- 1Department of Anesthesia, College of Medicine and Health Sciences, Bahirdar University, Bahirdar, Ethiopia
- 2Department of Anesthesia, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Background: Postoperative sore throat is the most frequent complication in pediatric patients after general anesthesia. This study aimed to investigate the incidence of postoperative sore throat in patients undergoing general anesthesia with tracheal intubation or laryngeal mask airway.
Methods: A hospital-based multicenter prospective observational cohort study was conducted. Proportional allocation was done with a total of 424 patients from March 1 to June 30, 2022. The information was entered into the Epi-Data software version 4.6 and analyzed with Stata 14. Socio–demographic, surgical, and anesthetic-related characteristics were analyzed using descriptive statistics. A p-value of less than 0.2 was the cutpoint of bivariate logistic regression analysis, and p-values of less than 0.05 were regarded as statistically significant in multivariate logistic regression to determine the presence and strength of association between independent variables and postoperative sore throat.
Results: A total of 411 patients were included in this study, with a response rate of 96.9%. The overall proportion of patients who developed postoperative sore throat was 45% (95% CI: 40.18–49.84). Patients who had anesthesia for more than two hours (AOR = 8.23: 95% CI = 4.08–16.5), those who were intubated by undergraduate anesthesia students (AOR = 2.67: 95% CI = 1.53–4.67), and those who had been intubated using tracheal tube (AOR = 2.38: 95% CI = 1.15–4.92) were significantly associated with the level of postoperative sore throat.
Conclusions and recommendations: We concluded that intubated children with ETT have a high incidence of post-operative sore throat. Tracheal tube usage, intubation by undergraduate students, and more than two hours of anesthesia duration were associated factors. The incidence of sore throat can be decreased with the use of a laryngeal mask airway, intubation by a senior anesthetist, and shortening of anesthesia time.
1. Introduction
General anesthesia is the most commonly used type of anesthesia for a surgical procedure involving an ETT or LMA for the maintenance of airway patency, resulting in postoperative complications (1–3).
A postoperative sore throat is a pain or discomfort in the patient's throat after receiving general anesthesia under tracheal tube or laryngeal mask airway (4–6). In the pediatric population, the incidence of postoperative sore throat following general anesthesia is not well understood and is thought to occur in 5%–41% of children with tracheal intubation (3, 7–11) and post-operative sore throat is also reported to be lower at 4%–13% in LMA use (12–16). In adult patients, up to 12%–60% get postoperative sore throat, which is a common and undesirable problem (6, 17, 18).
The multiple factors that contribute to post-operative sore throat include the choice of airway device, high tracheal tube cuff pressure, surgical manipulation of the airway, varying circuit humidification, airway suctioning, dehydration, and the type and length of anesthesia and surgery (7, 8, 19–21).
The exact time at which POST can occur is not clearly understood in the pediatric age group, even if some studies state that it occurs as early as 15 min after immediate postoperative time and reduces its incidence from 12 to 24 h (22, 23). However, the duration may continue after discharge, affecting patients' oral intake due to postoperative throat pain (8, 24).
Untreated POST will result in a longer discharge time, a negative experience with anesthesia, a longer postoperative recovery time, severe patient discomfort, distress, anxiety, dissatisfaction, increased hoarseness, and a reduction in patient life activity (3, 25–29).
The preventive and management techniques for POST in pediatric patients are essential for the early reduction of severe complications, including reduction of stimulation, use of the small-sized tube, reducing the number of attempts, use of a non–steroidal anti–inflammatory drug, lidocaine, nebulized magnesium and preemptive ketamine and steroids (30–34).
Postoperative pediatric sore throat is not extensively studied in sub-Saharan countries, even if the problem is significant. Therefore, we aimed to assess the incidence and associated factors of postoperative sore throat among pediatric patients in the Northwest Amhara Referral Hospitals, Ethiopia.
2. Methods
2.1. Study design, setting and period
A multicenter prospective observational cohort study was conducted. The study was conducted at Northwest Amhara comprehensive specialized hospitals, Ethiopia, from March 1 to June 30, 2022. The study took place at the University of Gondar Comprehensive Specialized Hospital, which has seven general surgery rooms; two obstetrics; two gynecology; and one ophthalmology operation room. Tibebe Ghion Specialized Hospital has seven general surgery rooms; two obstetrics and gynecology; two orthopedic operation rooms; and one ophthalmology operation room. Felege Hiwot Comprehensive Specialized Hospital has six general surgery rooms; two orthopedic; two obstetrics and gynecology rooms; and one ophthalmology operation room. The Debre Tabor Comprehensive Specialized Hospital has three general surgery rooms; two orthopedics; two obstetrics and gynecology operation rooms; and one ophthalmology operation room. The Debre Markos Comprehensive Specialized Hospital has three general surgery rooms; one orthopedic; two obstetrics and gynecology operation rooms; and one ophthalmology operation room. There is no distinct pediatric operating room in the above referral institutions.
Anaesthesia
Anaesthetic management was standardized. Standard patient monitoring, including an electrocardiogram, end-tidal carbon dioxide, pulse oximetry, and non-invasive arterial blood pressure, was performed. Because the study was cross-sectional and not controlled, anesthesia induction techniques were dependent on patient condition and anesthetist experience level. The cuff was inflated manually with air to a clinical endpoint of loss of an audible leak. The intra-cuff pressure was not measured because a hand-held manometer is not available in our setup.
