- 1Division of General Academic Pediatrics, Department of Pediatrics, Boston Medical Center, Boston University School of Medicine, Boston, MA, United States
- 2Division of General Pediatrics, Department of Pediatrics, MassGeneral Hospital for Children, Boston, MA, United States
- 3Department of Nutrition, Harvard T.H. Chan School of Public Health, Boston, MA, United States
- 4Division of Gastroenterology and Nutrition, MassGeneral Hospital for Children, Boston, MA, United States
- 5The Greater Boston Food Bank, Boston, MA, United States
Objective: To examine cross-sectional associations of food and housing security risks and healthy lifestyle parenting behaviors related to nutrition and physical activity among families with children with overweight/obesity.
Methods: We surveyed 407 parents of children ages 6–12 years with overweight/obesity. Exposures were measures of food and housing insecurity risk. Outcomes were healthy lifestyle parenting behaviors related to nutrition and physical activity. Logistic regression models for each exposure-outcome relationship were adjusted for parental educational attainment, parental cohabitation status, household size, and household income.
Results: In multivariable-adjusted models, food insecurity was associated with significantly lower odds of parent modeling exercise {aOR 0.60 [95% confidence interval (CI): 0.37, 0.96]} and parent modeling eating healthy foods [aOR 0.42 (95% CI: 0.24, 0.73)]. Housing insecurity was associated with significantly lower odds of parent modeling exercise [aOR 0.57 (95% CI: 0.35, 0.95)].
Conclusions: Food insecurity and housing insecurity may be barriers to parents adopting and modeling healthy lifestyle parenting behaviors related to physical activity and nutrition.
Introduction
Socio-economic and racial/ethnic disparities in childhood obesity have persisted (1, 2). In order to reduce disparities in childhood obesity, we must better understand the barriers and competing demands that families face, such as food and housing insecurity, and how these unmet social needs may impact healthy lifestyle behaviors.
Parents play an important role in promoting healthy lifestyle behaviors for their children by modeling eating healthy foods and exercise, and providing access to healthy food and physical activity opportunities. Studies have found a positive relationship between nutrition and physical activity-related parenting behaviors and children's healthy lifestyle behaviors (3, 4). Additionally, pediatric weight management interventions that incorporate parent participation have been found to be more effective (5). Given the critical role of parents in shaping healthy lifestyle behaviors of their children, we need to better understand whether stressors, such as food and housing insecurity, could make it more difficult for parents to carry out these healthy parenting behaviors.
Little is known about the impact of unmet social needs on healthy lifestyle parenting behaviors. While a few studies have examined associations of food insecurity with feeding practices of caregivers, predominantly assessed in infancy (6–9), no studies examining the impact of housing insecurity on healthy lifestyle parenting behaviors could be identified. The objective of this study was to examine the association between food and housing insecurity and healthy lifestyle parenting behaviors in a sample of predominantly low-income Hispanic families who have children with overweight or obesity. We hypothesized that food insecurity would be associated with parenting behaviors related to nutrition and that housing insecurity would be associated with parenting behaviors related to nutrition and physical activity.
Methods
We conducted a cross-sectional analysis of baseline data from the Clinic and Community Approaches to Healthy Weight trial, a two-arm randomized trial in two communities in Massachusetts with predominantly Hispanic, low-income populations. The study was conducted from 2017 to 2019 and aimed to compare the effects of two pediatric weight management interventions. Children were referred by primary care clinicians at participating federally qualified health centers and were eligible if they were ages 6 to 12 with a body mass index ≥ 85th percentile and had a parent that spoke English or Spanish. Children were ineligible if they had a sibling enrolled in the study, had a medical condition affecting their growth or physical activity, did not have a parent or guardian that could follow study procedures for 1 year, or their family was planning on leaving the health center within the study time frame. Primary care providers referred children to the study by electronic referral or electronic fax during a health care visit and a study coordinator subsequently contacted families by phone to obtain informed consent. Additional details regarding study design are published elsewhere (10). A total of 407 child-parent pairs were enrolled in the study, completed the baseline survey, and were included in this analysis. Baseline data used in this analysis were collected through a 20-minute phone survey with the child's parent or guardian, which was conducted prior to randomization assignment or distribution of intervention materials. The Massachusetts Department of Public Health Institutional Review Board approved the study.
