- 1Department of General Practice, Zhongshan Hospital, Fudan University, Shanghai, China
- 2Department of Health Management Centre, Zhongshan Hospital, Fudan University, Shanghai, China
- 3Shanghai Engineering Research Centre of AI Technology for Cardiopulmonary Diseases, Zhongshan Hospital, Fudan University, Shanghai, China
Background: Congenital birth defects (CBDs) are a major public health issue. This study aims to assess trends in the burden of CBDs between 1990 and 2019 across China based on the Global Burden of Disease Study 2019 (GBD 2019).
Methods: Indicators of the burden of CBDs included incidence, mortality, and disability-adjusted life years (DALYs). Metrics included number, rate, and age-standardized rate with 95% uncertainty intervals (UIs). Data were stratified by region [China, global, high-, middle-, low-socio-demographic index (SDI)], age, sex, and type of CBD. Average annual percentage changes (AAPC) and trends were evaluated.
Results: In China, between 1990 and 2019, the age-standardized incidence rate for CBDs showed an increasing trend, with an AAPC of 0.26% (0.11% to 0.41%), reaching 148.12 per 105 person-years (124.03 to 176.33) in 2019. Most CBDs were congenital heart anomalies, with an AAPC of 0.12% (−0.08% to 0.32%). The age-standardized mortality rate for CBDs showed a decreasing trend, with an AAPC of −4.57% (−4.97% to −4.17%), reaching 4.62 per 105 person-years (3.88 to 5.57) in 2019. Most mortality was associated with congenital heart anomalies, with an AAPC of −3.77% (−4.35% to −3.19%). The age-standardized DALYs rate for CBDs showed a decreasing trend, with an AAPC of −3.74% (−3.95% to −3.52%), reaching 480.95 per 105 person-years (407.69 to 570.04) in 2019.
Conclusions: Morbidity associated with CBDs increased in China between 1990 and 2019, accelerated by the adoption of the two-child policy, and ranked high globally. These findings emphasize the need for prenatal screening and primary and secondary prevention strategies.
1. Introduction
Congenital birth defects (CBDs) are structural and/or functional abnormalities that are present at birth. CBDs can develop at any stage of pregnancy, but most occur within the first three months of pregnancy. Globally, CBDs are the leading cause of infant mortality in the world (1, 2), with an estimated 3%–6% of infants, or nearly 8 million babies, born with severe birth defects each year (3). The true number of cases is likely higher, as terminations and stillbirths are not considered in these statistics. CBDs have become a major public health issue, leading to long-term disability and greatly impacting individuals, families, healthcare systems, and society.
Infant mortality is an important marker of the health of a society (4). The Sustainable Development Goals (SDGs) set by the World Health Organization (WHO) include a call to end, by 2030, preventable deaths of newborn babies, with all countries aiming to reduce infant mortality to at least as low as 12 per 1,000 live births (5). In China, tens of millions of infants are born every year (6, 7). Understanding the incidence and disease burden of CBDs in China will inform prevention and intervention measures against CBDs.
Most reports on the incidence and burden of CBDs are country-specific, and surveillance programs have been short (8, 9). In China, domestic reports on CBDs are relevant to a certain region or a specific congenital abnormality (10, 11). Long-term trends and the impact of recent changes in China's fertility policy on the occurrence of CBDs across China (12–15) are unknown. The objective of this study was to assess trends in the incidence and burden of CBDs between 1990 and 2019 across China based on the Global Burden of Disease Study 2019 (GBD 2019).
2. Methods
2.1. Data sources
GBD2019 data are accessible through a portal at the Institute for Health Metrics and Evaluation (IHME), University of Washington, United States. The GBD2019 dataset (https://ghdx.healthdata.org/gbd-2019) used modeling to estimate the burden of 369 diseases or injuries for 204 countries and territories worldwide between 1990 and 2019 (16, 17), stratified by factors such as cause, location, age, and sex.
In China, GBD2019 comprehensively estimated and evaluated the births and deaths of newborns in 31 provinces, autonomous regions, and municipalities, as well as the Hong Kong Special Administrative Region of China and the Macao Special Administrative Region of China (excluding Taiwan, China), using multiple data sources and adopting standardized and comparable methods. Data were mainly obtained from the China Health Statistics Yearbook, the China National Maternal and Child Health Surveillance System, China Vital Registration Birth Data, China Vital Registration Live Births Data, and some published literature or reports (16, 18).
2.2. Data extraction
The WHO attributes International Classification of Diseases (ICD), 10th version (https://icd.who.int/browse10/2010/en#/XVII) codes Q00-Q99 to eleven congenital malformations, deformations, and chromosomal abnormalities. Of these, data for neural tube defects, congenital heart anomalies, orofacial clefts, Down syndrome, Turner syndrome, Klinefelter syndrome, other chromosomal abnormalities, congenital musculoskeletal and limb anomalies, congenital urological anomalies, congenital anomalies of the digestive system, and other CBDs were available from the GBD.
Indicators of the burden of these CBDs, including incidence, mortality, and disability-adjusted life years (DALYs) were recorded. Metrics included number, rate, and age-standardized rate with 95% uncertainty intervals (UIs). Data were stratified by region [China, global, high-, middle-, low- socio-demographic index (SDI)], age, sex, and type of CBD. The SDI is a comprehensive indicator of a country's lag-distributed income per capita, average years of schooling, and the fertility rate in females under the age of 25 years (19). The data from China included in global, and China is classified as a High-middle SDI according to the SDI calculation rules. Age was categorized as 0–6 days, 7–27 days, 28–364 days, 1–4 years, 5–9 years, 10–14 years, 15–19 years, 20–54 years, and 55+ years after birth.
2.3. Statistical analysis
Data were sorted and analyzed using Excel 2021 software. The rate of change in incidence, mortality, and DALYs for CBDs between 1990 and 2019 was calculated as (2019 indicator value—1990 indicator value)/1990 indicator value × 100%. Trends in changes in incidence, mortality, and DALYs for CBDs between 1990 and 2019 were analyzed using Joinpoint Regression Program 4.7.0.0 software developed by the American Institute for Cancer Research (20). The number and location of segmentation points and corresponding P values were determined by the Monte Carlo permutation test, and the annual percentage change (APC) and average annual percentage change (AAPC) were calculated using log-linear regression. The incidence rate of CBDs between 2020 and 2030 in China was predicted using R-4.2.2 software. P < 0.05 was considered statistically significant.
