
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr. , 23 September 2022
Sec. Children and Health
Volume 10 - 2022 | https://doi.org/10.3389/fped.2022.976317
This article is part of the Research Topic Dietary and Lifestyle Factors Associated with Hypertension among Children and Adolescents View all 5 articles
Objective: We aimed to demonstrate characteristics of hypertension at three separate visits and its risk factors among children and adolescents based on a large school-based study in China.
Materials and methods: Based on a large-scale ongoing monitoring program conducted in Suzhou, China, 59,679 children and adolescents aged 7–17 years from 60 public schools were enrolled during 2020 to 2021. Height, weight, and blood pressure (BP) were measured. Additional BP would be measured for hypertensive students at least 2 weeks later. Confirmed hypertension was defined as simultaneously BP meeting above or equal to 95th percentile for age, sex, and height at three separate visits. Odds ratio (ORs), and 95% CIs were calculated by logistic regression to identify risk factors for hypertension.
Results: Prevalence of hypertension at three separate visits were 20.4, 6.3, and 3.1%, respectively. Prevalence of confirmed isolated systolic hypertension, isolated diastolic hypertension, and systolic and diastolic hypertension were 1.9, 0.3, and 0.9%, respectively. Hypertension prevalence for stages 1 and 2 were 2.6 and 0.6%. Different hypertension prevalence were found among various age and gender groups. Boys [OR, 1.137 (95% CI, 1.033–1.251)], high age [OR, 3.326 (95% CI, 2.950–3.751)], urban residents [OR, 1.579 (95% CI, 1.417–1.760)], high-socioeconomic status [OR, 1.156 (95% CI, 1.039–1.286)] and body mass index category including overweight [1.883 (95% CI, 1.665–2.129)], obesity [4.049 (95% CI, 3.625–4.523)], and thinness [OR, 0.457 (95% CI, 0.306–0.683)] were associated with confirmed hypertension.
Conclusion: A single BP measurement would overestimate hypertension prevalence, about 3% Chinese children were hypertensive, early, and effective intervention around risk factors for hypertension should be taken.
Globally, hypertension is one of the important risk factors for cardiovascular diseases (CVDs) and related premature deaths (1). It is worth noting that individuals with high blood pressure (BP) in childhood tend to have high BP in adulthood (2, 3), the occurrence of hypertension in adolescence is closely related to future target organ injuries (such as coronary artery calcification, ventricular hypertrophy, and increased carotid intima-media thickness) (4, 5). Previous studies have indicated that earlier onset of HTN would bring longer treatment cycle, harder BP control, and worse prognosis (2, 6). Therefore, understanding the prevalence and risk factors of hypertension among children and adolescents has the important public health and clinical significance (7).
Blood pressure is affected by physical and psychological state, white coat, and other aspects, which is prone to false positive of hypertension, resulting in unnecessary medical treatment, family burden, and psychological panic. Standardized BP measurement is essential to accurately understand the status of hypertension in children and adolescents. The American Association of Pediatrics “Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents” (AAP2017) (4) and 2018 Chinese health standard (CHS2018) “National Blood Pressure Reference for Chinese Han Children and Adolescents Aged 7–17 Years” (8) recommended that hypertension definition in children and adolescents should be based on at least three separate visits, with an interval of no less than 2 weeks. However, most epidemiological surveys about prevalence of hypertension have been conducted at only one occasion. At present, global prevalence of hypertension based on three separate visits among children and adolescents aged 6–19 years is 4.0% (9). However, limited studies based on three separate visits in China have been carried out. A study enrolled 44,396 urban children aged 6–17 from six major cities in China, and indicated that prevalence of hypertension was 4.0% (10). Another survey involving 7,786 adolescents aged 12–17 in two cities showed that prevalence of hypertension was 5.9% based on AAP2017 (11). We can find hypertension prevalence varied in different areas of China, considering China’s vast territory and large population, relevant research is still insufficient, especially in developed areas with a dense population.
