of randomised controlled trials. Surgeon. (2021) 19:365–79. doi: 10.1016/j.surge.2021.01.018
18. Goodman LF, Lin AC, Sacks MA, McRae JJLH, Radulescu A, Khan FA. Single site versus conventional laparoscopic appendectomy: some pain for no gain? J Surg Res. (2021) 264:321–6. doi: 10.1016/j.jss.2021.03.010
19. Hernandez-Martin S, Ayuso L, Molina AY, Pison J, Martinez-Bermejo MA, Perez-Martinez A. Transumbilical laparoscopic-assisted appendectomy in children: is it worth it? Surg Endosc. (2017) 31:5372–80. doi: 10.1007/s00464-017-5618-6
20. Zaman S, Mohamedahmed A, Stonelake S, Srinivasan A, Sillah AK, Hajibandeh S, et al. Single-port laparoscopic appendicectomy versus conventional three-port approach for acute appendicitis in children: a systematic review and meta-analysis. Pediatr Surg Int. (2021) 37:119–27. doi: 10.1007/s00383-020-04776-z
21. Chen Y, Guo S, Liu Y, Yuan J, Fan Z. Single-port laparoscopic appendectomy using a needle-type grasping forceps compared with conventional three-port laparoscopic appendectomy for patients with acute uncomplicated appendicitis: a single-center retrospective study. J Int Med Res. (2022) 50:3000605221119647. doi: 10.1177/03000605221119647
22. Fujii T, Tanaka A, Katami H, Shimono R. Intra-/extracorporeal single-incision versus conventional laparoscopic appendectomy in children: a systematic review and meta-analysis. J Laparoendosc Adv Surg Tech A. (2022) 32:702–12. doi: 10.1089/lap.2021.0738
23. Zhao L, Liao Z, Feng S, Wu P, Chen G. Single-incision versus conventional laparoscopic appendicectomy in children: a systematic review and meta-analysis. Pediatr Surg Int. (2015) 31:347–53. doi: 10.1007/s00383-015-3680-5
24. Kohler F, Reese L, Kastner C, Hendricks A, Muller S, Lock JF, et al. Surgical site infection following single-port appendectomy: a systematic review of the literature and meta-analysis. Front Surg. (2022) 9:919744. doi: 10.3389/fsurg.2022.919744
25. Aly OE, Black DH, Rehman H, Ahmed I. Single incision laparoscopic appendicectomy versus conventional three-port laparoscopic appendicectomy: a systematic review and meta-analysis. Int J Surg. (2016) 35:120–8. doi: 10.1016/j.ijsu.2016.09.087
26. Ohno Y. Role of the transumbilical laparoscopic-assisted single-channel, single-port procedure in an interval appendectomy for pediatric mass-forming appendicitis: a preliminary retrospective analysis. Asian J Endosc Surg. (2014) 7:232–6. doi: 10.1111/ases.12111
27. Miyo M, Urabe S, Hyuga S, Nakagawa T, Michiura T, Hayashi N, et al. Clinical outcomes of single-site laparoscopic interval appendectomy for severe complicated appendicitis: comparison to conventional emergency appendectomy. Ann Gastroenterol Surg. (2019) 3:561–7. doi: 10.1002/ags3.12277
28. Lee DJ, Kim KY, Ahn SK, Yoon SN, Cho JW, Lee SY, et al. Does the morphology of the umbilicus influence the incidence of surgical site infections in transumbilical single-incision laparoscopic appendectomy? J Minim Access Surg. (2022) 18:505–9. doi: 10.4103/jmas.jmas_157_21
29. Karam PA, Mohan A, Buta MR, Seifarth FG. Comparison of transumbilical laparoscopically assisted appendectomy to conventional laparoscopic appendectomy in children. Surg Laparosc Endosc Percutan Tech. (2016) 26:508–12. doi: 10.1097/SLE.0000000000000334
30. Echevarria S, Rauf F, Hussain N, Zaka H, Farwa UE, Ahsan N, et al. Typical and atypical presentations of appendicitis and their implications for diagnosis and treatment: a literature review. Cureus. (2023) 15:e37024. doi: 10.7759/cureus.37024
Keywords: children, single-incision, conventional, laparoscopy, appendectomy
Citation: Liu J, Chen G, Mao X, Jiang Z, Jiang N, Xia N, Lin A and Duan G (2023) Single-incision laparoscopic appendectomy versus traditional three-hole laparoscopic appendectomy for acute appendicitis in children by senior pediatric surgeons: a multicenter study from China. Front. Pediatr. 11:1224113. doi: 10.3389/fped.2023.1224113
Received: 17 May 2023; Accepted: 26 June 2023;
Published: 10 July 2023.
Edited by:
Hiroo Uchida, Nagoya University Graduate School of Medicine, JapanReviewed by:
Nicola Zampieri, University of Verona, ItalyYujiro Tanaka, Saitama Medical University, Japan
© 2023 Liu, Chen, Mao, Jiang, Jiang, Xia, Lin and Duan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nan Xia bG9vam91cm5leUAxNjMuY29t Aiqin Lin bGluYWlxaW45NDVAMTYzLmNvbQ== Guangqi Duan ZHVhbmd1YW5ncWl6ckAxMjYuY29t
†These authors have contributed equally to this work and share first authorship
Abbreviations THLA, three-hole laparoscopic appendectomy; SILA, single-incision transumbilical laparoscopic appendicectomy.
 Jie Liu
Jie Liu Guoxian Chen2,3,†
Guoxian Chen2,3,† Xiaowen Mao
Xiaowen Mao