
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr., 10 October 2022
Sec. Pediatric Infectious Diseases
Volume 10 - 2022 | https://doi.org/10.3389/fped.2022.994675
This article is part of the Research TopicChildhood Vaccination and COVID-19View all 17 articles
Background: There was a considerably slower uptake among children despite the high COVID-19 vaccination uptake amongst adults and adolescents in Singapore. This was concerning as unvaccinated children are at risk of severe COVID-19 infections and a source and reservoir of infections. We sought to understand the impact of social media on parental vaccine hesitancy and to determine the risk factors associated with vaccine hesitancy.
Methods: An electronic survey conducted from November 2021 to March 2022. Data on the demographic profiles of respondents and to classify them based on their vaccine hesitancy status. Data including the choice of social media used to obtain information on the COVID-19 pandemic, frequency of use were collected. Statistical significance was defined as p < 0.05.
Results: Six hundred and twenty-eight parents participated. 66.9% of parents were not vaccine hesitant. About a third (27.2%) considered themselves somewhat vaccine hesitant. Fathers were more vaccine hesitant than mothers. Vaccine hesitancy was also associated with having a lower household income, unvaccinated parents, knowing someone with an adverse reaction to the Covid 19 vaccine and having a low level of trust in their child's doctor. There was no significant difference with high usage of social media between parents who were not vaccine hesitant vs. those who were vaccine hesitant. Despite high usage of social media, about two thirds (62.7%) of parents preferred print material to obtain COVID-19 related information. Parental trust in their child's doctor was the most significant factor in determining vaccine hesitancy amongst parents. When the variables of gender, household income status, vaccine status were further analysed with a multinomial logistic regression model, vaccine hesitancy in a parent could be predicted with a 70% accuracy, and non-vaccine hesitancy with a 92.4% accuracy.
Conclusion: Newspapers and print media were the primary sources used in obtaining information on COVID-19 vaccine safety and efficacy, especially amongst parents with a higher household income. Healthcare providers should continue to establish rapport amongst parents, in particular the group with a lower household income to encourage higher paediatric COVID-19 vaccine uptake as well as correct COVID-19 related vaccine misconceptions or vaccine hesitancy, if present.
COVID-19 has had an immense impact on human health worldwide, with close to 600 million confirmed infections worldwide at the time of writing in August 2022 (1). While acute infections have claimed more than 6 million lives, post-acute sequelae of SARS-CoV-2 infection has also had both health and economic impacts. On 31st December 2020, the World Health Organisation (WHO) approved the emergency use of COVID-19 vaccines for adults during the COVID-19 pandemic (2). Despite the availability of the COVID-19 vaccines, vaccine hesitancy remained prevalent in many countries, limiting the success of COVID-19 vaccination programmes worldwide (3–6). This contributed to the COVID-19 pandemic and the advent of more potential virus mutant populations. By December 2021, the Singapore Ministry of Health had also approved the use of Paediatric Dose Pfizer-BioNTech/Comirnaty vaccine for children aged 5–11 years (7). However, the uptake of paediatric COVID-19 vaccination was significantly slower compared to the adult and adolescent COVID-19 vaccination drive (8). This was a worrying trend as unvaccinated children were found to be twice as likely to get hospitalised as compared to vaccinated children (9).
This trend was also observed in the United States of America (USA), where vaccinated adults were less likely to consent to have their children vaccinated against COVID-19 (10). A Bangladeshi study showed that parental vaccine hesitancy could be as high as 42.8% (11). Other Asian countries also demonstrated that parental hesitancy relatively lower at 10.8%–11.8%, in Taiwan and Vietnam respectively (12, 13). Studies in the United Kingdom (UK) have shown that higher social media and digital device usage among parents have been associated with greater hesitancy in vaccinating their children against COVID-19 (14). Additionally, social media use could also lead to a potentially higher likelihood of exposure to COVID-19 misinformation (15). A survey on the use of social media in Singapore estimated that 79.1% the population used some form of social media, wherein the more popular choices of social media were YouTube, Facebook and Instagram (16). Hence, social media usage could have a significant influence on COVID-19 vaccine hesitancy amongst Singaporean parents (17).