Exposures were measures of food and housing insecurity. Risk of food insecurity was assessed using the validated 2-item Hunger Vital Sign (11):
1. Within the past 12 months we worried whether our food would run out before we got money to buy more.
2. Within the past 12 months the food we bought just didn't last and we didn't have money to get more.
Response options included: often true, sometimes true, or never true. An affirmative response (often true or sometimes true) to either question was categorized as food insecure.
Risk of housing insecurity was assessed with questions from the National Survey of America's Families 2002 Questionnaire (12):
1. During the last 12 months, was there a time when you and your family were not able to pay your mortgage, rent or utility bills?
2. During the last 12 months, did you or your children move in with other people even for a little while because you could not afford to pay your mortgage, rent or utility bills?
Response options were yes/no. An affirmative response to either question was categorized as housing insecure.
Outcomes were assessed with individual items drawn from validated measures of parental support for physical activity (Activity Support Scale for Multiple Groups; ACTS-MG) (13) and parental feeding practices (Comprehensive Feeding Practices Questionnaire; CFPQ) (14). Each item was rated with a 4-point Likert scale (strongly agree = 4, agree = 3, disagree = 2, strongly disagree = 1), modified slightly from the Likert scale in the CFPQ to maintain consistency among items. These Likert scales were converted into a dichotomous agree (strongly agree or agree) or disagree (disagree or strongly disagree) for the purposes of this analysis:
1. I exercise or am physically active on a regular basis (13).
2. I take my child to places where he/she can be active (13).
3. I model healthy eating for my child by eating healthy foods myself (14).
4. Most of the food I keep in the house is healthy (14).
