- 1University of the Witwatersrand, Faculty of Health Sciences, Johannesburg, South Africa
- 2District Clinical Specialist Team, Johannesburg Health District, Johannesburg, South Africa
- 3Department of Paediatrics and Child Health, School of Clinical Medicine, Faculty of Health Sciences, University of Witwatersrand, Johannesburg, South Africa
Introduction: neonatal hypothermia has previously been noted in a large proportion of neonates born through Caesarean section at Chris Hani Baragwanath Hospital (CHBAH), yet no study in South Africa specifically explores the extent and severity of the threat of hypothermia to this population of neonates.
Objectives: to describe the proportion and severity of neonatal hypothermia in infants born via Caesarean section at CHBAH as well as to document and describe possible contributing factors to neonatal hypothermia in this population.
Methods: A neonatal unit's database records were reviewed for demographic information of patients and their mothers, clinical characteristics, body temperature and outcomes. Comparisons between normothermic and hypothermic neonates were performed.
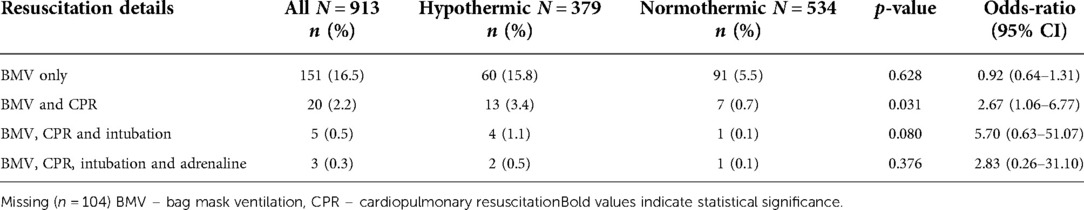
Results: Forty-one percent of neonates born via Caesarean section had hypothermia at birth, of whom 71%, 27% and 2% had mild, moderate and severe hypothermia, respectively. Prevalence of admission hypothermia was 42%. On average, neonates were born at term and were of normal birth weight. No maternal factors were found to be statistically significant. Bag-mask ventilation (BMV) and cardiopulmonary resuscitation (CPR) [3.4% vs. 0.7%, p-0.033; OR 2.67 (95% CI: 1.06–6.77)] and an elevated lactate [13.25 vs. 3.2 mmol/l, p-0.032; OR 1.13 (95% CI: 1.01–1.26)] were associated with hypothermia. In the multivariable logistic regression analysis hypothermia in neonates was associated with an elevated lactate.
Conclusions: Prevalence of hypothermia in neonates born by Caesarean section is high and further prospective studies are required to elucidate the factors contributing to this.
Introduction
The third sustainable development goal proposed by the World Health Organization speaks directly to improving healthcare. Surrogate measures for the healthcare of a country are the maternal and childhood mortality rates. Neonatal mortality in South Africa can be attributed to five main causes: prematurity, intrapartum events, infections, congenital abnormalities and miscellaneous causes (1). Hypothermia in neonates is known to contribute to neonatal mortality due to neonatal infections, prematurity and asphyxia (2).
Neonatal hypothermia was noted in a large proportion of neonates born through Caesarean section in data collected during a baseline audit for a Quality Improvement by the EMS services, yet no study in South Africa specifically explores the extent and severity of the threat of hypothermia to this population of neonates. A retrospective review at Chris Hani Baragwanath Academic Hospital (CHBAH) showed that hypothermia in neonates had a significant association with neonates born at 1 000 g (OR = 1.79), those requiring resuscitation (OR = 2.32) and, in contrast to other studies, were more likely to be born vaginally (OR = 1.48). This was proposed to be due to poor temperature control in delivery rooms as opposed to operating theatres and due to the fact that neonates born of Caesarean section were more likely to be attended to by a doctor, resulting in better control of temperature. The study also reports a higher mortality rate in hypothermic infants within a week of delivery (3). The severity of hypothermia in this study was not specified. This study thus aims to describe the proportion and severity of neonatal hypothermia in infants born via Caesarean section at CHBAH. The study also aims to document and describe possible contributing factors to neonatal hypothermia in the study population.
