- State Key Laboratory of Ophthalmology, Guangdong Provincial Key Laboratory of Ophthalmology and Visual Science, Guangdong Provincial Clinical Research Center for Ocular Diseases, Zhongshan Ophthalmic Center, Sun Yat-Sen University, Guangzhou, China
Objective: It is still controversial whether intermittent exotropia (IXT) affects myopic progression during the critical period of visual development. This study retrospectively analyzed the long-term myopic changes and the impact of IXT surgery on myopic progression in school-aged children with moderate IXT.
Methods: The medical records of 65 children from 5 to 13 years old with or without IXT between 2015 and 2021 were retrospectively reviewed. Patients whose spherical equivalent refraction (SER) were less than −3.00 diopter (D) were included and divided into three groups: IXT surgery group (Group A), which comprised 22 IXT patients who received IXT surgery, IXT observation group (Group B), which comprises 19 IXT patients who only received long-term observational follow-up; and normal control group (Group C), which comprised 24 normal controls without IXT. The main outcome measurement was the rate of myopic progression, which was defined as the mean myopic shift in SER per year.
Results: The 3- and 5-years long-term follow-up rates of myopic progression were −0.47 ± 0.28 D per year and −0.48 ± 0.23 D per year respectively in Group B, and those were significantly slower than that in Group C (−0.73 ± 0.32 D per year and −0.76 ± 0.19 D per year respectively). However, there was no significant difference in the rate of myopic progression between Group A and B or between Group A and C.
Conclusion: Moderate IXT may have lower rate of myopic progression in school-aged children. Whether IXT surgery influence the rate of myopic progression still needs further study.
Introduction
In school-aged children, myopia is the most common ocular disorder with increasing prevalence throughout the world and especially in Asia (1, 2), while intermittent exotropia (IXT) is the most common type of ocular misalignment in Asian countries (3, 4). While we know that esotropia is associated with hyperopia due to accommodation (5), the myopic progression in patients with IXT has not been rigorously studied. The role of accommodation in myopic progression has been continuously debated (6), and the increased accommodative demand to control the exodeviation in patients with IXT has been reported as a potential risk factor of myopic progression (7, 8). However, previous studies showed no correlation between myopic progression and IXT, and surgical correction of IXT did not alter the myopic progression (9, 10). But recent studies identified that the IXT surgery result in a faster myopic progression in the operated eye (11), and the non-dominant eye of IXT patient had a faster myopic progression (12). Additionally, it is still controversial to choose surgical correction of strabismus or not for moderate IXT patients (13), and the present study may provide a side evidence for this controversy in the perspective of myopia control.
Given that the association between myopic progression and IXT has not been established as well, the present study was conducted to investigate the relationship between moderate IXT and myopic progression and the impact of IXT surgery on myopic progression in school-aged children.
Subjects and methods
This retrospective study was approved by the Institutional Review Board of Zhongshan Ophthalmic Center, Sun Yat-sen University (2015MEKY055) and followed the tenets of the Declaration of Helsinki.
The medical records of consecutive school-aged children from 5 to 13 years old at the time of first visit in our department of strabismus with moderate IXT between January 2015 and January 2021 were retrospectively reviewed. The moderate IXT was defined as a minimum intermittent exodeviation of 15 prism diopters (PD) at distance with normal simultaneous perception documented using synoptophore (13). All patients had spherical equivalent refraction (SER) between +2.00 and −3.0 diopter (D) in both eyes at the time of first visit. The following exclusion criteria were applied: anisometropia is greater than 3.00 D between two eyes; astigmatism is greater than 3.00 D in any eye; amblyopia; any other combined strabismus; previous history of strabismus surgery; previous history or plan of myopia control treatment or binocular vision training; neurologic or systemic disorder. The patients with moderate IXT were divided into two groups: Group A consisted of the patients who underwent strabismus surgery, and Group B consisted of the patients who were followed-up for observation. The control group (Group C) was matched for age and refraction, and consisted of children with orthotropia determined by the cover test.
