- 1Division of Pediatrics, Toshima Hospital, Tokyo, Japan
- 2Graduate School of Public Health, St. Luke’s International University, Tokyo, Japan
- 3Department of Pediatrics, Juntendo University Faculty of Medicine, Tokyo, Japan
- 4Center for Medical Sciences, St. Luke’s International University, Tokyo, Japan
Whether severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is transmitted through breast milk remains controversial. This study aimed to determine the presence of SARS-CoV-2 in breast milk and assess its transmissibility to the child in infancy. Eleven samples were obtained from nine mothers with coronavirus disease 2019 (COVID-19). All but one sample had negative results on a reverse transcription-quantitative polymerase chain reaction. Among nine children, five were diagnosed with COVID-19, including one child whose mother's milk tested positive. Although SARS-CoV-2 RNA was detected in breast milk, its possible transmission via breastfeeding could not be established. Thus, we conclude that the physical attachment between mother and child is a conceivable transmission route.
1. Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spread globally, resulting in a pandemic. By the end of February 2022, approximately 430 million people had been infected with the virus and 5 million people had died of the disease (1).
Since the beginning of the pandemic, researchers have been investigating whether breast milk can be contaminated by SARS-CoV-2. Mother's milk has nutritional and immunologic benefits, so mothers with coronavirus disease 2019 (COVID-19) are recommended to breastfeed (2). Although most breast milk samples tested negative for SARS-CoV-2 on performing polymerase chain reaction (PCR) (3–6), a few studies have reported the presence of SARS-CoV-2 in breast milk (3, 5, 7, 8). However, these study samples were mainly obtained from puerperal mothers (4, 6, 9, 10). Breastfeeding is recommended for more than 1 year after birth (11), concerns are not only about neonates but also infants, because they are breastfed too. However, only a few studies have assessed infants breastfeeding from mothers with COVID-19 (3); therefore, additional studies are needed to examine whether SARS-CoV-2 transmission to older infants is possible through breast milk. Moreover, methods of milk collection in these studies were either not clearly reported or were inappropriate and hence might be responsible for viral contamination. For example, some samples were collected without the use of face masks (8) or the samples were self-collected (3).
2. Methods
Women who were currently breastfeeding their infants and were diagnosed with COVID-19 on reverse transcription-quantitative PCR (RT-qPCR) using nasopharyngeal swab samples were enrolled. Information regarding COVID-19 diagnosis for both mothers and infants was collected from their medical records. Written informed consent was obtained from the mothers.
Milk samples were collected under the guidance of the medical staff; mothers were instructed to wear face masks, milk collectors' hand hygiene was maintained using soap, and mothers' nipples were wiped using cotton with alcohol. The milk samples were immediately stored at −80°C. At the same time, we wiped the nipple with a swab, which we kept in virus transportation media.
RNA was isolated using the QIAamp Viral RNA Mini Kit (QIAGEN, Hilden, Germany) following standard instructions. RT-qPCR was performed using TaqMan Fast Virus 1-Step Master Mix (Thermo Fisher Scientific, Waltham, MA, USA) and the 2019-nCoV primer/probe set (Takara Bio Inc., Shiga, Japan). RT-qPCR was performed in a MicroAmp™ Fast Optical 96-well reaction plate with 20 µl of the mixture per well containing 5 µl of TaqMan Fast Virus 1-Step Master Mix, 4 µl of primer/probe mix, 6 µl of distilled deionized water (Nippon Gene, Tokyo, Japan), and 5 µl of extracted RNA solution. A standard curve was obtained using a healthy mother's milk, which was obtained from a mother who had no history of COVID-19, using the same procedure as described above. The healthy mother's milk was spiked with a positive control RNA mix (2019-nCoV; No. XA0142, Takara Bio Inc.) after RNase inactivation of the milk sample with AVL buffer from the QIAamp Viral RNA Mini Kit. Analysis was performed using Step One Plus™ (Applied Biosystems, Foster City, CA, USA), and the results were analyzed using Step One Plus™ software v2.3. RT-qPCR was conducted under the following thermal cycling conditions: 5 min at 50°C for reverse transcription, 20 s at 95°C for initial denaturation, 45 cycles of 3 s at 95°C for denaturing, 30 s at 60°C for annealing and extension, and hold at 4°C.
This study was approved by the ethical committee of Toshima Hospital.
