
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Pediatr., 05 June 2023
Sec. Children and Health
Volume 11 - 2023 | https://doi.org/10.3389/fped.2023.1181186
 Bo Peng1,2
Bo Peng1,2 Kara K. L. Reeves3,4*
Kara K. L. Reeves3,4* Shara W. Y. Lee5
Shara W. Y. Lee5 Tina H. Y. Chung3
Tina H. Y. Chung3 Heidi W. L. Hui3
Heidi W. L. Hui3 Alfred H. L. Leung3
Alfred H. L. Leung3 Johnson C. Y. Pang3,4
Johnson C. Y. Pang3,4
Introduction: The COVID-19 pandemic has impacted children and adolescents’ physical activity (PA), sleeping patterns, and psychological and behavioral health. Yet, little is known about the differences between those in countries with various economic statuses.
Methods: Articles published from database inception through 16 March 2022 were retrieved using CINAHL Complete, Cochrane Library, EMBASE, Medline, PubMed, and PsycINFO. High-quality studies that reported the number of participants with parameters associated with PA, sleeping patterns, and psychological and behavioral problems in young people aged under 18 years during the pandemic were included. We referenced the Canadian 24-Hour Movement Guidelines for PA and sleep duration to provide the event rate for young people who were not compliant with the guidelines. The event rate of young people who had decreased sleep quality and experienced psychological and behavioral problems were also investigated. A subgroup analysis was conducted to identify the differences in those in countries with diverse economic statuses. Funnel plot analysis and Egger's test were also conducted to identify any risk of publication bias.
Result: A total of 66 studies with 1,371,168 participants aged between 0 and 18 years, involving 27 countries, were included. During the pandemic, we identified that 41% (95% CI: 39%, 43%; I2 = 96.62) and 43% (95% CI: 34%, 52%; I2 = 99.42) of young people did not meet the PA and sleep duration recommendation guidelines. In addition, 31% (95% CI: 28%, 35%; I2 = 99.66) of young people had decreased their sleep quality. Yet, no significant difference was found across countries with different economic statuses. However, the event rates of participants with psychological and behavioral problems were 32% (95% CI: 28%, 36%; I2 = 99.85) and 19% (95% CI: 14%, 25%; I2 = 99.72), respectively. In addition, the rate of psychological problems was more severe in those who live in lower middle-income countries (p < 0.001), while the rate of behavioral problems was more severe in those who live in high-income countries (p = 0.001).
Discussion: During the pandemic, the discouragement of PA, poor sleep quality, and high risk of psychological and behavioral problems are concerning. A large number of young people did not comply with the recommendation guidelines. Timely implementation of recovery plans is critical to address the adverse effects on young people.
Systematic review registration: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=309209, identifier CRD42022309209.
The COVID-19 pandemic is considered the most severe health crisis in the century (1) due to its high transmission rate, constant viral evolution and mutation, and high rate of reinfection (2). The emergence of SARS-CoV-2 variants was responsible for sequential waves of infections across the globe (3). As of 8 May 2022, there were 517,072,612 confirmed cases and 6,275,907 deaths reported around the world, affecting over 226 countries and regions (4). In response to the pandemic, many countries have implemented numerous strategies such as social distancing, closure of schools and public places, home isolation, or even lockdown to prevent community transmission. Consequently, the ongoing pandemic has brought severe adverse impacts to the health systems and economies worldwide.
There are a growing number of studies examining the impact of the pandemic on physical activity (PA) and mental health among children and adolescents. A scoping review reported that a reduction in PA was reported in 57 (out of 74) studies in children and adolescents during the pandemic (5). Among the 57 studies, the decrease in time spent on PA ranged between 45 min and 91 min per day (5). Another meta-analysis reported a significant drop in the frequency of moderate-to-vigorous activities and step counts for those aged from 4 to 18 years (6). A decrease in PA has been significantly associated with psychological problems, including anxiety and depression symptoms, in children and adolescents during the pandemic (7, 8). A large meta-analysis reported that the prevalence of anxiety and depression among children and adolescents could reach 19% [95% confidence interval (CI): 14%, 25%, data from 22 studies] and 15% (95% CI: 10%, 21%, data from 16 studies), respectively (9). In addition, social isolation and quarantine induce negative behavioral impacts, such as irritability and inattention (9), sleep disturbance (9), screen time (10), change in dietary habits, and weight gain (11).
Several studies investigated the changes in PA and psychological health during the pandemic (6, 8, 12–15). PA has been shown to positively influence psychological and emotional health, cognitive function, and sleep quality (16). A systematic review indicated that PA improved psychological health in children and adolescents during the pandemic (17). Moreover, a lower level of anxiety, higher level of wellbeing, and better sleep quality were found in active adult participants, compared to those of the less active ones (18). The pandemic has affected the participation of PA in children and adolescents. Yet, PA remained beneficial to psychological health and sleep quality and should be encouraged. To promote participation in PA, Canada has issued the 24-Hour Movement Guidelines for children and youth (19), while the WHO released guidelines on physical activity, sedentary behavior, and sleep for preschool-aged children in 2019 (20) and updated the guidelines for children and adolescents in 2020 (21). Both guidelines recommend ≥180 min spent in a variety of physical activities including ≥60 min spent in moderate-to-vigorous PA for children under 5 years of age and at least 60 min per day of moderate-to-vigorous PA for children and youths over 5 years of age. However, some studies referenced the guidelines as outcome measures for PA during the pandemic (12–24). To the best of our knowledge, there is currently no systematic review and meta-analysis to investigate the rate of children and adolescents who were not meeting the guidelines. As the guidelines are important tools developed by the consensus of multiple experts and popularized in various countries, it is essential to gain insight into the rate of children and adolescents who were not compliant with the guidelines during the pandemic.
We also noticed that health inequities between different countries have undermined the efforts to bring the pandemic under control, including therapeutics, diagnostics, and distribution of vaccines. Historically, the infection and mortality rates were high among the most disadvantaged communities during the health crisis (25). A regression analysis involving 83 countries reported that a greater healthcare capacity was associated with fewer COVID-19 case fatalities [incidence rate ratio (IRR) = 0.5811] (26). Meanwhile, studies revealed that PA has decreased especially with a lower socioeconomic background (5). However, no study to date has investigated the differences between countries’ economic status and PA, sleeping patterns, and psychological and behavioral problems in children and adolescents during the pandemic.
This meta-analysis aimed to identify the event rate of children and adolescents who were not meeting the Canadian 24-Hour Movement Guidelines in PA and sleep duration, as well as the changes in PA levels, sleeping patterns, and psychological and behavioral problems in countries with different economic statuses during the pandemic. Alike to distinctions in infection rate and socioeconomic status, we hypothesized that there would be differences in all the outcomes across countries with different economic statuses. Particularly, the event rate of children and adolescents who were unable to meet the Canadian 24-Hour Movement Guidelines in PA and sleep duration were high during the pandemic. We also hypothesized that the event rates of decreased PA, sleep duration, and poor sleep quality were different among countries with different economic statuses and the event rates of psychological and behavioral problems during the pandemic were different among countries with different economic statuses.
This meta-analysis adhered to the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) and Meta-Analysis of Observational Studies in Epidemiology (MOOSE) guidelines. The protocol of this meta-analysis was published in the PROSPERO database (registration number: CRD42022309209). We systematically searched on CINAHL Complete, Cochrane Library, EMBASE, Medline, PubMed, and PsycINFO from database inception to 16 March 2022 without language restrictions for studies with quantitative data involving level of PA, sleeping patterns, and psychological and behavioral problems in children and adolescents (age ≤18 years) during the pandemic. For non-English articles, “Google Translate” was used, followed by a consultation of professional translations by native speakers. To ensure minimal missing data, we manually searched the reference list of all relevant studies. The search history is available in Supplementary Table S1, and the search terms are documented in Supplementary Table S2.
Studies that reported the number of participants with parameters associated with PA, sleeping patterns, and psychological and behavioral problems in young people aged under 18 years during the pandemic were included in this meta-analysis. Studies that involved participants who were not representable for the general young people population, such as studies that exclusively involved participants with pre-existing physiological or psychological health problems or student-athletes, were excluded. Abstracts, editorial comments, and unpublished studies were also excluded.
The quality of the included articles was assessed by two independent reviewers with reference to the following six items from the Downs and Black assessment tool adopted by the literature (27–29): (1) clearly stated aim; (2) clearly defined study population; (3) study sample representative of the source population; (4) attempt made to adjust for confounding; (5) attempt made to validate survey responses to intuitional records where possible; and (6) discussion of study limitations. One point was given for an item rated as yes and zero for an item rated as no or unable to determine. Studies that scored 5–6 points, 3–4 points, and 2 or lower points are considered high, moderate, and low quality, respectively. The certainty assessment followed the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach (30). The GRADE consists of four levels of certainty of evidence: very low, low, moderate, and high. The levels were assessed with five criteria: risk of bias, inconsistency, indirectness, imprecision, and publication bias. Each outcome was assessed by all criteria, and the overall score was taken by the lowest score of each criterion. A third reviewer resolved any disagreements regarding the scoring of the included studies.
