- 1Department of Clinical Midwifery, School of Midwifery, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 2Department of Epidemiology and Biostatistics, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 3Department of General Midwifery, School of Midwifery, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Background: Each year, approximately 2.7 million neonates die in their first month of life worldwide, and the majority of these deaths occur in low-income countries. According to the Global Burden of Disease estimation, 1.3 million annual incident cases of neonatal sepsis were reported worldwide, resulting in 203,000 sepsis-attributable deaths. Little is known about the time to death of neonates and predictors after admission with a diagnosis of sepsis. This study aimed to assess the incidence and predictors of death among neonates admitted to the neonatal intensive care unit with a diagnosis of sepsis in referral hospitals in Northwest Ethiopia.
Methods: A multicenter prospective follow-up study was conducted from November 11 to December 7, 2021. A stratified random sampling technique was employed to select 412 neonates. Neonates admitted with sepsis were followed until they develop event for a maximum of 28 days of age. A face-to-face interview was conducted with the mother of the neonate using a pretested and structured questionnaire, and neonatal charts were reviewed to collect baseline factors. Data were entered into Epi-data version 4.6 and exported to STATA version 14 for analysis. A bivariable and multivariable exponential Cox regression model was fitted to identify predictors of death. The adjusted hazard ratio (AHR) with 95% CI was calculated, and statistical significance was declared at a P-value of 0.05 in the multivariable analysis.
Results: A total of 75 (18.47%) neonates died during the study period, with a 95% CI of 14.82–22.60. The incidence rate of death was 28 (95% CI, 22, 35) per 1,000 person-days of observation, with a total follow-up time of 2,677 person-days of observation. Birth weight (<2,500 g) (AHR = 2.12, 95% CI: 1.01, 4.43), prematurity (AHR = 2.06, 95% CI: 1.02, 4.15), duration of labor >24 h (AHR = 3.89, 95% CI: 1.38, 11.01), breast feeding (AHR = 0.43, 95% CI: 0.23, 0.80), having respiratory distress syndrome (AHR = 1.77, 95% CI: 1.02, 306), oxygen saturation less than 90% (AHR = 2.23, 95% CI: 1.02, 306) were significant predictors of death among neonates admitted with sepsis.
Conclusion and recommendation: The incidence of neonatal mortality in this study was high. Early detection and appropriate management of patients’ presentations like respiratory distress syndrome and low oxygen saturation are necessary to reduce neonatal sepsis-related mortality. Special attention should be given to low birth weight and premature neonates and mothers should be encouraged to breastfeed their newborns after delivery.
Introduction
Neonatal sepsis is a systemic infection that occurs within the first 28 days of a newborn's life and includes septicemia, pneumonia, meningitis, arthritis, osteomyelitis, and a urinary tract infection (1). The 2005 International Pediatric Sepsis Consensus Conference defined neonatal sepsis as a systemic inflammatory response syndrome as a result of suspected or proven infection in a neonate (2). Based on the onset of symptoms, neonatal sepsis could be either early-onset sepsis (EOS) or late-onset sepsis (LOS). EOS manifests clinically within the first 72 h and is transmitted both prenatally and intrapartum. LOS, on the other hand, manifests clinically after 72 h of childbirth and is primarily acquired horizontally from the environment (1). Neonatal sepsis ranges from subclinical infection to severe focal or systemic manifestations like; respiratory distress, jaundice, vomiting, and poor feeding (2, 3).
Neonates are predisposed to infections during the perinatal period due to multiple exposures and a relatively compromised immune system. Neonatal conditions like low birth weight, an Apgar score of 7 or less at 5 min, not crying immediately at birth, and gestational age of 37 weeks or less were found to be risk factors for neonatal sepsis (4, 5). Previous pieces of evidence also showed that maternal age, wealth status, maternal urinary tract infections or sexually transmitted infections, intrapartum fever, antenatal care, the starting time of breastfeeding, resuscitation at birth, and nasogastric tube insertion are associated with neonatal sepsis (3, 4).
Neonatal mortality is a major public health problem worldwide, particularly in low-income countries. Every day, approximately 7,000 neonates die in their first month of life worldwide, and the majority of these deaths occurred in low-income countries, specifically in Sub-Saharan Africa, where there is a high burden of neonatal mortality which accounts for an estimated 49.6% of all under-five deaths. According to the Global Burden of Disease (GBD) Study in 2016–2017, an estimated 1.3 million annual incident cases of neonatal sepsis were reported worldwide, resulting in 203,000 sepsis-attributable deaths from which around 75% of the burden occurs in developing countries (6, 7). In Ethiopia, neonatal mortality is unacceptably high at 30 per 1,000 live births, which is far from the global Sustainable Development Goal (SDG) target of reducing neonatal mortality to 12 per 1,000 live births by 2030 (8) and one major cause of neonatal mortality in the country is neonatal sepsis (9). Even though there are effective treatments for neonatal sepsis, a significant number of neonatal deaths have been reported in different studies among hospital-admitted neonates (1, 10–12). There were study gaps in determining predictors for sepsis-related mortality in neonatal intensive care units in our country and the study area in particular. As a result, this study aimed to determine the incidence of death and predictors among neonates admitted with sepsis and the findings will help policy makers and clinicians in designing strategies to improve the quality of neonatal health services in the study area and at the country level, and thus leads to decreasing neonatal morbidity and mortality.
Methods and materials
Study design and period
A multicenter prospective follow-up study design was conducted from November 11 to December 7, 2021.
Study area and setting
This study was conducted in the neonatal intensive care unit (NICU) of five referral hospitals in northwest Ethiopia. We have included all 5 referral hospitals in Northwest Ethiopia namely; the University of Gondar Comprehensive Specialized Hospital, Debre Tabor Comprehensive Specialized Hospital, Debre Markos Comprehensive Specialized Hospital, Felege Hiwot Comprehensive Specialized Hospital, and Tibebe Ghion Specialized Hospital (13).