Methodology
A retrospective descriptive study was undertaken at Chris Hani Baragwanath Academic Hospital (CHBAH) Neonatology Unit for the period 1 January 2018 to 31 December 2018. The CHBAH neonatology unit comprises of an 18 bed neonatal intensive care unit (NICU), a 48 bed high care area, a 100 bed standard care nursery (SCN), a 19 bed Kangaroo Mother Care (KMC) ward. Approval for the retrospective review of the CHBAH Neonatology Unit's database was granted by the Human Research Ethics Committee [HREC] (Medical) in July 2020. Ethics amendment was applied for and granted in March 2021.
The study population included all neonates born via Caesarean section at CHBAH and excluded patients born outside of CHBAH – for example transferred into the hospital or born before arrival (BBA) and those patients without any body temperature data available.
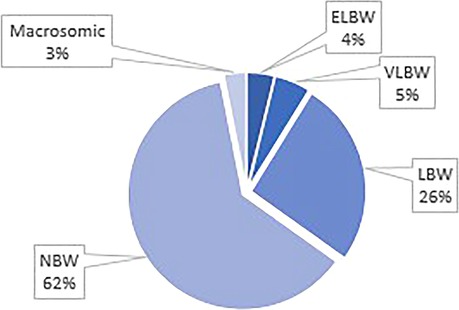
The data collected was secondary in nature, as it was collected from the Research Electronic Data Capture (REDCap) database of the CHBAH Neonatology Unit. The variables collected included: season of birth, birth weight, gestational age, body temperature, 1-minute APGAR score, neonatal biochemical parameters, indication for Caesarean section, resuscitation outcomes, neonatal illnesses as well as a number of maternal factors (age, parity, gravidity, race, HIV status, antenatal care received, antibiotics received, antenatal steroids administered and complications). Hypothermia was defined as an axillary temperature below 36.5 °C as per the World Health Organization (WHO) (4). This was further stratified into mild (36 °C–36.4 °C), moderate (32 °C–35.9 °C) and severe hypothermia (<32 °C). An axillary temperature within 30 min of birth was regarded as the birth temperature. The 4 seasons were defined as spring from 1 September to 30 November, summer from 