
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr. , 05 October 2022
Sec. Pediatric Pulmonology
Volume 10 - 2022 | https://doi.org/10.3389/fped.2022.974363
This article is part of the Research Topic Women in Pediatric Pulmonology 2021 View all 4 articles
 Taryn Jones1*
Taryn Jones1* Emmah Baque2
Emmah Baque2 Kerry-Ann F. O’Grady1,3
Kerry-Ann F. O’Grady1,3 Vikas Goyal3,4,5,6
Vikas Goyal3,4,5,6 Anne B. Chang3,4,7
Anne B. Chang3,4,7 Stewart G. Trost1,8
Stewart G. Trost1,8Background: Current bronchiectasis management guidelines recommend regular physical activity but a large proportion of children with bronchiectasis do not meet public health recommendations which call for 60 min or more of moderate-to-vigorous intensity physical activity daily. Knowing the factors that influence physical activity in children with bronchiectasis is necessary for the development of effective interventions to increase physical activity in this patient group. The objective of this study was to identify facilitators and barriers to physical activity in children with bronchiectasis unrelated to cystic fibrosis (CF) from the perspectives of children and their parents.
Materials and methods: This was a qualitative study informed by the theoretical domains framework (TDF). Children aged 7–15 years (8.8 years, 8.4–11.0) (median, interquartile range) and parents (45.8 years, 39.7–48.3) completed separate, semi-structured interviews (n = 21). Recordings were transcribed verbatim, and barriers and facilitators related to each TDF domain deductively coded. Emergent themes were inductively derived via consensus moderation.
Results: From the perspectives of children, fun with friends, organized sport and activities, and family co-participation in physical activity emerged as facilitators. Inability to keep up with their peers and time on technology emerged as barriers. From the perspectives of parents, instrumental and logistic support for physical activity and supportive social and physical activity environments emerged as facilitators, while management of symptoms associated with bronchiectasis emerged as a barrier.
Conclusion: Programs to increase physical activity in children with bronchiectasis should be fun, accessible, provide opportunities for social interaction and address barriers related to exercise tolerance, perceived competence, and presence of respiratory symptoms.
Bronchiectasis is a chronic lung disease with abnormal peripheral airway dilatation objectively documented on a chest computed tomography scan (1, 2). Globally, over the last two decades the prevalence of bronchiectasis is increasing and recognized as an important cause of chronic respiratory disease and morbidity in children and adults (3, 4). The disease process alters the mucociliary clearance that contributes to persistent infection, airway obstruction and progressive lung damage if not managed early and effectively (5). Children with bronchiectasis present with a persistent wet cough, shortness of breath and poor exercise tolerance (1, 6). Living with bronchiectasis symptoms impacts the daily lives of children including schooling, play, physical activity, and general wellbeing (7, 8). The long-term impacts of bronchiectasis include higher prevalence of chronic diseases including depression, anxiety, cardiac dysfunction, in addition to poorer quality of life (QoL) outcomes (8–12). Current bronchiectasis treatments include pharmacological agents and airway clearance techniques along with general recommendations to maintain a healthy diet and regular physical activity (13).
There is strong and consistent evidence in support of the beneficial effects of regular physical activity on cardiovascular fitness and musculoskeletal health in children (14, 15). Physical activity also improves airway clearance (16), one mainstay treatment of people with bronchiectasis (13, 17). Further, there is evidence to conclude that physical activity can positively impact mental health, in addition to the positive impacts on blood pressure, adiposity and cardiovascular risk factors such as inflammatory biomarkers (14). Furthermore, children who accrue 60 min of moderate to vigorous physical activity (MVPA) each day have a lower risk of developing chronic diseases such as type II diabetes and metabolic syndrome later in adulthood (18).
Current guidelines for the treatment and management of bronchiectasis recommend regular physical activity (19, 20). Yet, the available evidence suggests that a large proportion of children with bronchiectasis do not meet public health recommendations for physical activity and that interventions to promote regular physical activity are needed (21, 22). In a recent cross-sectional study, Joschtel et al. (21) recruited 46 children with bronchiectasis [mean age ± standard deviation (SD) 7.5 ± 2.6 years] and objectively measured physical activity over 7 days. An accelerometer was used to determine daily time spent in sedentary, light, and MVPA. As a percentage of waking hours, participants were sedentary for 57.5% of the time, in light-intensity physical activity for 38.5% of the time and in MVPA for just 6.7% of the time. From this study, only two participants (5.6%) met the daily 60-min MVPA recommendation as opposed to 42% of healthy children in the normative comparison group.
Currently, there is a large body of research exploring barriers and facilitators to physical activity in the typically developing pediatric population (23–25). Sterdt et al. (24) conducted a systematic review of reviews on the correlates of physical activity in children and adolescents. Sex (male), age, ethnicity, parental education, family income, and socioeconomic status and parent education emerged as demographic and biological factors consistently associated with physical activity. Perceived competence, self-efficacy perceptions, goal orientation, and perceived barriers emerged as psychological, cognitive and emotional factors consistently associated with physical activity. Previous physical activity and participation in community sports emerged as behavioral attributes and skills consistently associated with physical activity. Parental support and support from significant others emerged as social and cultural factors consistently associated with physical activity, while access to recreational facilities, programs, and time outdoors emerged as physical environmental factors consistently associated with physical activity.
Fewer studies have examined barriers and facilitators in children with chronic health conditions. Pianosi and Davis (26) examined selected correlates of physical activity in children with asthma. Positive self-perceptions of motor skills and attitudes toward physical activity were identified as facilitators to participation in physical activity, while being affected by overweight or obesity was identified as a barrier. In a literature review focused on children with chronic respiratory conditions, Denford et al. (27) completed a synthesis of qualitative work exploring the barriers and facilitators to physical activity in children and young people with cystic fibrosis (CF). From the seven studies reviewed, nine themes were identified perceptions of physical activity, value attributed to physical activity, social influences, competing priorities, fluctuating health, normality, control beliefs, coping strategies and availability of facilities.
While there is evidence for healthy children and children with asthma and CF, to date, no studies have examined barriers and facilitators of physical activity in children with non-CF bronchiectasis. Given the important differences between children with CF and those without (1), bronchiectasis-specific data are required. Therefore, in this study we aimed to identify facilitators and barriers to physical activity in children with bronchiectasis from the perspectives of the parents and children.
Participants for this study were recruited from respiratory clinics at the Queensland Children’s Hospital (QCH) or Gold Coast University Hospital (GCUH). The QCH and GCUH are large tertiary public hospitals that offer free or low-cost services as part of Australian public health system. Before or after their scheduled appointment, a member of the research team (TJ) discussed the study requirements with families to gauge interest and screen for eligibility. To be eligible, children (1) had a confirmed bronchiectasis diagnosis not related to CF; (2) were aged 6–15 years; and (3) were being managed by a respiratory physician. Families expressing an interest in the study were given a participant information sheet and consent form to consider their participation in the study. Prior to participation in the study, written informed consent was obtained from parents/guardians. Ethical approval for this study was received by the Queensland Children’s Hospital Human Research Ethics Committee (LNR/19/QCHQ/54135).