In this study, we aimed to compare the social and demographic features of parents with and without hesitancy towards vaccines administration in their offspring. Secondly, we also aimed to determine the impact of social media and device usage by parents in Singapore on COVID-19 vaccine hesitancy. Using the risk factors associated with vaccine hesitancy in parents found in our study, we developed a multinomial logistic regression model to predict COVID-19 vaccine hesitancy amongst parents.
A prospective, anonymous and voluntary electronic survey modified from “Measuring vaccine hesitancy: The development of a survey tool” was used (18, 19) (Supplementary Table).
The survey was conducted between 12 November 2021 and 5 March 2022 through FormSG, a secure electronic platform. The study was publicised on the official social media platforms of the National University Hospital of Singapore (NUH) and disseminated via email to hospital staff. Posters with QR codes to access the electronic survey were also placed strategically around the hospital, including the Paediatrics and Obstetrics wards and outpatient clinics. Respondents had to be at least 21 years old and be parents. No compensation was provided to the study participants for participating in the study.
This study was approved by the National Healthcare Group Domain Specific Ethics Board (NHG DSRB Domain B, Reference No. 2021- 00900) in Singapore.
Demographic data of respondents and their children was obtained. Time spent on social media (including Facebook, YouTube, Twitter, Weibo, Instagram) and total device usage per week were self-reported by the participants, and then classified as either high or low usage; high usage being defined as more than 12 h per week of social media use and/or 6 h per day of device use. Vaccine hesitancy was a self-assessed variable. Results were analyzed using Chi-square for categorial data and regression analysis was also performed with Statistical Programme for Social Sciences (SPSS), IBM version 27. Statistical significance was defined to be 2-sided when p < 0.05.
Table 1 shows the demographic data of the 628 parents who participated in the survey. More than two thirds (69.1%) were mothers, with a median of 2 children. Majority (90.1%) had at least pre-university education and were married (90.6%). The median family income bracket of participants were $4,000–$9,999 Singapore dollars per month (1 USD = 1.35 Singapore dollars), which corresponded to the median income of the Singaporean household (Department of Statistics, Singapore). More than two thirds (72.1%) of the respondents were Singaporeans. The modal housing types were 4 to 5 room Housing Development Board (HDB) flats (i.e., public housing) or executive condominiums. With regards to the parents' COVID-19 vaccine status, majority (99.2%) had received at least a dose of the COVID-19 vaccine. 61.4% had at least 1 child eligible for paediatric COVID-19 vaccine and 27.6% had at least 1 adolescent eligible for vaccine. Social media use in the respondents were reported to be 1 to 12 h per week with 1 to 6 h per day on digital devices. They also spent a mode of less than an hour on television every day (Table 2).