The age, sex, weight, and physical status of the patients were recorded on a standardized form. Routine informed consent for surgery and anesthesia was obtained before the patient's arrival in the operating room. The type and duration of surgery, the intraoperative airway device used [Endotracheal tube (ETT), Laryngeal Mask Airway (LMA)], the grade of intubation, and the patient's position during surgery were noted. After the end of surgery, the airway devices were removed when patients were able to respond to commands. The patients were taken to the post-anesthesia care unit, from which they were shifted to the ward after adequate recovery.
2.2. Study population, inclusion and exclusion criteria and study variables
All pediatric surgical patients admitted at Comprehensive Specialized Hospitals of Northwest Amhara, Ethiopia, from March 1 to June 30, 2022, were considered the source population, and all pediatric surgical patients operated under general anesthesia with ETT or LMA whose age was 6–18 years were considered the study population.
All pediatric surgical patients, both elective and emergency procedures, aged 6–18 years who were operated on under general anesthesia with ETT or LMA within the study period were included in the study, whereas surgical procedures in oral, nasal, and throat surgery; recent respiratory infection; recent preoperative throat pain; postoperative need for a mechanical ventilator; and intensive care were excluded from the study.
The incidence of postoperative sore throat was the primary outcome variable, and the level of severity and associated factors of postoperative sore throat were the secondary outcome variables.
2.3. Sample size determination
The sample size was determined by applying a p-value of 50% to a single proportion formula. The sample size was calculated with a 95% confidence interval (CI) and a 5% margin of error. Because no other study with the same sociodemographic and study population characteristics has been carried out. So
Then n = 385. Where (p) represent the estimated proportion, (z) level of confidence, (d) margin of error, and n = desired sample size. Using 385 plus a 10% non-response rate of 39, the total sample size was calculated to be n = 424.
2.4. Sampling procedure
A multi-center consecutive sampling method was used until the target sample was fully obtained. Additionally, we distributed the sample within each institution using the proportionate allocation approach. We determined the final sample in each hospital by multiplying the total number of calculated sample sizes by the number of patients operated on in the last four months in each hospital, divided by the total number of cases operated in five hospitals. The final number of samples used during the analysis was 411, and because of incomplete data, 13 patients were removed.
2.5. The assessment methods and questionnaire
Self-reporting of pain is the ideal method for children who are able to do so. The pain assessment process may also include parents or guardians because their pain ratings are closely related to those of their children. The direct self-report technique can be used to evaluate postoperative patient complaints to help identify their magnitude and contributing factors. A child's self-reported throat pain was graded on a four-point severity scale, and the existence or absence of a sore throat was evaluated by a Yes/No response in an observational cohort study. The pain scale was greater than or equal to 1, and if there was no postoperative throat pain, it was rated as No on a four-point categorical scale with 0 denoting no throat pain, 1 denoting mild throat pain (complain when asked), 2 denoting moderate throat pain (complain of throat pain by itself), and 3 denoting severe throat pain (including change in voice or hoarseness).
2.6. Operational definitions
Junior anesthetist: BSC holder and senior anesthesist: MSc holder
Pediatric patients: Age range from 6 years to 18 years (35–37)
To determine whether POST is present or absent, the category pain scale is used. The absence of a sore throat was reported as no, whereas mild, moderate, and severe sore throats were rated as yes (35, 36, 38).
2.7. Data collection procedures
The questionnaire and checklist were adapted through the review of different previous similar studies (9, 23, 39–41). The questionnaire was initially prepared in English, then translated to Amharic, and then translated back into English three times to check for consistency. A structured questionnaire was used to collect the data through a face-to-face interview and a checklist for reviewing client charts. The Amharic version of the questionnaire was used for data collection.
The data was gathered by five trained BSC anesthetists, and one senior anesthetist was working as a supervisor. An interview and a review of the records are both steps in the data collection process. The data collection method used for POST was the direct self-report method. It was collected in the post-anesthesia care unit and patient wards. The presence or absence of a sore throat was noted at intervals of two hours, six hours, and twenty-four hours. Additionally, the degree of pain was assessed and classified as mild, moderate, and severe. Patients with both elective and emergency procedures were included. A record review that included information on the patient, anesthesia, and surgical procedures was also conducted in addition to the data collector interview. The questionnaires and checklists were filled out completely and collected daily after checking the completeness and consistency of the data.
2.8. Data quality assurance
A pretest at UOGCSH was conducted to assess the questionnaire's clarity, language accent, and grammatical corrections. 22 patients were included in this pretest. To maintain the quality of the data, the data collectors and supervisors were trained for 3 days on the objective of the study, the content of the questionnaire, how to fill out the questionnaire, respondent rights, informed consent, and interview technique, as well as how to maintain the confidentiality and privacy of the study subjects. The principal investigators and supervisors gave feedback and corrections daily to the data collectors. The data were cleaned, coded, and imported into EpiData version 4.6 before being exported to Stata version 14.
