- Department of Ophthalmology, Nanjing Tongren Hospital, School of Medicine, Southeast University, Nanjing, China
Aim: Inflammation is involved in the development of myopia. n-3 polyunsaturated fatty acids (n-3 PUFAs) have vasodilating and anti-inflammatory effects, which may be involved in controlling myopia. It is of great significance to explore the relationship between n-3 PUFA intakes and juvenile myopia in order to control and alleviate myopia among teenagers through dietary intervention.
Methods: Sociodemographic data, information of nutrient intakes, cotinine, PUFAs, and eye refractive status of 1,128 juveniles were extracted from the National Health and Nutrition Examination Survey (NHANES) database in this cross-sectional study. PUFAs contained total polyunsaturated fatty acid (TPFAs), alpha-linolenic acid, octadecatetraenoic acid, eicosapentaenoic acid (EPA), docosapentaenoic acid (DPA), and docosahexaenoic acid (DHA). Covariates were screened by comparison among groups of normal vision, low myopia, and high myopia. The association between n-3 PUFA intakes and the risk of juvenile myopia was evaluated using univariate and multivariate logistic regression analyses with odds ratios (ORs) and 95% confidence intervals (CIs).
Results: Among the juveniles, 788 (70.68%) had normal vision, 299 (25.80%) had low myopia, and 41 (3.52%) had high myopia. There were significant differences in average EPA and DHA intakes among the three groups, and mean DPA and DHA intakes in the normal vision group were lower than those in the low myopia group (P < 0.05). After adjustment for age, gender, TPFAs, and cotinine, a high dietary intake of EPA (≥11 mg/1,000 kcal) in juveniles seemed to be associated with the risk of high myopia (OR = 0.39, 95% CI: 0.18–0.85), while no significant associations were identified between n-3 PUFA intakes and the risk of low myopia.
Conclusion: A high dietary intake of EPA may be associated with a decreased risk of high myopia among juveniles. A further prospective study is needed to validate this observation.
Introduction
Myopia is a complex disease caused by genetic and environmental factors, which occurs in childhood and early adulthood, and has become a major cause of blindness (1). Myopia is a major public health issue worldwide and is expected to affect 49.8% of the global population in 2050, of which 20% could develop high myopia (2). Myopia-associated complications such as cataract, glaucoma, and retinal detachment can have serious impacts on juveniles and cause a great socioeconomic burden (3–5). Therefore, it is of great importance to explore effective interventions to prevent and alleviate juvenile myopia.
Dietary intervention may be an effective and safe way for the prevention and control of myopia in juveniles, in addition to pharmacological and optical tools. A recent study based on untargeted metabolomics showed that the amounts of serum fatty acid (FA) metabolites were reduced in myopic human subjects, and, in particular, the levels of serum docosahexaenoic acid (DHA) were significantly lower (6). These results indicated that FA metabolism may play a role in the occurrence and development of myopia. The effects of DHA and eicosapentaenoic acid (EPA) on promoting vascular smooth muscle cell relaxation and vasodilation have been identified to be associated with the inhibition of myopia development (7, 8). In the development of myopia, significant thinning of choroidal thickness and a decrease in choroidal blood perfusion are thought to cause local hypoxia in the retina and sclera, promoting axial elongation and subsequently accelerating myopia development (9–12). A study reported that EPA and its metabolites were associated with inhibition of choroidal thinning and myopia progression in mice (13). An in vitro experiment showed that DHA or EPA could antagonize hypoxia-induced myofibroblast trans-differentiation in cultured human scleral fibroblasts (2). In addition, oral n-3 polyunsaturated fatty acid (n-3 PUFA) supplementation partially alleviated choroidal blood perfusion induced by near work in human subjects (2). Herein, we speculated that higher dietary intakes of n-3 PUFAs may be protective against myopia.
The aim of this study was to explore the association between dietary intakes of n-3 PUFAs, including alpha-linolenic acid (ALA), octadecatetraenoic acid (SDA), EPA, docosapentaenoic acid (DPA), and DHA, and the risk of juvenile myopia to provide some dietary references for the clinical prevention and treatment of juvenile myopia.
Methods
Study design and population
Data for this cross-sectional study were extracted from the National Health and Nutrition Examination Survey (NHANES) database, a representative survey research program to assess the health and nutritional status of adults in the United States of America. Regular data collection of the NHANES is carried out on approximately 5,000 persons from 15 areas since 1999 and examined in 2-year periods. The NHANES is a multistage stratified sampling database, and our statistical analyses were based on a public link address (https://wwwn.cdc.gov/nchs/nhanes/). Permission was obtained to use the data in this study: https://www.cdc.gov/nchs/data_access/restrictions.htm.
