
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr., 08 June 2023
Sec. Pediatric Neurology
Volume 11 - 2023 | https://doi.org/10.3389/fped.2023.1117455
Objectives: To assess whether decreased regional cerebral oxygen saturation (rScO2) is associated with the emergence delirium (ED) following general anesthesia in the pediatric population.
Methods: A retrospective observational cohort study was conducted on 113 children (ASA I–III) aged 2–14 years who underwent selective surgery under general anesthesia between 2022-01 and 2022-04. Intraoperatively, the rScO2 was monitored using a cerebral oximeter. The Pediatric Anesthesia Emergence Delirium (PAED) score was used to evaluate the patients for ED.
Results: The incidence of ED was 31%. Low rScO2 was reported in 41.6% of patients, who had a higher incidence of ED (P < 0.001) than those who did not experience desaturation. Logistic regression analysis revealed that decreased rScO2 was significantly associated with incident ED events [odds ratio (OR), 10.77; 95% confidence interval, 3.31–35.05]. Children under 3 years of age had a higher incidence of ED after rScO2 desaturation during anesthesia compared to older children (OR, 14.17 vs. 4.64).
Conclusion: Intraoperative rScO2 desaturation significantly increased the incidence of ED following general anesthesia. Monitoring should be enhanced to improve the oxygen balance in vital organs to improve the quality and safety of anesthesia.
The occurrence of emergence delirium (ED) in children is related to emergence quality and medical care cost, and its prevalence varies widely in different studies, ranging up to 80% (1–3). ED is considered a type of behavioral disorder and a neurological complication that develops after general anesthesia in children and can involve hypoactive (i.e., lethargy and inattentiveness) or hyperactive (i.e., agitation and restlessness) signs, or a mixture. The most common ED risk factors are the presence of endotracheal intubation, preschool age, volatile anesthetics, ophthalmologic and otolaryngology surgical procedures, history of behavioral problems, negative behavior on induction, preoperative anxiety level, and postoperative pain (4). Studies on delirium among surgical patients have found that this brain organ dysfunction is independently associated with prolonged cognitive impairment, extended hospital stays, increased cost of care, and increased mortality (5–7). Previous studies have suggested that reduced regional cerebral oxygen saturation (rScO2) during surgery may also be clinically relevant to cognitive dysfunction (8, 9), and may contribute to the development of ED. Near-infrared spectroscopy (NIRS) allows real-time, noninvasive monitoring of rScO2 (10). Therefore, NIRS may help identify pediatric patients at risk for ED and alleviate brain desaturation during general anesthesia.
Intraoperative decreases in basal rScO2 values of 20% or more are harmful and are associated with postoperative cognitive dysfunction in adults (11). However, the level of brain function impairment due to intraoperative rScO2 reduction is unclear. According to studies, severe rScO2 reduction during non-cardiac surgery is rare compared with mid- or low-level rScO2 reduction in the pediatric population (12, 13). Previous studies demonstrated that even a decrease in rScO2 of less than 10% from baseline values might reflect high intraoperative bleeding or postoperative behavioral changes in children (12, 14). This is attributable to how the brains of children are immature, have different tolerance, and regulate hypoxia differently compared to adults. Thus, we defined rScO2 >10% below baseline values as regional cerebral oxygen desaturation.
The primary objective of this study was to assess whether a decline in rScO2 of >10% from baseline levels was correlated with an elevated incidence of ED in pediatric patients undergoing general anesthesia.
This retrospective observational study was performed at Beijing Children's Hospital, China. The use of fully anonymized cohort data for research purposes was approved by the Ethics Committee of Beijing Children's Hospital, Capital Medical University, National Center for Children's Health (2021-E-114-Y), without the need for informed consent. All data were anonymized for extraction and analysis.
We identified a cohort of children aged 2–14 years with rScO2 monitoring using NIRS during surgery under total intravenous general anesthesia between 2022 and 01-01 and 2022-04-30. Children with autism, developmental delay, cognitive impairment, or neurological or neuromuscular diseases were excluded.