2.9. Data processing and analysis
Each completed questionnaire was coded on a pre-arranged coding sheet by the principal investigator to minimize errors. Data was entered into a computer using EpiData version 4.6 and exported to Stata version 14 for additional cleaning and analysis. Sorting and cross-tabulation were used to clean the data. Multicollinearity was examined using the variance inflation factor (VIF), which had a value of 1.17. Using the Shapiro-Wilk test, normality was examined for continuous variables. A Hosmer and Lemeshow test was conducted to evaluate the goodness of fit of the binary logistic regression model, and a p-value of 0.2 was obtained. The findings were presented according to the variables through text, tables, and graphs.
Initially, bivariable logistic regression analysis was performed between the dependent variable and each of the independent variables. Then all variables with a p-value <0.2 from the bivariable logistic regression analysis were fitted into the multivariable logistic regression model to control for possible confounders. An adjusted odds ratio (AOR) with a 95% confidence interval (CI) was used to measure the strength and significance of the association. A p-value <0.05 also indicated the presence of a statistically significant association between postoperative sore throat and independent variables.
3. Results
3.1. Socio-demographic characteristics of the respondents
A total of 411 pediatric patients participated in this study, with an overall response rate of 96.9%. In this study, the median age was 10 years [interquartile range (IQR): 7–13]. 52.6% of the total participants were male. 81.8% of the pediatric patients had an ASA I. Preoperative NPO status for the patient was 56% for less than or equal to 8 h. 68.9% of patients had scheduled operations on an elective basis. Abdominal and urological operations accounted for the majority of the surgical patients (54.7%) (Table 1).
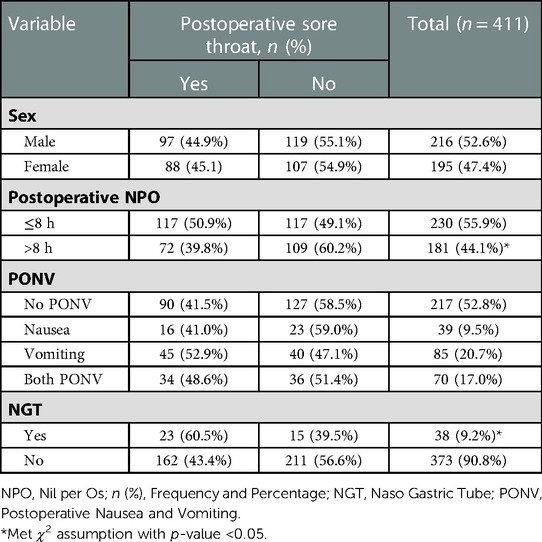
Table 1. Patients sociodemographic and surgery-related characteristics of pediatric patients at Northwest Amhara Referral Hospitals, from March 1 to June 30, 2022 (N = 411).
At two hours after surgery, the postoperative surgical pain level assessment revealed that 26.3% of patients reported no pain, 43.8% reported mild pain, 23.1% reported moderate pain, and 6.8% reported severe pain.
At six hours, 15.3% reported no pain, 37.0% reported moderate discomfort, 44.7% mild pain, and 3.0% reported moderate to severe pain.
At 24 hours, 62.8% of patients reported no pain, while 33.9%, 4.1%, and 0.2%, respectively, reported mild, moderate, and severe pain.
3.2. Anesthesia-related characteristics of pediatric patients
Among 411 patients, 84.9% of pediatric patients underwent ETT intubation, while all remaining patients underwent LMA. 94.2% of patients had intubation performed with a grade I laryngoscopy view. All patients under ETT intubation had cuffed tubes. During the perioperative period, airways are not used in 88.1% of patients. The median tube size was 5 centimeters [interquartile range (IQR) 4.5–5.5] (Table 2).
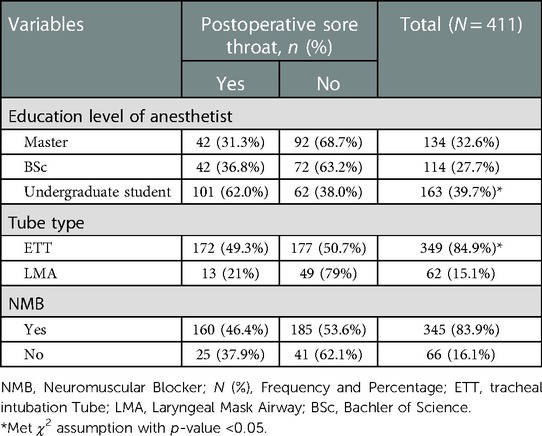
Table 2. Anesthesia-related variables of pediatric patients at northwest amhara referral hospitals, from march 1 to June 30, 2022 (N = 411).
Regarding the induction of anesthesia, 44.5% of patients were induced with ketamine, 21.7% of patients were induced with propofol, 4.1% of patients were induced with thiopental, and 29.7% of patients were induced with both ketamine and propofol. In terms of analgesia, 91.7% of patients received an opioid, 1.7% received diclofenac, 6.1% received paracetamol, and 0.5% received ketamine analgesia. Steroid (dexamethasone) was administered to 98% of the patients.
3.3. Incidence of postoperative sore throat, in each hospital, and the occurrence in each time of observation among pediatric patients
The overall proportion of patients who developed postoperative sore throat was 45% (95% CI: 40.18–49.84). The incidence of POST was included in a patient who underwent general anesthesia with ETT or LMA up to 24 h (Table 3).