A total of 2,011 juveniles aged 12–19 years who underwent refraction measurements were initially included. Information on their n-3 PUFA and energy intakes was obtained. Participants without information on refraction measurements, FAs, cotinine, energy intake, and history of eye surgery were excluded. Since the NHANES survey protocol was approved by the Ethics Review Board (ERB) of the National Center for Health Statistics (NCHS), data were de-identified, and informed consent was obtained from all participants; approval from our Institutional Review Board was not required for this study.
n-3 PUFA measurement and the definition of myopia
In the NHANES, the method modified by Lagerstedt et al. was used to determine FAs (14). A total of 30 dietary FAs were quantitated. In brief, hexane along with an internal standard solution were used for the total extraction and recovery of FA. The extract was derivatized to form pentafluorobenzyl esters and injected into a capillary gas chromatograph column. The lower limit of detection of EPA, DHA, and DPA was 0.79, 1.84, and 0.24 µmol/L, respectively. FAs were detected using an Agilent 7890 B gas chromatograph equipped with a flame ionization detector and an Agilent DB-WAX capillary column (30 m × 0.25 μm × 0.25 μm) (15). In this study, the intakes of total polyunsaturated fatty acids (TPFAs) and n-3 PUFAs including ALA (g), SDA (g), EPA (g), DPA (g), and DHA (g) were calculated as energy density (kcal) separately (mg/1,000 kcal).
The refractive status of the eye was objectively assessed by non-cycloplegic objective auto-refractor (Nidek ARK-760) measurements in the vision database. Recorded refractive errors (median of three repeated measures) were included in the analyses only if a confidence of at least 5 (ranging from 1 to 9) was achieved at the time of measurement. Spherical equivalent refractions (SERs, i.e., average of the refractions in two principal meridians) were calculated from the right eye data of all included juveniles. Given that no cycloplegic agent was used in measuring refractive errors, this more conservative definition of myopia was employed to avoid misclassification of myopia. In this study, myopia was defined as an SER value ≤−1.0 diopter (D), and high myopia was defined as an SER value ≤−5.0 D. Participants were divided into three groups: normal vision (SER > −1.0), low myopia (SER ≤ −1.0), and high myopia (SER ≤ −5.0 D) (16).
Covariates
Plasma PUFA levels may be influenced by gender, age, race, education level, family poverty impact ratio (PIR), activity, body mass index (BMI) (17, 18), prescription medication use, and dietary supplement use, which were considered potential confounders and adjusted for in this study (19). BMI was calculated as weight (kg) divided by the square of height (m2). Dietary nutrient and energy intakes were estimated from two 24-h dietary recall interviews by the United States Department of Agriculture (USDA) automated multiple-pass method (AMPM). The first interview was conducted in person, and a subsequent interview was conducted 3–10 days after the first one via a phone call. A dietary supplement questionnaire, as part of the NHANES household interview, was used to assess dietary supplements such as vitamins and minerals. The consumption frequency, duration, and dosage of each dietary supplement were recorded over the prior 30 days, which can be used to calculate the average daily intake of nutrients. The nutrient content of foods was determined by using the relevant Food and Nutrient Database for Dietary Studies (FNDDS) for each NHANES release.
Statistical analysis
The data in this study were weighted, so continuous data were expressed as mean and standard error (SE) in the large weighted sample. Analysis of variance (ANOVA) was used to reflect the differences between groups. Categorical data were represented as [N (%)], and the chi-square test was used to analyze the differences between groups. Univariate and multivariate logistic regression analyses were used to explore the association between n-3 PUFA intakes and the risk of juvenile myopia. Model 1 was a crude model, Model 2 was adjusted for age and sex, and Model 3 was adjusted for age, gender, TPFA, and cotinine. The evaluation indicators were odds ratios (ORs) and 95% confidence intervals (CIs). All statistical tests were two-sided. P < 0.05 was considered significant. Analyses were performed with SAS 9.4 (SAS Institute Inc., Cary, NC, United States). Multiple imputation and sensitivity analysis were performed on missing data, as shown in Supplementary Table S1.
Results
Characteristics of juveniles
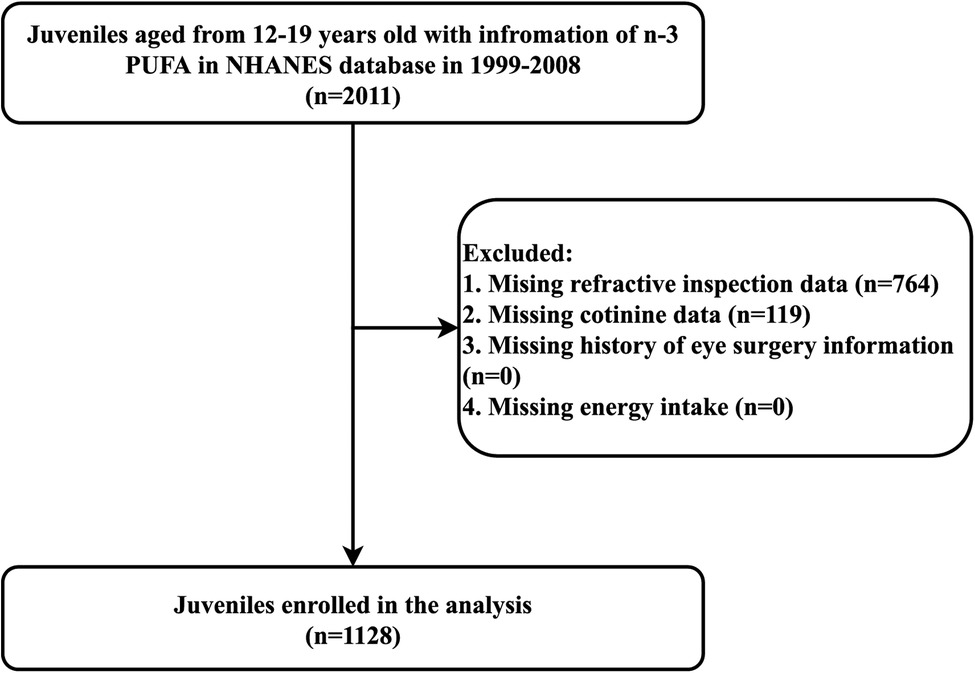
Figure 1 shows the flow chart of data screening. A total of 2,011 juveniles aged 12–19 years with information on n-3 PUFA intakes from the NHANES database between 1999 and 2008 were initially included. After excluding those with missing information on refraction measurements (n = 764) and cotinine (n = 119), 1,128 juveniles were finally eligible for this study.