1 December to 28 February, autumn from 1 March to 31 May and winter from 1 June to 31 August. A normal birthweight (NBW) was defined as a weight between 2.5 and 4.0 kilograms (kg), macrosomia as > 4.0 kg, low birthweight (LBW) as < 2.5 kg, very low birthweight (VLBW) < 1.5 kg and extremely low birthweight (ELBW) as < 1 kg.
Anonymised data was analyzed with aid of the statistical package Stata (version 16). Chi-square tests were used to determine statistical significance of categorical variables. Continuous variables were analyzed as normally or non-normally distributed using histogram functions. Statistical significance of continuous variables was determined by t-tests and Mann-Whitney U tests (Wilcoxon Rank Sum test) for normally and non-normally distributed variables respectively. Logistic regression models were used to determine odds ratios. For the multivariable regression model variables with a p-values <0.1 were included and those variables with few observations were excluded. The meconium aspiration variable was omitted from the linear regression due to no observations in the non-hypothermia group.
Results
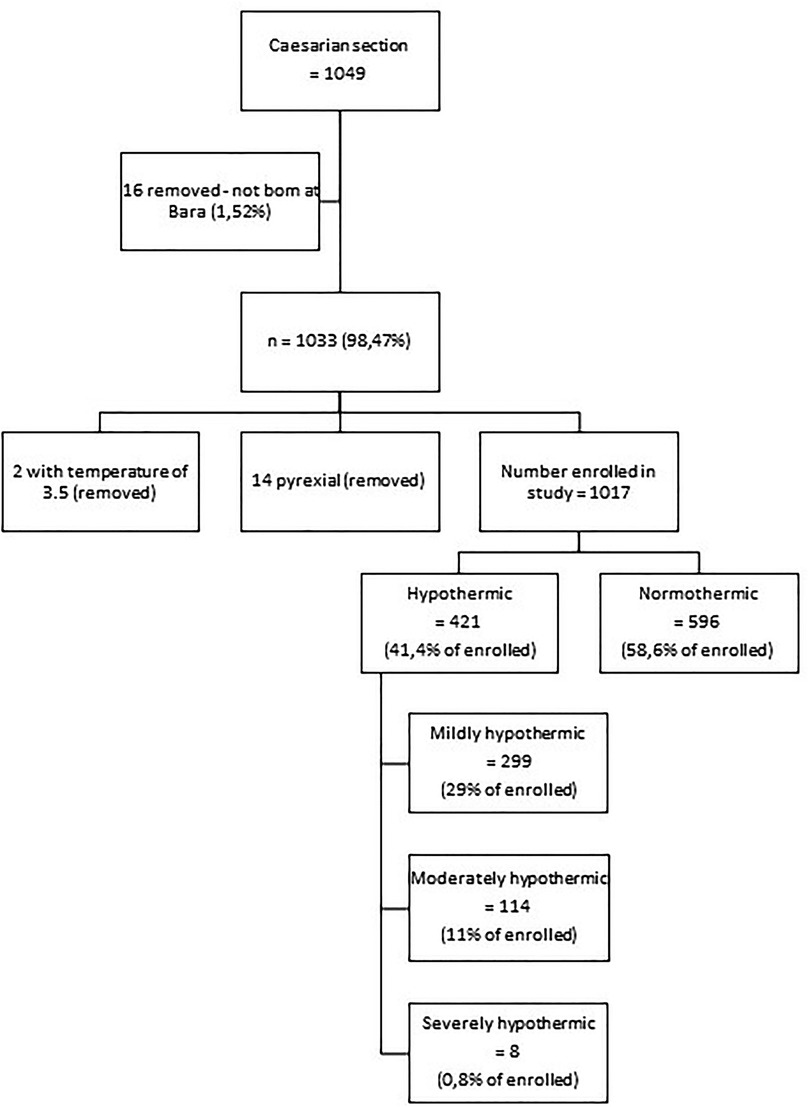
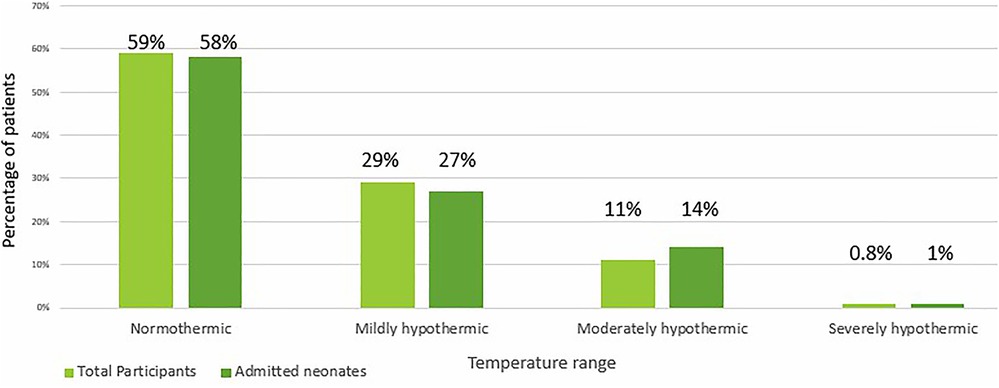
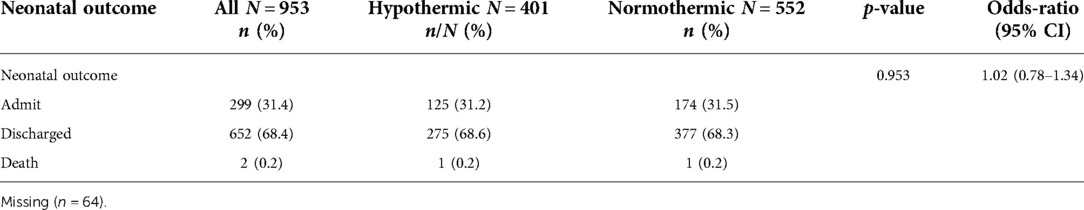
Of the 1,049 neonates born by Caesarean section at CHBAH during the study period, 1,017 (96.95%) were enrolled into the study (Figure 1). Forty-one percent (n = 421) had hypothermia at birth, of whom 71% (n = 299), 27% (n = 114) and 2% (n = 8) had mild, moderate and severe hypothermia, respectively (Figure 1). Additionally, of the 299 infants admitted to the neonatal wards at CHBAH, 42% (n = 125) were hypothermic (Figure 2). There were no significant differences when divided into mild, moderate and severe hypothermic groups. (Figure 2). The admitted infants were a subset of the study participants.
