- Department of Pediatric Surgery, Guizhou Provincial People’s Hospital, Guizhou, China
Purpose: The aim of this study was to develop and validate a nomogram for predicting surgical intervention in pediatric intussusception after hydrostatic reduction.
Methods: Children with intussusception who had treated with sonographically guided saline hydrostatic reduction as an initial treatment were enrolled in this study. The enrolled patients were randomly selected for training and validation sets, and the split ratio was 7:3. The medical records of enrolled patients were retrospectively reviewed. The patients were divided into a surgery and a non-surgery group according to the results of the nonsurgical reduction. A model for predicting the risk of surgical treatment was virtualized by the nomogram using logistic regression analysis.
Results: The training set consisted of 139 patients and the validation set included 74. After logistic regression analysis using training set, duration of symptoms, bloody stools, white blood cells (WBCs), creatine kinase isoenzyme (CK-MB), long-axis diameter, poor prognostic signs by ultrasound and mental state were identified as the independent predictors of surgical intervention for intussusception. A model that incorporated the above independent predictors was developed and presented as a nomogram. The C-index of the nomogram in the validation set was 0.948 (95% CI, 0.888–1.000). The calibration curve demonstrated a good agreement between prediction and observation. The decision curve analysis (DCA) curve showed that the model achieved a net benefit across all threshold probabilities.
Conclusion: Based on the predictors of duration of symptoms, bloody stools, WBCs, CK-MB, long-axis diameter, poor prognostic signs by ultrasound and mental state, we developed a nomogram for predicting surgical intervention after hydrostatic reduction. This nomogram could be applied directly to facilitate pre-surgery decision for pediatric intussusception.
Introduction
Intussusception is the most common abdominal emergency in infants and toddlers, which is defined as the invagination of proximal bowel into the distal bowel (1, 2). The prevalence of intussusception is about 1–4 per 2000 infants and children, and the most common type is ileocolic intussusception (3). Early treatment is critical for intussusception in order to reduce the risk of secondary peritonitis, sepsis and bowel perforation (4).
Treatment modalities for intussusception include both non-surgery and surgery procedures. Pneumatic or hydrostatic reduction through anorectal enema is the main treatment of choice for the non-surgery procedure (5). Pneumatic reduction using air is very effective for intussusception treatment with advantages such as low cost and decreased risk of perforations (2). However, the use of the pneumatic reduction technique will increase the risk of exposure to radiation (6). Hydrostatic reduction using normal saline needs to be guided by ultrasound, which can avoid the radiation. Both of the 2 non-surgery techniques can be performed safely and exhibits high success rates (6). Currently, ultrasound-guided hydrostatic reduction has been suggested as the first choice for intussusception treatment in several studies, because it has a higher success rate, shorter hospital stay and no radiation risk comparing to pneumatic reduction (6–8). When non-surgery treatment is contraindicated or has failed, surgery procedures will be conducted.
Previously, risk factors for non-surgical intussusception reduction failure or predictors for surgery requirements have been investigated in several studies. For example, Khorana et al. (9) found that risk factors such as age, symptom duration, rectal bleeding and abdominal distension were closely associated with nonsurgical reduction failure. Wu et al. (10) identified that symptoms for at least 2 days before surgery and long intussusception were predictors for patients with intussusception at high risk of needing surgery. In addition, He and colleagues (11) found that sonographic features including the presence of peritoneal fluid and trapped fluid in the intussusception were the important risk factors for failure of hydrostatic intussusception reduction.
Although, the above works have contributed to the prediction of hydrostatic reduction failure, there is still lack of validated predictive tools. The aim of this study was to develop and validate a nomogram for predicting surgical intervention in pediatric intussusception after hydrostatic reduction.
Materials and methods
Patients
This retrospective study was approved by the Ethics Committee of Guizhou Provincial People's Hospital in accordance with the Declaration of Helsinki. Due to the nature of retrospective study, the informed consent was waived.
Inclusion criteria included the following: (1) all the patients enrolled were children below 7 years of age; (2) patients had a diagnosis of intussusception by a senior sonographer; (3) patients had treated with sonographically guided saline hydrostatic reduction as an initial treatment. Recurrent patients or patients with insufficient medical records were excluded from this study.
Data collection
The enrolled patients were randomly selected for training and validation sets, and the split ratio was 7:3. The training set was used to train the prediction model. The validation data were used to validate the model.
The medical records of enrolled patients were retrospectively reviewed. All the enrolled patients were treated with hydrostatic reduction as an initial treatment. If non-surgery treatment was failure, surgery procedures would be conducted. The patients were divided into a surgery and a non-surgery group according to the results of the nonsurgical reduction.