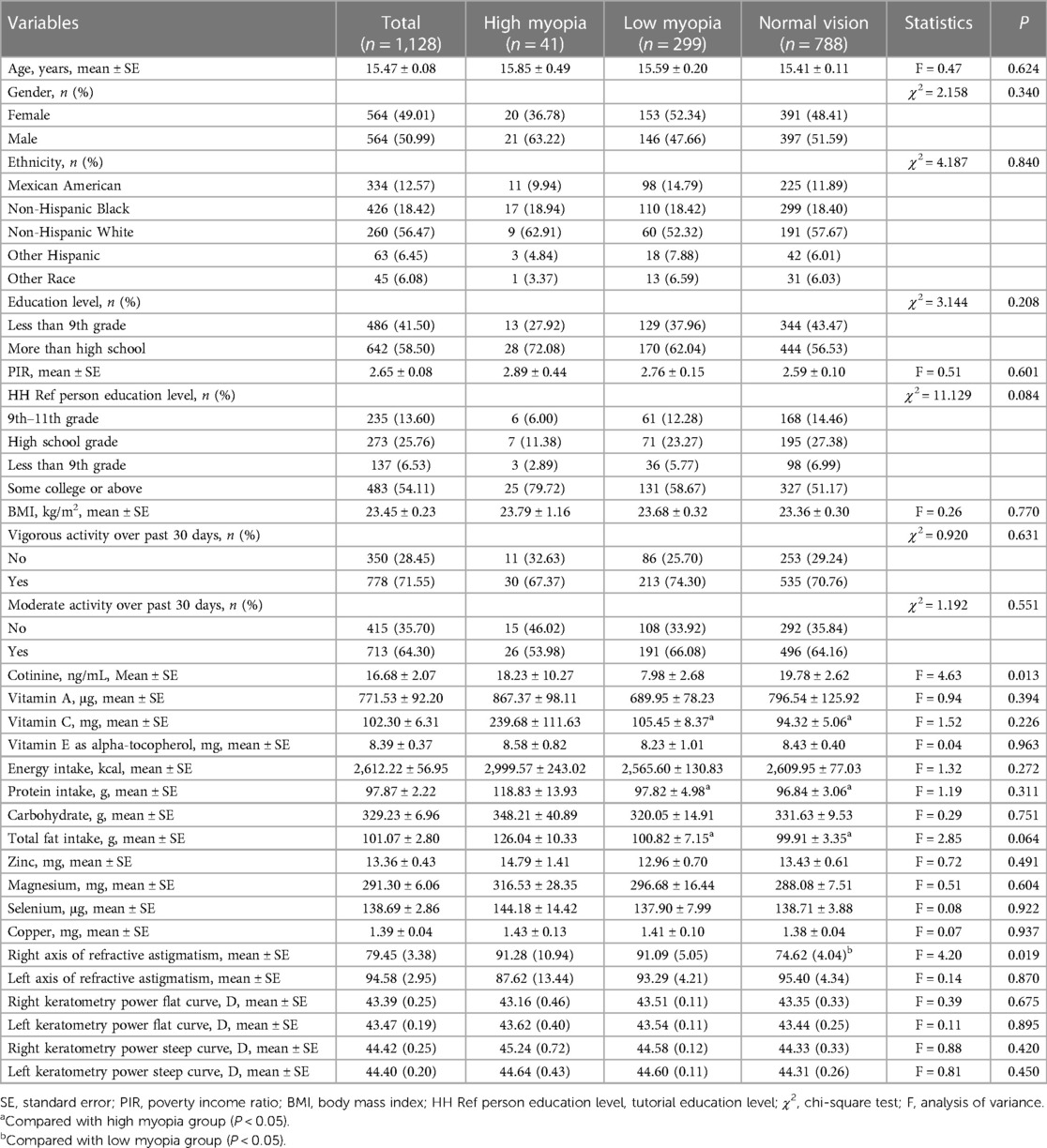
Table 1 shows the characteristics of juveniles with normal vision, low myopia, and high myopia. Among 1,128 juveniles, 788 (70.68%) had normal vision, 299 (25.80%) had low myopia, and 41 (3.52%) had high myopia. The average age of the participants was 15.47 ± 0.08 years, and the number of males and females was equal (both n = 564). There were significant differences in the average cotinine level and the axis of refractive astigmatism in right eyes among the normal vision, low myopia, and high myopia groups (all P < 0.05). Significant differences were observed in the intakes of vitamin C, protein, and total fat between the normal vision group and the high myopia group, and between the low myopia group and the high myopia group (all P < 0.05).