Therefore, we conducted a large school-based study in Suzhou, a metropolis of the Yangtze River Delta in China, aiming to evaluate the prevalence of hypertension and hypertension subtype at three separate visits, and identify relevant risk factors.
The current study was based on a large-scale ongoing school-based monitoring program (HPPCA) conducted in Suzhou, China. Detailed information about HPPCA has been published elsewhere (12). In short, HPPCA provided free annual health check-ups for all school-based students aged 6–17 years in Suzhou to assess the growth and development of children and adolescents. Physical examinations were conducted at general hospitals, disease prevention and control centers, or community healthcare facilities.
During 2020 to 2021, 60 public schools, including two primary schools, two junior high schools and two senior high schools from 10 counties/districts, were chosen using stratified random sampling method. All the students from the selected schools were invited to participate in the survey. Notably, participants with significant organ (i.e., heart, lung, liver, kidney) diseases and abnormal body changes, disabilities, and deformities were not included in this study. Finally, a total of 59,679 children and adolescents aged 7–17 years were included in this present study after excluding incomplete anthropometric information (n = 136).
All HPPCA work was carried out with the consent of participants and their parents. This study was approved by the Ethics Committee of Suzhou Center for Disease Prevention and Control.
All the physical examinations were carried out by professionally trained health workers using the same type of age-appropriate equipment and following the same procedures. Weight and height were measured with children in light clothing and without shoes. Height and weight were accurate to 0.1 cm and 0.1 kg, respectively. Body mass index (BMI) was calculated as weight (kg) divided by the square of the height (m) (12). Underweight, normal weight, overweight, and obesity were defined according to the latest Chinese Health standards of age- and sex-specific BMI cutoffs for children and adolescents, respectively (13, 14).
Systolic BP (SBP) and diastolic BP (DBP) were measured using validated oscillometric devices (OMRON HBP-1300, HBP-1320, etc.) after each subject had rested for at least 15 min in a sitting position. An appropriate cuff was used to measure BP in children and adolescents. In total, three consecutive BP values were measured at 2-min intervals each time, and the average of the two closest BP readings was recorded.
Hypertension was defined as systolic BP (SBP) and/or diastolic BP (DBP) equal to or above the age-, sex-, and height-specific 95th percentile according to CHS2018 (8). Participants with hypertension at the first visit should be underwent a second BP measurement at least 2 weeks later; if BP was more than 95th percentile at the second visit, a third BP measurement should be taken following the same process. Confirmed hypertension was defined as simultaneously BP meeting above or equal to 95th percentile at three separate visits.
In order to distinguish hypertension phenotypes, isolated systolic hypertension (ISH) was defined as SBP ≥ P95 and DBP < P95, isolated diastolic hypertension (IDH) was defined as DBP ≥ P95 and SBP < P95, while systolic and diastolic hypertension (SDH) was defined as SBP ≥ P95 and DBP ≥ P95. Meanwhile, children with hypertension was be staged. Stage 1 is defined by BP between the 95th and 99th percentiles plus 5 mm Hg. Stage 2 is defined by BP ≥ 99th percentile plus 5 mm Hg.
Continuous variables were described as means ± SDs, while categorical variables were presented as numbers and percentages. Considering the differences in the age and sex distributions between our sample and the total population, we standardized the prevalence estimates by age and sex on the basis of 2020 Suzhou population census data.1 In order to compare with other researches, prevalence of hypertension were presented based on CHS2018 (8), AAP2017 (4), and CHL2018 (15), respectively. Estimate values (95% CIs) were presented.
In total, two sample Student’s t-tests (for continuous variables) or chi-square test (for categorical variables) were used to compare the differences across subgroups. Various socioeconomic status (SES) including relatively high SES (HSES) and relatively low SES (LSES) were distinguished based on GDP per capita from the statistics in Suzhou.2 Binary logistic regression was performed to identify related factors using hypertension at three visits as the dependent variable after adjustment for related covariates. All the statistical analyses were performed in R 3.2.2 software. The statistical significant level was defined as P-values less than 0.05 (2-sided).
