- 1Department of Anesthesiology, Suzhou Wujiang District Children’s Hospital, Suzhou, China
- 2Department of Anesthesiology, Children’s Hospital of Soochow University, Suzhou, China
Objective: To explore the effect of esketamine nasal drops on pain in children after tonsillectomy using low-temperature plasma ablation.
Methods: 76 children who underwent tonsillectomy between May 2020 and July 2021, were randomly divided into two groups of 38 cases each. Patients in the control group were treated with conventional medication, while those in the study group were treated with esketamine nasal drops, along with the routine drug treatment. Pain levels of children in the two groups were compared within 1–3 days post-surgery, and the pseudomembrane formation and shedding-off time and recovery time were statistically analyzed.
Results: The pain level of children in the study group was lower than that of the control group 1–3 days post-surgery. The pseudomembrane formation and shedding-off time and recovery time in the study group were shorter than in the control group (P < 0.05). There was no significant difference in the incidence of adverse reactions between the two groups, and there were no serious adverse reactions in the two groups (P > 0.05).
Conclusion: It is safe to use esketamine nasal drops in children after tonsillectomy using low temperature plasma ablation, and this is found to reduce pain and shorten the recovery time.
1. Introduction
Tonsillar hypertrophy is reported as the sensation of a foreign body in the throat, or difficulty when swallowing, and can block the throat leading to obstructed breathing (1, 2). In recent years, low temperature plasma ablation has been widely used in the field of otorhinolaryngology overseas (3). This technique can maintain the safety of local mucosal tissue structures, however, postoperative pain is common. The pain affects sleep, food intake, and daily activities of children, and is not conducive to postoperative recovery (4, 5). Esketamine has strong anesthetic and analgesic effects. However, most of the current studies on esketamine focus on the treatment of depression, and there are few studies on its analgesic effects. Based on this, we explored the effect of esketamine nasal drops on pain in children after tonsillitis using low-temperature plasma ablation, to provide reference for clinical observation. Details of the study are presented in the following sections.
2. Data and methods
2.1. General profile
With the approval of the Medical Ethics Committee of our hospital, 76 children with tonsillar hypertrophy who were admitted to our hospital from May 2020 to July 2021 were selected as the research participants and randomly divided into two groups of 38 patients each. There were 22 males and 16 females in the control group. Their ages ranged from 3 to 10 years old, with an average age of (6.28 ± 1.13) years; 23 cases had Grade II tonsils and 15 cases had Grade III tonsils. There were 23 males and 15 females in the study group. Their ages ranged from 3 to 11 years old, with an average age of (6.32 ± 1.11) years; 22 cases had Grade II tonsils and 16 cases had Grade III tonsils. The general data of the two groups were similar (P > 0.05).
2.2. Inclusion and exclusion criteria
(1) Inclusion criteria: ① Patients who underwent low-temperature plasma ablation; ② All children whose families signed the informed consent form voluntarily.
(2) Exclusion criteria: ① Patients with cognitive dysfunction; ② Patients with congenital diseases; ③ Patients with liver and kidney dysfunction; ④ Patients with psychiatric illnesses.
2.3. Methods
Tonsillectomy was performed using the US Low Temperature Plasma Surgery System (Smith & Nephew Co., Ltd., UK) and Evac 70° cutter head (using EIC5874-01, Evac 70° cutter head), with an energy level of 7.
Method: 10 min before induction of anesthesia, intravenous injection of esketamine 0.5 mg/kg and dexmedetomidine 1.0 μg/kg were diluted to 10 ml with 0.9% sodium chloride solution. Postoperative diet care was carried out. Half an hour later, the patient was allowed to have cold drinks such as iced milk and ice cream without impurities, which they were advised to swallow slowly to reduce the wound pain and bleeding. Three hours after surgery if there was no bleeding, the patients could eat liquid foods, such as milk, rice congee, soup, and the nursing personnel ensured that the temperature of the food was not too high, and was suitably warm or cold. Some types of fruit and fruit juice containing fruit acid may cause pain as they irritate the wound and this could affect the healing of the wound, hence, patients were advised to consume less of these or not to consume them directly.
2.3.1. Control group
Routine drug treatment—post-surgery, the anti-inflammatory drug cefdinir dispersible tablets (Tianjin Central Pharmaceutical Co., Ltd., GYZZ H20060980) were given orally at 15 mg/kg, three times a day (tid).
2.3.2. Study group
Along with routine drug treatment, patients of the study group were additionally treated with esketamine nasal drops: Esketamine hydrochloride from Jiangsu Hengrui Pharmaceutical Co., Ltd., GYZZ H20193336, 2 drops per nostril at a time, once in the morning and once in the evening daily.