n-3 PUFA intakes among juveniles with normal vision, low myopia, and high myopia
Table 2 presents a comparison of n-3 PUFA intakes among the three groups. In the unprocessed data, the differences in EPA (P = 0.049) and DHA (P = 0.047) intakes were statistically significant among the normal vision, low myopia, and high myopia groups. Compared with juveniles with low myopia, those with normal vision consumed significantly less DPA (0.03 vs. 0.04 g) and DHA (0.16 ± 0.01 vs. 0.20 ± 0.03 g) intakes. Moreover, in terms of energy density, the mean intakes of EPA (P = 0.006) and DHA (P = 0.002) were also significantly different among the three groups. The average intakes of EPA (49.50 ± 7.06 vs. 21.65 ± 8.45 g) and DHA (88.73 ± 12.18 vs. 44.25 ± 10.47 g) in juveniles with low myopia were significantly higher than those in juveniles with high myopia. The intakes of DPA and DHA in juveniles with normal vision were lower than those in juveniles with low myopia (P < 0.05).
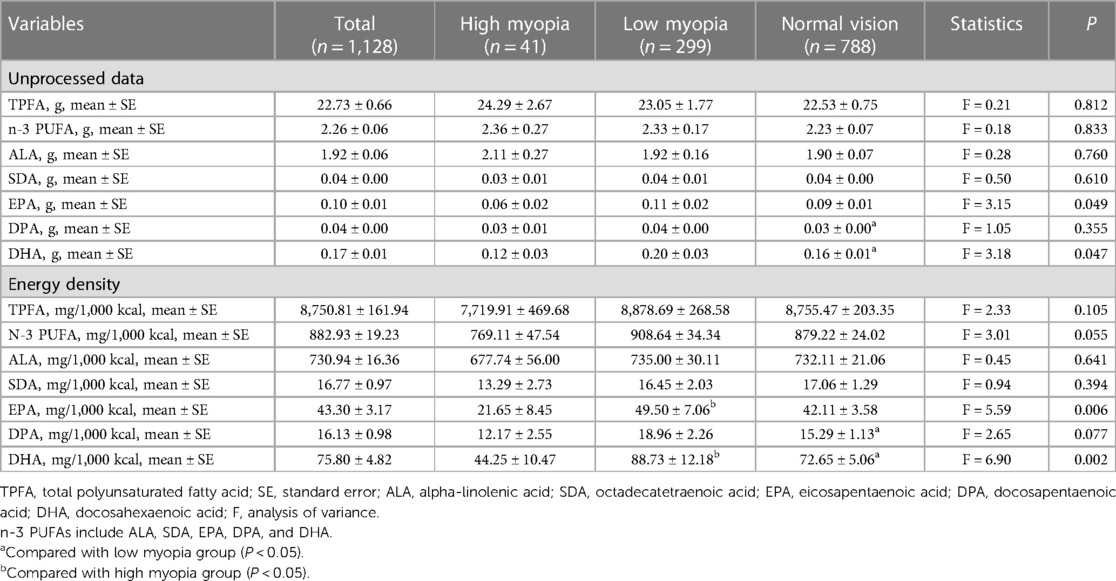
Table 2. Comparison for n-3 PUFA intake among juveniles with normal vision, low myopia, and high myopia.