3. Results
3.1. Incidence, mortality, and DALYs for CBDs stratified by region
The incidence, mortality, and disability-adjusted life years (DALYs) for CBDs between 1990 and 2019 in China, globally, and high-, middle-, and low-SDI regions, expressed as numbers, rates, and age-standardized rates, are summarized in Tables 1–3, respectively. The AAPC in the age-standardized incidence rate for CBDs between 1990 and 2019 was 0.26% (95% CI: 0.11% to 0.41%) in China, 0.01% (95% CI: −0.03% to 0.05%) globally, −0.27% (95% CI: −0.32% to −0.21%) in high SDI regions, −0.11% (95% CI: −0.17% to −0.04%) in middle SDI regions, and −0.02% (95% CI: −0.06% to 0.01%) in low SDI regions (Table 1). The AAPC in the age-standardized mortality rate for CBDs between 1990 and 2019 was −4.57% (95% CI: −4.97% to −4.17%) in China, −1.79% (95% CI: −1.84% to −1.74%) globally, −2.40% (95% CI: −2.50% to −2.30%) in high SDI regions, −2.62% (95% CI: −2.74% to −2.51%) in middle SDI regions, and −1.16% (95% CI: −1.23% to −1.09%) in low SDI regions (Table 2). The AAPC in the age-standardized DALY rate for CBDs between 1990 and 2019 was −3.74% (95% CI: −3.95% to −3.52%) in China, −1.75% (95% CI: −1.82% to −1.69%) globally, −2.16% (95% CI: −2.22% to −2.10%) in high SDI regions, −2.49% (95% CI: −2.59% to −2.39%) in middle SDI regions, and −1.25% (95% CI: −1.31% to −1.19%) in low SDI regions (Table 3). Incidence and mortality rates at birth and age-standardized incidence and mortality rates (per 100,000) for CBDs between 1990 and 2019 in China, globally, and high-, middle-, and low-SDI regions are shown in Figures 1, 2. Incidence and mortality rates at birth, age-standardized incidence and mortality rates, and trends for CBDs (per 100,000) between 1990 and 2019 in China are shown in Figures 3, 4. The predicted incidence rate for CBDs (per 100,000) between 2020 and 2030 in China is shown in Figure 5. A world map of the changes in age-standardized incidence, mortality, and DALY rates for CBDs between 1990 and 2019 is shown in Figure 6. The age-standardized incidence rate of CBDs (%) between 1990 and 2019 in China, globally, and in India is shown in Supplementary Figure S1.
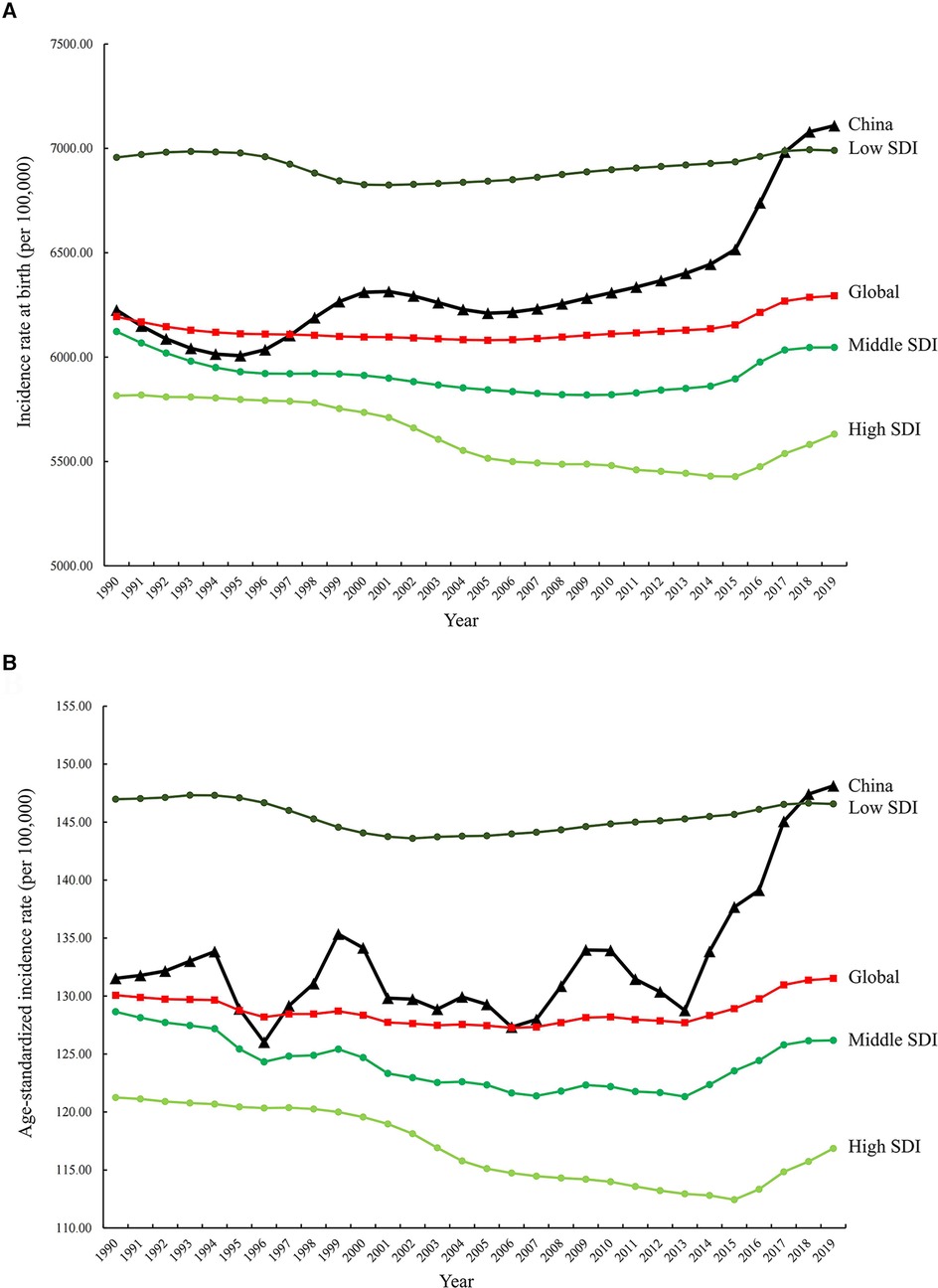
Figure 1. Incidence rates at birth (A) and age-standardized incidence rates (B) (per 100,000) for CBDs between 1990 and 2019 in China, globally, and high-, middle-, and low-SDI regions. SDI: Socio-Demographic Index.
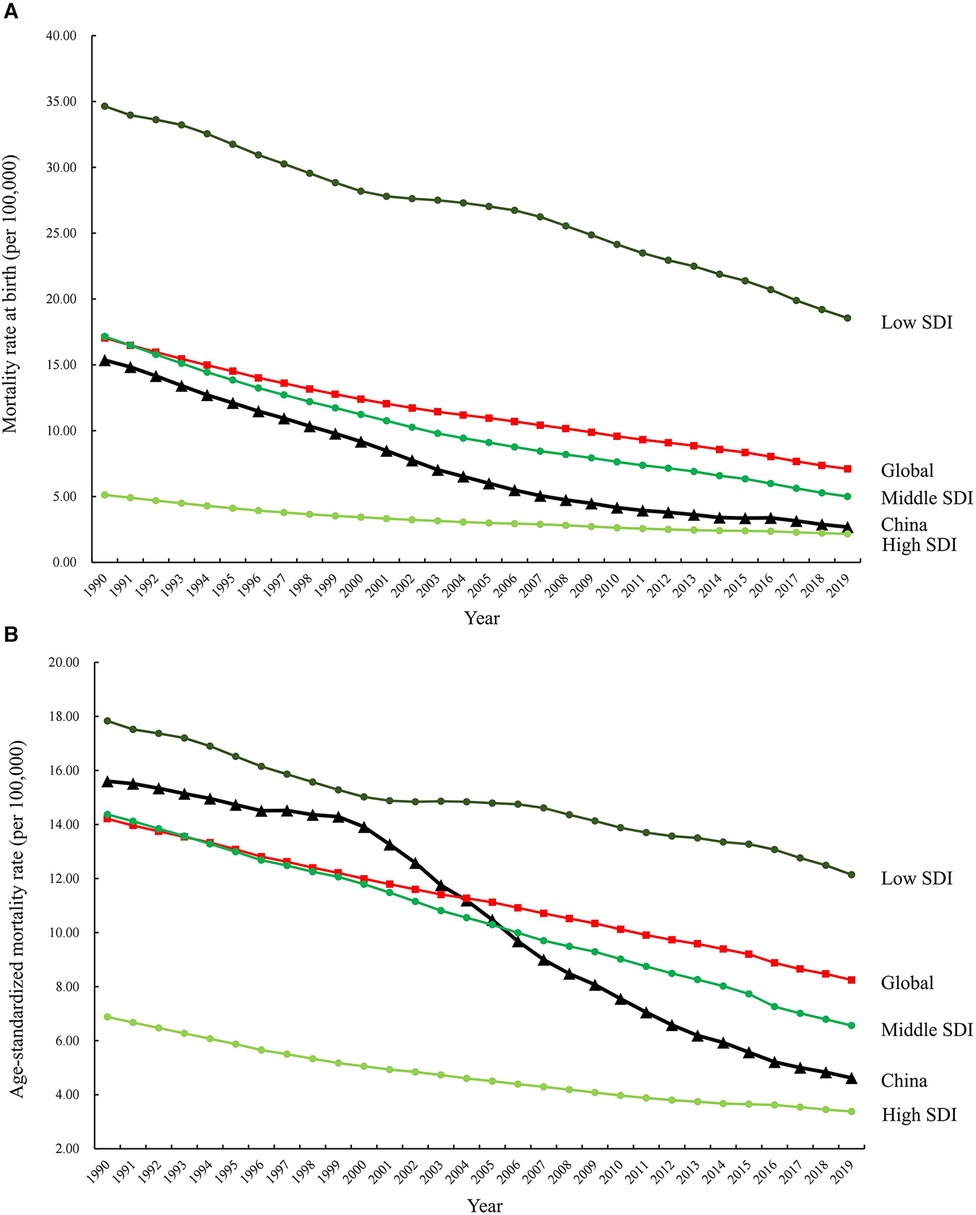
Figure 2. Mortality rates at birth (A) and age-standardized mortality rates (B) (per 100,000) for CBDs between 1990 and 2019 in China, globally, and high-, middle-, and low-SDI regions. SDI: Socio-Demographic Index.
