Abstract
Objectives:
This study examined the effectiveness of Byrd's EarWell system for the treatment of auricular helix adhesion.
Methods:
The newborns with helix adhesion were treated with ear molding. The photos of pinna were taken before, during, and after the treatment. The immediate and long-term outcomes, as well as the complications, were assessed by two independent plastic surgeons.
Study design:
A retrospective study. Data on family history, neonatal weight, gestational age, delivery method, laterality, gender, age of initiating treatment, medical comorbidities, duration of treatment, and follow-up time were collected.
Study site and period:
From 2019 to 2021, infants treated with the EarWell System in the Eye and ENT Hospital of Fudan University were enrolled in this study.
Results:
A total of 46 newborns (66 ears) with helix adhesion were included. The average onset time of treatment was 4.57 ± 3.63 weeks. The average duration of treatment was 7.40 ± 2.05 weeks. 97.0% ears’ (64/66) immediate results were excellent or good. During long-term follow-up, 95.5% ears achieved excellent or good outcomes. Age of initiation treatment significantly affected immediate (p = 0.001) and long-term (p = 0.004) outcomes.
Conclusions:
EarWell System was an effective method to correct auricular helix adhesion. Using this approach, patients with helix adhesion could avoid surgeries. Age of initiation treatment was the predictor of successful correction.
Introduction
Ear anomalies are common in newborns, with the incidence rate ranging from 15% to 50% (1, 2). An abnormal auricular appearance can cause mental distress. Some studies have found that children with ear anomalies would experience more anxiety, negative self-perception, and interpersonal problems (3–5). So the treatment of ear anomalies is very important for children's psychosocial health (6, 7).
In the past, ear anomalies could only be corrected with surgery. The helix adhesion is a type of mild auricular malformation. Due to the adhesion, the chondrocutaneous component is mildly defective. Scapha skin flap technique and inlay cartilage graft technique are used to correct helical adhesion (8). The potential complications of surgery included wound infection, hemorrhage, and anesthesia-related risks (9). Donor-site deformities, pigmentation of skin grafts, and scarring of the postauricular–mastoid region are still of concern (8). What is more, children could not undergo otoplastic surgeries until they are 5 or 6 years old (10). It has been reported that as age increases, an increasing number of patients experience mood disorders. Thus, it is very important to find a proper treatment that could be initiated at a young age (4).
Recently, the EarWell system, a non-invasive treatment, has been demonstrated to treat neonatal abnormal ears safely and effectively (11, 12). Auricular deformities, as well as some sorts of mild ear malformations, could benefit from this correction system. Nonsurgical methods might be effective for correction auricular adhesion malformation. This study was designed to examine the effectiveness of Byrd's ear molding technique for auricular helix adhesion.
Patients and methods
Definition of helix adhesion
Based on the observation of Odili (13) and Chul Park (8), we proposed a modified definition of helix adhesion. Helix adhesion is present when the helix is partially adherent to the scaphoid fossa or antihelix, and there is no intervening layer of skin between the two layers of cartilage (Figure 1). When present, it creates a mild kink in the normal curvature of the helical rim which may consider as less cosmetically pleasant. Due to the adhesion, the cartilage and skin components were slightly defective.
Figure 1
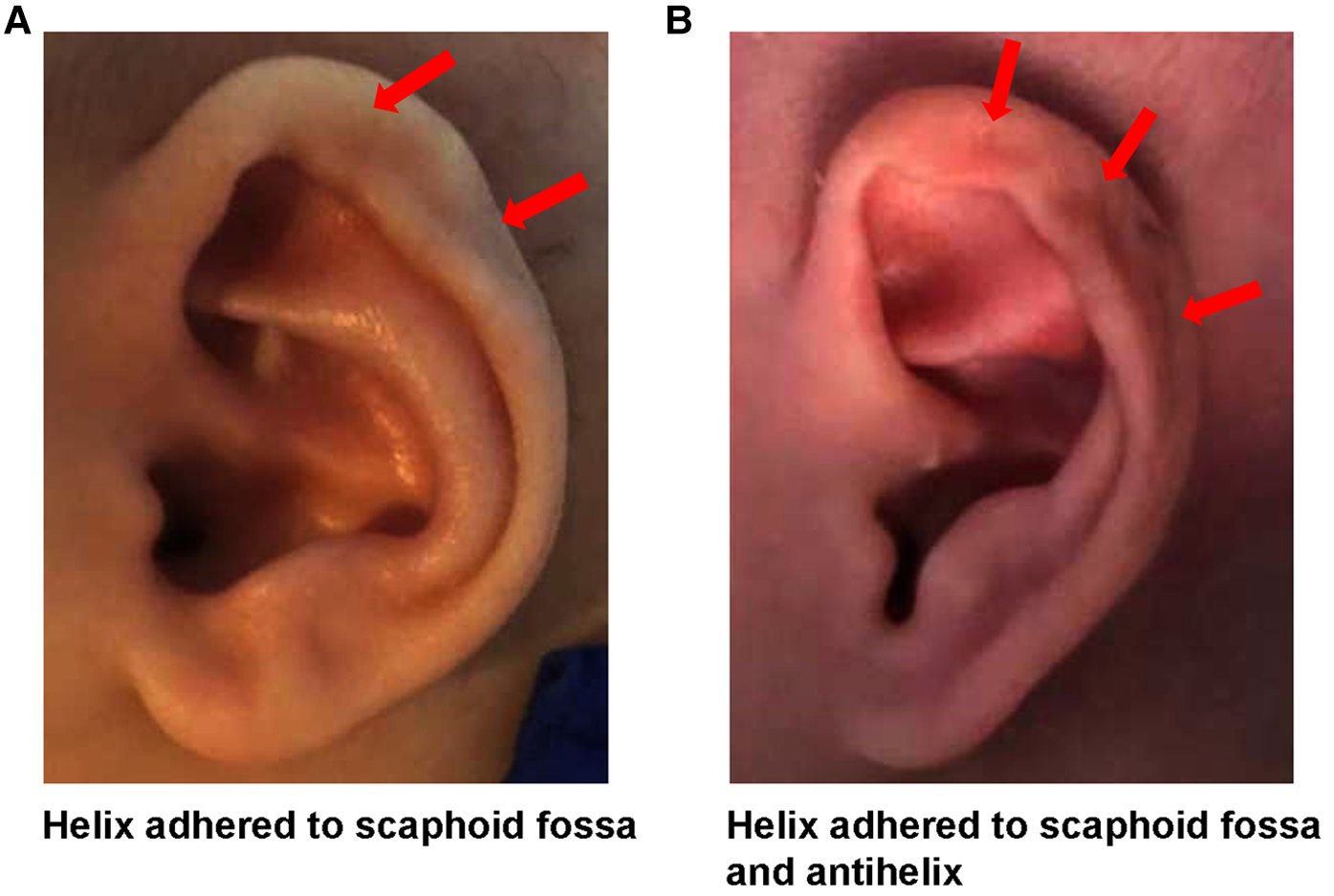
Auricular adhesion anomaly.