3. Results
3.1. Study samples
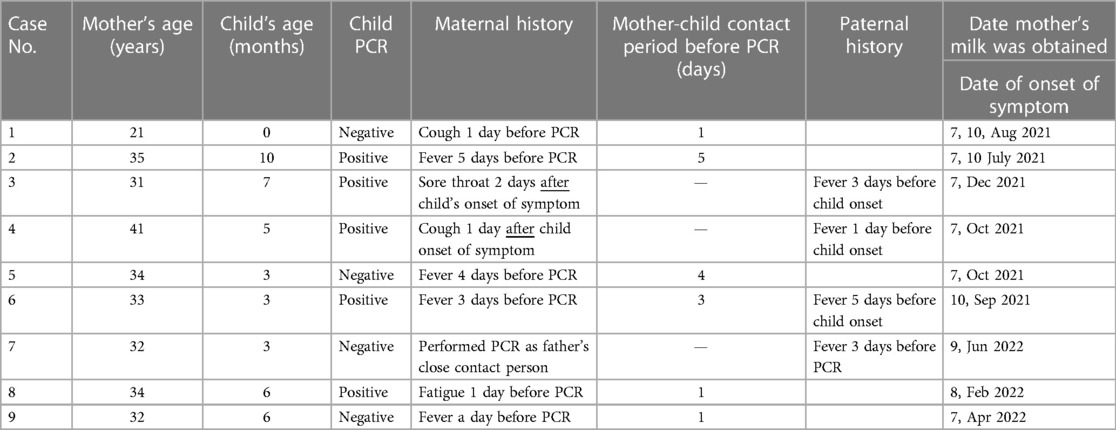
A total of nine mothers diagnosed with COVID-19 based on SARS-CoV-2 PCR results were included in this study. In total, 11 milk samples were obtained from the participants. Table 1 shows the characteristics of the mothers. In Table 1, maternal age and child age are shown with the case number, followed by the PCR results of the children and maternal history. In mothers diagnosed with COVID-19 before child onset of COVID-19, the period from maternal onset to child onset is included. The following column shows paternal history from the medical records if it was available. In the last line, the date of the breast milk collection has been included. Among the nine infants, five tested positive for COVID-19 on SARS-CoV-2 PCR. Of these five infants with COVID-19, the mothers of two developed COVID-19 symptoms after they did, and their fathers had symptoms before the infants were subjected to the SARS-CoV-2 PCR test.
3.2. Results of RT-qPCR
All samples, except for case 4, tested negative on RT-qPCR. Of three of the tested samples from case 4, two were positive, with Ct values of 34.6 and 36.1 and copy number of 2.48 ± 1.56 copies/µl in the extracted RNA solution (1.06 ± 0.67 copies/µl in the breast milk). We performed RT-qPCR again on this sample and the result was positive. We also performed RT-qPCR with the sample of an RT-qPCR-positive case obtained by wiping the mother's nipples, and the results were negative.
4. Discussion
In this study, we tested the breast milk of women with COVID-19 whose offspring were aged 0–10 months. One of the samples had a positive SARS-CoV-2 PCR result but a negative result for the swab sample collected from the nipple skin.
Most previous studies have focused on puerperal mothers (4, 6, 9, 10). However, because the breastfeeding period extends beyond the neonatal period, and the characteristics that might be responsible for this viral transmission through breast milk might change over time (12), we included mothers who had older infants. In addition, in our study, we tested the nipple skin surface of the mothers to examine the possibility of virus transmission through this route.
In the present study, five mother–infant pairs were diagnosed with COVID-19 (cases 2, 3, 4, 6, and 8). Among these five infants, the mothers of two infants developed COVID-19-related symptoms after their infants' diagnosis (cases 3 and 4), and their fathers were the suspected source of infection. Our experience supports the idea that infants are already colonized by SARS-CoV-2 and that breastfeeding brings greater benefit than harm (13). Although the sample size was small, older infants were more likely to have positive results (positive infants were 3, 6, 6, 7, and 10 months old, whereas negative infants were 0, 3, 3, and 6 months old). This difference could be because older children are more likely to be exposed to infected people as well as infection sources. This idea is supported by the opinion that the main route of transmission of SARS-CoV-2 is via infected droplets of caregivers (13). In our study, we used hygiene methods during sample collection to exclude contamination of droplets from the mothers to the breast milk samples. Moreover, the sample obtained from the skin of the mother whose milk had a positive SARS-CoV-2 PCR result showed a negative SARS-CoV-2 PCR result. This suggests that the positive SARS-CoV-2 PCR result of the mother's milk was not due to droplet contamination. In the present study, we found that five of nine infants were infected with COVID-19, and it is more likely that the SARS-CoV-2 infection occurred not via the mother's milk but rather via droplets, as discussed in a previous study (13).