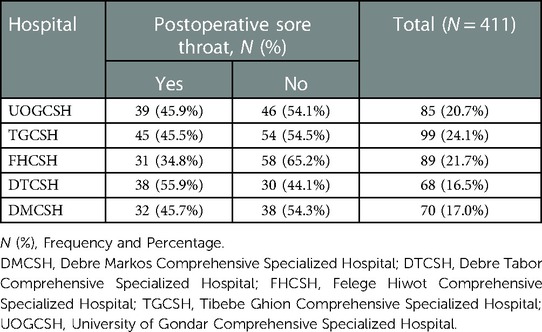
Table 3. The distribution of patients in each hospital in frequency and percentage at Northwest Amhara Referral Hospitals, from March 1 to June 30, 2022(N = 411).
POST occurred in 17.8% of patients at two hours, with mild, moderate, and severe cases accounting for 79.5%, 12.3%, and 8.2% of the cases, respectively. The incidence of POST at 6 h was 22.4%, and mild, moderate, and severe cases made up 58.7%, 30.4%, and 10.9%, respectively. At 24 h, the incidence was 4.8%, with mild and moderate cases accounting for 80.0% and 20.0%, respectively (Figure 1).
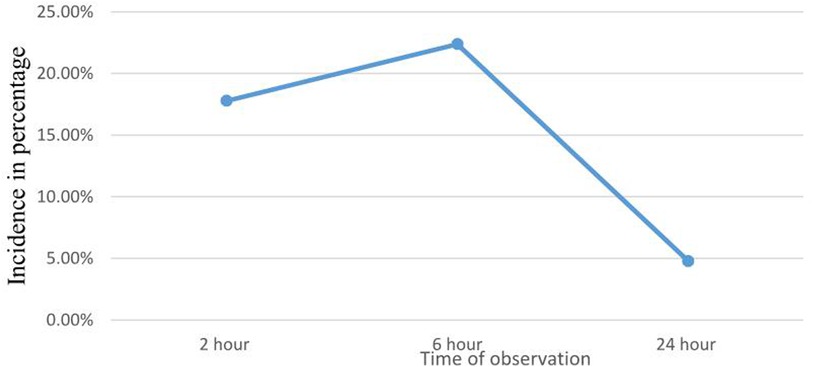
Figure 1. Incidence of POST in each time of observation among pediatric patients at Northwest Amhara Referral Hospitals, from March 1 to June 30, 2022 (N = 411).
3.4. Factors associated with postoperative sore throat among pediatric surgical patients
3.4.1. Bi-variable analysis
In the bi-variate logistic regression analysis, variables with a p-value of <0.2 were considered to be factors associated with postoperative sore throat among pediatric surgical patients. These variables included the educational level of the anesthetists who intubated the patients, the tube type (ETT vs. LMA), the presence of NGT, the length of anesthesia, and the postoperative NPO time longer than 8 h (Table 4).
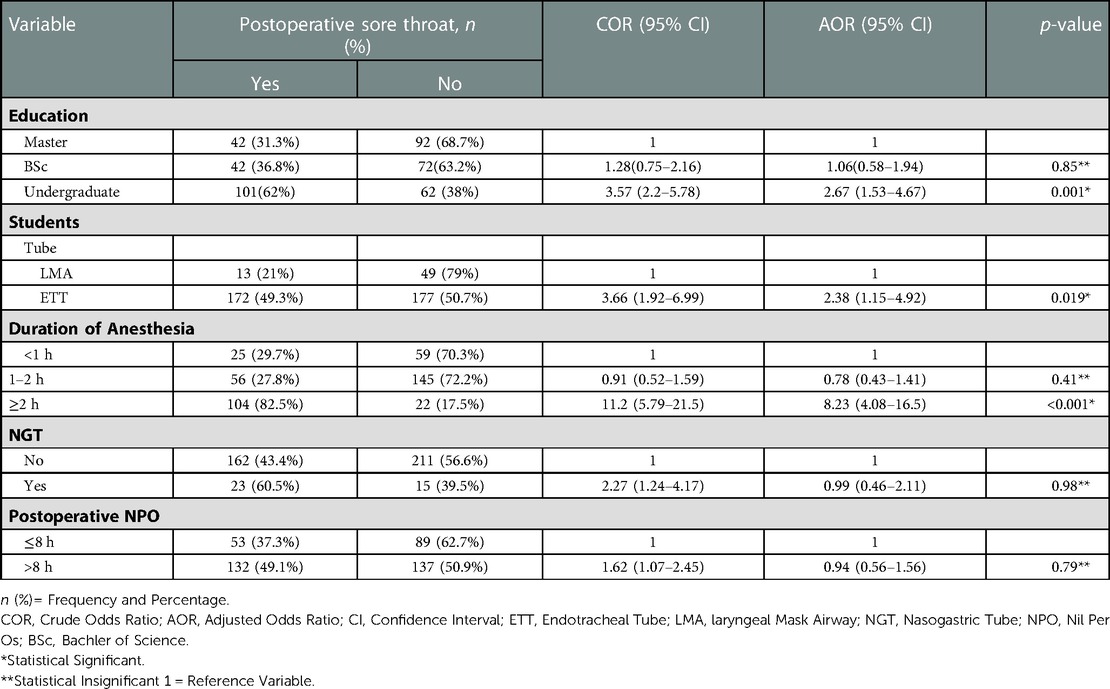
Table 4. Bivariate and multivariate logistic regression for POST among pediatric patients at northwest amhara referral hospitals, from march 1 to June 30, 2022(N = 411).
