
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Pediatr., 11 August 2022
Sec. Children and Health
Volume 10 - 2022 | https://doi.org/10.3389/fped.2022.979769
This article is part of the Research TopicThe Global Burden of COVID-19 on Children’s HealthView all 17 articles
 Alexandra M. Cardoso Pinto1*
Alexandra M. Cardoso Pinto1* Lasith Ranasinghe2
Lasith Ranasinghe2 Peter J. Dodd3
Peter J. Dodd3 Shyam Sundar Budhathoki4
Shyam Sundar Budhathoki4 James A. Seddon5,6
James A. Seddon5,6 Elizabeth Whittaker5
Elizabeth Whittaker5Background: The COVID-19 pandemic has disrupted routine childhood vaccinations worldwide with low- and middle-income countries (LMICs) most affected. This study aims to quantify levels of disruption to routine vaccinations in LMICs.
Methods: A systematic review (PROSPERO CRD42021286386) was conducted of MEDLINE, Embase, Global Health, CINAHL, Scopus and MedRxiv, on the 11th of February 2022. Primary research studies published from January 2020 onwards were included if they reported levels of routine pediatrics vaccinations before and after March 2020. Study appraisal was performed using NHLBI tool for cross-sectional studies. Levels of disruption were summarized using medians and interquartile ranges.
Results: A total of 39 cross-sectional studies were identified. These showed an overall relative median decline of −10.8% [interquartile range (IQR) −27.6%, −1.4%] across all vaccines. Upper-middle-income countries (upper-MICs) (−14.3%; IQR −24.3%, −2.4%) and lower-MICs (−18.0%; IQR −48.6%, −4.1%) showed greater declines than low-income countries (−3.1%; IQR −12.8%, 2.9%), as did vaccines administered at birth (−11.8%; IQR −27.7%, −3.5%) compared to those given after birth (−8.0%; IQR −28.6%, −0.4%). Declines during the first 3 months of the pandemic (−8.1%; IQR −35.1%, −1.4%) were greater than during the remainder of 2020 (−3.9%; IQR −13.0%, 11.4%) compared to baseline.
Conclusion: There has been a decline in routine pediatric vaccination, greatest in MICs and for vaccines administered at birth. Nations must prioritize catch-up programs alongside public health messaging to encourage vaccine uptake.
Systematic review registration: Identifier: CRD42021286386.
The Coronavirus Disease 2019 (COVID-19) pandemic (hereafter, “the pandemic”) and its control measures have disrupted access to healthcare globally. A systematic review performed during the first months of the pandemic found an overall 37% reduction in health service utilization, including hospital admissions, diagnostic and treatment services, highest during March and April 2020 (1). In May 2020, the World Health Organization (WHO) released the first Pulse Survey amongst Ministry of Health officials globally; nearly 90% reported disruptions to essential health services (2). Disruptions were greater in low-income countries (LICs) than high-income countries (HICs) (2). Immunization services were amongst those most frequently reported to be affected (2), with UNICEF estimating that 23 million children did not receive routine vaccinations during 2020; 3.7 million more than in 2019 (3).
Two further Pulse Surveys were published in May 2021 (4) and February 2022 (5). These showed that over 90% of countries reported continued healthcare disruptions. Of particular importance is the increased disruption to immunization services; whilst in May 2021 over one third of nations reported disruptions to immunization services (4), this rose to nearly half of nations in the subsequent survey (5). These findings raise concern regarding vaccine-preventable childhood morbidity and mortality. A modeling study by researchers at Johns Hopkins School of Public Health estimated a possible 9.8–44.7% increase in monthly deaths in children under-5 years caused by pandemic-related disruptions to healthcare, including vaccinations (6).
Routine vaccinations are fundamental for the health of children. A modeling study, investigating 10 pediatric vaccines, predicted that between 2000 and 2019, ~37 million deaths were prevented in low- and middle-income countries (LMICs) through vaccination (7). This represents a 45% decrease in mortality compared to a no-vaccine scenario, with most of the avoided deaths in children under 5 years (7). Most vaccines in this study are part of the WHO list of universally recommended immunizations, which include: Bacille Calmette-Guérin (BCG), Hepatitis B, Polio, diphtheria-tetanus-pertussis-containing (DTP) including Pentavalent, Haemophilus influenzae type b, Pneumococcal (conjugate), Rotavirus, Measles-containing (MCV), Rubella and Human Papillomavirus (HPV) vaccinations (8). Widespread access to these vaccines is essential to achieve universal health and wellbeing—part of Sustainable Development Goal (SDG) 3—in addition to other SDGs indirectly, including the reduction of poverty, malnutrition and achieving economic prosperity (9, 10). However, prior to the pandemic, the WHO had already highlighted large disparities in vaccine coverage worldwide. For example, in 2019, coverage of the third dose of DTP vaccine was only 73% in Africa, compared to 95% in Europe (11); inequalities which may widen with pandemic-related disruptions (9, 10, 12, 13).
Given a lower initial coverage of routine vaccinations, greater disruptions to healthcare during the pandemic, higher burden of vaccine-preventable diseases and lower available financial and infrastructural resources, LMICs are likely to encounter further challenges in the recovery of missed vaccinations (2, 4, 5, 11, 12). Gaining insight into the extent of pandemic-related disruptions to vaccination services is essential to plan effective catch-up vaccination programs, avoid vaccine-preventable disease epidemics and establish guidance to prevent disruptions in future global health emergencies. Therefore, the aim of this study is to measure the impact of the COVID-19 pandemic on routine childhood vaccination in LMICs.
A systematic review of published and pre-print literature were performed.
Six databases were searched: Medline, EMBASE and Global Health via Ovid, CINAHL, and Scopus. No field limits were applied. MedRxiv titles and abstracts were also searched, using the “medrxivr” package on R (14, 15). All searches were performed on the 11th of February 2022 and limited to publications from January 2020 onwards. The search strategy contained three concepts: COVID-19, immunization and specific vaccines or vaccine-preventable diseases (Supplementary Table S1). Additionally, a concept on general terms for routine vaccines was included, using proximity Boolean terms. This limited the number of irrelevant results, namely those related to COVID-19 vaccines. The search contained relevant keywords, including variations, and subject headings (Supplementary materials 2–7 contain full search strategies).
References of all relevant reviews, meeting and conference summaries, and all included studies, were screened for inclusion. Full-text versions of relevant abstracts were searched for in the previously mentioned databases and relevant journals. If unavailable, abstract authors were contacted to request access to full-texts.
Primary research studies reporting the levels, or changes in levels, of vaccine coverage or administration before (any time between January 2015 to March 2020) and during the pandemic (March 2020 onwards) in LMICs were included. Studies had to include data for LMICs regarding any vaccine universally recommended by the WHO, published from 2020 onwards. Non-primary research and modeling studies, such as those predicting the impact of the pandemic on future vaccination levels without accompanying observed measurements, were excluded. Language restrictions were only applied at full-text stage; studies not in English, Portuguese, French or Spanish were translated to English using Google Translate. Studies were only excluded if the translation was unclear.
Deduplication was performed on EndNote 20, and then Covidence, where screening was undertaken. Given the high number of identified studies, initial screening was performed by title to exclude clearly irrelevant results, followed by abstract. Eligibility was confirmed in full-text review. Screening was performed by two reviewers independently with discrepancies resolved by consensus.