With reference to the inclusion and exclusion criteria, the titles and abstracts for potential studies were screened by two independent reviewers, and the full texts of the remaining articles were evaluated. Disagreements were resolved by a third reviewer. The relevant data were extracted in the included studies by the same reviewers using a standardized data retrieval sheet. The number of participants was extracted and separated into two groups based on their responses to the level of PA, sleeping patterns, and psychological and behavioral problems during the pandemic.
PA level: We followed the Canadian 24-Hour Movement Guidelines to separate participants into either a “meeting recommendation” group or “not meeting recommendation” group if appropriate (19). The guidelines recommend participants aged 1–2 years to have at least 180 min spent in a variety of physical activities at any intensity, including energetic play and spread throughout the day; aged 3–4 years to have at least 180 min spent in a variety of physical activities including at least 60 min spent in moderate-to-vigorous physical activities; and aged 5–17 years to have at least 60 min per day of moderate-to-vigorous physical activity (19). For dichotomous and polychotomous variables that did not report data reflecting the Canadian 24-Hour Movement Guidelines, we separated participants into two groups: decreased and/or no participation in PA and increased and/or no change in participation in PA. The number of participants who had decreased PA, no participation in PA, or not meeting the recommendation guidelines was compared to the number of those who had increased or no change in PA or meeting the recommendation guidelines.
Sleeping pattern: For sleep duration, we followed the Canadian 24-Hour Movement Guidelines (19). The guidelines recommend participants aged 1–2 years to have 11–14 h; aged 3–4 years to have 10–13 h; aged 5–13 years to have 9–11 h; and aged 14–17 years to have 8–10 h of sleep per day (19). We separated the participants into either the “meeting recommendation” group or the “not meeting recommendation” group. For those studies that did not provide data indicating the guidelines, we separated participants into two groups: having changes in sleep duration and no change in sleep duration. For sleep quality, we separated participants into two groups: worsened sleep quality and improved and/or no change in sleep quality. The number of participants who had changes in sleep duration, were not meeting recommendation guidelines, and had decreased sleep quality was compared to the number of those who had no change in sleep duration, were meeting the recommendation guidelines, and had no change or improved sleep quality.
Psychological and behavioral problems: We separated participants who were at risk or had an increase of psychological or behavioral problems into one group and who were at no risk or had a decrease of or no change in psychological or behavioral problems into another group. The number of participants with psychological or behavioral problems was compared to the number of those without psychological or behavioral problems.
In addition, confounding variables including countries’ economic status were assessed by a subgroup analysis. With reference to World Bank (2020), countries’ economic statuses were separated into four income groups: low-, lower middle-, upper middle-, and high-income countries (31). The classifications were based on gross national income per capita in current US dollars with less than 1,036, 1,036–4,045, 4,046–12,535, and more than 12,535 dollars for low-, lower middle-, upper middle-, and high-income countries, respectively (31). The authors of selected articles would be contacted, and any missing data were reported if applicable.
Comprehensive Meta-Analysis version 3.0 (BioStat, Englewood, NJ, United States) was used for statistical analysis. The targeted outcomes were presented as event rates with 95% confidence intervals (CIs) and presented in forest plots. Heterogeneity was reported as I2, and a random effect model was selected if heterogeneity was 50% or above. The subgroup analysis was performed and compared by countries’ income levels. Funnel plot analysis was implemented to assess the risk of publication bias. Egger's test was conducted to identify any risk of publication bias, with p ≤ 0.05 considered a potential publication bias. If publication bias was indicated, the trim-and-fill method was used to recompute the combined effect. A sensitivity analysis was implemented to assess the robustness of all outcomes.
A total of 12,731 studies were retrieved from the databases. After excluding 5,415 duplicated studies, another 7,027 studies were excluded by screening the titles and abstracts. Furthermore, 227 studies were removed after assessing the full tests based on the inclusion and exclusion criteria. Finally, a total of 66 studies were included in our meta-analysis (22–24, 32–94). The PRISMA flowchart of the study selection is presented in Figure 1, and the reasons for exclusion are documented in Supplementary Table S3. No authors were contacted as it was unnecessary in this study.
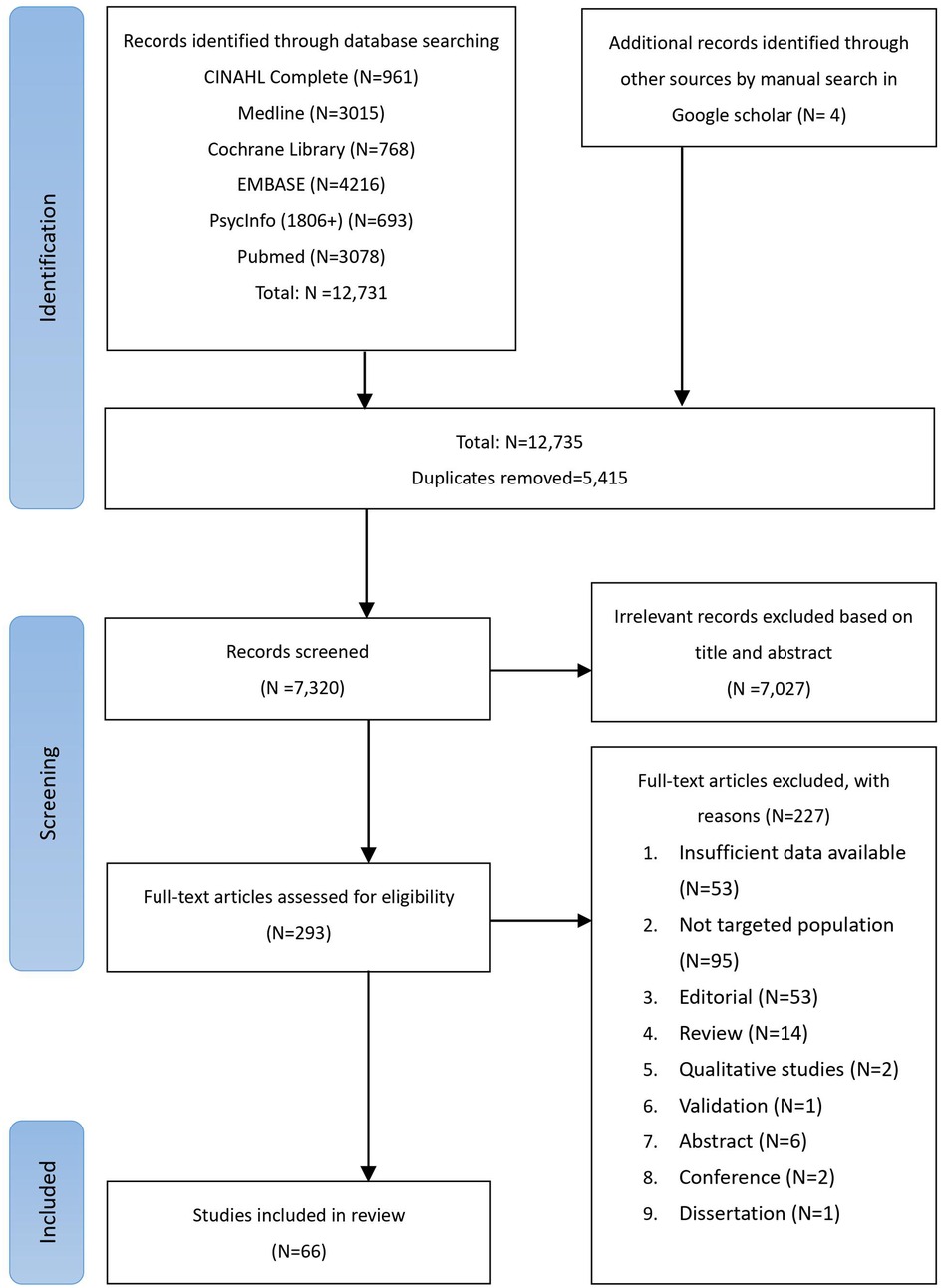
Figure 1. PRISMA flowchart of study selection. PRISMA, Preferred Reporting Items for Systematic Review and Meta-Analyses.
A total of 1,371,168 participants aged between 0 and 18 years, involving 27 countries, were included, most of which had the data collection period conducted in 2020. The characteristics of the included studies are described in Table 1. Most studies utilized a validated or self-designed questionnaire as a measuring tool for outcome measurement. Three studies used a wrist-worn accelerometer to measure PA levels or sleep duration (22, 52, 55), and one study employed a direct observational approach to measure PA levels (62). The number of participants, details of the measurement parameters, and tools in each group are tabulated in Supplementary Tables S4–S8.