3.4.2. Multi-variable analysis
In multivariable logistic analysis, a p-value of <0.05 was considered statistically significant. The tracheal intubation, the length of anesthesia, and the education level of the anesthetists were factors associated with postoperative sore throat.
Anesthesia lasting more than two hours was 8.23 times more likely to occur POST compared with less than two hours, with 82.5% (AOR = 8.23; CI = 4.08–16.5). Using ETT was 2.38 times more likely to occur POST in comparison to using LMA, with an occurrence of 49.3% (AOR = 2.38; CI = 1.15–4.92). Intubations performed by undergraduate students were 2.67 times more likely to result in POST (62%) than those by junior and senior anesthetists (AOR: 2.67, CI = 1.53–4.67) (Table 4).
4. Discussion
Children who undergo ETT or LMA under general anesthesia frequently experience a postoperative sore throat. To the best of our knowledge, no published study has assessed the incidence of POST and its risk factors in pediatric patients in Ethiopia. If prevention and treatment strategies are not implemented during the perioperative phase, postoperative sore throat increases postoperative patient dissatisfaction, anxiety and decreasing the postoperative quality of recovery (42). The main focus of this study was to assess the incidence and associated factors of POST in pediatric surgical patients after general anesthesia ETT vs. LMA.
In this study, the incidence of POST among children after surgery was 45%, with a 95% confidence interval (CI) of (40.1–49.84). This finding is in line with studies conducted in the UK and Korea that showed 41% and 49.5%, respectively (35, 43). The possible explanation might be due to a similar data collection technique. In this study, the incidence of POST among pediatric patients was higher as compared to studies conducted in the UK and Australia, with an incidence of 36.5% and 22.6%, respectively (8, 9). The possible reasons for this difference might be sample size and the study population's socio–demographic characteristics. The incidence of POST was assessed in this study at 2, 6, and 24 h, with a higher incidence at 6 h than at 2 and 24 h. The majority of the patients experience mild POST, followed by moderate and severe. This finding is supported by a study conducted in Pakistan (36), the UK (8), and Korea (35).
POST in pediatric patients is affected by different variables. Among the factors that displayed a statistically significant link in the multivariate logistic regression were patients intubated by undergraduate students, duration of anesthesia greater than 2 h, and use of ETT for intubation (Table 4).
In this study, anesthesia lasting longer than two hours was a statistically significant factor in the occurrence of POST. Anesthesia lasting more than two hours was 8.23 times more likely to result in POST than less than two hours, with an incidence rate of 82.5% (AOR = 8.23; CI = 4.08–16.5). This finding was supported by a study conducted in the UK that showed a longer duration of anesthesia can cause POST with an occurrence of 55.2% (8). The possible explanation for this finding, in general, is that the longer the tracheal tube was in place, the longer the anesthesia lasted, and this caused irritation, inflammation, and ischemia to the airway structure and postoperative dehydration (22). Therefore, keep in mind that shortening the process can help to reduce complications.
In this study, there was a statistically significant association between the use of ETT and POST in pediatric patients when compared to the use of LMA. Using ETT was 2.38 times more likely to occur POST in comparison to using LMA, with an occurrence of 49.3% (AOR = 2.38; CI = 1.15–4.92). This finding was supported by a study conducted in the UK (8), and Australia (9), with 54.7%, and (19%) respectively. In contrast to ETT, POST was less likely to develop when LMA was used, even though it continues to have a role in the development of POST. In our study, 84.9% of patients underwent general anesthesia for surgery utilizing an ETT rather than using an LMA (15.1%). The idea that ETT use on a patient's airway or trachea could cause structural injury, airway mucosal inflammation, and congestion in addition to activating pain receptors in the trachea, which may result in POST, accounts for this finding (44, 45). As a result, even though ETT is typically employed, smooth intubation and extubation may reduce the risk of POST.
Intubation by undergraduate anesthesia students was significantly related to POST and was 2.67 times more likely to result in POST (62%) than those by junior and senior anesthetists (AOR 2.67, CI 1.53–4.67). This finding, which is supported by a study conducted in Switzerland, showed that complications were more likely to emerge when intubation was carried out by lower training individuals, with a 1.7-fold increased risk of postoperative complications (46). Multiple stimulations and attempts during tube insertion and extubation time could be the causes. Therefore, by being aware of the triggering circumstances, the likelihood of complications during anesthesia practice may be decreased.
The use of NGT and prolonged postoperative NPO duration were not significantly associated during multivariate logistic regression analysis in this study, with an AOR of 0.99 (CI = 0.46–2.11) and an AOR of 0.94 (CI = 0.56–1.56), respectively. An investigation carried out in the UK supported this prolonged postoperative NPO period and was not associated with POST in pediatric patients (8). Furthermore, the adult study discovered that the use of NGTs is a significant risk factor for the development of POST in the United Kingdom (47) and Ethiopia (48). However, research on pediatric patients found no conclusive correlation.
