- 1Department of Cardiology, Children’s Memorial Health Institute, Warsaw, Poland
- 2Polish Paediatric Society, Warsaw, Poland
- 3Working Group on Sports Cardiology, Polish Cardiac Society, Warsaw, Poland
- 4Sports and Exercise Medicine Division, University of Padova Department of Medicine, Padova, Italy
- 5Clinical Network of Sports and Exercise Medicine of the Veneto Region, Padova, Italy
- 6The European Academy of Paediatrics, EAP, Brussels, Belgium
- 7Institute of Medical Sciences, Medical College of Rzeszów University, Rzeszów, Poland
- 8Department of Paediatric Gastroenterology and Nutrition, Medical University of Warsaw, Warsaw, Poland
- 9Childcare Worldwide, Padova, Italy
- 10Adelson School of Medicine, Ariel University, Ariel, Israel
- 11Maccabi Health Services, Pediatric Clinic, Tel Aviv, Israel
- 12The European Confederation of Primary Care Paediatricians (ECPCP), Lyon, France
- 13Dana-Dwek Children’s Hospital, Tel Aviv Sourasky Medical Center, Tel Aviv, Israel
- 14School of Medicine, European University Cyprus, Nicosia, Cyprus
- 15Paediatric Department, Larnaca General Hospital, Larnaca, Cyprus
- 16Department of Paediatrics, Paediatric Oncology and Immunology, Pomeranian Medical University, Szczecin, Poland
- 17Department of Geriatrics, Medical University of Lodz, Lodz, Poland
- 18The Polish Society of Sports Medicine, Wroclaw, Poland
- 19Department of Physiotherapy, College of Physiotherapy, Wroclaw, Poland
- 20Kinder-Permanence Hospital Zollikerberg, Zollikerberg, Switzerland
- 21Working Group on Paediatric Cardiology, Polish Cardiac Society, Warsaw, Poland
- 22Institute of Health Sciences, Medical College of Rzeszów University, Rzeszów, Poland
The European Academy of Paediatrics (EAP) and the European Confederation of Primary Care Paediatricians (ECPCP) emphasize the importance of promoting healthy lifestyles within the pediatric population. Many health professionals have questions concerning adequate levels of physical activity for both the healthy pediatric population and for those who may have specific complications. Unfortunately, the academic literature that provides recommendations for participation in sport activities within the pediatric population that have been published during the last decade in Europe is limited and is mainly dedicated to specific illnesses or advanced athletes and not toward the general population. The aim of part 1 of the EAP and ECPCP position statement is to assist healthcare professionals in implementing the best management strategies for a pre-participation evaluation (PPE) for participation in sports for individual children and adolescents. In the absence of a uniform protocol, it is necessary to respect physician autonomy for choosing and implementing the most appropriate and familiar PPE screening strategy and to discuss the decisions made with young athletes and their families. This first part of the Position Statement concerning Sport Activities for Children and Adolescents is dedicated to healthy young athletes.
Introduction
The European Academy of Paediatrics (EAP) and the European Confederation of Primary Care Paediatricians (ECPCP) emphasize the importance of promoting healthy lifestyles for the pediatric population within every age range. The main conclusion from the study entitled “Youth sport participation trends in Europe - An output of Erasmus+,” which presented the findings of an international study on the involvement rates of youth in organized sports during 2017–2020, was a noticeable decline in participation in most sports for boys and girls (1). Therefore, there is an urgent need to increase support and retention of participation in sports from a young age along with essential physical activity (PA) counseling at every visit to the doctor.
Physical activity (PA) is essential for appropriate physical, emotional, and psychosocial growth of the pediatric population as well for patients with different diseases (2–4). The benefits of participation in sports are well-known in the scientific literature (2, 3, 5–8). The European Society of Cardiology (ESC) supports PA as a Class IA guideline for the prevention and management of cardiovascular (CV) disease (9). In 2022, the World Health Organization (WHO) suggested that children between the ages of 5 and 17 years accumulate a minimum of 60 min of moderate-to-vigorous PA (MVPA) per day that includes a variety of endurance activities (10). The WHO also recommends performing regular vigorous intensity aerobic activities and bone and muscle-strengthening activities at least 3 days a week for all age groups (5, 10, 11). Despite the widely accepted benefits of PA, recent data (2020) showed that the majority (81%) of children aged 11–17 years participate in MVPA less than 1 h a day with girls being less physically active than boys in most countries (12). Restrictions during the COVID-19 pandemic have affected children's PA levels. Therefore, promoting PA in the pediatric population should be a priority to recover pre-pandemic activity levels (13, 14).
Aim
The sudden death of a young athlete (sudden athlete death, SAD) is a tragic and rare event, reported to occur in one to two cases out of 100,000 athletes each year (15, 16). A lack of knowledge of the current guidelines diminishes confidence in identifying children who may be at increased risk of injury (17–20) or even SAD (16, 21) as a result of participation in sports (22). Unfortunately, the academic literature that provides recommendations for participation in sport activities within the pediatric population that have been published during the last decade in Europe is limited and is mainly dedicated to specific illnesses or advanced athletes and not toward the general population. The aim of this EAP and ECPCP statement is not to present obligatory recommendations for sport pre-participation evaluation (PPE), but rather to summarize information based on analyses of the relevant literature and expert opinions regarding sports and exercise. This EAP statement reviews the key points of a patient's medical history and physical examination that should alert the clinician and guide healthcare professionals to make the best decisions for sports safety in their practice.
Recommendations for physical activity and sport participation for the population of children and adolescents published in the literature
In 2019, the American Academy of Pediatrics (AAP) published “The Fifth Edition of PPE Monograph,” which is an approach to sports PPE that should be considered by healthcare professionals as a guide to help recognize whether a particular medical condition requires special care in young athletes (23).
In Europe, literature concerning sports PPE guidelines in the pediatric population is limited:
• In 2011, recommendations for PA, recreational sports, and exercise training for children and adolescents with congenital heart disease were published by the Exercise, Basic, and Translational Research Section of the European Association of Cardiovascular Prevention and Rehabilitation, the European Congenital Heart and Lung Exercise Group, and the Association for European Paediatric Cardiology (AEPC) (24).
• In 2012, the Polish Society of Sports Medicine (PSSM) published a position regarding age criteria during qualification for training in selected sport disciplines (25).
• In 2017, the EAP published a resolution related to health, integrity, and doping in sports for the pediatric population and young adults (26).
• Cardiovascular pre-participation screening recommendations for young athletes were published in 2017 by the AEPC (27).
• Guidelines for participation in competitive sports for patients with congenital heart disease (CHD) older than 16 years were published in 2020 by the Section of Sports Cardiology and Exercise of the European Association of Preventive Cardiology Group (EAPC) and the ESC working on adult CHD and AEPC (28). In 2020, the European Childhood Obesity Group and the EAP published specific birth to adolescence age-appropriate PA recommendations based on a search of the published literature (3).
• In 2021, the European Federation of Sports Medicine Associations (EFSMA) along with nine other organizations published “Pre-participation medical evaluation for elite athletes: EFSMA recommendations on standardized pre-participation evaluation form in European countries” (29).
• In 2021, the ESC published guidelines on the task force for cardiovascular disease prevention in clinical practice (30).
Age-specific pre-participation cardiovascular evaluation (PPCE) proposals for Swiss pediatric and adolescent athletes (under 18 years of age) were published in 2022 (31).
Definitions
Physical activity and sports
According to the WHO glossary of terms, PA is defined as “any active bodily movement resulting from the contraction of skeletal muscles that raises energy expenditure above resting metabolic level” (5). The types of PA included aerobic exercise, muscle strengthening, balance, and flexibility exercises (32) to be performed at least three times per week as part of minimum 60 min daily routine (33). The dose of exercise can be determined using the frequency, intensity, time, and type of exercise (FITT) principles (34). Detailed guidelines for following FITT principles for PA within the healthy pediatric population are described in literature (34, 35).
Classification of sports and athletes
There are various types of sport activity which can be defined under different settings (5) such as:
• Leisure sports: recreational PA without pressure to play, continuous play, or play at a higher intensity based on the willingness of the subject. Any participants may stop or lower the intensity of their involvement at any time.
• Competitive sports: organized, competitive, and skillful PA within established rules of the sport.
• Exercise training: specialized, structured, planned methods and programs of PA used to enhance a participant's physical abilities.
A young athlete is defined as an individual, either amateur or professional, who participates in regular training and official sports competitions (36, 37). All PA can be described according to dynamic and static components, as shown in Table 1 (38).
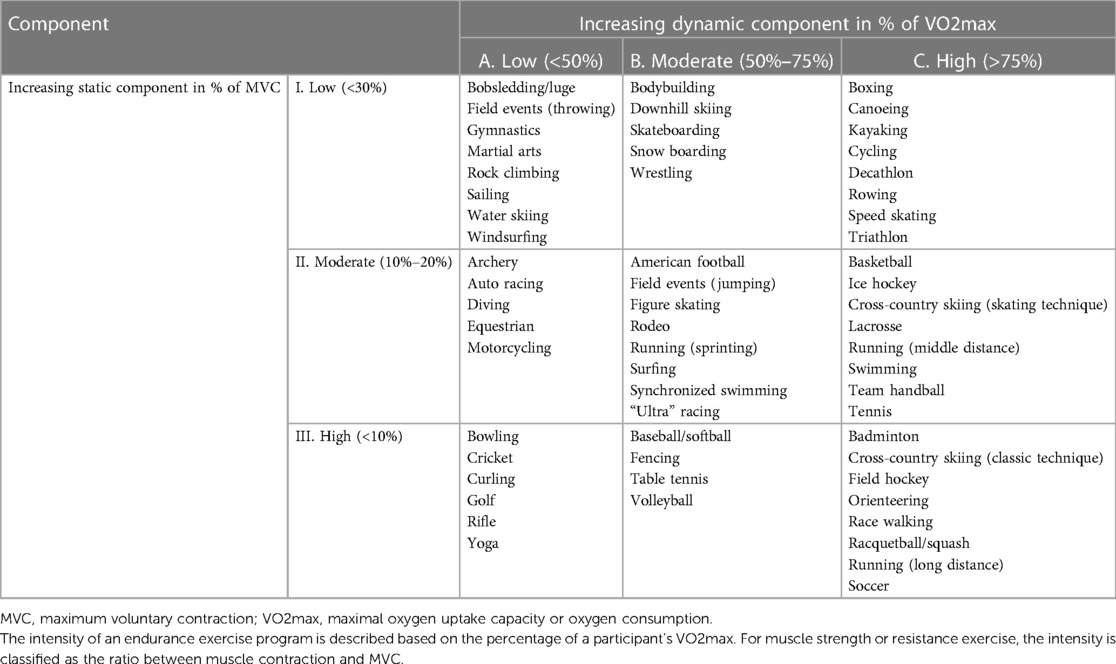
Table 1. Classification of sports according to dynamic and static components (37).
Exercise trainings are specialized and planned methods and programs of PA for increasing functional capacity, performance, or cardiorespiratory fitness (39, 40). Recommendations should describe the amount (frequency, intensity, duration) and types of PA (4, 28, 34). Three stages of all exercise training are (1) a 10–15 min warm-up period, (2) the specific exercise training, and (3) a 10 min cool-down period with stretching. Adequate recovery time should be provided between training sessions (12–48 h depending on the intensity of the training session and conditioning of the participant).
Age criteria for qualifying children and adolescents for participation in sports
General age criteria for participation in sports
Pediatric and adolescent athletes who are younger than 18 years of age may be defined as participating in competitive sports at a high level if they are practicing in a team setting for at least 6 h per week (31). Not all exercises have the same consequences for an individual's health status, whether positive or negative (40, 41). The peak age range for involvement in sports is between the ages of 10–14 years, although currently athletes begin specialized training at an increasingly younger age (42). This may be due to greater pressure for achievement from coaches or parents (43).
In 2014, the United States Olympic Committee along with the National Governing Bodies used the long-term athlete development principles to create the American Development Model (42). They created five stages including the following: (1) discover, learn, and play (ages 0–12 years); (2) develop and challenge (ages 10–16 years); (3) train and compete (ages 13–19 years); (4) high performance or participate and succeed (ages ≥15 years); and (5) mentor and thrive (for life).