The overall quality grading of included studies was moderate to high based on the six items in the Downs and Black assessment tool. Most studies failed to score on item 4, which was related to failure to attempt to adjust for confounding. Some studies did not use validated questionnaires for data collection, therefore failed to score on item 5. As for the certainty of outcomes, all outcomes were graded as moderate, which was mostly due to high inconsistency with I2 > 90% and a moderate risk of bias. The Downs and Black assessment of all included studies and the GRADE score of all outcomes are presented in Supplementary Tables S9 and S10, respectively.
The event rates of participants not meeting the recommendation guidelines of PA level and sleep duration during the pandemic are presented in forest plots in Figures 2, 3. The event rates of participants not meeting the PA and sleep duration recommendation guidelines were 41% (95% CI: 39%, 43%; I2 = 96.62) and 43% (95% CI: 34%, 52%; I2 = 99.42), respectively. In the subgroup analysis, we could only retrieve data for high- and upper middle-income countries. The event rates of participants not meeting PA recommendation guidelines were 40% (95% CI: 37%, 42%; I2 = 95.94) for high-income countries and 44% (95% CI: 40%, 48%; I2 = 98.78) for upper middle-income countries. Likewise, the event rates of participants not meeting the sleep duration recommendation guidelines were 53% (95% CI: 41%, 65%; I2 = 99.48) for high-income countries and 31% (95% CI: 20%, 43%; I2 = 98.78) for upper middle-income countries. No significant difference was observed between the income level countries in meeting the recommendation guidelines of PA level (p = 0.063) and sleep duration (p = 0.172).
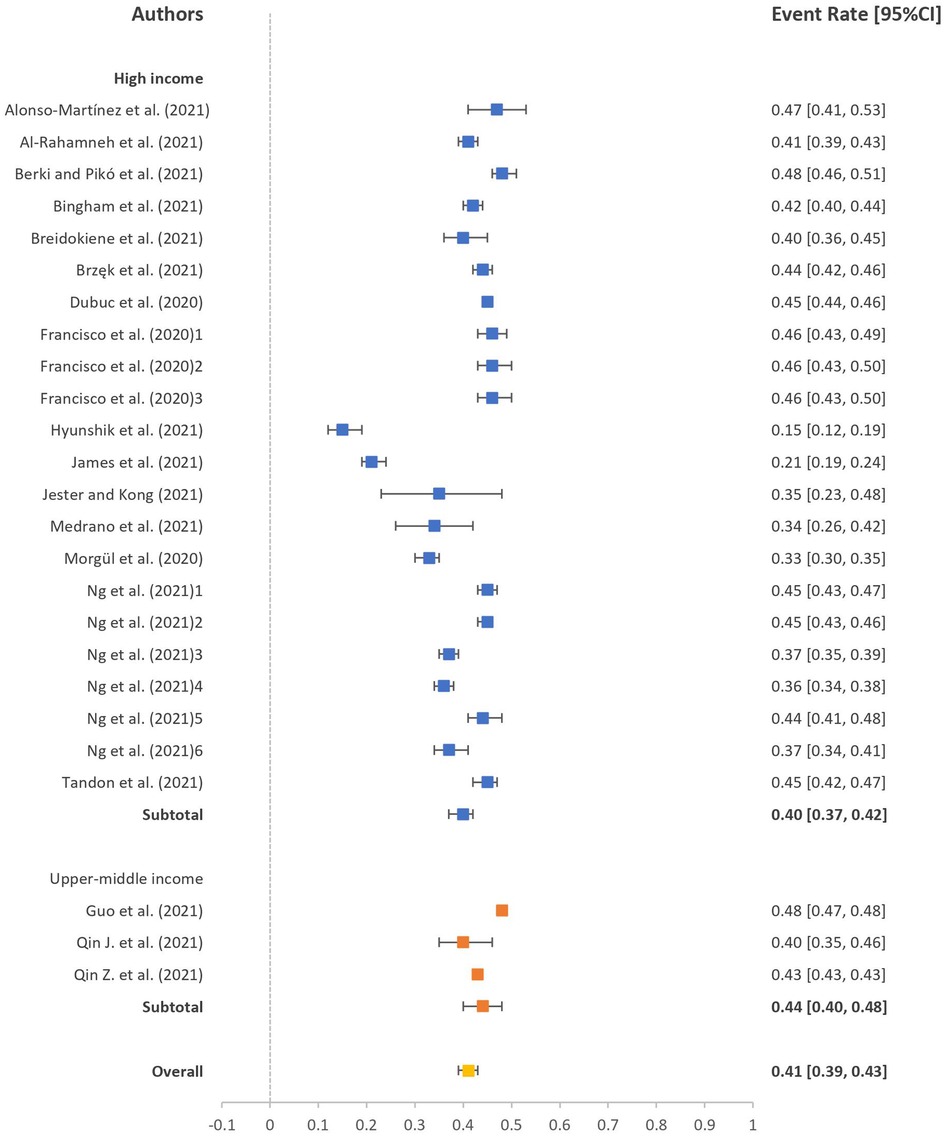
Figure 2. Event rate of participants not meeting PA recommendation guidelines. PA, physical activity.
The pooled event rates of participants with decreased PA, with no participation in PA, or who are not meeting the PA recommendation guidelines and with changes in sleep duration and sleep quality during the pandemic are presented in forest plots in Supplementary Figures S1–S3. Among them, the event rate was 61% (95% CI: 58%, 65%; I2 = 99.64) for participants with decreased PA, 34% (95% CI: 26%, 42%; I2 = 99.88) for participants with changes in sleep duration, and 31% (95% CI: 28%, 35%; I2 = 99.66) for participants with poorer sleep quality. We were able to conduct the subgroup analysis for high-, upper middle-, and lower middle-income countries for the pooled PA level. The event rates of participants with decreased PA levels were 60% (95% CI: 56%, 64%; I2 = 99.33) for high-income countries, 63% (95% CI: 55%, 70%; I2 = 99.88) for upper middle-income countries, and 79% (95% CI: 10%, 99%; I2 = 98.57) for lower middle-income countries. No significant difference was seen among the three income levels (p = 0.769). As for the pooled sleep duration and sleep quality, the event rate of participants with changes in sleep duration was 40% (95% CI: 30%, 52%; I2 = 99.81) for high-income countries and 25% (95% CI: 16%, 37%; I2 = 99.62) for upper middle-income countries, and that of participants with poorer sleep quality was 37% (95% CI: 24%, 51%; I2 = 99.73) for high-income countries and 31% (95% CI: 28%, 35%; I2 = 97.50) for upper middle-income countries. No significant difference was seen among income level countries in sleep duration (p = 0.059) and sleep quality (p = 0.397).
The event rates of participants with psychological and behavioral problems during the pandemic are presented in a forest plot (Supplementary Figures S4, S5). The event rates of participants with psychological and behavioral problems were 32% (95% CI: 28%, 36%; I2 = 99.85) and 19% (95% CI: 14%, 25%; I2 = 99.72), respectively. In the subgroup analysis, the event rates of participants with psychological problems were 45% (95% CI: 38%, 52%; I2 = 99.16) for high-income countries, 24% (95% CI: 20%, 29%; I2 = 99.91) for upper middle-income countries, and 70% (95% CI: 42%, 88%; I2 = 97.57) for lower middle-income countries. We observed a significant difference among all three income levels (p < 0.001), between high-income and upper middle-income countries (p < 0.001), and between upper middle- and lower middle-income countries (p = 0.001). However, there was no significant difference between high-income and lower middle-income countries (p = 0.087). For behavioral problems, the event rates of participants with behavioral problems were 27% (95% CI: 19%, 36%; I2 = 99.75) for high-income countries and 9% (95% CI: 5%, 16%; I2 = 99.66) for upper middle-income countries. Similarly, we identified a significant difference between both income level countries (p = 0.001).
Publication bias was evaluated by funnel plot and Egger's test. The funnel plots of all outcomes are presented in Supplementary Figure S6. The funnel plots and Egger's test indicated that there was publication bias among the studies on participants with decreased PA (p = 0.008), changes in sleep duration (p = 0.001), and psychological problems during the pandemic (p < 0.001). However, other outcomes resided in symmetric funnel plots shape and results of Egger's test showed no significant publication bias (PA guidelines, p = 0.220; sleep duration guidelines, p = 0.270; sleep quality, p = 0.432; behavioral problems, p = 0.673). After adjustment using the trim-and-fill method, the event rates were 61% (95% CI: 57%, 64%) instead of 61% (95% CI: 58%, 65%) for participants with decreased PA level and 27% (95% CI: 24%, 30%) instead of 32% (95% CI: 28%, 36%) for participants with psychological problems. However, the event rate for changes in sleep duration remained unchanged after the trim-and-fill method.