Due to the lack of a cuff manometer, we were unable to determine whether or not there was a significant correlation between cuff pressure and POST in this study. However, a previous study on cuff pressure revealed that cuff pressure greater than 20 cmH2O was a predictor of the occurrence of POST (9, 49). This can be brought on by increased airway pressure, which might result in ischemia, pressure sores, and the onset of throat pain (50). Cuffed ETT was not statistically linked in our study. However, a study using un–cuffed ETT demonstrates that it is a risk factor for the emergence of POST (9). The justification offered was that using an un–cuffed one causes an increase in the rate of reintubation, repeated stimulation, and mucosal injury (51). In our study, there was no correlation between POST and patients who underwent orotracheal intubation and we did not compare with nasotracheal intubation, because there were no patients who underwent nasotracheal intubation. However, a Canadian study found that nasotracheal intubation is a risk factor for the development of POST (22).
5. Strength and limitations of the study
5.1. Strength
According to our research, this is the first study of its kind to be conducted in Ethiopia. It also lays the groundwork for more research. Sufficient sample sizes were used in the investigation, which comprised multiple study centers.
5.2. Limitations
All pediatric age groups were not addressed in the study. Response bias may emerge as a result of the use of self-report data gathering techniques. The suctioning and extubation techniques as well as number of attempt to intubate were not evaluated. Due to the lack of a cuff manometer, we were unable to determine ETT cuff pressure.
6. Conclusions
Post-operative sore throat was common among pediatric patients in the study areas within the first 24 h following anesthesia. Significant risk factors for postoperative sore throat in pediatric patients after surgery and anesthesia were longer than two hours of anesthesia, ETT intubation, and intubation with undergraduate anesthesia students.
7. Recommendations
To the anesthetists: We recommend anesthetists use LMA when appropriate, reducing anesthesia time wasted during surgery in one or more ways. Remove the tube early, and put more of a priority on training for atraumatic intubation attempts. High-risk patients are better intubated by senior anesthetists. Based on other study findings, it is better to use airway blunt medication to reduce postoperative sore throat.
To the researchers: We encourage researchers to carry out randomized control trials based on ETT vs. LMA and awake vs. deep extubation. The effect of tracheal intubation cuff pressure on postoperative sore throat by the use of a cuff manometer.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
An ethical clearance was obtained from the school of medicine, College of Medicine and Health Sciences on behalf of the University of Gondar ethical review board with the number SOM/14/04/2022. “All methods were performed in accordance with the relevant guidelines and regulations”. A written support letter was obtained from Debre Markos Comprehensive Specialized Hospital, Debre Tabor Comprehensive Specialized Hospital, Felege Hiwot Comprehensive Specialized Hospital, and Tibebe Ghion Comprehensive Specialized Hospital. After the purpose and objective of the study had been informed, written participant assent and parental consent were obtained from each study participant. Participants were also informed that their participation was voluntarily and that they could stop or leave the participation at any time if they were not comfortable. The data collection tools were anonymous and kept participants’ privacy during the interview by interviewing them alone to maintain the confidentiality of any information provided by participants.
Author contributions
Conceptualization: MTM, YBB, YAN, and DYM. Data curation: MTM, YBB, YAN, and DYM. Formal analysis: MTM, YBB, YAN, and DYM. Investigation: MTM. Methodology: MTM, YBB, YAN, and DYM. Project administration: MTM. Resources: MTM. Software: MTM, YBB, YAN, and DYM. Supervision: MTM, YBB, YAN, and DYM. Validation: MTM, YBB, YAN, and DYM. Visualization: MTM. Writing – original draft: MTM and YBB. Writing – review & editing: YAN and DYM. All authors contributed to the article and approved the submitted version.
Acknowledgments
We would like to forward our deepest appreciation and thanks to the University of Gondar, College of medicine and health sciences, and school of medicine for providing Ethical clearance. We would also like to extend our thanks to Comprehensive specialized Hospitals administrators for the provision of support letter and staff cooperation during the data collection period. We are deeply grateful to study participants, data collectors, and supervisors who participated in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Brown EN, Purdon PL, Van Dort CJ. General anesthesia and altered states of arousal: a systems neuroscience analysis. Annu Rev Neurosci. (2011) 34:601. doi: 10.1146/annurev-neuro-060909-153200
2. Jaensson M, Lassinantti Olowsson L, Nilsson U. Does the size of the endotracheal tube affect the risk for sore throat following surgery in woman?: a randomized controlled study. 9th World congress for nurse anesthetists, Haag, Nederländerna, 4–8 juni 2010 (2010).
3. Higgins P, Chung F, Mezei G. Postoperative sore throat after ambulatory surgery. Br J Anaesth. (2002) 88(4):582–4. doi: 10.1093/bja/88.4.582
4. McHardy F, Chung F. Postoperative sore throat: cause, prevention and treatment. Anaesthesia. (1999) 54(5):444–53. doi: 10.1046/j.1365-2044.1999.00780.x
5. Scuderi PE. Postoperative sore throat: more answers than questions. Anesth Analg. (2010) 111(4):831–2. doi: 10.1213/ANE.0b013e3181ee85c7
6. Macario A, et al. Which clinical anesthesia outcomes are important to avoid? The perspective of patients. Anesth Analg. (1999) 89(3):652. doi: 10.1213/00000539-199909000-00022
7. Cozine K, Stone J. Determinants of postoperative sore throat. In: Anesthesiology. Philadelphia, PA, United States: Lippincott-Raven Publ 227 East Washington SQ (1993).