In 2012 in Europe, the Polish Society of Sports Medicine (PSSM) published its position regarding age criteria during qualification for training in selected disciplines in the pediatric population (25). The criteria were developed depending on developmental age, because calendar age is not always an accurate indicator of a child's growth (44). General age criteria for participation in sports proposed by the PSSM for children and adolescents are as follows (25): (1) younger than 6 years (all disciplines based on natural forms of movements in the form of game and play involving movement); (2) older than 6 years (the disciplines based on natural forms of movement, developing coordination of movement that does not exert a selective load on the skeletal system); (3) older than 8 years (sport disciplines that develop agility, speed, and movement dynamics); (4) older than 10 years (sport disciplines that develop endurance and strength); (5) older than 13 years (disciplines involving a full range of endurance training); and (6) older than 15 years (disciplines in which a full range of static strength exercises can be introduced).
Individual differences in growth and maturation can lead to unforeseen consequences in competitive sports and an increased risk of injury, especially in athletes who are constitutionally smaller and/or delayed in maturation. Therefore, there has been a long tradition of proposals for selecting athletes based on physical characteristics rather than chronological age. This strategy is called “bio-banding” and involves grouping and/or assessing athletes based on size and/or maturity status rather than chronological age (45). According to Tanner, biological age determined by puberty stages (46, 47) is more appropriate than chronological age and should be used in assessments of young athletes. Maturation is the process of a child's growth toward obtaining adult stature. All humans experience maturation differently. Females tend to mature faster than boys, but post-pubertal boys will experience greater increases in strength and power due to testosterone and other androgen hormones. Maturation should be measured in young athletes to properly monitor their growth and wellbeing (48). While bio-banding puts athletes into groups based on physical attributes, it does not preclude the inclusion of psychological and/or technical skills. For example, boys that may have matured early may be discouraged from competing or training with older participants if they lacked the technical competence and/or mental maturity to provide a safe and positive experience (49). Implications of somatic growth and maturation for sport participation, overuse injuries in adolescents during times of rapid growth, and concepts of bio-banding for both training and competition based on biological maturation for youth sports (50, 51) will be discussed in a separate part of the Position of the European Academy of Paediatrics and the European Confederation of Primary Care Paediatricians.
Pre-participation physical evaluation
The main scope of sports PPE is to maximize safe participation. It should be individually adjusted to the participant especially during obligatory general pediatric consultations between the age of 0 and 18.
The objectives of the PPE are as follows (23, 52–56):
• Primary objectives: disclosure of defects that may limit participation and determine conditions that may be life-threatening or disabling.
• Secondary objectives: an indication of the general health of a child, examination of the level of maturation, provisions enabling an opportunity to answer questions, and introduction of the athlete into local sports.
• Other objectives: classification of an athlete according to individual qualifications, compliance with legal and insurance requirements for athletic programs, and provision of opportunities for children to compete.
In European countries, local and state requirements determine who has the authority to perform a PPE. General practitioners are responsible for conducting a PPE for children wishing to participate in sports, but in some countries, the determination of sport eligibility depends on the opinion of sport and exercise medicine (SEM) specialists, especially for top-level competitive sports (29, 57–62). The utility of the sports PPE in healthy populations has been questioned in recent years. The determination of relative contraindications should be made by an attending physician, who decides whether the patient is eligible for competitive sports or if further specific examinations are required. Although 3.2%–19.2% of athletes have a significant disclosure during the PPE, only 0.3%–1.3% of athletes are ultimately disqualified from involvement based on findings from the PPE (62–64). The Italian pre-participation evaluation program, diagnostic yield, rate of disqualification, and cost analysis, was published in 2020 (65). The PPE is commonly required by sports organizations to fulfill legal and insurance requirements for involvement in competitive sports, and mainly SEM specialists are qualified to conduct such PPEs (29).
The examination should be performed several weeks before a sporting event allowing time for additional examinations or treatment if needed. The AAP recommends a PPE at least 6 weeks prior to the beginning of the season to allow additional assessment and/or rehabilitation prior to competition (66). This may be too short of a time window because multiple specialists often collaborate with each performing a specific evaluation. The primary care physician needs to have time to assimilate all of the information for clinical decision-making and pre-competition screening.
Depending on governmental, state, or sport society requirements, a PPE should be repeated at least every 1–2 years or more frequently for selected sports or for selective health problems in athletes, especially in top-level athletes (59, 67, 68).
Forms of pre-participation physical evaluation
The diagnostic components of PPE are health status, anthropometry, functional capacity, and exercise capacity. For the PPE, both the American and European Societies currently recommend a thorough investigation of personal history, family history, and a limited physical examination to determine the general health of the athlete (23, 29, 55, 59, 64, 66). The physical assessment should include vital signs such as visual acuity and cardiovascular, pulmonary, abdominal, skin, genitalia, neurologic, and musculoskeletal examinations. Parental verification of personal and family history is also recommended.
The EFSMA emphasizes the need for an implementation of a standardized PPE among European countries to ensure the best care for adult athletes (29). Until now, very few reports on periodic health evaluations by PPE in adolescent elite athletes exist (68–70). In 2009, the International Olympic Committee published a Consensus Statement on the Periodic Health Evaluation of Olympic athletes, explaining the purposes and procedures of the PPE in adults (68). The youth PPE was shown to be efficient in diagnosing different disorders, enabling rapid treatment in 12% of Italian Olympic athletes (69). The AAP published standardized physical examination forms as tables with questions about family and athlete history and physical exams, as well as for young athletes with special needs for clearance decisions concerning participation in sports (23).
The pre-participation evaluation does not only focus on elements that determine known problems that affect sport involvement (71). During a PPE, a consulting physician can also educate the participants about injury prevention or concussion, first-aid and external defibrillator–cardioverter support performance, dietary counseling (72), and the effects of nutritional supplements (73). Finally, the PPE may provide an appropriate approach for preventing any doping practices (26).
The past several years, especially during the COVID-19 pandemic, has seen a rapid growth of electronic sports (eSports) media, thanks to the increasing availability of online games and broadcasting technologies (74), and numerous injuries may occur in the participants (eAthletes) (75). The potential benefits of a pre-participation evaluation and injury prevention program in eSports will be discussed in a separate part of the Position of the European Academy of Paediatrics and the European Confederation of Primary Care Paediatricians.
General considerations during a PPE to assess the overall health of a young athlete
wIt has been reported that in up to 58% of young athletes who do not positively pass the PPE screening, the decision to deny may be based on medical history alone or dizziness with exercise, history of asthma, body mass index (BMI), elevated systolic blood pressure, visual acuity, heart murmur, or problems detected during musculoskeletal examination (76). A pre-participation health evaluation in a cohort of adolescent athletes competing in Youth Olympic Games showed that PPE led to a diagnosis of pathological conditions in 12% of the population (69). The most prevalent diseases identified were cardiovascular and pulmonary diseases (4.5% each), followed by endocrine alterations (2%) and infectious, neurological, and psychiatric disorders (0.4% each). Cardiovascular disease was found in 3.9% of elite adult athlete cohort participants who underwent a comprehensive cardiovascular evaluation prior to participation in the Olympic Games (77).
Personal history
Personal history should identify past red flags and present medical conditions as well as previous surgeries and associated consequences such as past injuries, history of passing out, episodes of syncope or dizziness, any medicines currently being taken, vaccinations, history of allergies and anaphylaxis, infection diseases, headache, seizures, and any potential cardiovascular warning signs (high blood pressure, heart murmur, high cholesterol, myocarditis) (23, 56). Boys should be diagnosed for testicular pain. Girls should be asked about their menstruation. The physician should also inquire about smoking and vaping, alcohol intake, drugs, diet pills, or supplements, including steroids.
It is very important during a PPE to inquire about the actual type, amount, and intensity of exercise training, associated chest pain or heart palpitations experienced during or post exercise, trouble breathing during exercise, dizziness or syncope during exercise, and the presence of excessive, unexpected, or unexplained fatigue during exercise.
During a PPE, the consulting physician should inquire about dietary habits and eating disorders. Suggested diets for young athletes were presented in a Position Statement of the American Dietetic Association, Dietitians of Canada, and the American College of Sports Medicine (72). Further important components of a PPE are screening for mental health disorders (78). A list of recommended personal history questions from different systems during PPE in young athletes are summarized in Table 2.
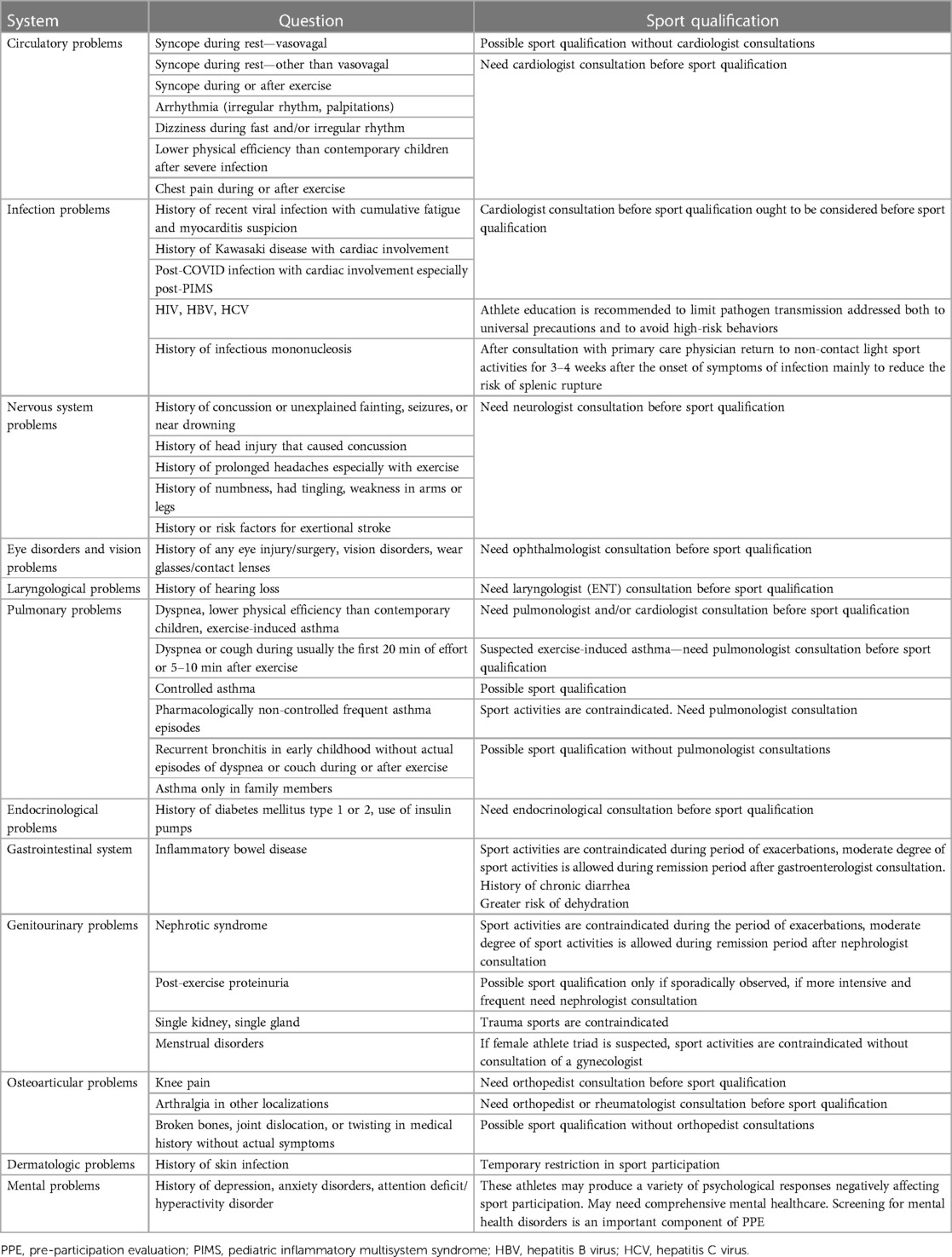
Table 2. List of recommended personal history questions from different systems during sports PPE in young athletes.
Family history
The PPE family history is designed to recognize athletes at risk, especially in those with a family history including SAD. Most sudden deaths have been attributed to congenital or acquired cardiovascular malformations (36, 79). Other causes of sudden death include heat stroke, cerebral aneurysm, asthma, commotio cordis, and sickle cell trait (80). Any athlete with a family history of the following conditions requires a full evaluation and cardiological follow-up (23, 24, 28, 29, 59, 81, 82). If anyone in the athlete's family:
• Died of heart problems or had sudden cardiac arrest before the age of 50 years or died for no apparent reason before the age of 50 years [to include sudden infant death syndrome (SIDS), unexplained car accident, drowning].