The theoretical domains framework (TDF) informed the development of the interview guides for parents and children. The TDF is designed to assist researchers and health practitioners understand health behavior change, design interventions, and assess implementation problems (28, 29). The framework was developed and validated by Michie et al. (28) through a robust consensus process with a multi-disciplinary group of behavioral and implementation science researchers. This group identified 128 theoretical constructs from 33 existing behavior change and psychological frameworks relevant to implementation science to include 14 theoretical domains in the TDF.
Separate interview guides were developed for children (see Table 1) and parents (see Table 2) based on selected domains of the TDF. For example, the question, “Do you feel that you are able to play and join in physical activity in the same way as your friends?” reflected the “Beliefs about Capabilities” domain of the TDF. Similarly, the question to parents “Do you feel your child has the skills needed to play with their peers?” reflected the “Skills” domain of the TDF. Prior to recruiting participants, the interview guide was piloted with three parents and two children not included in the study. Following the pilot, the ordering of some questions was modified, and additional conversational prompts included. The pilot interviews were not included for analysis. The parent interview guide included questions that related to the domains of knowledge, skills, social/professional role and identity, beliefs about capabilities, optimism, beliefs about consequences, reinforcement, intensions, environmental context and resources, social influences and emotion. The child interview guide included questions that related to the domains of knowledge, skills, social/professional role and identity, beliefs about capabilities, optimism, beliefs about consequences, reinforcement, intensions, social influences and emotion.
Participants completed a single interview with a researcher (TJ) via videoconference (due to COVID-19 restrictions). Parent interviews occurred prior to child interviews. The parent was present during the child’s interview (either sitting with or nearby), but the questions were directed to the child. Interviews were digitally recorded and transcribed verbatim. Transcriptions were compared to the recording for accuracy, fully de-identified, and assigned a unique study identification number. Recruitment to the study continued until saturation had been reached (i.e., no new information was offered by participants). Interviews were completed between August 2020 and July 2021.
Qualitative data from the interviews were analyzed using thematic analysis. The analysis was completed in two stages with a deductive then inductive approach. The first stage involved coding participant’s responses to questions in each TDF domain as a “barrier” or “facilitator.” Initially, two members of the research team (EB and TJ) read through three randomly selected transcripts (two child and one parent) line by line and coded responses as a “barrier” or “facilitator.” Barriers were responses that referred to sentiments that prevented or hindered children’s physical activity. Facilitators were responses that referred to views that increased or supported children’s physical activity. The researchers then compared their independent coding to verify agreement and resolve discrepancies. After agreement was verified, TJ read each transcript and coded responses as either a “barrier” or “facilitator.”
Stage two of data analysis involved separate thematic analyses of text coded as “barriers” or “facilitators” in stage one. An inductive approach was used to identify recurrent themes for children and parents using the six steps identified by Braun and Clarke (30) which include: becoming familiar with the interview, initial coding, generating themes, reviewing themes, defining the name of the themes, and writing up the analysis. After reading the transcripts TJ commenced initial coding. Initial codes were assigned based on the content of the transcript. For example, if a parent spoke about their backyard pool, this text would have two initial codes of “yard” and “swimming pool.” Throughout the initial coding phase, two members of the research team (EB and TJ) met to review the codes to ensure that the code names reflected the content of the transcripts and reach consensus on the codes. Once initial coding was complete, all members of the research team discussed initial code groupings based on the content and sentiments. Initial code groupings were then compared and aggregated to form subthemes. Differences in initial code grouping and subthemes were discussed until consensus was reached. From there, a process of consensus moderation was used to identify final emergent themes. Differences were discussed until consensus was reached and themes named. NVivo 12 (QSR International Pty. Ltd.) was used to manage and organize the textual data.
From the 21 families approached in hospital clinics, 11 families consented (11 parents and 10 children). All parent respondents were female, with a median age (IQR) of 45.7 (39.7–48.3) years. Eleven children were scheduled for an interview and ten children completed interviews (one child was unable to participate due to ongoing illness). Children were aged from seven to 15 years (8.8 years, 8.8–11.0). Two of the 10 children were females. Parent interviews ranged from 21 to 54 min (mean duration 33 ± 10.1 min) and child interviews between 12 and 28 min (mean duration 20 ± 5.6 min). Socio-economic indexes for areas (SEIFA) is derived from Australia’s census data and ranks areas according to relative socio-economic advantage and disadvantage (31). SEIFA scores are transformed into deciles where one represents the most disadvantaged areas and then represents the most advantaged. In the current study participant’s SEIFA decile ranged from three to eight, so was well distributed across low to high areas of socioeconomic status. Families who participated in this study resided in postcodes that offered a variety of affordable and accessible activities and organized sports.
The TDF domain, initial codes, initial code groupings, subthemes, and final emergent themes related to children’s facilitators and barriers to physical activity are shown in Tables 3, 4, respectively. From the perspectives of children, fun with friends, organized sport and activities, and family co-participation in physical activity emerged as facilitators. Difficulty of keeping up with their peers emerged as the primary barrier. Below, individual themes are presented with illustrative quotes from participants.