8. Miskovic A, et al. A prospective observational cohort study on the incidence of postoperative sore throat in the pediatric population. Pediatr Anesth. (2019) 29(12):1179–85. doi: 10.1111/pan.13757
9. Calder A, et al. Predictors of postoperative sore throat in intubated children. Pediatr Anesth. (2012) 22(3):239–43. doi: 10.1111/j.1460-9592.2011.03727.x
10. Splinter W, et al. Postoperative sore throat in children and the laryngeal mask airway. Can J Anaesth. (1994) 41(11):1081–3. doi: 10.1007/BF03015658
11. Miyerbekov Y, Mutagirov V, Batyrhanov M. Can we reduce airway management complications in children? Laryngeal mask vs. Endotracheal tube: 19AP5–2. Eur J Anaesthesiol. (2010) 27(47):256. doi: 10.1097/00003643-201006121-00826
12. Abdi W, et al. Sparing the larynx during gynecological laparoscopy: a randomized trial comparing the LMA supreme™ and the ETT. Acta Anaesthesiol Scand. (2010) 54(2):141–6. doi: 10.1111/j.1399-6576.2009.02095.x
13. McGinn G, Haynes S, Morton N. An evaluation of the laryngeal mask airway during routine paediatric anaesthesia. Pediatr Anesth. (1993) 3(1):23–8. doi: 10.1111/j.1460-9592.1993.tb00029.x
14. Füllekrug B, et al. The laryngeal mask airway: anesthetic gas leakage and fiberoptic control of positioning. J Clin Anesth. (1993) 5(5):357–63. doi: 10.1016/0952-8180(93)90097-X
15. Janssens M, Marechal J. The laryngeal mask–Liège experience. Acta Anaesthesiol Belg. (1991) 42(4):199–206.1796728
16. Maltby J, Loken R, Watson N. The laryngeal mask airway: clinical appraisal in 250 patients. Surv Anesthesiol. (1991) 35(1):12. doi: 10.1097/00132586-199102000-00013
17. Biro P, Seifert B, Pasch T. Complaints of sore throat after tracheal intubation: a prospective evaluation. Eur J Anaesthesiol. (2005) 22(4):307–11. doi: 10.1017/S0265021505000529
19. Loeser EA, et al. The influence of endotracheal tube cuff design and cuff lubrication on postoperative sore throat. Surv Anesthesiol. (1983) 27(6):341. doi: 10.1097/00132586-198312000-00012
20. Bennett M, Isert P, Cumming R. Postoperative sore throat and hoarseness following tracheal intubation using air or saline to inflate the cuff—a randomized controlled trial. Anaesth Intensive Care. (2000) 28(4):408–13. doi: 10.1177/0310057X0002800409
21. Chandler M. Tracheal intubation and sore throat: a mechanical explanation: apparatus. Anaesthesia. (2002) 57(2):155–61. doi: 10.1046/j.1365-2044.2002.02329.x
22. El-Boghdadly K, Bailey CR, Wiles MD. Postoperative sore throat: a systematic review. Anaesthesia. (2016) 71(6):706–17. doi: 10.1111/anae.13438
23. Lee JY, et al. Incidence and risk factors of postoperative sore throat after endotracheal intubation in Korean patients. J Int Med Res. (2017) 45(2):744–52. doi: 10.1177/0300060516687227
24. Calder A, et al. Predictors of postoperative sore throat in intubated children-reply. Pediatr Anesth. (2012) 22:596–7. doi: 10.1111/j.1460-9592.2012.03871.x
25. Lehmann M, et al. Postoperative patient complaints: a prospective interview study of 12,276 patients. J Clin Anesth. (2010) 22(1):13–21. doi: 10.1016/j.jclinane.2009.02.015
26. Kim MS, et al. A randomized comparison of the i-gel™ with the self-pressurized air-Q™ intubating laryngeal airway in children. Pediatr Anesth. (2015) 25(4):405–12. doi: 10.1111/pan.12609
27. Hameed M, Samad K, Ullah H. Comparison of two supraglottic airway devices on postoperative sore throat in children: a prospective randomized controlled trial. Rev Bras Anestesiol. (2020) 70:240–7.
28. Tanaka Y, et al. Lidocaine for preventing postoperative sore throat. Cochrane Database Syst Rev. (2015) 7.35658164
29. Lee JH, et al. Effects of topical dexamethasone in postoperative sore throat. Korean J Anesthesiol. (2017) 70(1):58–63. doi: 10.4097/kjae.2017.70.1.58
30. Al-Qahtani AS, Messahel FM. Quality improvement in anesthetic practice–incidence of sore throat after using small tracheal tube. Middle East J Anaesthesiol. (2005) 18(1):179–83.