All subjects included in this study underwent a complete ophthalmic examination and cycloplegic refraction annually for 5 years. Cycloplegic refraction was measured by subjective refraction following the topical administration of 1% tropicamide, and full corrections of refractive errors were prescribed. Ocular dominance was determined by the hole-in-the card test as previously described (14). Unilateral recession-resection surgery was performed on non-dominant eye in all subjects of Group A right after the initial presentation.
The main outcome measurement for myopic progression was the myopic shift rate, which was defined as the mean SER change per year (11). The interocular differences of myopic progression were analyzed for the comparison between right eye and left eye, between dominant eye and non-dominant eye, and between operated eye and non-operated eye, respectively (Supplementary Table S1). As there was no significant difference detected between two eyes, the average SER of two eyes were obtained for each subject and used for further comparative analysis of myopic shift rates among three groups.
Statistical analysis
Statistical analysis was performed using the Statistical Package for Social Sciences program (version 22.0, SPSS Inc, Chicago, Illinois, USA). Means and standard deviations (SD) along with ranges were used to describe the clinical features in Tables 1, 2. Levene's test, Kruskal–Wallis test, and Mann–Whitney U-test were performed to evaluate differences between groups.
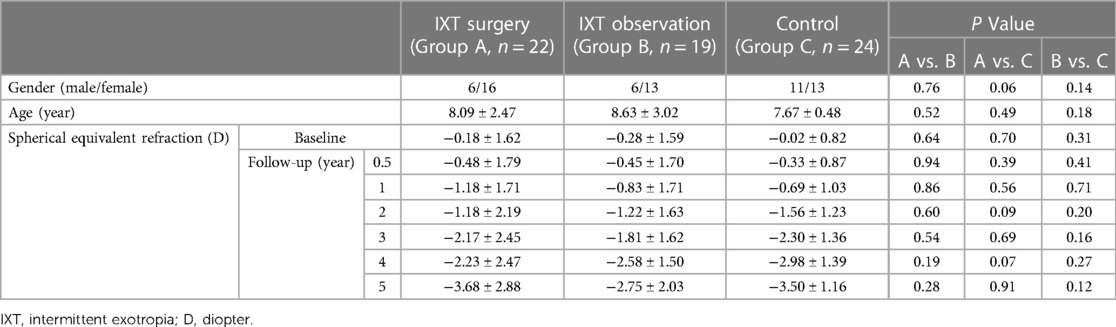
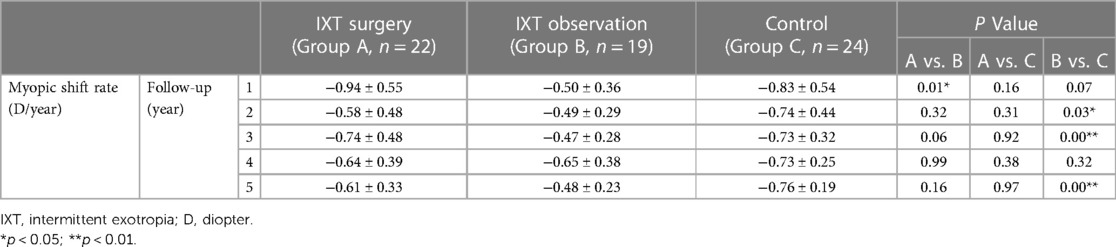
Table 1. Baseline demographic characteristics and spherical equivalent refraction changes of studied subjects in different groups.