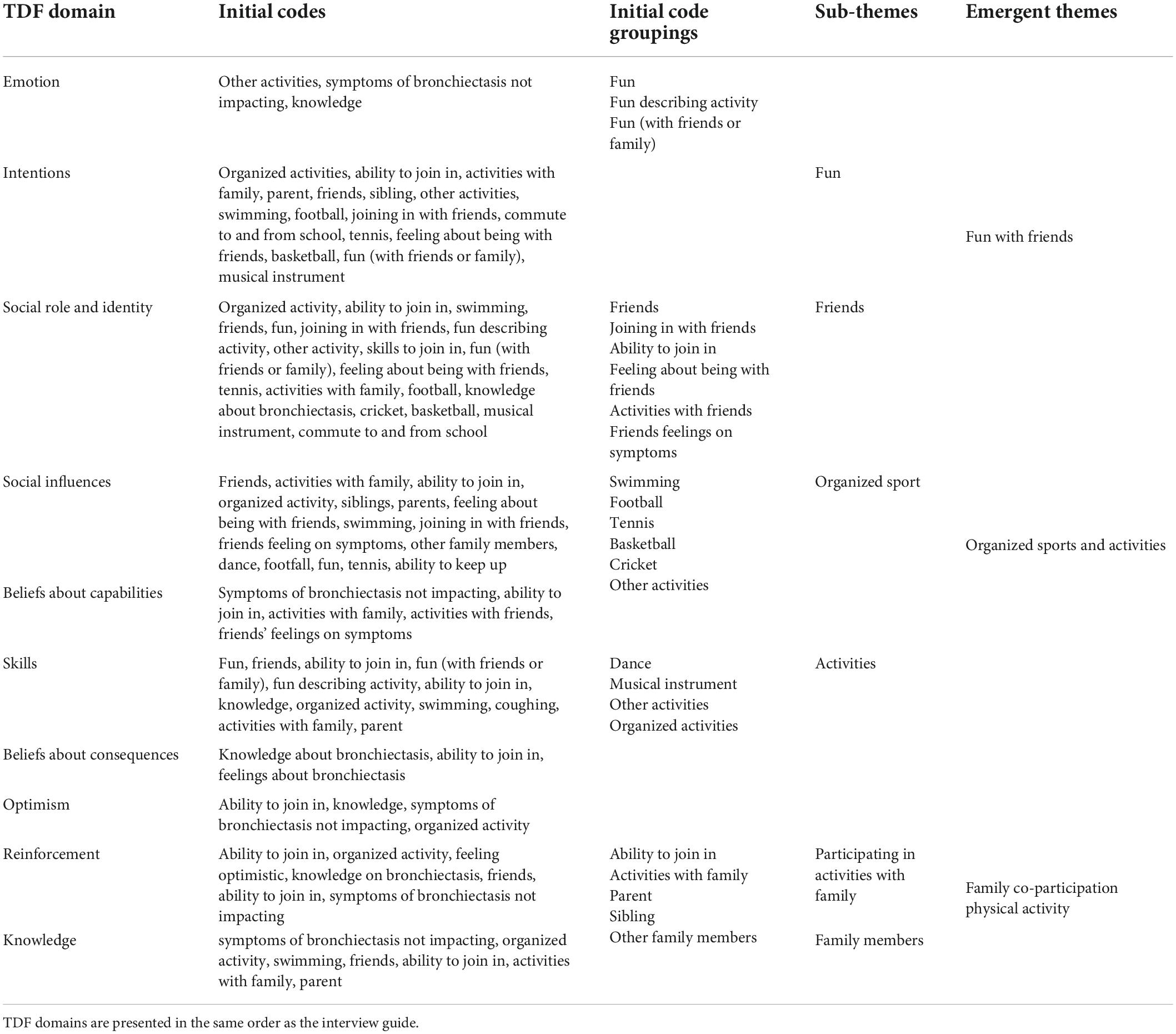
Table 3. Development of themes relating to facilitators for physical activity from the perspective of children.
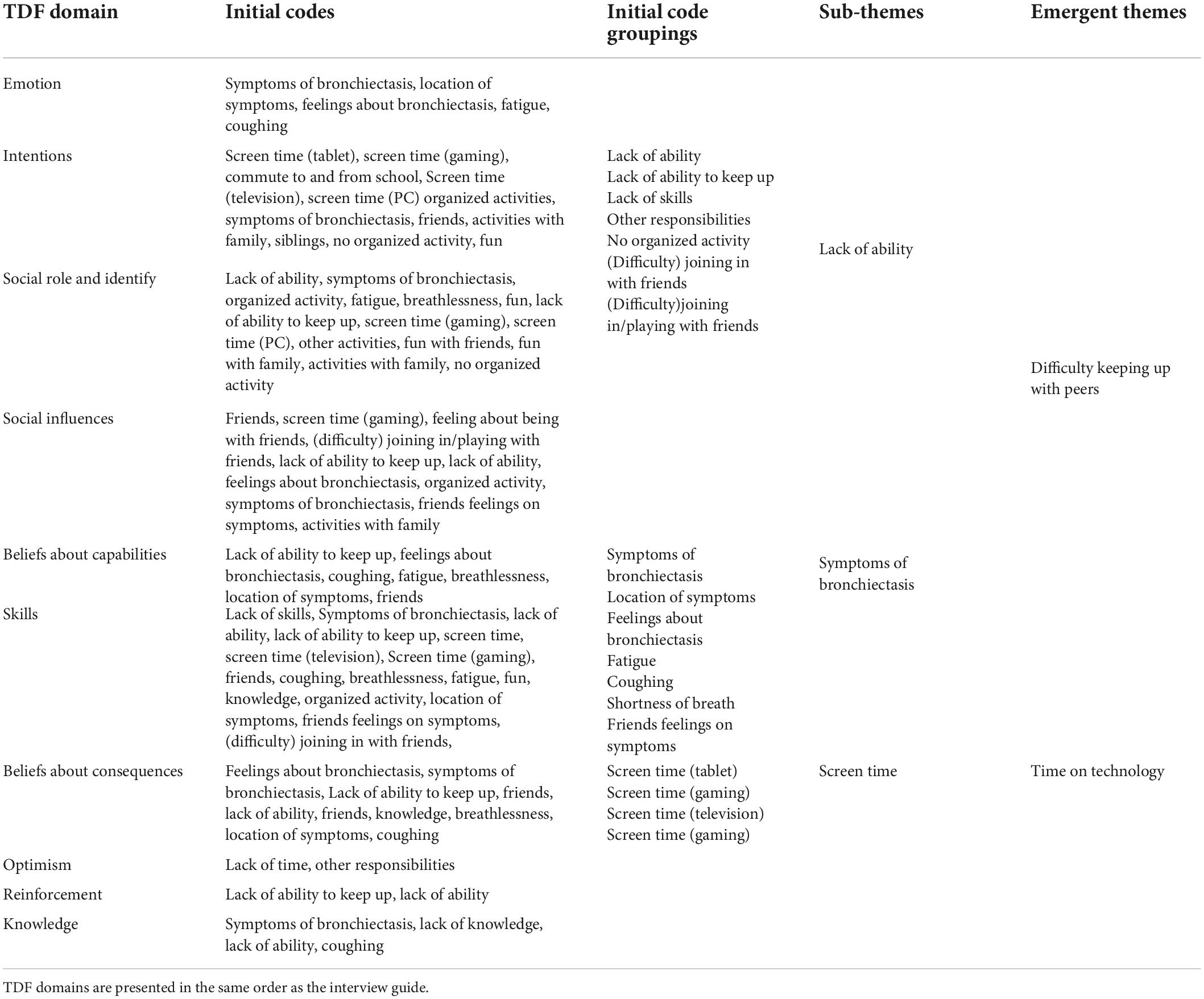
Table 4. Development of themes relating to barriers for physical activity from the perspective of children.
When discussing physical activity and games and play, children consistently spoke about having fun with their friends. Children reported they liked to play games with their friends, whether it be organized sport, school lunch time play or playground visits. They valued being included by their friends.
“I really like playing soccer, because I want to play soccer and I have my best friend that she normally comes over and we go down to the track…I like to go out and I like doing it with all my friends.” Ch04
“My friends get me to go up and make sure I am involved with the game.” Ch01
Most children talked about participation in organized sport and activities across the year. There were a large variety of activities with swimming and football [football (known as soccer in Australia), rugby league and Australian Rules Football] the most frequently reported. Common organized activities included dance and musical instruments.