• Had any type of heart problem, primary pulmonary hypertension, arterial hypertension, family and hypercholesterolemia.
• Had syncope, presyncope, or unexplained seizures.
• Had significant arrhythmia, an ablation procedure, an implanted pacemaker, or defibrillator.
• Had exercise-induced asthma.
• Had any of the following genetic disorders including hypertrophic cardiomyopathy (HCM), dilated cardiomyopathy (DCM), arrhythmogenic right ventricular cardiomyopathy (ARVC), Marfan syndrome, and Ehlers–Danlos syndrome and channelopathies such as Brugada syndrome (BRS), long-QT syndrome (LQTS), or short-QT syndrome (SQTS).
Sudden death in young athletes is rare and is usually caused by a genetic or congenital structural cardiac disorder (83–85), so detailed family history may help in identifying athletes especially at risk of primary arrhythmia syndromes (23, 27, 67). The issues raised within a family history may be quite obscure to the athlete and family, but young athletes and their parents should still be informed by their physician why such data from the PPE are essential for lowering SAD risk. Importantly, any abnormal finding in the family history and/or physical examination including abnormal prior cardiovascular testing results and a positive family history including premature death (<50 years) and/or genetic cardiomyopathy in a first-degree relative requires further investigation, as suggested by international guidelines (15, 36).
Significant elements of a physical examination
Physical examinations must primarily screen the musculoskeletal, cardiovascular, and nervous systems. Abnormal breath sounds in the lungs should be diagnosed. The PPE may also include a dental and vision evaluation (risk of soft tissue lesions). The evaluation of vision can be performed using a standard vision chart (standard Snellen eye chart) with specification on the use of glasses or contact lenses.
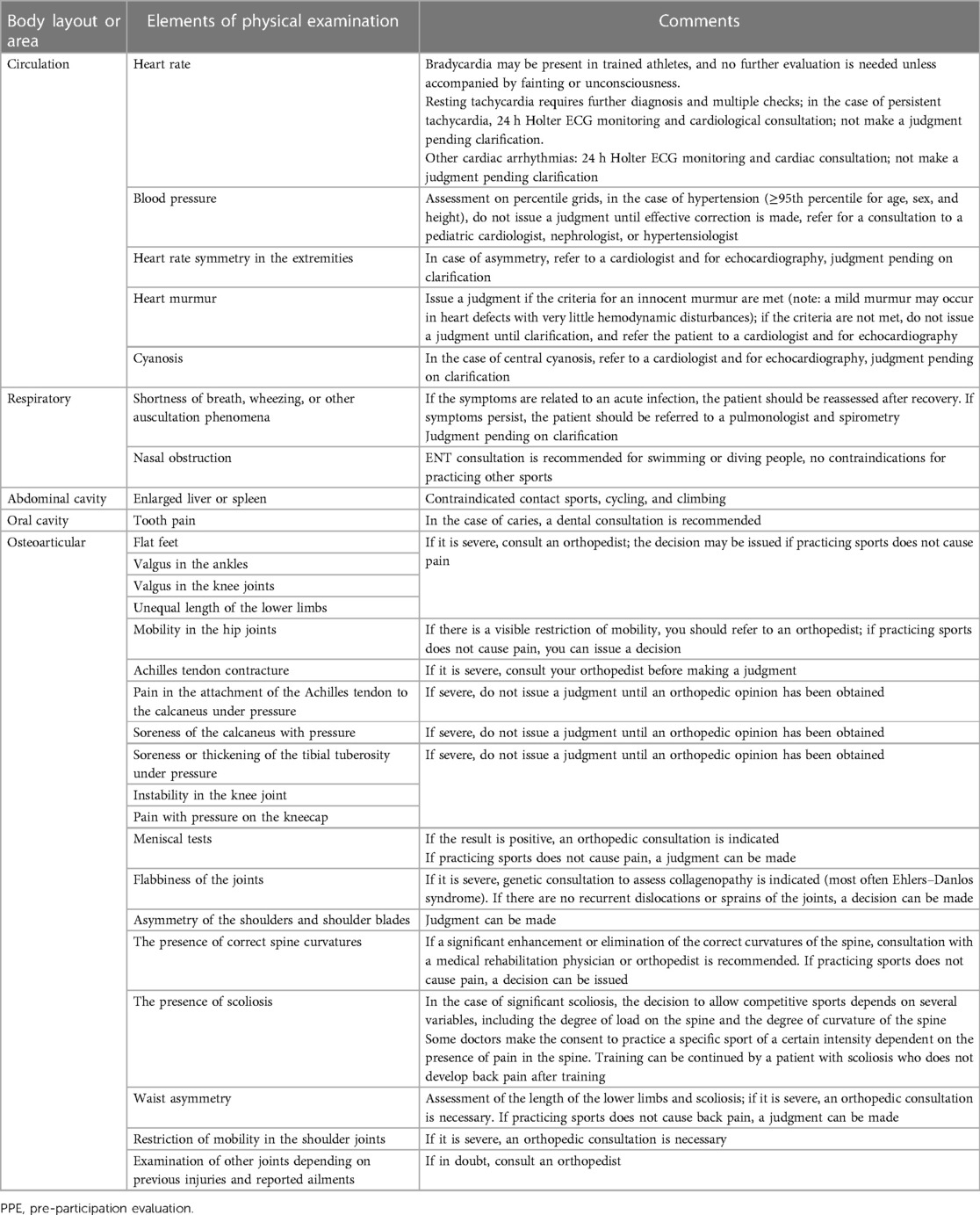
A critical component of a PPE is an anthropometric examination that includes somatoscopy, taking into account measurement of weight, height, BMI, sitting height, body composition, and girth measurements (29, 85, 86). Table 3 contains a summary of significant elements of a physical examination from different systems during a sports PPE.
Musculoskeletal system
Evidence for injury incidence and the long-term effects of participating in sports in the pediatric population are limited (17, 18, 87, 88). A musculoskeletal assessment is recommended to examine joints (89, 90), physical function (flexibility, posture, gait, muscle strength, joint laxity), and regional abnormalities (spine, upper extremity, lower extremity) (55, 62, 91). Of the conditions identified during the PPE, 14% required follow-up before clearance for participation (92, 93).
The first component of the orthopedic PPE is a complete history of previous injuries and surgeries. A previous musculoskeletal injury is a major risk factor for re-injury, especially if the original injury was not rehabilitated properly (92, 94).
The second component of the orthopedic PPE is the physical examination. The examination should evaluate spinal anomalies, deformity, and back pain (95). Back pain was reported in about 8% of young teenage athletes mainly from combat sports, team sports, explosive strength sports, and endurance sports (96). It is known that injury in anatomic regions such as the knees, ankles, and shoulders have a higher risk of future injury (97).
Suggested examples of quick musculoskeletal examinations are offered by the American Medical Society for Sports Medicine (AMSSM) in online educational resources (98). In 2021, the American College of Sports Medicine published Musculoskeletal and Sports Medicine Curriculum Guidelines for Pediatric Residents (99).
Nervous system
The neurological assessment is focused on the abnormal conditions observed during present and previous examinations (100, 101). Youth with a history of concussion should have a neurological assessment (102). Vision and/or hearing loss must be corrected, and consultation with an ophthalmologist or laryngologist may be necessary.
Abdomen
An abdominal assessment can be brief in the absence of a significant history of gastrointestinal (103–106) or nephrological diseases (81, 107–109). Splenic enlargement and history of recent infectious mononucleosis (Epstein–Barr virus infection) are temporary contraindications to sports because splenic rupture is a risk (110). An examination for boys should include assessment of the groin and genitalia. Privacy and chaperones should be present when such evaluations are included, asking for their consent (a second healthcare professional should stay in the room during these examinations). Genitourinary assessment in boys is particularly justified in the case of collision sports, because it is necessary to further protect boys having a single testicle.
Cardiovascular system
Most of the cases of SAD occur in individuals with a pre-existing cardiac abnormality, and in young athletes (<35 years), instances of SAD are mostly due to inherited or congenital cardiac disorders. In 2005, the Study Group of Sports Cardiology of the Working Group on Cardiac Rehabilitation and Exercise Physiology and the Working Group on Myocardial and Pericardial Diseases of the ESC published a common European protocol for cardiovascular pre-participation screening of young competitive athletes for the prevention of SAD which are termed “the Lausanne recommendations” (111). A position paper from 2017 promoted by the EHRA, and the EACPR reviewed the evidence regarding the appropriate diagnostic methods to determine selected heart conditions at risk in SAD (15).
It is obligatory during a PPE to inquire about cardiovascular disease in family history (112, 113) with a high life-threatening risk of cardiac arrest during exercise in young athlete (114). Since 1982, it has been mandatory for every Italian competitive athlete to undergo an annual PPE that includes an assessment of the CV system including non-CV evaluations to identify diseases that pose a risk of SAD during sports or other conditions that may threaten the athlete's health (113, 115). The ESC (111) and the AHA (116) suggested the adoption of a 14-element SAD screening tool during the PPE that contains medical history questions and four assessment elements. Table 4 presents a proposed set of screening questions concerning cardiological problems to be addressed during a PPE.
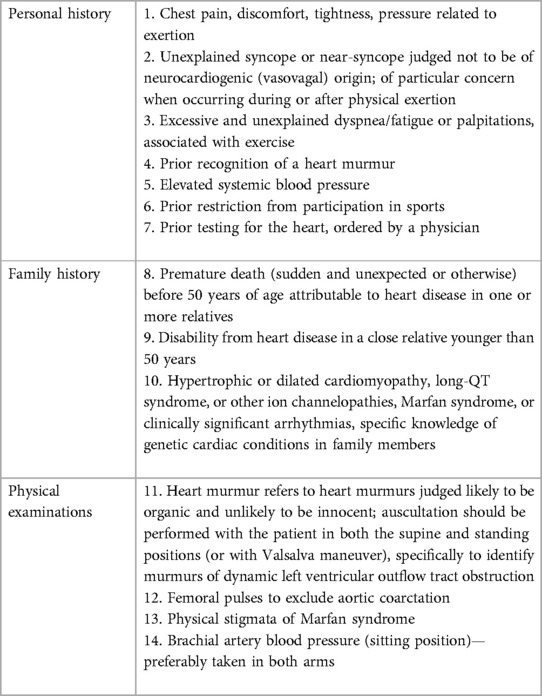
Table 4. The 14-element ESC (92) and AHA (96) questionnaire for pre-participation cardiovascular screening of competitive athletes.
The use of an electrocardiogram (ECG) is proposed as a screening tool in young athletes to identify potentially life-threatening arrhythmias (e.g., channelopathies, pre-excitation syndromes), structural congenital heart disease, and cardiomyopathies (21, 111). Data relating to the use of ECG during a PPE are controversial especially in the United States (117, 118) but may be required for highly trained athletes by some sports organization. In the absence of clear evidence, the AMSSM respects physician autonomy in implementing an ECG as the most appropriate PPE cardiovascular screening strategy (117). The EFSMA statement from 2015 on ECG for PPE concluded that ECG is very sensitive in heart screening (119). In Italy, cardiovascular PPE protocols including ECG prior to competitive sports practice was adopted by the ESC in 2005 as the “common European protocol” (111) and implemented by many National European Sport Associations during screening of top-level adult athletes (120, 121). In Europe, cardiovascular screening that includes ECG before playing sports in youth is supported by some governing bodies. In selected individual athletes, further non-invasive or invasive cardiac evaluation may be required before the final decision of clearance for participation after the initial cardiovascular PPE (111, 116). In Switzerland, it is recommended that all young athletes practicing with a team with a training load of at least 6 h per week undergo PPCE based on medical history and physical examination from the age of 12 years onward. Inclusion of a standard 12-lead ECG evaluation is also suggested for all post-pubertal athletes (or older than 15 years) with an analysis in accordance with the International Criteria for ECG Interpretation in Athletes (31).
Specific individual history and physical examination forms
Laboratory tests
There are no routine laboratory tests that have been proven to be useful and cost-effective as elements of a PPE (67). Routine laboratory or other tests during the PPE have not been supported by sports medicine societies (67, 122).