In total, 59,679 children and adolescents aged 7–17 years were included in our analysis at the first visit, mean age was 12.3 ± 3.0 years. Among them, 31,106 (52.1%) were boys, 28,750 (48.2%) were urban residents, and 31,261 (52.4%) were among LSES group. Mean values of SBP and DBP were 110.5 ± 13.4 and 68.7 ± 8.6 mm Hg, respectively. Prevalence of underweight, overweight, and obesity were 4.5, 18.1, and 15.8%, respectively (Table 1).
Compared with boys, girls had lower height, weight, and BMI (P < 0.001). There was no significant difference in residential region between boys and girls (P = 0.124). LSES group seemed to have higher portion of boys than HSES groups (P = 0.008). At all three visits, boys obviously had higher SBP than girls (P < 0.001), while girls had higher DBP than boys at second visit (P = 0.013), DBP did not show significant differences between boys and girls at first visit and third visit (P > 0.05).
Based on the CHS2018, we identified 12,160 hypertensive subjects at the first visit, with a crude prevalence of 20.4% (95% CI, 20.1–20.7%), the crude prevalence of hypertension at the second visit was 6.3% (95% CI, 6.1–6.5%). After 3 separate visits, 1,871 subjects had high BP, the crude and standardized prevalence of confirmed hypertension was 3.1% (95% CI, 3.0–3.3%]), and 2.9% (95% CI, 2.8–3.1%), respectively (Figure 1 and Table 2). Similar decreased trends of hypertension prevalence with three visits were found in boys and girls (Supplementary Table 1).
The prevalence of crude hypertension was 5.8% (95% CI, 5.2–6.4%) using AAP2017 and 4.9% (95% CI, 4.3–5.5%) using CHL2018, both of which were significantly higher than the estimate (3.1%) based on the CHS2018 (P < 0.001). Similar results were found among boys and girls (Supplementary Table 2).
Prevalence of hypertension phenotypes defined by CHS2018 were presented from the first visit to the third visit as in Table 2 and Supplementary Table 1. In total, the confirmed hypertension prevalence for stages 1 and 2 were 2.6 and 0.6%. While, the prevalence of confirmed ISH, IDH, and SDH were 1.9, 0.3, and 0.9%, respectively.
In total, the proportions of ISH slightly increased from visit 1 to visit 3 (50.4, 54.3, and 59.7%, respectively), and the proportions of IDH slightly decreased (30.7, 17.2, and 10.9% from visit 1 to visit 3, respectively), while the proportions of SDH increased from visit 1 to visit 2, and stabilized at visit 3 (18.9, 29.2, and 29.4%, respectively). Similar trends were found in both boys and girls (Figure 2). Proportions of hypertension phenotypes by age group and weight status at the third visit were presented (Supplementary Figure 1). Boys aged 12–17 years old and girls aged 7–11 years old had the highest proportion of ISH, overweight boys had the highest proportion of ISH, while normal weight girl had the highest proportion of ISH.
As shown in Table 3, high age, urban, HSES, thinness, overweight, and obesity were associated with hypertension at first visit. At the third visit, boys [OR, 1.137 (95% CI, 1.033–1.251)], high age [OR, 3.326 (95% CI, 2.950–3.751)], urban residents [OR, 1.579 (95% CI, 1.417–1.760)], HSES [OR, 1.156 (95% CI, 1.039–1.286)], and adiposity including overweight [OR, 1.883 (95% CI, 1.665–2.129)], and obesity [OR, 4.049 (95% CI, 3.625–4.523)] were associated with increased risk of confirmed hypertension. While those with thinness had a lower risk [OR, 0.457 (95% CI, 0.306–0.683)], when compared with normal weight subjects. We evaluated these risk factors across three separate visits; and found different risk levels at different visits. For example, the OR of obesity to hypertension increased from the first visit [2.374 (95% CI, 2.253–2.501)] to the third visit [4.049 (95% CI, 3.625–4.523)] (P < 0.001).