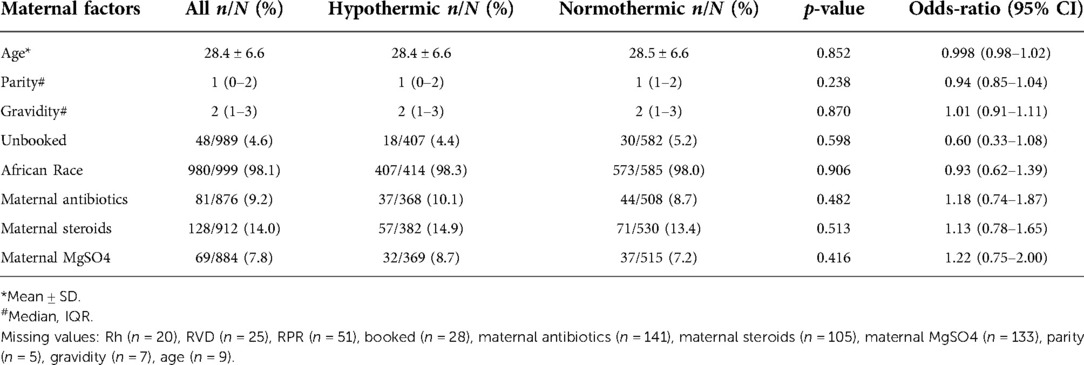
Maternal characteristics
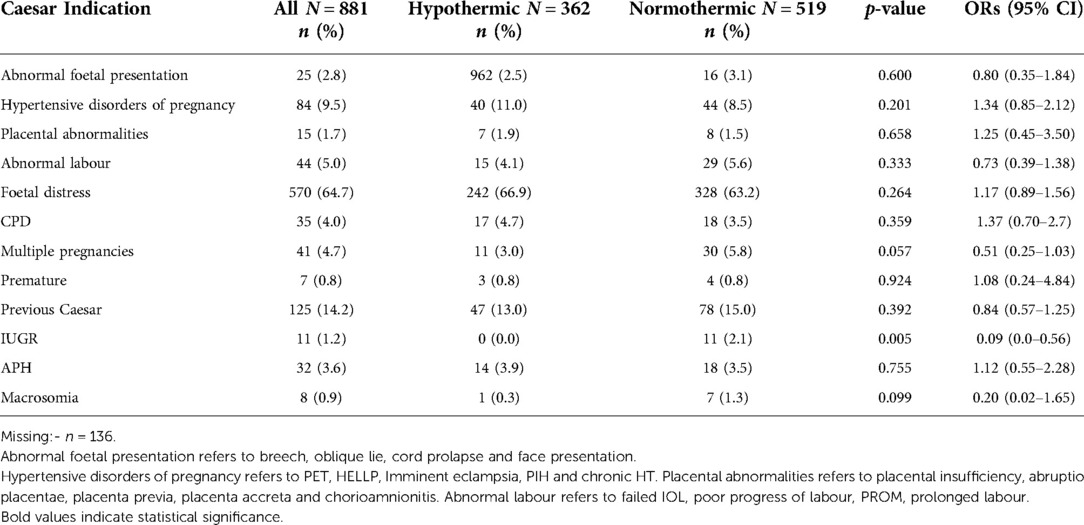
Most mothers in our study were African, with no Caucasians. They had a mean age of 28.4±6.6 years and were having their second child (mean 2±2). 25.3% were HIV positive and only 4.6% did not receive antenatal care. Receiving antibiotics, steroids or magnesium sulphate was not found to be associated with neonatal hypothermia (Table 1). The commonest indication for Caesarean section was foetal distress (64.7%). Neonates requiring Caesarean section for intrauterine growth restriction (IUGR) were less likely to be hypothermic [0% vs. 2.1%, OR 0.09 (95% CI: 0.00–0.56)] (Table 2).