The robustness of our results was examined by the leave-out-one sensitivity analysis. Our results were not modified with the stepwise exclusion of each study. More details are displayed in Supplementary Table S11.
The current systematic review and meta-analysis explored the effects of the pandemic on PA, sleep duration, and sleep quality, as well as psychological and behavioral problems among children and adolescents in countries with different economic statuses. We have identified the event rate of children and adolescents who were not compliant with the Canadian 24-Hour Movement Guidelines in PA and sleep duration in countries during the pandemic. We have also provided the event rate of children and adolescents with discouraging PA performance including decreased PA, no participation in PA, or not meeting the recommendation guidelines, changes in sleeping patterns, and psychological and behavioral problems in countries with different economic statuses during the pandemic. To the best of our knowledge, this is the first meta-analysis that objectively examines the effect of the pandemic on these parameters for young people living in different countries with different economic statuses.
Our results supported the hypothesis that the event rates of children and adolescents who were unable to meet the Canadian 24-Hour Movement Guidelines in PA and sleep duration were high during the pandemic. However, although we hypothesized there would be differences in those across countries with different economic statuses, our results had shown otherwise. Decreased PA during the pandemic and failure to comply with the PA recommendation guidelines were reported during the pandemic (5, 95). This was also reflected in our results with 61% (95% CI: 58%, 65%) of children and adolescents with discouraging PA performance and 41% (95% CI: 39%, 43%; I2 = 96.62) of children and adolescents who did not meet the PA recommendation guidelines during the pandemic. However, no significant difference was found among countries with high-, upper middle-, and lower middle-income groups for the pooled PA (p = 0.769) and compliance with PA recommendation guidelines (p = 0.063).
In addition, 43% (95% CI: 34%, 52%; I2 = 99.42) of children and adolescents did not meet the guidelines for sleep duration, and 34% (95% CI: 26%, 42%; I2 = 99.88) of them had changed, either increased or decreased, their sleep duration during the pandemic. However, there was no significant difference in sleep duration among countries with different economic statuses (p = 0.432). These findings were in line with a previous systematic review that reported sleep duration did not change in 43% of participants on weekdays and in 46.2% on weekends (96). During the pandemic, home confinement negatively affected families’ incomes that had relevant impacts on the socioeconomic context, especially among the people who live in low-income countries and suffer from aggravating social and health inequalities (97). It was plausible that preschoolers with lower-income parents were less likely to have adequate PA and poorer sleep quality during the pandemic (98). However, our systematic review and meta-analysis found that people living with different incomes did not show a significant difference in PA. In addition, the pooled event rate of the low sleep quality was 31% (95% CI: 28%, 35%; I2 = 99.66). Similarly, there was no significant difference among the countries with different incomes (p = 0.307). The results supported that the decrease in PA, sleep duration, and sleep quality in young people is not associated with the incomes of the countries that they are living in. Contrariwise, our results may be biased because there were scanty studies included from lower middle-income countries, and no studies could be found from low-income countries.
A systematic review of recent studies showed that psychological problems were often found during lockdown or social isolation periods (99). Similar findings were observed in our systematic review and meta-analysis in which the pooled event rate of psychological problems was 32% (95% CI: 28%, 36%; I2 = 99.85). Our results also partially supported the hypothesis that the event rates of psychological and behavioral problems were different among countries with different economic statuses (100–102). In the subgroup analysis, there were significant differences in the event rates between high-income and upper middle-income countries and between upper middle-income and lower middle-income countries for psychological problems (both p < 0.001). However, there was no significant difference in the event rate between high-income and lower middle-income countries for psychological problems. Although the inconsistency might be due to the limited number of studies for lower middle-income countries, the event rate for children and adolescents in middle lower-income countries remains the highest at 70% (95% CI: 42%, 88%; I2 = 97.57) among the event rates of those in high- and upper middle-income countries. As a result, this meta-analysis provides evidence that the socioeconomic context can influence psychological problems among young people and the mental health needs of children and adolescents were high, especially in middle lower-income countries (103, 104).
Throughout the pandemic, authorities have implemented measures for protection such as social restrictions and self-isolation, which could explain the increased behavioral problems among young people (105). Our findings supported that 19% (95% CI: 14%, 25%; I2 = 99.72) of children and adolescents had behavioral problems during the pandemic. Although most countries applied restrictive measures to control the spread of the virus, we found that the influence on behavioral problems among young people in high- and upper middle-income countries differ significantly (p = 0.001). Household income is an important part of the family socioeconomic status that is associated with behavior problems of young people (106, 107). Young people living in lower-income countries may have more stress responses induced by fears of infection, lack of personal space, and family financial situation (108, 109), resulting in prolonged effects on mental wellbeing such as an increase in social isolation and mood disturbances (110). As a result, a higher rate of behavioral problems can be found during the pandemic in lower-income countries. However, our findings showed that behavioral problems among young people in high-income countries were unexpectedly higher with 27% (95% CI: 19%, 36%; I2 = 99.75) than those among young people in upper middle-income countries with 9% (95% CI: 5%, 16%; I2 = 99.66). This may result from the influence of this pandemic and its measures on parents and young people. The diversity of infection rates and different protective measures may contribute more impacts on behavioral problems among young people in high-income countries than in lower-income countries. However, a recent study reported that an increase in income is unrelated to behavioral problems in children and adolescents during the pandemic (111). Furthermore, a meta-analysis revealed that to positively influence the psychological and behavioral health of children and adolescents, a combined intervention including economic support and social care is critical (112). An economic intervention, such as cash allowance, alone was ineffective and inadequate, despite encouraging an increase in spending among children and adolescents, which showed no significant impact on mental health (112). Moreover, it is stated that one in eight children has mental health disorders in high-income countries that require interventions (113). Yet, even in high-income countries, most are not receiving adequate services (113). However, this meta-analysis only identified statistics in high-income countries (113). We novelty compared the event rate in countries with different income levels, and the results were aligned. The rate of young people with behavioral problems was higher in high-income countries. We urge policymakers to assess risk and strategically allocate finite resources for interventions. Particularly, monetary support alone was inadequate, and a holistic approach including public investment and promotion in mental health services and community support is needed. Further studies are recommended to identify the influences of the pandemic on young people's behaviors and propose all-rounded solutions to the impending behavioral problems in the long run.
Furthermore, the reduction in exercise duration (114) and longer periods of sedentary behavior in young people may induce serious health burdens to society (115, 116). Sleep duration and sleep quality closely affect psychological wellbeings and behavioral conduct, such as the ability to control inner states or responses toward thoughts, attention, emotions, or even performance (117, 118). Our findings observed that 32% and 19% of the young population experienced psychological and behavioral problems, respectively, during the pandemic and were associated with the economic status of the country. The crisis of the pandemic induced a sharp reduction of fiscal revenues for different countries, especially in countries with lower middle- and low-income groups, which result in an added burden to the most vulnerable individuals, including children and adolescents (119). The increase in poverty and inequality induced by the pandemic may change the quantity and nature of PA and sleeping patterns among young people. In addition, the rate of psychological and behavioral problems among young people during the pandemic was alarming and urged policymakers, scientists, and practitioners to identify solutions for attenuating the adverse changes (120).
The studies included in this meta-analysis only represented high-, upper middle-, and lower middle-income countries. No study reported our targeted outcomes in low-income countries. The impacts of poverty and inequality induced by the pandemic on the PA, sleeping patterns, psychological wellbeings, and behavioral changes in children and adolescents in low-income countries are unknown. This could be attributed to the limited data retrieved in the included studies that met our inclusion criteria. In addition, although we searched six scientific databases with no language restriction, we expected that the findings may cover nearly all relevant published articles. There was an inevitable possibility that additional relevant articles might have been missed due to the restriction of our search to these six databases. However, we minimized the possibility of missing data by manually searching the reference lists of all relevant studies. Therefore, we believed that the number of studies missing from our meta-analysis was likely small and would have a limited impact on our results. Lastly, our outcomes showed high heterogenicity (I2 > 90%). This is expected as the outcome measures used to measure PA, sleeping patterns, and psychological and behavioral problems were diversified. We attempted to control the influences of high heterogenicity by using a random effect model and assessed the publication bias with funnel plots and Egger's test. Moreover, potential publication bias is a factor that should be taken seriously, as it could easily exaggerate the effects when none exists. We have adjusted the results with the trim-and-fill method to lessen the publication bias, but the potential influence of publication bias should, nevertheless, be cautious when interpreting the results, especially for the event rate for changes in sleep duration.
The discouragement of PA during the pandemic has affected young people negatively. Changes in PA levels, sleep duration, poorer sleep quality, and psychological and behavioral problems were seen among young people in countries with different economic statuses. Moreover, 41% of the young population did not meet the recommendations for PA, and 43% of the young population did not meet the recommendations for sleep duration during the pandemic. In addition, the rate of psychological problems was more severe in those who live in lower middle-income countries, while the rate of behavioral problems was more severe in those who live in high-income countries. Also, studies on the changes in PA, sleep duration, sleep quality, and psychological and behavioral problems in lower middle- and low-income countries were scanty. Further studies are necessary to investigate the impacts of the pandemic on children and adolescents, especially in lower middle- and low-income countries.