The data collected included clinical features (such as, age, gender, weight, temperature at admission, vomiting, bloody stools, abdominal mass, mental status, and duration of symptoms), ultrasonic image characteristics (such as long-axis diameter and location of the mass, enlarged lymph node, absence of blood flow in the intussusception, and fluid trapped within the intussusception), and laboratory tests [white blood cells (WBCs), platelets (PLTs), C-reaction protein (CRP), fibrinogen (FIB), and creatine kinase isoenzyme (CK-MB), serum kalium (K), serum sodium (Na), and serum chloride (Cl)]. The sonographic poor prognostic signs of hydrostatic reduction were defined if one of the following signs was presented: enlarged lymph node in intussusception, thick peripheral hypoechoic rim, fluid trapped within the intussusception, free intraperitoneum fluid and the absence of blood flow in the intussusception. When the child had somnolence, listlessness, no crying and pale face, it indicated that the child's mental state was poor.
Statistical analysis
The data in this study were analyzed by R4.0.3 software. There was no missing data for the final statistical analysis. On the basis of Harrell's guidelines (12), when the outcome is binary, the minimum value of the frequencies of the two response levels should be greater than 10 times the number of predictors. Our study included 73 patients with surgical reduction and 126 patients without surgical reduction. Thus the limiting sample size is 73, and based on Harrell's guidelines, no more than 7 predictors can be accommodated. The normal distribution of continuous variables was evaluated by using the Kolmogorov-Smirnov test. Continuous data with normal distribution were expressed as mean ± SD and compared by Student's t-test; data with a non-normal distribution were expressed by median with range and compared by Mann–Whitney U test. The qualitative data were expressed as percentages and compared by Chi-square or Fisher's exact tests. To assess independent predictors of surgical treatment for intussusception, a twostep approach was used. In the first step, the univariable analysis was done. Then, variables selected based on clinical and statistical grounds were included in a multivariable logistic regression model. The odds ratios (ORs) for surgical treatment were calculated by logistic regression analysis. A model for predicting the risk of surgical treatment was then virtualized by the nomogram based on these independent variables using the training set. The validation set was used to confirm the newly established nomogram. The concordance index (c-index) was used to evaluate the predictive accuracy of the model. Sensitivity and specificity were evaluated by receiver operating characteristics curve (ROC). Furthermore, the clinical value of the model was evaluated by decision curve analysis (DCA). A p-value < 0.05 was considered as statistically significant.
