- 1Department of Pediatric and OB/GYN Social Work, Johns Hopkins Children’s Center, Baltimore, United States
- 2Department of Pediatrics, Johns Hopkins School of Medicine, Baltimore, United States
Sudden Unexpected Infant Death (SUID) from sleep-related causes is a leading cause of infant mortality worldwide. Sudden Infant Death Syndrome (SIDS) is one of the primary causes of SUID attributed to one or more environmental or behavioral determinants surrounding safe sleep practices among infants. The focus of many interventions on mitigating sleep-related infant deaths have addressed visible determinants pertaining to bed sharing, safe sleep surfaces, and removal of blankets, toys and other choking or strangulation hazards. Tobacco reduction and cessation have not been at the heart of any infant safe sleep interventions although addressing tobacco exposure is one of the primary safe sleep recommendations of the American Academy of Pediatrics. To date, there has not been a comprehensive review published on tobacco-related components across safe sleep interventions to reduce the risk of SIDS and SUID as the basis to contribute towards decreasing the rate of infant mortality. This review synthesizes the best practices, strategies, education, and additional interventions centered on addressing tobacco exposure as a risk factor for sleep-related infant deaths. Ten peer-reviewed studies were identified between 1995 and 2021 and integrated into this narrative review. There were three cross-sectional studies, three campaigns, one multi-center case control study, two randomized controlled trials, and two group comparison studies. Strengths and limitations of each approach are delineated followed by recommendations for future campaign, research, program, and practice endeavors to account for the totality of pertinent modifiable risk factors that contribute towards heightened infant mortality from sleep-related causes.
Introduction
Sudden Unexpected Infant Death (SUID) is one of the leading causes of infant mortality across the world. Approximately, 3,400 infants under one year of age die annually from SUID in the United States (1). In fact, the vast majority of SUID cases are attributed to sleep-related causes. Furthermore, nearly 40% of SUID cases arise from Sudden Infant Death Syndrome (SIDS) (2). SIDS is characterized as the sudden unexpected death of an infant less than one year of age marked by the onset of the fatal episode resulting during sleep which remains unexplained after a thorough investigation inclusive of complete autopsy and review of the circumstances of death along with the clinical history (3). There are many environmental and behavioral determinants that can serve as both protective and risk factors for SIDS. Several of these determinants include sleep surfaces, environmental tobacco exposure, and heating conditions (4). All of them constitute environmental conditions in the Triple Risk Model which delineates the interface of infant vulnerability and critical time of development with environmental conditions in heightening an infant's susceptibility to SIDS (5).
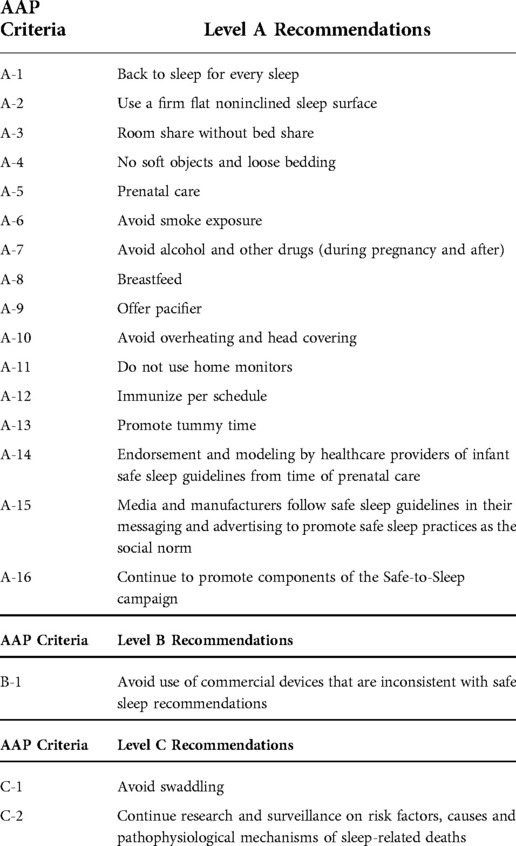
The American Academy of Pediatrics (AAP) delineates recommendations for safe sleep practices as SIDS and SUID reduction measures among infants (Table 1). These recommendations include the following: supine sleep position, firm sleep surface, no bed-sharing, no soft objects and loose bedding, avoidance of smoke exposure, no overheating, breastfeeding, among many more (4). Each of these recommendations presents a target for intervention. Of note, the predictive and causal factors of SIDS and SUID are multifactorial. Focusing on one or a couple of these determinants (e.g., safe sleep surfaces) does not comprehensively account for the totality of pertinent risk factors that contribute towards the incidence and prevalence of infant mortality attributed to sleep-related deaths.
Many of these risk factors embody social determinants of health. The built environment, access to healthcare resources and services, socioeconomic status, and many more social determinants are inter-related and can impact health outcomes in either positive or adverse directions. Cultural factors also could represent either risk or protective factors. Both tobacco use and bed-sharing are significantly more prevalent in Eastern cultures, thereby heightening risk of sleep-related infant deaths across these communities (6).
Tobacco exposure is one of the leading forms of environmental smoke exposure that significantly increases the risk of SIDS and SUID among infants. From a postnatal perspective, environmental smoke exposure can impact the growth and immune system of infants given their smaller skin body composition (fat, muscle, and bone proportions) and compromise their airway which can further create respiratory complications that could be life-threatening, especially during time of sleep (7, 8). Prematurity and low birth weight attributed to prenatal tobacco exposure also heighten the risk of SIDS among infants (9). Of note, prenatal tobacco exposure creates an increasingly hypoxic environment for the fetus which potentially has implications for reducing brainstem-mediated cardiorespiratory control and sleep arousal for neonates postnatally (10). Similarly, unsafe sleep surfaces that are not in line with the AAP safe sleep recommendations represent a risk factor for SIDS.