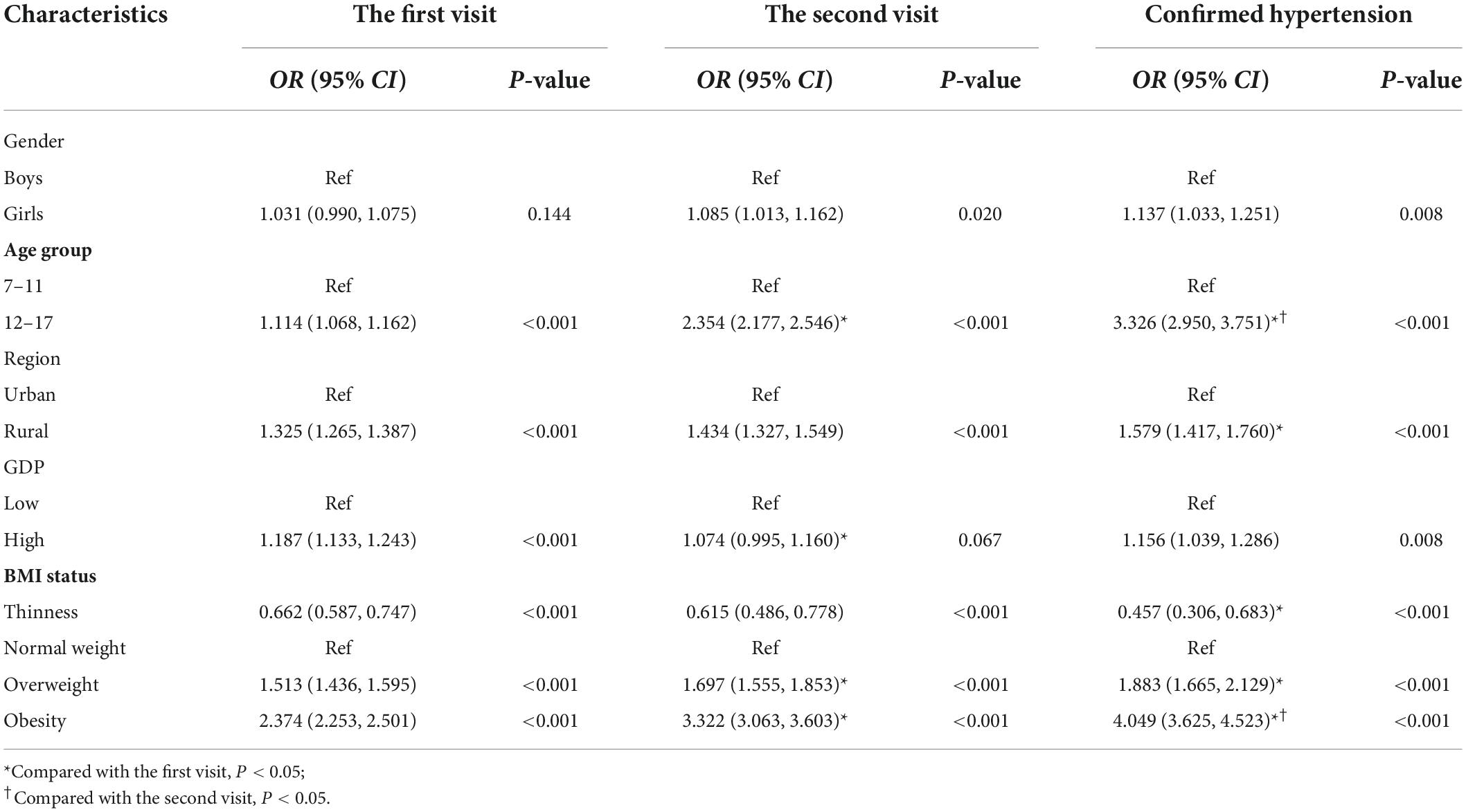
Table 3. Multivariate logistic regression analyses of the risk factors for hypertension at three separate visits.