Results
Clinical characteristics
From July 2020 to February 2022, 210 patients with intussusception who had been treated with sonographically guided saline hydrostatic reduction as an initial treatment were screened in this study. Among them, 3 patients with age above 7 years old and 8 patients with insufficient medical records were excluded. Finally, a total of 199 patients who met the inclusion criteria were enrolled in this study. 139 patients were assigned to training set, while 60 patients were assigned to validation set. Surgical reduction was performed in 35.97% of cases (50/139) in training set and 38.33% of cases (23/60) in validation set, respectively. There were no significant differences between the two sets in surgical reduction (p = 0.751) or clinical characteristics. The comparative clinical characteristics among the training and validation sets are shown in Table 1.
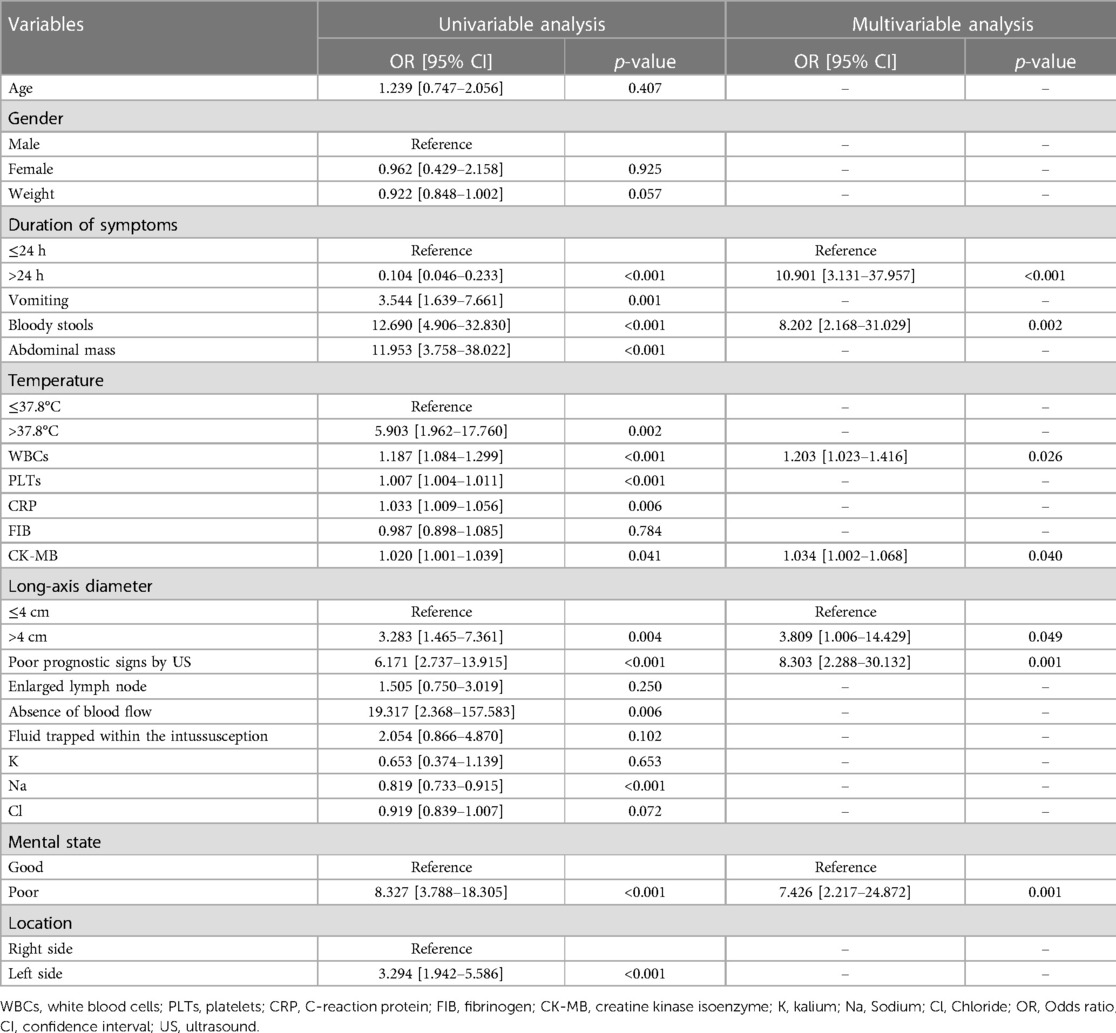
Development of the nomogram
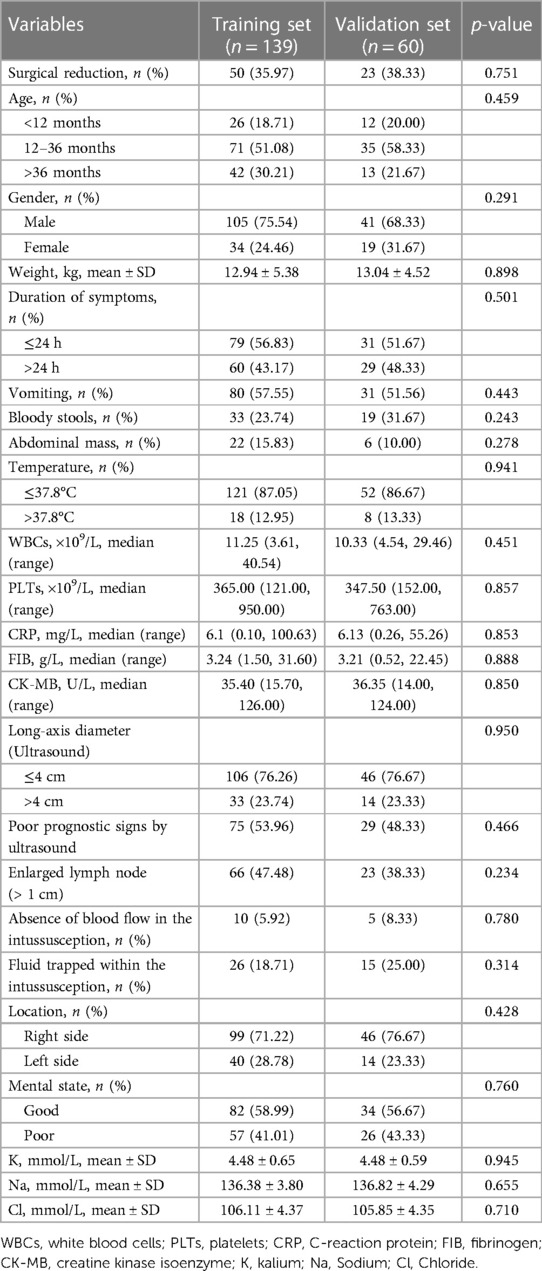
The univariable analysis using the training set showed that duration of symptoms (p < 0.001), vomiting (p = 0.001), bloody stools (p < 0.001), abdominal mass (p < 0.001), temperature (p = 0.002), WBCs (p < 0.001), PLTs (p < 0.001), CRP (p = 0.006), CK-MB (p = 0.041), long-axis diameter (p = 0.004), poor prognostic signs by ultrasound (p < 0.001), absence of blood flow in the intussusception (p = 0.006), serum Na (p < 0.001), mental state (p < 0.001) and intussusception location (p < 0.001) were the significant factors for surgical intervention of intussusception. These 15 clinical candidate predictors were selected for the multivariable analysis. After multivariable analysis was done, duration of symptoms (odds ratio [OR] = 10.901; 95% confidence interval [CI] = 3.131–37.957; p < 0.001), bloody stools (OR = 8.202; 95% CI = 2.168–31.029; p = 0.002), WBCs (OR = 1.203; 95% CI = 1.023–1.416; p = 0.026), CK-MB (OR = 1.034; 95% CI = 1.002–1.068; p = 0.040), long-axis diameter (OR = 3.809; 95% CI = 1.006–14.429; p = 0.049), poor prognostic signs by ultrasound (OR = 8.303; 95% CI = 2.288–30.132; p = 0.001), and mental state (OR = 7.426; 95% CI = 2.217–24.872; p = 0.001) were identified as the independent predictors of surgical intervention for intussusception. The results of the univariable and multivariable analyses are listed in Table 2. Then, a model that incorporated the above independent predictors was developed and presented as a nomogram (Figure 1).