Data were extracted from included studies using a pre-defined data extraction sheet designed on Microsoft Excel, including the following parameters: publication details (doi, authors, title, year published), study details (design, scope, data source, sample size, location(s) of study, country income-level classification, population, sampling methods, funding, conflicts of interest), outcome of interest details (date span of data in pre-COVID and COVID periods, use of controls, vaccines included, outcome title and outcome units), results for each outcome of interest, methods of analysis and conclusions. Outcomes of interest included number of vaccines administered pre- and during COVID-19 pandemic; vaccine coverage—defined as the number of individuals receiving a certain vaccine as a percentage of the target population for that vaccine in a specific time-period—pre- and during COVID-19 pandemic; and proportional or percentage change in either outcome. Where available, outcomes pre- and during COVID-19 pandemic were extracted per smallest unit of time available, usually per month. Where data were only available in graphical format, WebPlotDigitizer 4.5 (16) was used for extraction.
Studies underwent quality and bias assessment using National Heart, Lung and Blood Institute (NHLBI) checklist for observational studies (17). Data from 8 randomly selected studies (20% of total) were extracted by two reviewers. Given that all data extracted was identical, the remaining extractions were performed by a single reviewer. Bias assessments were performed fully by two reviewers and discrepancies resolved by consensus.
As there are no universally-accepted guidelines for conducting systematic reviews and meta-analyses of proportional changes, a guide published in BMC Medical Research Methodology (18), the Cochrane Handbook for Systematic Reviews of Interventions (19) and COSMOS-E guidelines (20) were consulted and adapted as appropriate.
Although a meta-analysis was planned it was not performed because studies were found to have substantial methodological variation, including in the vaccines studied, scope of data and locations. Furthermore, only a minority of studies reported uncertainty levels and other data required for meta-analysis. Instead, studies were summarized using medians and interquartile ranges (IQRs). The outcome unit was mean relative percentage change between levels of vaccination pre-COVID-19 pandemic (from January 2015 to February 2020) and during the pandemic (April 2020 to December 2021). Where percentage changes were not reported, these were calculated using pre-pandemic and pandemic values. Timelines for each study varied according to availability of data (Supplementary Figure S2). March 2020 was excluded from studies that reported data per month as this was considered a transition point.
Subgroup analyses by timing of vaccination (birth or afterwards), individual routine vaccine, WHO world region and income-level were performed. Results were also subdivided by decline during the first 3-months of the pandemic (April-June 2020) and the remainder of the pandemic, to identify potential recovery. The data extraction sheet on Microsoft Excel was used to determine which studies could be included in each subgroup.
This systematic review was registered on PROSPERO (CRD42021286386) and followed PRISMA 2020 guidelines (Supplementary Tables S3, S4) (21, 22).
Amendments to chosen databases were instituted after consultation with an expert librarian. This included the removal of Web of Science, as this had significant overlap with Scopus and the addition of MedRxiv for pre-prints.
Following the screening of 7,705 studies, 39 were included in the review (Figure 1).
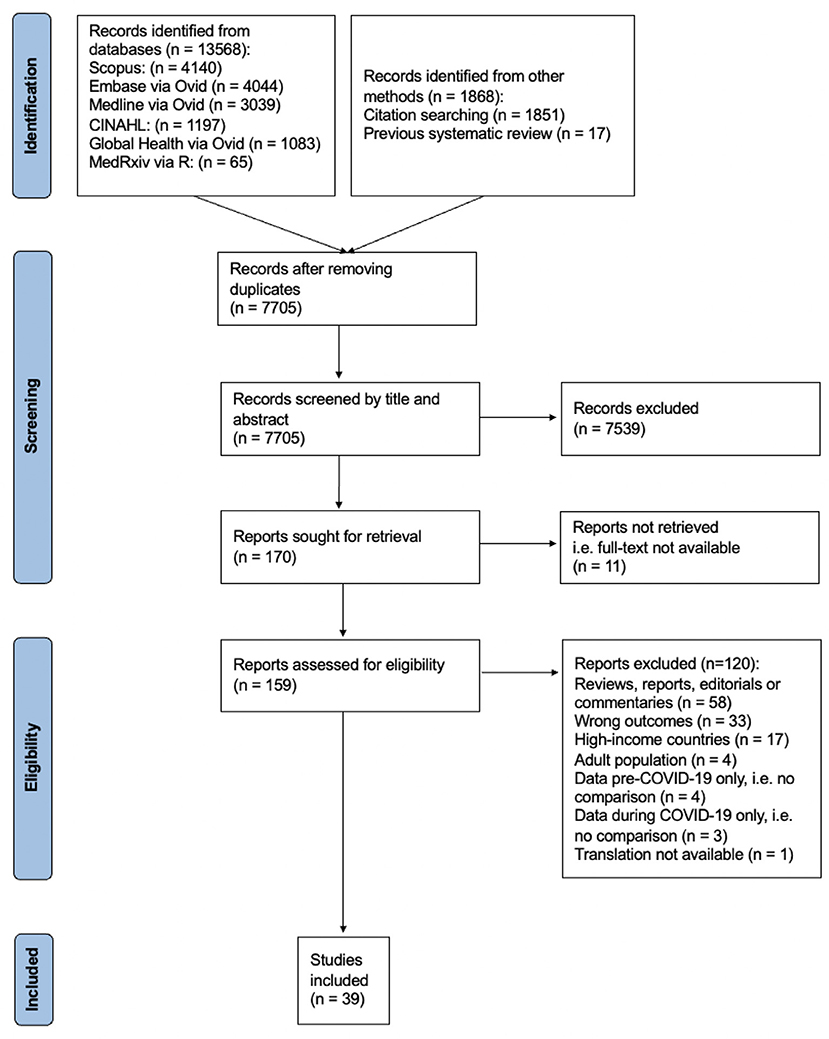
Figure 1. PRISMA flow diagram summarizing identification, screening, exclusion, and inclusion of studies (see Supplementary Figure 1 for detailed PRISMA 2020 flow diagram).
All studies were cross-sectional, utilizing data from health records (Table 1). Most reported levels of administered vaccines (n = 29) and the remainder reported vaccine coverage. Studies spanned 6 WHO regions unevenly, with Africa (53.8%) being the most common. Additionally, several countries appear repeatedly in different studies (Supplementary Table S2). Most studies reported national-level data (n = 17) or data from multiple health centers or regions (n = 11); the remainder were single-center studies and one survey-based study with unclear scope. Data were available for all WHO universally recommended vaccines apart from HPV, with levels of pentavalent or DTP (n = 33), MCV (n = 27) and BCG (n = 20) vaccines most frequently reported.