Results
A total of 65 school-aged children from 5 to 13 years old with or without IXT were included in this retrospective study. The IXT surgery group (Group A) comprised 22 patients with moderate IXT who received strabismus surgery, the IXT observation group (Group B) comprised 19 patients with moderate IXT who only received long-term observational follow-up, and the control group (Group C) comprised 24 normal subjects without IXT. The baseline demographic characteristics showed no significant intergroup difference in gender and age (Table 1). The initial mean SER were similar in three studied groups, which were −0.18 ± 1.62 D, −0.28 ± 1.59 D, and −0.02 ± 0.82 D, respectively. No intergroup difference of SER was detected at each follow-up evaluation either, although myopic progressions were detected in all studied groups. The changes of myopic status in the three studied groups were shown in Figure 1.
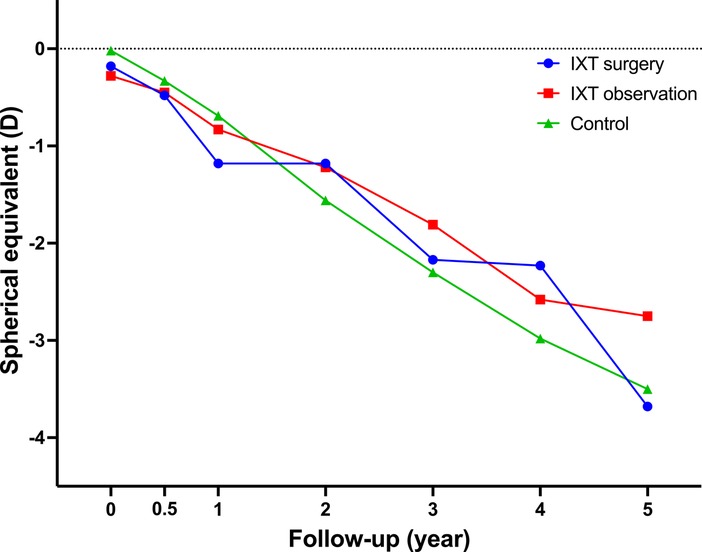
Figure 1. The changes of myopic status in the three studied groups. All three groups showed similar myopic shift without statistically significant differences during the follow-up period. IXT, intermittent exotropia; D, diopter.
The myopic shift rates of studied groups at each follow-up are shown in Table 2. Between two groups (Group B and C) without surgical intervention, the mean myopic shift rates in patients with moderate IXT (Group B) were significantly lower than in normal controls (Group C) at 2-year (p = 0.03), 3-year (p < 0.001), and 5-year (p < 0.001) follow-up evaluation. In the patients with moderate IXT (Group A and B), the mean myopic shift rate in patients who underwent strabismus surgery (Group A) was significantly higher than the observation group (Group B) at early postoperative follow-up (p = 0.01 at 1-year follow-up), however, no difference was noted in the mean myopic shift rates between these two groups subsequently. The changes of myopic shift rates in the three studied groups are shown in Figure 2.
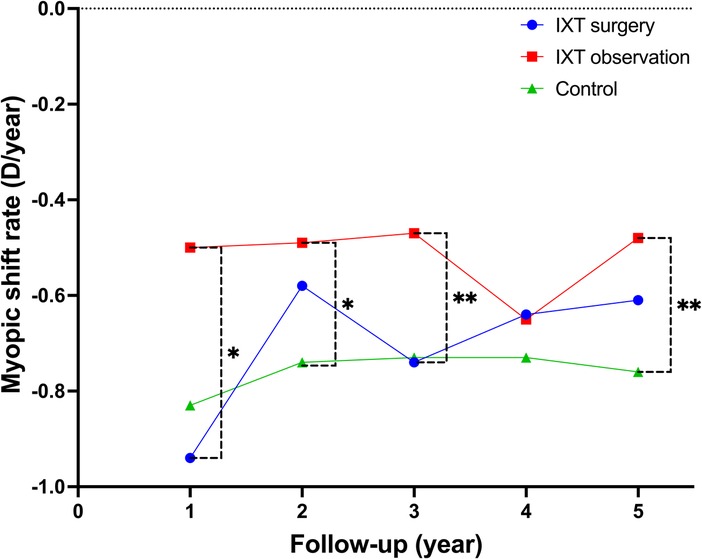
Figure 2. The changes of myopic shift rates in the three studied groups. Statistically significant differences in the mean myopic shift rates were detected between IXT observation group and control group at 2-, 3-, and 5-year follow-up. On the other hand, a statistically significant difference in the mean myopic shift rate was detected between IXT surgery group and IXT observation group only at 1-year follow-up. IXT, intermittent exotropia; D, diopter.