Anesthesia was induced using propofol 2–3 mg·kg−1, sufentanil 0.3–0.5 mcg·kg−1, and cisatracurium 0.1 mg·kg−1 to facilitate endotracheal intubation. After tracheal intubation, an anesthesia machine was connected to control the breathing. Anesthesia was maintained using propofol (8–10 mg·kg−1·h−1) and remifentanil (0.3–0.4 mcg·kg−1·min−1), with the dose adjusted to the analgesic requirements (systolic blood pressure maintained within 20% of baseline values). Ibuprofen (10 mg·kg−1 i.v.) was administered intraoperatively for postoperative analgesia, and fentanyl was used as required during emergence. Mechanical ventilation was adjusted to maintain an end-tidal CO2 between 35 and 45 mmHg. Body temperature was monitored using a nasopharyngeal thermometer and was maintained between 36.5°C and 37.5°C using a warm air blanket.
The Pediatric Anesthesia Emergence Delirium (PAED) score was used to assess whether a child experienced delirium after general anesthesia (Supplementary Table S1). While the patients were undergoing recovery in the PACU, a measurement based on the PAED scale scores within 15 min following extubation. The restlessness and agitation appeared within 15 min, an assessment of the agitation and pain degree was started immediately. The onset of ED was defined as the first evaluation of each patient with a PAED score ≥10. The Pediatric Anesthesia Behavior (PAB) score was used to evaluate children's behavior and mood before the induction of anesthesia (Supplementary Table S2).
Data were routinely collected using a standardized electronic anesthesia system (Docare, MedicalSystem Company). Information collected included demographic data (i.e., age, sex, and weight), PAB and PAED scores, rScO2 level, type of surgery, intraoperative hemorrhage, and anesthesia duration. Cerebral NIRS was performed using the FORE-SIGHT ELITE Cerebral Oxygen Saturation Monitor (NIRS, CAS Medical Systems Inc., Branford, CT, USA) with the medium bihemispheric sensors. When used with medium sensors, the module is indicated for use on pediatric subjects ≥3 kg. The sensor was placed bilaterally on the patient's forehead prior to the induction of anesthesia in operating room, and the rScO2 value was considered the baseline, for children who couldn't cooperate, we would use toys or animations to distract them and gain enough time to obtain the basal values; rScO2 values of the right and left frontal monitors were recorded simultaneously. The pooled value of rScO2 (mean value of the left and right sides) was used for analysis. Cerebral desaturation was defined as a decrease in rScO2 of ≥10% from the baseline for at least 3 min. Depending on the degree of decline of rScO2 compared to the baseline, we divided it into three levels and two groups: normal rScO2 group: decrease <10% (i.e., no desaturation); low rScO2 group: decrease of 10%–20% or >20%.
Histograms and the Kolmogorov–Smirnov test were used to assess normality. Continuous variables were expressed as the mean ± standard deviation or median (interquartile interval), as appropriate. To assess differences between the two groups, the t-test was used for normally distributed continuous variables, whereas the Wilcoxon rank-sum test was used for non-normally distributed continuous variables. For categorical variables, the χ2 test and Fisher's exact test were used. We further characterized associations between ED and rScO2 levels by logistic regression analyses adjusted for age, sex, weight, surgery type, PAB and PAED scores, hemorrhage, and anesthesia duration. We calculated the odds ratios (ORs) with 95% confidence intervals (CIs) for the risk of ED, progressively adjusted for the above variables. Statistical analyses were performed using the International Business Machines Statistical Package for the Social Sciences (SPSS) Statistics version 21.0 (SPSS Inc., Chicago, IL, USA) and GraphPad Prism 9.1 (GraphPad Software Company, San Diego, CA, USA). We selected a significance threshold of P < 0.05 for comparisons between groups.
The enrollment data and patient demographic characteristics of the 113 patients included in this study are summarized in Table 1. There were no statistically significant differences in age, sex, weight, and PAB scores between the two groups. The incidence of ED was 31.0% (35/113). Low rScO2 was reported in 41.6% (47/113) of patients who had higher PAED scores (P < 0.001) and with a higher incidence of ED (P < 0.001) than patients who did not experience desaturation during general anesthesia. In addition, patients in the low rScO2 group had greater bleeding and longer duration of anesthesia than those in the normal rScO2 group.