The female and male athlete triad syndrome in top-level young athletes
The female athlete triad syndrome with symptoms of amenorrhea, decreased bone mineral density (frequent stress fractures, osteoporosis), and disordered eating may appear in the absence of a balanced diet (123–125). The male athlete triad syndrome occurs most frequently in adolescent and young adult male endurance and weight-class athletes and includes low energy availability with or without disordered eating, functional hypothalamic hypogonadism, and osteoporosis or low bone mineral density (125, 126). In 2014, the International Olympic Committee (IOC) changed the term athlete triad to relative energy deficiency in sports (RED-S) (127). This concept allows identification of energy deficiency as a key to the disruption of several physiological functions of different areas, such as reproduction, bone, endocrine, metabolic, hematological, growth and development, physiological, cardiovascular, gastrointestinal, and immunological, with consequences for the performance and health of the athlete in general (128).
Doping laws
During a PPE, it is necessary to inform a child or adolescent who is eligible for competitive sports that he or she must meet the requirements of doping laws (26, 129, 130). Establishing a Therapeutic Use Exemptions Certificate is therefore mandatory if subjects need to take any of the prohibited substances or medical therapies listed each year by the World Anti-Doping Agency (www.wada-ama.org) (131).
Sport disciplines associated with increased risk of undesirable health consequences
Sports recommendations for young athletes should also be concerned with the particular form of PA. Healthcare providers should recognize individual risks for the pediatric athlete in participating in the sport discipline chosen, because some sport disciplines may have particular constraints and may be subject to specific medical examinations. According to the government regulations in France, sport disciplines with a higher risk of injury for athletes are as follows (130, 132): (1) practiced in a specific environment (mountaineering, underwater diving, caving), (2) competition fighting, in which the fight may end as a result rendering them unconscious and incapable of defending themselves, (3) involving the use of firearms or compressed air, (4) involving the use of motorized land vehicles (except for radio-controlled automobile model making), (5) aeronautical sport disciplines practiced in competition (except for model aircraft), (6) parachuting, and (7) rugby fifteens, rugby thirteen, and rugby sevens.
Some PA might be related to a higher risk of injury if unconsciousness occurs (e.g., in swimming, climbing, or horseback riding), and some other types of PA have a high risk of collision or trauma (e.g., in athletes with implanted electrical cardiological devices or with congenital bleeding disorders who are taking anticoagulants) (19, 24, 28, 133). Sport disciplines have been classified as non-contact, limited contact, or with contact/collision which were described in detail by the AAP (23, 52).
The safe age categories for combat sport disciplines are proposed below with criteria that are considered in the most frequently practiced sport disciplines: (1) participation in boxing for children and youth is not recommend, and (2) children younger than 12 years may participate only in non-contact sports involving training and competition in a form of technique demonstration or directed combat with task performance. They can participate in competition with non-contact activities. In disciplines not involving kicking or hitting, children can participate in training and competition from the age of 9–10 years in accordance with the regulations of sport federations, and (3) youth older than 12 years, who have participated in training and non-contact disciplines for at least 9 months, may participate in classes and training sessions and compete in combat sports with limited contact if the training or competition does not involve fighting using hand or leg blows with full force (25).
In all combat sports that include hitting or kicking, or use of weapons, participants should use protection for the mouth, genitals, breast (girls), and other body parts according to regulations (25). Table 5 contains a list of recommended significant personal history questions to be asked during a PPE before qualification for selected sport disciplines for young athletes associated with increased risk of undesirable health consequences.
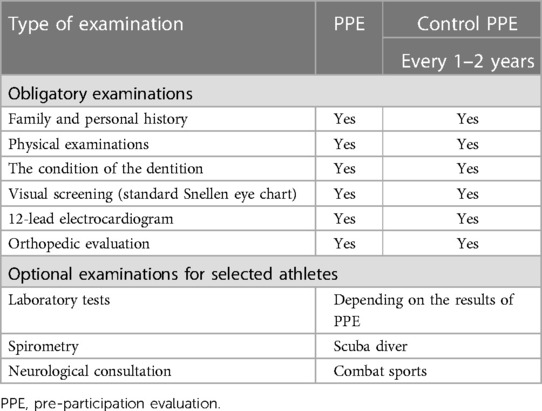
Table 5. List of recommended diagnostic examinations during the first pre-participation physical evaluation and repeated every 1–2 years during repetitive control evaluation of young athletes.
Young athlete medical eligibility form
After the results of the PPE are analyzed, athletes will likely be classified according to one of the following (29):
• Medically eligible for sports performance without restriction.
• Medically eligible with recommendation for further management.
• Not medically eligible for sports performance: for all sport disciplines or a selected discipline, temporary or constantly contraindicated.
Healthcare professionals should provide written guidelines with restrictions and permissions regarding adequate levels of PA and exercise. Determination of sports eligibility depends on historical and current examination findings and the sport in which the athlete desires to participate. Fever, acute illness, and viral myocarditis are conditions temporarily limiting sport participation. Limiting activity is also important for preventing complications such as dehydration or thermoregulatory problems. Some athletes will require further re-evaluation (e.g., referral to cardiology, neurology, or orthopedic specialists) (28, 95, 99, 100) and treatment (e.g., treatment of hypertension or exercise-induced bronchospasm, ablation of accessory pathway in WPW syndrome, implantation of cardioverter defibrillator) (28), or they should be included in a physiotherapy program (e.g., after an orthopedic operation) before a return to play (RTP). Participation in PA should be assessed regularly.
Table 6 contains a list of proposed diagnostic examinations during the first PPE which should be repeated every 1–2 years for a repetitive control evaluation of young athletes.
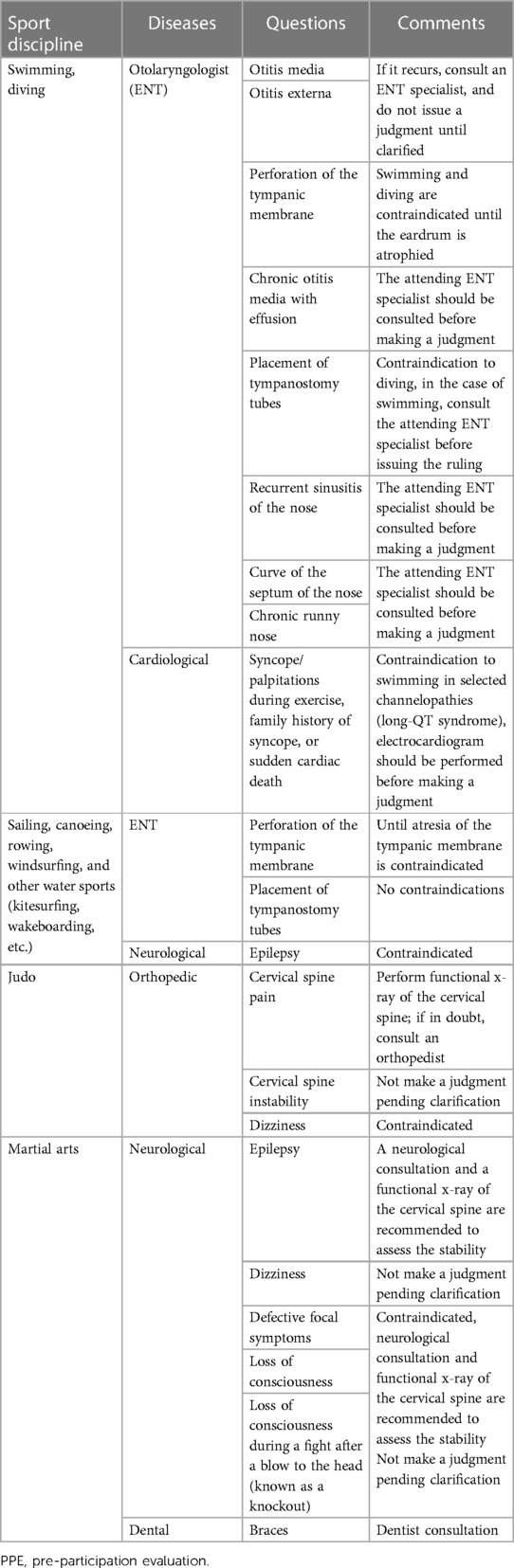
Table 6. List of recommended significant personal history questions during PPE before qualification to selected sport discipline in young athletes with increased risk of undesirable health consequences.
Evaluation for resumption of physical activity/sport activity for a child/adolescent with COVID-19 infection
Serious consideration needs to be given to RTP policies regarding COVID-19 infections in the pediatric and adolescent population. The AAP guidance from 2022 suggested that all eligible participants should receive a primary course of COVID-19 vaccine or booster doses when recommended (135). A history of COVID-19 infection and symptoms should also be included in the PPE (135). Any young athlete who tests positive for current COVID-19 infection, even if asymptomatic, should avoid all training and games until cleared by a physician. Long COVID is diagnosed when symptoms persist for more than 3 months (136). This condition includes many clinical symptoms such as fatigue, breathlessness, brain fog, depression, and inability to return to normal PA. Coronavirus disease has also created a new condition termed pediatric multisystem inflammatory syndrome (PIMS) (137). Multi-organ changes during PIMS can involve the cardiovascular, respiratory, kidney, gastrointestinal, and neurological systems.
The decision to return to PA after COVID-19 should take into account the duration of the disease, the severity of respiratory or cardiac symptoms (138), as well as the presence of comorbidities, and the capacity and the intensity of the planned exercise (139). In 2022, the Scientific Council of the Deutsche Gesellschaft fur Sportmedizin und Pravention (DGSP) published guidelines for returning to sports after COVID-19 that was addressed to elite athletes (140). It recommended limiting PA with a 3-day training pause after the time of diagnosis for an asymptomatic course of COVID-19. Mild competitions may be possible after a total of 10 days have elapsed after the symptoms have disappeared. In a recent document from 2022, the AAP recommends that members of the pediatric population have a minimum of 2-week rest period without exercises (134). Symptomatic patients should limit PA for 2–4 weeks. In Europe, athletes are advised to wait to RTP for a minimum of 10 days from the onset of symptoms, plus a minimum of 7 days from the resolution of COVID-19 symptoms (141). Because of the limited information on COVID-19 and exercise, it is strongly advised that all athletes who have had COVID-19 be cleared for participation by their primary care physician (134). If primary care physicians have any questions regarding their patients’ readiness to return to competition, they should feel free to refer them to a pediatric medical subspecialist. Any child with a history of a positive COVID-19 test, regardless of whether they had symptoms, should be screened for chest pain, shortness of breath, syncope, and palpitations and have a complete physical exam (142, 143). Youth who have had moderate or severe symptoms of COVID-19 should be referred to a cardiologist (144, 145).
Table 7 summarizes sports recommendations based on the severity of symptoms for children and adolescents according to the WHO definitions of COVID-19 infection (146).