Descriptive statistics were used to characterize the overall sample stratified by exposures. A separate logistic regression model was created for each exposure-outcome combination. We included a priori confounders in adjusted models that have strong theoretical associations with the exposures and outcomes and have been controlled for in similar studies in the literature (7, 8, 15, 16). Confounders included: parental educational attainment, parental cohabitation status, household size, and household income. The household income variable was dichotomized with a cutoff of $20,000, which is approximately 100% of the federal poverty level for a family of 4 in 2017 (17). Individuals with missing data were excluded from the adjusted models. A significance level of α = 0.05 was used for all statistical tests. Data were analyzed using SAS version 9.4.
Results
Descriptive statistics of 407 parent and child participant pairs are presented in Table 1. Overall, 69% of families reported an income of $20,000 or less and 93% of children were Hispanic. Forty nine percent of families screened positive for food insecurity and 30% screened positive for housing insecurity.
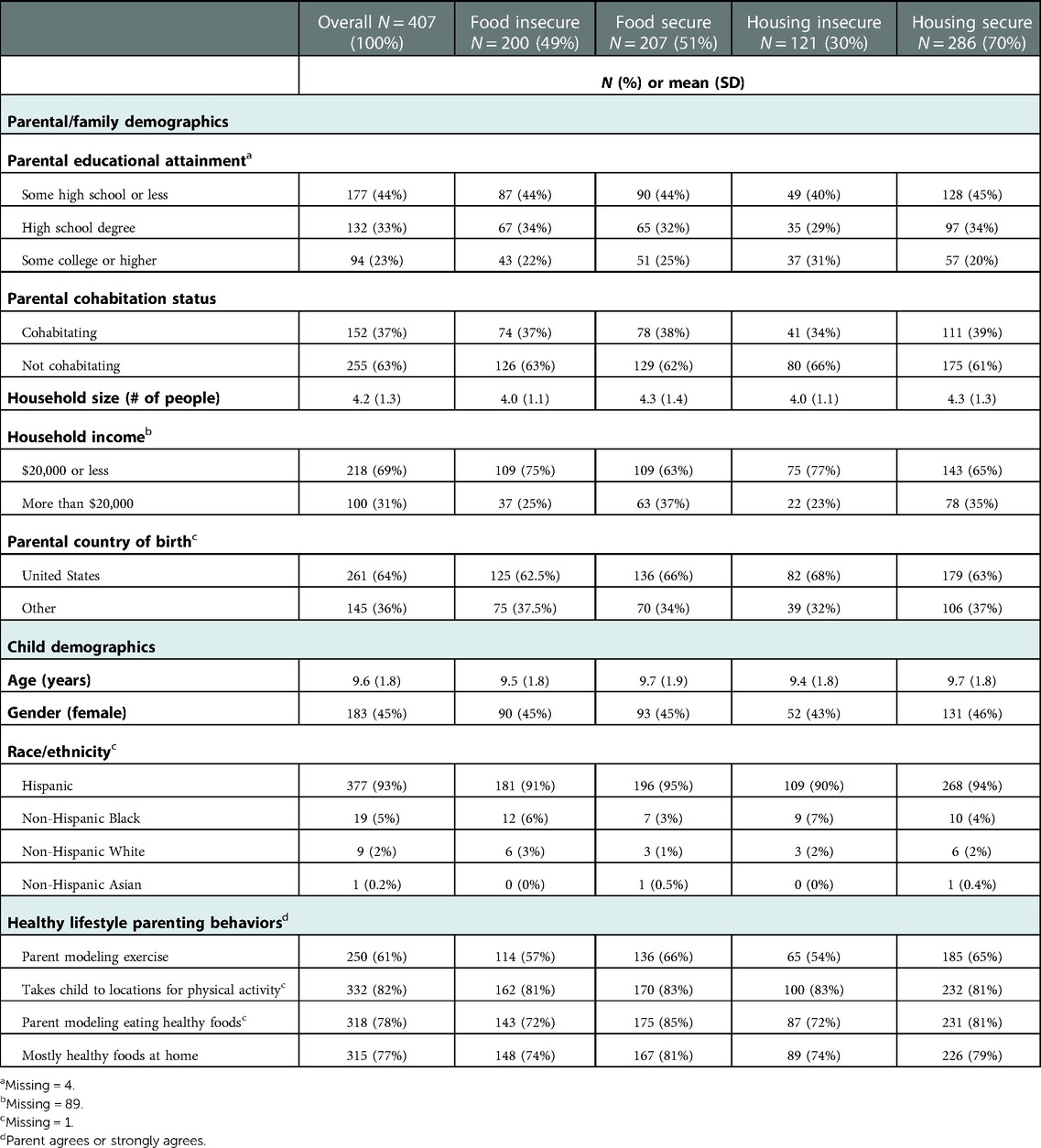
Table 1. Sample characteristics in the Clinic and Community Approaches to Healthy Weight trial by food and housing security status (N = 407).
In the unadjusted model (Table 2), food insecurity was not statistically significantly associated with parent modeling exercise {OR 0.69 [95% confidence interval (CI): 0.46, 1.03]}, whereas after adjusting for confounders, the confidence interval narrowed slightly and the association was statistically significant [aOR 0.60 (95% CI: 0.37, 0.96)]. In the unadjusted model, food insecurity was associated with lower odds of parent modeling eating healthy foods [OR 0.44 (CI: 0.27, 0.73)] and the association remained significant in the fully-adjusted model [aOR 0.42 (95% CI: 0.24, 0.73)]. In the partially-adjusted model (not adjusted for income), food insecurity was associated with keeping mostly healthy foods at home [aOR 0.59 (95% CI: 0.36, 0.96)] and after adjusting for income the effect estimate was similar with a slightly widened confidence interval [aOR 0.61 (95% CI: 0.36, 1.04)]. In unadjusted and fully-adjusted models, there were no significant associations between food insecurity and taking child to locations for physical activity.
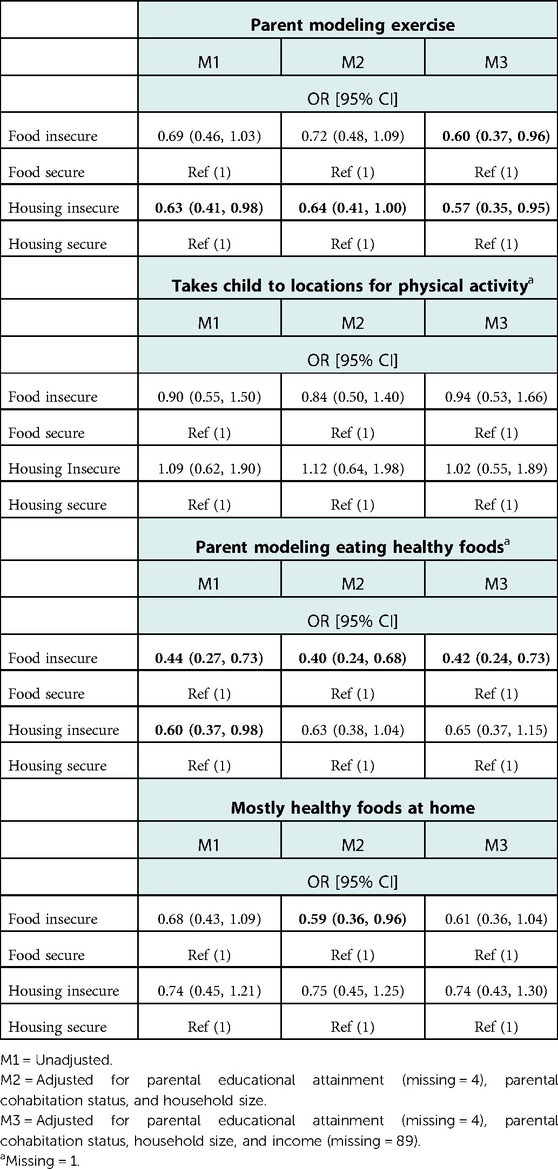
Table 2. Logistic regression models for association between food and housing security status and healthy lifestyle parenting behaviors (N = 407).