Samples from only mothers with mild-to-moderate symptoms were analyzed herein. A previous study reported that RNAemia results in severe symptoms (14), while another study reported that viral load is associated with COVID-19 severity (15). Because breast milk is produced from blood, more frequent viral contamination may occur in the breast milk of severe patients. However, because breastfeeding is recommended only in mothers who are adequately healthy (5), we believe that our results can provide guidance to most infected women who are breastfeeding their infants.
This study had some limitations. First, the presence of RNA does not indicate infection (16). In a previous study, instances of positive PCR with negative viral cultures have been reported (3). Infection routes were reported to be mainly respiratory and orofecal (17). However, some studies have reported gastrointestinal infection of SARS-CoV-2 (18), and the transmission of infection from breast milk to infants via the gastrointestinal route is a possibility. Second, we did not consider the time of day, which might influence the variation in viral concentrations (12). Finally, we could not conduct an analysis based on samples from the early phase of infection, as the patients were admitted depending on hospital bed availability. In addition, the days that milk samples were obtained were different. However, the period was short between day 7 and day 10.
Because a standard procedure to identify antibodies against SARS-CoV-2 in breast milk is already available, further studies might shed more light on the protective aspects of breast milk against mother-to-infant viral transmission.
5. Conclusion
In mothers with COVID-19, virus transmission via breastfeeding is not plausible, and breastfeeding under hygienic conditions is recommended.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics Committee of Toshima Hospital. The patients/participants provided their written informed consent to participate in this study.
Author contributions
Conceptualization, YM, MR, TS, and HS Methodology, KH, SY, and TK Data curation, SY and TK Writing the original draft preparation, YM, HS and SY Writing review and editing, SY, YM, and MR Supervision, KH, TS, TN, and MR. All authors contributed to the article and approved the submitted version.
Funding
This research was funded by Toshima Hospital.
Acknowledgments
We thank Yumiko Sakurai for assisting in the experiment's procedures.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Available at: https://www.bing.com/search?q=WHO%E3%80%80COVID-19&qs=n&form=QBRE&sp=-1&pq=who+covid-19&sc=8-12&sk=&cvid=DCAE982D0F254F06BAA20B5311692003 (2021).
2. Kimberlin DW, Puopolo KM. Breast milk and COVID-19: what do we know? Clin Infect Dis. (2021) 72(1):131–2. doi: 10.1093/cid/ciaa800
3. Chambers C, Krogstad P, Bertrand K, Contreras D, Tobin NH, Bode L, et al. Evaluation for SARS-CoV-2 in breast milk from 18 infected women. Jama. (2020) 324(13):1347–8. doi: 10.1001/jama.2020.15580
4. Lang GJ, Zhao H. Can SARS-CoV-2-infected women breastfeed after viral clearance? J Zhejiang Univ Sci B. (2020) 21(5):405–7. doi: 10.1631/jzus.B2000095
5. Bhatt H. Should COVID-19 mother breastfeed her newborn child? A literature review on the safety of breastfeeding for pregnant women with COVID-19. Curr Nutr Rep. (2021) 10(1):71–5. doi: 10.1007/s13668-020-00343-z
6. Salvatori G, De Rose DU, Concato C, Alario D, Olivini N, Dotta A, et al. Managing COVID-19-positive maternal-infant dyads: an Italian experience. Breastfeed Med. (2020) 15(5):347–8. doi: 10.1089/bfm.2020.0095