“I played soccer, a bit of swimming, umm all different sports but soccer’s kinda the main one.” Ch06
“…in dancing I do ballet, tap, jazz, jazz funk… I’m going to start contemporary. I also play football but, I’m changing to boxing next year.” Ch11
Children spoke about their family and the activities they do together. Children spoke about their siblings and how they spend their time trampolining, bike riding and swimming being the most frequently mentioned activities.
“I play with (sister), we muck around with each other, and I play with (brother)… we bounce on the tramp” Ch04
“Sometimes me and my brother just go riding around the street.” Ch05
“…we get to do swimming with my mum and sister” Ch11
Children also spoke about time spent with parents for less structured activities such a bike riding, swimming and backyard ball games.
“…I hop on my bike and we run around, I ride around and mum follows me around” Ch07
“so basically, um, it’s really fun. Sometimes dad will take us to the park. Other times we’ll do a scooter. Sometimes we’ll catch up with some friends.” Ch08
“Yeah. I find it easy to go out and kick the footy with dad some afternoons.” Ch01
Children discussed how it was difficult for them to keep up with their friends when playing sports and doing physical activity. Children expressed the challenges in joining games or play as they perceived themselves to be slower at running and that they needed to practice new skills and activities more than their peers. All children spoke about how coughing and having difficulty breathing during exercise was a barrier to physical activity.
“…it was hard cause basically, I just stand there while everyone else was kicking goals and stuff.” Ch07
“like when I am running, my lungs get puffed out a lot… like I have to stop and take five breaths, then I get tackled” Ch02
“But, I just like give up over time…I’ll be playing and sometimes I have to sit down for a rest, sometimes because I get pretty worn out…” Ch05
“…it makes me stop, cough. It makes me stop, wait a minute, and then I have to cough and then catch my breath and then go back on learning for like 2 min and then do it and then do it again… I just stand there and watch people do stuff…because I keep on stopping a lot and losing my friends” Ch07
Children spoke about screen time across a range of devices including home computers, televisions, tablets and phones. Screen time was discussed across many questions irrespective of TDF domain and occasionally brought up without a question being asked.
“…running you have to do actual more fitness where Xbox you’re just sitting on your couch” Ch05
“…Sometimes my friend will come over, we mainly only play Terraria together because they were, Yeah, but Ah, and because they love playing on the old Xboxes, are usually on the when you have the best stuff and everything.” Ch07
“Play on my iPad. I watch TV and stuff.” Ch10
“I play my iPad until it dies.” Ch02
The TDF domain, initial codes, initial code groupings, subthemes, and final emergent themes related to children’s facilitators and barriers to physical activity are shown in Tables 5, 6, respectively. Logistic and instrumental support and supportive social and physical activity environments emerged as facilitators, while management of symptoms associated with bronchiectasis emerged as the primary barrier. Individual themes are presented with illustrative quotes from participants.
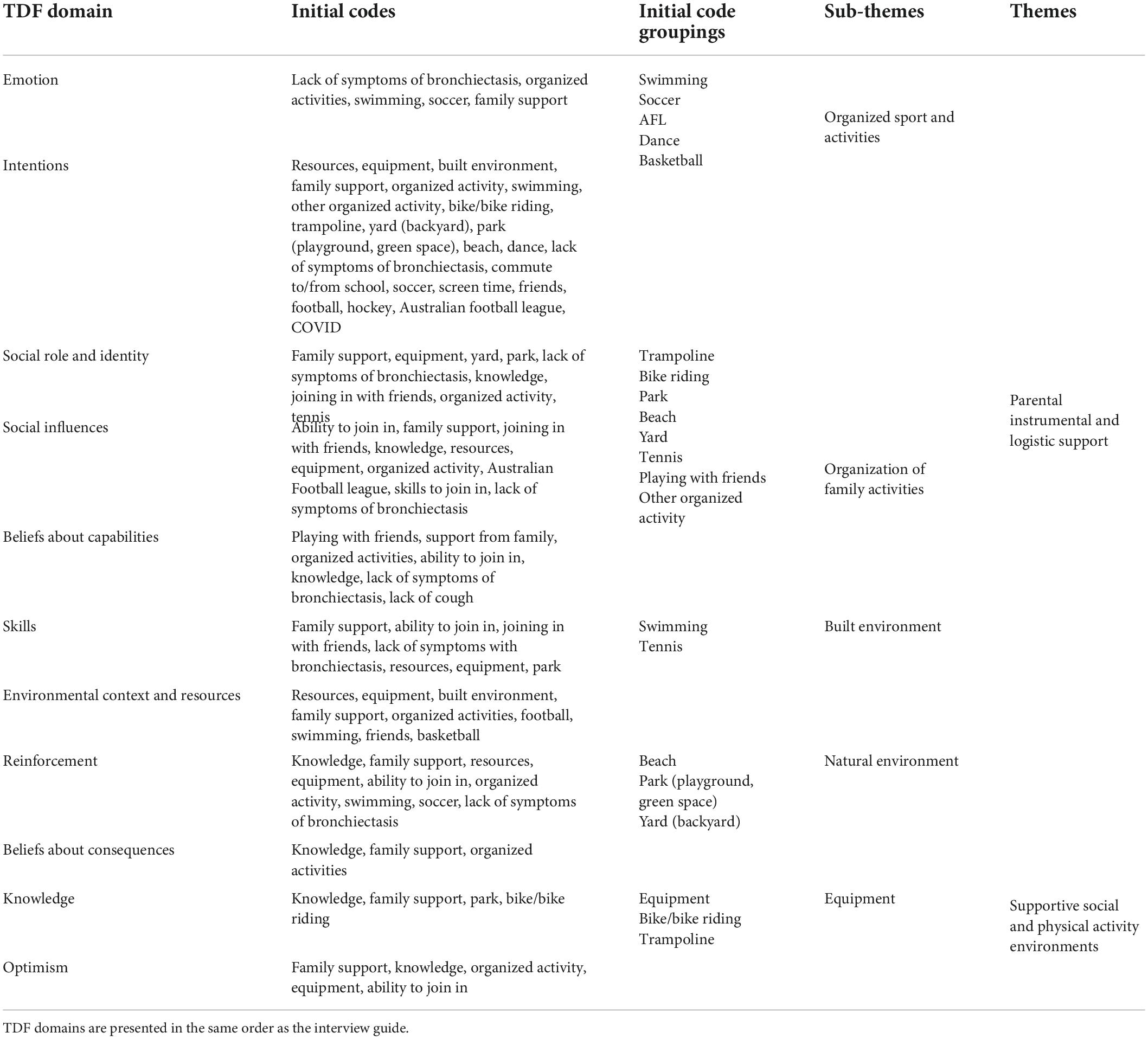
Table 5. Development of themes relating to facilitators for physical activity from the perspective of parents.