Patient selection
This retrospective study was approved by the intuitional review board of the Eye and ENT Hospital of Fudan University— a high-volume ear reconstruction center in China. The written informed consent was obtained before starting standard molding treatment. Only infants with a solitary helical adhesion and undergoing external splinting with EarWell system according to Byrd's method (14, 15) met inclusion criteria. Infants who fail to complete molding treatment would be excluded. Between May 2019 and May 2021, a total of 46 infants were enrolled in this study. Demographic and clinical data collected included family history, neonatal weight, gestational age, delivery method, laterality, gender, age at the time of initiating treatment, medical comorbidities, duration of treatment, and date of the last follow-up. Ear photos were taken before, during, and after treatment. A retrospective parents’ satisfaction survey was completed after the last follow-up.
Treatment process
At the first visit, the molding device was placed by a senior surgeon carefully. Patients were asked to follow up weekly. During treatment, we would adjust the device if necessary. If any complications occurred, the treatment was suspended for 2 to 3 days and local use of antibiotic ointment. Once the skin healed, the ear would continue molding. The complications would be carefully checked and addressed. Outpatient treatment continued for 2 weeks after achieving ear normalization.
Immediate results were assessed by comparing the pre-treatment photos with images that were taken immediately after the infants completed treatment. Ears followed for more than 6 months were considered as “long-term” outcomes. To evaluate the immediate and long-term (≥ 6 months after treatment end) effectiveness, photographs of each ear were taken and compared by two independent and experienced plastic surgeons. Outcomes were graded based on the standards proposed by Byrd (1) (see Supplementary Figure S1). If the two surgeons had disagreements, a third, independent, plastic surgeon was consulted. None of these three surgeons was involved in the treatment process. Ears which were graded excellent or good were considered to achieve successful results.
Statistical analysis
SPSS software (version 20.0; IBM, New York) was used for statistical analyses. Continuous variables were described as means and standard deviations (SD), and categorical variables were described as frequencies and percentages. Chi-square test was used to calculate p values. A value of p < 0.05 was considered statistically significant.
Results
Patient characteristics
A total of 46 infants with 66 ears were recruited. The basic patient demographics were listed in Table 1. There were 33 (71.7%) newborns who initiated ear molding before 6 weeks of age. Only 4.4% (4/46) patients started EarWell system treatment after 3 months of age. Three (6.5%) cases were premature. Meanwhile, their weights were less than 2500 g. More than half (58.7%) of the babies were born via natural birth. The number of the male and the female was very close (24 vs. 22). 18 patients were found with a normal ear, and an abnormal ear with helical adhesion. 8 patients had a helix adhesion ear at one side, and an abnormal ear of other type on the other side. Almost half patients (43.5%, 20/46) had helix adhesion ear on both sides. None of them had a family history of helical adhesion. The average duration of treatment was 7.40 ± 2.05 weeks, and the median treatment time was 7.00 weeks (range: 3.71–14.14 weeks). Follow-up time was defined as the number of days between the time of last visit and the end of treatment, and the average follow-up time was 14.60 ± 6.88 months, and the median follow-up time was 13.27 weeks (range: 6.10–32.8 weeks).