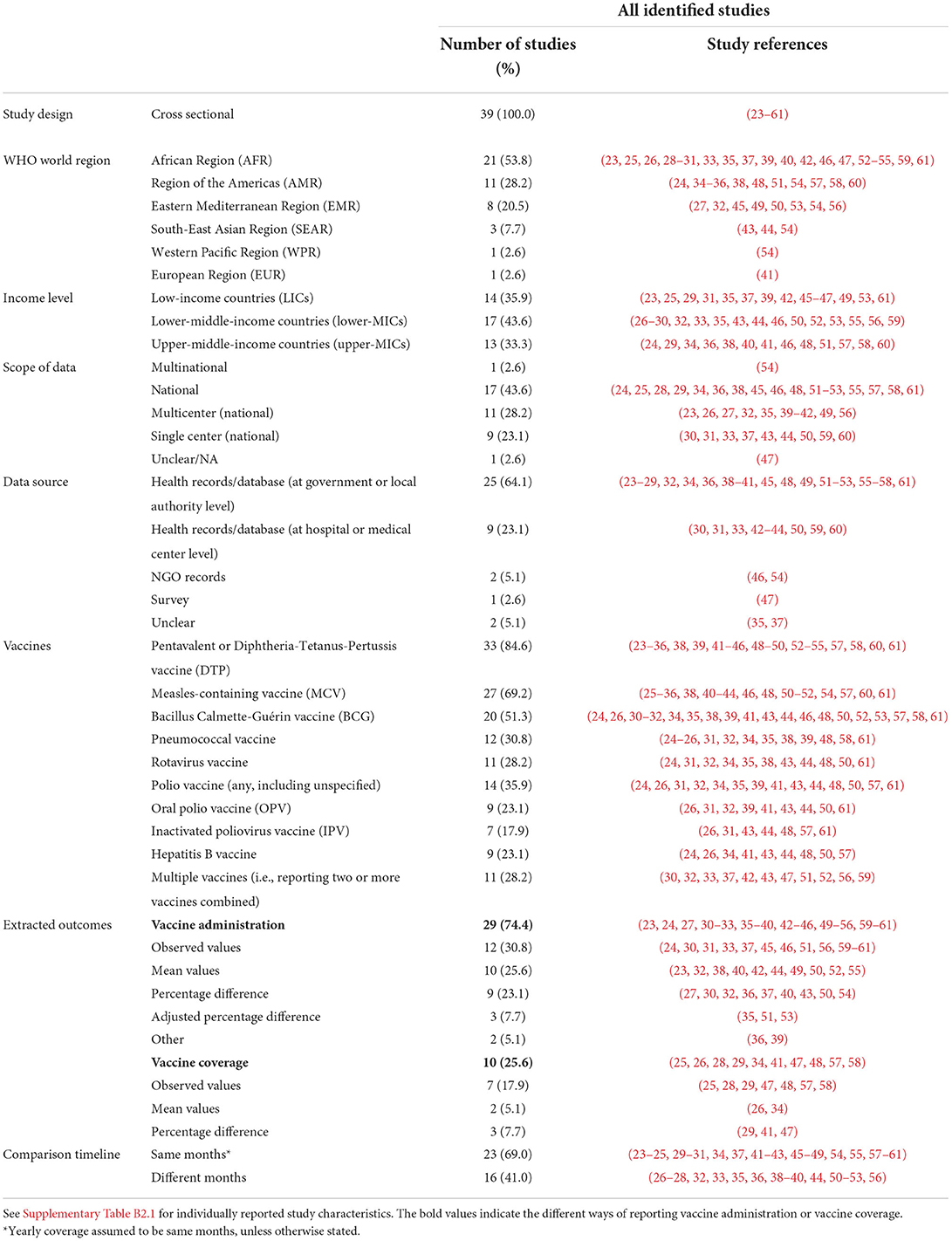
Table 1. Summary of study characteristics for studies reporting changes to vaccination levels (n = 39).
Timelines varied across studies (Supplementary Figure S2), with the median timespan being January 2019 (IQR: December 2017–July 2019) to September 2020 (IQR: June 2020–November 2020).
Overall, the quality of most studies was moderate; few studies considered confounders such as seasonality and population changes, and most did not report total population of the study or participation rates (Figure 2).

Figure 2. NHLBI assessments for included studies [Overall scores: good (G), moderate (M), poor (P)].
The overall median relative percentage change was −10.8% (IQR −27.6%, −1.4%) (Figure 3). This value was calculated using 331 observations, representing 45 countries (Table 2). The decline in studies reporting numbers of vaccines administered (−13.2%, IQR −44.7%, −2.0%) was greater than those reporting vaccination coverage (−3.5%, IQR −15.7%, 0.0%).
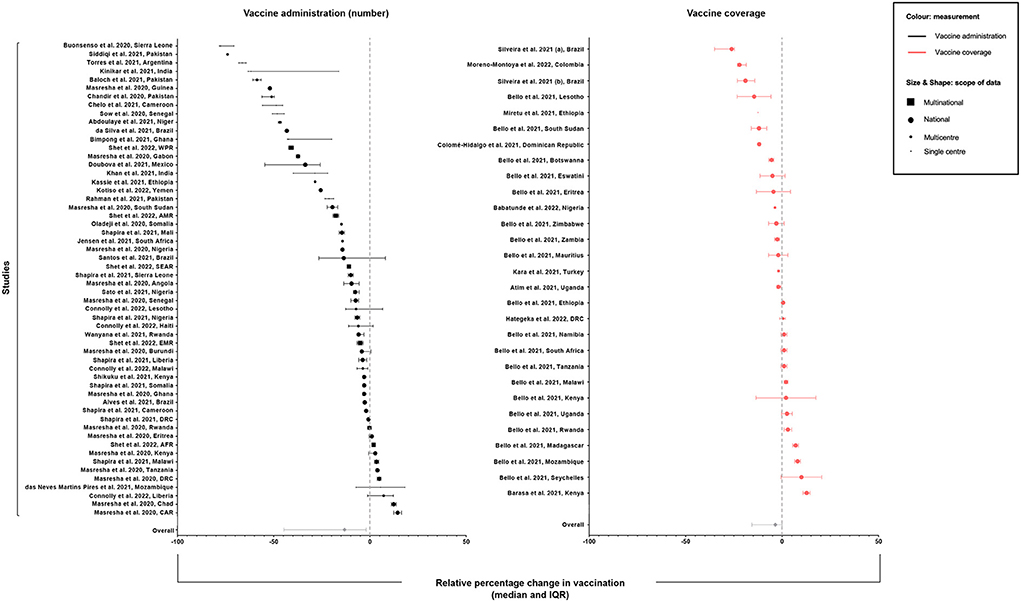
Figure 3. Median relative percentage change (±IQR) in vaccination coverage or number of vaccines administered per study and overall across all studies.
The median decline was greater in upper-middle income countries (MICs) (−14.3%, IQR −24.3%, −2.4%) and lower-MICs (−18.0%, IQR −48.6%, −4.1%) than LICs (−3.1%, IQR −12.8%, 2.9%) (Figure 4). There were 19 (70.4%) LICs represented in this analysis, compared to 12 (21.8%) and 14 (25.5%) upper-MICs and lower-MICs, respectively.
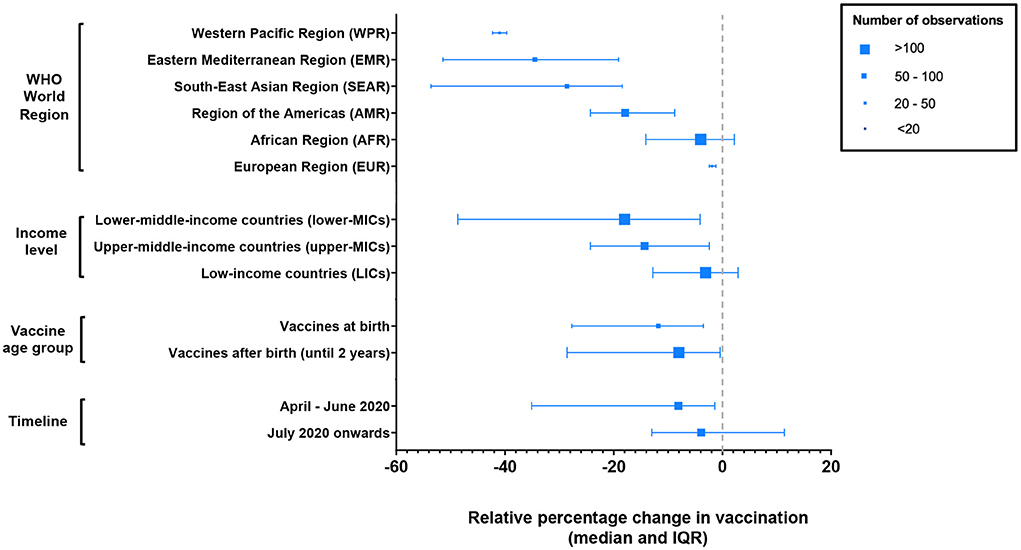
Figure 4. Median relative percentage change (±IQR) in vaccination by WHO world region, income level and vaccine age group.