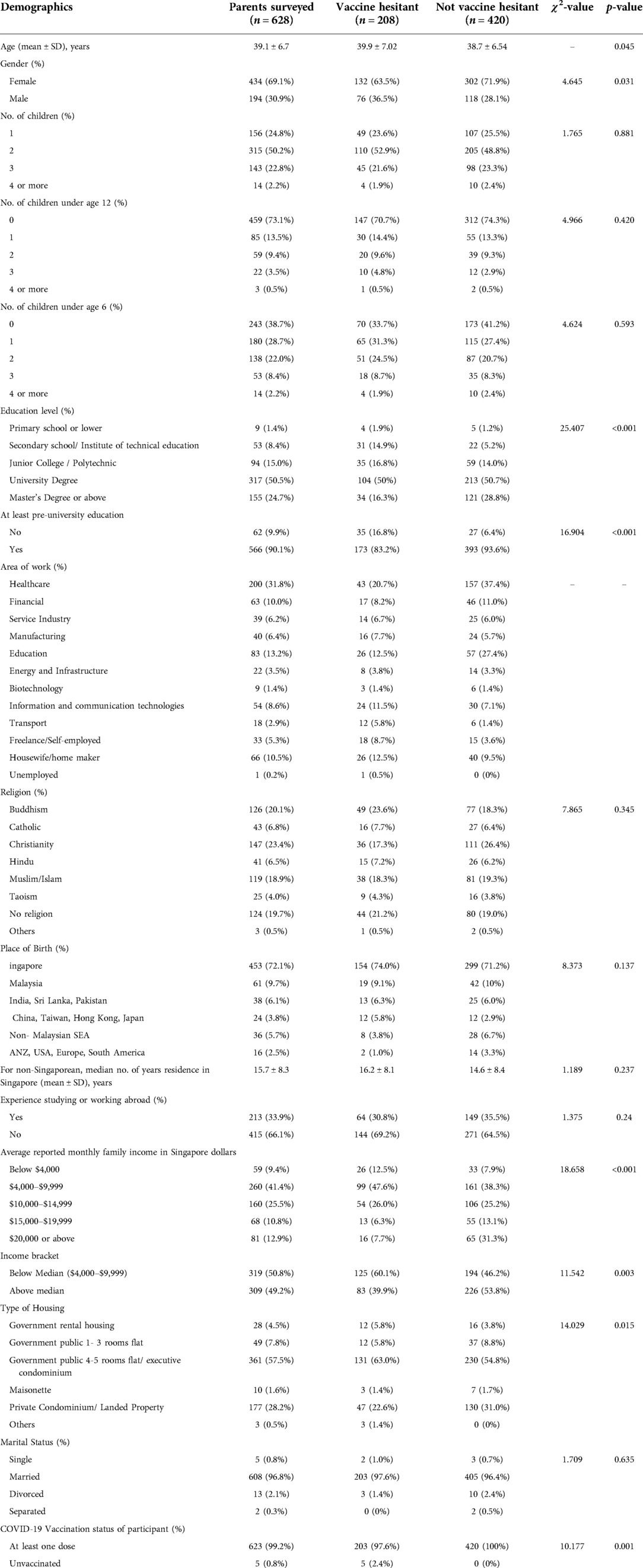
Table 1. Demographics of participants and comparison of the vaccine hesitant vs. non-hesitant parents.
Two thirds of the respondents (66.9%) identified as not vaccine hesitant. A third (27.2%) considered themselves somewhat hesitant towards childhood vaccination.
Mothers were less vaccine hesitant than fathers (71.9% vs. 63.5%, p < 0.05; Table 1). Vaccine hesitancy was significantly associated with lower education level, lower household income as well as being unvaccinated for COVID-19. There was no difference with high usage of social media and device use between both groups.
Majority (91.6%) acknowledged that they could make shared parental decisions with their children's doctor and discuss their concerns openly. More than half (59.6%) trusted their child's doctor fully while 39.8% reported that they somewhat trusted their doctor. Childhood vaccine hesitant parents were less likely to trust their child's doctor compared to parents who were not vaccine hesistant (41.8% vs. 68.3%, p < 0.001; Table 2).
Parents reported that the more common sources of COVID-19 related updates were from printed media (i.e., newspapers) (62.7%) and then Facebook (56.8%) and Instagram (24.8%) (Figure 1). Twitter and Weibo were the less likely to be used among respondents to obtain updates. YouTube and Instagram were also used infrequently.