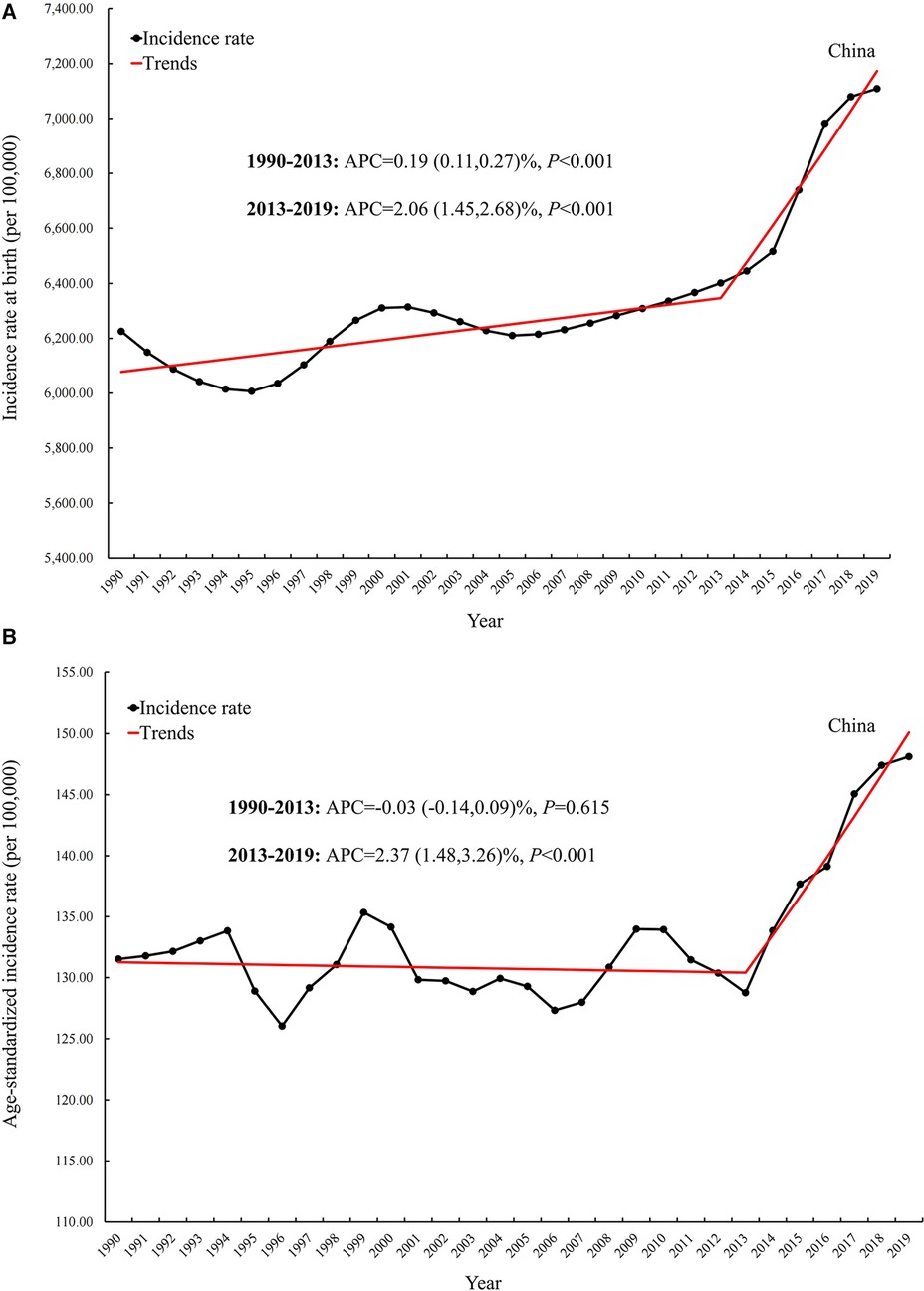
Figure 3. Incidence rate and trend at birth (A) and age-standardized incidence rate and trend (B) for CBDs (per 100,000) between 1990 and 2019 in China. APC: Annual percentage change.