Most interventions to address infant safe sleep have focused on a cluster of SIDS-related risk factors. These interventions have primarily involved addressing the most visible environmental determinants related to safe sleep surfaces and furniture (11). In fact, not a single safe sleep intervention has ever addressed every single safe sleep recommendation outlined by the AAP. Furthermore, tobacco reduction or cessation has also never been at the heart of any of these interventions likely given that the provider (e.g., pediatrician, family practitioner, obstetrician) for the SUID reduction intervention may not always be the provider (e.g., internist, family practitioner) for the recipient (caregivers) of the intervention. In addition, part of the complexities surrounding this issue center on variations in tobacco control policies (e.g., smokefree legislation, tobacco cessation) around tobacco exposure among the pediatric population (12). Of note, tobacco cessation efforts have demonstrated success among caregivers of infants and children in several prior studies (13) which further yields promise in integrating relevant content into infant sleep safety interventions. However, it has been integrated in parts of some safe sleep interventions as the basis to account for more SIDS-related risk factors. Furthermore, each of these risk factors impacts one another. In fact, multiple risk factors for SIDS are cumulative in effect. For example, infants sleeping in prone positions amidst shared bed spaces are more likely to be at a higher risk for SIDS with increased tobacco exposure (8).
It is crucial to account for both caregiver tobacco use and passive tobacco exposure given that they both contribute significantly towards increasing the risk of sleep-related infant deaths. Furthermore, both constitute the leading cause of environmental exposure among children and are inclusive of both traditional and electronic nicotine delivery systems (ENDS). In light of the growing vaping epidemic in recent years, the use of ENDS products across sociodemographics has continued to rise (14). Of note to date, there is limited knowledge on the long-term effects of the chemicals found in e-cigarettes, vape pens, and additional ENDS products which in turn heightens risk on the unknown health consequences of vaping and e-cigarette use and exposure on infants both pre and post-birth.
Infants are at a nearly three-fold increased risk of dying from SIDS if their mother smokes (15, 16). Furthermore, nearly two-thirds of SIDS-related deaths among infants could be prevented without both maternal smoking during pregnancy and passive tobacco exposure post-birth (15, 17–19). Addressing tobacco use and exposure prenatally continues to be a standard of practice; however, it is imperative to provide tobacco reduction and cessation support to caregivers on a continuum since risk of relapse increases significantly postnatally (20). In addition, it is crucial to account for caregivers from all walks of life that are or will be involved in the care of the infant both prenatally and postnatally inclusive of pregnant women, adoptive parents, and caregivers who identify across different gender groups.
To date, a comprehensive review of the literature has not been conducted to identify tobacco-related components of interventions to promote safe sleep practices as a predictor of reducing infant mortality attributed to sleep-related causes. The goals of this review are the following: (1) critically examine the best practices, strategies, education, messaging, and other interventions to address tobacco use in promoting safe sleep practices among infants; (2) assess outcomes that results from these clinical and organizational efforts; (3) reflect on strengths and limitations of each tobacco-related component across interventions; and (4) propose future directions in research and practice to target tobacco use as a modifiable risk factor for SIDS and SUID as the basis to contribute towards decreasing the risk of infant mortality.
Materials and methods
Search strategy
A narrative review of peer-reviewed literature on strategies, best practices, education and additional interventions on promoting safe sleep practices to reduce the risk of SIDS in infants across a range of community and healthcare settings was conducted in April 2022. The medical, public health, and psychosocial databases reviewed were the following: Medline, APA PsychInfo, Cochrane Review, Academic Search Premier, CINAHL, ERIC, and EBSCO. Key terms used across searches were the following: variants of sudden infant death syndrome, tobacco, smoking, vaping, neonate/infant/newborn/baby, pediatric, caregiver, parent, guardian, intervention, promotion, education, strategy, and best practices.
Eligibility criteria
Peer-reviewed journal articles were included that involved practices, interventions, and strategies to address tobacco use and exposure as a risk factor for sleep-related deaths as the basis to and promote safe sleep practices among infants. Any articles that did not include tobacco-related components in the implementation of SIDS and SUID reduction interventions were excluded from this review.
Procedure
Two authors independently reviewed all titles and abstracts across each selected database. Any differences concerning full-text inclusion were resolved through consensus. The authors then independently abstracted data across all included studies on best practices, strategies, education, and any other intervention characteristics, tobacco-related findings, and additional descriptive and qualitative information on the nature and implementation of interventions. Findings were subsequently compared and discrepancies were resolved through active discussions amongst the authors.
Ethics
Institutional review board approval was not required for this narrative review.