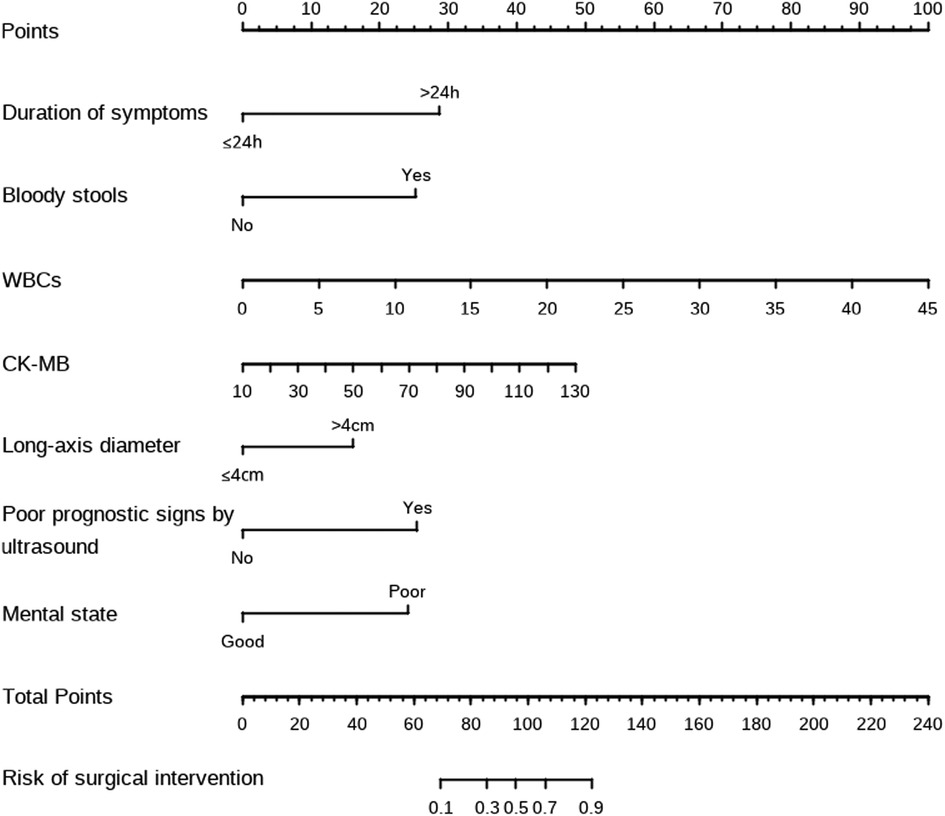
Figure 1. The nomograms for predicting the risk of surgical intervention in pediatric intussusception after hydrostatic reduction.
Validation of the nomogram
The C-index for the prediction nomogram was 0.940 (95% CI, 0.903–0.978) in the training set (Figure 2A). The Hosmer-Lemeshow test found no statistical significance in the training set (p = 0.174).
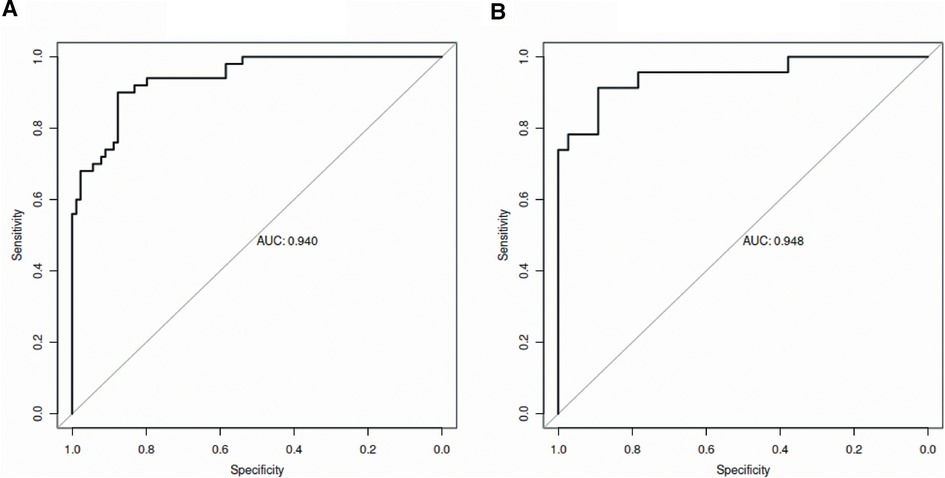
Figure 2. ROC curves of the established model in the training set (A) and validation set (B). ROC, receiver operating characteristic; AUC, area under the curve.