2.4. Evaluation indices
We compared the pain severity between the two groups 1–3 days post-surgery using the Visual Analogue Scale/Score (VAS) (6) used for pain assessment. Facial makeup VAS (F-VAS) was based on the VAS with a number of cartoon expressions to make the rating more intuitive and visual, which was suitable for children over 3 years old. There are eleven grades in this scale, with scores from 0 to 10: 0 means no pain, and 10 means the highest pain. A score is selected from 0 to 10 based on how the patient is feeling as an indicator of the level of pain. A score of 1 to ≤3 indicates mild pain that the patient can tolerate. Scores ≥4–6 means that the patient's pain affects sleep but it can be endured. Scores 7–10 indicate severe pain that the patient is unable to bear. All data will be collected by specialized clinical staff. The pseudomembrane formation and shedding-off time and the recovery time were analyzed statistically. The pseudomembrane which has formed is a thin white pseudomembrane with clean surface grows in the wound of the tonsil fossa. The tonsil fossa wound should be evaluated every one hour after surgery by the direct observation of clinical personnel. If the pseudomembrane is cloudy and thickened or accompanied by significant bad breath, the wound may be infected. The criteria for recovery are determined by the subjective feelings of the patient, which means that the patient no longer has the discomfort of the surgical site, can live independently and normally, and can eat normally. The clinical staff followed up the children and their parents every day to inquire about the recovery condition and recorded it.
2.5. Statistical methods
SPSS 22.0 software was used to process the data with as the measurement data; the independent sample T test was used to analyze differences between groups and the paired sample t test was used for within groups. The data were expressed in percentage, and statistically significant differences were identified using χ2 test (P < 0.05).
3. Results
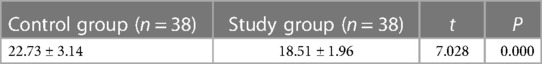
3.1. Pain levels of children in both groups 1–3 days post-surgery
The VAS pain scores 1 to 3 days post-surgery in the study group were lower than those in the control group, and the difference was statistically significant (P < 0.05) See Table 1.
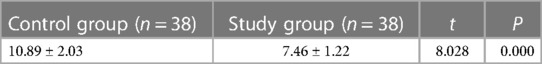
3.2. Formation time of wound pseudomembrane
The formation time of the wound pseudomembrane was shorter in the study group than that in the control group, and the difference was statistically significant (P < 0.05) See Table 2.
3.3. Shedding-off time of pseudomembrane
The shedding off time of pseudomembrane in the study group was shorter than that in the control group, and the difference was statistically significant (P < 0.05) See Table 3.
3.4. Recovery time
The recovery time in the study group was shorter than that in the control group, and the difference was statistically significant (P < 0.05) See Table 4.
3.5. Adverse reactions
One case of dizziness and one case of nausea and vomiting were reported in the control group, while two cases of dizziness and one case of nausea and vomiting were reported in the study group, and the difference was not statistically significant (P > 0.05). There were no serious adverse reactions in the two groups.
4. Discussion
There are two kinds of tonsillar hypertrophy—physiological hypertrophy and pathological hypertrophy. Most pathological tonsillar hypertrophy, and severe symptoms of physical tonsillar hypertrophy, such as frequent snoring during sleep in children, require surgical treatment. Tonsillectomy has a long history, and currently, the risks associated with surgery are steadily reducing with the continuous improvement of surgical methods and techniques from tonsillectomy to low-temperature plasma ablation. At present, the majority of children's tonsillectomy is performed by using some form of plasma methods as plasma surgery involves less bleeding, shorter operation time, and shorter time of general anesthesia for children, thus the postoperative recovery for children is relatively faster (7, 8).
Low-temperature plasma radiofrequency ablation involves tissue cutting at a relatively low temperature, about 40 °C–70 °C, and can achieve the purpose of hemostasis while cutting, thereby reducing the additional damage to the tissue by the high temperature, relieving the pain of patients and shortening the recovery time (9–15). This technique has been widely used in otorhinolaryngology surgery in China and overseas, and even in orthopedic and arthroscopic surgeries. At present, common otorhinolaryngology surgeries using low-temperature plasma radiofrequency ablation, including palatopharyngoplasty, tonsillectomy, adenoidectomy, epiglottic cyst resection, and vocal cord mass resection, have achieved good therapeutic effects (16–20).