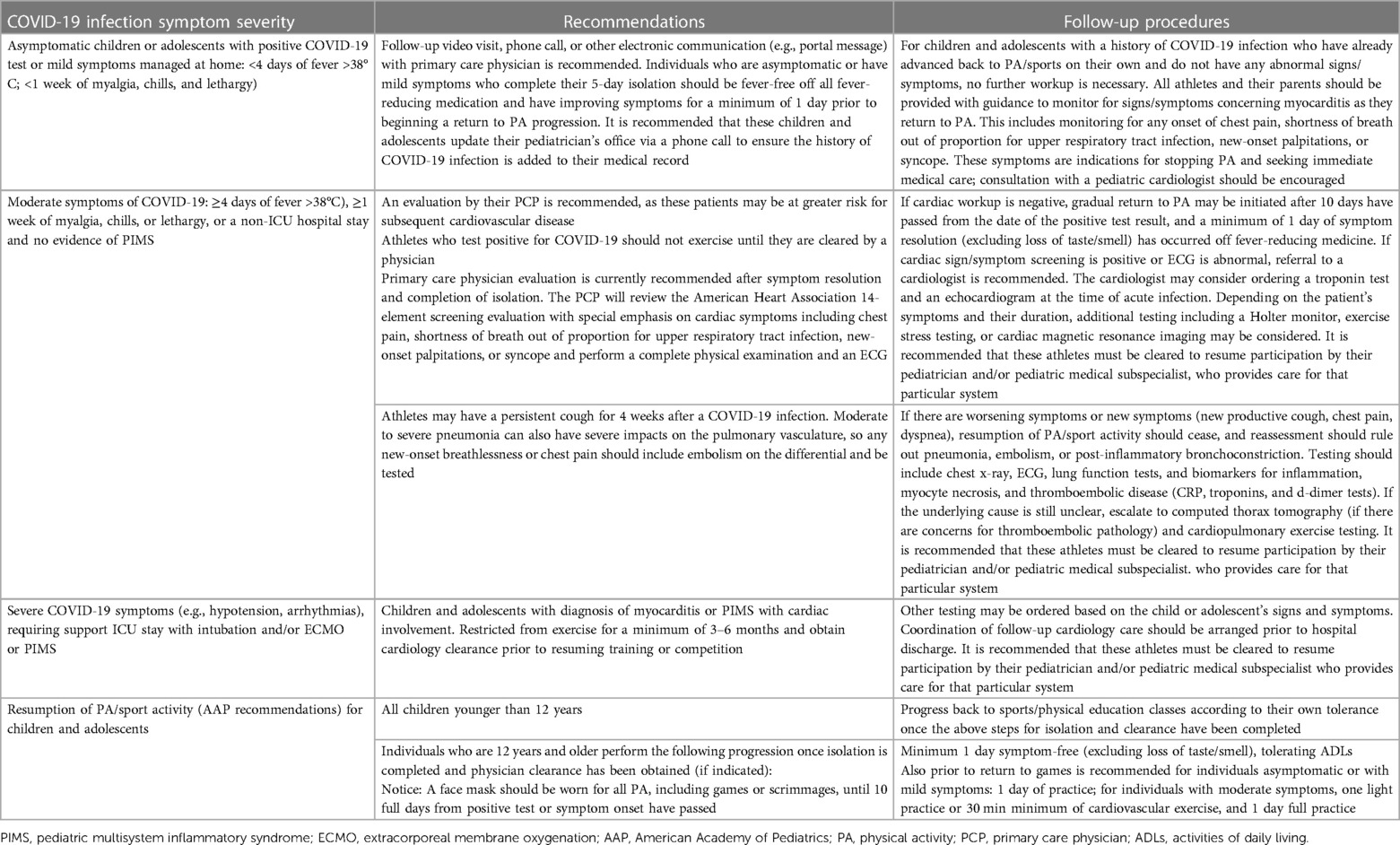
Table 7. Recommendations for resumption of physical activity/sport activity based on the severity of symptoms for children and adolescents with COVID-19 infection.
When returning to PA, children and adolescents should gradually increase the frequency, training volume (duration of training session, miles, repetitions), and intensity of activity to avoid injury. Based on an assessment of current and previous activity levels, young athletes should return to activity at 25%–50% of the volume and intensity at which they were participating previously (147). Finally, it is important to consider not only the physical but also the mental wellbeing of athletes before RTP (148). Counseling or psychotherapy should be considered for those having difficulty coping or for those experiencing emotional distress (149).
Sports and exercise medicine
Sport and exercise medicine is a new multidisciplinary medical specialty that supports all subjects and patients who want to engage in PA, exercise, and sports. These medical specialists are also experts regarding the performance of athletes while maintaining their health (57). In Europe, there are countries where SEM is not a medical specialty (150–152). As a result, athletes’ screening programs performed by a pediatrician may differ. Pre-participation physical evaluations certified by SEM are mandatory or strongly recommended mainly for competitive sports (151). In opinion of the EFSMA, it is essential that medical specialists involved in sport and exercise medicine aspire to create a standard of care for athletes at all levels, including a standardized digital PPE among European countries (29, 58).
Summary
Currently, there are no uniform and accepted guidelines for a PPE protocol to be implemented by primary care physicians in Europe for the general pediatric population. The first part of the EAP and the ECPCP position statement presents and summarizes the criteria which are considered to be the most frequently practiced in sports PPE based on expert opinion, reflecting an analysis of the current literature. The aim of this statement is to assist health professionals in implementing the best management programs for sports PPE in individual children and adolescents.
In the absence of a uniform protocol, it is necessary to respect physician autonomy for choosing and implementing the most appropriate and familiar PPE screening strategy and to discuss the decisions made with young athletes and their families (117). This first part of the Position Statement concerning Sport Activities for Children and Adolescents is dedicated to healthy young athletes and does not cover all problems of sport participation in the pediatric population.
EAP and ECPCP statement for pediatrician and primary care pediatricians concerning pre-participation physical evaluation in young athletes: summary
1. The utility of the sports PPE in the healthy population has been questioned in recent years, but the EAP and the ECPCP strongly recommend performing such evaluation in children and adolescents because the main scope of sports PPE is to maximize safe participation in the pediatric population of athletes.
2. In European countries, local and state requirements determine who is authorized to carry out sports PPE: usually these are general practitioners or pediatricians, but in some countries, the determination of sports eligibility depends on the opinion of the sport and exercise medicine specialist, especially for top-level competitive sports.
3. The timing of the sports PPE should be several weeks before a competition in order to incorporate additional examinations or treatment if needed and should be repeated at least every 1–2 years or more frequently depending on government, state, or sport society requirements, in selected type of sports or for selective health problems in athletes, especially in top-level athletes.
4. In the opinion of the EAP and the ECPCP, sports PPE should include diagnostic elements such as health status, anthropometry, functional capacity, and exercise capacity. The PPE history is designed to identify athletes at risk, especially in athletes with a family history of sudden death. Parental verification of individual and family history is recommended. A physical examination should include an evaluation of biological maturation and vital signs such as visual acuity and a cardiovascular, pulmonary, abdominal, skin, genitalia, neurologic, and musculoskeletal assessment.
5. The EAP and the ECPCP recommend educating athletes during the PPE in topics such as injury prevention or concussion, first-aid and external defibrillator–cardioverter support performance, dietary counseling, the effects of nutritional supplements, and doping practices.
6. Because most of the cases of cardiac death in pediatric athletes occur during exercise in individuals with pre-existing cardiac abnormalities, mostly due to inherited or congenital cardiac disorders, the EAP and the ECPCP strongly recommend to apply protocol proposed by the ESC for a cardiovascular PPE of athletes for the prevention of SAD; the so-called “the Lausanne recommendations.”
7. In the opinion of the EAP and the ECPCP, an electrocardiogram is a very sensitive screening tool for young athletes to determine heart disease or cardiomyopathies. According to ESC recommendations, it is recommended to include an ECG in a PPE cardiovascular screening before practicing sports.
8. Healthcare providers should recognize the individual risks of a pediatric athlete participating in a chosen sport discipline because some sport disciplines may have particular constraints and are subject to a specific medical assessment.
9. Young athletes should be classified as (1) medically eligible for sports performance without restriction, (2) medically eligible with recommendation for further evaluation, or (3) under treatment or not medically eligible for sports performance for all sport disciplines or a selected discipline temporary or constantly contraindicated. Young athletes should receive recommendations regarding appropriate levels of PA and exercise.
10. The EAP and the ECPCP encourages collaborative decision-making with the athlete and his or her family or caregiver.
11. Serious consideration needs to be given to return-to-play policies regarding COVID-19 infections in the pediatric and adolescent population. The EAP and the ECPCP strongly recommend that a history of COVID-19 infection and symptoms also be included in the PPE, and any young athlete who tests positive for current COVID-19 infection, even if asymptomatic, should cease all trainings and games until medical approval is obtained.
12. The aim of presented first part of the EAP and the ECPCP position statement is to assist healthcare professionals in implementing the best management strategies for sports pre-participation in individual children and adolescents.
13. In the absence of a uniform sports PPE protocol for children and adolescents in Europe, this EAP and ECPCP statement is not a formal recommendation for PPE, but rather a summary of practical applications and suggestions based on a current narrative review. In the opinion of the EAP and the ECPCP, it is necessary to respect physician autonomy for choosing and implementing the most appropriate and familiar PPE screening strategy and to discuss the decisions made with young athletes and their families.
Author contributions
AT-K and DN: study design. AT-K, JW, and MK-D: data collection. AT-K, DN, TK, AB, MK-D, and AH: data analysis and interpretation. AT-K, DN, and JW: manuscript preparation. AM, ŁD, SdT, ZG, SB, JP-P, and GH: critical revision. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Emmonds S, Weaving D, Lara-Bercial S, Till K. Youth sport participation trends in Europe. Leeds, UK: ICOACHKIDS (2021). p. 1–38. doi: 10.13140/RG.2.2.30102.88644
2. Riner WF, Sellhorst SH. Physical activity and exercise in children with chronic health conditions. J Sport Health Sci. (2013) 2:12–20. doi: 10.1016/j.jshs.2012.11.005
3. Wyszynska J, Ring-Dimitriou S, Thivel D, Weghuber D, Hadjipanayis A, Grossman Z, et al. Physical activity in the prevention of childhood obesity: the position of the European Childhood Obesity Group and the European Academy of Pediatrics. Front Pediatr. (2020) 8:535705. doi: 10.3389/fped.2020.535705
4. West SL, Banks L, Schneiderman JE, Caterini JE, Stephens S, White G, et al. Physical activity for children with chronic disease; a narrative review and practical applications. BMC Pediatr. (2019) 19:12. doi: 10.1186/s12887-018-1377-30
5. Fiona C, Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, et al. World Health Organization 2020 guidelines on physical activity and sedentary behavior. Br J Sports Med. (2020) 54:1451–62. doi: 10.1186/s12966-020-01037-z
6. Reiner M, Niermann C, Jekauc D, Woll A. Long-term health benefits of physical activity–a systematic review of longitudinal studies. BMC Publ Health. (2013) 13:813. doi: 10.1186/1471-2458-13-813
7. Biddle SJ, Asare M. Physical activity and mental health in children and adolescents: a review of reviews. Br J Sports Med. (2011) 45:886–95. doi: 10.1136/bjsports-2011-090185
8. Sampasa-Kanyinga H, Colman I, Goldfield GS, Janssen I, Wang J, Podinic I, et al. Combinations of physical activity, sedentary time, and sleep duration and their associations with depressive symptoms and other mental health problems in children and adolescents: a systematic review. Int J Behav Nutr Phys Act. (2020) 17:72. doi: 10.1186/s12966-020-00976-x
9. Niebauer J, Börjesson M, Carre F, Caselli S, Palatini P, Quattrini F, et al. Recommendations for participation in competitive sports of athletes with arterial hypertension: a position statement from the sports cardiology section of the European Association of Preventive Cardiology (EAPC). Eur Heart J. (2018) 39:3664–71. doi: 10.1093/eurheartj/ehy511
10. World Health Organization. Physical activity (2022). Available at: https://www.who.int/teams/health-promotion/physical-activity/global-status-report-on-physical-activity-2022. (Accessed December 10, 2022)
11. Chaput JP, Willumsen J, Bull F, Chou R, Ekelund U, Firth J, et al. 2020 WHO guidelines on physical activity and sedentary behaviour for children and adolescents aged 5–17 years: summary of the evidence. Int J Behav Nutr Phys Act. (2020) 17:141. doi: 10.1186/s12966-020-01037-z
12. Guthold R, Stevens GA, Riley LM, Bull FC. Global trends in insufficient physical activity among adolescents: a pooled analysis of 298 population-based surveys with 1·6 million participants. Lancet Child Adolesc Health. (2020) 4:23–35. doi: 10.1016/S2352-4642(19)30323-2
13. Palermi S, Vecchiato M, Pennella S, Marasca A, Spinelli A, De Luca M, et al. The impact of the COVID-19 pandemic on childhood obesity and lifestyle: a report from Italy. Pediatr Rep. (2022) 14:410–8. doi: 10.3390/pediatric14040049
14. Neville RD, Lakes KD, Hopkins WG, Tarantino G, Drape CE, Beck R, et al. Global changes in child and adolescent physical activity during the COVID-19 pandemic: a systematic review and meta-analysis. JAMA Pediatr. (2022) 11:e222313. doi: 10.1001/jamapediatrics.2022.2313
15. Mont L, Pelliccia A, Sharma S, Biff A, Borjesson M, Brugada J, et al. Pre-participation cardiovascular evaluation for athletic participants to prevent sudden death: position paper from the EHRA and the EACPR, branches of the ESC. Endorsed by APHRS, HRS, and SOLAECE. Eur J Prev Cardiol. (2017) 24:41–69. doi: 10.1177/2047487316676042
16. Maron BJ, Haas TS, Doerer JJ, Thompson PD, Hodges JS. Comparison of U.S. and Italian experiences with sudden cardiac deaths in young competitive athletes and implications for preparticipation screening strategies. Am J Cardiol. (2009) 104:276–80. doi: 10.1016/j.amjcard.2009.03.037
17. McGuine T. Sports injuries in high school athletes: a review of injury-risk and injury-prevention research. Clin J Sport Med. (2006) 16:488–99. doi: 10.1097/01.jsm.0000248848.62368.43
18. Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. (2007) 42:311–9.17710181
19. Herring H, Kibler WB, Putukian M, Solomon GS, Boyajian-O’Neill L, Dec KL, et al. Selected issues in sport-related concussion (SRCI mild traumatic brain injury) for the team physician: a consensus statement. Br J Sports Med. (2021) 55:1251–61. doi: 10.1136/bjsports-2021-104235
20. Caine D, Maffulli N, Caine C. Epidemiology of injury in child and adolescent sports: injury rates, risk factors, and prevention. Clin Sports Med. (2008) 27:19–50. doi: 10.1016/j.csm.2007.10.008
21. Harmon KG, Zigman M, Drezner JA. The effectiveness of screening history, physical exam, and ECG to detect potentially lethal cardiac disorders in athletes: a systematic review/metaanalysis. J Electrocardiol. (2015) 48:329–38. doi: 10.1016/j.jelectrocard.2015.02.001
22. Joy EA, Pescatello LS. Pre-exercise screening: role of the primary care physician. Isr J Health Policy Res. (2016) 5:29. doi: 10.1186/s13584-016-0089-0
23. Bernhardt D, Roberts WO. Chapter 5, general considerations, of the history, physical examination, and medical eligibility. In: Bernhardt D, Roberts WO, editors. Preparticipation physical evaluation (PPE) monograph. 5th ed. Illinois, USA: American Academy of Pediatrics, American Academy of Family Physicians, American College of Sports Medicine, American Medical Society for Sports Medicine, American Medical Society for Sports Medicine, American Orthopaedic Society for Sports Medicine, and American Osteopathic Academy of Sports Medicine (2019). p. 35–42.