Results
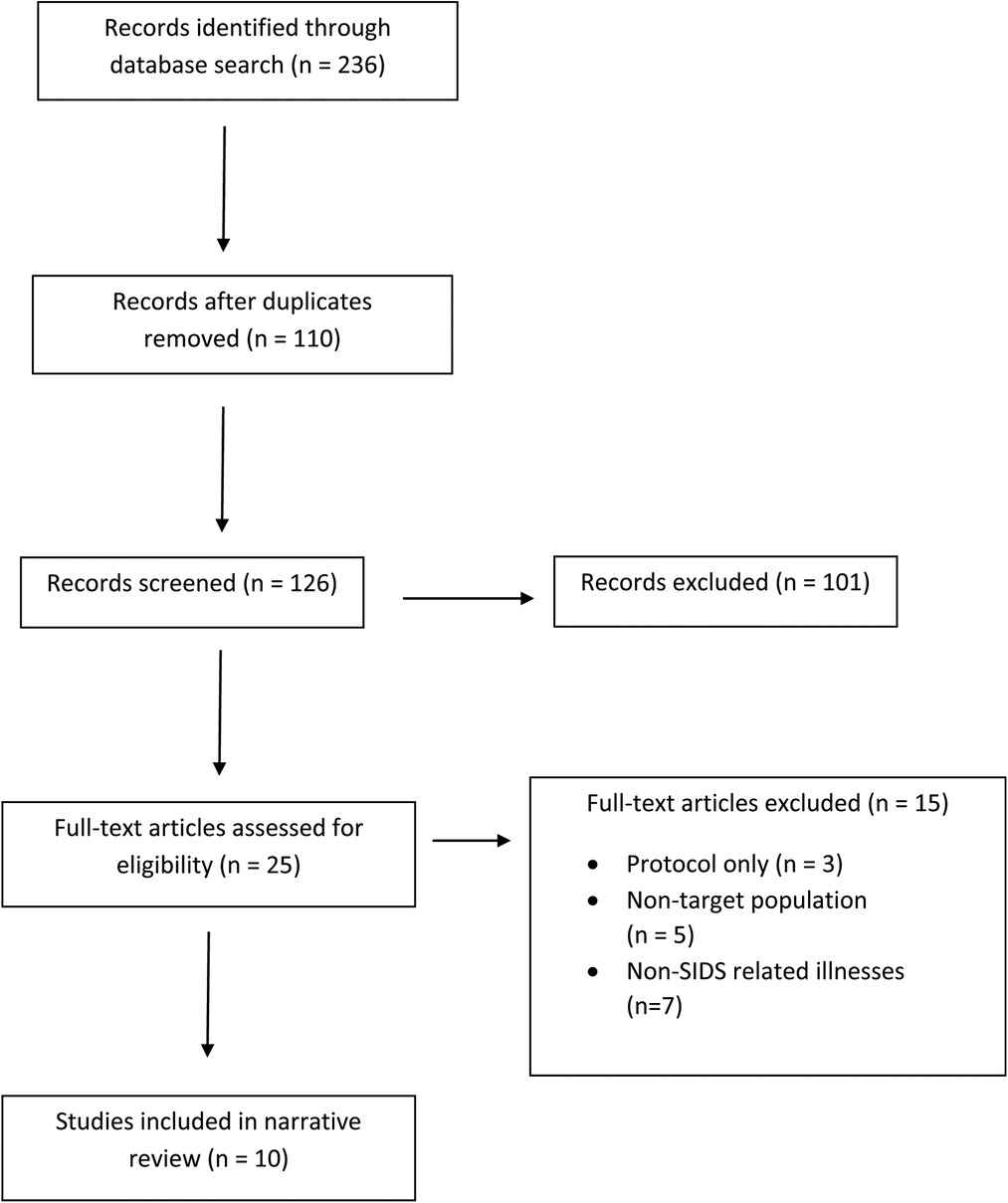
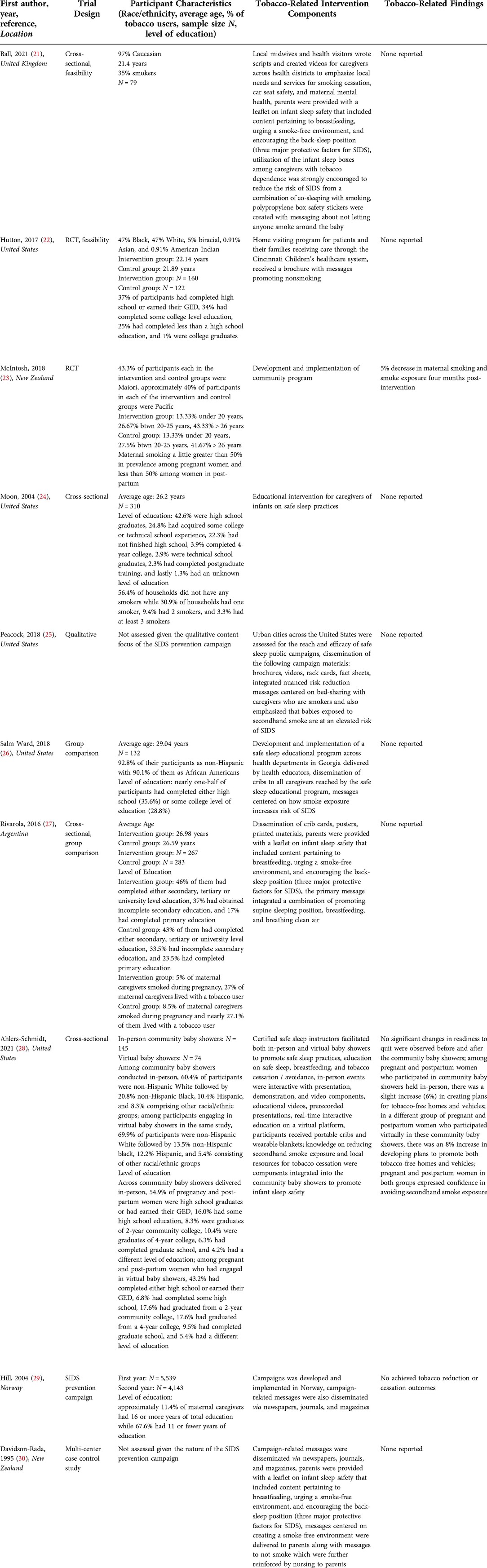
A cumulative total of 236 records were identified across the databases reviewed from the past 26 years. 110 of these records were duplicates and ultimately excluded. Among the remaining 126 records, 101 of them were subsequently excluded for one or more of the following reasons: (1) did not contain full-text articles; (2) intervention components did not involve addressing tobacco dependence; and (3) did not implement interventions. 25 remaining full-text articles were examined for inclusion in this narrative review. Fifteen of them were ultimately further excluded for the following reasons: (1) non-target population; (2) presented only a study protocol; and (3) focused on a range of pediatric illnesses outside of SIDS. Ten of them ultimately met the criteria for presenting best practices, strategies, education, and any other interventions to address tobacco use as a risk factor for SIDS as elucidated in Figure 1. Ethics or IRB approval was obtained in seven studies (21–27). A consolidated breakdown of each study's design, intervention components, and outcomes can be found in Table 2.