Tonsillectomy is performed in the throat of children—there is intense postoperative pain and there is risk of respiratory tract obstruction. In clinical practice, cefdinir dispersible tablets are generally given orally, which are broad-spectrum antibiotics of cephalosporins and can be generally used for treating inflammation caused by various sensitive bacterial infections. The results of this study have shown that using esketamine nasal drops in children after tonsillitis using low-temperature plasma ablation, can improve pain symptoms and shorten the recovery time. As a novel N-methyl-D-aspartic acid (NMDA) receptor antagonist in the spinal cord, esketamine has a stronger affinity with NMDA receptors and μ opioid receptors clinically, and only half of the dose of ketamine is required to obtain a relatively satisfactory anesthesia effect. In addition, the clearance rate of esketamine is significantly higher than that of ketamine, and the incidence of adverse reactions is reduced. Dexmedetomidine has the effects of sedation and analgesia, anti-anxiety, and inhibition of salivary gland secretion, without significant inhibition on respiration (21, 22). Studies have shown that ketamine combined with dexmedetomidine can provide ideal anesthesia effects for pediatric bronchoscopy and percutaneous kidney puncture biopsy (23–25). Previous studies have confirmed that esketamine has a strong anesthetic effect, which can reduce the amount of analgesic used after surgery, prolong the duration of analgesia, and prevent hyperalgesia caused by opioids. However, the effect of using esketamine nasal drops for pain in children after tonsillitis using low temperature plasma ablation has not been reported yet. There are many methods of clinically administering esketamine. In this study, esketamine was used intranasally. The results showed that the pain in children in the study group was lower than that in the control group 1–3 days post-surgery. The postoperative wound surface pseudomembrane formation and shedding time and the recovery time of the study group were shorter than those of the control group.
In summary, the use of esketamine nasal drops in children after tonsillitis using low-temperature plasma ablation can improve pain symptoms and shorten the recovery time.
Data availability statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Children's Hospital of Soochow University Ethics Committee. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
Conception and design of the research: YL. Acquisition of data: QQ. Analysis and interpretation of the data: HL. Statistical analysis: HL. Writing of the manuscript: QQ. Critical revision of the manuscript for intellectual content: YL. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Zuo H, Niu Y, Zhang C, Huang J, Wang L, Du S. Clinical efficacy of low-temperature plasma ablation versus conventional tonsillectomy in China: a meta-analysis. J Clin Otolaryngol Head and Neck Surg. (2018) 32(4):10. doi: 10.13201/j.issn.1001-1781.2018.04.007
2. Baudouin R, Blumen M, Chaufton C, Chabolle F. Adult sleep apnea and tonsil hypertrophy: should pharyngoplasty be associated with tonsillectomy. Sleep and Breathing. (2019) 23(2):917–23. doi: 10.1007/s11325-019-01864-w
3. Sun B, Wang F, Yang S, Han Z, Han J, Shen Y, et al. Analysis of complications of low-temperature plasma assisted adenotonsil surgery in children. Clin J Otorhinolaryngol Head and Neck Surg. (2017) 31(22):4. doi: 10.13201/j.issn.1001-1781.2017.22.004
4. Li H, Li Y, Guo Z, Hao L, Li Y, Tang Y, et al. Low-temperature plasma radiofrequency ablation in phantom limb pain: a case report. Brain Circ. (2018) 4(2):62. doi: 10.4103/bc.bc_7_17
5. Long S, Zhao S, Huang M, Li Y, Lou X. Effect of low temperature plasma radiofrequency ablation under nasal endoscope on children with snoring complicated with allergic rhinitis. China Med Rev. (2019) 16(12):4. CNKI:SUN:YYCY.0.2019-12-024
6. Ren J, Wu Y, Wang W. Effect of postoperative pain on cognitive dysfunction in rats and its mechanism. Shandong Med. (2017) 57(36):3. doi: 10.3969/j.issn.1002-266X.2017.36.013
7. Qiu S, Liu D, Zhong J, Luo Q, Liu S. Chinese Journal of otorhinolaryngology head and neck surgery. Chinese Journal of Otorhinolaryngology Head and Neck Surgery. (2017) 52(2):2. doi: 10.3760/cma.j.issn.1673-0860.2017.02.010
8. Sarmento Castro J, Costa CC, Pereira H, Oliveira R, Santos P. Fiberoptic intubation in a child with previous unexpected difficult airway due to lingual tonsil hypertrophy. Revista Española de Anestesiología y Reanimación (English Edition). (2019) 66(9):478–82. doi: 10.1016/j.redar.2019.03.002
9. Guo Y, Li X, Liu J, Dou Z, Yang L, Pang H. Analysis of factors influencing the effect of low-temperature plasma ablation. China Med Rev. (2021) 18(4):4.