The WHO world regions showing the greatest declines were WPR (−41.0%; IQR −42.3%, −39.7%), EMR (−34.5%, IQR −51.4%, −19.1%) and SEAR (−28.6%, IQR −53.6%, −18.4%). Regions showing the least declines were EUR (−1.9%, IQR −2.4%, −1.2%), followed by AFR (−4.0%, IQR −14.1%, 2.2%). However, whilst 35 countries from the AFR region were included in this analysis, the remaining regions had 6 or fewer represented countries [excluding Shet et al. (54)]. The study by Shet et al. (54) is an observational study summarizing global WHO vaccination coverage data which was included in the analysis for AFR, AMR, EMR, SEAR and WPR regions.
Vaccines administered at birth showed a median decline of −11.8% (IQR −27.7%, −3.5%) and vaccines after birth a decline of −8.2% (IQR −28.8%, −0.6%). Vaccines showing the greatest degrees of decline were polio vaccines (−16.6%, IQR −50.9%, −3.9%) and rotavirus vaccines (−22.4%, IQR −45.2%, −6.9%). Those showing the least declines were PCV (−4.7%, IQR −31.1%, 0.8%), followed by MCV (−5.2%, IQR −21.2%, 1.7%) and DTP or pentavalent vaccines (−7.4%, IQR −23.9%, −0.1%).
Declines during the first three months of the pandemic, that is April to June 2020, were greater (−8.1%, IQR −35.1%, −1.4%) than declines during the remainder of the pandemic relative to baseline, for time periods available (−3.9, −13.0, 11.4%).
Overall, a median decline of over 10% was seen in routine childhood vaccination in LMICs. Most countries represented in the analysis were from the WHO African region. Drops were greatest for vaccines given at birth, and in MICs. The drop in the first 3 months of the pandemic appears greater than later in the pandemic, suggesting a degree of recovery, although declines persist.
The decline in vaccination coverage corroborates findings from a previous systematic review which narratively synthesized evidence from LMICs and HICs in early 2021 (62), and the three WHO Pulse Surveys (2, 4, 5), all of which identified global disruptions to routine vaccination programs. The second Pulse Survey categorized results by income-level, also demonstrating that a greater proportion of MICs reported disruptions than LICs (4). Reasons for this are unclear, but maybe a consequence of publication bias, particularly as fewer MICs are represented in WHO data, and this study, than LICs. Alternative reasons to be explored include differences in stringency of COVID-19 measures, support from non-governmental organizations, such as the Global Alliance for Vaccines and Immunization (GAVI), and degrees of urbanization, particularly if these areas are found to have been more affected than rural areas.
This study found evidence that the median decline in vaccination during the first 3 months of 2020 was greater than the decline in the remainder of that year. This suggests there may have been some recovery in vaccination levels since the start of the pandemic, but declines persist. This corroborates findings from the third Pulse Survey; 53% of countries that participated in all three survey rounds reported disruptions to immunizations, compared to 56% in the first round, suggesting little improvement (5). By contrast, literature from England (63), France (64), Sweden (65), Japan (66) and the United States (67) suggests vaccination is recovering in these HICs, although not always returning to pre-pandemic levels. Data from these studies are from 2020; more recent data are needed for definitive conclusions on recovery. One study from Sierra Leone has since published data on vaccination declines until March 2021 by quarter. This dynamic analysis showed that despite improvements in vaccination levels in every quarter, most vaccines continued to show declines of over 10% by March 2021 (68). If recovery is greater in HICs than LMICs, these findings raise concern over potential widening of global inequalities in vaccination (13).
Given WHO recommendations to continue vaccination during the pandemic (69, 70), disruptions to maternal health services may explain part of the observed decline in vaccines delivered at birth. Observational studies from Bangladesh (71) and Nepal (72) have shown reductions in institutional deliveries of 10–20% and over 50%, respectively, during the first 3 months of the pandemic. By the end of 2021, 26% of countries still reported a decline in facility-based births to the WHO (5). The BCG vaccine was also thoroughly investigated for its use against COVID-19 (73), which may have led to temporary shortages in its supply, as was reported in Japan (74, 75). It is possible, however, that the finding that vaccines delivered in hospital soon after birth fell more than vaccines given in primary care later in infancy, is a result of the way data are collected and reported, or a function of the different studies included in this review.
The reasons behind disruptions to vaccinations are likely multifactorial. WHO findings suggest that 76% of reasons underlying disruptions to health-services stem from disruptions to healthcare service provision (5). A multinational study of IMPRINT members also identified fear of COVID-19 as a reason for delayed vaccination (76). Reasons for disruption are likely to vary according to each country's experience of the pandemic, including public health messaging and lockdown measures.
Vaccine hesitancy may also have contributed to declines in vaccination. Although vaccine hesitancy existed prior to COVID-19, hesitancy may have been exacerbated by the pandemic. A Norwegian study investigated factors associated with vaccine hesitancy during the COVID-19 pandemic and found that the greatest predictors of hesitancy were perceived risks of vaccinations and preference for natural immunity (77). Trust for information shared by health officials appeared to reduce risk of hesitancy (77). However, in instances where health professionals are themselves unsure of vaccine safety—as happened with COVID-19 vaccination—and share this publicly, such as through social media, trust in healthcare professionals might instead increase hesitancy. Similarly, government messaging discouraging vaccination, as was seen in Brazil with regards to COVID-19 vaccination (78), also has potential to translate into hesitancy across other vaccines.
Declines in routine childhood vaccination raise concern over future morbidity and mortality of vaccine-preventable diseases. Prior to the pandemic, many LMICs already had rates of vaccination coverage below the levels necessary to eliminate these diseases or achieve herd immunity (11). Such setbacks bring nations further away from achieving these targets. A modeling study predicted that an 18.5% decline in routine child vaccinations would result in a 10% increase in severely malnourished children, with declines in WHO universally recommended vaccines independently responsible for ~15 thousand additional deaths every three months (6). An older modeling study investigating the impact of falls in BCG coverage estimated that a 10% annual decline in BCG coverage worldwide could lead to over 11,700 tuberculosis deaths in children up to 15 years old (79).