To our knowledge, this is the largest study to investigate hypertension prevalence after three separate visits and its risk factors among school-based children and adolescents in China. It provides BP status reference for developed areas in China. We also found that boys, high age, urban residents, HSES, and abnormal weight (thinness, overweight, and obesity) were associated with confirmed hypertension.
Most of the previous studies reporting the prevalence of hypertension among children and adolescents have been conducted at only one occasion. Based on the China Health and Nutrition Survey in 2015, prevalence of hypertension among children and adolescents aged 7–17 years was 19.2% defined by CHL2018 (16), and 12.8% defined by CHS2018 (17). These results were significantly higher than our results, which might be explained mainly by the number of BP visits. Substantial decreases in the prevalence of hypertension in children across different visits were reported by previous studies. A school-based survey performed in 7,832 Chinese children and adolescents showed that the prevalence of hypertension decreased substantially across three separate visits, with the prevalence of 17.2, 8.6, and 4.9%, respectively (18). In addition, a meta-analysis including 21 studies with 179,561 subjects aged 3–20 years showed that the prevalence of hypertension was 12.1, 5.6, and 2.7% across the three separate visits (19). In this study, prevalence of hypertension also decreased similarly across three visits. In sum, about 70–80% subjects with hypertension at the first visit returned to normal BP at the third visit. Overestimate of hypertension prevalence among children would result in psychological panic of parents and children, and unnecessary medical and family burden. These findings emphasized that BP should be measured on at least three different occasions to estimate the true prevalence of hypertension, which was also recommended by CHS2018, AAP2017, and CHL2018.
A survey involving 7,786 adolescents aged 12–17 years in two cities showed that the prevalence of hypertension was 5.9% based on AAP2017, and 8.4% based on CHL2018 (11), both of which were higher than results in this study using same references. Other studies conducted in China such as Jinan (4.9%) (18) and Chongqing (6.0%) (20) also had higher prevalence of hypertension. Recently, a systematic review and meta-analysis included 25 studies of 341,281 participants reported the prevalence of hypertension among Chinese children was 9.8% (95% CI: 7.9–11.9%) (21). Another meta- analysis included 39 articles of 796,512 subjects indicated hypertension prevalence was 9.1% (95% CI: 7.4–10.7%) (22). The great discrepancy with our study might be the uncertain number of BP visits and the BP references in the review. A review reported that global prevalence of hypertension based on three separate visits from 47 researches of 186,630 children and adolescents aged 6–19 years was 4.00% (95% CI, 3.29–4.78%) (9), another previous review report included 21 studies with 179,561 children aged 3–20 years was 2.7% (95% CI = 2.1–3.3%) (19). Our result lay between these two results (9, 19).
Overweight/obesity have been found to increase the risk of hypertension at three visits. With the increases of BP follow-up times, the correlations between overweight and obesity with hypertension increased compared with the normal children. The Chinese National Survey on Students’ Constitution and Health (1995–2014) showed that the attributable risk ratio of overweight and obesity with hypertension was 19.2% in 2014 (23). The obesity-induced adolescent hypertension may be mediated partly by the activation of the sympathetic nervous system, which included insulin resistance and secretion of leptin. It highlights that keeping a healthy weight can serve as an important intervention to control BP level in children and adolescents. Boys had higher prevalence of elevated BP than girls in our study, higher prevalence of overweight and obesity among boys may explain this phenomenon to some extent (24). Meanwhile, adolescents aged 12–17 years had higher risk of hypertension than children aged 7–11 years, and hypertension prevalence of children aged 7–11 years decreased significantly greater at the second and third visit than adolescents aged 12–17 years. Possible explanations for the age differences included intense hormonal changes and elevated insulin resistance during pubertal period. It suggested that repeated blood pressure measurements had a greater significance for the low age group. Relative higher hypertension prevalence in adolescents determined that hypertension detection of adolescents of the high age group should be taken as the key management population, which is consistent with previous study (10, 18).