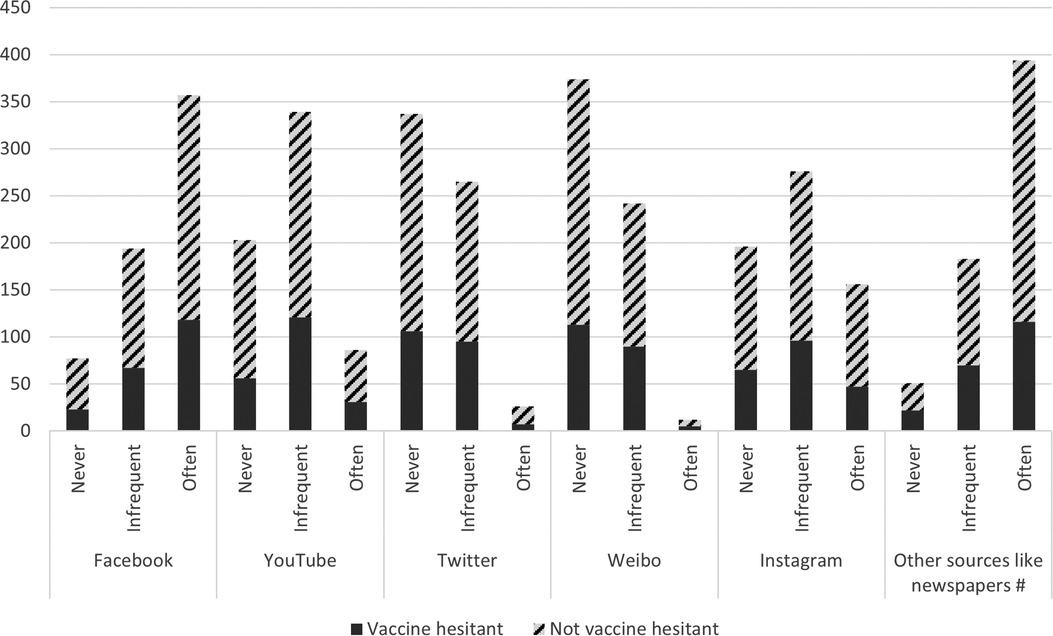
Figure 1. Frequency of use of social media, newspapers or other print materials and television to obtain information about COVID-19 for all parents.
There was no difference between vaccine hesitant and non-hesitant parents in their use of social media to obtain information about the COVID-19 pandemic. However, parents who were not vaccine hesitant were more likely to use other sources such as newspapers frequently to obtain COVID-19 related information as compared to vaccine hesitant parents. (66.2% vs. 55.8%, p < 0.01).
Vaccine hesitant parents who had an education level of pre-university level and below, were less likely to use printed media to obtain COVID-19 related information. (80.6% vs. 91.0%, p < 0.05).
Almost half (46.2%) of respondents knew someone with a bad reaction to the vaccine personally. They were also more likely to be vaccine hesitant (57.2% vs. 40.5%, p < 0.01) as compared to parents who did not personally know anyone with a bad reaction to the vaccine.
Using the various associated risk factors identified in Table 3, a logistic regression model was formed. Trust in their child's doctor was found to be the most significant factor influencing a parent's decision in childhood vaccination. Knowing someone with a bad vaccine reaction, gender of respondents and housing type were not statistically significant when the regression model was used.
When the variables of gender, household income status, vaccine status were further analysed with a multinomial logistic regression model, vaccine hesitancy in a parent could be predicted with a 70% accuracy, and non-vaccine hesitancy with a 92.4% accuracy.
This is a multi-ethnic study done in Southeast Asia which lends a unique perspective of parental values in vaccinating their children against COVID-19. In our study, vaccine hesitancy in parents was found to be correlated with being a father, lower household income levels, parents' own unvaccinated status with a 92.4% accuracy. These associations may allow healthcare workers in identifying and tailoring their approach in making shared parental decision making with parents who may be vaccine hesitant.
A key finding by our study which could impact the rate of vaccination uptake amongst the paediatric population is the importance of parental trust in their children's primary healthcare provider. This was identified as the most significant factor contributing to the COVID-19 vaccine uptake amongst parents in our study. In fact, the COVID-19 National Preparedness Collaborators had identified that a high level of trust is not only associated with higher vaccine uptake but also lower levels of infection rates during the pandemic (20). We recommend that healthcare providers opportunistically discuss vaccine safety during routine healthcare encounters, to guide parents in making informed decisions regarding COVID-19 vaccination for their children.