Discussion
The present retrospective study on 65 school-aged children showed a significant overall myopic progression in all studied groups. Although we failed to find a statistically significant intergroup difference of SER during follow-up period, we detected intergroup differences in myopic shift rates between Group A and Group B (p = 0.01 at 1-year) at early postoperative follow-up and between Group B and Group C (p = 0.03 at 2-year, p < 0.001 at 3-year, and p < 0.001 at 5-year) in long-term follow-up. These findings are not consistent with previous studies (9, 10), which reported that IXT itself or surgical correction of IXT did not alter the myopic progression.
In the present study we set the inclusion criteria of age as 5–13 years old, and the mean ages of three studied groups were 8.09 ± 2.47, 8.63 ± 3.02, and 7.67 ± 0.48 respectively. Simple myopia usually occurs in early school-age of 5–13 years old, and the myopic progression has been reported to cease at 15–16 years of age (15–17). So, the school-age is the most critical period for the progression of myopia. Besides, the refractive status of the enrolled subjects in all three studied groups were mild myopia at initial presentation. In view of children with myopia showed faster myopic progression (18), we investigated myopic shift rates in school-aged children with mild myopia, in order to identify the impact of IXT and surgical correction of IXT on myopic progression in these specific population. In addition, we chose the children only with moderate IXT who manifest obvious exodeviation frequently but with only partial impairment of binocular single vision, and it was different from previous studies containing a various severity of IXT (9, 10).
No significant difference detected between dominant eye and non-dominant eye among three studied groups in our study, however, it has been reported that the non-dominant eye had a faster myopic progression which associated with severe IXT caused by greater gap between the required accommodative demand and response (12). The results of our study can be explained by the specific type of moderate IXT patients which included in the present study, and the impact of moderate IXT on the myopic progression of the non-dominant eye might be not as strong as severe IXT. In contrast, the moderate IXT children in Group B showed slow myopic progression than the normal control in Group C. The moderate IXT children had relatively better control of exodeviation, which indicated that sufficient accommodative response compared with accommodative demand in these moderate IXT children to control normal ocular alignment. The mechanism involved in the control of IXT is still of limited understanding (19), and coupled accommodation and vergence responses are needed for compensating the additional convergence demand when overcoming the exodeviation to achieve normal alignment in IXT patients (20). The control of IXT is typically driven by neither accommodative effort alone nor convergence effort alone. In moderate IXT patients with good control, over-accommodation secondary to fusional convergence may easily overcome the gap between the required accommodative demand and actual accommodative response. So, for the moderate IXT children in the present study, achieving normal alignment did not conflict with having clear image on the retina, and possibly resulted in reduction of the myopic shift rates. The impact of the moderate IXT on myopic progression has been reconfirmed by removing this probable protective factor, the myopic shift rates remained unchanged after surgical correction of IXT (Group A vs. Group C).
The previous studies reported a significant myopic progression in the operated eye following surgical correction of IXT in early school-aged children (11, 21, 22), although other reports showed no significant change in myopic progression after IXT surgery (10, 23). A faster myopic shift in the operated eye might be caused by either surgical procedure or accommodative lag in the non-dominant eye. In present study, we detected a transient myopic shift induced by IXT surgery (Group A vs. Group B at 1-year), however, no significant difference was detected between operated eye and non-operated eye in Group A. So, it is still unclear whether the IXT surgical procedure or surgical removal of IXT is responsible for the transient myopic change.