Considering regional and ethnic differences in BP, in order to compare with other researches, we also applied AAP2017 and CHL2018 to evaluate hypertension prevalence. Compared with the results using CHS2018, the prevalence of hypertension across three visits were higher applying the AAP2017, and results of CHL2018 were the highest. Our findings were consistent with the results with relevant studies based on a single BP visit (25, 26). However, relevant comparisons using CHS2018 were limited. A study among the Chinese children and adolescents evaluated hypertension prevalence across three visits, and showed that results of CHL2018 were higher than those using AAP2017 (11). The divergence in height distributions may explain the difference in hypertension prevalence applying various references. Great height differences for both males and females at the same percentile among various references existed, and the gap increased in late puberty, especially. These differences would bring different BP values of the same age, sex, and height percentile (25). One point needs to be noted, a statistical definition is still the principal method for childhood hypertension evaluation. In the future, longitudinal studies should be conducted to explore the clinical effects of different BP levels, which would be useful for accurate assessment of BP (27).
Previous studies indicated that young adults with ISH, IDH, and SDH were all positively associated with higher risks of CVD than non-hypertensive persons, with SDH being the highest, and IDH higher or close to ISH (28, 29). Nevertheless, impact of ISH, IDH, and SDH during childhood on future CVD are still limited, identification of children with ISH, IDH, and SDH may improve to identify risk level. ISH usually reflects essential hypertension (30). In the present study, it was the most frequent phenotype, its proportion increases with times of BP measurements. Interestingly, there were substantial differences in the proportions of hypertension subtypes between boys and girls, such as 66.7% of ISH in boys and 51.6% of ISH in girls at third visit (30). We spectated that puberty and hormones may play a very important role on hypertension development. Previous study indicated estrogen was essential for the enhancement of endothelium-dependent vasodilation and regulation of smooth muscle cells.
Our study had several strengths. To our knowledge, this is the first study to report hypertension prevalence across three separate visits in eastern China using various references. Besides, the second and third visits were completed by the school’s healthcare personnel, keeping this school-based study with high-participation rate to minimize selection bias (second visit: 96.9%, third visit: 98.5%). In addition, BP measurements with favorable environment by familiar school personnel reduced white-coat hypertension and masked hypertension.
However, limitations of the present study should be noted. First, only children whose BP at least 95th percentile were followed to have the subsequent BP measurements, which would result in underestimated prevalence of hypertension. Second, since students were from only 1 developed region, the generalizability of the present findings might be limited to represent developed regions in China, and this needs to be confirmed. Third, we did not collect information about lifestyle factors (eating behavior, salt intake, and physical activity), mental health, and environmental exposures. Finally, a cross-sectional study design would limit us to identify causal associations of hypertension with risk factors, and health effects of hypertension should be further evaluated.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Ethics Committee of Suzhou Center for Disease Prevention and Control. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
HY and AG contributed to the design and concept of the manuscript. JH was responsible for the analysis, interpretation of data, and manuscript drafting. DH, ZD, and BH organized the database. HL performed the statistical analysis. HS and JY were responsible for the critical revision of the manuscript for intellectual content. All authors wrote this manuscript and gave final approval of the submitted and published versions.