Sample characteristics
Sample sizes across studies ranged from 74 to 500 (21–24, 26–28). Ages of participants among studies ranged from less than 20 years to greater than 40 years (21–24, 26, 27, 29).
Deliverers of interventions
In one study, certified safe sleep instructors facilitated both in-person and virtual baby showers to promote safe sleep practices (28). In another study, local midwives and health visitors wrote scripts and created videos for caregivers across health districts to emphasize local needs and services for smoking cessation, car seat safety, and maternal mental health (21). Health educators in two studies facilitated an educational intervention for caregivers of infants on safe sleep practices (24, 26). In another study, pediatricians, neonatologists, obstetricians, residents, licensed midwives, and nurses provided information to families of infants on safe sleep practices (27).
Settings
In one study, baby showers were held both virtually and in-person across four rural counties (28). Another study recruited participants from two regions in the United Kingdom (21). In two different studies, campaigns were developed and implemented internationally in New Zealand and Norway (29, 30). Urban cities across the United States were assessed for the reach and efficacy of safe sleep public campaigns in a different study (25). Another study was also conducted in New Zealand through the development and implementation of a community-based program (23). One study involved implementing a home visiting program for patients and their families receiving care through the Cincinnati Children's healthcare system (22). Another study involved development and implementation of a safe sleep educational program across health departments in Georgia (26). A different study involved recruiting caregivers of infants in a WIC clinic at the Children's National Medical Center (24). Lastly, one study was implemented at maternity centers in Argentina (27).
Study designs
Study designs were diverse across studies and included the following: cross-sectional to assess feasibility (21, 22, 24, 27, 28), SIDS prevention campaigns (25, 29, 30), multi-center case control study (30), randomized controlled trial (22, 23), and group comparison (26, 27).
Data analyses
Data analyses across studies were primarily quantitative in nature and included the following: descriptive statistics, frequencies and percentages, McNemar tests across paired dichotomous variables, Friedman test, chi-square, paired sample t-tests, the Mann-Whitney Wilcoxon test for independent samples, Shapiro-Wilk test, linear mixed effects model, quantile-quantile plot, ratios of risk factor prevalence with stratified contingency table analysis, and logistic regression analysis (22, 23, 26–29). These analyses assessed descriptive contexts of variables as well as among pairs and groups.
One study involved conducting qualitative analyses through assessing the content of messages across campaign materials and interviews (25).
Quantitative data analyses were conducted using both SPSS (26, 28, 29) and SAS (21). Qualitative data analyses were performed with Atlas (25).
Methods of health communication
In five studies, participants were reached via messages delivered through a range of diverse mass media methods that included social media, radio advertisements, posters, billboards, printed materials (e.g., pamphlets, leaflets, stickers) and fliers (22, 25–28). In addition, participants in two studies were recruited in the community by healthcare providers as well as maternal and child health programs and health departments (28, 30). Campaign-related messages were also disseminated via newspapers, journals, and magazines in two studies (29, 30).
Provision of resources
Participants in one study received portable cribs and blankets (28). In another study, caregivers received infant sleep boxes made of polypropylene with wearable fleece baby blankets and fitted cotton sheets (21). One study involved the dissemination of cribs to all caregivers reached by the safe sleep educational program (26). In three studies, parents were provided with a leaflet on infant sleep safety that included content pertaining to breastfeeding, urging a smoke-free environment, and encouraging the back-sleep position (three major protective factors for SIDS) (21, 27, 30). In another study, the control group received a brochure with messages promoting nonsmoking (22). Baby beds were provided to participants in a different study (23).
Education
In one study, knowledge on reducing secondhand smoke exposure and local resources for tobacco cessation were components integrated into the community baby showers to promote infant sleep safety (28). In another study, utilization of the infant sleep boxes among caregivers with tobacco dependence was strongly encouraged to reduce the risk of SIDS from a combination of bed-sleeping with smoking (21). Also in this study, polypropylene box safety stickers were created with messaging about not letting anyone smoke around the baby (21). Of note, this program was conducted in the United Kingdom where there is less emphasis on discouraging bed-sharing than in the U.S. In a different study, messages centered on creating a smoke-free environment were delivered to parents along with messages to not smoke which were further reinforced by nurses to parents (30). Two campaigns in Houston, TX and Washington DC integrated nuanced risk reduction messages centered on bed-sharing with caregivers who are smokers and also emphasized that babies exposed to secondhand smoke are at an elevated risk of SIDS (25). Similarly in another study, messages centered on how smoke exposure increases risk of SIDS (26). These messages on mediating secondhand smoke exposure to promote a smoke-free and vape-free environment resonate with messages from the Safe-to-Sleep and Cribs for Kids national campaigns (31, 32). Both of these campaigns promote adherence to the AAP infant sleep safety recommendations as the basis to optimize conditions for supporting an infant in sleeping safely and soundly without risk for any adverse consequences resulting from environmental and behavioral risk factors. Each of these campaigns has a visible presence across the U.S. and has existed for greater than twenty years (31, 32). In a different study, the primary message integrated a combination of promoting supine sleeping position, breastfeeding, and breathing clean air (27).