Table 1
| Characteristics | No. (%) |
|---|---|
| Age of initiation treatment | |
| ≤6 wk | 33 (71.7) |
| 6 wk–3 m | 11 (23.9) |
| ≥3 m | 2 (4.4) |
| Gestational age, wk | |
| 28–37 | 3 (6.5) |
| 37–42 | 42 (91.3) |
| ≥42 | 1 (2.2) |
| Neonatal weight, g | |
| <2500 | 3 (6.5) |
| 2500–4000 | 40 (87.0) |
| ≥4000 | 3 (6.5) |
| Delivery method | |
| Natural birth | 27 (58.7) |
| Cesarean delivery | 19 (41.3) |
| Gender | |
| Male | 24 (52.2) |
| Female | 22 (47.8) |
| Affected ears | |
| Unilateral | 18 (39.1) |
| Bilateral | |
| Both helix adhesion | 20 (43.5) |
| Helix adhesion + Other type | 8 (17.4) |
| Duration of treatment, wk | |
| Mean ± SD | 7.40 ± 2.05 |
| Median (range) | 7.00 (3.71-14.14) |
| Follow-up time, m | |
| Mean ± SD | 14.60 ± 6.88 |
| Median (range) | 13.27 (6.10-32.80) |
Clinical characteristics of the 46 newborns with helix adhesion.
wk, weeks; m, months; g, gram; SD, standard deviation.
It was interesting that we found one dizygotic twin pair (Figure 2). They both suffered from helical adhesion. They were premature with birth weights less than 2500 g and started ear molding at 34 days of birth. This implied that genetic factors might contribute to helical adhesion.
Figure 2
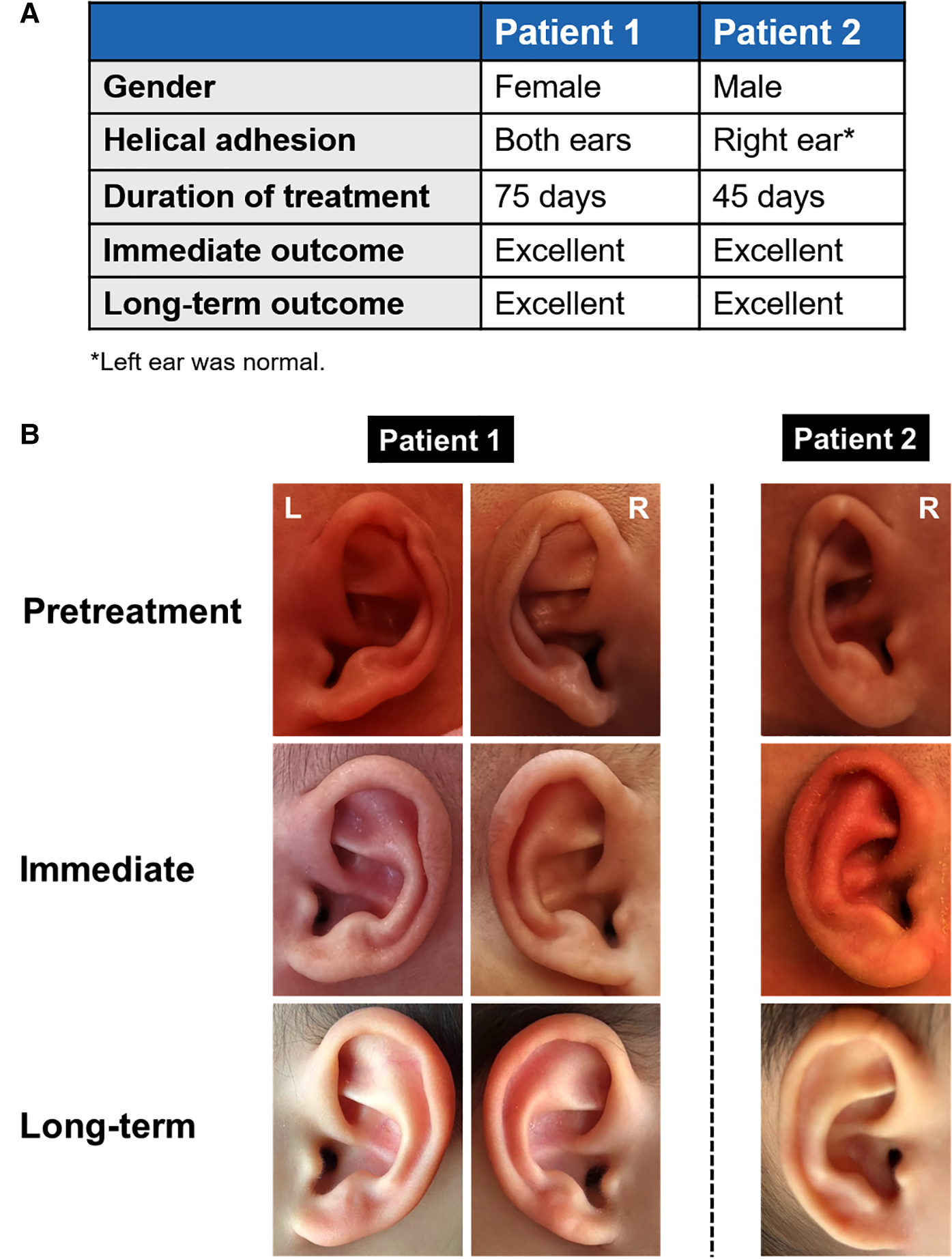
One dizygotic twin pair with helix adhesion.