The C-index of the nomogram for the prediction of surgical intervention for intussusception in the validation set was 0.948 (95% CI, 0.888–1.000, Figure 2B). The calibration curve demonstrated a good agreement between prediction and observation in the validation set (Figure 3). Furthermore, the Hosmer-Lemeshow test yielded a nonsignificant statistic in the validation set (p = 0.873), indicating that no departure from a perfect fit was found. To evaluate the clinical usefulness of the model, we conducted DCA in the validation set. The DCA curve showed that the model achieved a net benefit across all threshold probabilities (Figure 4).
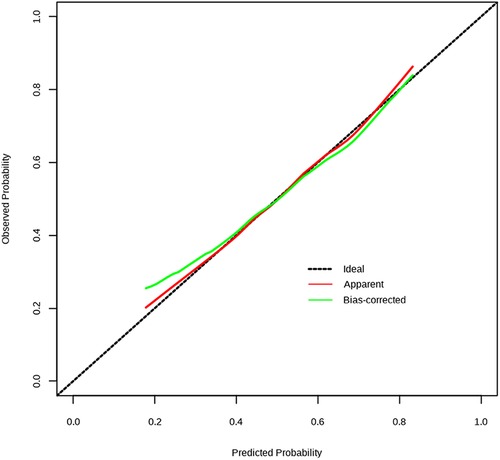
Figure 3. Calibration curve of the model in the validation set. The Y-axis represents the actual surgical intervention rate. The x-axis represents the predicted risk of surgical intervention. The dotted line represents a perfect prediction by an ideal model. The green line (bias corrected) represents the bootstrap-corrected performance of our nomogram, and the red line (apparent) represents the apparent accuracy of the nomogram.
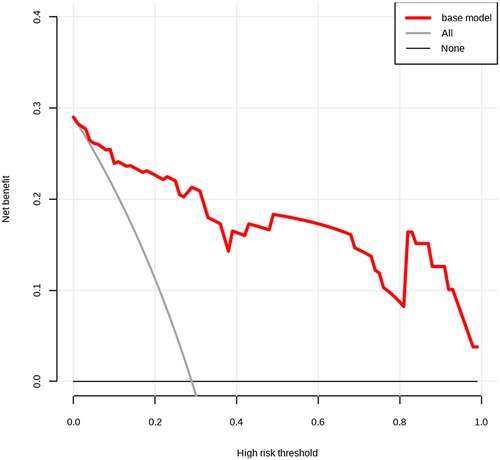
Figure 4. Decision curve analysis (DCA) for the predictive model. The net benefit was produced against the high-risk threshold. The red line represents the predictive model. The application of this predictive model would add net benefit compared with either the treat-all or the treat-none strategies.
Discussion
In the present study, an effective nomogram that used clinicopathologic risk factors to predict surgical intervention in pediatric intussusception was developed and validated. Risk factors such as duration of symptoms, bloody stools, WBCs, CK-MB, long-axis diameter, poor prognostic signs by ultrasound and mental state were incorporated into the nomogram based on the training set. In the validation set, our nomogram was identified as a highly predictive tool that could be applied directly.
Nomograms are a pictorial representation of a complex mathematical formula (13). To our best knowledge, there are few studies focusing on the development of nomograms for intussusceptions. Recently, Ting et al. (14) developed a nomogram to predict pathological intussusceptions in children. Episode time, mass length and infection history were identified as the independent predictors (14). In the present study, we used multiple logistic regression analysis to develop a preoperative nomogram that predicted surgical intervention for pediatric intussusception after hydrostatic reduction. Duration of symptoms, bloody stools, WBCs, CK-MB, long-axis diameter, poor prognostic signs by ultrasound and mental state were regarded as the predictors incorporating in the nomogram.
It has been reported that long duration of symptoms of intussusceptions was related to the increase of intestinal viability loss (9). Thus, several previous studies indicated that duration of symptoms was associated with failed non-surgery reduction. For instance, Reijnen et al. (15) found that a duration of symptoms >48 h was a risk factor for failure of hydrostatic reduction. Khorana et al. (9) reported that duration of symptoms >72 h was one of the predictors of failed non-surgery reduction (9). Similarly, Huang et al. (16) demonstrated that duration of symptoms was the independent risk factor for surgical reduction of intussusceptions. In this study, we also found that duration of symptoms was an independent predictor for surgical intervention after hydrostatic reduction. However, the cutoff value of this study was set as 24 h which was different from the studies mentioned above. The reason may be due to the duration of symptoms in the most of enrolled patients in this study did not reach 48 h.