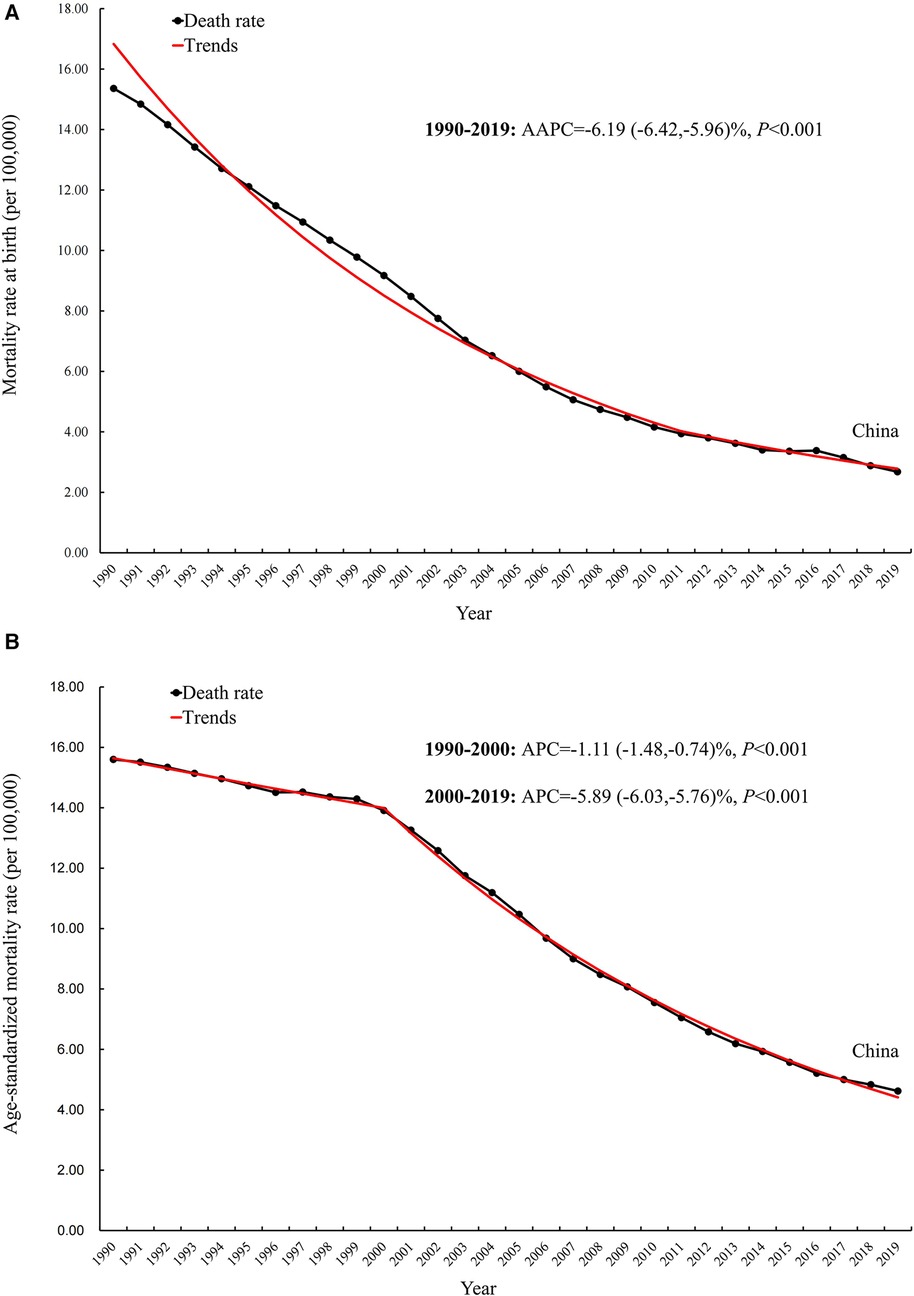
Figure 4. Mortality rate and trend at birth (A) and age-standardized mortality rate and trend (B) for CBDs (per 100,000) between 1990 and 2019 in China. AAPC, average annual percentage changes; APC: Annual percentage change.
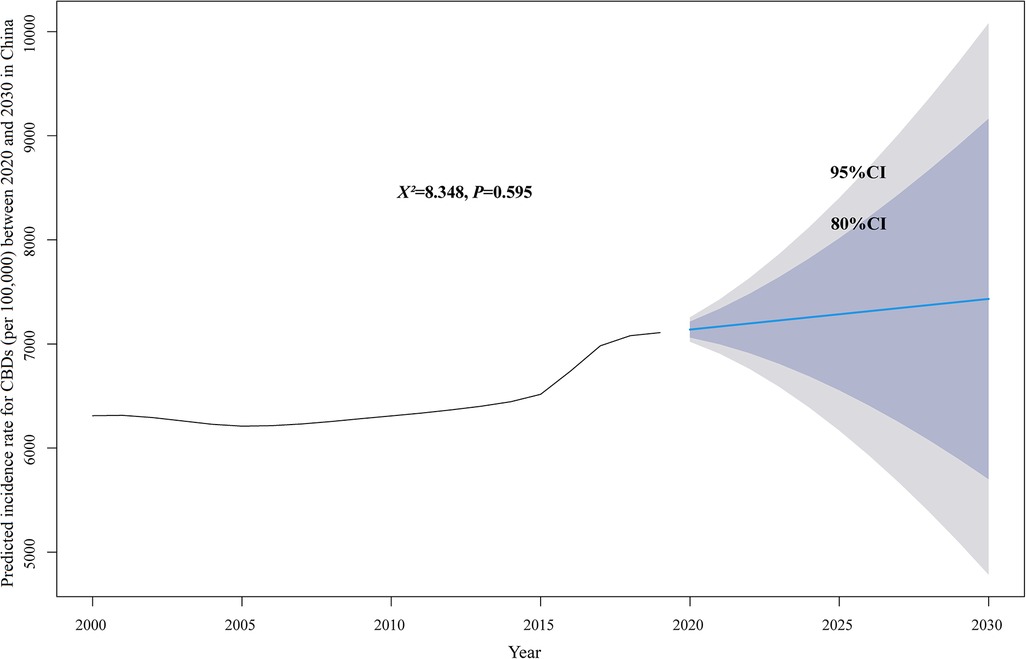
Figure 5. Predicted incidence rate for CBDs (per 100,000) between 2020 and 2030 in China. CI, confidence interval.
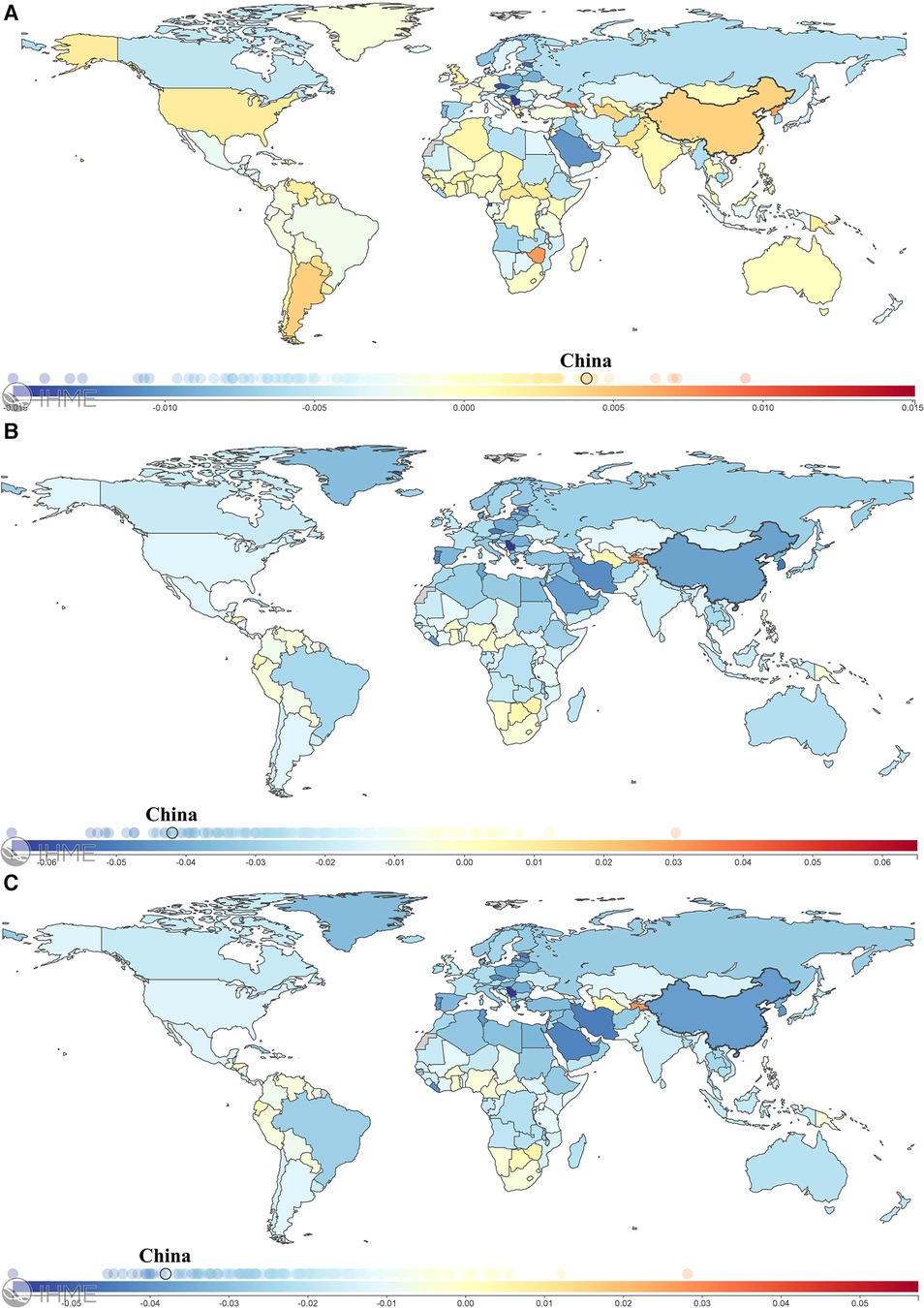
Figure 6. A world map of the changes in age-standardized incidence (A), mortality (B), and DALY (C) rates for CBDs between 1990 and 2019. DALYs, Disability-Adjusted Life Years. Figures from the Institute for Health Metrics and Evaluation (IHME), an independent global health research center at the University of Washington (cited from: https://vizhub.healthdata.org/gbd-compare/).