Immediate treatment outcomes
Ears with good or excellent outcomes were considered successful in terms of corrections. Most ears (58/66, 87.9%) were graded excellent. Six ears were good, and one ear was fair. No ears' immediate results were poor. Therefore, the immediate success rate was 97.0 percent (64/66, Table 2). The 2 ears with fair immediate outcomes were from a female patient, with 2500 g birth weight. This patient initiated correction at 112 days (exceeding 3 months after birth) and was treated for 50 days (7.14 weeks). This patient was found to have ulcer and dermatitis simultaneously.
Table 2
| Characteristics | Immediate outcomesa | Long-term outcomes | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Excellent | Good | Fair | Success rateb | Excellent | Good | Fair | Poor | Success rateb | |
| Age of initiation treatment | |||||||||
| ≤ 6 wk | 45 | 5 | 0 | 100% | 44 | 6 | 0 | 0 | 100% |
| 6 wk–3 m | 12 | 1 | 0 | 100% | 8 | 4 | 1 | 0 | 92.3% |
| ≥ 3 m | 1 | 0 | 2 | 33.3% | 1 | 0 | 0 | 2 | 33.3% |
| Gestational age, wk | |||||||||
| 28–37 | 3 | 1 | 0 | 100% | 4 | 0 | 0 | 0 | 100% |
| 37–42 | 53 | 5 | 2 | 96.7% | 47 | 10 | 1 | 2 | 95.0% |
| ≥ 42 | 2 | 0 | 0 | 100% | 2 | 0 | 0 | 0 | 100% |
| Neonatal weight, g | |||||||||
| <2500 | 3 | 1 | 0 | 100% | 4 | 0 | 0 | 0 | 100% |
| 2500–4000 | 50 | 5 | 2 | 96.5% | 46 | 9 | 0 | 2 | 96.5% |
| ≥ 4000 | 5 | 0 | 0 | 100% | 3 | 1 | 1 | 0 | 80.0% |
| Side | |||||||||
| Left | 30 | 5 | 1 | 97.2% | 27 | 7 | 1 | 1 | 94.4% |
| Right | 28 | 1 | 1 | 96.7% | 26 | 3 | 0 | 1 | 96.7% |
| Affected ears | |||||||||
| Unilateral | 17 | 1 | 0 | 100% | 15 | 3 | 0 | 0 | 100% |
| Bilateral | |||||||||
| Both helix adhesion | 34 | 4 | 2 | 95.0% | 31 | 6 | 1 | 2 | 92.5% |
| Helix adhesion + Other type | 7 | 1 | 0 | 100% | 7 | 1 | 0 | 0 | 100% |
| Gender | 29 | 5 | 0 | 100% | 25 | 8 | 1 | 0 | 97.1% |
| Male | 29 | 1 | 2 | 93.8% | 28 | 2 | 0 | 2 | 93.8% |
| Female | |||||||||
| Complications | 7 | 1 | 2 | 80.0% | 5 | 3 | 0 | 2 | 80.0% |
| Yes | 51 | 5 | 0 | 100% | 48 | 7 | 1 | 0 | 98.2% |
| No | |||||||||
| Delivery method | 34 | 4 | 0 | 100% | 30 | 7 | 1 | 0 | 97.4% |
| Natural birth | 24 | 2 | 2 | 92.9% | 23 | 3 | 0 | 2 | 92.9% |
| Cesarean delivery | 58 | 6 | 2 | 97.0% | 53 | 10 | 1 | 2 | 95.5% |
Immediate and long-term outcomes of the 66 ears with helix adhesion.
wk, weeks; m, months; g, gram.
No ears’ immediate results were poor.
The ears which were graded excellent or good were considered to achieve successful results.
Examples of helix adhesion ears treated using the EarWell System were shown in Figure 3. Ten (15.2%, 10/66) ears were found with dermatitis and pressure ulcers.