In the unadjusted model (Table 2), housing insecurity was significantly associated with lower odds of parent modeling exercise [OR 0.63 (95% CI: 0.41, 0.98)] and this association remained significant in the fully-adjusted model [aOR 0.57 (95% CI: 0.35, 0.95)]. In the unadjusted model, housing insecurity was associated with lower odds of parent modeling eating healthy foods [OR 0.60 (95% CI: 0.37, 0.98)], but this association was no longer significant in the fully-adjusted model [aOR 0.65 (95% CI: 0.37, 1.15)]. In unadjusted and fully-adjusted models, there were no significant associations between housing insecurity and taking child to locations for physical activity or keeping mostly healthy foods at home.
Discussion
In this study of predominantly low-income Hispanic children with overweight or obesity, food insecurity was associated with lower odds of parental modeling of exercise and parental modeling of eating healthy foods and housing insecurity was associated with lower odds of parental modeling of exercise, after adjustment for confounders.
Our study's finding that food insecurity was associated with healthy lifestyle parenting behaviors related to nutrition is consistent with previous literature demonstrating associations between food insecurity and feeding practices, predominantly in infants and toddlers (6–9). A potential mechanism to explain our study's food insecurity findings may be that families without stable availability of, and access to, a quality food supply might not have the resources to model healthy eating.
Our finding that food and housing insecurity were associated with lower odds of parent modeling of exercise may be due to limitations in parental bandwidth due to competing demands, high levels of stress, or lack of access to consistent spaces for exercise. There is a lack of literature on housing insecurity and parenting behaviors with which our results can be compared. However, we know that housing instability is negatively associated with the health of both caregivers (15, 18) and children (15, 16). These associations could potentially be mediated through nutrition and physical activity-related behaviors of caregivers.
The study sample was predominantly Hispanic and low-income and included only parents of children with overweight or obesity, which provides new insight into parenting behaviors in this population; however, these associations may not generalize to other populations. No causal conclusions can be made from this analysis given the cross-sectional design. Due to concern of respondent burden with lengthy study measures, outcome measures were limited to individual items drawn from larger validated measures, which may limit validity. Additionally, the ACTS-MG was validated with African American and non-Hispanic white parents (13) and the CFPQ was validated with predominantly Caucasian parents with a higher median income and children of slightly younger age (4 to 6 years of age) relative to our sample (14), so the validity of the measures in our sample of predominantly Hispanic parents of school-aged children is unknown. Since exposure and outcome measures were self-reported, there is the potential for social desirability bias. Particularly, with the outcome measures, parents were asked questions regarding healthy foods, which requires them to subjectively report whether food is healthy and results in more variability compared to directly measuring the dietary quality of foods kept in the house and consumed by parents. While we did not use the comprehensive 18-item United States Department of Agriculture (USDA) food insecurity measure which may identify additional dimensions of food insecurity, the 2-item Hunger Vital Sign is a widely used measure that assesses for food insecurity risk and has been validated across multiple populations including caregivers of young children (11), youth and adolescents (19), and adults (20). There is no gold standard measure to screen for housing insecurity and existing screening tools capture different dimensions of housing-related risk (21). The 2-item housing insecurity measure used in this analysis primarily assessed for housing affordability and did not assess for other dimensions such as overcrowding, multiple moves, or homelessness, which may have different associations with the outcomes. We considered the possibility of examining the co-occurrence of food and housing insecurity by structuring the exposure as 4 mutually exclusive groups that incorporate both food and housing into one variable, however we were unable to perform this analysis due to limitations in sample size. Lastly, the household income variable had a large number of missing responses (n = 89), which were thought to be missing not at random (likely higher rates of missing for lower income levels), which resulted in the selection of a complete case analysis approach.