Bloody stools are one of the classic signs of intussusception, which have been regarded as the poor predictor of intussusception (17). In 2014, He et al. (11) retrospectively reviewed the medical records of 288 cases of intussusception and found that bloody stool is one of the most important risk factors for failure of hydrostatic intussusception reduction. Consistent with He's study, Khorana et al. (9) also identified that bloody stool was a predictor of failed reduction. As expected, using multiple logistic regression analysis, the presence of bloody stools was also demonstrated as an independent predictor for surgical intervention after hydrostatic reduction in the present study.
Our study demonstrated for the first time that WBCs count and CK-MB were independent predictors for surgical intervention of intussusception. Although limited studies have revealed the relationship between WBCs count and failure of hydrostatic intussusception reduction, the association between WBCs count and intestinal necrosis has been revealed previously. In Chen's study, they found that patients underwent intestinal resection due to intestinal necrosis had significantly higher WBCs count than those without any resection (18). In 2020, Chen et al. (19) developed a prediction model that used WBCs count as an important risk factor. Chen's prediction model has been validated to predict the occurrence of intestinal necrosis well (19). It has been reported that CK-MB in blood could reflect ischemia of intestinal smooth muscle to some extent (19). Intestinal ischemia will result in intestinal necrosis, causing the synthesis of large amounts of CK or CK-MB into the blood. A previous study showed that the level of CK-MB in blood was markedly evaluated in the rat model of intestinal ischemia (20). Thus, the CK-MB may also relate to the presence of intestinal necrosis. Since the intestinal necrosis is the main reason for non-surgical intussusception reduction failure or surgery requirements, we have reasons to believe that WBCs count and CK-MB maybe associated with surgical intervention after hydrostatic reduction. But this conclusion should be confirmed by further studies with larger sample size.
Long-axis diameter is one of the important factors affecting the success rate of non-surgical intussusception reduction. Duc et al. (21) found that surgical intussusception had a significantly smaller diameter than non-surgical intussusception. Zhang et al. (22) reported that intussusception recurrence was prone with greater mass diameter. Consistent with previous studies, logistic regression analysis used in this study showed that long-axis diameter was identified as an independent predictor of surgical intervention for intussusception. Longer diameter was prone with higher risk of surgical intervention.
Diarrhea and vomiting are early symptoms of intussusception (23). In this study, the children may have vomit and diarrhea before hospitalization, which may cause dehydration of the children, with listless, lethargic, pale and other symptoms. Poor mental state reflects dehydration of the child. Patients with dehydration showed significantly higher risk of failure in treatment using hydrostatic reduction (24). Therefore, mental state as a prognostic factor of intussusception was of great significance. The poor prognosis signs by ultrasound were reported to be associated with the reduction failure in many studies. Khorana et al. (25) found that the poor prognosis signs by ultrasound was an important prognostic factor for the nonsurgical reduction. Furthermore, poor prognosis signs by ultrasound were also included as a prognostic factor for failed reduction in Chiang Mai University Intussusception Failed Score (CMUI) (26). This scoring system showed a high specificity and a high affinity for prediction of failed reduction (26). In the present study, the poor prognosis signs by ultrasound were identified as an independent predictor for surgical intervention as found in previous studies.
Other risk factors such as age, light weight (9, 25), temperature >37.8°C (9, 22) and location of mass (9) were identified as independent predictors for non-surgical intussusception reduction failure in previous studies. However, in the present study, these factors did not show strong association with surgical intervention after hydrostatic reduction. The rejection of these factors in the nomogram may be the result of nuances in the data set or confounding by other predictors (27).
After the nomogram was constructed, we validated it in the validation set. The AUC of the model was as high as 0.907 in the validation set. Additionally, calibration curve analysis and Hosmer-Lemeshow test further showed good calibration of our model in the validation set. Finally, we evaluated the clinical usefulness of the model by DCA and found that the model achieved a net benefit across all threshold probabilities, indicating that the nomogram has high clinical usefulness in our studied population.
The present study has several limitations. First, the nomogram was established based on data obtained from a single center in China. This may cause selection bias. Second, all data in the present study were collected retrospectively and the sample size of this study was relatively small. Finally, the nomogram we developed did not be validated by external dataset. Further prospective studies are needed to validate our model.