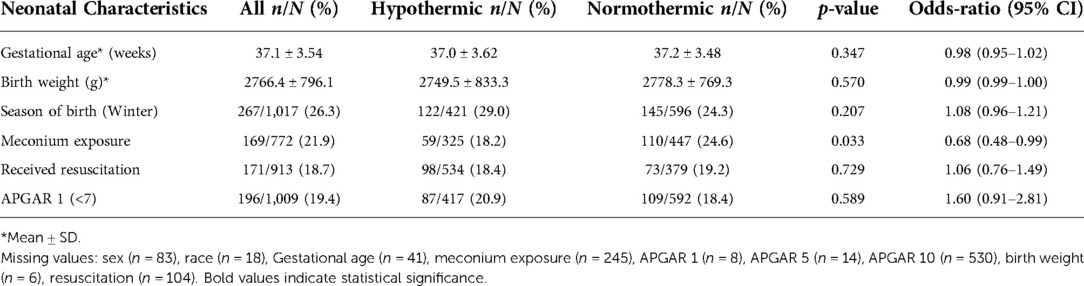
Neonatal characteristics
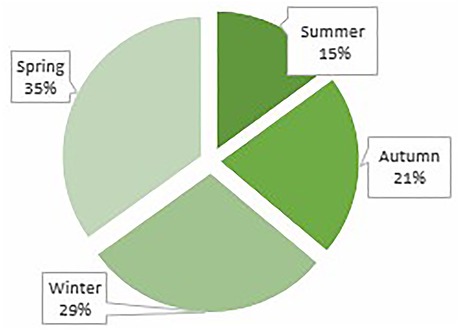
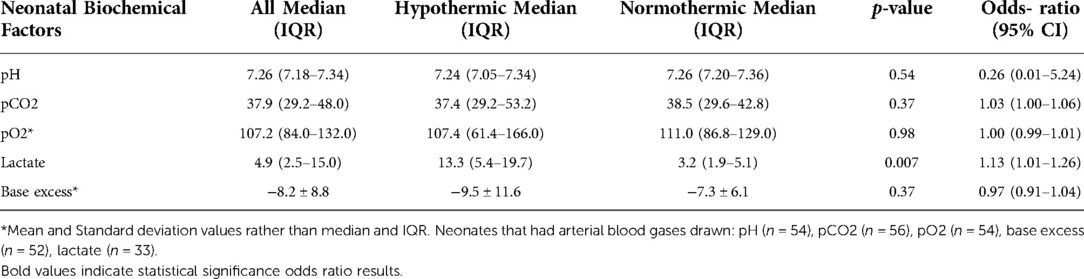
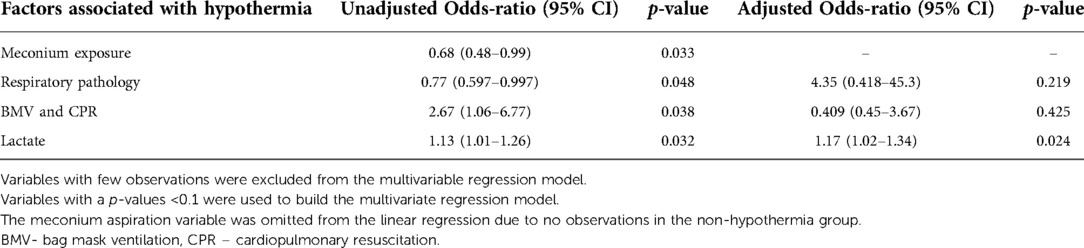
Twenty-five percent of the study population (n = 251) were HIV exposed, 14% (n = 128) received antenatal steroids, 54% (n = 508) were male, 33% (n = 323) were premature and 21.9% (n = 169) were exposed to meconium. The mean gestational age and birth weight were 37.1 (±3.54) weeks, 2766.4 (±796.1) grams respectively. In 19.4% (n = 196) of neonates, the 1 min Apgar score was <7. Neonates who were exposed to meconium were less likely to be hypothermic [18.2% vs. 24.6%, OR 0.68 (95% CI: 0.48–0.99)] (Table 3). Hypothermic neonates were mostly born in spring followed by winter (Figure 3) and most were of normal birth weight (Figure 4). In addition, there were a larger number of deliveries in spring (5030) followed by winter (4799). Approximately 18.7% (n = 171) of all the neonates required resuscitation at birth (Table 4). Neonates who received both bag mask ventilation (BMV) and cardiopulmonary resuscitation (CPR) were more likely to be hypothermic than those who did not [3.4% vs. 0.7%, OR 2.67 (95% CI: 1.06–6.77)] (Table 4). However, other respiratory interventions such as nasal cannula, nasal continuous positive airway pressure (nCPAP), receiving surfactant or assisted ventilation were not significantly associated with the temperature of neonates. Being hypothermic increased the likelihood of having an elevated lactate [median lactate of 13.25 vs. 3.2 mmol/l, OR 1.13 (95% CI: 1.01–1.26)] (Table 5). Only a small proportion of neonates had an arterial blood gas (ABG) drawn as ABGs are only done in sick neonates.