Population and sample
All neonates with a diagnosis of neonatal sepsis admitted to the Neonatal Intensive Care Unit (NICU) in referral hospitals of North West Ethiopia during the study period were the study population. All neonates with neonatal sepsis admitted to neonatal intensive care units and start treatment were included in this study and neonates with major congenital abnormalities were excluded from the study. The sample size of the study was calculated using the following assumptions; the probability of an event from the previous study (14.7%), the incidence of mortality among admitted neonates with sepsis from a study conducted at Mizan Tepi University Teaching Hospital, Southwest Ethiopia (14). Probability of type 1 error or alpha 0.05, power of the study 80%, 95% confidence level, and 10% withdrawal probability from the study. The sample size was also calculated considering different hazard ratios (HR) of significant predictors from the previous studies including birth weight neonatal age at admission, maternal infection, and length of hospital stay and the largest sample size was considered as a final sample size.
Where E is the number of required event for the study.
Then the required total number of individuals was found from the formula:
Where, N is calculated sample size and P(E) is the probability of an event from the previous study. Finally considering a 10% withdrawal probability, we use a final sample size of 412.
A stratified random sampling was employed to select neonates admitted with sepsis in the selected referral hospitals. The sample size was allocated proportionally to each hospital based on the hospital’s patient flow (average number of neonates admitted in each hospital). Then study subjects were selected using systematic random sampling techniques in which every other neonate admitted with sepsis were included in the study during the study period.
Variables of the study
Dependent variable
Time to death of neonates admitted with sepsis.
Independent variables
Socio-demographic factors of the mother (age, sex, residence, income, educational level).
Obstetric factors (gravidity, mode of delivery, duration of delivery, history of ANC, place of delivery, Premature rupture of membranes, abortion, stillbirth).
Clinical characteristics of neonate (gestational age, birth weight, dehydration, breastfeeding status, oxygen saturation, jaundice, RDS, asphyxia, seizure, hypoglycemia).
Operational definition
Time to death; is calculated from the time of the initiation of treatment till the death of the neonate.
Censored: neonates who did not experience death during the follow-up period including lost follow-up, referred to other health institution, discharged with improvement, or stayed with admission beyond 28 days of neonatal age.
Neonate: newborn from birth to 28 days old (15).
Neonatal sepsis: sepsis diagnosed clinically by professionals or attending physicians during admission of the neonate (16).
Low birth weight: a birth weight of less than 2,500 g at birth (17).
Data collection tools and procedure
A pretested and structured Amharic-version questionnaire was used to collect the data. Maternal sociodemographic characteristics were collected using face-to-face interviews, and obstetrics and baseline clinical characteristics of the neonate were recorded during admission. Then the neonates were followed until discharged, died, and were lost to follow-up. One MSc nurse supervisor and two BSc data collectors were recruited in each referral hospital to collect the data.
The data collectors and supervisors were trained for 1 day on the objective of the study, how to extract the treatment outcome from a chart, and the basics of interviewing before the actual data collection. A structured questionnaire was first prepared in English and then translated to Amharic and back to English by language experts to check consistency and conceptual similarity. The data collection process was closely monitored by the principal investigator and the supervisors throughout the data collection period. Filled questionnaires were checked regularly for completeness of information, and any problems were immediately discussed with the data collectors. A pre-test was conducted on 5% of the sample size in Debre Markos Referral Hospital before the actual data collection period.
Data processing and analysis
Data were entered into EpiData version 4.6.0.6 and exported into STATA version 14 for analysis. Frequency tables, percentages, and median were used to describe the data. The hazard of death among neonates admitted with sepsis across different categories of the covariates was compared by using the nelson Aalen curves and log-rank tests. The Cox proportional hazard (PH) assumption was checked graphically by the log-minus-log function and statistically by Schoenfeld residual (global) test and the assumption was fulfilled. Cox PH and three parametric models (Exponential, Weibull, and Gompertz) were fitted to identify the predictors of death among neonates admitted with sepsis. The best model was selected using Akaike Information criteria (AIC), Bayesian information criteria (BIC), and log-likelihood criteria. The exponential regression model was selected as the best model with the lowest AIC and BIC. The Goodness of fit of the model was assessed by using the cox-snell residual technique. The Shared Frailty model was checked to see a random effect, an unobserved multiplicative effect on the hazard rate, for all individuals in the same hospital. But the frailty for the hospital was not statistically significant (theta = 0.24, x2 = 0.11, P-value = 0.372).
A bivariable and multivariable exponential regression model was fitted to identify predictors of mortality. Variables with a P-value of 0.2 in the bivariable analysis were entered into the multivariable analysis. The adjusted hazard ratio (AHR) with 95% CI was calculated, and statistical significance was declared at P-value of 0.05 in the multivariable analysis.
Results
Socio-demographic characteristics of mothers
A total of 406 neonates were included in the study, providing a response rate of 95.5%. The mean age of the mothers was 29 years with a standard deviation of 4.7 years. More than two-thirds 276 (67.98%) of the mothers of the neonates were between the ages of 25 and 34 years; 384 (94.58%) were married; 123 (30.30%) were unable to read and write, and 198 (48.77%) were housewives (Table 1).
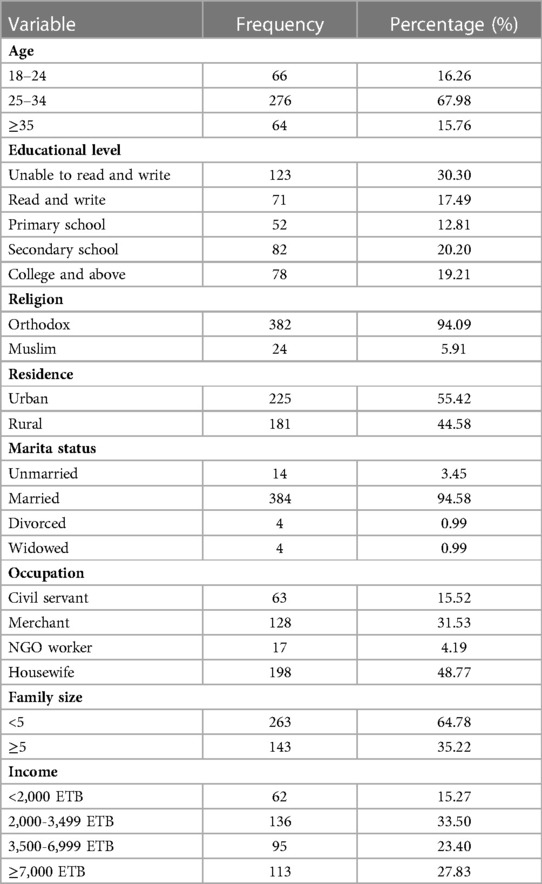
Table 1. Maternal socio-demographic characteristics of neonates admitted with sepsis at NICU in referral hospitals of north west Ethiopia, 2021 (N = 406).