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary Material.
BP initiated this study. All authors contributed to the design of the meta-analysis and performed the literature search. JP and KR performed the selection and interpretation of data and drafted the manuscript including tables and figures. All authors contributed to critical revision of the manuscript. All authors contributed to the article and approved the submitted version.
This study was supported by a grant from the Caritas Institute of Higher Education for publication (reference codes IDG210101 and IDG220228P).
The authors would like to acknowledge Charis Pang Wai Yue for her contributions to the study design and editing of the figures and tables.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2023.1181186/full#supplementary-material.
1. World Health Organization. Weekly epidemiological update on COVID-19—4 May 2022. (2022). Available online at: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19—4-may-2022 (accessed on 7 May 2022).
2. van Kampen JJ, van de Vijver DA, Fraaij PL, Haagmans BL, Lamers MM, Okba N, et al. Duration and key determinants of infectious virus shedding in hospitalized patients with coronavirus disease-2019 (COVID-19). Nat Commun. (2021) 12(1):1–6. doi: 10.1038/s41467-020-20568-4
3. Khan NA, Al-Thani H, El-Menyar A. The emergence of new SARS-CoV-2 variant (omicron) and increasing calls for COVID-19 vaccine boosters-the debate continues. Travel Med Infect Dis. (2022) 45:102246. doi: 10.1016/j.tmaid.2021.102246
4. Worldometers T. COVID-19 coronavirus pandemic (2022). Available at: https://www.worldometers.info/coronavirus/. (accessed on 12th May 2022).
5. Rossi L, Behme N, Breuer C. Physical activity of children and adolescents during the COVID-19 pandemic—a scoping review. Int J Environ Res Public Health. (2021) 18(21):11440. doi: 10.3390/ijerph182111440
6. Wunsch K, Kienberger K, Niessner C. Changes in physical activity patterns due to the COVID-19 pandemic: a systematic review and meta-analysis. Int J Environ Res Public Health. (2022) 19(4):2250. doi: 10.3390/ijerph19042250
7. Zhang X, Zhu W, Kang S, Qiu L, Lu Z, Sun Y. Association between physical activity and mood states of children and adolescents in social isolation during the COVID-19 epidemic. Int J Environ Res Public Health. (2020) 17(20):7666. doi: 10.3390/ijerph17207666
8. Pang JCY, Chan ELS, Lau HMC, Reeves KKL, Chung TH, Hui HW, et al. The impacts of physical activity on psychological and behavioral problems, and changes in physical activity, sleep and quality of life during the COVID-19 pandemic in preschoolers, children, and adolescents: a systematic review and meta-analysis. Front Peadiatr. (2023) 11:1015943. doi: 10.3389/fped.2023.1015943
9. Dragioti E, Li H, Tsitsas G, Lee KH, Choi J, Kim J, et al. A large-scale meta-analytic atlas of mental health problems prevalence during the COVID-19 early pandemic. J Med Virol. (2022) 94(5):1935–49. doi: 10.1002/jmv.27549
10. Panda PK, Gupta J, Chowdhury SR, Kumar R, Meena AK, Madaan P, et al. Psychological and behavioral impact of lockdown and quarantine measures for COVID-19 pandemic on children, adolescents and caregivers: a systematic review and meta-analysis. J Trop Pediatr. (2021) 67(1):fmaa122. doi: 10.1093/tropej/fmaa122
11. Abdulsalam NM, Khateeb NA, Aljerbi SS, Alqumayzi WM, Balubaid SS, Almarghlani AA, et al. Assessment of dietary habits and physical activity changes during the full COVID-19 curfew period and its effect on weight among adults in Jeddah, Saudi Arabia. Int J Environ Res Public Health. (2021) 18(16):8580. doi: 10.3390/ijerph18168580
12. Stockwell S, Trott M, Tully M, Shin J, Barnett Y, Butler L, et al. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: a systematic review. BMJ Open Sport Exerc Med. (2021) 7(1):e000960. doi: 10.1136/bmjsem-2020-000960
13. Oostrom TG, Cullen P, Peters SA. The indirect health impacts of the COVID-19 pandemic on children and adolescents: a review. J Child Health Care. (2022):13674935211059980. doi: 10.1177/13674935211059980
14. Gjaka M, Feka K, Bianco A, Tishukaj F, Giustino V, Parroco AM, et al. The effect of COVID-19 lockdown measures on physical activity levels and sedentary behaviour in a relatively young population living in Kosovo. J Clin Med. (2021) 10(4):763. doi: 10.3390/jcm10040763
15. Lesser IA, Nienhuis CP. The impact of COVID-19 on physical activity behavior and well-being of Canadians. Int J Environ Res Public Health. (2020) 17(11):3899. doi: 10.3390/ijerph17113899
16. Dimitri P, Joshi K, Jones N. Moving more: physical activity and its positive effects on long term conditions in children and young people. Arch Dis Child. (2020) 105(11):1035–40. doi: 10.1136/archdischild-2019-318017
17. Okuyama J, Seto S, Fukuda Y, Funakoshi S, Amae S, Onobe J, et al. Mental health and physical activity among children and adolescents during the COVID-19 pandemic. Tohoku J Exp Med. (2021) 253(3):203–15. doi: 10.1620/tjem.253.203
18. Akbari HA, Pourabbas M, Yoosefi M, Briki W, Attaran S, Mansoor H, et al. How physical activity behavior affected well-being, anxiety and sleep quality during COVID-19 restrictions in Iran. Eur Rev Med Pharmacol Sci. (2021) 25(24):7847–57. doi: 10.26355/eurrev_202112_27632
19. Tremblay MS, Carson V, Chaput J-P, Connor Gorber S, Dinh T, Duggan M, et al. Canadian 24-hour movement guidelines for children and youth: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. (2016) 41(6):S311–27. doi: 10.1139/apnm-2016-0151
20. World Health Organization. Guidelines on physical activity, sedentary behaviour and sleep for children under 5 years of age: summary. World Health Organization. (2019). https://apps.who.int/iris/handle/10665/325147.
21. World Health Organization. WHO guidelines on physical activity and sedentary behaviour: web annex: evidence profiles. (2020).
22. Alonso-Martínez AM, Ramírez-Vélez R, García-Alonso Y, Izquierdo M, García-Hermoso A. Physical activity, sedentary behavior, sleep and self-regulation in Spanish preschoolers during the COVID-19 lockdown. Int J Environ Res Public Health. (2021) 18(2):1–8. doi: 10.3390/ijerph18020693
23. Brzęk A, Strauss M, Sanchis-Gomar F, Leischik R. Physical activity, screen time, sedentary and sleeping habits of Polish preschoolers during the COVID-19 pandemic and WHO’s recommendations: an observational cohort study. Int J Environ Res Public Health. (2021) 18(21):11173. doi: 10.3390/ijerph182111173
24. Francisco R, Pedro M, Delvecchio E, Espada JP, Morales A, Mazzeschi C, et al. Psychological symptoms and behavioral changes in children and adolescents during the early phase of COVID-19 quarantine in three European countries. Front Psychiatry. (2020) 11:1329. doi: 10.3389/fpsyt.2020.570164
25. Bambra C, Riordan R, Ford J, Matthews F. The COVID-19 pandemic and health inequalities. J Epidemiol Community Health. (2020) 74(11):964–8. doi: 10.1136/jech-2020-214401
26. Khan JR, Awan N, Islam MM, Muurlink O. Healthcare capacity, health expenditure, and civil society as predictors of COVID-19 case fatalities: a global analysis. Front Public Health. (2020) 8:347. doi: 10.3389/fpubh.2020.00347
27. Vasilevska M, Ku J, Fisman DN. Factors associated with healthcare worker acceptance of vaccination: a systematic review and meta-analysis. Infect Control Hospit Epidemiol. (2014) 35(6):699–708. doi: 10.1086/676427
28. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. (1998) 52(6):377. doi: 10.1136/jech.52.6.377
29. Luo C, Yang Y, Liu Y, Zheng D, Shao L, Jin J, et al. Intention to COVID-19 vaccination and associated factors among health care workers: a systematic review and meta-analysis of cross-sectional studies. Am J Infect Control. (2021) 49(10):1295–304. doi: 10.1016/j.ajic.2021.06.020
30. Aurora RN, Morgenthaler TI. On the goodness of recommendations: the changing face of practice parameters. Sleep. (2010) 33(10):1273–6. doi: 10.1093/sleep/33.10.1273
31. Hamadeh N, Rompaey CV, Metreau E. New World Bank country classifications by income level: 2021–2022 (2021). Available at: https://blogs.worldbank.org/opendata/new-world-bank-country-classifications-income-level-2021-2022. (accessed on 21st May 2022).