Our findings suggest that parents with lower household incomes were more comfortable using social media as opposed to print material as a sole source of information. In contrast, despite the relatively high usage of social media and digital devices in Singapore, parents with a higher level of education preferred to obtain information regarding COVID-19 vaccines from newspaper and print material rather than social media. Thus, to ensure that critical information on vaccine safety is disseminated across all socioeconomic strata, the medium through which information is provided is important. Our findings suggest that a multi-pronged approach including different media forms directed at different socioeconomic groups would be necessary for a successful vaccine information campaign.
Our findings of the influence of social media and device usage contradicts that of findings reported by other studies (12, 13, 20–24). In our study, high usage of digital devices and social media use did not influence the vaccination choices made by parents in Singapore. These findings are contrary to the findings reported by the European and American adults as well as Japanese parents. One explanation for this is that supplementing social media usage with consumption of print media decreased vaccine hesitancy in the parents in our study, thus highlighting that it may not be the usage of social media but the exclusive reliance on social media for health information that leads to high vaccine hesitancy. Another explanation is that it may not be the usage of formal or informal sources of information, but rather than level of trust that an individual puts in the sources, which is more highly predictive of vaccine hesitancy (24). Hence, the availability of reliable vaccine safety information through mainstream news media could play an additive role in supplementing social media users with information that encourages parents to vaccinate their children, thus increasing COVID-19 vaccine uptake.
Due to our convenient sampling of parents from the hospital, there was an over-representation of those working in healthcare, as well as those who consult medical professionals for health issues. In addition, we expect that unvaccinated parents may be under-represented, as they may be less inclined to fill up a survey about vaccines. Taken together, our study may under-estimate vaccine hesitancy among parents in Singapore. Finally, as with self-reported surveys, there is a possibility of recall bias resulting in over- or underestimation of the events reported. A bigger study including other Asian societies with diverse socio-economic backgrounds will allow for further exploration of the problem of vaccine hesitancy, which has been identified by the World Health Organisation to be a key threat to human health.
In conclusion, newspaper and print media with reliable vaccine safety information appears to be a useful tool in educating parents about vaccine safety and efficacy, especially among highly educated parents in Singapore. Trust in the child's doctor was found to be a significant factor in childhood vaccine hesitancy.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by National Healthcare Group Domain Specific Ethics Board (NHG DSRB Domain B, Reference No. 2021- 00900). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
JML, YZ and LYL contributed to the conception and design of the study. CWTS, TAP and LYL collected, cleaned and verified the data. CWTS, YZ and LYL jointly wrote the first draft of the manuscript. All authors contributed to the article and approved the submitted version.
JML received funding from Khoo Teck Puat – National University Children's Medical Institute (KTP-NUCMI) to conduct this research.
The authors would like to thank the NUHS paediatric department administrative staff, the NUHS corporate communications staff, the staff and nurses in the clinics of Khoo Teck Puat –National University Children's Medical Institute, National University Health System, Singapore, for their support and assistance, despite their tireless fight in the COVID-19 pandemic. We would also like to thank all the parents who had participated in the survey for their invaluable time and patience to complete this survey. Lastly, we would like to thank Ms Sheena Nishanti Ramasamy for her assistance with manuscript formatting and submission.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2022.994675/full#supplementary-material.
1. World Health Organization. WHO coronavirus (COVID-19) dashboard (2022). Available from: https://covid19.who.int/?mapFilter=vaccinations (Accessed August 22, 2022).