Baseline clinical characteristics of neonates
Out of 406 neonates enrolled, 234 (57.64%) were males, and the majority of the neonates, 392 (96.55%), were less than 1 week old at admission. About 217 (43.35%) neonates had a birth weight of less than 2,500 g. More than half of the neonates, 230 (56.65%), were initiated breastfeeding, and about 91 (22.41%) of the neonates had RDS and 13 (3.20%) had PNA at admission. Twenty-five (6.16%) of the neonates had a history of previous admission, and more than half (63.55% and 60.34%) had a normal WBC count and platelet count, respectively. Almost all (99%) of the neonates initiated their treatments with ampicillin and gentamicin. The first antibiotic was changed for 57 (14.04%) of the neonates, and 48 (84.21%) of them were due to a poor response to the first antibiotic (Table 2).
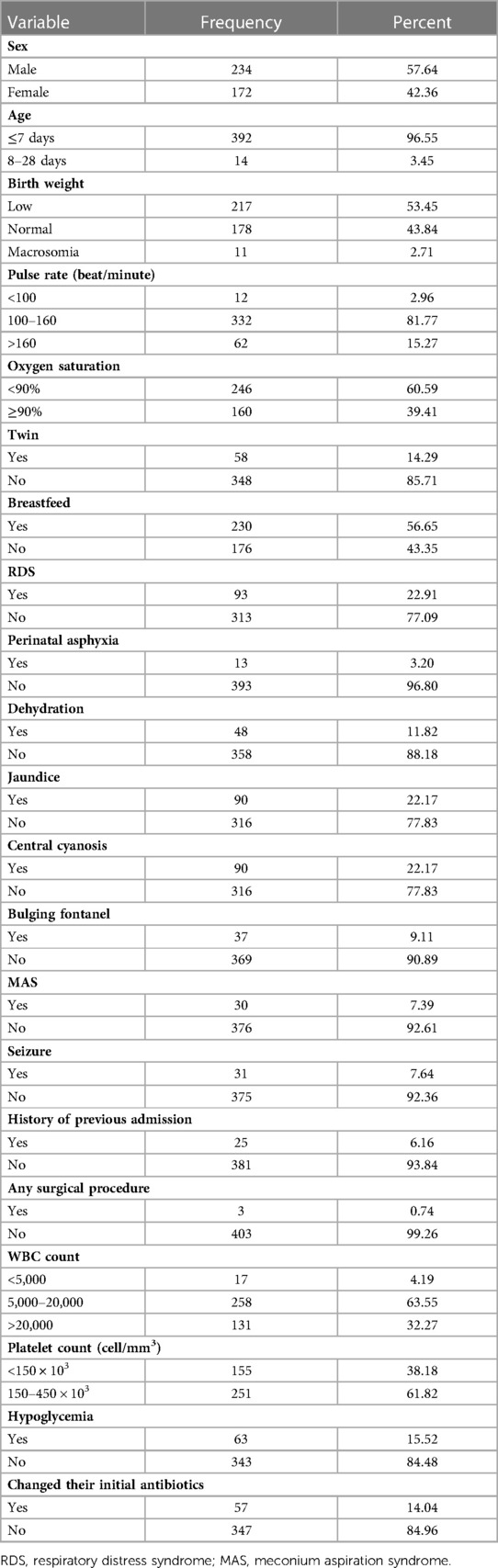
Table 2. Baseline characteristics of the neonates admitted with sepsis at NICU in referral hospitals of northwest Ethiopia, 2021 (N = 406).
Obstetrical characteristics
More than half of the mothers (54.93%) received antenatal care. Thirty-five (8.62%) of the mothers had a history of stillbirth, and 47 (11.58%) had a history of abortion. Sixty-five (16.01%) of the mothers had hypertensive disorders of pregnancy during the current pregnancy; of them, 61 (93.8%) had pre-eclampsia and four (6.22%) had eclampsia. More than three-fourths (82.02%) of the neonates were delivered at hospitals, and more than half (66.75%) were delivered spontaneously. Nearly half (47.04%) of the women had a history of premature rupture of membrane (PROM), of them 16 (8.38%) had a latency period of eighteen and more hours (Table 3).
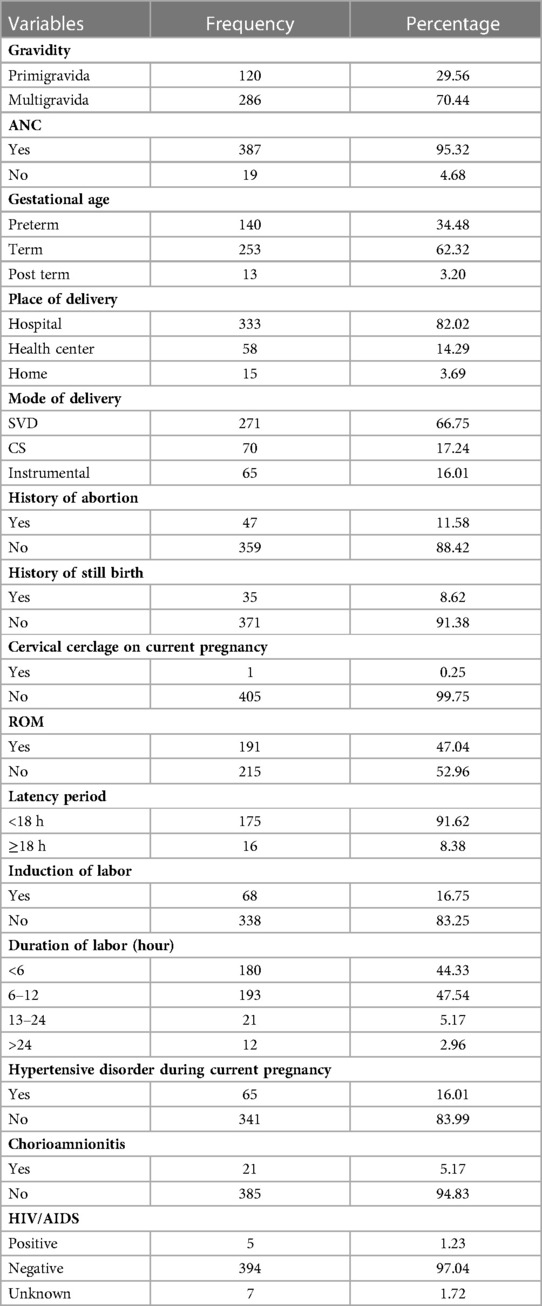
Table 3. Obstetrical characteristics of mothers of the neonates admitted with sepsis at NICU in referral hospitals of northwest Ethiopia, 2021 (N = 406).