7. Groß R, Conzelmann C, Müller JA, Stenger S, Steinhart K, Kirchhoff F, et al. Detection of SARS-CoV-2 in human breastmilk. Lancet. (2020) 395(10239):1757–8. doi: 10.1016/S0140-6736(20)31181-8
8. Tam PCK, Ly KM, Kernich ML, Spurrier N, Lawrence D, Gordon DL, et al. Detectable severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in human breast milk of a mildly symptomatic patient with coronavirus disease 2019 (COVID-19). Clin Infect Dis. (2021) 72(1):128–30. doi: 10.1093/cid/ciaa673
9. Hinojosa-Velasco A, de Oca PVB, García-Sosa LE, Mendoza-Durán JG, Pérez-Méndez MJ, Dávila-González E, et al. A case report of newborn infant with severe COVID-19 in Mexico: detection of SARS-CoV-2 in human breast milk and stool. Int J Infect Dis. (2020) 100:21–4. doi: 10.1016/j.ijid.2020.08.055
10. Yang N, Che S, Zhang J, Wang X, Tang Y, Wang J, et al. Breastfeeding of infants born to mothers with COVID-19: a rapid review. Ann Transl Med. (2020) 8(10):618. doi: 10.21037/atm-20-3299
11. Westerfield KL, Koenig K, Oh R. Breastfeeding: common questions and answers. Am Fam Physician. (2018) 98(6):368–73.30215910
12. Moro GE, Bertino E. Breastfeeding, human milk collection and containers, and human milk banking: hot topics during the COVID-19 pandemic. J Hum Lact. (2020) 36(4):604–8. doi: 10.1177/0890334420934391
13. Calil V, Krebs VLJ, Carvalho WB. Guidance on breastfeeding during the COVID-19 pandemic. Rev Assoc Med Bras. (2020) 66(4):541–6. doi: 10.1590/1806-9282.66.4.541
14. Eberhardt KA, Meyer-Schwickerath C, Heger E, Knops E, Lehmann C, Rybniker J, et al. RNAemia corresponds to disease severity and antibody response in hospitalized COVID-19 patients. Viruses. (2020) 12(9):1045. doi: 10.3390/v12091045
15. Chen L, Wang G, Long X, Hou H, Wei J, Cao Y, et al. Dynamics of blood viral load is strongly associated with clinical outcomes in coronavirus disease 2019 (COVID-19) patients: a prospective cohort study. J Mol Diagn. (2021) 23(1):10–8. doi: 10.1016/j.jmoldx.2020.10.007
16. Krogstad P, Contreras D, Ng H, Tobin N, Chambers CD, Bertrand K, et al. No evidence of infectious SARS-CoV-2 in human milk: analysis of a cohort of 110 lactating women. Pediatr Res. (2022) 92(4):1140–5. doi: 10.1038/s41390-021-01902-y
17. Vella F, Senia P, Ceccarelli M, Vitale E, Maltezou H, Taibi R, et al. Transmission mode associated with coronavirus disease 2019: a review. Eur Rev Med Pharmacol Sci. (2020) 24(14):7889–904. doi: 10.26355/eurrev_202007_22296
Keywords: breastfeeding, mother milk, COVID-19, SARS-CoV-2, pandemic
Citation: Murano Y, Yamahira S, Shoji H, Hisata K, Koshizaka T, Nakazawa T, Shimizu T and Rahman M (2023) Evaluation of the transmission of SARS-CoV-2 through breast milk: a case series. Front. Pediatr. 11:1160790. doi: 10.3389/fped.2023.1160790
Received: 7 February 2023; Accepted: 23 May 2023;
Published: 22 June 2023.
Edited by:
Tapas Bandyopadhyay, Atal Bihari Vajpayee Institute of Medical Sciences and Dr. Ram Manohar Lohia Hospital, IndiaReviewed by:
Bharti Yadav, All India Institute of Medical Sciences Jodhpur, IndiaPrathik Bandiya, Indira Gandhi Institute of Child Health, India
© 2023 Murano, Yamahira, Shoji, Hisata, Koshizaka, Nakazawa, Shimizu and Rahman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yayoi Murano eW11cmFub0BqdW50ZW5kby5hYy5qcA==
Abbreviations SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; COVID-19, coronavirus disease 2019; PCR, polymerase chain reaction; RT-qPCR, reverse transcription-quantitative PCR.
 Yayoi Murano
Yayoi Murano Shinya Yamahira
Shinya Yamahira Hiromichi Shoji
Hiromichi Shoji Ken Hisata3
Ken Hisata3 Takuya Koshizaka
Takuya Koshizaka Tomoyuki Nakazawa
Tomoyuki Nakazawa Toshiaki Shimizu
Toshiaki Shimizu