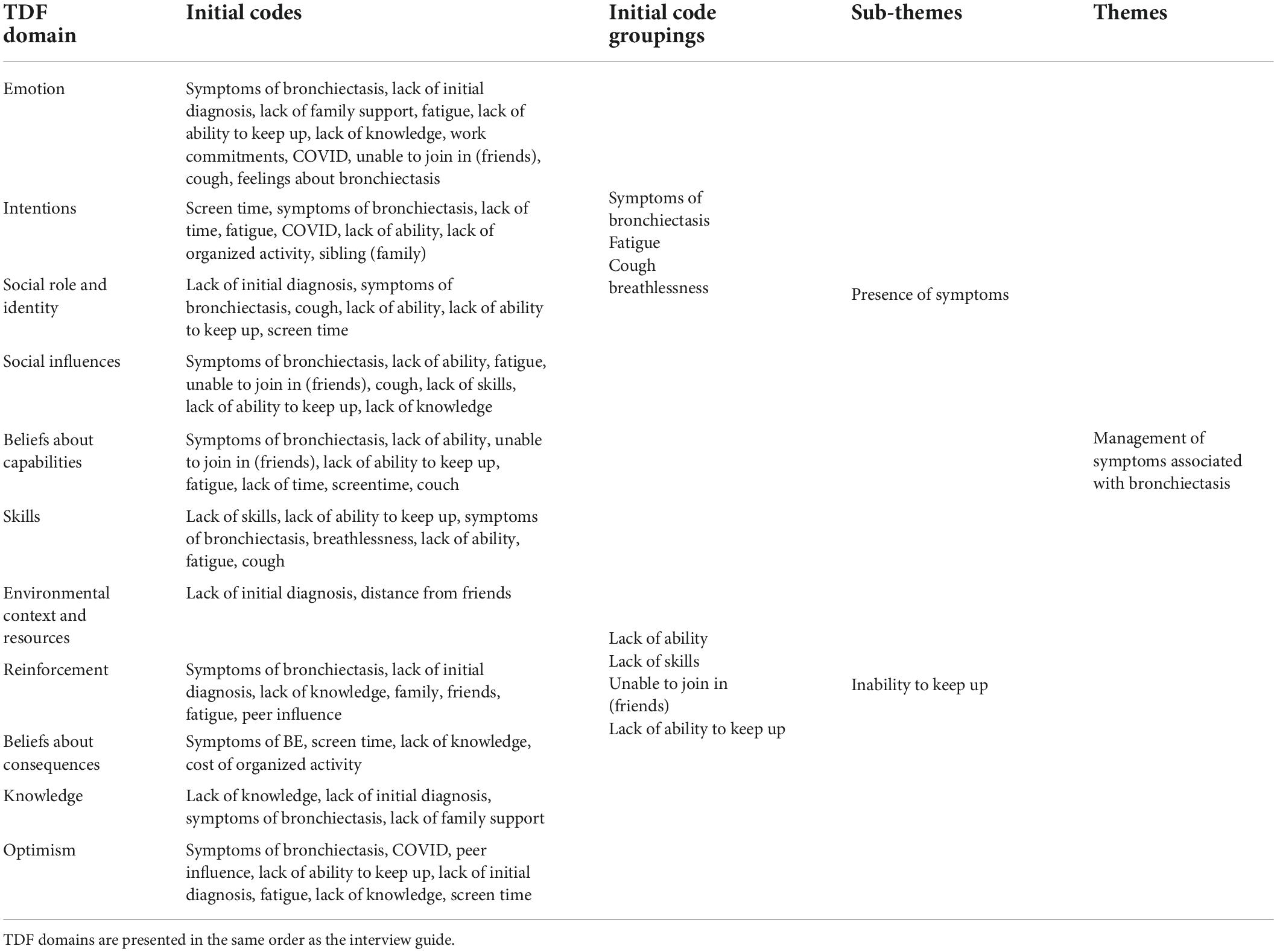
Table 6. Development of themes relating to barriers for physical activity from the perspective of parents.
Similar to the children, parents described their child’s involvement in a variety of organized sports and activities (swimming being the most popular) and gave examples of how they routinely organized family outings and activities that provided children with physical activity such as games at home like handball, trampolining and going to playgrounds, parks and beaches.
“… 3 days a week would be with soccer. He was doing swimming squad there for a while as well, so that was early mornings and the occasional afternoon as well.” Par06
“Activity-wise, we try to get out a lot. I take them to the park. He rides his scooter. He’s learning how to ride a bike.” Par02
“It hasn’t been hard to say, hey, let’s go down for a bike ride. Let’s go to the skate park and he’s happy to spend 2 or 3 h there easily…we play tennis, as a family. We don’t play competition tennis or anything like that. No, I mean tennis wise we will go down and spend, you know, half our time just hitting with him and throwing balls… but now he plays quite well with us” Par01
Parents identified having the right equipment and supportive physical activity environments as facilitators to their child’s physical activity. Parents spoke about the equipment and resources available either at home or locally that supported physical activity. Trampolines, bikes, and basic sporting equipment likes balls and racquets were commonly reported to be available at home. Parents not only spoke about access to parks and nature areas in their community but also the size of their backyards and the presence of footpaths to promote walking.
“…in the summer he’s in the pool and in the winter, he’s, I’ve just bought him another trampoline… The trampoline has been amazing, because especially when he is sick, he goes out there and it helps him cough and get rid of bit of the rubbish.” Par05
“There’s a little park up the road we might go to that, he’ll go bike riding out on the street with these friends or things we might go find a new park. He loves to climb. So, generally we stick to like the climbing tree park or anything that’s got something on it for him to climb.” Par07
“…we don’t have a huge backyard but we’ve got enough…and we’ve got the park down the road to play football…yeah, he climbs trees when he plays with the kid next door.” Par02
Parents discussed the presence of bronchiectasis symptoms such as coughing, volume of mucus, shortness of breath, and fatigue as barriers to their child’s participation in physical activity.
“He’s slow with his running, because of the coughing. At the time, we didn’t know, it was–we just knew that it was mucus, and it was making it difficult for him to–because he would always stop and cough up all the phlegm.” Par02
“He gets worn out probably quicker. He doesn’t seem to have as much dexterity or strength as they do… He tends to fatigue really quickly compared to them. That’s probably the most pronounced difference” Par09
“…when he does get that little cough and he starts to get the gunk he knows or my chest is hurting, that’s generally a sign that we’ve got to take it easy, take a step back… He’s quite wiped out by the time we do finish school. So, at the moment, he just sort of comes home, he has a snack.… but sometimes he’ll get out and he’ll ride a bike or play with his friends outside but during, as the week progresses, he gets quite tired pretty quickly.” Par07
This study is the first to investigate the facilitators and barriers to participation in physical activity in children with bronchiectasis. Children and their parents presented unique perspectives and distinct themes relating to barriers and facilitators to participation in physical activity. Facilitators to physical activity from the perspectives of children included family co-participation in physical activity, having fun with friends and participating in a variety of organized sport and activities. Children identified an inability to keep up with their peers and screen time as barriers to physical activity. Supportive social and physical activity environments and parental logistic and instrumental support were facilitators to physical activity according to patents and the management of symptoms associated with bronchiectasis a key barrier.