Readiness to quit
In one study, no significant changes in readiness to quit were observed before and after the community baby showers (28).
Environmental changes
In one study among pregnant and postpartum women who participated in community baby showers held in-person, there was a slight increase (6%) in creating plans for tobacco-free homes and vehicles (28). Of note in the same study in a different group of pregnant and postpartum women who participated virtually in these community baby showers, there was an 8% increase in developing plans to promote both tobacco-free homes and vehicles (28). Pregnant and postpartum women in both groups expressed confidence in avoiding secondhand smoke exposure.
Tobacco cessation
There was no achieved tobacco reduction or cessation outcomes overall in one study that implemented a campaign across Norway (29). In fact, the prevalence of maternal smoking in the post-partum timeframe increased by approximately 3% following the campaign. Of note, among mothers who were 40 years of age and older in the same study, the prevalence of maternal smoking decreased by almost 5%. Furthermore, prevalence of maternal smoking was nearly 3.8 times higher among younger mothers than older mothers. In another study, there was a 5% decrease in maternal smoking and smoke exposure four months post-intervention (23).
Discussion
We conducted a comprehensive narrative review of ten studies that described a range of different strategies, best practices, campaigns, and programs that accounted for tobacco exposure as a risk factor for SIDS and SUID to optimize safe sleep practices among caregivers of infants. However, none of the studies accounted for tobacco exposure as a primary focus of any intervention or an integral part of any SIDS reduction interventions. Content of tobacco-related messages across most of these studies was not clearly elucidated. Furthermore in the studies with tobacco-related messages, content centered on tobacco abstinence and/or reducing secondhand smoke exposure which are in line with content across both the Safe-to-Sleep and Cribs for Kids national campaigns to promote a tobacco-free environment for infants (31, 32). Studies only offered resources on safe sleep furniture, not any resources related to tobacco reduction or cessation among caregivers. Of note, only one study revealed tobacco-related outcomes pertaining to reduction or cessation. However, all studies integrated content on tobacco dependence and exposure as intervention components. An incomplete understanding exists of strategies to address more of the modifiable risk factors that can substantially elevate the risk of infant mortality from sleep-related deaths among infants. In our review, we have characterized pertinent components of each study design and key findings across studies. Furthermore, our review delineates both strengths and limitations of existing approaches as the basis to propose recommendations for future research and practice endeavors that can account for more environmental and behavioral determinants of SIDS and SUID inclusive of tobacco exposure.
Limitations in resource provision
Of note, none of the studies involved provision of concrete tobacco cessation resources (e.g Nicotine Replacement Therapy products, referrals to tobacco treatment clinics, concurrent substance use and mental health treatment, etc.). The only concrete resources supplied across studies were cribs, boxes, pack-n-plays, and baby beds (21, 23, 26, 28). These resources address a couple of the AAP Safe Sleep recommendations for building a safe sleep environment for infants with firm sleep surfaces which seek to promote supine sleeping position and eliminate soft objects, loose bedding, and bed sharing. It is crucial for future interventions to also provide resources that can address more of the prescribed environmental recommendations inclusive of tobacco exposure.
Delimitations of interventions
In addition across interventions, not only were resources supplied pertaining to safe sleep surfaces for infants, most interventions also heavily focused time and consideration on addressing unsafe sleep surfaces as a risk factor for SIDS and SUID. It is imperative to note that there are a range of significant preventable risk factors that can elevate an infant's risk of mortality from sleep-related causes that include tobacco exposure which can compromise the infant's airway and create subsequent complications in breathing that can be life-threatening.
Findings across these studies as well as through prior national infant safe sleep campaigns elucidate that tobacco reduction and cessation are not emphasized enough to reduce the risk of infant deaths postnatally attributed to behavioral and environmental determinants. Minimizing tobacco exposure is one of the guidelines published in 2022 by the American Academy of Pediatrics to optimize infant sleep safety. Oftentimes, postnatal care does not involve tobacco reduction or cessation care that was initiated prenatally. In turn, we are recommending that future work account for these outcomes.
In fact to date, there has not been a single intervention that has either exclusively or significantly focused on tobacco use as a modifiable risk factor for sleep-related infant deaths. Designing a comprehensive intervention that accounts for the complete range of behavioral and environmental determinants will likely mitigate the risk of infant mortality on a larger scale by addressing all potential preventable causes of them.
Sources of environmental tobacco exposure
Of note, only two studies assessed whether there were any additional tobacco users at home (24, 27). It is important for future studies to identify all sources of environmental smoke exposure as the basis to mitigate them and thereby contribute towards the goal of SIDS and SUID reduction to subsequently decrease the rate of infant mortality.
Children's literature
In one study among the intervention group, a children's book was published and include content on safe sleep recommendations (22). This book was narrative in nature and integrated a wealth of descriptive strategies on creating a healthy and safe sleep environment for infants. Of note, this book did not include any content on addressing smoke exposure as a threat to the safety of infants. The control group in this study received brochures with messages about not smoking. As previously mentioned, addressing tobacco exposure is one of the AAP's safe sleep recommendations. The fact that it was not accounted for suggests minimal importance of it and contributes to the knowledge gap in understanding and addressing the range of environmental determinants that surround the increased risk of SIDS and SUID. Children's books offer creative opportunities to engage caregivers of infants that include parents, grandparents, extended family members, child care providers, foster families and any other legal guardians of children. Future books could illustratively account for smoke exposure alongside additional safe sleep recommendations to engage this caregiver population and heighten their knowledge and awareness of more risk factors for sleep-related infant deaths.