After adjusting for age, sex, and weight, the OR for ED was 7.88 (95% CI, 3.07–20.21) in patients with rScO2 desaturation compared with those with normal rScO2 during general anesthesia (Table 2). After progressive adjustment for various independent variables, decreased rScO2 remained significantly associated with incident ED events (OR, 10.77; 95% CI, 3.31–35.05). Logistic regression analyses with different levels of decreased rScO2 showed that patients with rScO2 decline of >20% had approximately 20 times higher odds of developing ED than patients with no rScO2 desaturation. This value was approximately seven-fold higher for rScO2 decline between 10% and 20%. Subgroup analysis by age (Figure 1) revealed a higher incidence of ED during the emergence period after experiencing rScO2 desaturation under anesthesia when patient was younger than 3 years old than in older children (OR, 14.17 vs. 4.64).
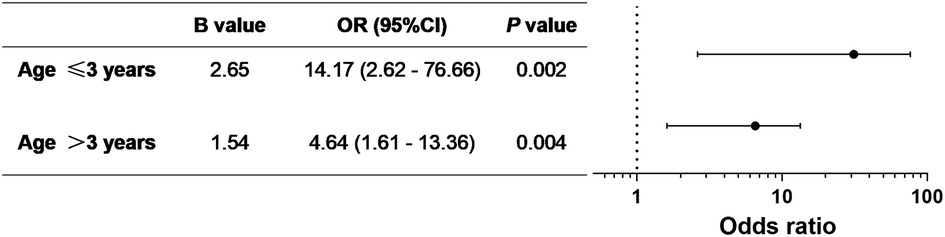
Figure 1. Logistic regression analysis of the association between rScO2 desaturation and ED in different age groups.
This study found that among children who received general anesthesia, a decrease in rScO2 of more than 10% from baseline was associated with ED. There is no standardized definition for pathological brain region desaturation (15, 16), specifically among children. The definition of hypoxia is based on a comparison of rScO2 with its own baseline. Children exhibit wide variations in baseline rScO2 because of comorbidities and their immature brains are more vulnerable to anesthetics (17). Our study was conducted on a heterogeneous population of children undergoing various operations, such as urologic, gastrointestinal, and orthopedic surgeries.
Cerebral perfusion index, systemic oxygenation, and cerebral metabolism, which may be influenced by anesthesia, can affect rScO2 values (18, 19). In addition, oxygen extraction from cerebral neurons affects rScO2 values; impaired extraction manifests as normal or increased rScO2 values. Our patients were less likely to suffer from impaired cerebral oxygen extraction because their underlying physical condition was generally good, while they maintained sufficient oxygen saturation (SpO2 > 98%) and adequate body temperature and hemodynamics during general anesthesia.
Cerebral NIRS measures cerebral oxygen saturation in the region under the forehead stickers. However, in children, this regional cerebral oxygen saturation may reflect the balance between the consumption and supply of oxygen of not only in a local area under the forehead but also in most of the brain due to a more immature self-regulating cerebral system (20, 21). This may explain why, in our study, a reduction in rScO2 of >10% of baseline was associated with increased odds of ED (OR 10.77), even if the reduction was less than the threshold of 20% commonly used in adults. This was consistent with Gómez-Pesquera et al. (14). The analysis of different levels of decreased rScO2 showed that pediatric patients whose rScO2 desaturation exceeded 20% of the baseline under general anesthesia had a higher risk of ED (OR 20.84 vs. 7.40). Of all patients in this study, only seven had rScO2 desaturation >20% below baseline; of these, five experienced ED. The more severe rScO2 desaturation, the higher incidence of ED. Therefore, when using intraoperative rScO2 monitoring in pediatric patients, the threshold criteria for rScO2 desaturation should be decreased, and the anesthesiologist must be alert when desaturation decreases by >10%.
Younger pediatric patients with immature brains might be more vulnerable to anesthetic effects (22–24). Thus, we stratified the data by age to determine differences in the impact of rScO2 desaturation on ED at different ages (Figure 1). In our cohort, rScO2 desaturation could lead to ED regardless of the patient's age; i.e., rScO2 desaturation was an independent risk factor for ED. Children younger than 3 years who experienced rScO2 desaturation during general anesthesia were at greater risk of ED than those older than 3 years. The younger the age, the more severe the effect of rScO2 desaturation.
This study had limitations. First, rScO2 monitoring was not a routine clinical practice at our institute. The number of cases included in the analysis was small, especially when a stratified analysis was performed. Therefore, the OR value for rScO2 desaturation ≥20% had a wider CI. Second, our study focused on the implications of decreased rScO2, and we did not analyze increases in rScO2 from the baseline, which are also related to cognitive deterioration. Third, we did not evaluate other factors that may influence the development of ED, such as intraoperative and postoperative pain; a future study on risk factor analysis might choose to include these factors.