2. World Health Organization (WHO). WHO issues its first emergency use validation for a COVID-19 vaccine and emphasizes need for equitable global access (2020). Available from: https://www.who.int/news/item/31-12-2020-who-issues-its-first-emergency-use-validation-for-a-covid-19-vaccine-and-emphasizes-need-for-equitable-global-access (Accessed April 13, 2022).
3. Alfieri NL, Kusma JD, Heard-Garris N, Davis MM, Golbeck E, Barrera L, et al. Parental COVID-19 vaccine hesitancy for children: vulnerability in an urban hotspot. BMC Public Health. (2021) [cited 2021 Oct 28] 21(1):1662. doi: 10.1186/s12889-021-11725-5
4. Zhang M-X, Lin X-Q, Chen Y, Tung T-H, Zhu J-S. Determinants of parental hesitancy to vaccinate their children against COVID-19 in China. Expert Rev. Vaccines. (2021) [cited 2021 Oct 5] 20:1339–49. doi: 10.1080/14760584.2021.1967147
5. Schwarzinger M, Watson V, Arwidson P, Alla F, Luchini S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Health. (2021) 6(4):e210–21. doi: 10.1016/S2468-2667(21)00012-8
6. Hamdan B, Singh M, Polavarapu S, Jordan M, / Melhem TR, M N. COVID-19 vaccine hesitancy among university students in Lebanon. Epidemiol Infect. (2021) 149:e242. doi: 10.1017/S0950268821002314
7. Ministry of Health (MOH) Singapore. Expert Committee on COVID-19 vaccination recommends using the paediatric dose Pfizer-BioNTech/Comirnaty vaccine for children aged 5–11 years and extending booster vaccination to persons aged under 30 years [News Highlight); (2022). Available from: https://www.moh.gov.sg/news-highlights/details/expert-committee-on-covid-19-vaccination-recommends-using-the-paediatric-dose-pfizer-biontech-comirnaty-vaccine-for-children-aged-5-11-years-and-extending-booster-vaccination-to-persons-aged-under-30-years (Accessed March 2, 2022)).
8. Ministry of Health (MOH) Singapore. Vaccination Statistics (2022). Available from: https://www.moh.gov.sg/covid-19/vaccination/statistics (Accessed March 2, 2022).
9. Shi DS, Whitaker M, Marks KJ, Anglin O, Milucky J, Patel K, et al. Hospitalizations of children aged 5–11 years with laboratory-confirmed COVID-19 — COVID-NET, 14 states, march 2020–February 2022. MMWR Morb Mortal Wkly Rep. (2022) 71:574–81. doi: 10.15585/mmwr.mm7116e1
10. Rane MS, Robertson MM, Westmoreland DA, Teasdale CA, Grov C, Nash D. Intention to vaccinate children against COVID-19 among vaccinated and unvaccinated US parents. JAMA Pediatr. (2022) 176(2):201–3. doi: 10.1001/jamapediatrics.2021.5153
11. Ali M, Ahmed S, Bonna AS, Sarkar A-S, Islam MA, Urmi TA, et al. Parental coronavirus disease vaccine hesitancy for children in Bangladesh: a cross-sectional study [version 2; peer review: 3 approved]. F1000Res. (2022) 11:90. doi: 10.12688/f1000research.76181.1
12. Allington D, McAndrew S, Moxham-Hall VL, Duffy B. Media usage predicts intention to be vaccinated against SARS-COV-2 in the US and the UK. Vaccine. (2021) 39:18. doi: 10.1016/j.vaccine.2021.02.054
13. Science Daily. Social media use increases belief in COVID-19 misinformation, survey finds. (2020). Available from: www.sciencedaily.com/releases/2020/12/201214090118.htm (Accessed February 27, 2022).