It is not the first time that a disease outbreak has impacted healthcare. A systematic review found a decline in children's health services, including over 20% in pentavalent vaccinations, during the West Africa Ebola outbreak in 2014–2016 (80). Given its high transmissibility (81), the risk of measles outbreaks following declines in vaccination is particularly concerning; Guinea, Liberia and Sierra Leone all had significant rises in measles cases for up to 2 years following the Ebola outbreak (82). Vaccine-preventable disease outbreaks have already been reported during the pandemic for measles and polio (83, 84), including a polio outbreak in Malawi reported in February 2022 (85). Wild poliovirus was eliminated in Africa in 2020 (86); this outbreak brings major setbacks to polio eradication. Declines in vaccination are likely to increase the frequency and severity of these outbreaks. The fall in rotavirus vaccination is also concerning, as diarrhea has been reported as the second most common cause of death in children aged under five, excluding neonates, globally (87)—with rotavirus being the most common cause of severe or fatal diarrhea (88).
Furthermore, declines in surveillance and treatment have also been observed; over half of African countries reported reductions to suspected measles cases and lab specimens in 2020 (89). Whilst lockdown measures including school closures may have reduced transmission, considering the increasing trend in suspected measles cases between 2017 and 2019, declines are likely consequences of under-reporting (89). The combination of declines in vaccination with reduced healthcare-seeking behavior and less robust surveillance raise concern over increased prevalence, transmission, and severity of infections.
Efforts to recover lost vaccinations, such as catch-up programs, should be prioritized. Additionally, it is vital for nations to invest in public health campaigns encouraging attendance to essential health-services, including vaccinations. National investigations exploring factors disrupting vaccination programs and the extent of disruption for individual vaccines should also be performed, to ensure targeted approaches to catch-up programs. There may also be regional differences to investigate (77). These data would enable the prioritization of populations and vaccines with the highest level of disruption and risk of transmission. Greater understanding would also enable the development of guidance to prevent similar disruptions in future pandemics.
There are several limitations that should be acknowledged. First, given the substantial methodological heterogeneity between studies and missing participation rates for most studies, a meta-analysis was not performed. The analysis is descriptive, and measures of effect must be interpreted with caution. In addition, there is lack of representation from several world regions, with most studies reporting data from African countries. Similarly, there is low representation of MICs. Furthermore, available data is mainly from 2020; more recent data is required to establish reliable conclusions. These data limitations emphasize the need for recent national-level data from more countries and per vaccine, to improve the generalizability of findings and inform more meaningful analyses, respectively. Moreover, studies measuring levels of vaccine administration and coverage were included and assumed equal; however, this assumes that there is no change in population from pre-pandemic to pandemic time-periods. Most studies also did not account for confounders such as seasonality or secular trends. Finally, this study did not explore reasons behind disruptions to vaccination, including the potential impact of vaccination hesitancy during the COVID-19 pandemic.
Overall, this study found a drop in routine childhood vaccination in LMICs during the COVID-19 pandemic, with some evidence of recovery in 2020. To avoid increases in child mortality due to the resurgence of vaccine-preventable diseases, LMICs must now focus on recovery of lost vaccination through catch-up programs and strong public health messaging to encourage attendance to health services for routine vaccinations.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
AC, JS, and EW designed the study and protocol. AC conducted first round of study screening, data extraction, and appraisal, conducted data analysis, and wrote the first draft of the manuscript. LR conducted second round of study screening, data extraction, and appraisal. JS and EW supervised the work. All authors provided critical feedback that helped shape the research, discussed results and contributed to the final version of the manuscript.
Open access publication fees for this manuscript were covered by the Imperial College Open Access Fund. JS was supported by a Clinician Scientist Fellowship jointly funded by the UK Medical Research Council (MRC) and the UK Department for International Development (DFID) under the MRC/DFID Concordat agreement (MR/R007942/1).
The authors would like to thank Rebecca Jones for the feedback and advice regarding the search strategy.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2022.979769/full#supplementary-material
1. Moynihan R, Sanders S, Michaleff ZA, Scott AM, Clark J, To EJ, et al. Impact of Covid-19 pandemic on utilisation of healthcare services: a systematic review. BMJ Open. (2021) 11:e045343. doi: 10.1136/bmjopen-2020-045343
2. World Health Organization. Pulse Survey on Continuity of Essential Health Services During the Covid-19 Pandemic. (2020). Available online at: https://www.who.int/publications/i/item/WHO-2019-nCoV-EHS_continuity-survey-2020.1 (accessed April 07, 2022).
3. UNICEF. Covid-19 Pandemic Leads to Major Backsliding on Childhood Vaccinations, New Who, Unicef Data Shows. (2021). Available online at: https://www.unicef.org.uk/press-releases/covid-19-pandemic-leads-to-major-backsliding-on-childhood-vaccinations-new-who-unicef-data-shows/ (accessed February 09, 2022).
4. World Health Organization. Second Round of the National Pulse Survey on Continuity of Essential Health Services During the Covid-19 Pandemic. (2021). Available online at: https://www.who.int/publications/i/item/WHO-2019-nCoV-EHS-continuity-survey-2021.1 (accessed April 07, 2022).
5. World Health Organization. Third Round of the Global Pulse Survey on Continuity of Essential Health Services During the Covid-19 Pandemic: World Health Organization. (2022). Available online at: https://apps.who.int/iris/handle/10665/351527 (accessed April 07, 2022).
6. Roberton T, Carter ED, Chou VB, Stegmuller AR, Jackson BD, Tam Y, et al. Early estimates of the indirect effects of the Covid-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study. Lancet Glob Health. (2020) 8:e901–e8. doi: 10.1016/S2214-109X(20)30229-1
7. Li X, Mukandavire C, Cucunubá ZM, Echeverria Londono S, Abbas K, Clapham HE, et al. Estimating the health impact of vaccination against ten pathogens in 98 low-income and middle-income countries from 2000 to 2030: a modelling study. Lancet. (2021) 397:398–408. doi: 10.1016/S0140-6736(20)32657-X
8. World Health Organization. Who Recommendations for Routine Immunization: Summary Tables. (2021). Available online at: https://www.who.int/teams/immunization-vaccines-and-biologicals/policies/who-recommendations-for-routine-immunization—summary-tables (accessed February 16, 2022).
9. United, Nations,. Ensure Healthy Lives and Promote Well-Being for All at All Ages. Available from: https://sdgs.un.org/goals/goal3 (accessed February 09, 2022).
10. World Health Organization. Immunization Agenda 2030: A Global Strategy to Leave No One Behind. (2020). Available online at: https://www.who.int/teams/immunization-vaccines-and-biologicals/strategies/ia2030 (accessed April 12, 2022).
11. World Health Organization. Progress and Challenges with Achieving Universal Immunization Coverage. (2020). Available online at: https://www.who.int/publications/m/item/progress-and-challenges-with-achievinguniversal-immunization-coverage (accessed May 11, 2022).
12. Zar HJ, Dawa J, Fischer GB, Castro-Rodriguez JA. Challenges of Covid-19 in children in low- and middle-income countries. Paediatr Respir Rev. (2020) 35:70–4. doi: 10.1016/j.prrv.2020.06.016
13. Chandir S, Siddiqi DA. Inequalities in Covid-19 disruption of routine immunisations and returning to pre-covid immunisation rates. Lancet Reg Health West Pac. (2021) 10:100156. doi: 10.1016/j.lanwpc.2021.100156
14. R Core Team,. R: A Language Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing. (2022). Available online at: https://www.R-project.org/ (accessed February 28, 2022).