Time to death of neonates admitted with sepsis
A total of 406 neonates admitted with sepsis were followed for a median follow-up period of 6 days (IQR: 3–8 days), with minimum and maximum follow-up periods of half a day and 26 days, respectively. Of the total study subjects, 75 (18.47%, 95% CI: 14.82, 22.60) neonates died during the study period. The incidence rate of death was 28 (95% CI, 22, 35) per 1,000 person-days of observation, with a total follow-up time of 2,677 person-days of observation. The cumulative hazard of death among neonates admitted with sepsis on the first, third, sixth, eighth, and 26th day of admission were 3.53% (95% CI: 2.09, 5.86), 9.68% (95% CI: 7.07, 13.19), 18.08% (95% CI: 14.22, 2.283), 22.57% (95% CI: 17.96, 28.15), and 35.51% (95% CI: 26.77, 46.07), respectively (Figure 1).
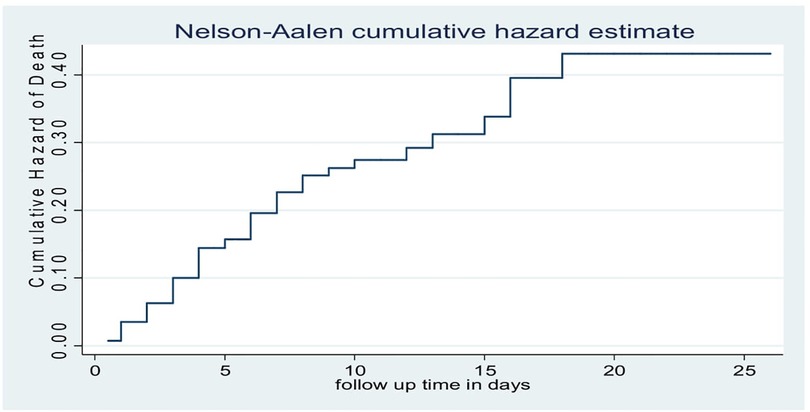
Figure 1. Nelson–Aalen cumulative hazard estimate of neonates admitted with sepsis at N1CU in referral hospitals of northwest Ethiopia, 2021 (N = 406).
The Nelson-Aalen curve shows that the hazard of death among neonates admitted with sepsis differs across different baseline clinical characteristics of the neonates. Preterm neonates, low birth weight neonates, and neonates with less than 90% oxygen saturation at admission had a higher hazard of mortality as compared to their counterparts (Figure 2).
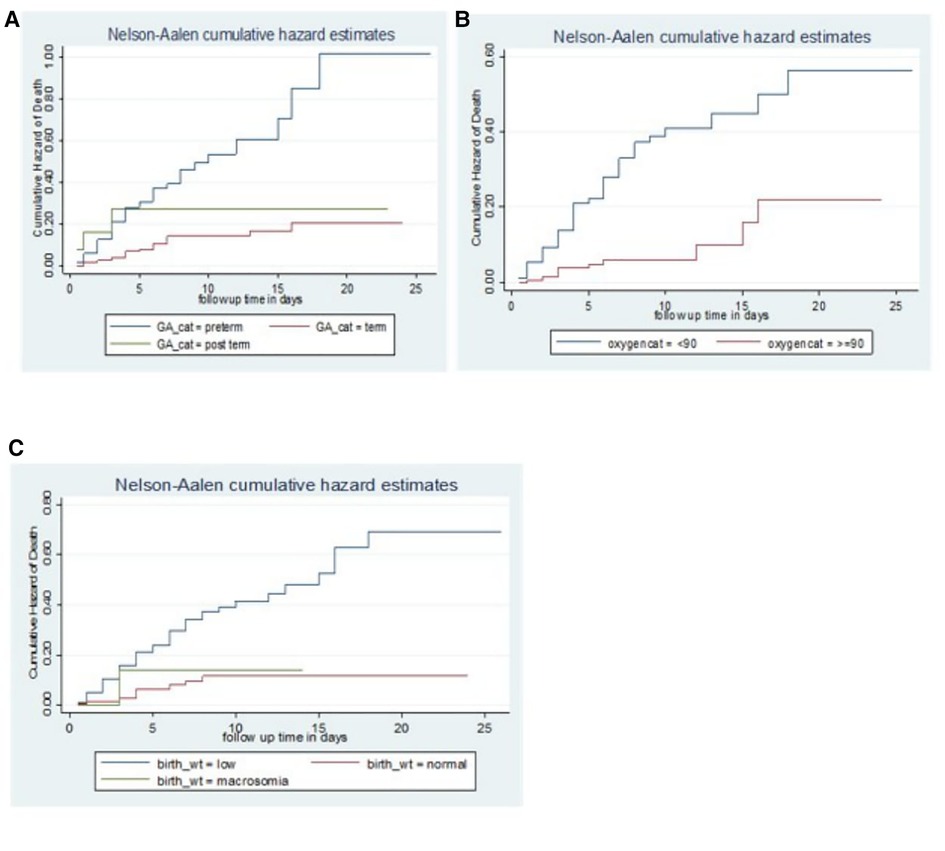
Figure 2. Nelson–Aalen cumulative hazard curve showing different hazards across different categories of the covariates (gestational age (A), oxygen saturation (B), and birth weight (C)).