Having fun with friends was identified by the children as a key facilitator to physical activity and was discussed throughout the interviews across multiple TDF domains. Similar sentiments of “enjoyment,” “fun,” “peers,” and “friends” were expressed in qualitative studies of children with CF (32, 33). In a recent study of children with CF, it was reported that friends and friendship groups could positively influence physical activity (34). A multi-disciplinary team of health practitioners, including respiratory physicians, nurses, physiotherapists, and exercise physiologists, are involved in the management of bronchiectasis and well positioned to advocate strategies to increase physical activity. Our findings suggest that health professionals can support children with bronchiectasis by assisting families to identify physical activity options that include peers and are, by nature, enjoyable. Whenever possible, therapeutic exercise programs for children with bronchiectasis could involve peers or siblings and include active games that are developmentally appropriate and fun.
Participation in organized sport and activities was also identified as a facilitator to physical activity. Children discussed their participation in organized activities and sports throughout the interviews and in response to multiple questions from different TDF domains. There is consistent evidence from qualitative studies involving children with chronic health conditions that supports the role of organized sport and other recreational activities in promoting regular physical activity (35, 36). Just as pharmacological agents and airway clearance techniques are prescribed for children with bronchiectasis; organized sport and active recreational activities can be recommended as a strategy to promote physical activity. When appropriate, health professionals should encourage children to try new organized sports and activities if previous experiences have not been as successful or engaging as hoped.
Parent support and co-participation was another key facilitator of children’s physical activity. Children explicitly spoke about playing active games, sport, and other activities with parents and caregivers. This finding in consistent with the results of previous studies investigating parental influences on physical activity in children with CF, asthma, and other chronic health conditions (27, 35). A parent’s belief that physical activity will positively impact symptoms, along with their motivation and due diligence in planning physical activity experiences for their children were examples of parental supports described in a study of children with asthma, CF and type I diabetes (35). In a systematic review that included 35 children with CF, Denford et al. (27) found parental support in the form of planning, structuring and providing physical activity opportunities for their children to be important influences on children’s participation in physical activity. Collectively, these findings highlight the need for parents and caregivers to be educated about the benefits of participating in physical activity with their child and the importance of providing the logistic and instrumental support required for ongoing participation in physical activity, sport, and physically active recreational pursuits.
The inability to keep up with peers was identified as the predominant barrier to participation in physical activity, with the presence of bronchiectasis symptoms and lack of motor skill proficiency key contributors. Children spoke about their breathlessness, coughing and feeling fatigued when participating in physical activity with their peers. These observations are consistent with results of studies involving children with CF. In those studies, it was common for children with CF to acknowledge that their symptoms, such as tiredness or breathlessness could limit participation in physical activity (32, 34). In addition to poor exercise tolerance, children repeatedly spoke about their lack of skills or their inability to play games and sports with their peers. This finding is consistent with the results of a recent study examining the relationship between fundamental movement skill proficiency and physical activity in children with bronchiectasis (37). In that study, fewer than 5% of children demonstrated mastery of locomotor skills such as run, gallop, hop, and leap; while fewer than 10% demonstrated mastery of object control skills such as two-handed strike, overarm throw, and underarm throw. Only 17.4% of children with bronchiectasis achieved their age equivalency for locomotor skills and just 8.7% achieved their age equivalency for object control skills (37). Importantly, children achieving their age equivalency for fundamental movement skills exhibited significantly higher levels of MVPA than children not achieving their age equivalency (51.7 vs. 36.7 min/day). Collectively these findings highlight the need for exercise programs to address poor exercise tolerance and fundamental movement skill proficiency for this patient group.
Screen-based digital technology such as smartphones, iPads, video games, computers and television were discussed by children as a barrier to physical activity. Children found it easier to spend time on screens than participating in physical activity. The negative impact of excessive screentime on child health is well documented (38–40). Whilst it is unknown if children with chronic respiratory conditions such as CF, asthma and bronchiectasis spend more time on screens than their healthy peers, it has been identified that only a small percentage of children with bronchiectasis are sufficiently active for health benefit (21). Health professionals can promote autonomy supportive parenting strategies that manage or limit screen time. For example, a family media plan encourages families to reflect on family values, consider the purpose of screen time, and create appropriate goals and rules (41, 42). Parents offered informed perspectives in relation to the barriers and facilitators to physical activity. Parental logistic and instrumental support for physical activity emerged as a key facilitator. This theme was consistent with children’s perspectives on parental support and co-participation as a facilitator of physical activity. Parents talked about signing up, paying fees, providing transport before and after school, and organizing family activities that promoted physical activity. Similar findings regarding the role of parental support for physical activity have been reported for children with CF (35, 43). Parents of children with cerebral palsy similarly identified the importance of logistic and instrumental support for physical activity in terms of advocacy, motivation and communication with trainers and coaches (44). These findings suggest that health professionals should encourage parents and caregivers of children with bronchiectasis to set goals for their child’s participation in physical activity.
Parents identified a supportive built environment and support from extended family and friends and as key facilitators. Parents discussed the value of having basic sporting equipment such as balls and racquets at home, along with bikes, trampolines, large backyards, and in some cases, swimming pools. In a unique perspective, parents also identified walkable neighborhoods and easy access to local parks and nature areas as important positive influences on their child’s physical activity behavior. The influence of the built environment on physical activity among children with chronic respiratory conditions has received little research attention. Happ et al. (43) reported that having access to a bicycle as part of a home-based exercise program was a facilitator to physical activity among children with CF. In this study social environments included parents, extended family, siblings, friends, and neighbors. Extended family members such as grandparents provide logistic support to enable physical activity in addition to motivation and encouragement. Friends and siblings support physical activity via active play at home and in local parks, playgrounds and sporting fields. Health professionals can provide information about local parks and facilities in addition to programs or activities that support physical activity.
For parents, the management of symptoms associated with bronchiectasis was the key barrier to physical activity. They described how symptoms such as coughing, breathlessness, vomiting and fatigue negatively prevented their child from participating in physical activity. Identical findings have been reported for parents of children with asthma and CF (27, 32, 35). Children with bronchiectasis may have ongoing symptoms that impact their daily lives including schooling, play, physical activity, and general wellbeing (6). While physical activity may be limited during periods of exacerbation when children are unwell, exercise may in fact play an important role in managing symptoms and preventing future declines in lung function. In a study of adults with bronchiectasis, an 8-week therapeutic exercise program significantly reduced the number of exacerbations over a 12-month period (45). Further evidence focusing on the potential benefits of physical activity and the health impacts of therapeutic exercise programs is needed for children with bronchiectasis.