Tobacco control policies and legislation
Tobacco control measures have the potential to be effective in the form of legislation, taxation and social engineering. Findings from the World Health Organization's MPOWER report uncovered that 23 countries (Seychelles, Mauritius, Costa Rica, Brazil, Panama, Surinam, Colombia, Canada, Uruguay, Argentina, United Kingdom, Turkey, Portugal, Russia, Ireland, Romania, Estonia, Denmark, Spain, Norway, Iran, Australia and New Zealand) obtained the highest scores with respect to the implementation and enforcement of their tobacco control policies and legislation including smoke-free regulations, advertising bans, taxation, and uptake in the visibility of health warnings on cigarette packages (33). For example in Norway, smoking is entirely prohibited. Ever since the tobacco prohibition was implemented across restaurants, public transport, schools, healthcare institutions, as well as across all public office spaces in 2004, the prevalence of smoking in pregnancy has significantly decreased from 26% in 1999 to nearly 2% in 2021 (34). After the enactment of smoke-free legislation in Brazil, the average infant mortality rate declined substantially from 24.5 to 13.0 deaths per 1,000 live births from 2000 to 2016. During this time, the neonatal mortality in Brazil declined from 15.6 to 9.0 deaths per 1000 live births (35). It follows that integration of these tobacco control measures could also translate to addressing tobacco-related components of sleep-related infant deaths on a continuum from prenatal to postnatal care.
Program expansion recommendations
There were several studies that involved development and implementation of community programs to address risk factors for SIDS and SUID as the basis to decrease preventable infant deaths (22, 23, 26). All of these interventions were implemented postnatally. Future endeavors could involve consideration of integrating tobacco dependence treatment in SIDS reduction approaches prenatally that could extend post-birth on a continuum for caregivers which could also heighten focus on tobacco-related outcomes both prenatally and postnatally. As previously mentioned, not a single study involved provision of tobacco cessation resources including medications, counseling, and referrals to tobacco treatment clinics. It is crucial for future programs to account for these resources as the basis to more comprehensively address more risk factors for infant mortality from sleep-related causes and follow as many AAP Safe Sleep recommendations as possible. Furthermore, accounting for cultural considerations, patient and family preferences, and varying degrees of health literacy can also reach and engage more subgroups within the target population of these diverse caregivers. Of note, cultural groups vary in their perspectives on what a safe sleep environment looks like (e.g., with respect to safe sleep furniture, severity of tobacco exposure, etc). Community programs can reach increasingly more caregivers who could benefit from these resources, inform delivery of care in line with the goals, values, and preferences of these caregivers, and in turn contribute towards decreasing the rate of infant mortality attributed to environmental and behavioral risk factors.
Campaign-building recommendations
Several studies involved the development and implementation of campaigns to heighten knowledge and awareness of SIDS across a range of both traditional and nontraditional sources of media (25, 29, 30). It is unclear about the totality of messages delivered through this campaign and specifically with respect to tobacco-related messages as part of creating a safe sleep environment for infants. Among the messages shared in these studies, tobacco-related content centered on promoting smoke-free homes and vehicles and minimizing secondhand smoke exposure – both informational appeals similar in nature to the Safe-to-Sleep and Cribs for Kids national campaigns. Perhaps accounting for messages containing fear-based and emotional/psychological appeals in line with some of the well-known tobacco cessation campaigns (e.g., the CDC Tips from Former Smokers and the FDA's Every Try Counts and the Real Cost) along with tips and strategies to quit could be helpful in future campaigns to address tobacco exposure as a risk factor for SIDS (36–39). However before integrating any of these appeals into future endeavors, it is crucial to test each of them prior to implementation given the implication that this typology of intervention has the potential to be traumatic for caregivers. Furthermore, these campaigns have extended onto social media platforms that in turn increase the global reach for caregivers who comprise the primary target population for these campaigns. It follows that addressing more SIDS-related risk factors through the dissemination of messages across community, national, and global infant safe sleep campaigns could ultimately seek to reduce SIDS and SUID as part of the leading causes of infant mortality across the world.
Limitations of this narrative review
This review's primary limitation is that we did not conduct a systematic review with meta-analyses. The narrative design of this review was more descriptive and qualitative in nature and in turn did not involve conducting composite statistical analyses. These limitations delimited rigorous examination of study biases. It follows that we could not critically assess whether any of the interventions, strategies, and practices pertaining to addressing tobacco exposure as a risk factor for SIDS could be directly related to health outcomes for infants and their caregivers. Lastly, we reviewed studies only published in English which could certainly be another limiting factor of this review.
Conclusions
Existing interventions to mitigate sleep-related infant deaths do not account for more of the AAP Safe Sleep recommendations and delimit the reach and scope of their interventions with their focus on exclusive risk factors for SIDS and SUID. It is crucial for future interventions to account for the depth and breadth of more risk factors that are modifiable and could contribute towards the larger goal of reducing infant mortality overall by decreasing the risk of infant deaths attributed to sleep-related causes. More methods of health communication could focus content on emotional/psychological and fear-based appeals along with tips and strategies to promote tobacco cessation as a safe sleep recommendation alongside optimization of additional environmental and behavioral determinants constituting safe sleep practices. Children's books, programs, and campaigns offer unique opportunities to reach caregivers of infants and heighten their knowledge and awareness on SIDS and SUID reduction.