This study was supported by the National Natural Science Foundation of China (grants: 81602911 and 82204070), Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD), and Gusu Health Talents Program Training Project in Suzhou, China (GSWS2020100).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2022.976317/full#supplementary-material
1. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2018) 392:1789–858. doi: 10.1016/S0140-6736(18)32279-7
2. Yang L, Sun J, Zhao M, Liang Y, Bovet P, Xi B. Elevated blood pressure in childhood and hypertension risk in adulthood: a systematic review and meta-analysis. J Hypertens. (2020) 38:2346–55. doi: 10.1097/HJH.0000000000002550
3. Azegami T, Uchida K, Tokumura M, Mori M. Blood pressure tracking from childhood to adulthood. Front Pediatr. (2021) 9:785356. doi: 10.3389/fped.2021.785356
4. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. (2017) 140:e20171904. doi: 10.1542/peds.2017-1904
5. Li Z, Duan Y, Zhao M, Magnussen CG, Xi B. Two-year change in blood pressure status and left ventricular mass index in Chinese children. Front Med. (2021) 8:708044. doi: 10.3389/fmed.2021.708044
6. Wang C, Yuan Y, Zheng M, Pan A, Wang M, Zhao M, et al. Association of age of onset of hypertension with cardiovascular diseases and mortality. J Am Coll Cardiol. (2020) 75:2921–30. doi: 10.1016/j.jacc.2020.04.038
7. Gartlehner G, Vander Schaaf EB, Orr C, Kennedy SM, Clark R, Viswanathan M. Screening for hypertension in children and adolescents: updated evidence report and systematic review for the US preventive services task force. JAMA. (2020) 324:1884–95. doi: 10.1001/jama.2020.11119
8. Dong Y, Ma J, Song Y, Dong B, Wang Z, Yang Z, et al. National blood pressure reference for Chinese Han children and adolescents aged 7 to 17 years. Hypertension. (2017) 70:897–906. doi: 10.1161/HYPERTENSIONAHA.117.09983
9. Song P, Zhang Y, Yu J, Zha M, Zhu Y, Rahimi K, et al. Global prevalence of hypertension in children: a systematic review and meta-analysis. JAMA Pediatr. (2019) 173:1154–63. doi: 10.1001/jamapediatrics.2019.3310
10. Dong J, Dong H, Yan Y, Cheng H, Zhao X, Mi J, et al. Prevalence of hypertension and hypertension phenotypes after three visits in Chinese urban children. J Hypertens. (2021) 40:1270–7. doi: 10.1097/HJH.0000000000002977
11. Liu K, Li C, Gong H, Guo Y, Hou B, Chen L, et al. Prevalence and risk factors for hypertension in adolescents aged 12 to 17 years: a school-based study in China. Hypertension. (2021) 78:1577–85. doi: 10.1161/HYPERTENSIONAHA.121.17300
12. Hu J, Liu J, Wang J, Shen M, Ge W, Shen H, et al. Unfavorable progression of obesity in children and adolescents due to Covid-19 pandemic: a school-based survey in China. Obesity. (2021) 29:1907–15. doi: 10.1002/oby.23276
13. National Health Commission of the People’s Republic of China [NHCPRC].Screening for Overweight and Obesity among School-Age Children and Adolescents. Beijing: National Health Commission of the People’s Republic of China (2018).
14. National Health Commission of the People’s Republic of China [NHCPRC].Screening Standard for Malnutrition of School-Age Children and Adolescents. Beijing: National Health Commission of the People’s Republic of China (2014).
15. Joint Committee for Guideline Revision [JCGR]. 2018 Chinese guidelines for prevention and treatment of hypertension-a report of the revision committee of Chinese guidelines for prevention and treatment of hypertension. J Geriatr Cardiol. (2019) 16:182–241. doi: 10.11909/j.issn.1671-5411.2019.03.014
16. Ye X, Yi Q, Shao J, Zhang Y, Zha M, Yang Q, et al. Trends in prevalence of hypertension and hypertension phenotypes among chinese children and adolescents over two decades (1991-2015). Front Cardiovasc Med. (2021) 8:627741. doi: 10.3389/fcvm.2021.627741
17. Ma SJ, Yang L, Zhao M, Xi B. [Changing trends in the levels of blood pressure and prevalence of hypertension among chinese children and adolescents from 1991 to 2015]. Chin J Epidemiol. (2020) 41:178–83. [Article in Chinese]. doi: 10.3760/cma.j.issn.0254-6450.2020.02.008
18. Zhang Q, Yang L, Zhang Y, Zhao M, Liang Y, Xi B. Hypertension prevalence based on three separate visits and its association with obesity among Chinese children and adolescents. Front Pediatr. (2019) 7:307. doi: 10.3389/fped.2019.00307
19. Sun J, Steffen LM, Ma C, Liang Y, Xi B. Definition of pediatric hypertension: are blood pressure measurements on three separate occasions necessary? Hypertens Res. (2017) 40:496–503. doi: 10.1038/hr.2016.179
20. Zhang XX, Xiong F, Zhu M, Luo YY, Wang FL, Zeng Y, et al. [An investigation of the prevalence situation of hypertension among children from 6 to 18 years old in Chongqing]. Chongqing Med. (2016) 45:1951–3. [Article in Chinese]. doi: 10.3969/j.issn.1671-8348.2016.14.025
21. Wang L, Song L, Liu B, Zhang L, Wu M, Cao Z, et al. Trends and status of the prevalence of elevated blood pressure in children and adolescents in China: a systematic review and meta-analysis. Curr Hypertens Rep. (2019) 21:88. doi: 10.1007/s11906-019-0992-1
22. Xu CX, Du CX, Wu GR, Guo BB. [Meta analysis of prevalence and influencing factors of hypertension in Chinese children and adolescents]. Modern Prevent Med. (2021) 48:4276–80, 311. [Article in Chinese].