In conclusion, a >10% decrease in rScO2 from baseline was associated with ED among children who received general anesthesia. Patients under 3 years old were more likely to develop ED after experiencing rScO2 desaturation under general anesthesia. Intraoperative monitoring should be strengthened to maintain the oxygen supply and demand balance of vital organs, reduce complications, improve the quality of anesthesia, and ensure patient safety.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
LL and ZG were responsible for study conception, data acquisition, the inclusion and exclusion of studies, data extraction, data analysis, and writing the manuscript. JZ was responsible for the inclusion and exclusion of studies, data extraction, and writing the manuscript. FZ and FW were responsible for data acquisition, supervision, and review of the manuscript for important intellectual content. XW and GL were responsible for checking the data of the outcomes, data analysis and interpretation, and drafting the article. All authors contributed to the article and approved the submitted version.
We would like to thank the medical officers and nurses of the Department of Anesthesiology, Beijing Children's Hospital, for their role in patient care during the study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. The reviewer CW declared a shared parent affiliation with the author(s) to the handling editor at time of review.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2023.1117455/full#supplementary-material
1. Gooden R, Tennant I, James B, Augier R, Crawford-Sykes A, Ehikhametalor K, et al. The incidence of emergence delirium and risk factors following sevoflurane use in pediatric patients for day case surgery, Kingston, Jamaica. Rev Bras Anestesiol. (2014) 64(6):413–8. doi: 10.1016/j.bjan.2013.09.011
2. Chandler JR, Myers D, Mehta D, Whyte E, Groberman MK, Montgomery CJ, et al. Emergence delirium in children: a randomized trial to compare total intravenous anesthesia with propofol and remifentanil to inhalational sevoflurane anesthesia. Paediatr Anaesth. (2013) 23(4):309–15. doi: 10.1111/pan.12090
3. Tsiotou AG, Malisiova A, Kouptsova E, Mavri M, Anagnostopoulou M, Kalliardou E. Dexmedetomidine for the reduction of emergence delirium in children undergoing tonsillectomy with propofol anesthesia: a double-blind, randomized study. Paediatr Anaesth. (2018) 28(7):632–8. doi: 10.1111/pan.13397
4. Gao Z, Zhang J, Nie X, Cui X. Effectiveness of intravenous ibuprofen on emergence agitation in children undergoing tonsillectomy with propofol and remifentanil anesthesia: a randomized controlled trial. J Pain Res. (2022) 15:1401–10. doi: 10.2147/JPR.S363110
5. Saczynski JS, Marcantonio ER, Quach L, Fong TG, Gross A, Inouye SK, et al. Cognitive trajectories after postoperative delirium. N Engl J Med. (2012) 367(1):30–9. doi: 10.1056/NEJMoa1112923
6. Ely EW, Shintani A, Truman B, Speroff T, Gordon SM, Harrell FE, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. J Am Med Assoc. (2004) 291(14):1753–62. doi: 10.1001/jama.291.14.1753
7. Girard TD, Jackson JC, Pandharipande PP, Pun BT, Thompson JL, Shintani AK, et al. Delirium as a predictor of long-term cognitive impairment in survivors of critical illness. Crit Care Med. (2010) 38(7):1513–20. doi: 10.1097/CCM.0b013e3181e47be1
8. Murkin JM. Cerebral oximetry: monitoring the brain as the index organ. Anesthesiology. (2011) 114(1):12–3. doi: 10.1097/ALN.0b013e3181fef5d2
9. Yu Y, Zhang K, Zhang L, Zong H, Meng L, Han R. Cerebral near-infrared spectroscopy (NIRS) for perioperative monitoring of brain oxygenation in children and adults. Cochrane Database Syst Rev. (2018) 1(1):CD010947. doi: 10.1002/14651858.CD010947.pub2
10. Scheeren T, Kuizenga MH, Maurer H, Struys M, Heringlake M. Electroencephalography and brain oxygenation monitoring in the perioperative period. Anesth Analg. (2019) 128(2):265–77. doi: 10.1213/ANE.0000000000002812