24. Takken T, Giardini A, Reybrouck T, Gewillig M, Hövels-Gürich HH, Longmuir PE, et al. Recommendations for physical activity, recreation sport, and exercise training in paediatric patients with congenital heart disease: a report from the Exercise, Basic & Translational Research Section of the European Association of Cardiovascular Prevention and Rehabilitation, the European Congenital Heart and Lung Exercise Group, and the Association for European Paediatric Cardiology. Eur J Prev Cardiol. (2012) 19:1034–65. doi: 10.1177/1741826711420000
25. Kostka T, Furgal W, Gawroński W, Bugajski A, Czamara A, Klukowski K, et al. Recommendations of the Polish Society of Sports Medicine on age criteria while qualifying children and youth for participation in various sports. Br J Sports Med. (2012) 46:159–62. doi: 10.1136/bjsports-2011-090043
26. Crawley FP, Hoyer P, Mazur A, Siderius L, Grosek S, Stiris T, et al. Health, integrity, and doping in sports for children and young adults. A resolution of the European Academy of Paediatrics 2017. Eur J Pediatr. (2017) 176:825–8. doi: 10.1007/s00431-017-2894-z
27. Fritsch P, Pozza RD, Ehringer-Schetitska D, Jokinen E, Herceg-Cavrak V, Hidvegi E, et al. Cardiovascular pre-participation screening in young athletes: recommendations of the Association of European Paediatric Cardiology. Cardiol Young. (2017) 27:1655–60. doi: 10.1017/S1047951117001305
28. Budts W, Pieles GE, Roos-Hesselink JW, Sanz de la Garza M, D'Ascenzi F, Giannakoulas G, et al. Recommendations for participation in competitive sport in adolescent and adult athletes with congenital heart disease (CHD): position statement of the sports cardiology & exercise section of the European Association of Preventive Cardiology (EAPC), the European Society of Cardiology (ESC) Working Group on adult congenital heart disease and the sports cardiology, physical activity and prevention working group of the Association for European Paediatric and Congenital Cardiology (AEPC). Eur Heart J. (2020) 41:4191–9. doi: 10.1093/eurheartj/ehaa501
29. Ionescu AM, Pitsiladis YP, Rozenstoka S, Bigard X, Löllgen H, Bachl N, et al. Preparticipation medical evaluation for elite athletes: EFSMA recommendations on standardized preparticipation evaluation form in European countries. BMJ Open Sport Exerc Med. (2021) 7:e001178. doi: 10.1136/bmjsem-2021-001178
30. Visseren FLJ, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M, et al. 2021 ESC guidelines on cardiovascular disease prevention in clinical practice developed by the task force for cardiovascular disease prevention in clinical practice with representatives of the European Society of Cardiology and 12 medical societies with the special contribution of the European Association of Preventive Cardiology (EAPC). Eur Heart J. (2021) 42:32273337. doi: 10.1093/eurheartj/ehab484
31. Albiński M, Balmera C, Wilhelmd M, Meyere P, Gassa M, Schmiedf C, et al. Paediatric and adolescent athletes in Switzerland: age-adapted proposals for pre-participation cardiovascular evaluation. Swiss Med Wkly. (2022) 152:w30128. doi: 10.4414/SMW.2022.w30128
32. Andriyani FD. Physical activity guidelines for children. J Pendidik Jasm Indones. (2014) 10:61–7. doi: 10.21831/jpji.v10i1.5691
33. Michel J, Bernier A, Thompson LA. Physical activity in children. JAMA Pediatr. (2022) 176:622. doi: 10.1001/jamapediatrics.2022.0477
34. Takken T, Hulzebos EH. Exercise testing and training in chronic childhood conditions. Hong Kong Physiother J. (2013) 31:58–63. doi: 10.1016/j.hkpj.2013.05.002
35. Edouard P, Gautheron V, D’Anjou MC, Pupier L, Devillard X. Training programs for children: literature review. Ann Readapt Med Phys. (2007) 50:510–9; 499–509. doi: 10.1016/j.annrmp.2007.04.015
36. Pelliccia A, Sharma S, Gati S, Back M, Borjesson M, Caselli S, et al. 2020 ESC guidelines on sports cardiology and exercise in patients with cardiovascular disease. The task force on sports cardiology and exercise in patients with cardiovascular disease of the European Society of Cardiology (ESC). Eur Heart J. (2021) 42:17–96. doi: 10.1093/eurheartj/ehaa605
37. Kinney J, Velghe J, Fee J, Isserow S, Drezner JA. Defining athletes and exercisers. Am J Cardiol. (2019) 123:532–5. doi: 10.1016/j.amjcard.2018.11.001
38. Mitchell JH, Haskell W, Snell P, Van Camp SP. Task force 8: classification of sports. J Am Coll Cardiol. (2005) 45:1364–7. doi: 10.1016/j.jacc.2005.02.015
39. Takken T, Bongers BC, van Brussel M, Haapala E, Hulzebos EH. Cardiopulmonary exercise testing in pediatrics. Ann Am Thorac Soc. (2017) 14(1 Suppl):S123–6. doi: 10.1513/AnnalsATS.201611-912FR
40. Jayanthi N, Schley S, Cumming SP, Myer GD, Saffel H, Hartwig T, et al. Developmental training model for the sport specialized youth athlete: a dynamic strategy for individualizing load-response during maturation. Sports Health. (2021) 14:142–53. doi: 10.1177/19417381211056088
41. Dalton SE. Overuse injuries in adolescent athletes. Sports Med. (1992) 13:58–70. doi: 10.2165/00007256-199213010-00006
42. Brenner JS, AAP Council on Sports Medicine and Fitness. Sports specialization and intensive training in young athletes. Pediatrics. (2016) 138:e20162148. doi: 10.1542/peds.2016-2148
43. Washington RL, Bernhardt DT, Gomez J, Johnson MD, Martin TJ, Rowland JW, et al. Organized sports for children and preadolescents. Pediatrics. (2001) 107:1459–62. doi: 10.1542/peds.107.6.1459
44. Beunen GP, Rogol AD, Malina RM. Indicators of biological maturation and secular changes in biological maturation. Food Nutr Bull. (2006) 27(4 Suppl Growth Standard):S244–S56. doi: 10.1177/15648265060274S508
45. Malina RM. Children and adolescents in the sport culture: the overwhelming majority to the select few. J Exerc Sci Fit. (2009) 7:S1–10. doi: 10.1016/S1728-869X(09)60017-4
46. Marshall WA, Tanner JM. Variations in pattern of pubertal changes in girls. Arch Dis Child. (1969) 44(235):291–303. doi: 10.1136/adc.44.235.291
47. Marshall WA, Tanner JM. Variations in the pattern of pubertal changes in boys. Arch Dis Child. (1970) 45(239):13–23. doi: 10.1136/adc.45.239.13
48. Brown KA, Patel DR, Darmawan D. Participation in sports in relation to adolescent growth and development. Transl Pediatr. (2017) 6(3):150–9. doi: 10.21037/tp.2017.04.03
49. Lloyd RS, Oliver JL, Faigenbaum AD, Myer GD, De Ste Croix MBA. Chronological age vs. biological maturation: implications for exercise programming in youth. J Strength Cond Res. (2014) 28:1454–64. doi: 10.1519/JSC.0000000000000391
50. Bergeron MF, Mountjoy M, Armstrong N, Chia M, Côté J, Emery CA, et al. International Olympic committee consensus statement on youth athletic development. Br J Sports Med. (2015) 49(13):843–51. doi: 10.1136/bjsports-2015-094962
51. Côté J, Lidor R, Hackfort D. ISSP position stand: to sample or to specialize? Seven postulates about youth sport activities that lead to continued participation and elite performance. Int J Sport Exerc Psychol. (2009) 9:7–17. doi: 10.1080/1612197X.2009.9671889
52. van Brussel M, van der Net J, Hulzebos E, Hulzebos E, Helders PJM, Takken T. The Utrecht approach to exercise in chronic childhood conditions: the decade in review. Pediatr Phys Ther. (2011) 23:2–14. doi: 10.1097/PEP.0b013e318208cb22
53. Philpott JF, Houghton K, Luke A. Physical activity recommendations for children with specific chronic health conditions: juvenile idiopathic arthritis, hemophilia, asthma, and cystic fibrosis. Clin J Sport Med. (2010) 20:167–72. doi: 10.1097/JSM.0b013e3181d2eddd
54. Miller SM, Peterson AR, Bernhardt DT. The preparticipation sports evaluation. Pediatr Rev. (2019) 40:108–28. doi: 10.1542/pir.32-5-e53
55. Sanders B, Blackburn TA, Boucher B. Clinical commentary preparticipation screening—the sports physical therapy perspective. Int J Sports Phys Ther. (2013) 8:180–93.23593556
56. Rice SG, American Academy of Pediatrics Council on Sports Medicine and Fitness. Medical conditions affecting sports participation. Medical conditions affecting sports participation. Pediatrics. (2008) 121:841–8. doi: 10.1542/peds.2008-0080
57. Cullen M. Developing a new specialty—sport and exercise medicine in the UK. J Sports Med. (2010) 1:11–4. doi: 10.2147/oajsm.s7627
58. Jayanthi N, Pinkham C, Dugas L, Patrick B, Labella C. Sports specialization in young athletes: evidence-based recommendations. Sports Health. (2013) 5:251–7. doi: 10.1177/1941738112464626
59. Tanne C, Pongas M. French preparticipation physical evaluation for children in 2020: what has changed? Arch Pediatr. (2020) 27:338–41. doi: 10.1016/j.arcped.2020.06.006
60. van Hattum JC, Verwijs SM, Rienks R, Bijsterveld NR, de Vries ST, Pinto YM, et al. The Netherlands sports cardiology map: a step towards sports cardiology network medicine for patient and athlete care. Neth Heart J. (2021) 29:129–34. doi: 10.1007/s12471-020-01530-x
61. Pruna R, Lizarraga A, Domínguez D. Medical assessment in athletes. Med Clin. (2018) 150:268–74. doi: 10.1016/j.medcli.2017.09.008
62. Pi-Rusinool R, María Sanz-de la Garza M, Grazioli G, García M, Sitges M, Drobnic F. Pre-participation medical evaluation in competitive athletes: the experience of an international multisport club. Apunts Sports Med. (2022) 57:100369. doi: 10.1016/j.apunsm.2021.100369
63. Fuller CM, McNulty CM, Spring DA, Arger KM, Bruce SS, Chryssos BE, et al. Prospective screening of 5,615 high school athletes for risk of sudden cardiac death. Med Sci Sports Exerc. (1997) 29:1131–8. doi: 10.1097/00005768-199709000-00003
64. Koester MC, Amundson CL. Preparticipation screening of high school athletes: are recommendations enough? Phys Sportsmed. (2003) 31:35–8. doi: 10.3810/psm.2003.08.460
65. Vessella T, Zorzi A, Merlo L, Pegoraro C, Giorgiano F, Trevisanato M, et al. The Italian preparticipation evaluation programme: diagnostic yield, rate of disqualification and cost analysis. Br J Sports Med. (2020 Feb) 54(4):231–7. doi: 10.1136/bjsports-2018-100293
66. Lehman PJ, Carl RL. The preparticipation physical evaluation. Pediatr Ann. (2017) 46:e85–92. doi: 10.3928/19382359-20170222-01