10. Zuo X, Chen J, Chen S, Otolaryngology DO. Clinical effect of low temperature plasma ablation under nasal endoscope in the treatment of nasal hemangioma. J Vasc and Endovasc Surg. (2019) 5(3):203–7.
11. Gu Y, Zhang Z, Huhe M, Shi S. Clinical evaluation of low-temperature plasma knife in adult tonsillectomy. Chongqing Med. (2017) 46(12):3. doi: 10.3969/j.issn.1671-8348.2017.12.035
12. Chen L, Department O. Therapeutic effect of low temperature plasma ablation on chronic hypertrophic rhinitis. China Continuing Med Edu. (2019) 11(5):77–9.
13. Chen FM. Therapeutic effect of low temperature plasma radiofrequency ablation on 42 children with snoring. China & Foreign Med Treat. (2019) 38(16):116–9.
14. Hao Y, Guo X. Effect of low-temperature plasma tonsillectomy and traditional tonsillectomy on chronic tonsillitis in adults. Shanxi Med J. (2019) 48(21):3. CNKI:SUN:SXYY.0.2019-21-035
15. Guo Y, Dou Z, Xiaolin LI, Tang Y, Yang L, Yan W. Efficacy of low temperature plasma ablation combined with epidural tube in discogenic low back pain. China Med Herald. (2018) 15(28):111–4.
16. Yang Z, Zhang X, Xin S, Dong J. Effect of low-temperature plasma ablation on tonsillectomy in children. Hebei Pharmaceutical Sci. (2021) 43(9):4.
17. Zhong L, Wen LH, Deng LB. Clinical effect of low-temperature plasma radiofrequency ablation on early laryngeal cancer and precancerous laryngeal lesions. Guangxi Med J. (2017) 39(10):1480–2.
18. Liu H, Gu Q, Gao B, Wang M, Xu J. Application of low-temperature plasma technique in the surgical treatment of giant tonsil in children. Chin J Integrated Traditional and Western Med Otolaryngol. (2020) 28(6):3. doi: 10.16542/j.cnki.issn.1007-4856.2020.06.015
19. Jing J, Li L, Zheng L, Wu Y, Jiang S, Zhang L, et al. Research on the efficacy of laryngendoscopic low-temperature plasma ablation on early glottic cancer. J BUON. (2020) 8(20):2382–8.
20. Jiang SM, Gong XC, Ding RL, Zheng J, Zheng S. Effects comparison of low temperature plasma radiofrequency ablation and CO_2 laser treatment on voice function of patients with laryngeal precancerous lesions. Chin J of General Pract. (2019) 17(06):966–8+973. doi: 10.16766/j.cnki.issn.1674-4152.000837
21. Chen Z, Xiao L, Wang H, Wang G. Research progress of new antidepressant ketamine. J Clin Psychiatry. (2019) 29(6):426–8. CNKI:SUN:LCJS.0.2019-06-024
22. Liu Y, Li X. Effects of esketamine combined with hydromorphone on postoperative analgesia and postpartum depression after cesarean section. Shandong Med. (2021) 61(19):84–7. doi: 10.3969/j.issn.1002-266X.2021.19.022
23. Lu H, Yu G, Guo Y, Yue C. Effects of esketamine on early postoperative pain and cognitive function in patients with benign bone tumors. J Xinxiang Med College. (2021) 38(6):516–9. doi: 10.7683/xxyxyxb.2021.06.004
24. Tao Y, Zeng Y, Peng L. Effect of microinfusion of low-dose esketamine on postpartum depression in cesarean delivery women. Front Med (Lausanne). (2021) 11(7):6–8.
Keywords: children, esketamine nasal drops, low temperature plasma ablation, tonsillar hypertrophy, tonsillectomy
Citation: Qian Q, Liu HX and Li YQ (2023) Effect of esketamine nasal drops on pain in children after tonsillectomy using low temperature plasma ablation. Front. Pediatr. 11:1110632. doi: 10.3389/fped.2023.1110632
Received: 5 January 2023; Accepted: 12 June 2023;
Published: 17 July 2023.
Edited by:
Antonino Morabito, University of Florence, ItalyReviewed by:
Zahoor Ahmad, Counties Manukau District Health Board, New ZealandLuca Leone, University of Florence, Italy
© 2023 Qian, Liu and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yue Qing Li bGl5dWVxaW5seThAb3V0bG9vay5jb20=
†These authors have contributed equally to this work
 Qiu Qian1,†
Qiu Qian1,† Yue Qing Li
Yue Qing Li