Figure 3
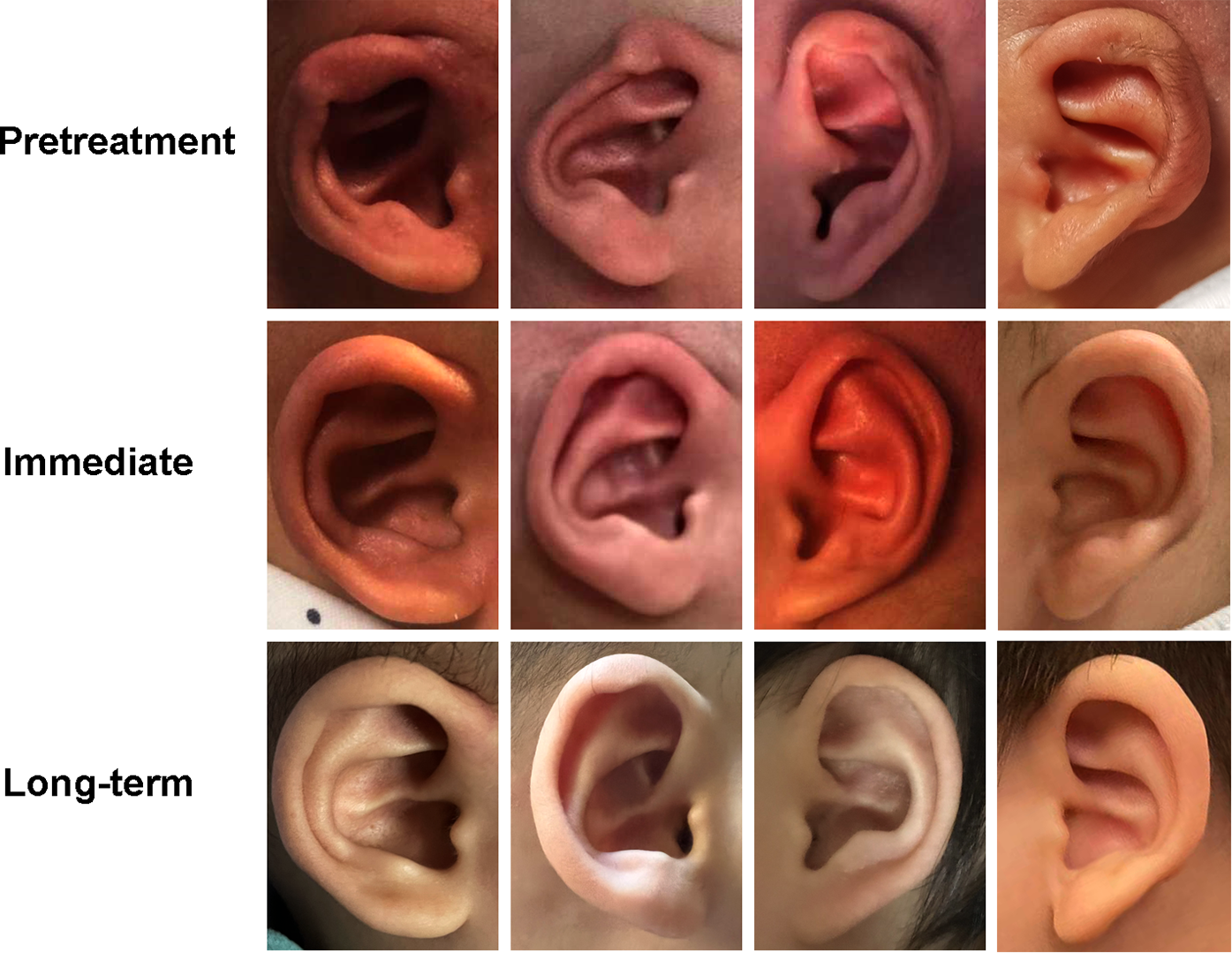
Examples of successful correction for helical adhesion.
Long-term treatment outcomes
When evaluating the long-term effectiveness of ear molding technique for helix adhesion, 53 ears (80.3%) were graded excellent, and 10 (15.2%) were graded good (Table 2). So the long-term success rate was 95.5 percent (63/66). One ear's long-term grading was fair. This ear was from a male patient. He had helix adhesion ears on both sides. This patient initiated correction at 52 days (7.43 weeks) and was treated for 56 days (8 weeks). The immediate outcomes of his 2 ears were excellent. However, these 2 ears fail to maintain normal shape over time. The grading changed from excellent to good (left ear) and from excellent to fair (right ear). We noticed that the 2 ears with fair immediate outcomes got worse during long-term follow-up, and they were graded poor at the last visit. These 2 ears were also from a single person, who initiated molding at the age of 3.7 months after birth.
Age of initiation treatment affects molding effectiveness
As shown in Table 3, there was a significant difference in the age of initiation treatment between patients with successful and unsuccessful immediate results (p = 0.001). Long-term outcomes were also significantly correlated with the age of initiation treatment (p = 0.004).
Table 3
| Variables | Immediate outcome | P value | Long-term outcome | P value | ||
|---|---|---|---|---|---|---|
| Success | Failure | Success | Failure | |||
| Age of initiation treatment | 0.001 | 0.004 | ||||
| < 3 months | 63 | 0 | 62 | 1 | ||
| ≥ 3 months | 1 | 2 | 1 | 2 | ||
Age of initiation treatment affecting molding effectiveness for helix adhesion ear.
Complications
During treatment, the babies were examined weekly. Ten (15.2%) ears experienced complications (Figure 4). Dermatitis and ulcers were observed in 7 and 5 ears (2 ears with the two complications simultaneously), respectively.