Conclusion
In conclusion, we developed a nomogram based on clinical risk factors to predict surgical intervention in pediatric intussusception after hydrostatic reduction. Duration of symptoms, bloody stools, WBCs, CK-MB, long-axis diameter, poor prognostic signs by ultrasound and mental state were identified as predictors and incorporated into the nomogram. Our internal validation demonstrated that this nomogram could be applied directly to facilitate pre-surgery decision for pediatric intussusception. However, our nomogram is just the adjunct for the pre-surgery decision and cannot be used instead of the contraindication for the non-surgical reduction.
Data availability statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by ethics committee of Guizhou Provincial People's Hospital. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
Conception and design of the research: YT, ML, YZ, XW Acquisition of data: YZ, XF, ML Analysis and interpretation of the data: XW, FL, YT Statistical analysis: YZ, XW, YT, ML Obtaining financing: None. Writing of the manuscript: YZ, XW Critical revision of the manuscript for intellectual content: YT, ML. All authors contributed to the article and approved the submitted version.
Funding
Study on the correlation between NRF2/HO-1 pathway and growth and metastasis of colorectal cancer, a project supported by the Science and Technology Fund of Guizhou Health Commission, gzwkj2021-177.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Fahiem-Ul-Hassan M, Mufti GN, Bhat NA, Baba AA, Buchh M, Wani SA, et al. Management of intussusception in the era of ultrasound-guided hydrostatic reduction: a 3-year experience from a tertiary care center. J Indian Assoc Pediatr Surg. (2020) 25(2):71–5. doi: 10.4103/jiaps.JIAPS_208_18
2. Marsicovetere P, Ivatury SJ, White B, Holubar SD. Intestinal intussusception: etiology, diagnosis, and treatment. Clin Colon Rectal Surg. (2017) 30(1):30–9. Edoi: 10.1055/s-0036-1593429
3. Talabi AO, Famurewa OC, Bamigbola KT, Sowande OA, Afolabi BI, Adejuyigbe O. Sonographic guided hydrostatic saline enema reduction of childhood intussusception: a prospective study. BMC Emerg Med. (2018) 18(1):46. doi: 10.1186/s12873-018-0196-z
4. Demirel BD, Hancıoğlu S, Dağdemir B, Ceyhan Bilgici M, Yagiz B, Bıçakcı Ü, et al. Ultrasound-guided hydrostatic reduction of ileo-colic intussusception in childhood: first-line management for both primary and recurrent cases. Acta Chir Belg. (2022) 122(4):248–52. doi: 10.1080/00015458.2021.1900521
5. Doo JW, Kim SC. Sedative reduction method for children with intussusception. Medicine (Baltimore). (2020) 99(5):e18956. doi: 10.1097/MD.0000000000018956
6. Xie X, Wu Y, Wang Q, Zhao Y, Chen G, Xiang B. A randomized trial of pneumatic reduction versus hydrostatic reduction for intussusception in pediatric patients. J Pediatr Surg. (2018) 53(8):1464–8. doi: 10.1016/j.jpedsurg.2017.08.005
7. Liu ST, Tang XB, Li H, Chen D, Lei J, Bai YZ. Ultrasound-guided hydrostatic reduction versus fluoroscopy-guided air reduction for pediatric intussusception: a multi-center, prospective, Cohort Study. World J Emerg Surg. (2021) 16(1):3. doi: 10.1186/s13017-020-00346-9
8. Yang H, Wang G, Ding Y, Li Y, Sun B, Yue M, et al. Effectiveness and safety of ultrasound-guided hydrostatic reduction for children with acute intussusception. Sci Prog. (2021) 104(3):368504211040911. doi: 10.1177/00368504211040911
9. Khorana J, Singhavejsakul J, Ukarapol N, Laohapensang M, Siriwongmongkol J, Patumanond J. Prognostic indicators for failed nonsurgical reduction of intussusception. Ther Clin Risk Manag. (2016) 12:1231–7. doi: 10.2147/TCRM.S109785
10. Wu TH, Huang GS, Wu CT, Lai JY, Chen CC, Hu MH. Clinical characteristics of pediatric intussusception and predictors of bowel resection in affected patients. Front Surg. (2022) 9:926089. doi: 10.3389/fsurg.2022.926089
11. He N, Zhang S, Ye X, Zhu X, Zhao Z, Sui X. Risk factors associated with failed sonographically guided saline hydrostatic intussusception reduction in children. J Ultrasound Med. (2014) 33(9):1669–75. doi: 10.7863/ultra.33.9.1669