67. Conley KM, Bolin DJ, Carek PJ, Konin JG, Neal TL, Violette D. National athletic trainers’ association position statement: preparticipation physical examinations and disqualifying conditions. J Athl Train. (2014) 49:102–20. doi: 10.4085/1062-6050-48.6.05
68. Ljungqvist A, Jenoure P, Engebretsen L, Alonso JM, Bahr R, Clough A, et al. The international olympic committee (IOC) consensus statement on periodic health evaluation of elite athletes. Br J Sports Med. (2009) 43:631–43. doi: 10.1136/bjsm.2009.064394
69. Adami PE, Squeo MR, Quattrini FM, Di Paolo FM, Pisicchio C, Giacinto BD, et al. Pre-participation health evaluation in adolescent athletes competing at Youth Olympic Games: proposal for a tailored protocol. Br J Sports Med. (2019) 53:1111–6. doi: 10.1136/bjsports-2018-099651
70. Mayer F, Bonaventura K, Cassel M, Mueller S, Weber J, Scharhag-Rosenberger F, et al. Medical results of preparticipation examination in adolescent athletes. Br J Sports Med. (2012) 46:524–30. doi: 10.1136/bjsports-2011-090966
71. Solomon ML, Briskin SM, Sabatina N, Steinhoff JE. The pediatric endurance athlete. Curr Sports Med Rep. (2017) 16:428–34. doi: 10.1249/JSR.0000000000000428
72. Manore M, Barr S, Butterfield G. Nutrition and athletic performance: position of the American Dietetic Association, Dietitians of Canada, and the American College of Sports Medicine. J Am Diet Assoc. (2000) 100:1543–6. doi: 10.1016/j.jada.2009.01.005
73. Committee on Nutrition, Council on Sports Medicine and Fitness. Sports drinks and energy drinks for children and adolescents: are they appropriate? Pediatrics. (2011) 127:1182–9. doi: 10.1542/peds.2011-0965
74. Wattanapisit A, Wattanapisit S, Wongsiri S. Public health perspectives on eSports. Public Health Rep. (2020) 135(3):295–8. doi: 10.1177/0033354920912718
75. Rossoni A, Vecchiato M, Brugin E, Tranchita E, Adami PE, Bartesaghi M, et al. The eSports medicine: pre-participation screening and injuries management—an update. Sports (Basel). (2023) 11(2):34. doi: 10.3390/sports11020034
76. Rifat SF, Ruffin MT, Gorenflo DW. Disqualifying criteria in a preparticipation sports evaluation. J Fam Pract. (1995) 41(1):42–50.7798065
77. Pelliccia A, Adami PE, Quattrini F, Squeo MR, Caselli S, Verdile L, et al. Are Olympic athletes free from cardiovascular diseases? Systematic investigation in 2352 participants from Athens 2004 to Sochi 2014. Br J Sports Med. (2017) 51(4):238–43. doi: 10.1136/bjsports-2016-096961
78. Tofler IR, Grant J, Butterbaug GJ. Developmental overview of child and youth sports for the twenty-first century. Clin Sports Med. (2005) 24:783–804. doi: 10.1016/j.csm.2005.05.006
79. Maron BJ, Doerer JJ, Haas TS, Tierney DM, Mueller FO. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980–2006. Circulation. (2009) 119(8):1085–92. doi: 10.1161/CIRCULATIONAHA.108.804617
80. Van Camp SP, Bloor CM, Mueller FO, Cantu RC, Olson HG. Nontraumatic sports death in high school and college athletes. Med Sci Sport Exerc. (1995) 27(5):641–7. doi: 10.1249/00005768-199505000-00005
81. Raj SVS, Patel DR, Ramachandran L. Chronic kidney disease and sports participation by children and adolescents. Transl Pediatr. (2017) 6:207–14. doi: 10.21037/tp.2017.06.03
82. McCambridge TM, Benjamin HJ, Brenner JS, Cappetta CT, Demorest RA, Gregory AJM, et al. Athletic participation by children and adolescents who have systemic hypertension. Pediatrics. (2010) 125:1287–94. doi: 10.1542/peds.2010-0658
83. Harmon KG, Asif IM, Maleszewski JJ, Owens DS, Prutkin JM, Salerno JC, et al. Incidence, cause, and comparative frequency of sudden cardiac death in national collegiate athletic association athletes: a decade in review. Circulation. (2015) 132:1019. doi: 10.1161/CIRCULATIONAHA.115.015431
84. Corrado D, Basso C, Rizzoli G, Schiavon M, Thiene G. Does sports activity enhance the risk of sudden death in adolescents and young adults? J Am Coll Cardiol. (2003) 42:1959–63. doi: 10.1016/j.jacc.2003.03.002
85. Schwarzfischer P, Weber M, Gruszfeld D, Socha P, Luque V, Escribano J, et al. BMI and recommended levels of physical activity in school children. BMC Public Health. (2017) 24:595. doi: 10.1186/s12889-017-4492-4
86. de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. (2007) 85:660–7. doi: 10.2471/blt.07.043497
87. Zazryn TR, McCrory PR, Cameron PA. Injury rates and risk factors in competitive professional boxing. Clin J Sport Med. (2009) 19:20–5. doi: 10.1097/JSM.0b013e31818f1582
88. Steffen K, Engebretsen L. More data needed on injury risk among young elite athletes. Br J Sports Med. (2010) 44:485–9. doi: 10.1136/bjsm.2010.073833
89. Toivo K, Kannus P, Kokko S, Alanko L, Heinonen OJ, Korpelainen R, et al. Musculoskeletal examination in young athletes and non-athletes: the Finnish health promoting sports club (FHPSC) study. BMJ Open Sport Exerc Med. (2018) 4:e000376. doi: 10.1136/bmjsem-2018-000376
90. Garrick JG. Preparticipation orthopedic screening evaluation. Clin J Sport Med. (2004) 14:123–6. doi: 10.1097/00042752-200405000-00003
91. Paterno MV, Taylor-Haas JA, Myer GD, Hewett TE. Prevention of overuse sports injuries in the young athlete. Orthop Clin North Am. (2013) 44:553–64. doi: 10.1016/j.ocl.2013.06.009
92. Joy EA, Paisley TS, Price R, Rassner L, Thiese SM. Optimizing the collegiate preparticipation physical evaluation. Clin J Sport Med. (2004) 14:183–7. doi: 10.1097/00042752-200405000-00012
93. Boyajian-O'neill L, Cardone D, Dexter W, Difiori J, Bert Fields K, Jones D, et al. Determining clearance during the preparticipation evaluation. Physician Sportsmed. (2004) 32:29–41. doi: 10.1080/00913847.2004.11440756
94. Carek PJ, Mainous AG. A thorough yet efficient exam identifies most problems in school athletes. J Fam Pract. (2003) 52(2):127–34.12585990
95. Auvinen JP, Tammelin TH, Taimela SP, Zitting PJ, Mutanen PO, Karppinen JI. Musculoskeletal pains in relation to different sport and exercise activities in youth. Med Sci Sports Exerc. (2008) 40:1890–900. doi: 10.1249/MSS.0b013e31818047a2
96. Müller J, Müller S, Stoll J, Fröhlich K, Otto C, Mayer F. Back pain prevalence in adolescent athletes. Scand J Med Sci Sports. (2017) 27:448–54. doi: 10.1111/sms.12664
97. Shigematsu R, Katoh S, Suzuki K, Nakata Y, Sasai H. Sports specialization and sports-related injuries in Japanese school-aged children and adolescents: a retrospective descriptive study. Int J Environ Res Public Health. (2021) 18:7369. doi: 10.3390/ijerph18147369
98. American Medical Society for Sports Medicine. Physical examination videos. Available at: http://amssm.blogspot.com/p/videos.html. (Accessed November 20, 2022)
99. Coleman N, Beasley M, Briskin S, Chapman M, Cuff S, Demorest RA, et al. Musculoskeletal and sports medicine curriculum. Guidelines for pediatric residents. Curr Sports Med Rep. (2021) 20:218–28. doi: 10.1249/JSR.0000000000000830
100. McCrory P, Matser E, Cantu R, Ferrigno M. Sports neurology. Lancet Neurol. (2004) 3:345–440. doi: 10.1016/S1474-4422(04)00810-5
101. Conidi FX, Drogan O, Giza CC, Kutcher JS, Alessi AG, Crutchfield KE. Sports neurology topics in neurologic practice. A survey of AAN members. Neurol Clin Practice. (2014) 4:153–60. doi: 10.1212/01.CPJ.0000437697.63630.71
102. Zazryn TR, McCrory PR, Cameron PA. Neurologic injuries in boxing and other combat sports. Phys Med Rehabil Clin N Am. (2009) 20:227–39. doi: 10.1016/j.pmr.2008.10.004
103. Koon G, Atay O, Lapsia S. Gastrointestinal considerations related to youth sports and the young athlete. Transl Pediatr. (2017) 6:129–36. doi: 10.21037/tp.2017.03.10
104. Bi L, Triadafilopoulos G. Exercise and gastrointestinal function and disease: an evidence-based review of risks and benefits. Clin Gastroenterol Hepatol. (2003) 1:345–55. doi: 10.1053/s1542-3565(03)00178-2
105. Berzigotti A, Saran U, Dufour JF. Physical activity and liver diseases. Hepatology. (2016) 63:1026–40. doi: 10.1002/hep.28132
106. de Oliveira EP. Runner’s diarrhea: what is it, what causes it, and how can it be prevented? Curr Opin Gastroenterol. (2017) 33:41–6. doi: 10.1097/MOG.0000000000000322
107. Smart NA, Williams AD, Levinger I, Selig S, Howden E, Coombes JS, et al. Exercise and Sports Science Australia (ESSA) position statement on exercise and chronic kidney disease. J Sci Med Sport. (2013) 16:406–11. doi: 10.1016/j.jsams.2013.01.005
108. Martínez-Majolero V, Urosa B, Hernández-Sánchez S. Physical exercise in people with chronic kidney disease—practices and perception of the knowledge of health professionals and physical activity and sport science professionals about their prescription. Int J Environ Res Public Health. (2022) 19:656. doi: 10.3390/ijerph19020656
109. Baker LA, March DS, Wilkinson TJ, Billany RE, Bishop NC, Castle EM, et al. Clinical practice guideline exercise and lifestyle in chronic kidney disease. BMC Nephrol. (2022) 23:75. doi: 10.1186/s12882-021-02618-1
110. Bartlett A, Williams R, Hilton M. Splenic rupture in infectious mononucleosis: a systematic review of published case reports. Injury. (2016) 47:531–8. doi: 10.1016/j.injury.2015.10.071
111. Corrado D, Pelliccia A, Bjørnstad HH, Vanhees L, Biffi A, Borjesson M, et al. Cardiovascular pre-participation screening of young competitive athletes for prevention of sudden death: proposal for a common European protocol. Consensus statement of the study group of sport cardiology of the working group of cardiac rehabilitation and exercise physiology and the working group of myocardial and pericardial diseases of the European society of cardiology. Eur Heart J. (2005) 26:516–24. doi: 10.1093/eurheartj/ehi108
112. Pieles GE, Oberhoffer R. The assessment of the paediatric athlete. J Cardiovasc Transl Res. (2020) 13:306–12. doi: 10.1007/s12265-020-10005-8
113. Behera SK, Pattnaik T, Luke A. Practical recommendations and perspectives on cardiac screening for healthy pediatric athletes. Curr Sports Med Rep. (2011) 10:90–8. doi: 10.1249/JSR.0b013e3182141c1e
114. Löllgen H, Löllgen R. Genetics, genetic testing and sports: aspects from sports cardiology. Life Sci Soc Policy. (2012) 8:32. doi: 10.1186/1746-5354-8-1-32