15. McGuinness LA, Schmidt L. Medrxivr: accessing and searching medrxiv and biorxiv preprint data in R. J Open Source Softw. (2020) 5:2651. doi: 10.21105/joss.02651
16. Rohatgi A,. Webplotdigitizer 4.5 Pacifica, California, USA. (2021). Available online at: https://automeris.io/WebPlotDigitizer
17. National Heart Lung Blood Institute. Study Quality Assessment Tools: Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. (2021). Available online at: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed February 21, 2022).
18. Barker TH, Migliavaca CB, Stein C, Colpani V, Falavigna M, Aromataris E, et al. Conducting proportional meta-analysis in different types of systematic reviews: a guide for synthesisers of evidence. BMC Med Res Methodol. (2021) 21:189. doi: 10.1186/s12874-021-01381-z
19. Higgins JPTTJ, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane Handbook for Systematic Reviews of Interventions Version 63: Cochrane. Chichester: John Wiley and Sons (2019).
20. Dekkers OM, Vandenbroucke JP, Cevallos M, Renehan AG, Altman DG, Egger M. Cosmos-E: guidance on conducting systematic reviews and meta-analyses of observational studies of etiology. PLoS Med. (2019) 16:e1002742. doi: 10.1371/journal.pmed.1002742
21. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The prisma 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
22. Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. Prisma 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. (2021) 372:n160. doi: 10.1136/bmj.n160
23. Abdoulaye MB, Oumarou B, Moussa H, Anya B-PM, Didier T, Nsiari-Muzeyi BJ, Katoto P, Wiysonge CS. The impact of the Covid-19 pandemic on health service utilisation in the city of Niamey: a study conducted in 17 health care facilities from January to June 2020. Pan Afr Med J. (2021) 39:159. doi: 10.11604/pamj.2021.39.159.28282
24. Alves JG, Figueiroa JN, Urquia ML. Impact of Covid-19 on immunization of Brazilian infants. Int J Infect Dis. (2021) 107:252–3. doi: 10.1016/j.ijid.2021.04.089
25. Atim MG, Kajogoo VD, Amare D, Said B, Geleta M, Muchie Y, et al. Covid-19 and health sector development plans in Africa: the impact on maternal and child health outcomes in Uganda. Risk Manag Healthc Policy. (2021) 14:4353–60. doi: 10.2147/RMHP.S328004
26. Babatunde OA, Olatunji MB, Omotajo OR, Ikwunne OI, Babatunde AM, Nihinlola ET, et al. Impact of Covid-19 on routine immunization in Oyo State, Nigeria: trend analysis of immunization data in the pre- and post-index case period; 2019–2020. Pan Afr Med J. (2022) 41:54. doi: 10.11604/pamj.2022.41.54.28575
27. Baloch AA, Baig N, Baloch F, Suhag Z. Impact on the utilization of reproductive, maternal, newborn and child health care services at primary health care level during first wave of Covid-19 outbreak in Pakistan. Cureus. (2021) 13:e17430. doi: 10.7759/cureus.17430
28. Barasa E, Kazungu J, Orangi S, Kabia E, Ogero M, Kasera K. Indirect health effects of the Covid-19 pandemic in Kenya: a mixed methods assessment. BMC Health Serv Res. (2021) 21:740. doi: 10.1186/s12913-021-06726-4
29. Bello IM, Lebo E, Shibeshi ME, Akpan GU, Chakauya J, Masresha BG, et al. Implementation of integrated supportive supervision in the context of coronavirus 19 pandemic: its effects on routine immunization and vaccine preventable surveillance diseases indicators in the East and Southern African Countries. Pan Afr Med J. (2021) 38:164. doi: 10.11604/pamj.2021.38.164.27349
30. Bimpong KA, Nuertey BD, Seidu AS, Ajinkpang S, Abdul-Mumin A. Decline in uptake of childhood vaccinations in a tertiary hospital in Northern Ghana during the Covid-19 pandemic. Biomed Res Int. (2021) 2021:10. doi: 10.1155/2021/6995096
31. Buonsenso D, Cinicola B, Kallon MN, Iodice F. Child healthcare and immunizations in sub-saharan Africa during the Covid-19 pandemic. Front Pediatr. (2020) 8:517. doi: 10.3389/fped.2020.00517
32. Chandir S, Siddiqi DA, Mehmood M, Setayesh H, Siddique M, Mirza A, et al. Impact of Covid-19 pandemic response on uptake of routine immunizations in Sindh, Pakistan: an analysis of provincial electronic immunization registry data. Vaccine. (2020) 38:7146–55. doi: 10.1016/j.vaccine.2020.08.019
33. Chelo D, Nguefack F, Enyama D, Nansseu R, Feudjo Tefoueyet G, Mbassi Awa HD, et al. Impact and projections of the Covid-19 epidemic on attendance and routine vaccinations at a pediatric referral hospital in cameroon. Arch Pediatr. (2021) 28:441–50. doi: 10.1016/j.arcped.2021.05.006
34. Colomé-Hidalgo M, Campos JD, Gil de Miguel Á. Tracking the impact of the Covid-19 pandemic on routine infant vaccinations in the dominican republic. Hum Vaccin Immunother. (2022) 18:1972708. doi: 10.1080/21645515.2021.1972708
35. Connolly E, Boley EJ, Fejfar DL, Varney PF, Aron MB, Fulcher IR, et al. Childhood immunization during the Covid-19 pandemic: experiences in Haiti, Lesotho, Liberia and Malawi. Bull World Health Organ. (2022) 100:115–26C. doi: 10.2471/BLT.21.286774
36. da Silva TMR, de Sá A, Vieira EWR, Prates EJS, Beinner MA, Matozinhos FP. Number of doses of measles-mumps-rubella vaccine applied in Brazil before and during the Covid-19 pandemic. BMC Infect Dis. (2021) 21:1237. doi: 10.1186/s12879-021-06927-6
37. Mucufo JR, Mupueleque MA. Zakus D, et al. Covid-19 pandemic impact on maternal and child health services access in nampula, mozambique: a mixed methods research. BMC Health Serv Res. (2021) 21:860. doi: 10.1186/s12913-021-06878-3
38. Doubova SV, Leslie HH, Kruk ME, Perez-Cuevas R, Arsenault C. Disruption in essential health services in mexico during Covid-19: an interrupted time series analysis of health information system data. BMJ Glob Health. (2021) 6:e005671. doi: 10.1136/bmjgh-2021-006204
39. Hategeka C, Carter SE, Chenge FM, Katanga EN, Lurton G, Mayaka SM, et al. Impact of the Covid-19 pandemic and response on the utilisation of health services in public facilities during the first wave in Kinshasa, the democratic republic of the Congo. BMJ Glob Health. (2021) 6:e005955. doi: 10.1136/bmjgh-2021-005955
40. Jensen C, McKerrow NH. Child health services during a Covid-19 outbreak in Kwazulu-Natal Province, South Africa. S Afr Med J. (2021) 111:114–9. doi: 10.7196/SAMJ.2021v111i2.15243
41. Kara A, Ilbay S, Topac O, Arabulan EA, Tezer H, Tavukcu N, et al. Alteration in vaccination rates and an evaluation of physicians' perceptions of the possible impact of the SARS-CoV-2 pandemic on childhood vaccinations in Ankara, Turkey. Hum Vaccines Immunother. (2021) 17:3457–62. doi: 10.1080/21645515.2021.1923345
42. Kassie A, Wale A, Yismaw W. Impact of coronavirus diseases-2019 (Covid-19) on utilization and outcome of reproductive, maternal, and newborn health services at governmental health facilities in South West Ethiopia, 2020: comparative cross-sectional study. Int J Womens Health. (2021) 13:479–88. doi: 10.2147/IJWH.S309096
43. Khan A, Chakravarty A, Mahapatra J. Impact of Covid-19 pandemic on childhood immunization in a tertiary health-care center. Indian J Community Med. (2021) 46:520–3. doi: 10.4103/ijcm.IJCM_847_20
44. Kinikar AA. Impact of Covid-19 lockdown on immunization at a public tertiary care teaching hospital. Curr Pediatr Res. (2021) 25:1–3.