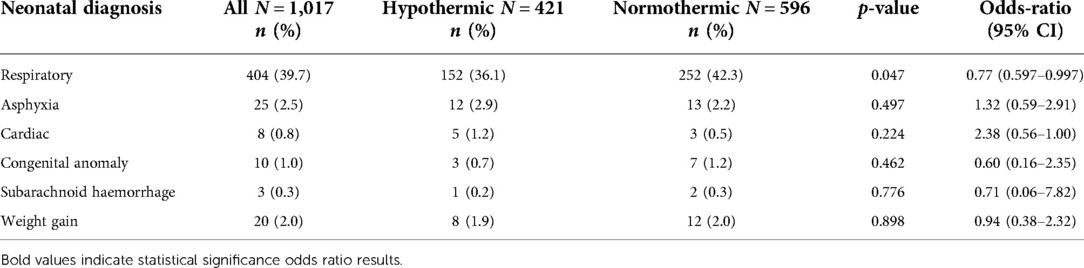
Morbidity and mortality outcomes
Overall, 39.7% (n = 404) of the neonates were found to have a respiratory pathology, 2.5% (n = 25) were asphyxiated, 0.8% (n = 8) had a cardiac pathology, 1.0% (n = 10) had a congenital anomaly, 0.3% (n = 3) had subarachnoid haemorrhages and 2.0% (n = 20) were admitted for weight gain (Table 6). Neonates with hypothermia were less likely to have respiratory pathology (36.1% vs. 42.3%; p-0.047). Table 6. Thirty-one percent of (n = 299) neonates required admission, whereas 68% (n = 652) were discharged (Table 7). Only 0.2% (n = 2) neonates demised, 1 of which was hypothermic. It is believed that both deaths were stillbirths as their APGAR scores at 1 min were both 0.
Factors associated with hypothermia
Having had CPR, respiratory pathology, and an elevated lactate were associated with hypothermia. In the multivariate logistic regression model, neonates who were hypothermic were more likely to have an elevated lactate. (Table 8). Maternal factors were not found to significantly contribute to neonatal hypothermia.
Discussion
Most of the hypothermic patients in our cohort had mild hypothermia. Incidence of hypothermia in our study population and those neonates admitted were generally comparable. Neonates who were moderately and severely hypothermic had higher admission rates though this was not significant.
Only a small number of neonates required an arterial blood gas, with neonates who were hypothermic being more likely to have an elevated serum lactate. Elevated serum lactate results from anaerobic respiration, when oxygen demand is higher than the oxygen supply that the body is receiving. Therefore, low body temperature may reflect thermoregulatory failure due to insufficient energy secondary to a lack of oxygen or metabolite (5). Of the 13 neonates with elevated lactate and hypothermia, 11 had an APGAR score at 1 min less than 7 (84.6%). Hence, they received resuscitation and therefore had an element of encephalopathy; however, only 2 met the definition for intrapartum asphyxia; as the other neonates improved their APGAR scores at 5 min after resuscitation. Lactate takes longer than pH to normalize (6). Our study design did not allow for ascribing causation between hypothermia and higher lactate levels but the association is interesting to note.
Neonates who were hypothermic were more likely to have an elevated lactate. Hypothermia may be associated with hypoxia, poor perfusion and metabolic acidosis (2). This causes a build up of lactate in hypothermic neonates. In the current study hypothermic neonates were not hypoxic but had a metabolic acidosis which was not significant. Other causes of a high lactate would need to be investigated.
BMV together with CPR as a means of resuscitation at birth was also associated with hypothermia (p = 0.031). A possible explanation for this could be that during emergency resuscitations, neonates were exposed for adequate chest compressions to be delivered. This finding is similar to a study done in Bangladesh (OR = 2.43) (7) and a study done in Iran (OR = 1.91) (8).
Patients with respiratory pathology are closely monitored, as they often go on to require ventilation and admission to ICU. For this reason, it is believed that they were found to be less hypothermic in this study as they were likely kept warmer as a general measure. A study in Denmark found that neonates with hypothermia had an increase odds of having respiratory distress syndrome and bronchopulmonary dysplasia, however when these results were adjusted for confounders the findings were not significant (9). Complications of respiratory distress syndrome, need for respiratory support and an increase in admission to the NICU or standard care nursery are seen with a higher prevalence in neonates who are hypothermic (10, 11).