Model comparison and model fitness
Cox PH and three parametric models (Exponential, Weibull, and Gompertz) were fitted to identify the predictors of death among neonates admitted with sepsis. The exponential regression model was selected as the best model with the lowest AIC and BIC. The Cox proportional hazard (PH) assumption was fulfilled, as shown both graphically by the log-minus-log function and statistically by the Schoenfeld residual test (global test, X2 = 20.80, P-value = 0.7035).
Model fitness
The overall goodness of fit of the exponential regression model was tested by applying the Cox-Snell residual plots. As shown in Figure 3, the line associated with the Cox-Snell residual of the exponential Cox regression model was closer to 45° straight lines of the origin which indicate that model is well-fitted.
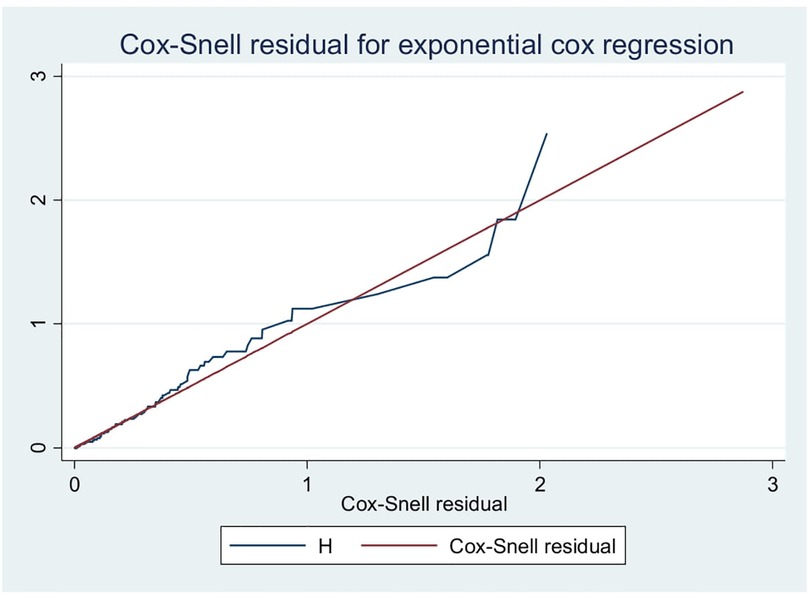
Figure 3. Cox-Snell residual test for overall adequacy of the model fitted for time to death among neonates admitted with a diagnosis of neonatal sepsis.
Predictors of death among neonates admitted with sepsis
On the multivariable exponential regression; duration of labor, breastfeeding status of the neonate, gestational age, birth weight, baseline oxygen saturation, and experiencing RDS at admission were significant predictors of death among neonates admitted with sepsis.
The hazard of neonatal death was two times (AHR = 2.06, 95% CI: 1.02, 4.15) higher among preterm neonates as compared to term neonates. Neonates who were delivered with greater than 24 h of labor duration had four times (AHR = 3.89, 95% CI: 1.38, 11.01) higher risk of death than those who were delivered with 6–12 h of labor duration. The hazard of neonatal death was 2 times (AHR = 2.12, 95% CI: 1.01, 4.43) higher for neonates whose weight was less than 2,500 g compared to normal birth weight neonates. The hazard of death among breastfed neonates was reduced by 57% (AHR = 0.43, 95% CI: 0.23, 0.80) as compared to neonates who were not breastfed. The hazard of neonatal death was two times (AHR = 1.77, 95% CI: 1.02, 306) higher among neonates with respiratory distress syndrome as compared to their counterparts. Neonates whose oxygen saturation was less than 90% at admission had two times (AHR = 2.23, 95% CI: 1.07, 4.61) higher hazard of death than neonates with oxygen saturation ≥90% (Table 4).
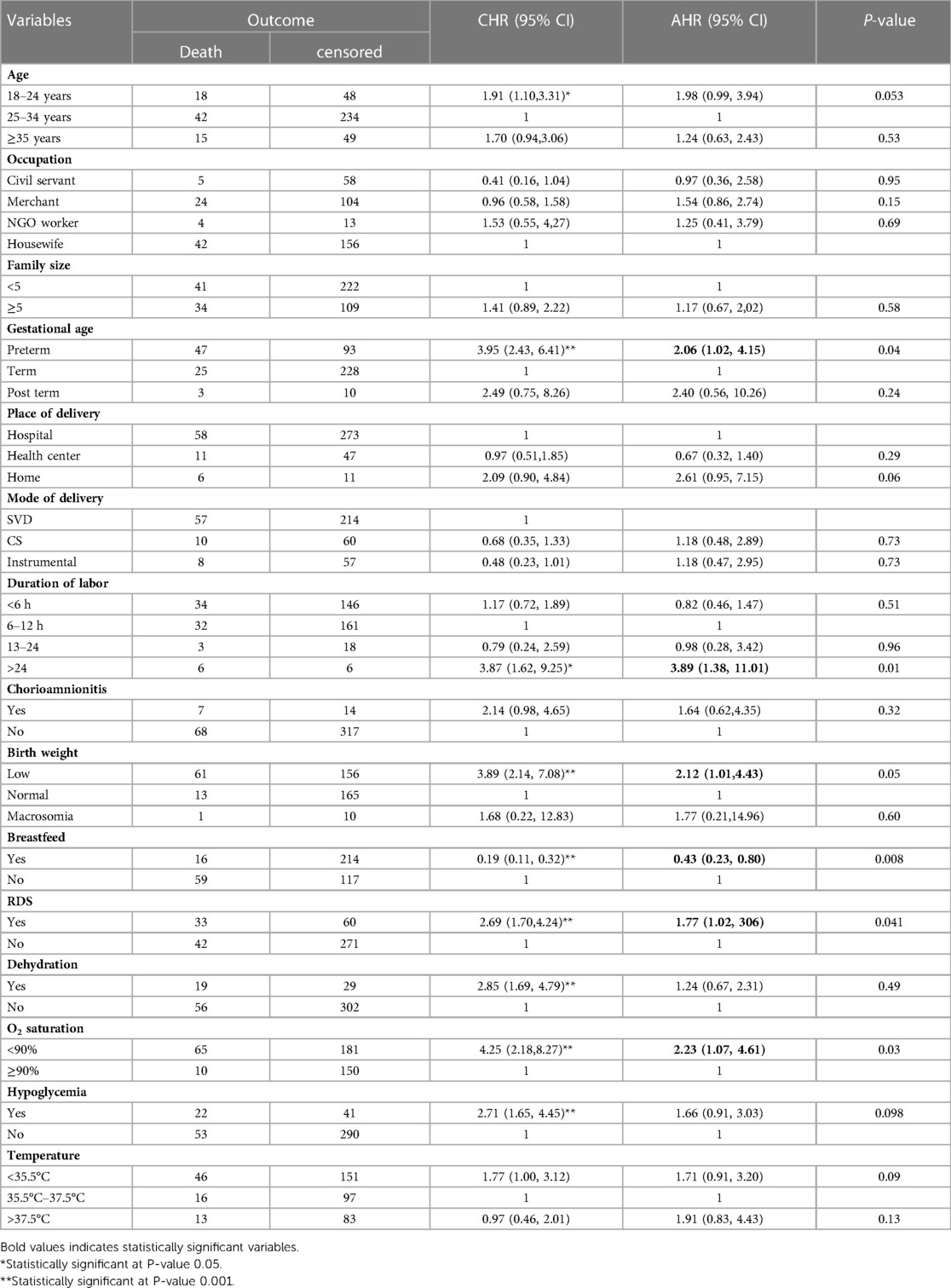
Table 4. Predictors of death among neonates admitted with neonatal sepsis at NICU of northwest Ethiopia referral hospitals, 2021.