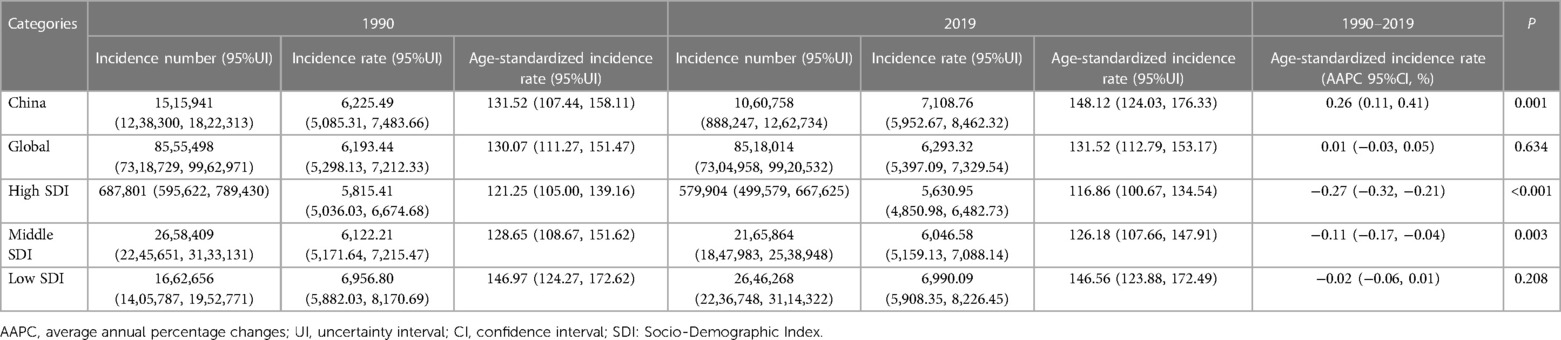
Table 1. Incidence for CBDs between 1990 and 2019 in China, globally, and high-, middle-, and low-SDI regions, expressed as numbers, rates, and age-standardized rates.
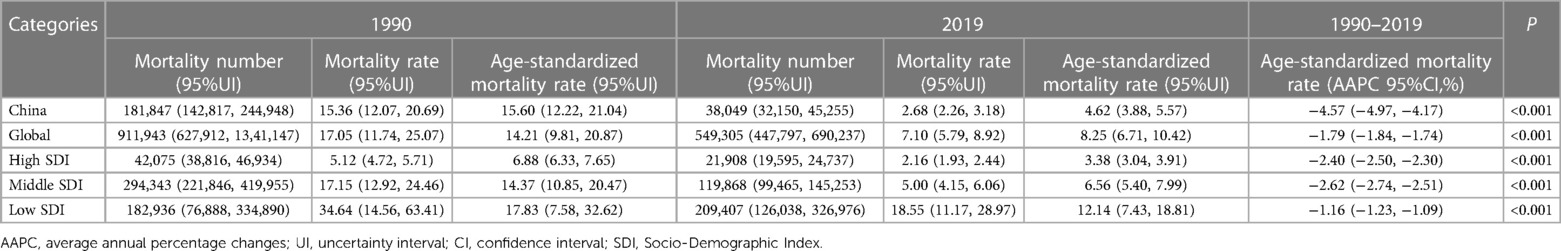
Table 2. Mortality for CBDs between 1990 and 2019 in China, globally, and high-, middle-, and low-SDI regions, expressed as numbers, rates, and age-standardized rates.
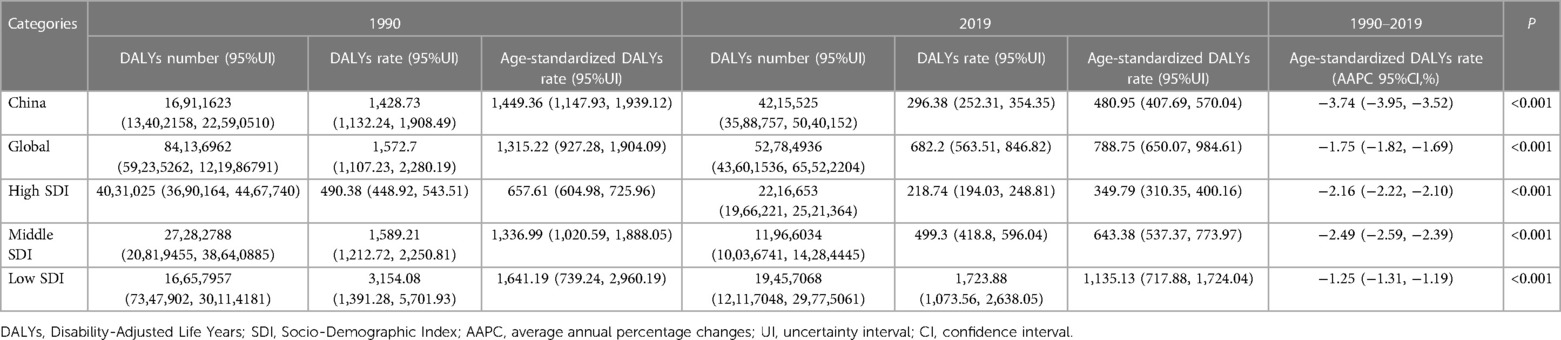
Table 3. DALYs for CBDs between 1990 and 2019 in China, globally, and high-, middle-, and low-SDI regions, expressed as numbers, rates, and age-standardized rates.
3.2. Incidence, mortality, and DALYs for CBDs stratified by sex and type of CBD
The incidence and mortality for CBDs between 1990 and 2019 in China stratified by sex and type of CBD, expressed as numbers, rates, and age-standardized rates, are summarized in Tables 4, 5. The AAPC in the age-standardized incidence rate for CBDs between 1990 and 2019 was 0.28% (95% CI: 0.12% to 0.44%) in males and 0.12% (95% CI: −0.08% to 0.32%) for congenital heart anomalies (Table 4). The AAPC in the age-standardized mortality rate for CBDs between 1990 and 2019 was −4.49% (95% CI: −4.87% to −4.12%) in males and −3.77% (95% CI: −4.35% to −3.19%) for congenital heart anomalies (Table 5). The incidence and mortality for each type of CBD between 1990 and 2019 expressed as numbers, rates, and trends in China are summarized in Supplementary Tables S1, S2.