This study is unique in the pediatric bronchiectasis literature, includes children and parents as participants and includes only those with current diagnoses. Participants were recruited from two specialist pediatric pulmonology clinics in south-east Queensland, Australia, and may not reflect other demographics. It would be appropriate for future studies to include participants from diverse geographical areas and clinical settings to establish if the findings are consistent. The perspectives of health professionals where not gathered for this study. Future studies could include health professionals as participants to gather their perspectives on barriers and facilitators to physical activity in children with bronchiectasis.
In summary, the current study provided insights into the factors that influence physical activity behavior in children with bronchiectasis. Having fun with friends, participating in organized sport and activities, and family co-participation in physical activity were facilitators from the perspectives of children. Inability to keep up with their peers and time on technology emerged as barriers. From the perspectives of parents, instrumental and logistic support for physical activity and supportive social and physical activity environments emerged as facilitators, while management of symptoms associated with bronchiectasis emerged as a barrier. Programs to increase physical activity in children with bronchiectasis should therefore be fun, accessible, and provide opportunities for social interaction. Therapists involved in the delivery of physical activity programs should consider poor exercise tolerance, low perceived competence, developmental delays in motor skill proficiency, and the management of symptoms. Presently, there are limited community options which provide these opportunities. The findings of this study should inform the design and implementation of therapeutic exercise programs for children with bronchiectasis.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by Queensland Children’s Hospital. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
ST oversaw the conduct of the study. AC, VG, and TJ supported the recruitment. TJ interviewed the participants, reviewed the transcripts and coded, and drafted the manuscript. ST, EB, K-AO’G, and TJ analyzed the data. ST, EB, K-AO’G, AC, and VG reviewed the manuscript. All authors had a role in informing the conceptual framework used in coding and analysis of the data collected, read, and approved the final manuscript.
This work was supported by National Health and Medical Research Council Grant (APP11606123).
We thank the parents and children who participated in the interviews.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Chang AB, Bush A, Grimwood K. Bronchiectasis in children: diagnosis and treatment. Lancet. (2018) 392:866–79. doi: 10.1016/S0140-6736(18)31554-X
2. Goyal V, Grimwood K, Marchant JM, Masters IB, Chang AB. Paediatric chronic suppurative lung disease: clinical characteristics and outcomes. Eur J Pediatr. (2016) 175:1077–84. doi: 10.1007/s00431-016-2743-5
3. Quint JK, Smith MP. Paediatric and adult bronchiectasis: diagnosis, disease burden and prognosis. Respirology. (2019) 24:413–22. doi: 10.1111/resp.13495
4. Wurzel DF, Chang AB. An update on pediatric bronchiectasis. Expert Rev Respir Med. (2017) 11:517–32. doi: 10.1080/17476348.2017.1335197
5. Bush A, Floto RA. Pathophysiology, causes and genetics of paediatric and adult bronchiectasis. Respirology. (2019) 24:1053–62. doi: 10.1111/resp.13509
6. Kapur N, Masters IB, Newcombe P, Chang AB. The burden of disease in pediatric non-cystic fibrosis bronchiectasis. Chest. (2012) 141:1018–24. doi: 10.1378/chest.11-0679
7. Lovie-Toon YG, Grimwood K, Byrnes CA, Goyal V, Busch G, Masters IB, et al. Health-resource use and quality of life in children with bronchiectasis: a multi-center pilot cohort study. BMC Health Serv Res. (2019) 19:561. doi: 10.1186/s12913-019-4414-5
8. Bahali K, Gedik AH, Bilgic A, Cakir E, Ustabas Kahraman F, Keskin Osmanoglu N, et al. The relationship between psychological symptoms, lung function and quality of life in children and adolescents with non-cystic fibrosis bronchiectasis. Gen Hosp Psychiatr. (2014) 36:528–32. doi: 10.1016/j.genhosppsych.2014.05.019
9. Akalin F, Koroglu TF, Bakac S, Dagli E. Effects of childhood bronchiectasis on cardiac functions. Pediatr Int. (2003) 45:169–74. doi: 10.1046/j.1442-200x.2003.01692.x
10. Alzeer AH, Al-Mobeirek AF, Al-Otair HA, Elzamzamy UA, Joherjy IA, Shaffi AS. Right and left ventricular function and pulmonary artery pressure in patients with bronchiectasis. Chest. (2008) 133:468–73. doi: 10.1378/chest.07-1639
11. Olveira C, Olveira G, Gaspar I, Dorado A, Cruz I, Soriguer F, et al. Depression and anxiety symptoms in bronchiectasis: associations with health-related quality of life. Qual Life Res. (2013) 22:597–605. doi: 10.1007/s11136-012-0188-5
12. Giron Moreno RM, Fernandes Vasconcelos G, Cisneros C, Gomez-Punter RM, Segrelles Calvo G, Ancochea J. Presence of anxiety and depression in patients with bronchiectasis unrelated to cystic fibrosis. Arch Bronconeumol. (2013) 49:415–20. doi: 10.1016/j.arbres.2013.01.012
13. Chang AB, Fortescue R, Grimwood K, Alexopoulou E, Bell L, Boyd J, et al. European respiratory society guidelines for the management of children and adolescents with bronchiectasis. Eur Respir J. (2021) 58:2002990. doi: 10.1183/13993003.02990-2020
14. Strong WB, Malina RM, Blimkie CJR, Daniels SR, Dishman RK, Gutin B, et al. Evidence based physical activity for school-age youth. J Pediatr. (2005) 146:732–7. doi: 10.1016/j.jpeds.2005.01.055
15. Okely AD, Salmon J, Vella S, Cliff D, Timperio A, Tremblay M, et al. A Systematic Review to Update the Australian Physical Activity Guidelines for Children and Young People. Canberra: Commonwealth of Australia (2012).