Discussion
The findings of multivariable exponential regression analysis of this study identified; gestational age less than 37 weeks (prematurity), duration of labor >24 h, birth weight <2.5 kg, not breastfeeding, respiratory distress syndrome, and Oxygen saturation <90% at admission as predictors of mortality among neonates admitted with sepsis. In this study, 18.47% (95% CI 14.82, 22.60) of neonates died during the follow-up period. The incidence rate of death was 28 (95% CI, 22, 35) per 1,000 person-days of observation, with a total follow-up time of 2,677 person-days of observation. This finding is in line with studies conducted in southwest Ethiopia, in which the death rate associated with sepsis was 14.7% (14), Jimma (22.4%) (18), and Turkey 22.2% (19).
This finding is lower than the study conducted in central India where the mortality rate was 38.24% (20). This inconsistency might be related to the source of data that the Indian study used only referred neonates with maternal and neonatal risk factors of sepsis. Neonates with maternal and neonatal risk factors may have a higher chance of death. Our study considered neonates admitted to NICU regardless of maternal and fetal status. The rate was lower than other studies conducted in Iraq (44.2%) (11), Nigeria (68%) (10), and Brazil (26.1%) (21).
The reason for variation may be due to the current government's attention to reduce neonatal mortality through sustainable development goals.
On the other hand, the rate of neonatal death due to sepsis is higher than studies conducted in North West Ethiopia (4%) (22), western India (7%) (23), Mexico (9.5%) (24), and Malaysia (3.3%) (25). This difference might be explained by socio-economic and health service-related factors.
The current study revealed that low birth weight is a predictor of neonatal mortality among neonates admitted with sepsis. The hazard of mortality doubles for low birth weight neonates when compare to normal birth weight neonates. This finding is in line with studies conducted in Turkey (19), Mexico (24), Pakistan (1), and Nigeria (26). It is known that low-birth weight babies often have difficulty staying warm in normal temperatures and an inability to maintain their body temperature because they have so little body fat. This may increase the risk of death.
Prematurity had shown a significant association with the risk of sepsis-related neonatal mortality with the hazard of death 2 times higher among neonates born before 37 completed weeks of gestation compared to term neonates. This result is consistent with studies conducted in, Durame southern Ethiopia (27), Pakistan (1), Mexico (24), and India (23). It is well known that premature neonates face numerous physiologic challenges and fatal conditions as they adjust to extrauterine life and may not respond to treatments.
The current study showed that neonates who breastfeed after delivery had a reduced risk of death by 57% in comparison with their counters. A study conducted in India also revealed feeding as a protective factor against mortality in babies with neonatal septicemia (28) and this result is supported in previous studies done in Ethiopia (17) and Thailand (29). Since breast milk is a source of nutrients and bioactive factors that help to optimal growth and development, and to fight infections, the risk of death might be reduced in this group of neonates. It is also good to note that neonates who are severely sick might not be able to suck breast milk (30).
In this study, respiratory distress syndrome was identified as the predictor of neonatal mortality from sepsis. Neonates with respiratory distress syndrome were two times more likely to die of neonatal sepsis. This finding is comparable with previous studies conducted in Ethiopia (22, 27) and Nigeria (31). This could be because babies with respiratory distress don’t have surfactant that helps to prevent the collapse of small air sacs in the lungs which increases the risk of neonatal mortality.
This study shows that neonates who were delivered with greater than 24 h of labor duration had four times higher risk of death than those who were delivered with 6–12 h of labor duration. This result is supported by previous studies done in central and southern Ethiopia (32, 33). The possible reason is that prolonged labor might lead to obstructed labor which frequently results in asphyxia that can result in stillbirth, neonatal demise, cerebral palsy, and developmental disabilities (34).
In this study, neonates who had oxygen saturation less than 90% had two times higher hazard of death than neonates with oxygen saturation ≥90%. This finding is supported by other studies done on preterm infants (35, 36). This can be explained by the fact that low oxygen saturation in the blood can affect the oxygen concentration in the body's tissues, including the organs and muscles which results in cell death (37).
Limitations of the study
The gold standard for the diagnosis of sepsis is culture. However, this study identifies sepsis cases based on clinical manifestation. This may have an impact on the incidence of neonatal mortality among neonates with sepsis, because neonates with sepsis may be negative for their cultures.