Table 4. Incidence for CBDs between 1990 and 2019 in China stratified by sex and type of CBD, expressed as numbers, rates, and age-standardized rates.
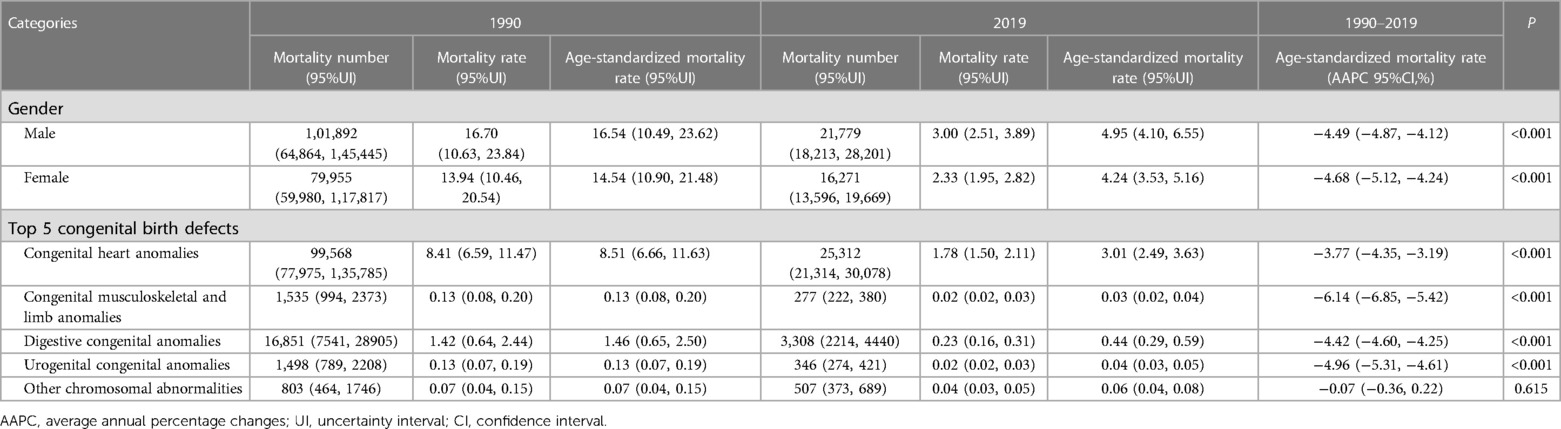
Table 5. Mortality for CBDs between 1990 and 2019 in China stratified by sex and type of CBD, expressed as numbers, rates, and age-standardized rates.
3.3. Age distribution of mortality for CBDs between 1990 and 2019 in China and globally
The mortality for CBDs between 1990 and 2019 in China and globally stratified by age (0–6 days, 7–27 days, 0–28 days) expressed as numbers, rates, and trends are summarized in Table 6. In China, the AAPC in the mortality rate at 0–6 days between 1990 and 2019 was −3.35% (−3.67% to −3.02%). In 2019, the number of deaths at 0–6 days was 7,253, and the number of deaths at 0–28 days was 10,602. Globally, the AAPC in the mortality rate at 0–6 days between 1990 and 2019 was −1.30% (−1.37% to −1.24%). In 2019, the number of deaths at 0–6 days was 173,853, and the number of deaths at 0–28 days was 231,283. Data for all age groups are summarized in Supplementary Table S3.
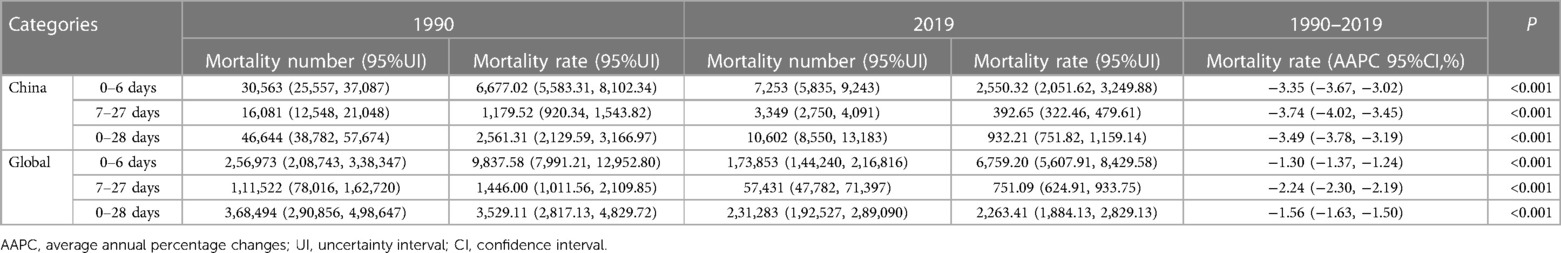
Table 6. Mortality for CBDs between 1990 and 2019 in China and globally stratified by age, expressed as numbers, rates, and trends.
4. Discussion
This study assessed trends in the incidence and burden of CBDs between 1990 and 2019 across China based on the GBD 2019. Findings showed an increase in the morbidity associated with CBDs in China. This was most apparent since 2013, likely due to the easing of the one-child policy (6). In 1979, China's total permanent population exceeded 962 million (21). The Chinese government introduced the one-child policy (13) as a population planning initiative. In 2013, with rapid economic development, the aging population, and the decline of the fertility rate (14), China eased its population policy, which eventually allowed all couples to have two children (15).
In 2016, the number of live births in China rose to 17.86 million, an increase of 7.9% since 2015 (22). After the two-child policy, births to women of advanced maternal age and those with maternal characteristics (e.g., diabetes mellitus) associated with birth defects increased (7, 12, 23–25). Accordingly, this study data show the age-standardized incidence rate for CBDs in China has been increasing since 2013, and the upward trend is predicted to continue between 2020 and 2030. It is recommended that the government and the health department improve access to quality maternal care for all pregnant women, including prenatal screening, vaccination, and vitamins and minerals, to prevent CBDs.
The present study showed the age-standardized incidence rate for CBDs between 1990 and 2019 across China was higher than the rate globally and in high- or middle-SDI regions, but lower than in low-SDI regions. Consistent with this, previous reports indicate the age-standardized incidence rate for CBDs is most severe in low-SDI regions of the world (4, 26). In China, in recent years, the age-standardized incidence rate for CBDs was slightly higher than the rate in low-SDI regions, possibly due to the introduction of the two-child policy. The higher age-standardized incidence rate for CBDs in China during this period may be due to its national conditions. Despite rapid economic development in recent years, China's development has been of low quality, and rural populations still make up the majority. Women in rural areas may be exposed to substances like pesticides and tobacco, and lack awareness of their harmful effects. Additionally, they are less likely to receive multivitamin supplements during pregnancy (27), unlike women in high- or middle-SDI regions who have better access to resources to address these hazards. According to the United Nations “World Population Prospects 2022” report (28), the world's population has reached 8 billion, and India is predicted to replace China as the world's most populous country in 2023. The age-standardized incidence rate for CBDs in India has been steadily increasing. Comparing China with India, which did not have a population planning initiative, confirms that the change in population policy in 2013 increased the incidence rate of CBDs in China. The preventative methods used by China to reduce CBDs may help other countries, such as India, strengthen national policies aimed at birth defect prevention and control.