Author contributions
Conceptualization, AJ; methodology, AJ; writing—original draft preparation, AJ; writing—review and editing, AJ and MJ. All authors contributed to the article and approved the submitted version.
Funding
This research was supported by an award from GlaxoSmithKline that paid for the APC. Funds from GlaxoSmithKline were not used to support salary or any other element in the development of the manuscript
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion. Sudden unexpected infant death and sudden infant death syndrome. Atlanta, GA, USA: Centers for Disease Control and Prevention (2022).
2. Centers for Disease Control and Prevention. Sudden Unexpected Infant Death and Sudden Infant Death Syndrome. (2020). Availabler at: https://www.cdc.gov/sids/data.htm
3. Krous HF, Beckwith JB, Byard RW, Rognum TO, Bajanowski T, Corey T, et al. Sudden infant death syndrome and unclassified sudden infant deaths: a definitional and diagnostic approach. Pediatrics. (2004) 114:234–8. doi: 10.1542/peds.114.1.234
4. Moon RY, Carlin RC, Hand I. The task force on sudden infant death syndrome and the committee on fetus and newborn; sleep-related infant deaths: updated 2022 recommendations for reducing infant deaths in the sleep environment. Pediatrics. (2022) 150:e2022057990. doi: 10.1542/peds.2022-057990
5. Filiano JJ, Kinney HC. A perspective on neuropathologic findings in victims of the sudden infant death syndrome: the triple-risk model. Biol Neonate. (1994) 65:194–7. doi: 10.1159/000244052
6. Ahn YM, Yang K, Ha HI, Cho JA. Cultural variation in factors associated with sudden infant death during sleep. BMC Pediatr. (2021) 21:1–13. doi: 10.1186/s12887-021-02894-8
7. Rayfield S, Plugge E. Systematic review and meta-analysis of the association between maternal smoking in pregnancy and childhood overweight and obesity. J Epidemiol Community Health. (2017) 71:162–73. doi: 10.1136/jech-2016-207376
8. Anderson ME, Johnson DC, Batal HA. Sudden infant death syndrome and prenatal maternal smoking: rising attributed risk in the back to sleepera. BMC Med. (2005) 3:1–7. doi: 10.1186/1741-7015-3-4
9. Avşar TS, McLeod H, Jackson L. Health outcomes of smoking during pregnancy and the postpartum period: an umbrella review. BMC Pregnancy Childbirth. (2021) 254:1–9. doi: 10.1186/s12884-021-03729-1
10. Hakeem GF, Oddy L, Holcroft CA, Abenhaim HA. Incidence and determinants of sudden infant death syndrome: a population-based study on 37 million births. World J Pediatr. (2015) 11:41–7. doi: 10.1007/s12519-014-0530-9
11. Salm Ward TC, Balfour GM. Infant safe sleep interventions, 1990-2015: a review. J Community Health. (2016) 41:180–96. doi: 10.1007/s10900-015-0060-y
12. Been JV, Sheikh A. Tobacco control policies in relation to child health and perinatal health outcomes. Arch Dis Child. (2018) 103:817–9. doi: 10.1136/archdischild-2017-313680
13. Jawed A, Jassal M. Hard to reach or just not enough? A narrative review of inpatient tobacco cessation programs in pediatrics. Int J Environ Res Public Health. (2021) 18:13423. doi: 10.3390/ijerph182413423
14. Sapru S, Vardhan M, Li Q, Guo Y, Li X, Saxena D. E-cigarettes use in the United States: reasons for use, perceptions, and effects on health. BMC Public Health. (2020) 20:1–10. doi: 10.1186/s12889-020-09572-x
15. Mawick A, Pfeiffer H, Vennemann M. Sudden infant death syndrome: deletions of glutathione-S-transferase genes M1 and T1 and tobacco smoke exposure. Int J Leg Med. (2021) 135:1375–83. doi: 10.1007/s00414-021-02556-5
16. Haglund B, Cnattingius S. Cigarette smoking as a risk factor for sudden infant death syndrome: a population-based study. Am J Public Health. (1990) 80:29–32. doi: 10.2105/AJPH.80.1.29
17. Blair PS, Fleming PJ, Bensley D, Smith I, Bacon C, Taylor E, et al. Smoking and the sudden infant death syndrome: results from 1993 to 5 case-control study for confidential inquiry into stillbirths and deaths in infancy confidential enquiry into stillbirths and deaths regional coordinators and researchers. Br Med J. (1996) 313:198. doi: 10.1136/bmj.313.7051.195
18. Mitchell EA, Ford RPK, Stewart AW, Taylor BJ, Becroft DMO, Thompson JMD, et al. Smoking and the sudden infant death syndrome. Pediatrics. (1993) 91:893–6. doi: 10.1542/peds.91.5.893
19. Schoendorf KC, Kiely JL. Relationship of sudden infant death syndrome to maternal smoking during and after pregnancy. Pediatrics. (1992) 90:905–8. doi: 10.1542/peds.90.6.905
20. Amiri S, Saadat SH. Smoking and smoking relapse in postpartum: a systematic review and meta-analysis. Addict Disord Their Treat. (2021) 20:486–99. doi: 10.1097/ADT.0000000000000282
21. Ball HL, Taylor CE, Yuill CM. A box to put the baby in: uK parent perceptions of two baby box programmes promoted for infant sleep. Int J Environ Res Public Health. (2021) 18:1–13. doi: 10.3390/ijerph182111473