Conclusion
The incidence of neonatal mortality among neonates admitted with the diagnosis of neonatal sepsis was high. Gestational age less than 37 weeks (prematurity), duration of labor >24 h, birth weight <2.5 kg, not breastfeeding, respiratory distress syndrome, and oxygen saturation <90% were significant predictors of neonatal mortality. Therefore, early detection and appropriate management of patients’ presentations like respiratory distress syndrome and low oxygen saturation are necessary to reduce neonatal sepsis-related mortality. Special attention should be given to low birth weight and premature neonates and mothers should be encouraged to breastfeed their newborns after delivery.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Ethical clearance was obtained from the Institutional Review Board (IRB) of the School of Midwifery, University of Gondar (Ref.No. SMIDW/23/2014 E.C). Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author contributions
SA: conception, design, acquisition of data, analysis, interpretation of data, drafting the article. YA: conception, design, acquisition of data, analysis, interpretation of data, revising the manuscript critically for important intellectual content. WA: design, and revising the manuscript critically for important intellectual content. GA: acquisition of data and revising the manuscript critically for important intellectual content. BR: conception, design, acquisition of data, analysis, interpretation of data, revising the manuscript critically for important intellectual content. All authors contributed to the article and approved the submitted version.
Funding
This research was supported by the University of Gondar, but the University has no role in this manuscript.
Acknowledgments
We would like to thank the University of Gondar for its financial support to conduct the study. We would like also to extend our gratitude to the supervisors, data collectors, and study participants.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ANC, ante natal care; AHR, adjusted hazard ratio; AIC, akaike information criteria; BIC, Bayesian information criteria; CBC, complete blood count; CHR, crude hazard ratio; CS, Cesarean section; ETB, Ethiopian birr; EOS, early onset sepsis; GA, gestational age; GBD, global burden of disease; LOS, late onset sepsis; MAS, meconium aspiration syndrome; NGO, naos gastric open; NICU, neonatal intensive care unit; PH, proportional hazard; PNA, perinatal asyphyxia; PROM, premature rapture of member; SVD, spontaneous vertex delivery; RDS, respiratory distress syndrome; VLBW, very low birth weight.
References
1. Atif M, Zia R, Malik I, Ahmad N, Sarwar S. Treatment outcomes, antibiotic use and its resistance pattern among neonatal sepsis patients attending bahawal Victoria hospital, Pakistan. PloS One. (2021) 16(1):e0244866. doi: 10.1371/journal.pone.0244866
2. Hematyar M, Najibpour R, Bayesh S, Hojjat A, Farshad A. Assessing the role of clinical manifestations and laboratory findings in neonatal sepsis. Arch Pediatr Infect Dis. (2017) 5(1):e29985. doi: 10.5812/pedinfect.29985
3. Shane AL, Sánchez PJ, Stoll BJ. Neonatal sepsis. Lancet. (2017) 390(10104):1770–80. doi: 10.1016/S0140-6736(17)31002-4
4. Gebremedhin D, Berhe H, Gebrekirstos K. Risk factors for neonatal sepsis in public hospitals of mekelle city, north Ethiopia, 2015: unmatched case control study. PloS One. (2016) 11(5):e0154798. doi: 10.1371/journal.pone.0154798
5. Murthy S, Godinho MA, Guddattu V, Lewis LES, Nair NS. Risk factors of neonatal sepsis in India: a systematic review and meta-analysis. PloS One. (2019) 14(4):e0215683. doi: 10.1371/journal.pone.0215683
6. Fleischmann C, Reichert F, Cassini A, Horner R, Harder T, Markwart R, et al. Global incidence and mortality of neonatal sepsis: a systematic review and meta-analysis. Arch Dis Child. (2021) 106(8):745–52.33483376
7. Muller-Pebody B, Johnson A, Heath P, Gilbert R, Henderson K, Sharland M, et al. Empirical treatment of neonatal sepsis: are the current guidelines adequate? Arch Dis Child Fetal Neonatal Ed. (2011) 96(1):F4–8. doi: 10.1136/adc.2009.178483
9. Mengesha HG, Sahle BW. Cause of neonatal deaths in northern Ethiopia: a prospective cohort study. BMC Public Health. (2017) 17(1):1–8. doi: 10.1186/s12889-016-3979-8
10. Arowosegbe AO, Ojo DA, Dedeke IO, Shittu OB, Akingbade OA. Neonatal sepsis in a Nigerian tertiary hospital: clinical features, clinical outcome, aetiology and antibiotic susceptibility pattern. South Afr J Epidemiol Infect. (2017) 32(4):127–31. doi: 10.4102/sajid.v32i4.37
11. Sabeeh JD. Predictors of mortality outcome in neonatal sepsis. Med J Basrah Univ. (2007) 25(1):11–8. doi: 10.33762/mjbu.2007.48118
12. Zea-Vera A, Ochoa TJ. Challenges in the diagnosis and management of neonatal sepsis. J Trop Pediatr. (2015) 61(1):1–13. doi: 10.1093/tropej/fmu079
13. Demisse AG, Alemu F, Gizaw MA, Tigabu Z. Patterns of admission and factors associated with neonatal mortality among neonates admitted to the neonatal intensive care unit of university of gondar hospital, northwest Ethiopia. Pediatric Health Med Ther. (2017) 8:57. doi: 10.2147/PHMT.S130309
14. Wale A, Chelkeba L. Treatment outcome and associated factors of neonatal sepsis at mizan tepi university teaching hospital, south west Ethiopia: a prospective observational study. Pediatric Health Med Ther. (2021) 12:467–79. doi: 10.2147/PHMT.S322069
15. Wynn JL. Defining neonatal sepsis. Curr Opin Pediatr. (2016) 28(2):135. doi: 10.1097/MOP.0000000000000315
16. MacDonald MG, Seshia MM. Avery's neonatology: Pathophysiology and management of the newborn. 7th ed. Philadelphia: Wolters Kluwer (2016).
17. Alemayehu A, Alemayehu M, Arba A, Abebe H, Goa A, Paulos K, et al. Predictors of neonatal sepsis in hospitals at wolaita Sodo town, southern Ethiopia: institution-based unmatched case-control study, 2019. Int J Pediatr. (2020) 2020:3709672.33178290
18. Awoke M. Treatment outcome of neonatal sepsis and its predictors among neonates admitted to pediatric unit of jimma university medical center, south-west Ethiopia. (2018). http://10.140.5.162//handle/123456789/3691
19. Turhan EE, Gürsoy T, Ovalı F. Factors which affect mortality in neonatal sepsis. Türk Pediatri Arşivi. (2015) 50(3):170.