Figure 4
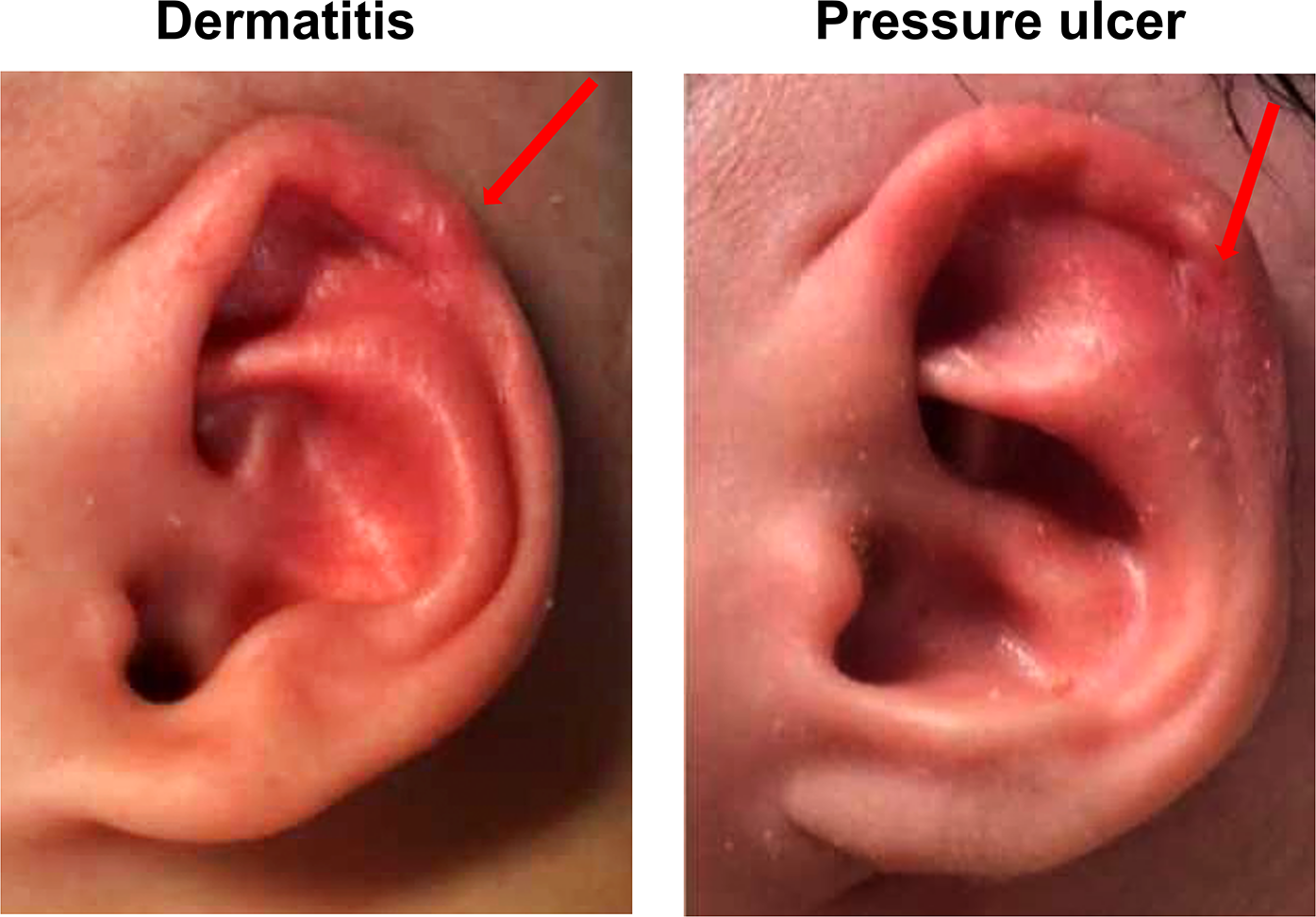
Complications of the EarWell system.
Parents' satisfaction
Among the 46 infants' parents, 39.1% (18/46) felt extremely satisfied, 56.5% (26/46) satisfied, only 4.4% (2/46) neutral. No dissatisfaction or extreme dissatisfaction with the treatment results was observed (Figure 5).
Figure 5

Parents’ satisfaction rates.
Discussion
There have been few previous studies of helical adhesion. In this study, we investigated the use of EarWell Infant Ear Correction System for patients with helical adhesion. We found the immediate and long-term success rates were 97.0% and 95.5%, respectively. The results of this study suggest that EarWell System can have favorable outcomes for helical adhesion. In addition, parent satisfaction with the treatment was also high (95.6%). Our results demonstrated that the age of initiation treatment was a significant predictor of both immediate (p = 0.001) and long-term corrections (p = 0.004). Infants initiating molding at early age had more stable outcomes. It is strongly advised to commence ear molding as soon as possible to attain an ideal ear shape for patients with helix adhesion.