32. Acosta D, Fujii Y, Joyce-Beaulieu D, Jacobs KD, Maurelli AT, Nelson EJ, et al. Psychosocial health of k-12 students engaged in emergency remote education and in-person schooling: a cross-sectional study. Int J Environ Res Public Health. (2021) 18(16):8564. doi: 10.3390/ijerph18168564
33. Al-Rahamneh H, Arafa L, Al Orani A, Baqleh R. Long-term psychological effects of COVID-19 pandemic on children in Jordan. Int J Environ Res Public Health. (2021) 18(15):7795. doi: 10.3390/ijerph18157795
34. Alves JM, Yunker AG, DeFendis A, Xiang AH, Page KA. Associations between affect, physical activity, and anxiety among US children during COVID-19. MedRxiv: the Preprint Server for Health Sciences. (2020).
35. Androutsos O, Perperidi M, Georgiou C, Chouliaras G. Lifestyle changes and determinants of children’s and adolescents’ body weight increase during the first COVID-19 lockdown in Greece: the COV-EAT study. Nutrients. (2021) 13(3):1–11. doi: 10.3390/nu13030930
36. Awais MA, Chaudhery MM, Khan MS, Butt AUA, Malik AR, Khan MN, et al. Factors contributing to distress among school and college-going adolescents during COVID-19 lockdown: a cross-sectional study conducted in Sibi Balochistan, Pakistan. J Educ Health Promot. (2021) 10:317. doi: 10.4103/jehp.jehp_1313_20
37. Azoulay E, Yackobovitch-Gavan M, Yaacov H, Gilboa I, Lopez A, Sheppes T, et al. Weight status and body composition dynamics in children and adolescents during the COVID-19 pandemic. Front Pediatr. (2021) 9:707773. doi: 10.3389/fped.2021.707773
38. Berasategi Sancho N, Idoiaga Mondragon N, Dosil Santamaria M, Eiguren Munitis A. The well-being of children in lock-down: physical, emotional, social and academic impact. Child Youth Serv Rev. (2021) 127:19–28. doi: 10.1016/j.childyouth.2021.106085
39. Berki T, Pikó BF. Sedentary lifestyle may contribute to the risk of depression during the COVID-19 pandemic: a snapshot of Hungarian adolescents. Eur J Ment Health. (2021) 16(2):99–119. doi: 10.5708/EJMH.16.2021.2.5
40. Bingham DD, Daly-Smith A, Hall J, Seims A, Dogra SA, Fairclough SJ, et al. COVID-19 lockdown: ethnic differences in children’s self-reported physical activity and the importance of leaving the home environment; a longitudinal and cross-sectional study from the born in Bradford birth cohort study. Int J Behav Nutr Phys Act. (2021) 18(1):1–19. doi: 10.1186/s12966-021-01183-y
41. Breidokienė R, Jusienė R, Urbonas V, Praninskienė R, Girdzijauskienė S. Sedentary behavior among 6-14-year-old children during the COVID-19 lockdown and its relation to physical and mental health. Healthcare (Basel). (2021) 9(6):756. doi: 10.3390/healthcare9060756
42. Campbell K, Weingart R, Ashta J, Cronin T, Gazmararian J. COVID-19 knowledge and behavior change among high school students in semi-rural Georgia. J Sch Health. (2021) 91(7):526–34. doi: 10.1111/josh.13029
43. Chaffee BW, Cheng J, Couch ET, Hoeft KS, Halpern-Felsher B. Adolescents’ substance use and physical activity before and during the COVID-19 pandemic. JAMA Pediatr. (2021) 175(7):715–22. doi: 10.1001/jamapediatrics.2021.0541
44. Chi X, Liang K, Chen S-T, Huang Q, Huang L, Yu Q, et al. Mental health problems among Chinese adolescents during the COVID-19: the importance of nutrition and physical activity. Int J Clin Health Psychol. (2021) 21(3):100218. doi: 10.1016/j.ijchp.2020.100218
45. Docimo R, Costacurta M, Gualtieri P, Pujia A, Leggeri C, Attinà A, et al. Cariogenic risk and COVID-19 lockdown in a paediatric population. Int J Environ Res Public Health. (2021) 18(14):7558. doi: 10.3390/ijerph18147558
46. Dragun R, Veček NN, Marendić M, Pribisalić A, Đivić G, Cena H, et al. Have lifestyle habits and psychological well-being changed among adolescents and medical students due to COVID-19 lockdown in Croatia? Nutrients. (2020) 13(1):97. doi: 10.3390/nu13010097
47. Dubuc M-M, Berrigan F, Goudreault M, Beaudoin S, Turcotte S. COVID-19 impact on adolescent 24 h movement behaviors. Int J Environ Res Public Health. (2021) 18(17):9256. doi: 10.3390/ijerph18179256.34501845
48. Dunton GF, Do B, Wang SD. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U.S. BMC Public Health. (2020) 20(1):1351. doi: 10.1186/s12889-020-09429-3
49. Erades N, Morales A. Impacto psicológico del confinamiento por la COVID-19 en niños españoles: un estudio transversal. Rev Psicol Clín con Niños Adoles. (2020) 7(3):27–34. doi: 10.21134/rpcna.2020.mon.2041
50. Ezpeleta L, Navarro JB, de la Osa N, Trepat E, Penelo E. Life conditions during COVID-19 lockdown and mental health in Spanish adolescents. Int J Environ Res Public Health. (2020) 17(19):1–13. doi: 10.3390/ijerph17197327
51. Ghanamah R, Eghbaria-Ghanamah H. Impact of COVID-19 pandemic on behavioral and emotional aspects and daily routines of Arab Israeli children. Int J Environ Res Public Health. (2021) 18(6):1–19. doi: 10.3390/ijerph18062946
52. Ghorbani S, Afshari M, Eckelt M, Dana A, Bund A. Associations between physical activity and mental health in Iranian adolescents during the COVID-19 pandemic: an accelerometer-based study. Children. (2021) 8(11):1–11. doi: 10.3390/children8111022
53. Gilbert AS, Schmidt L, Beck A, Kepper MM, Mazzucca S, Eyler A. Associations of physical activity and sedentary behaviors with child mental well-being during the COVID-19 pandemic. BMC Public Health. (2021) 21(1):1770. doi: 10.1186/s12889-021-11805-6
54. Guo Y-F, Liao M-Q, Cai W-L, Yu X-X, Li S-N, Ke X-Y, et al. Physical activity, screen exposure and sleep among students during the pandemic of COVID-19. Sci Rep. (2021) 11(1):8529. doi: 10.1038/s41598-021-88071-4
55. Hyunshik K, Jiameng M, Sunkyoung L, Ying G. Change in Japanese children’s 24-hour movement guidelines and mental health during the COVID-19 pandemic. Sci Rep. (2021) 11(1):22972. doi: 10.1038/s41598-021-01803-4
56. James M, Marchant E, Defeyter MA, Woodside J, Brophy S. Impact of school closures on the health and well-being of primary school children in Wales UK: a routine data linkage study using the HAPPEN survey (2018–2020). BMJ Open. (2021) 11(10):e051574. doi: 10.1136/bmjopen-2021-051574
57. Jester N, Kang P. COVID-19 pandemic: is teenagers’ health in crisis? An investigation into the effects of COVID-19 on self-reported mental and physical health of teenagers in secondary education. Public Health Pract (Oxf). (2021) 2:100099. doi: 10.1016/j.puhip.2021.100099
58. Jolliff A, Zhao Q, Eickhoff J, Moreno M. Depression, anxiety, and daily activity among adolescents before and during the COVID-19 pandemic: cross-sectional survey study. JMIR Form Res. (2021) 5(12):e30702. doi: 10.2196/30702
59. Jovanović GK, Zubalj ND, Majanović SK, Rahelić D, Rahelić V, Lončar JV, et al. The outcome of COVID-19 lockdown on changes in body mass index and lifestyle among Croatian schoolchildren: a cross-sectional study. Nutrients. (2021) 13(11):3788. doi: 10.3390/nu13113788
60. Kim SJ, Lee S, Han H, Jung J, Yang SJ, Shin Y. Parental mental health and children’s behaviors and media usage during COVID-19-related school closures. J Korean Med Sci. (2021) 36(25):e184. doi: 10.3346/jkms.2021.36.e184
61. Kim SY, Yoo DM, Min C, Choi HG. Changes in dietary habits and exercise pattern of Korean adolescents from prior to during the COVID-19 pandemic. Nutrients. (2021) 13(10):3314. doi: 10.3390/nu13103314
62. Lanza K, Durand CP, Alcazar M, Ehlers S, Zhang K, Kohl HW. School parks as a community health resource: use of joint-use parks by children before and during COVID-19 pandemic. Int J Environ Res Public Health. (2021) 18(17):9237. doi: 10.3390/ijerph18179237