23. Dong Y, Ma J, Song Y, Ma Y, Dong B, Zou Z, et al. Secular trends in blood pressure and overweight and obesity in Chinese boys and girls aged 7 to 17 years from 1995 to 2014. Hypertension. (2018) 72:298–305. doi: 10.1161/HYPERTENSIONAHA.118.11291
24. He H, Yang S, Qiu N, Qiao L, Ding Y, Luo J, et al. Sex-specific differences in related indicators of blood pressure in school-age children with overweight and obesity: a cross-sectional study. Front Pediatr. (2021) 9:674504. doi: 10.3389/fped.2021.674504
25. Zhang M, Zhang HT, Zha RS, Gui GP, Han D, Hu J, et al. Comparison of China reference with different national and international references: the prevalence of high blood pressure in 695,302 children and adolescents in a metropolis of Yangtze River Delta, China. Int J Hypertens. (2021) 2021:3976609. doi: 10.1155/2021/3976609
26. Fan H, Hou D, Liu J, Yan Y, Mi J. Performance of 4 definitions of childhood elevated blood pressure in predicting subclinical cardiovascular outcomes in adulthood. J Clin Hypertens. (2018) 20:508–14. doi: 10.1111/jch.13201
27. Bouhanick B, Sosner P, Brochard K, Mounier-Vehier C, Plu-Bureau G, Hascoet S, et al. Hypertension in children and adolescents: a position statement from a panel of multidisciplinary experts coordinated by the French society of hypertension. Front Pediatr. (2021) 9:680803. doi: 10.3389/fped.2021.680803
28. Yano Y, Stamler J, Garside DB, Daviglus ML, Franklin SS, Carnethon MR, et al. Isolated systolic hypertension in young and middle-aged adults and 31-year risk for cardiovascular mortality: the chicago heart association detection project in industry study. J Am Coll Cardiol. (2015) 65:327–35. doi: 10.1016/j.jacc.2014.10.060
29. Lee H, Yano Y, Cho SMJ, Park JH, Park S, Lloyd-Jones DM, et al. Cardiovascular risk of isolated systolic or diastolic hypertension in young adults. Circulation. (2020) 141:1778–86. doi: 10.1161/CIRCULATIONAHA.119.044838
Keywords: adolescents, blood pressure, children, hypertension, risk factors, three visits
Citation: Hu J, Ding Z, Han D, Hai B, Lv H, Yin J, Shen H, Gu A and Yang H (2022) Prevalence of hypertension and related risk factors among children and adolescents at three separate visits: A large school-based study in China. Front. Pediatr. 10:976317. doi: 10.3389/fped.2022.976317
Received: 23 June 2022; Accepted: 29 August 2022;
Published: 23 September 2022.
Edited by:
Vera Hermina Koch, University of São Paulo, BrazilReviewed by:
Paulo Cesar Koch Nogueira, Federal University of São Paulo, BrazilCopyright © 2022 Hu, Ding, Han, Hai, Lv, Yin, Shen, Gu and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Aihua Gu, YWlodWFndUBuam11LmVkdS5jbg==; Haibing Yang, eWhiaW5nMTExQDE2My5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.