14. Tsai CS, Hsiao RC, Chen YM, Yen CF. Factors related to caregiver intentions to vaccinate their children with attention-deficit/hyperactivity disorder against COVID-19 in Taiwan. Vaccines (Basel). (2021) 9(9):983. doi: 10.3390/vaccines9090983
15. Chu DT, Thi HV, Thi YVN, Nguyen M-A, Bui N-L, Hoang VT, et al. Willingness to receive COVID-19 vaccine booster doses for adults and their children in Vietnam. J Hum Behav Soc Environ. (2022) 1:13. doi: 10.1080/10911359.2022.2046235
16. Statista Research Department. Social network penetration in Singapore Q3 2020. (2022). Available from: https://www.statista.com/statistics/284466/singapore-social-network-penetration/ (Accessed April 20, 2022).
17. BestInSingapore. The complete guide to social media statistics in Singapore. (2022). Available from: https://www.bestinsingapore.co/singapore-social-media-statistics/ (Accessed April 27, 2022).
18. Larson HJ, Jarrett C, Schulz WS, Chaudhuri M, Zhou Y, Dube E, et al. Measuring vaccine hesitancy: the development of a survey tool. Vaccine. (2015) 33:34. doi: 10.1016/j.vaccine.2015.04.037
19. Gautier S, Luyt D, Davido B, Herr M, Cardot T, Rousseau A, et al. Cross-sectional study on COVID-19 vaccine hesitancy and determinants in healthcare students: interdisciplinary trainings on vaccination are needed. BMC Med Educ. (2022) 22:299. doi: 10.1186/s12909-022-03343-5
20. Bollyky TJ, Hulland EN, Barber RM, Collins JK, Kiernan S, Moses M. Pandemic preparedness and COVID-19: an exploratory analysis of infection and fatality rates, and contextual factors associated with preparedness in 177 countries, from Jan 1, 2020, to Sept 30, 2021. Lancet. (2022) 399:10334. doi: 10.1016/S0140-6736(22)00172-6
21. Horiuchi S, Sakamoto H, Abe SK, Shinohara R, Kushima M, Otawa S, et al. Factors of parental COVID-19 vaccine hesitancy: a cross sectional study in Japan. PLoS ONE. (2021) 16:12. doi: 10.1371/journal.pone.0261121; Aldakhil H, Albedah N, Alturaiki N, Alajlan R, Abusalih H. Vaccine hesitancy towards childhood immunizations as a predictor of mothers’ intention to vaccinate their children against COVID-19 in Saudi Arabia. J Infect Public Health. (2021) 14:10. doi: 10.1016/j.jiph.2021.08.028
22. Du F, Chantler T, Francis MR, Sun FY, Zhang X, Han K, et al. The determinants of vaccine hesitancy in China: a cross-sectional study following the Changchun Changsheng vaccine incident. Vaccine. (2020) 38:47. doi: 10.1016/j.vaccine.2020.09.075
23. Yoneoka D, Eguchi A, Nomura S, Kawashima T, Tanoue Y, Murakami M, et al. Identification of optimum combinations of media channels for approaching COVID-19 vaccine unsure and unwilling groups in Japan. Lancet Reg Health Western Pacific. (2022) 18:1. doi: 10.1016/j.lanwpc.2021.100330
Keywords: COVID-19, paediatric, parental attitudes, vaccination, social media
Citation: Low JM, Soo CWT, Phuong TA, Zhong Y and Lee LY (2022) Predicting vaccine hesitancy among parents towards COVID-19 vaccination for their children in Singapore. Front. Pediatr. 10:994675. doi: 10.3389/fped.2022.994675
Received: 15 July 2022; Accepted: 20 September 2022;
Published: 10 October 2022.
Edited by:
Yusra Habib Khan, Jouf University, Saudi ArabiaReviewed by:
Sumit Shah, University of Arkansas for Medical Sciences, United States© 2022 Low, Soo, Phuong, Zhong and Lee. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Youjia Zhong eW91amlhemhvbmdAbnVzLmVkdS5zZw==
†These authors have contributed equally to this work and share first authorship
Specialty Section: This article was submitted to Pediatric Infectious Diseases, a section of the journal Frontiers in Pediatrics
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.