63. Laurier C, Pascuzzo K, Beaulieu G. Uncovering the personal and environmental factors associated with youth mental health during the COVID-19 pandemic: the pursuit of sports and physical activity as a protective factor. Traumatology (Tallahass Fla). (2021) 27(4):354–64. doi: 10.1037/trm0000342
64. Lee DJ, So WY, Lee SM. The relationship between Korean adolescents’ sports participation, internal health locus of control, and wellness during COVID-19. Int J Environ Res Public Health. (2021) 18(6):1–13. doi: 10.3390/ijerph18062950
65. Li SH, Beames JR, Newby JM, Maston K, Christensen H, Werner-Seidler A. The impact of COVID-19 on the lives and mental health of Australian adolescents. Eur Child Adolesc Psychiatry. (2022). 31(9):1465–77. doi: 10.1007/s00787-021-01790-x
66. Liu Q, Zhou Y, Xie X, Xue Q, Zhu K, Wan Z, et al. The prevalence of behavioral problems among school-aged children in home quarantine during the COVID-19 pandemic in China. J Affect Disord. (2021) 279:412–6. doi: 10.1016/j.jad.2020.10.008
67. López-Gil JF, Tremblay MS, Brazo-Sayavera J. Changes in healthy behaviors and meeting 24-h movement guidelines in Spanish and Brazilian preschoolers, children and adolescents during the COVID-19 lockdown. Children. (2021) 8(2):1–10. doi: 10.3390/children8020083
68. Lu C, Chi X, Liang K, Chen S-T, Huang L, Guo T, et al. Moving more and sitting less as healthy lifestyle behaviors are protective factors for insomnia, depression, and anxiety among adolescents during the COVID-19 pandemic. Psychol Res Behav Manag. (2020) 13:1223–33. doi: 10.2147/PRBM.S284103
69. MacKenzie NE, Keys E, Hall WA, Gruber R, Smith IM, Constantin E, et al. Children’s sleep during COVID-19: how sleep influences surviving and thriving in families. J Pediatr Psychol. (2021) 46(9):1051–62. doi: 10.1093/jpepsy/jsab075
70. Medrano M, Cadenas-Sanchez C, Oses M, Arenaza L, Amasene M, Labayen I. Changes in lifestyle behaviours during the COVID-19 confinement in Spanish children: a longitudinal analysis from the MUGI project. Pediatr Obes. (2021) 16(4):e12731. doi: 10.1111/ijpo.12731
71. Mingazova EN, Akimova LV, Pozharskaya EN, Mingazov RN. Health risks of school-age children with distance learning in the first months of the spread of COVID-19. Probl Sotsial'noi Gig Zdr Ist Med. (2021) 29(Issue):588–92. doi: 10.32687/0869-866x-2021-29-s1-588-592
72. Mitra R, Moore SA, Gillespie M, Faulkner G, Vanderloo LM, Chulak-Bozzer T, et al. Healthy movement behaviours in children and youth during the COVID-19 pandemic: exploring the role of the neighbourhood environment. Health Place. (2020) 65:9. doi: 10.1016/j.healthplace.2020.102418
73. Mitra R, Waygood EOD, Fullan J. Subjective well-being of Canadian children and youth during the COVID-19 pandemic: the role of the social and physical environment and healthy movement behaviours. Prev Med Rep. (2021) 23:101404. doi: 10.1016/j.pmedr.2021.101404
74. Morgül E, Kallitsoglou A, Essau CA. Psychological effects of the COVID-19 lockdown on children and families in the UK. Rev Psicol Clín con Niños Adoles. (2020) 7(3):42–8. doi: 10.21134/rpcna.2020.mon.2049
75. Ng K, Cosma A, Svacina K, Boniel-Nissim M, Badura P. Czech adolescents’ remote school and health experiences during the spring 2020 COVID-19 lockdown. Prev Med Rep. (2021) 22:101386. doi: 10.1016/j.pmedr.2021.101386
76. Ng K, Cooper J, McHale F, Clifford J, Woods C. Barriers and facilitators to changes in adolescent physical activity during COVID-19. BMJ Open Sport Exerc Med. (2020) 6(1):e000919. doi: 10.1136/bmjsem-2020-000919
77. Pombo A, Luz C, Rodrigues LP, Cordovil R. Effects of COVID-19 confinement on the household routines of children in Portugal. J Child Fam Stud. (2021) 30(7):1664–74. doi: 10.1007/s10826-021-01961-z
78. Qin J, Ding Y, Gao J, Wu Y, Lv H, Wu J. Effects of COVID-19 on mental health and anxiety of adolescents aged 13–16 years: a comparative analysis of longitudinal data from China. Front Psychiatry. (2021) 12:695556. doi: 10.3389/fpsyt.2021.695556
79. Qin Z, Shi L, Xue Y, Lin H, Zhang J, Liang P, et al. Prevalence and risk factors associated with self-reported psychological distress among children and adolescents during the COVID-19 pandemic in China. JAMA Netw Open. (2021) 4(1):e2035487. doi: 10.1001/jamanetworkopen.2020.35487
80. Reséndiz-Aparicio JC. How the COVID-19 contingency affects children. Bol Med Hosp Infant Mex. (2021) 78(3):216–24. doi: 10.24875/bmhim.20000140
81. Sá C, Pombo A, Luz C, Rodrigues LP, Cordovil R. COVID-19 social isolation in Brazil: effects on the physical activity routine of families with children. Rev Paul Pediatr. (2020) 39:e2020159. doi: 10.1590/1984-0462/2021/39/2020159
82. Salzano G, Passanisi S, Pira F, Sorrenti L, La Monica G, Pajno GB, et al. Quarantine due to the COVID-19 pandemic from the perspective of adolescents: the crucial role of technology. Ital J Pediatr. (2021) 47(1):1–5. doi: 10.1186/s13052-021-00997-7
83. Schnaiderman D, Bailac M, Borak L, Comar H, Eisner A, Ferrari A, et al. Psychological impact of COVID-19 lockdown in children and adolescents from San Carlos de Bariloche, Argentina: parents’ perspective. Arch Argent Pediatr. (2021) 119(3):170–6. doi: 10.5546/aap.2021.eng.170
84. Siachpazidou DI, Kotsiou OS, Chatziparasidis G, Papagiannis D, Vavougios GD, Gogou E, et al. Action and reaction of pre-primary and primary school-age children to restrictions during COVID-19 pandemic in Greece. J Pers Med. (2021) 11(6):451. doi: 10.3390/jpm11060451
85. Szwarcwald CL, Malta DC, Barros MBA, de Souza Júnior PRB, Romero D, de Almeida WDS, et al. Associations of sociodemographic factors and health behaviors with the emotional well-being of adolescents during the COVID-19 pandemic in Brazil. Int J Environ Res Public Health. (2021) 18(11):6160. doi: 10.3390/ijerph18116160
86. Tandon PS, Zhou C, Johnson AM, Gonzalez ES, Kroshus E. Association of children’s physical activity and screen time with mental health during the COVID-19 pandemic. JAMA Network Open. (2021) 4(10):e2127892. doi: 10.1001/jamanetworkopen.2021.27892
87. Tornaghi M, Lovecchio N, Vandoni M, Chirico A, Codella R. Physical activity levels across COVID-19 outbreak in youngsters of Northwestern Lombardy. J Sports Med Phys Fitness. (2021) 61(7):971–6. doi: 10.23736/S0022-4707.20.11600-1
88. Ventura PS, Ortigoza AF, Castillo Y, Bosch Z, Casals S, Girbau C, et al. Children's health habits and COVID-19 lockdown in Catalonia: implications for obesity and non-communicable diseases. Nutrients. (2021) 13(5):1657. doi: 10.3390/nu13051657
89. Vuković J, Matić RM, Milovanović IM, Maksimović N, Krivokapić D, Pišot S. Children’s daily routine response to COVID-19 emergency measures in Serbia. Front Pediatr. (2021) 9:154. doi: 10.3389/fped.2021.656813
90. Wang L, Chen L, Jia F, Shi X, Zhang Y, Li F, et al. Risk factors and prediction nomogram model for psychosocial and behavioural problems among children and adolescents during the COVID-19 pandemic: a national multicentre study: risk factors of childhood psychosocial problems. J Affect Disord. (2021) 294:128–36. doi: 10.1016/j.jad.2021.06.077
91. Wang L, Hao Y, Chen L, Zhang YW, Deng HZ, Ke XY, et al. Psychological and behavioral functioning of children and adolescents during long-term home-schooling. Zhonghua yu Fang yi xue za zhi [Chin J Prev Med]. (2021) 55(9):1059–66. doi: 10.3760/cma.j.cn112150-20210602-00533
92. Wang L, Zhang Y, Chen L, Wang J, Jia F, Li F, et al. Psychosocial and behavioral problems of children and adolescents in the early stage of reopening schools after the COVID-19 pandemic: a national cross-sectional study in China. Transl Psychiatry. (2021) 11(1):342. doi: 10.1038/s41398-021-01462-z