This study data imply that male births were at higher risk of CBDs than female births between 1990 and 2019 in China. This may be due to the higher susceptibility of the Y chromosome than the X chromosome (29–31). Congenital heart anomalies were the leading type of CBD. In recent years, there was an alarming increase in congenital anomalies of the digestive system. This may be caused by genetic or environmental factors, with high mortality and poor prognosis. We recommend improving access to quality neonatal surgical care and strengthening the control of risk factors for congenital heart anomalies and congenital anomalies of the digestive system (32).
Globally, the under-five mortality rate has declined by 59% between 1990 and 2021 (https://data.unicef.org/topic/child-survival/under-five-mortality), but improving child survival in low-SDI regions remains an urgent concern. In China, the age-standardized mortality rate for CBDs decreased annually between 1990 and 2019, was lower than the rate globally and in middle-SDI regions, and is close to the level in high-SDI regions. Notably, in China, the age-standardized mortality rate for CBDs decreased after 2000. This progress is inextricably linked to the China Child Development Program (33), which was implemented in 2000. The China Child Development Program covers many aspects of policy, social security, health care, and education, and is updated every 10 years (34).
The present study indicates that CBDs were associated with high morbidity and low mortality in China between 1990 and 2019 compared with the trends in the global and high/middle/low-SDI, likely due to the market-oriented healthcare system, which has allowed medical institutions to become “self-sustaining”, and hospitals to offer “drug-based medical care” (35). Investment in preventative care is low, and most institutions are paid to treat rather than prevent disease, resulting in a lower mortality rate but no effective control of morbidity.
The mortality rate for CBDs between 1990 and 2019 in China was higher in males than females, with further research required to understand that difference. Congenital heart malformations were the leading cause of mortality from CBDs. Congenital heart malformations contribute to a significant disease burden globally (36), especially in China (37), warranting government investment in effective, accurate, and accessible medical services for diagnosis and treatment. Mortality associated with birth defects, in China and globally, occurred mainly in newborns, within one week of birth. Better management of newborns with CBDs is needed to improve the long-term survival of affected children.
In the past 30 years, China has had a high incidence rate of CBDs, causing a burden on families and society. However, the government has implemented policies and measures that have resulted in a significant decrease in CBDs deaths since 2000. Although the incidence rate may continue to increase due to two-child policies, medical technology advancements will control mortality rates. The government should continue to prioritize high-risk pregnant women and promote healthy habits (including healthy eating, regular sleep, appropriate exercise, and avoiding exposure to harmful substances) before conception to reduce fetal harm. Additionally, families with affected children should receive rehabilitation support to improve their quality of life.
4.1. Strengths and limitations
This study had several strengths. First, it provides comprehensive estimates of the trends and burden of CBDs at the national level in China. Second, China has a strict and well-developed birth registration and death reporting system for controlling the quantity and quality of the population, which guarantees the quality of the data. Last, the GBD2019 used standard methodology, which makes our estimates of the burden of CBDs in China comparable globally and with different SDI regions.
This study was associated with several limitations. First, the GBD 2019 had inherent limitations, which applied to this study. Second, data on incidence, mortality, and DALYs for CBDs across different provinces and economic regions, including urban and rural areas of China, were not available. Last, the dataset extends between 1990 and 2019, future studies with more recent data are warranted.
5. Conclusions
Morbidity associated with CBDs increased between 1990 and 2019 in China, accelerated by the adoption of the two-child policy, and ranked high globally. CBDs were more common in males than females, with congenital heart disease predominating. Mortality associated with birth defects occurred mainly in newborns, within one week of birth. These findings emphasize the need for prenatal screening and primary and secondary prevention strategies.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: http://ghdx.healthdata.org/gbd-results-tool.
Ethics statement
Ethical review and approval was not required for this study in accordance with the local legislation and institutional requirements. Written informed consent was not required for this study in accordance with the local legislation and institutional requirements.
Author contributions
Conceptualization: YZ, XL. Formal analysis: YZ, HZ, MP. Methodology: YZ, XL. Software: YZ, XL. Investigation: YZ, XC, SY, ZZ. Validation: ML, XL, SJ. Funding acquisition: XL, SJ. Writing—original draft: YZ, HZ, MP. Writing—review & editing: ML, XL, SJ. All authors contributed to the article and approved the submitted version.
Funding
This study was funded by a grant from the Shanghai Municipal Program for Medical Leading Talents (2019LJ15 to SJ) and the Fund of Management Science in Zhongshan Hospital Affiliated to Fudan University (2022ZSGL06 to SJ).
Acknowledgments
We thank Qinyuan Wu at Johns Hopkins University for the scientific editing of this manuscript. We are also grateful for the GBD Study 2019, which provided the original data for this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2023.1170755/full#supplementary-material.
Abbreviations
CBDs, Congenital birth defects; AAPC, Average annual percent change; APC, Annual percentage change; CI, Confidence interval; GBD, Global Burden of Disease; ICD, International Classification of Diseases; DALYs, Disability-Adjusted Life Years; SDI, Socio-Demographic Index.
References
1. Ko HS, Kim DJ, Chung Y, Wie JH, Choi SK, Park IY, et al. A national cohort study evaluating infant and fetal mortality caused by birth defects in Korea. BMJ Open. (2017) 7:e017963. doi: 10.1136/bmjopen-2017-017963
2. Bairoliya N, Fink G. Causes of death and infant mortality rates among full-term births in the United States between 2010 and 2012: an observational study. PLoS Med. (2018) 15:e1002531. doi: 10.1371/journal.pmed.1002531
3. Groisman B, Bermejo-Sánchez E, Romitti PA, Botto LD, Feldkamp ML, Walani SR, et al. Join world birth defects day. Pediatr Res. (2019) 86:3–4. doi: 10.1038/s41390-019-0392-x
4. Global, regional, and national progress towards sustainable development goal 3.2 for neonatal and child health: all-cause and cause-specific mortality findings from the global burden of disease study 2019. Lancet. (2021) 398:870–905. doi: 10.1016/S0140-6736(21)01207-1
5. GBD 2019 Under-5 Mortality Collaborators. Global, regional, and national progress towards Sustainable Development Goal 3.2 for neonatal and child health: all-cause and cause-specific mortality findings from the Global Burden of Disease Study 2019. Lancet. (2021) 398:870–905. doi: 10.1016/S0140-6736(21)01207-1