45. Kotiso M, Qirbi N, Al-Shabi K, Vuolo E, Al-Waleedi A, Naiene J, et al. Impact of the Covid-19 pandemic on the utilisation of health services at public hospitals in Yemen: a retrospective comparative study. BMJ Open. (2022) 12:e047868. doi: 10.1136/bmjopen-2020-047868
46. Masresha BG, Luce R Jr, Shibeshi ME, Ntsama B, N'Diaye A, Chakauya J, et al. The performance of routine immunization in selected African Countries during the first six months of the Covid-19 pandemic. Pan Afr Med J. (2020) 37:12. doi: 10.11604/pamj.supp.2020.37.1.26107
47. Miretu DG, Asfaw ZA, Addis SG. Impact of Covid-19 pandemic on vaccination coverage among children aged 15 to 23 months at Dessie Town, Northeast Ethiopia, 2020. Hum Vaccines Immunother. (2021) 17:2427–36. doi: 10.1080/21645515.2021.1883387
48. Moreno-Montoya J, Ballesteros SM, Rojas Sotelo JC, Bocanegra Cervera CL, Barrera-López P, De la Hoz-Valle JA. Impact of the Covid-19 Pandemic on Routine Childhood Immunisation in Colombia. Arch Dis Child. (2022) 107:e4. doi: 10.1136/archdischild-2021-321792
49. Oladeji O, Oladeji B, Farah A, Ali Y, Ayanle M. Assessment of effect of Covid 19 pandemic on the utilization of maternal newborn child health and nutrition services in somali region of Ethiopia. J Epidemiol Public Health. (2020) 5:458–69. doi: 10.26911/jepublichealth.2020.05.04.08
50. Rahman SU, Haq FU, Imran M, Shah A, Bibi N, Khurshid R, et al. Impact of the Covid-19 lockdown on routine vaccination in Pakistan: a hospital-based study. Hum Vacc Immunother. (2021) 17:1–7. doi: 10.1080/21645515.2021.1979380
51. Santos VS, Vieira SCF, Barreto IDC, de Gois-Santos VT, Celestino AO, Domingues C, et al. Effects of the Covid-19 pandemic on routine pediatric vaccination in Brazil. Exp Rev Vacc. (2021) 20:1661–6. doi: 10.1080/14760584.2021.1990045
52. Sato R. Pattern of vaccination delivery around Covid-19 lockdown in Nigeria. Hum Vacc Immunother. (2021) 17:2951–3. doi: 10.1080/21645515.2021.1908061
53. Shapira G, Ahmed T, Drouard SHP, Amor Fernandez P, Kandpal E, Nzelu C, et al. Disruptions in maternal and child health service utilization during Covid-19: analysis from eight Sub-Saharan African Countries. Health Policy Plan. (2021) 36:1140–51. doi: 10.1093/heapol/czab064
54. Shet A, Carr K, Danovaro-Holliday MC, Sodha SV, Prosperi C, Wunderlich J, et al. Impact of the SARS-CoV-2 pandemic on routine immunisation services: evidence of disruption and recovery from 170 countries and territories. Lancet Glob Health. (2022) 10:e186–e94. doi: 10.1016/S2214-109X(21)00512-X
55. Shikuku Duncan N, Nyaoke Irene K, Nyaga Lucy N, Ameh Charles A. Early indirect impact of Covid-19 pandemic on utilisation and outcomes of reproductive, maternal, newborn, child and adolescent health services in Kenya: a cross-sectional study. Afr J Reprod Health. (2021) 25:76–87. doi: 10.1101/2020.09.09.20191247
56. Siddiqi DA, Abdullah S, Dharma VK, Shah MT, Akhter MA, Habib A, et al. Using a low-cost, real-time electronic immunization registry in Pakistan to demonstrate utility of data for immunization programs and evidence-based decision making to achieve Sdg-3: insights from analysis of big data on vaccines. Int J Med Inform. (2021) 149:104413. doi: 10.1016/j.ijmedinf.2021.104413
57. Silveira MF, Tonial CT, Goretti K. Maranhao A, Teixeira AMS, Hallal PC, Maria B Menezes A, et al. Missed childhood immunizations during the Covid-19 pandemic in Brazil: analyses of routine statistics and of a national household survey. Vaccine. (2021) 39:3404–9. doi: 10.1016/j.vaccine.2021.04.046
58. Silveira MM, Conrad NL, Leivas Leite FP. Effect of Covid-19 on vaccination coverage in Brazil. J Med Microbiol. (2021) 70: 001466. doi: 10.1099/jmm.0.001466
59. Sow A, Gueye M, Boiro D, Ba A, Ba ID, Faye PM, et al. Effect of Covid-19 on routine immunization schedule in senegalese hospitals. Pan Afr Med J. (2020) 37:364. doi: 10.11604/pamj.2020.37.364.25805
60. Torres F, Dominguez P, Aruanno ME, Macherett MJ, Nocent ES, Risoli L, et al. Impact of the SARS-CoV-2 pandemic on the administration of vaccines as per the national immunization schedule in children younger than 2 years. Arch Argent Pediatr. (2021) 119:198–201. doi: 10.5546/aap.2021.eng.198
61. Wanyana D, Wong R, Hakizimana D. Rapid assessment on the utilization of maternal and child health services during Covid-19 in Rwanda. Public Health Action. (2021) 11:12–21. doi: 10.5588/pha.20.0057
62. Lassi ZS, Naseem R, Salam RA, Siddiqui F, Das JK. The impact of the Covid-19 pandemic on immunization campaigns and programs: a systematic review. Int J Environ Res Public Health. (2021) 18:988. doi: 10.3390/ijerph18030988
63. McDonald HI, Tessier E, White JM, Woodruff M, Knowles C, Bates C, et al. Early impact of the coronavirus disease (Covid-19) pandemic and physical distancing measures on routine childhood vaccinations in England, January to April 2020. Euro Surveill. (2020) 25:2000848. doi: 10.2807/1560-7917.ES.2020.25.19.2000848
64. Taine M, Offredo L, Drouin J, Toubiana J, Weill A, Zureik M, et al. Mandatory infant vaccinations in france during the Covid-19 pandemic in 2020. Front Pediatr. (2021) 9:666848. doi: 10.3389/fped.2021.666848
65. Falkenstein Hagander K, Aronsson B, Danielsson M, Lepp T, Kulane A, Schollin Ask L. National swedish survey showed that child health services and routine immunisation programmes were resilient during the early Covid-19 pandemic. Acta Paediatr. (2021) 110:2559–66. doi: 10.1111/apa.15912
66. Aizawa Y, Katsuta T, Sakiyama H, Tanaka-Taya K, Moriuchi H, Saitoh A. Changes in childhood vaccination during the coronavirus disease 2019 pandemic in Japan. Vaccine. (2021) 39:4006–12. doi: 10.1016/j.vaccine.2021.05.050
67. Patel Murthy B, Zell E, Kirtland K, Jones-Jack N, Harris L, Sprague C, et al. Impact of the Covid-19 pandemic on administration of selected routine childhood and adolescent vaccinations: 10 United States Jurisdictions, March–September 2020. MMWR Morb Mortal Wkly Rep. (2021) 70:840–5. doi: 10.15585/mmwr.mm7023a2
68. Mariani F, Valentini P, Yamba M, Turay AS, Bulubisi H, Moscato U, et al. Changes in childhood immunizations and intermittent preventive malaria treatment in a peripheral, referral immunization center during the first 12 months of Covid-19 pandemic in Sierra Leone, Western Africa. Front Pediatr. (2022) 10:774281. doi: 10.3389/fped.2022.774281
69. World Health Organization. Guidance on Routine Immunization Services During Covid-19 Pandemic in the Who European Region. (2020). Available online at: https://apps.who.int/iris/handle/10665/334123 (accessed April 26, 2022).