115. Decree of the Ministry of Health (18/02/1982). Rules for the health care of competitive sport activities, Italy.
116. Maron BJ, Thompson PD, Ackerman MJ, Balady G, Berger S, Cohen D, et al. American Heart Association Council on Nutrition, Physical Activity, and Metabolism. Recommendations and considerations related to preparticipation screening for cardiovascular abnormalities in competitive athletes: 2007 update: a scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism: endorsed by the American College of Cardiology Foundation. Circulation. (2007) 115:1643–55. doi: 10.1161/CIRCULATIONAHA.107.181423
117. Drezner JA, O'Connor FG, Harmon KG, Fields KB, Asplund CA, Asif IM, et al. AMSSM position statement on cardiovascular preparticipation screening in athletes: current evidence, knowledge gaps, recommendations and future directions. Clin J Sport Med. (2016) 26:347–61. doi: 10.1136/bjsports-2016-096781
118. Drezner JA, Sharma S, Baggish A, Papadakis M, Wilson MG, Prutkin JM, et al. International criteria for electrocardiographic interpretation in athletes: consensus statement. Br J Sports Med. (2017) 51:704–31. doi: 10.1136/bjsports-2016-097331
119. Löllgen H, Börjesson M, Cummiskey J, Bachl N, Debruyne A. The pre-participation examination in sports: EFSMA statement on ECG for pre-participation examination. Dtsch Z Sportmed. (2015) 66:151–5. doi: 10.5960/dzsm.2015.182
120. Panhuyzen-Goedkoop NM, Hoogsteen J. Preparticipation cardiovascular screening in young athletes in the Netherlands. Neth Heart J. (2005) 13:335–7. doi: 10.1136/bjsm.2009.064220
121. Bessem B, Groot FP, Nieuwland W. The Lausanne recommendations: a Dutch experience. Br J Sports Med. (2009) 43:708–15. doi: 10.1136/bjsm.2008.056929
122. Kreher JB. Diagnosis and prevention of overtraining syndrome: an opinion on education strategies. Open Access J Sports Med. (2016) 7:115. doi: 10.2147/OAJSM.S91657
123. Kelly AK, Hecht S. Council on sports medicine and fitness. The female athlete triad. Pediatrics. (2016) 138:138. doi: 10.1542/peds.2016-0922
124. Parmigiano TR, Zucchi EV, Araujo MP, Guindalini CS, Castro Rde A, Di Bella ZI, et al. Pre-participation gynecological evaluation of female athletes: a new proposal. Einstein (Sao Paulo). (2014) 12:459–66. doi: 10.1590/S1679-45082014AO3205
125. Nattiv A, De Souza MJ, Koltun KJ, Misra M, Kussman A, Williams NI, et al. The male athlete triad—a consensus statement from the female and male athlete triad coalition part 1: definition and scientific basis. Clin J Sport Med. (2021) 31:345–53. doi: 10.1097/JSM.0000000000000946
126. Fredericson M, Kussman A, Misra M, Barrack MT, De Souza MJ, Kraus E, et al. The male athlete triad—a consensus statement from the female and male athlete triad coalition part II: diagnosis, treatment, and return-to-play. Clin J Sport Med. (2021) 31:349–66. doi: 10.1097/JSM.0000000000000948
127. Mountjoy M, Sundgot-Borgen J, Burke L, Carter S, Constantini N, Lebrun C, et al. The IOC consensus statement: beyond the female athlete triad–relative energy deficiency in sport (RED-S). Br J Sports Med. (2014) 48:491–7. doi: 10.1136/bjsports-2014-093502
128. Mountjoy M, Sundgot-Borgen JK, Burke LM, Ackerman KE, Blauet C, Constantini N, et al. IOC consensus statement on relative energy deficiency in sport (RED-S): 2018 update. Br J Sports Med. (2018) 52:687–97. doi: 10.1136/bjsports-2018-099193
129. Deligiannis A, Björnstad H, Carre F, Heidbüchel H, Kouidi E, Panhuyzen-Goedkoop NM, et al. ESC Study Group of Sports Cardiology. ESC Study Group of Sports Cardiology position paper on adverse cardiovascular effects of doping in athletes. Eur J Cardiovasc Prev Rehabil. (2006) 13:687–94. doi: 10.1097/01.hjr.0000224482.95597.7a
130. International Standard for Therapeutic Use Exemptions (ISTUE). World Anti-Doping Agency (WADA). Guidelines for the 2021 International Standard for Therapeutic Use Exemptions (ISTUE) (2021). Available at: https://www.wada-ama.org/en/resources/world-anti-doping-program/guidelines-2021-international-standard-therapeutic-use. (Accessed November 21, 2022)
131. World Anti-Doping Agency (WADA). Available at: https://www.wada-ama.org/en/. (Accessed November 21, 2022)
132. Arrêté du 24 juillet 2017 fixant les caractéristiques de l'examen médical spécifique relatif à la délivrance du certificat médical de non-contre-indication à la pratique des disciplines sportives à contraintes particulière (2018) Available at: https://www.legifrance.gouv.fr/download/pdf?id=YIcwAEMdCyeuPKXrVNdEEmJt7k_q6rhfsY9gyk3jVGw=. (Accessed November 22, 2022)
133. McCrory P, Meeuwisse W, Dvorak J, Aubry M, Bailes J, Broglio S, et al. Consensus statement on concussion in sport—the 5th international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. (2017) 51:838–47. doi: 10.1136/bjsports-2017-097699
134. American Academy of Pediatrics. COVID-19 interim guidance: return to sports and physical activity. Available at: https://www.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/covid-19-interim-guidance-return-to-sports/. (Accessed November 22, 2022)
135. Bhatia RT, Marwaha S, Malhotra A, Iqbal Z, Hughes C, Börjesson M, et al. Exercise in the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) era: a question and answer session with the experts endorsed by the section of sports cardiology & exercise of the European association of preventive cardiology (EAPC). Eur J Prev Cardiol. (2020) 27:1242–51. doi: 10.1177/2047487320930596
136. Howard-Jones AR, Bowen AC, Danchin M, Koirala A, Sharma K, Yeoh DK, et al. COVID-19 in children: I. Epidemiology, prevention and indirect impacts. J Paediatr Child Health. (2022) 58:39–45. doi: 10.1111/jpc.15791
137. Sperotto F, Friedman KG, Son MBF, VanderPluym CJ, Newburger JW, Dionne A. Cardiac manifestations in SARS-CoV-2-associated multisystem inflammatory syndrome in children: a comprehensive review and proposed clinical approach. Eur J Pediatr. (2021) 180:307–22. doi: 10.1007/s00431-020-03766-6
138. Phelan D, Kim JH, Elliott MD, Wasfy MM, Cremer P, Johri AM, et al. Screening of potential cardiac involvement in competitive athletes recovering from COVID-19: an expert consensus statement. JACC Cardiovasc Imaging. (2020) 13:2635–52. doi: 10.1016/j.jcmg.2020.10.005
139. Löllgen H, Bachl N, Papadopoulou T, Shafik A, Holloway G, Vonbank K, et al. Recommendations for return to sport during the SARS-CoV-2 pandemic. BMJ Open Sport Exerc Med. (2020) 6:e000858. doi: 10.1136/bmjsem-2020-000858
140. Steinacker JM, Schellenberg J, Bloch W, Deibert P, Friedmann-Bette B, Grim C, et al. Recommendations for return-to-sport after COVID-19: expert consensus. Dtsch Z Sportmed. (2022) 73:127–36. doi: 10.5960/dzsm.2022.532
141. Elliott N, Martin R, Heron N, Elliott J, Grimstead D, Infographic BA. Graduated return to play guidance following COVID-19 infection. Br J Sports Med. (2020) 54:1174–5. doi: 10.1136/bjsports-2020-102637
142. Cafiero G, Passi F, Calo' Carducci FI, Gentili F, Giordano U, Perri C, et al.. Competitive sport after SARS-CoV-2 infection in children. Ital J Pediatr. (2021) 47(1):221. doi: doi: 10.1186/s13052-021-01166-6
143. Wilson MG, Hull JH, Rogers J, Pollock N, Dodd M, Haines J, et al. Cardiorespiratory considerations for return to-play in elite athletes after COVID-19 infection: a practical guide for sport and exercise medicine physicians. Br J Sports Med. (2020) 54:1157–61. doi: 10.1136/bjsports-2020-102710
144. Singer ME, Taub IB, Kaelber DC. Risk of myocarditis from COVID-19 infection in people under age 20: a population-based analysis. MedRxiv. Available at: https://pubmed.ncbi.nlm.nih.gov/34341797/. (Accessed November 23, 2022)
145. Martinez MW, Tucker AM, Bloom OJ, Green G, DiFiori JP, Solomon G, et al. Prevalence of inflammatory heart disease among professional athletes with prior COVID-19 infection who received systematic return-to-play cardiac screening. JAMA Cardiol. (2021) 6(7):745–52. doi: 10.1001/jamacardio.2021.0565
146. WHO. Living guidance for clinical management of COVID-19 (2021). Available at: https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-2 (Accessed April 26, 2022).
147. Caterisano A, Decker D, Snyder B, Feigenbaum M, Glass R, House P, et al. CSCCa and NSCA joint consensus guidelines for transition periods: safe return to training following inactivity. Strength Cond J. (2019) 14:1–23. doi: 10.1519/SSC.000000000000047
148. McGuine TA, Biese KM, Petrovska L, Hetzel SJ, Reardon C, Kliethermes S, et al. Mental health, physical activity, and quality of life of US adolescent athletes during COVID-19–related school closures and sport cancellations: a study of 13000 athletes. J Athl Train. (2021) 56:11–9. doi: 10.4085/1062-6050-0478.20
149. Hull JH, Loosemore M, Schwellnus M. Respiratory health in athletes: facing the COVID-19 challenge. Lancet Respir Med. (2020) 8:557–8. doi: 10.1016/S2213-2600(20)30175-2
150. Neunhaeuserer D, Niebauer J, Degano G, Baioccato V, Borjesson M, Casasco M, et al. Sports and exercise medicine in Europe and the advances in the last decade. Br J Sports Med. (2021) 55:1122–4. doi: 10.1136/bjsports-2021-103983
151. Tillett E, Haddad F. So you want to be … a sport and exercise medicine physician. Br J Hosp Med (Lond). (2009) 70:M176. doi: 10.12968/hmed.2009.70.Sup11.45073
Keywords: adolescents, children, physical evaluation, pre-participation, sport, young athlete
Citation: Turska-Kmieć A, Neunhaeuserer D, Mazur A, Dembiński Ł, del Torso S, Grossman Z, Barak S, Hadjipanayis A, Peregud-Pogorzelski J, Kostka T, Bugajski A, Huss G, Kowalczyk-Domagała M and Wyszyńska J (2023) Sport activities for children and adolescents: the Position of the European Academy of Paediatrics and the European Confederation of Primary Care Paediatricians 2023—Part 1. Pre-participation physical evaluation in young athletes. Front. Pediatr. 11:1125958. doi: 10.3389/fped.2023.1125958
Received: 16 December 2022; Accepted: 5 June 2023;
Published: 22 June 2023.
Edited by:
Steven Hirschfeld, Uniformed Services University of the Health Sciences, United StatesReviewed by:
Alan David Rogol, University of Virginia, United StatesDoina Anca Plesca, Carol Davila University of Medicine and Pharmacy, Romania
© 2023 Turska-Kmieć, Neunhaeuserer, Mazur, Dembiński, del Torso, Grossman, Barak, Hadjipanayis, Peregud-Pogorzelski, Kostka, Bugajski, Huss, Kowalczyk-Domagała and Wyszyńska. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Justyna Wyszyńska and5c3p5bnNrYUB1ci5lZHUucGw=
†ORCID Justyna Wyszyńska orcid.org/0000-0002-5786-6214
 Anna Turska-Kmieć1,2,3
Anna Turska-Kmieć1,2,3 Daniel Neunhaeuserer
Daniel Neunhaeuserer Łukasz Dembiński
Łukasz Dembiński Stefano del Torso
Stefano del Torso Zachi Grossman
Zachi Grossman Shimon Barak
Shimon Barak Adamos Hadjipanayis
Adamos Hadjipanayis Tomasz Kostka
Tomasz Kostka Gottfried Huss
Gottfried Huss Justyna Wyszyńska
Justyna Wyszyńska