6. Zhang X, Chen L, Wang X, Wang X, Jia M, Ni S, et al. Changes in maternal age and prevalence of congenital anomalies during the enactment of China's universal two-child policy (2013-2017) in zhejiang province, China: an observational study. PLoS Med. (2020) 17:e1003047. doi: 10.1371/journal.pmed.1003047
7. Li HT, Xue M, Hellerstein S, Cai Y, Gao Y, Zhang Y, et al. Association of China's universal two child policy with changes in births and birth related health factors: national, descriptive comparative study. Br Med J. (2019) 366:l4680. doi: 10.1136/bmj.l4680
8. Paudel P, Sunny AK, Gurung R, Gurung A, Malla H, Rana NB, et al. Burden and consequence of birth defects in Nepal-evidence from prospective cohort study. BMC Pediatr. (2021) 21:81. doi: 10.1186/s12887-021-02525-2
9. Mai CT, Isenburg JL, Canfield MA, Meyer RE, Correa A, Alverson CJ, et al. National population-based estimates for major birth defects, 2010-2014. Birth Defects Res. (2019) 111:1420–35. doi: 10.1002/bdr2.1589
10. Li L, Yu HT, Wang XD, Zhou F, Wang F, Wang CF. Analysis of birth defect rate trend of cleft lip and palate in Shanghai from 2007 to 2016. Chin J Stomatol. (2018) 53:301–06. doi: 10.3760/cma.j.issn.1002-0098.2018.05.003
11. Zhang XH, Chen YM, Sun Y, Qiu LQ. Analysis on the birth situation different fertility policy periods in monitoring area of birth defect population in Zhejiang province. Chin J Prev Med. (2020) 54:519–22. doi: 10.3760/cma.j.cn112150-20190706-0054
12. Feng XL, Wen C. Evaluation of a pilot program that integrated prenatal screening into routine antenatal care in western rural China: an interrupted time-series study. Lancet Reg Health West Pac. (2021) 6:100075. doi: 10.1016/j.lanwpc.2020.100075
13. Jiang Q, Li S, Feldman MW. China's population policy at the crossroads: social impacts and prospects. Asian J Soc Sci. (2013) 41:193–218. doi: 10.1163/15685314-12341298
14. Feng W, Gu B, Cai Y. The End of China's one-child policy. Stud Fam Plann. (2016) 47:83–6. doi: 10.1111/j.1728-4465.2016.00052.x
15. Zeng Y, Hesketh T. The effects of China's universal two-child policy. Lancet. (2016) 388:1930–38. doi: 10.1016/S0140-6736(16)31405-2
16. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet. (2020) 396:1204–22. doi: 10.1016/S0140-6736(20)30925-9
17. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet. (2020) 396:1223–49. doi: 10.1016/S0140-6736(20)30752-2
18. GHDx. Global Burden of Disease Study 2019 (GBD 2019) Data Input Sources Tool. Accessed 18 October, 2022. https://ghdx.healthdata.org/gbd-2019/data-input-sources?components=22&locations=6
19. Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950-2019: a comprehensive demographic analysis for the global burden of disease study 2019. Lancet. (2020) 396:1160–203. doi: 10.1016/S0140-6736(20)30977-6
20. Qiu H, Cao S, Xu R. Cancer incidence, mortality, and burden in China: a time-trend analysis and comparison with the United States and United Kingdom based on the global epidemiological data released in 2020. Cancer Commun (Lond). (2021) 41:1037–48. doi: 10.1002/cac2.12197
21. National Bureau of Statistics of China. Beijing: National Bureau of Statistics of China. Accessed 5 November, 2022. http://data.stats.gov.cn/english/
22. National Bureau of Statistics of China. 2016 National Economic and Social Development Statistical Bulletin of the People’s Republic of China. Accessed 5 November, 2022. http://www.stats.gov.cn/tjsj/zxfb/201702/t20170228_1467424.html
23. Goetzinger KR, Shanks AL, Odibo AO, Macones GA, Cahill AG. Advanced maternal age and the risk of Major congenital anomalies. Am J Perinatol. (2017) 34:217–22. doi: 10.1055/s-0036-1585410
24. Frederiksen LE, Ernst A, Brix N, Braskhøj Lauridsen LL, Roos L, Ramlau-Hansen CH, et al. Risk of adverse pregnancy outcomes at advanced maternal age. Obstet Gynecol. (2018) 131:457–63. doi: 10.1097/AOG.0000000000002504
25. Harris BS, Bishop KC, Kemeny HR, Walker JS, Rhee E, Kuller JA. Risk factors for birth defects. Obstet Gynecol Surv. (2017) 72:123–35. doi: 10.1097/OGX.0000000000000405
26. Higashi H, Barendregt JJ, Kassebaum NJ, Weiser TG, Bickler SW, Vos T. The burden of selected congenital anomalies amenable to surgery in low and middle-income regions: cleft lip and palate, congenital heart anomalies and neural tube defects. Arch Dis Child. (2015) 100:233–38. doi: 10.1136/archdischild-2014-306175
27. Zhang X, Li S, Wu S, Hao X, Guo S, Suzuki K, et al. Prevalence of birth defects and risk-factor analysis from a population-based survey in Inner Mongolia, China. BMC Pediatr. (2012) 12:125. doi: 10.1186/1471-2431-12-125
28. UN. World Population Prospects 2022: Summary of Results. Accessed 20 November, 2022. https://www.un.org/development/desa/pd/content/World-Population-Prospects-2022
29. Zhou Y, Mao X, Zhou H, Qin Z, Wang L, Cai Z, et al. Epidemiology of birth defects based on a birth defect surveillance system in southern Jiangsu, China, 2014-2018. J Matern Fetal Neonatal Med. (2022) 35:745–51. doi: 10.1080/14767058.2020.1731459
30. Xie D, Yang T, Liu Z, Wang H. Epidemiology of birth defects based on a birth defect surveillance system from 2005 to 2014 in hunan province, China. PLoS One. (2016) 11:e0147280. doi: 10.1371/journal.pone.0147280
31. Sokal R, Tata LJ, Fleming KM. Sex prevalence of major congenital anomalies in the United Kingdom: a national population-based study and international comparison meta-analysis. Birth Defects Res A Clin Mol Teratol. (2014) 100:79–91. doi: 10.1002/bdra.23218
32. Global PaedSurg Research Collaboration. Mortality from gastrointestinal congenital anomalies at 264 hospitals in 74 low-income, middle-income, and high-income countries: a multicentre, international, prospective cohort study. Lancet. (2021) 398(10297):325–39. doi: 10.1016/S0140-6736(21)00767-4
33. The Central People's Government of the People's Republic of China. The China Child Development Program (2001-2010). Accessed 11 November, 2022. http://www.gov.cn/ztzl/61/content_627720.htm
34. The Central People's Government of the People's Republic of China. The China Child Development Program (2021-2030). Accessed 12 November, 2022. http://www.gov.cn/xinwen/2021-09/27/content_5639545.htm
35. Meng Q, Mills A, Wang L, Han Q. What can we learn from China's health system reform. Br Med J. (2019) 365:l2349. doi: 10.1136/bmj.l2349
36. Global, regional, and national burden of congenital heart disease, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet Child Adolesc Health. (2020) 4:185–200. doi: 10.1016/S2352-4642(19)30402-X
Keywords: congenital birth defects, trend analysis, burden of disease, disability-adjusted life-years, China
Citation: Zhao Y, Zhang H, Peng M, Zhou Y, Cheng X, Yang S, Zhang Z, Liu M, Li X and Jiang S (2023) The burden of congenital birth defects between 1990 and 2019 in China: an observational study. Front. Pediatr. 11:1170755. doi: 10.3389/fped.2023.1170755
Received: 21 February 2023; Accepted: 24 April 2023;
Published: 12 May 2023.
Edited by:
Guodong Ding, Shanghai Jiao Tong University, ChinaReviewed by:
Akiko Suzuki, University of Missouri–Kansas City, United StatesMahmudur Rahman, Southern Cross University, Australia
© 2023 Zhao, Zhang, Peng, Zhou, Cheng, Yang, Zhang, Liu, Li and Jiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ming Liu bWluZ2xpdTE0QGZ1ZGFuLmVkdS5jbg== Xiaopan Li eGlhb3BhbmxpMDIyNEAxMjYuY29t Sunfang Jiang amlhbmcuc3VuZmFuZ0B6cy1ob3NwaXRhbC5zaC5jbg==
†These authors have contributed equally to this work
 Yajun Zhao1,†
Yajun Zhao1,† Haonan Zhang
Haonan Zhang Xuelin Cheng
Xuelin Cheng Xiaopan Li
Xiaopan Li