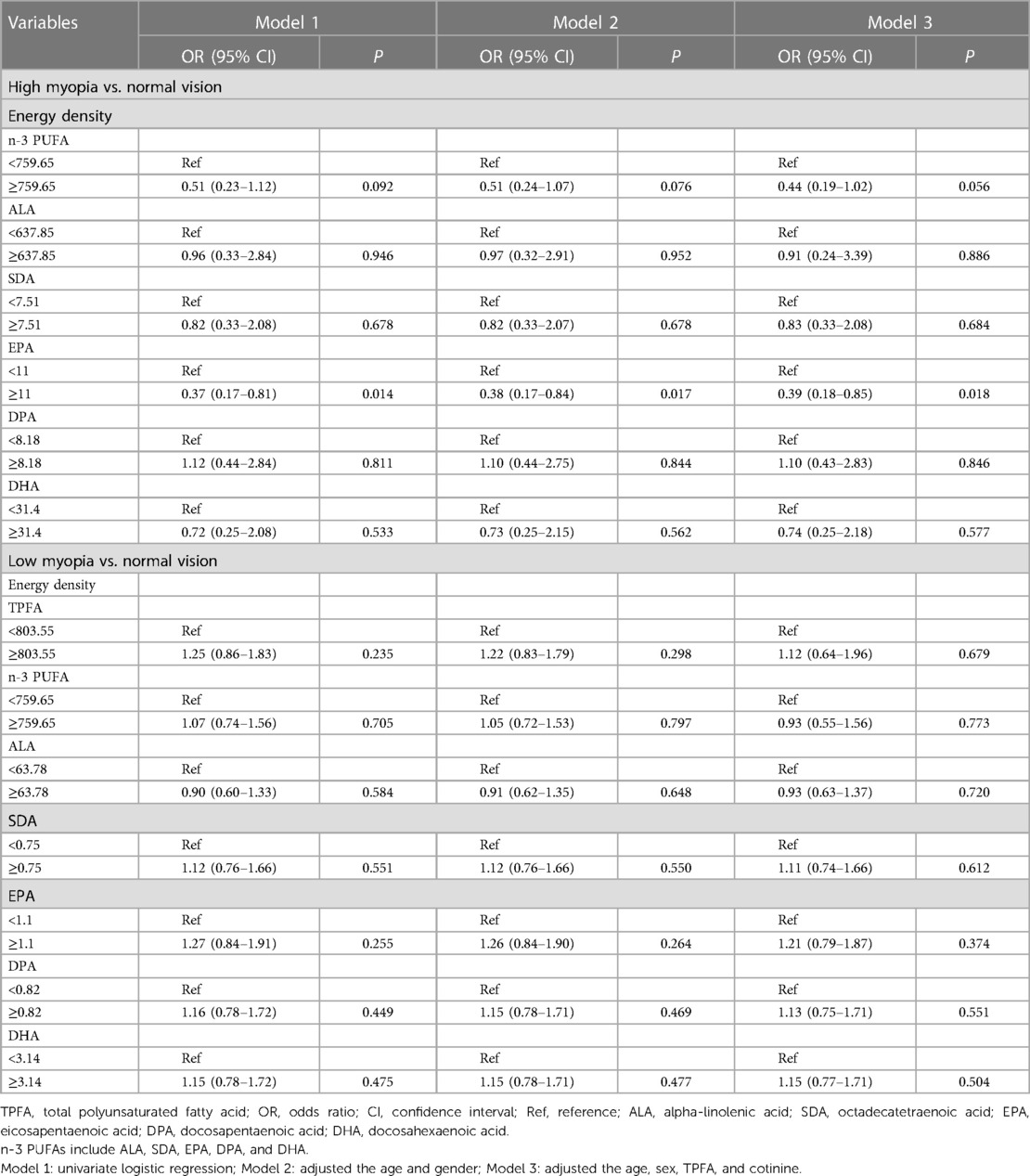
Association between n-3 PUFA intakes and the risk of juvenile myopia
Table 3 shows the association between the intakes of n-3 PUFAs (calculated by energy density) and the risk of juvenile myopia. After adjustment for covariates including age, gender, TPFA, and cotinine, a high dietary intake of EPA (≥11 mg/1,000 kcal) seemed to be associated with a decreased risk of high myopia (OR = 0.39, 95% CI: 0.18–0.85) in juveniles. However, no significant association was found between n-3 PUFA intakes and the risk of low myopia. Additionally, the intake of EPA ≥11 mg/1,000 kcal was not associated with the risk of low myopia (OR = 1.21, 95% CI: 0.79–1.87, P = 0.374).
Discussion
This study explored the association between n-3 PUFA intakes and the risk of juvenile myopia, and showed that a high dietary intake of EPA, calculated by energy density, was associated with a reduced risk of high myopia in juveniles. However, no association was found between n-3 PUFA intakes and the risk of low myopia.
Previous studies on myopia improvement with n-3 PUFAs were mostly conducted based on experimental animal models, and few have been explored in humans. Pan et al. (2) demonstrated that n-3 PUFAs, especially DHA, inhibited myopia development and that a decrease in choroidal blood perfusion induced by near work was partially alleviated by dietary n-3 PUFAs in human young adults. Ong et al. (20) found that n-3 oral nutritional supplements could improve visual acuity recovery after photorefractive keratectomy (PRK), suggesting that it may be a beneficial adjunct therapy for PRK patients. Similarly, the research study by Goyal et al. (21) demonstrated supplementation with n-3 FAs had a positive influence on tear secretion in patients undergoing laser in situ keratomileusis. In experimental animal myopia models (10, 12) and humans (22, 23), choroidal thickness and choroidal blood perfusion were significantly decreased, and these changes might subsequently trigger scleral hypoxia and subsequent myopia (11). n-3 PUFAs are essential for the synthesis of eicosanoids such as prostaglandins (PGs), prostacyclin (PGI), hydroperoxytetraenoic acid, hydroxyeicosatetraenoic acid, and lipoxins (24), which are involved in several physiological actions, including pro/anti-inflammatory response, pro/antiplatelet aggregatory response, vasodilation, vasoconstriction, immune response, and cell growth and proliferation, and metabolism imbalance could lead to several conditions. In addition, the vasodilating role of n-3 PUFAs in the cardiovascular system (25) and its neuroprotective capacity could also be observed in the retina and optic nerve (26, 27). The current study assumed that n-3 PUFAs may be involved in the relief of myopia through anti-inflammatory and choroid vasodilatation mechanisms.