12. Iasonos A, Schrag D, Raj GV, Panageas KS. How to build and interpret a nomogram for cancer prognosis. J Clin Oncol. (2008) 26(8):1364–70. doi: 10.1200/JCO.2007.12.9791
13. Balachandran VP, Gonen M, Smith JJ, DeMatteo RP. Nomograms in oncology: more than meets the eye. Lancet Oncol. (2015) 16(4):e173–80. doi: 10.1016/S1470-2045(14)71116-7
14. Ting X, Xufei D, Jiangbin L, Weijue X, Zhibao L, Guogang Y. Development and validation of a nomogram for predicting pathological intussusceptions in children prior to surgical intervention. Front Pediatr. (2022) 10:877358. doi: 10.3389/fped.2022.877358
15. Reijnen JA, Festen C, van Roosmalen RP. Intussusception: factors related to treatment. Arch Dis Child. (1990) 65(8):871–3. doi: 10.1136/adc.65.8.871
16. Huang HY, Huang XZ, Han YJ, Zhu LB, Huang KY, Lin J, et al. Risk factors associated with intestinal necrosis in children with failed non-surgical reduction for intussusception. Pediatr Surg Int. (2017) 33(5):575–80. doi: 10.1007/s00383-017-4060-0
17. Kimia AA, Williams S, Hadar PN, Landschaft A, Porter J, Bachur RG. Positive guaiac and bloody stool are poor predictors of intussusception. Am J Emerg Med. (2018) 36(6):931–4. doi: 10.1016/j.ajem.2017.10.051
18. Chen B, Cao J, Yan C, Zheng C, Chen J, Guo C. A promising new predictive factor for detecting bowel resection in childhood intussusception: the lymphocyte-C-reactive protein ratio. BMC Pediatr. (2021) 21(1):577. doi: 10.1186/s12887-021-03068-2
19. Chen W, Xiao J, Yan J, Liu R, Yang J, Xiao Y, et al. Analysis of the predictors of surgical treatment and intestinal necrosis in children with intestinal obstruction. J Pediatr Surg. (2020) 55(12):2766–71. doi: 10.1016/j.jpedsurg.2020.07.017
20. Li L, Shu F, Wang XQ, Wang F, Cai L, Zhao X, et al. Propofol alleviates intestinal ischemia/reperfusion injury in rats through p38 MAPK/NF-κB signaling pathway. Eur Rev Med Pharmacol Sci. (2021) 25(3):1574–81. doi: 10.26355/eurrev_202102_24867
21. Duc VT, Chien PC, Huyen LDM, Triet PNM, Hung PT, Thuy TM, et al. Differentiation between surgical and nonsurgical intussusception: a diagnostic model using multi-detector computed tomography. Acta Inform Med. (2021) 29(1):32–7. doi: 10.5455/aim.2021.29.32-37
22. Zhang Y, Shao CC, Wei XL, Ni PJ, Guan H, Zhao C, et al. Ultrasound findings to predict risk of recurrence in pediatric intussusception after air enema reduction. J Ultrasound Med. (2022) 41(5):1227–35. doi: 10.1002/jum.15814
23. Hsiao HJ, Wang CJ, Lee CC, Hsin YC, Yau SY, Chen SY, et al. Point-of-care ultrasound may reduce misdiagnosis of pediatric intussusception. Front Pediatr. (2021) 9:601492. doi: 10.3389/fped.2021.601492
24. Kusmayadi DD, Agnestivita LK, Indriasari V. Risk factors for failure of hydrostatic reduction in children with intussusception in Hasan Sadikin General Hospital. Med J Malaysia. (2022 Jul) 77(Suppl 1):38–41.35899887
25. Khorana J, Patumanond J, Ukarapol N, Laohapensang M, Visrutaratna P, Singhavejsakul J. Clinical prediction rules for failed nonoperative reduction of intussusception. Ther Clin Risk Manag. (2016) 12:1411–6. doi: 10.2147/TCRM.S115253
26. Khorana J, Sayuen C, Chanaturakarnnon S, Nate-Anong B, Singhavejsakul J, Tepmalai K, et al. Temporal validation of Chiang Mai university intussusception failed reduction score (Cmui). Int J Environ Res Public Health. (2022) 19(9):5289. doi: 10.3390/ijerph19095289
Keywords: intussusception, hydrostatic reduction, predictors, nomogram, risk factors
Citation: Zhuang Y, Wang X, Fan X, Li F, He G, Luo M and Tang Y (2023) Developing a nomogram for predicting surgical intervention in pediatric intussusception after hydrostatic reduction. Front. Pediatr. 11:1092548. doi: 10.3389/fped.2023.1092548
Received: 8 November 2022; Accepted: 7 April 2023;
Published: 31 May 2023.
Edited by:
Aydin Yagmurlu, Ankara University, TürkiyeReviewed by:
Erich Sorantin, Medical University of Graz, AustriaJiraporn Khorana, Chiang Mai University, Thailand
© 2023 Zhuang, Wang, Fan, Li, He, Luo and Tang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Miao Luo ZHJfdGFuZ3lpbmdtaW5nQHllYWgubmV0 Yingming Tang bHVvLm1pYW9zQGVtYWlsLmNu
†These authors have contributed equally to this work
 Yize Zhuang†
Yize Zhuang† Yingming Tang
Yingming Tang