22. Hutton JS, Gupta R, Gruber R, Berndsen J, DeWitt T, Ollberding NJ, et al. Randomized trial of a children’s book versus brochures for safe sleep knowledge and adherence in a high-risk population. Acad Pediatrics. (2017) 17:879–86. doi: 10.1016/j.acap.2017.04.018
23. McIntosh C, Trenholme A, Stewart J, Vogel A. Evaluation of a sudden unexpected death in infancy intervention programme aimed at improving parental awareness of risk factors and protective infant care practices. J Paediatr Child Health. (2018) 54:377–82. doi: 10.1111/jpc.13772
24. Moon RY, Oden RP, Grady KC. Back to sleep: an educational intervention with women, infants, and children program clients. Pediatrics. (2004) 113:542–7. doi: 10.1542/peds.113.3.542
25. Peacock NR, Altfeld S, Rosenthal AL, Garland CE, Massino JM, Smith SL, et al. Qualitative analysis of infant safe sleep public campaign messaging. Health Promot Pract. (2018) 19:203–12. doi: 10.1177/1524839917690339
26. Salm Ward TC, McClellan MM, Miller TJ, Brown S. Evaluation of a crib distribution and safe sleep educational program to reduce risk of sleep-related infant death. J Community Health. (2018) 43:848–55. doi: 10.1007/s10900-018-0493-1
27. Rivarola MR, Reyes P, Henson C, Bosch J, Atchabahian P, Franzosi R, et al. Impact of an educational intervention to improve adherence to the recommendations on safe infant sleep. Arch Argent Pediatr. (2016) 114:223–31. doi: 10.5546/aap.2016.eng.223
28. Ahlers-Schmidt CR, Schunn C, Hervey AM, Torres M, Nelson JEV. Promoting safe sleep, tobacco cessation, and breastfeeding to rural women during the COVID-19 pandemic: quasi-experimental study. JMIR Pediatr Parent. (2021) 4:e31908. doi: 10.2196/31908
29. Hill SAR, Hjelmeland B, Johannessen NM, Irgens LM, Skjaerven R. Changes in parental risk behavior after an information campaign against sudden infant death syndrome (SIDS) in Norway. Acta Paediatr. (2004) 93:250–4. doi: 10.1111/j.1651-2227.2004.tb00715.x
30. Davidson-Rada J, Caldis S, Tonkin SL. New Zealand’s SIDS prevention program and reduction in infant mortality. Health Educ Q. (1995) 22:162–71. doi: 10.1177/109019819502200205
31. National Institutes of Health. Safe to Sleep Public Education Campaign Led by NIH Eunice Kennedy Shriver National Institute of Child Health and Human Development. (2022). Available at: https://safetosleep.nichd.nih.gov/activities/campaign
32. Cribs for Kids. (2022). Available at: https://cribsforkids.org/
33. Heydari G. Which countries are the best in tobacco control? A quantitative analysis of the MPOWER 2017. J Glob Health Rep. (2019) 3:e2019039. doi: 10.29392/joghr.3.e2019039
34. The Norwegian Institute of Health. (2022). Available at: https://www.fhi.no/en/
35. Hone T, Szklo AS, Filippidis FT, Laverty AA, Sattamini I, Been JV, et al. Smoke-free legislation and neonatal and infant mortality in Brazil: longitudinal quasi-experimental study. Tob Control. (2020) 29:312–9. doi: 10.1136/tobaccocontrol-2019-054923
36. Murphy-Hoefer R, Davis KC, King BA, Beistle D, Rodes R, Graffunder C. Association between the tips from former smokers campaign and smoking cessation among adults, United States, 2012–2018. Prev Chronic Dis. (2020) 17:E97. doi: 10.5888/pcd17.200052
37. Davis KC, Patel D, Shafer P, Duke J, Glover-Kudon R, Ridgeway W, et al. Association between media doses of the tips from former smokers campaign and cessation behaviors and intentions to quit among cigarette smokers, 2012-2015. Health Educ Behav. (2017) 45:52–60. doi: 10.1177/1090198117709316
38. Xu X, Alexander RL, Simpson SA, Goates S, Nonnemaker JM, Davis KC, et al. A cost-effectiveness analysis of the first federally funded antismoking campaign. Am J Prev Med. (2014) 48:318–25. doi: 10.1016/j.amepre.2014.10.011
39. U.S. Food & Drug Administration. FDA launches new campaign: “The Real Cost” youth e-cigarette prevention campaign. (2020). Available at: https://www.fda.gov/tobacco-products/public-health-education-campaigns/real-cost-campaign
Keywords: sudden unexpected infant death, sudden infant death syndrome, infant safe sleep, tobacco, infant mortality, pediatrics
Citation: Jawed A and Jassal M (2022) When there is no air, the cradle will fall: A narrative review of tobacco-related content across infant safe sleep interventions. Front. Pediatr. 10:994702. doi: 10.3389/fped.2022.994702
Received: 15 July 2022; Accepted: 17 November 2022;
Published: 5 December 2022.
Edited by:
Steven Hirschfeld, Uniformed Services University of the Health Sciences, United StatesReviewed by:
Torleiv Rognum, University of Oslo, NorwayBryanne Colvin, Washington University in St. Louis, United States
© 2022 Jawed and Jassal. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Aysha Jawed YWphd2VkMUBqaG1pLmVkdQ==
Specialty Section: This article was submitted to Children and Health, a section of the journal Frontiers in Pediatrics
 Aysha Jawed
Aysha Jawed Mandeep Jassal
Mandeep Jassal