Studies have shown that neonates who are small for gestational age or low birthweight are more prone to hypothermia. Reasons cited for this are large head to body surface area and decreased insulation due to decreased body fat (10). Surprisingly neonates with IUGR were less likely to be hypothermic in this study although the group sizes for this comparison were very small. Merazzi et al. reported similar findings; where low birth weight neonates (< 2500 g) was not significantly associated with hypothermia and suggest that birth weight has a smaller effect on body temperature in healthy term and late preterm neonates (11). Heat loss in neonates occurs via 4 mechanisms which includes evaporation. Transepidermal water loss (TEWL) is inversely proportional to the gestational age with low TEWL in term neonates. Preterm neonates who are SGA have lower TEWL than preterm neonates who are appropriate for gestational age (12). Neonates with IUGR have a more developed dermis and epidermis and may be more equipped to maintain homeostasis as the skin barrier may be fully developed. We hypothesize that IUGR neonates have more mature skin and less subcutaneous fat and are thus less likely to lose heat via TEWL. The number of IUGR neonates are quite small in this study, thus it is difficult to make meaningful conclusions. Further studies are required to elucidate this hypothesis.
This study also evaluated the common factors known to be associated with neonatal hypothermia such as low birth weight, prematurity and season in which the neonate was born. In this study most neonates had a normal birth weight and were not premature. This could be due to the sample population selected as a high proportion of neonates who were born via Caesarean section were term neonates. Neonates in this study were mostly born in spring followed by winter. This could be explained by a seasonal variation in the number of deliveries with a higher proportion of neonates born in spring and winter, thus giving a relatively higher proportion of neonates being hypothermic. In addition, spring temperatures in Johannesburg can be as low as 8 to 12 °C (13).
The limitations of the study include the retrospective study design and missing variables. Thus, the study was not powered to fully elucidate the associated factors of hypothermia. The time at which temperatures was taken were not documented. Given that sicker neonates were more likely to have an ABG drawn, this lends itself to a selection bias in terms of the biochemical parameters documented.
Conclusion
Hypothermia is a significant contributor to morbidity and mortality in many settings and mild hypothermia is often prevalent in the setting of Caesarean delivery. Receiving CPR and having an elevated lactate was associated with hypothermia in this cohort. During resuscitation more concerted efforts should be put in to place to prevent hypothermia. There is a need for future studies investigating hypothermia in neonates born via Caesarean section including a non-Caesarean section control group.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Human Research Ethics Committee [HREC] (Medical) of the University of the Witwatersrand. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
All authors have contributed equally to this work. All authors contributed to the article and approved the submitted version.
Funding
This was a self-funded undertaking; no sponsorships were garnered for this research.
Acknowledgments
We would like to thank our supervisors, Dr. Nakwa, Dr. Mphahlele, Dr. Mokhachane and Dr. Jordaan for their unwavering patience with our lack of experience. Gratitude is extended to Dr. Matsena-Zingoni of the Wits Biostatistics team, who taught us how to use Stata. Thanks are due to Professor Thandrayen – for her assistance in streamlining our results and explaining to us how to better present them. This undertaking would not have been possible without the support of the collaborators in this article, thank you for all your contributions. We dedicate this research report to our parents: Hakima Allana and Suleman Cassim Patel; Mosidi Ramagaga; Gabrielle and Ferdinand Kruger; Ashley Vos; Ruwaida Manjoo; Abdul Kader Mansoor; Terry and Carla Rendel; Imran and Shiraza Zaheed; Silas and Josephinah Mohlala and spouses including Aviva Rosen and Rory Bennett as well as the neonates at Chris Hani Baragwanath Hospital.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Rhoda NR, Velaphi S, Gebhardt GS, Kauchali S, Barron P. Reducing neonatal deaths in South Africa: progress and challenges. S Afr Med J. (2018) 108(3):9–16. doi: 10.7196/samj.2017.v108i3b.12804