16. Lee AL, Button BM, Tannenbaum E-L. Airway-clearance techniques in children and adolescents with chronic suppurative lung disease and bronchiectasis. Front Pediatr. (2017) 5:2. doi: 10.3389/fped.2017.00002
17. Lee AL, Burge AT, Holland AE. Airway clearance techniques for bronchiectasis. Cochrane Database Syst Rev. (2015) 2015:CD008351. doi: 10.1002/14651858.CD008351.pub3
18. Janssen I, Leblanc AG. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act. (2010) 7:40. doi: 10.1186/1479-5868-7-40
19. Chang AB, Bell SC, Torzillo PJ, King PT, Maguire GP, Byrnes CA, et al. Chronic suppurative lung disease and bronchiectasis in children and adults in Australia and New Zealand thoracic society of Australia and New Zealand guidelines. Med J Aust. (2015) 202:130. doi: 10.5694/mjac14.00287
20. Pasteur MC, Bilton D, Hill AT. British thoracic society bronchiectasis non CFGG. British thoracic society guideline for non-CF bronchiectasis. Thorax. (2010) 65(Suppl 1.):i1–58. doi: 10.1136/thx.2010.136119
21. Joschtel B, Gomersall SR, Tweedy S, Petsky H, Chang AB, Trost SG. Objectively measured physical activity and sedentary behaviour in children with bronchiectasis: a cross-sectional study. BMC Pulm Med. (2019) 19:7. doi: 10.1186/s12890-018-0772-8
22. Chang AB, Boyd J, Bell L, Goyal V, Masters IB, Powell Z, et al. Clinical and research priorities for children and young people with bronchiectasis: an international roadmap. ERJ Open Res. (2021) 7:00122–2021. doi: 10.1183/23120541.00122-2021
23. Sallis JF, Prochaska JJ, Taylor WC. A review of correlates of physical activity of children and adolescents. Med Sci Sports Exerc. (2000) 32:963–75.
24. Sterdt E, Liersch S, Walter U. Correlates of physical activity of children and adolescents: a systematic review of reviews. Health Educ J. (2013) 73:72–89. doi: 10.1177/0017896912469578
25. Van Der Horst K, Paw MJCA, Twisk JWR, Van Mechelen WA. brief review on correlates of physical activity and sedentariness in youth. Med Sci Sports Exerc. (2007) 39:1241–50.
26. Pianosi PT, Davis HS. Determinants of physical fitness in children with asthma. Pediatrics. (2004) 113:e225–9. doi: 10.1542/peds.113.3.e225
27. Denford S, van Beurden S, Halloran P, Williams CA. Barriers and facilitators to physical activity among children, adolescents, and young adults with cystic fibrosis: a systematic review and thematic synthesis of qualitative research. BMJ Open. (2020) 10:e035261. doi: 10.1136/bmjopen-2019-035261
28. Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A, et al. Making psychological theory useful for implementing evidence based practice: a consensus approach. BJM Qual Safey. (2005) 14:26–33. doi: 10.1136/qshc.2004.011155
29. Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implementation Sci. (2012) 7:37. doi: 10.1186/1748-5908-7-37
30. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. (2006) 3:77–101. doi: 10.1191/1478088706qp063oa
31. Australian Bureau of Statistics. Technical Paper: Socio-Economic Indexes for Areas (SEIFA) 2016. Canberra: Commonwealth of Australia (2018).
32. Moola FJ, Faulkner GEJ, Schneiderman JE. “No Time to Play”: perceptions toward physical activity in youth with cystic fibrosis. Adapt Phys Activ Quart. (2012) 29:44–62. doi: 10.1123/apaq.29.1.44
33. Swisher AK, Erickson M. Perceptions of physical activity in a group of adolescents with cystic fibrosis. Cardiopulm Phys Ther J. (2008) 19:107–13.
34. Shelley J, Fairclough SJ, Knowles ZR, Southern KW, McCormack P, Dawson EA, et al. A formative study exploring perceptions of physical activity and physical activity monitoring among children and young people with cystic fibrosis and health care professionals. BMC Pediatr. (2018) 18:335. doi: 10.1186/s12887-018-1301-x
35. Fereday J, MacDougall C, Spizzo M, Darbyshire P, Schiller W. “There’s nothing I can’t do – I just put my mind to anything and I can do it”: a qualitative analysis of how children with chronic disease and their parents account for and manage physical activity. BMC Pediatr. (2009) 9:1. doi: 10.1186/1471-2431-9-1
36. Winn CON, Mackintosh KA, Eddolls WTB, Stratton G, Wilson AM, Rance JY, et al. Perceptions of asthma and exercise in adolescents with and without asthma. J Asthma. (2018) 55:868–76. doi: 10.1080/02770903.2017.1369992
37. Joschtel B, Gomersall SR, Tweedy S, Petsky H, Chang AB, Trost SG. (2021). Fundamental movement skill proficiency and objectively measured physical activity in children with bronchiectasis: a cross-sectional study. BMC Pulm Med. 21:269. doi: 10.1186/s12890-021-01637-w
38. Hale L, Guan S. Screen time and sleep among school-aged children and adolescents: a systematic literature review. Sleep Med Rev. (2015) 21:50–8. doi: 10.1016/j.smrv.2014.07.007
39. Stiglic N, Viner RM. Effects of screentime on the health and well-being of children and adolescents: a systematic review of reviews. BMJ Open. (2019) 9:e023191. doi: 10.1136/bmjopen-2018-023191
40. Janssen X, Martin A, Hughes AR, Hill CM, Kotronoulas G, Hesketh KR. Associations of screen time, sedentary time and physical activity with sleep in under 5s: a systematic review and meta-analysis. Sleep Med Rev. (2020) 49:101226. doi: 10.1016/j.smrv.2019.101226
41. Reid Chassiakos Y, Radesky J, Christakis D, Moreno MA, Cross C, Council On Communications And Media. Children and adolescents and digital media. Pediatrics. (2016) 138:e20162593. doi: 10.1542/peds.2016-2593
42. Strasburger VC, Hogan MJ, Mulligan DA, Ameenuddin N, Christakis DA, Cross C, et al. Children, adolescents, and the media. Pediatrics. (2013) 132:958–61. doi: 10.1542/peds.2013-2656
43. Happ MB, Hoffman LA, DiVirgilio D, Higgins LW, Orenstein DM. Parent and child perceptions of a self-regulated, home-based exercise program for children with cystic fibrosis. Nurs Res. (2013) 62:305–14.
44. Verschuren O, Wiart L, Hermans D, Ketelaar M. Identification of facilitators and barriers to physical activity in children and adolescents with cerebral palsy. J Pediatr. (2012) 161:488–94. doi: 10.1016/j.jpeds.2012.02.042
Keywords: bronchiectasis, pediatrics–children, exercise, theoretical domains framework (TDF), qualitative analysis
Citation: Jones T, Baque E, O’Grady K-AF, Goyal V, Chang AB and Trost SG (2022) Barriers and facilitators of physical activity in children with bronchiectasis: Perspectives from children and parents. Front. Pediatr. 10:974363. doi: 10.3389/fped.2022.974363
Received: 21 June 2022; Accepted: 13 September 2022;
Published: 05 October 2022.
Edited by:
Hannah C. Moore, The University of Western Australia, AustraliaReviewed by:
Clemax Couto Sant’anna, Federal University of Rio de Janeiro, BrazilCopyright © 2022 Jones, Baque, O’Grady, Goyal, Chang and Trost. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Taryn Jones, dDQwLmpvbmVzQGhkci5xdXQuZWR1LmF1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.