93. Zhang X, Zhu W, Kang S, Qiu L, Lu Z, Sun Y. Association between physical activity and mood states of children and adolescents in social isolation during the COVID-19 epidemic. Int J Environ Res Public Health. (2020) 17(20):1–12. doi: 10.3390/ijerph17207666
94. Zhu S, Zhuang Y, Ip P. Impacts on children and adolescents’ lifestyle, social support and their association with negative impacts of the COVID-19 pandemic. Int J Environ Res Public Health. (2021) 18(9):4780. doi: 10.3390/ijerph18094780
95. Moore SA, Faulkner G, Rhodes RE, Brussoni M, Chulak-Bozzer T, Ferguson LJ, et al. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: a national survey. Int J Behav Nutr Phys Act. (2020) 17(1):1–11. doi: 10.1186/s12966-020-00987-8
96. Kaditis AG, Ohler A, Gileles-Hillel A, Choshen-Hillel S, Gozal D, Bruni O, et al. Effects of the COVID-19 lockdown on sleep duration in children and adolescents: a survey across different continents. Pediatr Pulmonol. (2021) 56(7):2265–73. doi: 10.1002/ppul.25367
97. Almeida WDS, Szwarcwald CL, Malta DC, Barros MBA, Souza Júnior PRB, Azevedo LO, et al. Changes in Brazilians’ socioeconomic and health conditions during the COVID-19 pandemic. Rev Bras Epidemiol. (2021) 23:e200105. doi: 10.1590/1980-549720200105
98. Robbins LB, Ling J. Lifestyle behaviors and parents’ mental well-being among low-income families during COVID-19 pandemic. Nurs Res. (2022) 71(4):257–65. doi: 10.1097/NNR.0000000000000576
99. Panda PK, Gupta J, Chowdhury SR, Kumar R, Meena AK, Madaan P, et al. Psychological and behavioral impact of lockdown and quarantine measures for COVID-19 pandemic on children, adolescents and caregivers: a systematic review and meta-analysis. J Trop Pediatr. (2021) 67(1):fmaa122. doi: 10.1093/tropej/fmaa122
100. Kızılgeçit M, Yıldırım M. Fear of COVID-19, death depression and death anxiety: religious coping as a mediator. Arch Psychol Relig. (2023) 45(1):23–36. doi: 10.1177/00846724221133455
101. Yildirim M, Çağiş ZG, Crescenzo P, Crescenzo P, Ferrari G, Dhimal M, et al. Vulnerability and self-efficacy predict loneliness among the Turkish public during the COVID-19 pandemic. J Health Soc Sci. (2022) 7(4):410–21.
102. Yıldırım M, Kaynar Ö, Arslan G, Chirico F. Fear of COVID-19, resilience, and future anxiety: psychometric properties of the Turkish version of the dark future scale. J Pers Med. (2023) 13(4):597. doi: 10.3390/jpm13040597
103. Masoom Ali S, Yildirim M, Abdul Hussain S, Vostanis P. Self-reported mental health problems and post-traumatic growth among children in Pakistan care homes. Asia Pac J Soc Work Dev. (2020) 30(1):62–76. doi: 10.1080/02185385.2019.1710726
104. Güler A, Yıldırım M. Associations between acculturation, perceived discrimination and subjective well-being among Syrian adolescents living in Turkey. Int J Psychol. (2022) 57(2):171–80. doi: 10.1002/ijop.12795
105. Rajabi M. Mental health problems amongst school-age children and adolescents during the COVID-19 pandemic in the UK, Ireland and Iran: a call to action and research. Health Promot Perspect. (2020) 10(4):293. doi: 10.34172/hpp.2020.46
106. Lee DW, Shin J, Choi D-W, Kim K, Park E-C. Effects of household income change on children’s problem behavior: findings from a longitudinal study. J Adolesc Health. (2019) 65(4):527–35. doi: 10.1016/j.jadohealth.2019.05.003
107. Lansford JE, Malone PS, Tapanya S, Tirado LMU, Zelli A, Alampay LP, et al. Household income predicts trajectories of child internalizing and externalizing behavior in high-, middle-, and low-income countries. Int J Behav Dev. (2019) 43(1):74–9. doi: 10.1177/0165025418783272
108. Stein DJ, He Y, Phillips A, Sahakian BJ, Williams J, Patel V. Global mental health and neuroscience: potential synergies. Lancet Psychiatry. (2015) 2(2):178–85. doi: 10.1016/S2215-0366(15)00014-0
109. Singh S, Roy D, Sinha K, Parveen S, Sharma G, Joshi G. Impact of COVID-19 and lockdown on mental health of children and adolescents: a narrative review with recommendations. Psychiatry Res. (2020) 293:113429. doi: 10.1016/j.psychres.2020.113429
110. de Figueiredo CS, Sandre PC, Portugal LCL, Mázala-de-Oliveira T, da Silva Chagas L, Raony Í, et al. COVID-19 pandemic impact on children and adolescents’ mental health: biological, environmental, and social factors. Prog Neuropsychopharmacol Biol Psychiatry. (2021) 106:110171. doi: 10.1016/j.pnpbp.2020.110171
111. Miller P, Whitfield K, Betancur L, Votruba-Drzal E. Income dynamics and behavior problems in early childhood, middle childhood, and the transition to adolescence. J Appl Dev Psychol. (2021) 77:101345. doi: 10.1016/j.appdev.2021.101345
112. Zaneva M, Guzman-Holst C, Reeves A, Bowes L. The impact of monetary poverty alleviation programs on children’s and adolescents’ mental health: a systematic review and meta-analysis across low-, middle-, and high-income countries. J Adoles Health. (2022) 71(2):147–56. doi: 10.1016/j.jadohealth.2022.02.011
113. Barican JL, Yung D, Schwartz C, Zheng Y, Georgiades K, Waddell C. Prevalence of childhood mental disorders in high-income countries: a systematic review and meta-analysis to inform policymaking. BMJ Ment Health. (2022) 25(1):36–44. doi: 10.1136/ebmental-2021-300277
114. Wahl-Alexander Z, Camic CL. Impact of COVID-19 on school-aged male and female health-related fitness markers. Pediatr Exerc Sci. (2021) 33(2):61–4. doi: 10.1123/pes.2020-0208
115. Bates LC, Zieff G, Stanford K, Moore JB, Kerr ZY, Hanson ED, et al. COVID-19 impact on behaviors across the 24-hour day in children and adolescents: physical activity, sedentary behavior, and sleep. Children. (2020) 7(9):138. doi: 10.3390/children7090138
116. Paterson DC, Ramage K, Moore SA, Riazi N, Tremblay MS, Faulkner G. Exploring the impact of COVID-19 on the movement behaviors of children and youth: a scoping review of evidence after the first year. J Sport Health Sci. (2021) 10(6):675–89. doi: 10.1016/j.jshs.2021.07.001
117. Calkins SD, Fox NA. Self-regulatory processes in early personality development: a multilevel approach to the study of childhood social withdrawal and aggression. Dev Psychopathol. (2002) 14(3):477–98. doi: 10.1017/S095457940200305X
118. Yıldırım M, Öztürk A, Solmaz F. Fear of COVID-19 and sleep problems in Turkish young adults: mediating roles of happiness and problematic social networking sites use. Psihologija. (2023) (00):27. doi: 10.2298/PSI220412027Y
119. Bonaccorsi G, Pierri F, Cinelli M, Flori A, Galeazzi A, Porcelli F, et al. Economic and social consequences of human mobility restrictions under COVID-19. Proc Natl Acad Sci USA. (2020) 117(27):15530–5. doi: 10.1073/pnas.2007658117
Keywords: COVID-19, psychological problems, behavioral problems, physical activity, sleep problems, children and adolescents
Citation: Peng B, Reeves KKL, Lee SWY, Chung THY, Hui HWL, Leung AHL and Pang JCY (2023) Physical, psychological, and behavioral problems among children and adolescents in countries with different economic statuses during the COVID-19 pandemic: a systematic review and meta-analysis. Front. Pediatr. 11:1181186. doi: 10.3389/fped.2023.1181186
Received: 7 March 2023; Accepted: 2 May 2023;
Published: 5 June 2023.
Edited by:
Murat Yildirim, Ağrı İbrahim Çeçen University, TürkiyeReviewed by:
Fuyong Jiao, Xi'an Jiaotong University, China© 2023 Peng, Reeves, Lee, Chung, Hui, Leung and Pang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kara K. L. Reeves a3JlZXZlc0BjaWhlLmVkdS5oaw==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.