2. Lunze K, Bloom D, Jamison D, Hamer D. The global burden of neonatal hypothermia: systematic review of a major challenge for newborn survival. BMC Med. (2013) 11(1):1–11. doi: 10.1186/1741-7015-11-24
3. Ng’eny J, Velaphi S. Hypothermia among neonates admitted to the neonatal unit at a tertiary hospital in South Africa. J Perinatol. (2019) 40(3):433–8. doi: 10.1038/s41372-019-0539-y
4. World Health Organization. Maternal and Newborn Health/Safe Motherhood. (1997). Thermal protection of the newborn: a practical guide. World Health Organization. https://apps.who.int/iris/handle/10665/63986.1997
5. Seekamp A, van Griensven M, Hildebrandt F, Wahlers T, Tscherne H. Adenosine-Triphosphate in trauma-related and elective hypothermia. The journal of trauma: injury. Infection, and Critical Care. (1999) 47(4):673. doi: 10.1097/00005373-199910000-00011
6. Shah S, Tracy M, Smyth J. Postnatal lactate as an early predictor of short-term outcome after intrapartum asphyxia. J Perinatol. (2003) 24(1):16–20. doi: 10.1038/sj.jp.7211023
7. Akter S, Parvin R, Yasmeen B. Admission hypothermia among neonates presented to neonatal intensive care unit. J Nepal Paediatr Soc. (2013) 33(3):166–71. doi: 10.3126/jnps.v33i3.8312
8. Zayeri F, Kazemnejad A, Ganjali M, Babaei G, Nayeri F. Incidence and risk factors of neonatal hypothermia at referral hospitals in Tehran, Islamic Republic of Iran. East Mediterr Health J. (2007) 13(6):1308–18. doi: 10.26719/2007.13.6.1308
9. Jensen C, Ebbesen F, Petersen J, Sellmer A, Bach C, Henriksen T. Hypothermia at neonatal intensive care unit admission was not associated with respiratory disease or death in very preterm infants. Acta Paediatr. (2017) 106(12):1934–9. doi: 10.1111/apa.13998
10. Nguyen L, Mitsakakis N, Sucha E, Lemyre B, Lawrence S. Factors associated with hypothermia within the first 6 h of life in infants born at ≥34 weeks’ gestation: a multivariable analysis. BMC Pediatr. (2022) 22(1):427. doi: 10.1186/s12887-022-03512-x
11. Merazzi D, Bresesti I, Tagliabue P, Valsecchi M, De Lorenzo P, Lista G. Body temperature at nursery admission in a cohort of healthy newborn infants: results from an observational cross-sectional study. Ital J Pediatr. (2020) 46(1):46. doi: 10.1186/s13052-020-0810-z
12. Sedin G, Hammarlund K, Strömberg B. Transepidermal water loss in full-term and pre-term infants. Acta Paediatr Scand Suppl. (1983) 305:27–31. doi: 10.1111/j.1651-2227.1983.tb09855.x
13. Zijlma A. The Weather and Climate in South Africa. TripSavvy. 2019 [cited 10 January 2020]. Available at: https://www.tripsavvy.com/south-africa-weather-and-average-temperatures-4071461
Keywords: hypothermia, neonate, caesarean section, season, birth weight
Citation: Patel M, Ramagaga N, Kruger D, Lehnerdt G, Mansoor I, Mohlala L, Rendel D, Zaheed F, Jordaan M, Mokhachane M, Nakwa FL and Mphahlele R (2022) Hypothermia in neonates born by caesarean section at a tertiary hospital in South Africa. Front. Pediatr. 10:957298. doi: 10.3389/fped.2022.957298
Received: 30 May 2022; Accepted: 4 November 2022;
Published: 6 December 2022.
Edited by:
Andrew Steenhoff, Children's Hospital of Philadelphia, United StatesReviewed by:
Michael Espiritu, Weill Cornell Medical Center, NewYork-Presbyterian, United StatesWaldemar Carlo, University of Alabama at Birmingham, United States
© 2022 Patel, Ramagaga, Kruger, Lehnerdt, Mansoor, Mohlala, Rendel, Zaheed, Jordaan, Mokhachane, Nakwa and Mphahlele. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: M. Patel bWFyaWFtLnBhdGVsMTExQGdtYWlsLmNvbQ==
†These authors share senior authorship
Specialty Section: This article was submitted to Neonatology, a section of the journal Frontiers in Pediatrics
 Mariambibi Patel
Mariambibi Patel Neo Ramagaga
Neo Ramagaga Danielle Kruger
Danielle Kruger Grace Lehnerdt
Grace Lehnerdt Imraan Mansoor
Imraan Mansoor Lesedi Mohlala
Lesedi Mohlala Dylan Rendel
Dylan Rendel Fathima Zaheed
Fathima Zaheed Mimie Jordaan
Mimie Jordaan Mantoa Mokhachane
Mantoa Mokhachane Firdose Lambey Nakwa
Firdose Lambey Nakwa Ramatsimele Mphahlele
Ramatsimele Mphahlele