Ear cartilage can be remolded at an early age, usually no more than 3 months. So it is very important to recognize helical adhesion soon after birth. However, helical adhesion malformations are still poorly identified. From 1986 to 2015, some Japanese literature depicted a group of helical adhesion deformity of upper third auricular cartilage (16–19). Odili and Gault also observed this unusual deformity with helical adhering to the scapha and obliterated helical sulcus. They called this deformity fold-over helical rim (8). Different from lidding ear, there was no skin between the two layers of cartilage because the cartilage adhered tightly or fused. Chul Park (14) noticed similar auricular adhesion malformations and divided them into 3 groups: solitary helical adhesion (the helical cartilage is attached to the anterior scapha cartilage), solitary antihelical adhesion (the posterior scapha cartilage is attached to the posterior conchal wall cartilage), helical and antihelical adhesion. In this study, we defined helical adhesion as a mild malformation which presented as helix adhering to adjacent ear structures, such as scaphoid fossa or antihelix, with or without helix rim pleating. Our definition was more comprehensive and easier to understand and remember, thus it would help physicians identify the helical adhesion malformation more accurately and timely.
Almost all studies of helical adhesion focused on how to correct malformation with surgery. Korean researchers recommend scapha skin flap technique and inlay cartilage graft technique for helical adhesion (14, 20). A technique of composite concha tissue graft
on the transection site of the scapha (21) and a technique of redraping of the helical skin after helical cartilage correction using Tanzer's banner flap technique were also suggested (17, 22). In some cases requiring a conchal cartilage graft, patients were advised to delay the operation until reached 12 years old. In fact, as an invasive treatment, surgery would bring potential complications such as infection, hemorrhage, hypertrophic scar, skin necrosis, and so on. Besides, children usually began to forge a personal identity and a self-concept around the age of 6 years. Treatment delays would make it difficult for children to have normal social interactions, thus affecting their studies and mental health.
Encouragingly, ear molding as a non-invasive technique could correct auricular deformities and slight malformations safely and effectively. The molding could be initiated long before the onset of teasing, bullying, and loss of self-esteem (23). We found some ear molding studies may include several cases of helix adhesion, although these cases were not named helix adhesion, the morphological features of the ear figures indicated that patients were with the helix adhesion deformity (1, 11). However, as these helix adhesion cases were mixed with other deformities, the molding effect of helix adhesion cannot be determined. To the best of our knowledge, this is the first study to focus on the effectiveness of ear mold treatment for patients with helix adhesion malformations, and we found this type of malformation could be well corrected by molding technique. This study aimed to help people recognize the morphological features of helix adhesion and clarify this type of malformation could be early treated by a non-invasive ear correction system. We hope that more clinicians know helix adhesion and that more patients with helix adhesion could receive molding treatment in time and avoid surgical trauma.
There were several limitations of this research. First, it was a retrospective study and the design may have an inherent bias, so the results need to be confirmed by a prospective study. Besides, the conclusions were based on data from a single-center, and need to be validated in multi-center studies. During clinical practice, we found the ear cartilage and skin of neonatal could be extended by mechanical force. We would explore the mechanisms in future study.
Conclusions
The immediate and long-term outcomes of helix adhesion after molding treatment demonstrated that EarWell System was an effective and safe method. Doctors should recognize helical adhesion accurately and timely, and then help patients initiate molding in the early time to achieve favorable ear shape.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics Committee for Clinical Research, Eye and ENT Hospital of Fudan University. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
YF and TZ designed the research study; LC and CL conceptualized and designed the study and contributed to the statistical analyses, interpretation of data, and drafted the initial manuscript; AH, YC, and HT conceptualized and designed the study; and all authors reviewed and revised the manuscript critically for important intellectual content, read and approved the final manuscript as submitted, and agree to be accountable for all aspects of the work. All authors contributed to the article and approved the submitted version.
Funding
Supported by National Natural Science Foundation of China (81800920, 82172105) and Natural Science Foundation of Shanghai (20ZR1409900).
Acknowledgments
Supported by National Natural Science Foundation of China (81800920, 82172105) and Natural Science Foundation of Shanghai (20ZR1409900).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2022.990629/full#supplementary-material.
References
1.
DanialiLNRezzadehKShellCTrovatoMHaRByrdHS. Classification of newborn ear malformations and their treatment with the EarWell infant ear correction system. Plast Reconstr Surg. (2017) 139(3):681–91. 10.1097/PRS.0000000000003150
2.
WooTKimYSRohTSLewDHYunIS. Correction of congenital auricular deformities using the ear-molding technique. Arch Plast Surg. (2016) 43(6):512–7. 10.5999/aps.2016.43.6.512
3.
JiameiDJiakeCHongxingZWanhouGYanWGaifenL. An investigation of psychological profiles and risk factors in congenital microtia patients. J Plast Reconstr Aesthet Surg. (2008) 61:S37–43. 10.1016/j.bjps.2007.09.002
4.
LiDChinWWuJZhangQXuFXuZet alPsychosocial outcomes among microtia patients of different ages and genders before ear reconstruction. Aesthetic Plast Surg. (2010) 34(5):570–6. 10.1007/s00266-010-9502-1
5.
FanYLiuWFanXNiuXChenX. Psychosocial status of patients with unilateral and bilateral microtia before auricular reconstruction surgery. Int J Pediatr Otorhinolaryngol. (2021) 151:110928. 10.1016/j.ijporl.2021.11092
6.