The limitations of the present study are as follows. First, a relatively small sample size of the retrospective study induced small fluctuation in the changing curve of myopic shift rates (Figure 2). The sample size is approximately calculated as 110 if take the present study as a preliminary experiment, when the calculation assumes 5% type I error with 80% power. Second, we chose moderate IXT children to investigate the impact on myopic progression, but we did not analyze the effect in terms of the amount of deviation angle, the degree of control, the types of strabismus surgery, and the outcomes of surgical correction. Third, this trend has been observed in one regional province and may need larger studies before it can be applied globally.
The present study, which require confirmation in future, showed different results compared with previous studies in IXT patients (9, 10, 12), moderate IXT may have lower rate of myopic progression in school-aged children. Myopic progression is influenced by a number of factors (24). Therefore, the impact of IXT with different severity on myopic progression should be further analyzed considering various influencing factors, which may provide helpful evidences in determining the optimal choice for IXT treatments.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Institutional Review Board of Zhongshan Ophthalmic Center, Sun Yat-sen University (2015MEKY055). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
TS and ML conceived the study design. ML and LC collected data. ML analyzed the data. TS drafted and reviewed the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by Guangzhou Municipal Science and Technology Project (TS, 202201011225). The sponsor or funding organization had no role in the design or conduct of this research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2023.1192387/full#supplementary-material
References
1. Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. (2016) 123(5):1036–42. doi: 10.1016/j.ophtha.2016.01.006
2. Sankaridurg P, Tahhan N, Kandel H, Naduvilath T, Zou H, Frick KD, et al. IMI impact of myopia. Invest Ophthalmol Vis Sci. (2021) 62(5):2. doi: 10.1167/iovs.62.5.2
3. Govindan M, Mohney BG, Diehl NN, Burke JP. Incidence and types of childhood exotropia: a population-based study. Ophthalmology. (2005) 112(1):104–8. doi: 10.1016/j.ophtha.2004.07.033
4. Chia A, Roy L, Seenyen L. Comitant horizontal strabismus: an Asian perspective. Br J Ophthalmol. (2007) 91(10):1337–40. doi: 10.1136/bjo.2007.116905
5. Ip JM, Robaei D, Kifley A, Wang JJ, Rose KA, Mitchell P. Prevalence of hyperopia and associations with eye findings in 6- and 12-year-olds. Ophthalmology. (2008) 115(4):678–85.e1. doi: 10.1016/j.ophtha.2007.04.061
6. Logan NS, Radhakrishnan H, Cruickshank FE, Allen PM, Bandela PK, Davies LN, et al. IMI accommodation and binocular vision in myopia development and progression. Invest Ophthalmol Vis Sci. (2021) 62(5):4. doi: 10.1167/iovs.62.5.4
7. Walsh LA, LaRoche GR, Tremblay F. The use of binocular visual acuity in the assessment of intermittent exotropia. J AAPOS. (2000) 4(3):0154–7. doi: 10.1016/S1091-8531(00)70005-X
8. Horwood AM, Riddell PM. Evidence that convergence rather than accommodation controls intermittent distance exotropia. Acta Ophthalmol. (2012) 90(2):e109–17. doi: 10.1111/j.1755-3768.2011.02313.x
9. Ekdawi NS, Nusz KJ, Diehl NN, Mohney BG. The development of myopia among children with intermittent exotropia. Am J Ophthalmol. (2010) 149(3):503–7. doi: 10.1016/j.ajo.2009.10.009