20. Meshram RM, Gajimwar VS, Bhongade SD. Predictors of mortality in outborns with neonatal sepsis: a prospective observational study. Niger Postgrad Med J. (2019) 26(4):216–22. doi: 10.4103/npmj.npmj_91_19
21. de Paula Risso S, Nascimento LFC. Risk factors for neonatal death in neonatal intensive care unit according to survival analysis. Rev Bras Ter Intensiva. (2010) 22:19–26. doi: 10.1590/S0103-507X2010000100005
22. Tewabe T, Mohammed S, Tilahun Y, Melaku B, Fenta M, Dagnaw T, et al. Clinical outcome and risk factors of neonatal sepsis among neonates in felege hiwot referral hospital, bahir dar, amhara regional state, north west Ethiopia 2016: a retrospective chart review. BMC Res Notes. (2017) 10(1):1–7. doi: 10.1186/s13104-017-2573-1
23. Trotman H, Bell Y, Thame M, Nicholson A, Barton M. Predictors of poor outcome in neonates with bacterial sepsis admitted to the university hospital of the west indies. West Indian Med J. (2006) 55(2):80–4.16921699
24. Leal YA, Álvarez-Nemegyei J, Velázquez JR, Rosado-Quiab U, Diego-Rodríguez N, Paz-Baeza E, et al. Risk factors and prognosis for neonatal sepsis in southeastern Mexico: analysis of a four-year historic cohort follow-up. BMC Pregnancy Childbirth. (2012) 12(1):1–9. doi: 10.1186/1471-2393-12-1
25. Awaisu A, Sulaiman SAS, Ibrahim MIM, Abdulmumin S. Antimicrobials utilization and outcomes of neonatal sepsis among patients admitted to a university teaching hospital in Malaysia. East J Med. (2007) 12(1-2):6–14.
26. Shobowale E, Ogunsola F, Oduyebo O, Ezeaka V. A study on the outcome of neonates with sepsis at the lagos university teaching hospital. Int J Med Biomed Res. (2015) 4(1):41–9. doi: 10.14194/ijmbr.4.1.6
27. Bekele T, Merga H, Tesfaye T, Asefa H. Predictors of mortality among neonates hospitalized with neonatal sepsis: a case control study from southern Ethiopia. BMC Pediatr. (2022) 22(1):1. doi: 10.1186/s12887-021-03049-5
28. Bandyopadhyay T, Kumar A, Saili A, Randhawa V. Distribution, antimicrobial resistance and predictors of mortality in neonatal sepsis. J Neonatal Perinatal Med. (2018) 11(2):145–53. doi: 10.3233/NPM-1765
29. Tareen Z, Jirapradittha J, Sirivichayakul C, Chokejindachai W. Factors associated with mortality outcomes in neonatal septicemia in srinagarind hospital, Thailand. Neonat Pediatr Med. (2017) 3(131):2.
30. Cacho NT, Lawrence RM. Innate immunity and breast milk. Front Immunol. (2017) 8:584. doi: 10.3389/fimmu.2017.00584
31. Ogunlesi TA, Ogunfowora OB. Predictors of mortality in neonatal septicemia in an underresourced setting. J Natl Med Assoc. (2010) 102(10):915–22. doi: 10.1016/S0027-9684(15)30710-0
32. Bulto GA, Fekene DB, Woldeyes BS, Debelo BT. Determinants of neonatal sepsis among neonates admitted to public hospitals in central Ethiopia: unmatched case-control study. Global Pediatric Health. (2021) 8:2333794X211026186. doi: 10.1177/2333794X211026186
33. Mustefa A, Abera A, Aseffa A. Prevalence of neonatal sepsis and associated factors amongst neonates admitted in arbaminch general hospital, arbaminch, southern Ethiopia, 2019. J Pediatr Neonatal Care. (2020) 10(1):1–7. doi: 10.15406/jpnc.2020.10.00404
34. Lawn J, Shibuya K, Stein C. No cry at birth: global estimates of intrapartum stillbirths and intrapartum-related neonatal deaths. Bull World Health Organ. (2005) 83:409–17.15976891
35. Glass HC, Costarino AT, Stayer SA, Brett CM, Cladis F, Davis PJ. Outcomes for extremely premature infants. Anesth Analg. (2015) 120(6):1337–51. doi: 10.1213/ANE.0000000000000705
36. Sola A, Golombek SG, Montes Bueno MT, Lemus-Varela L, Zuluaga C, Domínguez F, et al. Safe oxygen saturation targeting and monitoring in preterm infants: can we avoid hypoxia and hyperoxia? Acta Paediatr. (2014) 103(10):1009–18. doi: 10.1111/apa.12692
Keywords: death, incidence, neonates, predictors, sepsis, Ethiopia
Citation: Abiy SA, Animut Y, Ambaw WM, Aragaw GM and Rade BK (2023) Incidence of death and its predictors among neonates admitted with sepsis in referral hospitals, northwest Ethiopia, a prospective cohort study. Front. Pediatr. 11:1129924. doi: 10.3389/fped.2023.1129924
Received: 22 December 2022; Accepted: 15 March 2023;
Published: 13 April 2023.
Edited by:
Zhangbin Yu, First Affiliated Hospital of Southern University of Science and Technology, ChinaReviewed by:
Haibo Peng, Baoan Women's and Children's Hospital, ChinaSuchandra Mukherjee, Institute of Post Graduate Medical Education And Research (IPGMER), India
© 2023 Abiy, Animut, Ambaw, Aragaw and Rade. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Saron Abeje Abiy c2Fyb25hYmVqZTMzQGdtYWlsLmNvbQ==
Specialty Section: This article was submitted to Neonatology, a section of the journal Frontiers in Pediatrics
 Saron Abeje Abiy
Saron Abeje Abiy Yaregal Animut
Yaregal Animut Worku Mequannt Ambaw1
Worku Mequannt Ambaw1 Getie Mihret Aragaw
Getie Mihret Aragaw Bayew Kelkay Rade
Bayew Kelkay Rade