The energy density of a food can be defined as the amount of metabolizable energy per unit weight of a food (kcal/g), derived from the macronutrient and moisture content of the food (28). As the most and least energy-dense nutrients, fat (9 kcal/g) and water (0 kcal/g) are the primary determinants of energy density (29). In the United Kingdom, children with myopia progression consumed more protein and lower fat and carbohydrate than children without progression (30). In Hong Kong, myopic children were more likely to report lower protein and fat intakes (31). We found that both protein and total fat intakes were lower in juveniles with normal vision and low myopia than those in juveniles with high myopia. However, Li et al. (32) found no significant association between specific nutrients or food groups and incident myopia, indicating that diet may not be associated with myopia in children (9 years old). The inconsistent results may be due to differences in the race, geography, and dietary habits of the study population. Prospective cohort studies are needed to further explore the effect of the nutrients on myopia in children.
Our findings showed that a high EPA intake (calculated by energy density) was associated with a reduced risk of high myopia in juveniles, but not with low myopia. A possible explanation is that the influence of diet and other environmental factors may be limited, as genetic factors may have a greater contribution to the early development of refractive errors (33). The diet of an infant at the age of 6 months consists mostly of formula or breast milk, and solid foods are gradually introduced from 6 to 12 months of age. The lack of variety in infant diets may result in limited variation in nutrient intakes, which may explain the observed negative findings (34). Moreover, a study suggested that metabolic changes in n-3 PUFAs occurred during the initial stages of myopia development, so early intervention targeting the PUFAs could ameliorate the onset and progression of myopia (2). Early intervention is particularly important because children who have developed myopia are continually exposed to myopic stimuli, such as increased near work, under which myopia is more likely to progress toward sight-threatening, high myopia (35). The retina has a complex and effective recycling system that ensures conservation of retinal DHA levels even in the presence of prolonged dietary n-3 PUFAs deficiency (36). In an animal model of form deprivation myopia (FDM), the levels of DHA and EPA were increased in the serum and the sclera, but decreased in the retina. DHA is abundant in the retina and plays an important role in the synthesis of disk membranes (37). It may be that a decrease in the serum DHA level enhances adaptation of the retina to metabolic stress. We hypothesized that the lack of significant improvement of n-3 PUFA supplementation in patients with low myopia may be due to the body's own metabolic compensatory mechanism, while sensitivity may be reduced in high myopia populations. In any case, the metabolism and function of n-3 PUFAs in high myopia are very complex. Further investigations are needed to probe into the role of n-3 PUFAs in myopia progression and identify the mechanism of action to lay a solid foundation for the treatment of human myopia.
The association between dietary n-3 PUFA intakes and the risk of myopia was explored in juveniles, which partially filled the gap in the relevant field and provided some references for the control of myopia by n-3 PUFA supplementation. However, there were some limitations in the study. This is a cross-sectional study, and the retrospective nature of the data makes it unable to reveal a causal association. The sample size for high myopia was small and modifiable confounders may have contributed to the negative results. The mechanism underlying the intake of these diets was unclear in the NHANES database, and further studies should take their effects on myopia into consideration. In addition, dietary intakes examined by the NHANES only reflected current dietary patterns, so prospective cohort studies are needed to investigate the association between long-term high n-3 PUFA intake and the risk of myopia in juveniles.
Conclusion
A high dietary intake of EPA may be associated with a decreased risk of high myopia among juveniles. Further prospective studies are needed to explore the impact of n-3 PUFAs on myopia risk reduction in order to relieve the social and economic burden and complications of myopia.
Data availability statement
Publicly available datasets were analyzed in this study. These data can be found here: NHANES database, https://wwwn.cdc.gov/nchs/nhanes/.
Ethics statement
The studies involving human participants were reviewed and approved by the National Center for Health Statistics of the US Centers for Disease Control and Prevention. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
ZZ and SL designed the study. ZZ wrote the manuscript. QY, XY, YL, KH, SX, NZ, and PZ collected, analyzed, and interpreted the data. SL critically reviewed, edited, and approved the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2023.1122773/full#supplementary-material.