These findings demonstrate that food and housing insecurity may be barriers to parents engaging in healthy lifestyle parenting behaviors related to physical activity and nutrition. As accountable care organizations move towards screening for unmet social needs, such as food and housing insecurity, clinicians and pediatric weight management interventions should address these needs as important components of healthy lifestyle change. Additionally, disparities in unmet social needs and child health outcomes, including obesity, may be impacted by historical inequities and systemic racism (22, 23). Upstream multi-level interventions including public policy to address food and housing security should be implemented with an eye towards decreasing disparities and improving health outcomes, particularly in low-income communities and communities of color.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: The data presented in this study are available on request. Requests to access these datasets should be directed toa2Vsc2V5LmVnYW5AYm1jLm9yZw==.
Ethics statement
The studies involving human participants were reviewed and approved by Massachusetts Department of Public Health Institutional Review Board. Written informed consent from the participants’ legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
Conceptualization, KAE, LF, EMT, ML, MP; methodology, KAE, LF, EMT, MP, ML, MS, CJK; formal analysis, ML and KAE; investigation, IC; data curation, ML; writing—original draft preparation, KAE; writing—review and editing, ML, MP, IC, MS, CJK, EMT, LF. All authors contributed to the article and approved the submitted version.
Funding
This research was funded by the Centers for Disease Control and Prevention National Center for Chronic Disease Prevention and Health Promotion (Award no.: U18DP006259). Egan was funded under grant number T32HS022242 from the Agency for Healthcare Research and Quality (AHRQ), U.S. Department of Health and Human Services. Fiechtner is supported by grant number K23HD090222 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Taveras was supported by grant K24DK105989 from the National Institute of Diabetes and Digestive and Kidney Diseases. Taveras is supported by grant K24HL159680 from the National Heart, Lung, and Blood Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Centers for Disease Control, the National Institutes of Health, AHRQ, U.S. Department of Health and Human Services, or any other funders.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ogden CL, Carroll MD, Fakhouri TH, Hales CM, Fryar CD, Li X, et al. Prevalence of obesity among youths by household income and education level of head of household—united States 2011–2014. Morb Mortal Wkly Rep. (2018) 67(6):186–9. doi: 10.15585/mmwr.mm6706a3
2. Hales CM, Carroll MD, Fryar CD, Ogden CL.. prevalence of obesity among adults and youth: United States, 2015–2016. Nchs Data Brief. (2017) 288:1–8. PMID: 29155689
3. Xu H, Wen LM, Rissel C. Associations of parental influences with physical activity and screen time among young children: a systematic review. J Obes. (2015) 2015:1–23. doi: 10.1155/2015/546925
4. Pearson N, Biddle SJ, Gorely T. Family correlates of fruit and vegetable consumption in children and adolescents: a systematic review. Public Health Nutr. (2009) 12(2):267–83. doi: 10.1017/S1368980008002589
5. Niemeier BS, Hektner JM, Enger KB. Parent participation in weight-related health interventions for children and adolescents: a systematic review and meta-analysis. Prev Med. (2012) 55(1):3–13. doi: 10.1016/j.ypmed.2012.04.021
6. Gross RS, Mendelsohn AL, Fierman AH, Racine AD, Messito MJ. Food insecurity and obesogenic maternal infant feeding styles and practices in low-income families. Pediatrics. (2012) 130(2):254–61. doi: 10.1542/peds.2011-3588
7. Orr CJ, Ben-Davies M, Ravanbakht SN, Yin HS, Sanders LM, Rothman RL, et al. Parental feeding beliefs and practices and household food insecurity in infancy. Acad Pediatr. (2019) 19(1):80–9. doi: 10.1016/j.acap.2018.09.007
8. Bronte-Tinkew J, Zaslow M, Capps R, Horowitz A, McNamara M. Food insecurity works through depression, parenting, and infant feeding to influence overweight and health in toddlers. J Nutr. (2007) 137(9):2160–5. doi: 10.1093/jn/137.9.2160
9. Feinberg E, Kavanagh PL, Young RL, Prudent N. Food insecurity and compensatory feeding practices among urban black families. Pediatrics. (2008) 122(4):e854–60. doi: 10.1542/peds.2008-0831
10. Fiechtner L, Perkins M, Biggs V, Langhans N, Sharifi M, O'Connor G, et al. Rationale and design of the clinic and community approaches to healthy weight randomized trial. Contemp Clin Trials. (2018) 67:16–22. doi: 10.1016/j.cct.2018.01.002
11. Hager ER, Quigg AM, Black MM, Coleman SM, Heeren T, Rose-Jacobs R, et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics. (2010) 126(1):e26–32. doi: 10.1542/peds.2009-3146
12. Abi-Habib N, Safir A, Triplett T, Cunningham P. National Survey of America's Families 2002 NSAF Questionnaire. (2004).