HorlockNVögelinEBradburyETGrobbelaarAOGaultDT. Psychosocial outcome of patients after ear reconstruction: a retrospective study of 62 patients. Ann Plast Surg. (2005) 54(5):517–24. 10.1097/01.sap.0000155284.96308.32
7.
JohnsALLucashREImDDLewinSL. Pre and post-operative psychological functioning in younger and older children with microtia. J Plast Reconstr Aesthet Surg. (2015) 68(4):492–7. 10.1016/j.bjps.2014.12.019
8.
ParkC. Upper auricular adhesion malformation: definition, classification, and treatment. Plast Reconstr Surg. (2009) 123(4):1302–12. 10.1097/PRS.0b013e31819e2679
9.
LennonCChinnaduraiS. Nonsurgical management of congenital auricular anomalies. Facial Plast Surg Clin North Am. (2018) 26(1):1–8. 10.1016/j.fsc.2017.09.001
10.
ZhangTYBulstrodeNChangKWChoYSFrenzelHJiangDet alInternational consensus recommendations on microtia, aural atresia and functional ear reconstruction. J Int Adv Otol. (2019) 15(2):204–8. 10.5152/iao.2019.7383
11.
PatelVMazzaferroDMSwansonJWTaylorJABartlettSP. Public perception of helical rim deformities and their correction with ear molding. J Craniofac Surg. (2020) 31(3):741–5. 10.1097/SCS.0000000000006400
12.
ChanSLSLimGJSPorYCChiangMFHoSSaffariSEet alEfficacy of ear molding in infants using the EarWell infant correction system and factors affecting outcome. Plast Reconstr Surg. (2019) 144(4):648e–58e. 10.1097/PRS.0000000000006057
13.
OdiliJIGaultDT. The foldover helical rim: reshaping the contour of an unusual deformity. Plast Reconstr Surg. (2008) 122(1):26e–7e. 10.1097/PRS.0b013e31817746fd
14.
ByrdHSLangevinCJGhidoniLA. Ear molding in newborn infants with auricular deformities. Plast Reconstr Surg. (2010) 126(4):1191–200. 10.1097/PRS.0b013e3181e617bb
15.
ZhangJLLiCLFuYYZhangTY. Newborn ear defomities and their treatment efficiency with earwell infant ear correction system in China. Int J Pediatr Otorhinolaryngol. (2019) 124:129–33. 10.1016/j.ijporl.2019.06.001
16.
NakamuraJTomonariHIzumiK. Minor auricular anomalies and their classification. Jpn J Plast Reconstr Surg. (1986) 6:268. 10.53045/jprs.1986-6268
17.
SawadaYNakajimaTYoshimuraY. Reconstruction of the folded ear deformity with the banner flap. Jpn J Plast Reconstr Surg. (1986) 29:605. 10.53045/jprs.1986-29605
18.
NakamuraJKuboEMaezawaN. Congenital adhesion of helix. Jpn J Plast Reconstr Surg. (1991) 34:805. 10.53045/jprs.1991-34805
19.
FukudaO. Helical adhesion deformity. In: FukudaOOrginoY, editors. Plastic surgery of external ear. Tokyo: Kokuseido (2005). p. 223–5.
20.
ParkCParkJY. Classification and algorithmic management of constricted ears: a 22-year experience. Plast Reconstr Surg. (2016) 137(5):1523–38. 10.1097/PRS.0000000000002120
21.
FukudaO. Reconstruction of the auricular scaphoid fossa with composite graft. Jpn J Plast Reconstr Surg. (1973) 16:380. 10.53045/jprs.1973-16380
22.
KawashimaTYamadaAUedaK. Reconstruction of the constricted ear by means of an autogenous cartilage graft. Jpn J Plast Reconstr Surg. (1991) 34:785. 10.53045/jprs.1991-34785
23.
FeijenMMvan CruchtenCPaynePE. Non-surgical correction of congenital ear anomalies: a review of the literature. Plastic and Reconstructive Surgery Global Open. (2020) 8(11):e3250. 10.1097/GOX.0000000000003250
Summary
Keywords
ear molding, helix adhesion, ear anomaly, outcome, long-term
Citation
Chen L, Li C, He A, Chen Y, Tong H, Fu Y and Zhang T (2022) Using ear molding to correct auricular helix adhesion deformity. Front. Pediatr. 10:990629. doi: 10.3389/fped.2022.990629
Received
12 July 2022
Accepted
21 October 2022
Published
15 November 2022
Volume
10 - 2022
Edited by
Jing He, Guangzhou Medical University, China
Reviewed by
John Martin Hempel, Ludwig Maximilian University of Munich, Germany Seyed Ehsan Saffari, Duke-NUS Medical School, Singapore
Updates
Copyright
© 2022 Chen, Li, He, Chen, Tong, Fu and Zhang.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yaoyao Fu fuyaoyao2007@126.com Tianyu Zhang tianyuzhang2006@126.com
These authors have contributed equally to this work
Specialty Section: This article was submitted to Pediatric Otolaryngology, a section of the journal Frontiers in Pediatrics
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.