References
1. Zhang P, Zhu H. Light signaling and myopia development: a review. Ophthalmol Ther. (2022) 11(3):939–57. doi: 10.1007/s40123-022-00490-2
2. Pan M, Zhao F, Xie B, Wu H, Zhang S, Ye C, et al. Dietary omega-3 polyunsaturated fatty acids are protective for myopia. Proc Natl Acad Sci U S A. (2021) 118(43):e2104689118. doi: 10.1073/pnas.2104689118
3. Sankaridurg P, Tahhan N, Kandel H, Naduvilath T, Zou H, Frick KD, et al. IMI impact of myopia. Invest Ophthalmol Vis Sci. (2021) 62(5):2. doi: 10.1167/iovs.62.5.2
4. Chen H, Liao Y, Zhou W, Dong L, Wang W, Wang X. The change of myopic prevalence in children and adolescents before and after COVID-19 pandemic in Suqian, China. PLoS One. (2022) 17(3):e0262166. doi: 10.1371/journal.pone.0262166
5. Yue Y, Liu X, Yi S, Liu B, Yi H, Li H. High prevalence of myopia and low hyperopia reserve in 4411 Chinese primary school students and associated risk factors. BMC Ophthalmol. (2022) 22(1):212. doi: 10.1186/s12886-022-02436-5
6. Du B, Jin N, Zhu X, Lu D, Jin C, Li Z, et al. A prospective study of serum metabolomic and lipidomic changes in myopic children and adolescents. Exp Eye Res. (2020) 199:108182. doi: 10.1016/j.exer.2020.108182
7. Limbu R, Cottrell GS, McNeish AJ. Characterisation of the vasodilation effects of DHA and EPA, n-3 PUFAs (fish oils), in rat aorta and mesenteric resistance arteries. PLoS One. (2018) 13(2):e0192484. doi: 10.1371/journal.pone.0192484
8. Zehr KR, Walker MK. Omega-3 polyunsaturated fatty acids improve endothelial function in humans at risk for atherosclerosis: a review. Prostaglandins Other Lipid Mediat. (2018) 134:131–40. doi: 10.1016/j.prostaglandins.2017.07.005
9. Wu H, Chen W, Zhao F, Zhou Q, Reinach PS, Deng L, et al. Scleral hypoxia is a target for myopia control. Proc Natl Acad Sci U S A. (2018) 115(30):E7091–100. doi: 10.1073/pnas.1721443115
10. Zhang S, Zhang G, Zhou X, Xu R, Wang S, Guan Z, et al. Changes in choroidal thickness and choroidal blood perfusion in Guinea pig myopia. Invest Ophthalmol Vis Sci. (2019) 60(8):3074–83. doi: 10.1167/iovs.18-26397
11. Zhao F, Zhang D, Zhou Q, Zhao F, He M, Yang Z, et al. Scleral HIF-1α is a prominent regulatory candidate for genetic and environmental interactions in human myopia pathogenesis. EBioMedicine. (2020) 57:102878. doi: 10.1016/j.ebiom.2020.102878
12. Zhou X, Zhang S, Zhang G, Chen Y, Lei Y, Xiang J, et al. Increased choroidal blood perfusion can inhibit form deprivation myopia in guinea pigs. Invest Ophthalmol Vis Sci. (2020) 61(13):25. doi: 10.1167/iovs.61.13.25
13. Mori K, Kuroha S, Hou J, Jeong H, Ogawa M, Ikeda SI, et al. Lipidomic analysis revealed n-3 polyunsaturated fatty acids suppressed choroidal thinning and myopia progression in mice. FASEB J. (2022) 36(6):e22312. doi: 10.1096/fj.202101947R
14. Lagerstedt SA, Hinrichs DR, Batt SM, Magera MJ, Rinaldo P, McConnell JP. Quantitative determination of plasma c8-c26 total fatty acids for the biochemical diagnosis of nutritional and metabolic disorders. Mol Genet Metab. (2001) 2001(73):38–45. doi: 10.1006/mgme.2001.3170
15. Yoo D, Lim Y, Son Y, Rho H, Shin C, Ahn TB. Dietary intake and plasma levels of polyunsaturated fatty acids in early-stage Parkinson’s disease. Sci Rep. (2021) 11(1):12489. doi: 10.1038/s41598-021-92029-x
16. Zhang R, Dong L, Yang Q, Zhou W, Wu H, Li Y, et al. Screening for novel risk factors related to high myopia using machine learning. BMC Ophthalmol. (2022) 22(1):405. doi: 10.1186/s12886-022-02627-0
17. Fisk HL, Irvine M, Miles EA, Lietz G, Mathers JC, Packard CJ, et al. Association of oily fish intake, sex, age, BMI and APOE genotype with plasma long-chain n-3 fatty acid composition. Br J Nutr. (2018) 120(1):23–32. doi: 10.1017/S000711451800106X
18. de Groot RHM, Emmett R, Meyer BJ. Non-dietary factors associated with n-3 long-chain PUFA levels in humans—a systematic literature review. Br J Nutr. (2019) 121(7):793–808. doi: 10.1017/S0007114519000138
19. Shan Z, Rehm CD, Rogers G, Ruan M, Wang DD, Hu FB, et al. Trends in dietary carbohydrate, protein, and fat intake and diet quality among US adults, 1999–2016. JAMA. (2019) 322(12):1178–87. doi: 10.1001/jama.2019.13771