10. Shin KH, Hyun SH, Kim IN, Paik HJ. The impact of intermittent exotropia and surgery for intermittent exotropia on myopic progression among early school-aged children with myopia. Br J Ophthalmol. (2014) 98(9):1250–4. doi: 10.1136/bjophthalmol-2013-304777
11. Park Y, Ahn YJ, Park SH, Shin SY. Interocular difference associated with myopic progression following unilateral lateral rectus recession in early school-aged children. Jpn J Ophthalmol. (2019) 63(6):474–82. doi: 10.1007/s10384-019-00689-0
12. Moon Y, Kim JH, Lim HT. Difference in myopia progression between dominant and non-dominant eye in patients with intermittent exotropia. Graefes Arch Clin Exp Ophthalmol. (2020) 258(6):1327–33. doi: 10.1007/s00417-020-04700-0
13. Shen T, Chen J, Kang Y, Deng D, Lin X, Wu H, et al. Surgical treatment versus observation in moderate intermittent exotropia (SOMIX): study protocol for a randomized controlled trial. Trials. (2023) 24(1):153. doi: 10.1186/s13063-023-07189-0.36855155
14. Tsuneyoshi Y, Negishi K, Tsubota K. Importance of accommodation and eye dominance for measuring objective refractions. Am J Ophthalmol. (2017) 177:69–76. doi: 10.1016/j.ajo.2017.02.013
15. Goss DA, Winkler RL. Progression of myopia in youth: age of cessation. Am J Optom Physiol Opt. (1983) 60(8):651–8. doi: 10.1097/00006324-198308000-00002
16. Saw S-M, Shih-Yen EC, Koh A, Tan D. Interventions to retard myopia progression in children: an evidence-based update. Ophthalmology. (2002) 109(3):415–21; discussion 422–4; quiz 425–6, 443. doi: 10.1016/s0161-6420(01)00972-1
17. Group C. Myopia stabilization and associated factors among participants in the correction of myopia evaluation trial (COMET). Invest Ophthalmol Vis Sci. (2013) 54(13):7871–84. doi: 10.1167/iovs.13-12403
18. Saw SM, Nieto FJ, Katz J, Schein OD, Levy B, Chew SJ. Factors related to the progression of myopia in Singaporean children. Optom Vis Sci. (2000) 77(10):549–54. doi: 10.1097/00006324-200010000-00009
19. Economides JR, Adams DL, Horton JC. Capturing the moment of fusion loss in intermittent exotropia. Ophthalmology. (2017) 124(4):496–504. doi: 10.1016/j.ophtha.2016.11.039
20. Mestre C, Neupane S, Manh V, Tarczy-Hornoch K, Candy TR. Vergence and accommodation responses in the control of intermittent exotropia. Ophthalmic Physiol Opt. (2023) 43(4):598–614. doi: 10.1111/opo.13093.36692334
21. Lee D, Kim M, Kim WJ, Kim MM. Changes in refractive error and axial length after horizontal muscle surgery for strabismus. J AAPOS. (2019) 23(1):20.e1–5. doi: 10.1016/j.jaapos.2018.08.010
22. Lee DC, Lee SY. Analysis of astigmatism outcomes after horizontal rectus muscle surgery in patients with intermittent exotropia. PLoS One. (2020) 15(10):e0240026. doi: 10.1371/journal.pone.0240026
23. Hong SW, Kang NY. Astigmatic changes after horizontal rectus muscle surgery in intermittent exotropia. Korean J Ophthalmol. (2012) 26(6):438–45. doi: 10.3341/kjo.2012.26.6.438
Keywords: intermittent exotropia, myopic progression, strabismus surgery, school-aged children, spherical equivalent
Citation: Shen T, Liang M and Chen L (2023) Myopic progression in school-aged children with moderate intermittent exotropia. Front. Pediatr. 11:1192387. doi: 10.3389/fped.2023.1192387
Received: 23 March 2023; Accepted: 7 August 2023;
Published: 16 August 2023.
Edited by:
Momcilo Jankovic, Fondazione MBBM, ItalyReviewed by:
Azim Siraj Azimuddin, Ministry of Health, BruneiManoj K. Manoharan, L V Prasad Eye Institute, India
© 2023 Shen, Liang and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tao Shen c2hlbnRhb0BtYWlsMi5zeXN1LmVkdS5jbg==
 Tao Shen
Tao Shen Mintong Liang
Mintong Liang