31. Ahuja V, Mitra S, Sarna R. Nebulized ketamine decreases incidence and severity of post-operative sore throat. Indian J Anaesth. (2015) 59(1):37–42. doi: 10.4103/0019-5049.149448
32. Lee J, et al. Combined intraoperative paracetamol and preoperative dexamethasone reduces postoperative sore throat: a prospective randomized study. J Anesth. (2017) 31(6):869–77. doi: 10.1007/s00540-017-2411-6
33. Zhao X, Cao X, Li Q. Dexamethasone for the prevention of postoperative sore throat: a systematic review and meta-analysis. J Clin Anesth. (2015) 27(1):45–50. doi: 10.1016/j.jclinane.2014.06.014
34. Gupta S, et al. Nebulized magnesium for prevention of postoperative sore throat. Br J Anaesth. (2012) 108(1):168–9. doi: 10.1093/bja/aer437
35. Yhim HB, Yoon SH. Effects of benzydamine hydrochloride on postoperative sore throat after extubation in children: a randomized controlled trial. BMC Anesthesiology, (2020) 20(1):77.32247315
36. Hameed M, Samad K, Ullah H. [Comparison of two supraglottic airway devices on postoperative sore throat in children: a prospective randomized controlled trial]. Braz J Anesthesiol. (2020) 70(3):240–7. doi: 10.1016/j.bjan.2020.03.006
37. Butler EK, et al. Epidemiology of pediatric surgical needs in low-income countries. PLoS One. (2017) 12(3):e0170968. doi: 10.1371/journal.pone.0170968
38. Canbay O, et al. Ketamine gargle for attenuating postoperative sore throat. Br J Anaesth. (2008) 100(4):490–3. doi: 10.1093/bja/aen023
39. Hunduma JC, Merga HT. Predictors of postoperative sore throat among surgical patients at Ethiopian teaching hospitals. J Clin Med Res. (2016) 8(1):1–11. doi: 10.5897/JCMR2016.0280
40. Chang J-E, et al. Effect of endotracheal tube cuff shape on postoperative sore throat after endotracheal intubation. Anesth Analg. (2017) 125(4):1240–5. doi: 10.1213/ANE.0000000000001933
41. Wong JGL, et al. Impact of laryngeal mask airway cuff pressures on the incidence of sore throat in children. Pediatr Anesth. (2009) 19(5):464–9. doi: 10.1111/j.1460-9592.2009.02968.x
42. Yu J, Ren L, Min S. Nebulized pharmacological agents for preventing postoperative sore throat: a systematic review and network meta-analysis. PLOS ONE (2020) 15(8):e0237174.32776966
43. Perrott C, et al. Perioperative experiences of anesthesia reported by children and parents. Pediatric Anesthesia (2018) 28(2):149–56.29266767
44. Navarro RM, Baughman VL. Lidocaine in the endotracheal tube cuff reduces postoperative sore throat. J Clin Anesth. (1997) 9(5):394–7. doi: 10.1016/S0952-8180(97)00068-8
45. Mitobe Y, et al. A literature review of factors related to postoperative sore throat. J Clin Med Res. (2022) 14(2):88–94. doi: 10.14740/jocmr4665
46. Mamie C, et al. Incidence and risk factors of perioperative respiratory adverse events in children undergoing elective surgery. Paediatr Anaesth. (2004) 14(3):218–24. doi: 10.1111/j.1460-9592.2004.01169.x
47. Kloub R. Sore throat following tracheal intubation. Middle East J Anaesthesiol. (2001) 16(1):29–40.11281045
48. Gemechu BM, Gebremedhn EG, Melkie TB. Risk factors for postoperative throat pain after general anaesthesia with endotracheal intubation at the University of Gondar Teaching Hospital, Northwest Ethiopia, 2014. Pan Afr Med J. (2017) 27:127. doi: 10.11604/pamj.2017.27.127.10566
49. Felten ML, et al. Endotracheal tube cuff pressure is unpredictable in children. Anesth Analg. (2003) 97(6):1612–6. doi: 10.1213/01.ANE.0000087882.04234.11
50. Hoffman RJ, et al. Linear correlation of endotracheal tube cuff pressure and volume. West J Emerg Med. (2009) 10(3):137.19718371
Keywords: children, anesthesia complications, intubation, postoperative, sore throat
Citation: Molla MT, Bizuneh YB, Nigatu YA and Melesse DY (2023) High incidence rate of postoperative sore throat in intubated children at Northwest Amhara Comprehensive Specialized Hospitals, Ethiopia. A multicenter study. Front. Pediatr. 11:1037238. doi: 10.3389/fped.2023.1037238
Received: 5 September 2022; Accepted: 13 February 2023;
Published: 1 March 2023.
Edited by:
Jing Wu, Tianjin University, China© 2023 Molla, Bizuneh, Nigatu and Melesse. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yosef Belay Bizuneh cGhhbnVlbHlvc2VmQGdtYWlsLmNvbQ==
Specialty Section: This article was submitted to Children and Health, a section of the journal Frontiers in Pediatrics
Abbreviations AOR, Adjusted Odds Ratio; CI, Confidence Interval; COR, Crude Odds Ratio; ETT, Endotracheal Tube; LMA, Laryngeal Mask Airway; NPO, Nil Per Os; POST, Postoperative Sore Throat.
 Misganaw Terefe Molla
Misganaw Terefe Molla Yosef Belay Bizuneh
Yosef Belay Bizuneh Yonas Addisu Nigatu
Yonas Addisu Nigatu Debas Yaregal Melesse
Debas Yaregal Melesse