11. Ghosh A, Elwell C, Smith M. Review article: cerebral near-infrared spectroscopy in adults: a work in progress. Anesth Analg. (2012) 115(6):1373–83. doi: 10.1213/ANE.0b013e31826dd6a6
12. Liu L, Qiang Z, Zhang J, Ren Y, Zhao X, Fu W, et al. Effect of hemoglobin content on cerebral oxygen saturation during surgery for scoliosis in pediatric patients. BMC Anesthesiol. (2021) 21(1):165. doi: 10.1186/s12871-021-01382-x
13. Olbrecht VA, Skowno J, Marchesini V, Ding L, Jiang Y, Ward CG, et al. An international, multicenter, observational study of cerebral oxygenation during infant and neonatal anesthesia. Anesthesiology. (2018) 128(1):85–96. doi: 10.1097/ALN.0000000000001920
14. Gómez-Pesquera E, Poves-Alvarez R, Martinez-Rafael B, Liu P, Alvarez J, Lorenzo-López M, et al. Cerebral oxygen saturation and negative postoperative behavioral changes in pediatric surgery: a prospective observational study. J Pediatr. (2019) 208:207–213.e1. doi: 10.1016/j.jpeds.2018.12.047
15. Conforti A, Giliberti P, Mondi V, Valfré L, Sgro S, Picardo S, et al. Near infrared spectroscopy: experience on esophageal atresia infants. J Pediatr Surg. (2014) 49(7):1064–8. doi: 10.1016/j.jpedsurg.2014.01.010
16. Moerman A, Wouters P. Near-infrared spectroscopy (NIRS) monitoring in contemporary anesthesia and critical care. Acta Anaesthesiol Belg. (2010) 61(4):185–94.21388077
17. Gao Z, Zhang J, Wang X, Yao M, Sun L, Ren Y, et al. A retrospective study of electroencephalography burst suppression in children undergoing general anesthesia. Pediatr Investig. (2021) 5(4):271–6. doi: 10.1002/ped4.12287
18. Razlevice I, Rugyte DC, Strumylaite L, Macas A. Assessment of risk factors for cerebral oxygen desaturation during neonatal and infant general anesthesia: an observational, prospective study. BMC Anesthesiol. (2016) 16(1):107. doi: 10.1186/s12871-016-0274-2
19. Guo JY, Fang JY, Xu SR, Wei M, Huang WQ. Effects of propofol versus sevoflurane on cerebral oxygenation and cognitive outcome in patients with impaired cerebral oxygenation. Ther Clin Risk Manag. (2016) 12:81–5. doi: 10.2147/TCRM.S97066
20. Vavilala MS, Lee LA, Lam AM. The lower limit of cerebral autoregulation in children during sevoflurane anesthesia. J Neurosurg Anesthesiol. (2003) 15(4):307–12. doi: 10.1097/00008506-200310000-00003
21. Jildenstål P, Widarsson Norbeck D, Snygg J, Ricksten SE, Lannemyr L. Cerebral autoregulation in infants during sevoflurane anesthesia for craniofacial surgery. Paediatr Anaesth. (2021) 31(5):563–9. doi: 10.1111/pan.14146
22. Tsukamoto M, Taura S, Yamanaka H, Hitosugi T, Kawakubo Y, Yokoyama T. Age-related effects of three inhalational anesthetics at one minimum alveolar concentration on electroencephalogram waveform. Aging Clin Exp Res. (2020) 32:1857–64. doi: 10.1007/s40520-019-01378-1
23. Cornelissen L, Kim SE, Purdon PL, Brown EN, Berde CB. Age-dependent electroencephalogram (EEG) patterns during sevoflurane general anesthesia in infants. Elife. (2015) 4:e06513. doi: 10.7554/eLife.06513
Keywords: emergence delirium, regional cerebral oxygen saturation, general anesthesia, children, desaturation
Citation: Li L, Gao Z, Zhang J, Zhang F, Wang F, Wang X and Li G (2023) Reduced regional cerebral oxygen saturation increases risk for emergence delirium in pediatric patients. Front. Pediatr. 11:1117455. doi: 10.3389/fped.2023.1117455
Received: 6 December 2022; Accepted: 25 May 2023;
Published: 8 June 2023.
Edited by:
Jo Madeleine Wilmshurst, University of Cape Town, South AfricaReviewed by:
Souhayl Dahmani, Assistance Publique Hopitaux De Paris, France© 2023 Li, Gao, Zhang, Zhang, Wang, Wang and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jianmin Zhang emhhbmdqaWFubWluQGJjaC5jb20uY24=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.