13. Davison KK, Li K, Baskin ML, Cox T, Affuso O. Measuring parental support for children's physical activity in white and African American parents: the activity support scale for multiple groups (ACTS-MG). Prev Med. (2011) 52(1):39–43. doi: 10.1016/j.ypmed.2010.11.008
14. Musher-Eizenman D, Holub S. Comprehensive feeding practices questionnaire: validation of a new measure of parental feeding practices. J Pediatr Psychol. (2007) 32(8):960–72. doi: 10.1093/jpepsy/jsm037
15. Sandel M, Sheward R, Ettinger de Cuba S, Coleman SM, Frank DA, Chilton M, et al. Unstable housing and caregiver and child health in renter families. Pediatrics. (2018) 141(2):e20172199. doi: 10.1542/peds.2017-2199
16. Sandel M, Sheward R, Ettinger de Cuba S, Coleman S, Heeren T, Black MM, et al. Timing and duration of Pre- and postnatal homelessness and the health of young children. Pediatrics. (2018) 142(4):e20174254. doi: 10.1542/peds.2017-4254
17. Department of Health and Human Services, Office of the Secretary. Annual Update of the HHS Poverty Guidelines. Fed Regist. (2017) 82(19):8831–32. Available at: https://www.govinfo.gov/app/details/FR-2017-01-31
18. Suglia SF, Duarte CS, Sandel MT. Housing quality, housing instability, and maternal mental health. J Urban Heal. (2011) 88(6):1105–16. doi: 10.1007/s11524-011-9587-0
19. Baer TE, Scherer EA, Fleegler EW, Hassan A. Food insecurity and the burden of health-related social problems in an urban youth population. J Adolesc Heal. (2015) 57(6):601–7. doi: 10.1016/j.jadohealth.2015.08.013
20. Gundersen C, Engelhard EE, Crumbaugh AS, Seligman HK. Brief assessment of food insecurity accurately identifies high-risk US adults. Public Health Nutr. (2017) 20(8):1367–71. doi: 10.1017/S1368980017000180
21. De Marchis EH, Ettinger de Cuba SA, Chang L, Sheward RS, Doran KM, Gottlieb LM, et al. Screening discordance and characteristics of patients with housing-related social risks. Am J Prev Med. (2021) 61(1):e1–e12. doi: 10.1016/j.amepre.2021.01.027
22. Odoms-Young A, Bruce M. Examining the impact of structural racism on food insecurity: implications for addressing racial/ethnic disparities. Fam Community Heal. (2018) 41(Suppl 2 Suppl, Food Insecurity and Obesity):S3–6. doi: 10.1097/FCH.0000000000000183
Keywords: food insecurity, housing insecurity, childhood obesity, parenting behaviors, nutrition, physical activity
Citation: Egan KA, Luo M, Perkins M, Castro I, Sandel M, Kistin CJ, Taveras EM and Fiechtner L (2023) Association between unmet social needs and healthy lifestyle parenting behaviors. Front. Pediatr. 11:1015610. doi: 10.3389/fped.2023.1015610
Received: 9 August 2022; Accepted: 17 January 2023;
Published: 23 February 2023.
Edited by:
Meixian Zhang, Taizhou Hospital of Zhejiang Province Affiliated to Wenzhou Medical University, ChinaReviewed by:
Sarah Goff, University of Massachusetts Amherst, United StatesLiliana Aguayo, Emory University, United States
© 2023 Egan, Luo, Perkins, Castro, Sandel, Kistin, Taveras and Fiechtner. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kelsey A. Egan S2Vsc2V5LmVnYW5AYm1jLm9yZw==
Specialty Section: This article was submitted to Pediatric Obesity, a section of the journal Frontiers in Pediatrics
 Kelsey A. Egan
Kelsey A. Egan Man Luo
Man Luo Meghan Perkins
Meghan Perkins Ines Castro2
Ines Castro2 Elsie M. Taveras
Elsie M. Taveras Lauren Fiechtner
Lauren Fiechtner