20. Ong NH, Purcell TL, Roch-Levecq AC, Wang D, Isidro MA, Bottos KM, et al. Epithelial healing and visual outcomes of patients using omega-3 oral nutritional supplements before and after photorefractive keratectomy: a pilot study. Cornea. (2013) 32(6):761–5. doi: 10.1097/ICO.0b013e31826905b3
21. Goyal P, Jain AK, Malhotra C. Oral omega-3 fatty acid supplementation for laser in situ keratomileusis-associated dry eye. Cornea. (2017) 36(2):169–75. doi: 10.1097/ICO.0000000000001108
22. Wang S, Wang Y, Gao X, Qian N, Zhuo Y. Choroidal thickness and high myopia: a cross-sectional study and meta-analysis. BMC Ophthalmol. (2015) 15:70. doi: 10.1186/s12886-015-0059-2
23. Yang YS, Koh JW. Choroidal blood flow change in eyes with high myopia. Korean J Ophthalmol. (2015) 29(5):309–14. doi: 10.3341/kjo.2015.29.5.309
24. Shahidi F, Miraliakbari H. Omega-3 (n-3) fatty acids in health and disease: part 1—cardiovascular disease and cancer. J Med Food. (2004) 7(4):387–401. doi: 10.1089/jmf.2004.7.387
25. Bercea CI, Cottrell GS, Tamagnini F, McNeish AJ. Omega-3 polyunsaturated fatty acids and hypertension: a review of vasodilatory mechanisms of docosahexaenoic acid and eicosapentaenoic acid. Br J Pharmacol. (2021) 178(4):860–77. doi: 10.1111/bph.15336
26. Garcia-Medina JJ, Rubio-Velazquez E, Foulquie-Moreno E, Casaroli-Marano RP, Pinazo-Duran MD, Zanon-Moreno V, et al. Update on the effects of antioxidants on diabetic retinopathy: in vitro experiments, animal studies and clinical trials. Antioxidants (Basel). (2020) 9(6):561. doi: 10.3390/antiox9060561
27. Walchuk C, Suh M. Nutrition and the aging retina: a comprehensive review of the relationship between nutrients and their role in age-related macular degeneration and retina disease prevention. Adv Food Nutr Res. (2020) 93:293–332. doi: 10.1016/bs.afnr.2020.04.003
28. Ello-Martin JA, Ledikwe JH, Rolls BJ. The influence of food portion size and energy density on energy intake: implications for weight management. Am J Clin Nutr. (2005) 82(1 Suppl):236S–41S. doi: 10.1093/ajcn/82.1.236S
29. Bazshahi E, Pourreza S, Imani H, Azadbakht L, Ebaditabar M, Davarzani S, et al. The association of dietary energy density and body composition components in a sample of Iranian adults. Front Nutr. (2021) 8:751148. doi: 10.3389/fnut.2021.751148
31. Edwards MH. Do variations in normal nutrition play a role in the development of myopia? Optom Vis Sci. (1996) 73(10):638–43. doi: 10.1097/00006324-199610000-00002
32. Li M, Tan CS, Foo LL, Sugianto R, Toh JY, Sun CH, et al. Dietary intake and associations with myopia in Singapore children. Ophthalmic Physiol Opt. (2021) 42(2):319–26. doi: 10.1111/opo.12929
33. Chua SY, Ikram MK, Tan CS, Lee YS, Ni Y, Shirong C, et al. Relative contribution of risk factors for early-onset myopia in young Asian children. Invest Ophthalmol Vis Sci. (2015) 56(13):8101–7. doi: 10.1167/iovs.15-16577
34. Chua SY, Sabanayagam C, Tan CS, Lim LS, Toh JY, Chong YS, et al. Diet and risk of myopia in three-year-old Singapore children: the GUSTO cohort. Clin Exp Optom. (2018) 101(5):692–9. doi: 10.1111/cxo.12677
35. Vongphanit J, Mitchell P, Wang JJ. Prevalence and progression of myopic retinopathy in an older population. Ophthalmology. (2002) 109(4):704–11. doi: 10.1016/s0161-6420(01)01024-7
36. Jeffrey BG, Weisinger HS, Neuringer M, Mitchell DC. The role of docosahexaenoic acid in retinal function. Lipids. (2001) 36(9):859–71. doi: 10.1007/s11745-001-0796-3
Keywords: n-3 PUFA, myopia, juvenile, NHANES, cross-sectional study
Citation: Zhou Z, Li S, Yang Q, Yang X, Liu Y, Hao K, Xu S, Zhao N and Zheng P (2023) Association of n-3 polyunsaturated fatty acid intakes with juvenile myopia: A cross-sectional study based on the NHANES database. Front. Pediatr. 11:1122773. doi: 10.3389/fped.2023.1122773
Received: 13 December 2022; Accepted: 27 March 2023;
Published: 17 April 2023.
Edited by:
Siti Nurliyana Abdullah, University of Brunei Darussalam, BruneiReviewed by:
Mohd Aziz Husni, Hospital Tengku Ampuan Afzan, MalaysiaNadir Ali, Royal Cornwall Hospital Trust, United Kingdom
© 2023 Zhou, Li, Yang, Yang, Liu, Hao, Xu, Zhao and Zheng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sizhen Li U2l6aGVubGlydG9uZ3JlbkBvdXRsb29rLmNvbQ==
Specialty Section: This article was submitted to Children and Health, a section of the journal Frontiers in Pediatrics
 Zixiu Zhou
Zixiu Zhou Sizhen Li
Sizhen Li