70. World Health Organization. Maintaining Essential Health Services: Operational Guidance for the Covid-19 Context. (2020). Available online at: https://www.who.int/publications/i/item/WHO-2019-nCoV-essential_health_services-2020.2 (accessed April 26, 2022).
71. Sigma A, Hossain S, Hossain I, Bhuiyan K, Hossain SMI, Rob U, et al. Trends in maternal health services in bangladesh before, during and after Covid-19 lockdowns: evidence from national routine service data Dhaka: population council (2020) 1–5. doi: 10.31899/rh14.1037
72. Kc A, Gurung R, Kinney MV, Sunny AK, Moinuddin M, Basnet O, et al. Effect of the Covid-19 pandemic response on intrapartum care, stillbirth, and neonatal mortality outcomes in Nepal: a prospective observational study. Lancet Glob Health. (2020) 8:e1273–81. doi: 10.1016/S2214-109X(20)30345-4
73. Gonzalez-Perez M, Sanchez-Tarjuelo R, Shor B, Nistal-Villan E, Ochando J. The Bcg vaccine for Covid-19: first verdict and future directions. Front Immunol. (2021) 12:632478. doi: 10.3389/fimmu.2021.632478
74. Namkoong H, Horita N, Ebina-Shibuya R. Concern over a Covid-19-related Bcg shortage. Int J Tuberc Lung Dis. (2020) 24:642–3. doi: 10.5588/ijtld.20.0240
75. Senoo Y, Suzuki Y, Takahashi K, Tsuda K, Tanimoto T. Prioritizing infants in a time of bacille calmette-guerin vaccine shortage caused by premature expectations against Covid-19. QJM. (2020) 113:773–4. doi: 10.1093/qjmed/hcaa179
76. Saso A, Skirrow H, Kampmann B. Impact of Covid-19 on immunization services for maternal and infant vaccines: results of a survey conducted by imprint-the immunising pregnant women and infants network. Vaccines. (2020) 8:556. doi: 10.3390/vaccines8030556
77. Ebrahimi OV, Johnson MS, Ebling S, Amundsen OM, Halsoy O, Hoffart A, et al. Risk, trust, and flawed assumptions: vaccine hesitancy during the Covid-19 pandemic. Front Public Health. (2021) 9:700213. doi: 10.3389/fpubh.2021.700213
78. Fernandez M, Matta G, Paiva E. Covid-19, Vaccine hesitancy and child vaccination: challenges from Brazil. Lancet Reg Health Am. (2022) 8:100246. doi: 10.1016/j.lana.2022.100246
79. Harris RC, Dodd PJ, White RG. The potential impact of Bcg vaccine supply shortages on global paediatric tuberculosis mortality. BMC Med. (2016) 14:138. doi: 10.1186/s12916-016-0685-4
80. Brolin Ribacke KJ, Saulnier DD, Eriksson A, von Schreeb J. Effects of the West Africa Ebola virus disease on health-care utilization: a systematic review. Front Public Health. (2016) 4:222. doi: 10.3389/fpubh.2016.00222
81. Guerra FM, Bolotin S, Lim G, Heffernan J, Deeks SL Li Y, et al. The basic reproduction number (R(0)) of measles: a systematic review. Lancet Infect Dis. (2017) 17:e420–8. doi: 10.1016/S1473-3099(17)30307-9
82. Masresha BG, Luce R Jr, Weldegebriel G, Katsande R, Gasasira A, Mihigo R. The impact of a prolonged ebola outbreak on measles elimination activities in Guinea, Liberia and Sierra Leone, 2014–2015. Pan Afr Med J. (2020) 35(Suppl. 1):8. doi: 10.11604/pamj.supp.2020.35.1.19059
83. Dixon MG, Ferrari M, Antoni S, Li X, Portnoy A, Lambert B, et al. Progress toward regional measles elimination: worldwide, 2000–2020. MMWR Morb Mortal Wkly Rep. (2021) 70:1563–9. doi: 10.15585/mmwr.mm7045a1
84. Alleman MM, Jorba J, Henderson E, Diop OM, Shaukat S, Traoré MA, et al. Update on Vaccine-Derived Poliovirus Outbreaks - Worldwide, January 2020-June 2021. MMWR Morb Mortal Wkly Rep. (2021) 70:1691–9. doi: 10.15585/mmwr.mm7049a1
85. World Health Organization Africa. Malawi Declares Polio Outbreak. (2022). Available online at: https://www.afro.who.int/news/malawi-declares-polio-outbreak (accessed July 16, 2022).
86. World Health Organization. Global Polio Eradication Initiative Applauds Who African Region for Wild Polio-Free Certification. (2020). Available onlien at: https://www.who.int/news-room/detail/25-08-2020-global-polio-eradication-initiative-applauds-who-african-region-for-wild-polio-free-certification (accessed July 16, 2022).
87. Liu L, Oza S, Hogan D, Chu Y, Perin J, Zhu J, et al. Global, regional, and national causes of under-5 mortality in 2000–15: an updated systematic analysis with implications for the sustainable development goals. Lancet. (2016) 388:3027–35. doi: 10.1016/S0140-6736(16)31593-8
88. Walker CLF, Rudan I, Liu L, Nair H, Theodoratou E, Bhutta ZA, et al. Global burden of childhood pneumonia and diarrhoea. Lancet. (2013) 381:1405–16. doi: 10.1016/S0140-6736(13)60222-6
Keywords: immunization, routine vaccines, LMICs, child health, vaccine-preventable diseases, vaccination hesitancy
Citation: Cardoso Pinto AM, Ranasinghe L, Dodd PJ, Budhathoki SS, Seddon JA and Whittaker E (2022) Disruptions to routine childhood vaccinations in low- and middle-income countries during the COVID-19 pandemic: A systematic review. Front. Pediatr. 10:979769. doi: 10.3389/fped.2022.979769
Received: 27 June 2022; Accepted: 22 July 2022;
Published: 11 August 2022.
Edited by:
Anna Camporesi, Ospedale dei Bambini Vittore Buzzi, ItalyReviewed by:
Danilo Buonsenso, Catholic University of the Sacred Heart, ItalyCopyright © 2022 Cardoso Pinto, Ranasinghe, Dodd, Budhathoki, Seddon and Whittaker. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alexandra M. Cardoso Pinto, YWxleGFuZHJhLmNhcmRvc28tcGludG8xOEBpbXBlcmlhbC5hYy51aw==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.