- 1Centre on Climate Change and Planetary Health, Department of Public Health, Environments and Society, London School of Hygiene and Tropical Medicine, London, United Kingdom
- 2Department of Infectious Disease Epidemiology, London School of Hygiene and Tropical Medicine, London, United Kingdom
- 3Division of Paediatrics and Adolescence Medicine, Faculty of Medicine, Institute of Clinical Medicine, University of Oslo, Oslo, Norway
- 4Department of Paediatrics and Adolescent Health, University of Botswana, Gaborone, Botswana
Background: Increased rates of exclusive breastfeeding could significantly improve infant survival in low- and middle-income countries. There is a concern that increased hot weather due to climate change may increase rates of supplemental feeding due to infants requiring fluids, or the perception that infants are dehydrated.
Objective: To understand how hot weather conditions may impact infant feeding practices by identifying and appraising evidence that exclusively breastfed infants can maintain hydration levels under hot weather conditions, and by examining available literature on infant feeding practices in hot weather.
Methods: Systematic review of published studies that met inclusion criteria in MEDLINE, EMBASE, Global Health and Web of Science databases. The quality of included studies was appraised against predetermined criteria and relevant data extracted to produce a narrative synthesis of results.
Results: Eighteen studies were identified. There is no evidence among studies of infant hydration that infants under the age of 6months require supplementary food or fluids in hot weather conditions. In some settings, healthcare providers and relatives continue to advise water supplementation in hot weather or during the warm seasons. Cultural practices, socio-economic status, and other locally specific factors also affect infant feeding practices and may be affected by weather and seasonal changes themselves.
Conclusion: Interventions to discourage water/other fluid supplementation in breastfeeding infants below 6 months are needed, especially in low-middle income countries. Families and healthcare providers should be advised that exclusive breastfeeding (EBF) is recommended even in hot conditions.
Introduction
The World Health Organization (WHO) recommends that infants are exclusively breastfed for the first 6 months of their life (1). Breast milk safely fulfills all nutritional and energy needs for the first few months of life and contains antibodies which are protective against childhood infections (2). A Lancet review of data from 153 countries found that exclusive breastfeeding (EBF) reduced infant mortality by 88% and was protective against infections and being overweight in later life and diabetes (2). EBF for the first 6months of life is one of the most effective interventions to promote adequate growth and prevent neonatal, infant, and childhood illness (3).
Infants in LMICs tend to experience longer durations of breastfeeding compared to those in high income countries (HICs) (2, 4). However, rates of early initiation of breastfeeding (the first hour after delivery is important for future breastmilk production) and EBF remain low in LMICs (2). Just over 40% of infants are exclusively breastfed until 6 months of age (with considerable variation in rates between settings) (5).
The initiation and duration of EBF can be determined by a range of factors including maternal employment, quality of care provided in health facilities, and local practices (6–8). Breastfeeding advice is provided by health workers, peers and family circles, and cultural beliefs can be highly influential on maternal intention to breastfeed exclusively (9–11). Past studies have detailed the common practice of giving supplementary water and/or tea to infants below the age of 6 months in many countries with hot climates (12, 13). Having or perceiving an inadequate milk supply is also associated with supplementing breastmilk with other foods or liquids (9, 14, 15). Another factor commonly identified with supplementing breast milk, particularly in hot climates, is a belief that the breastfeeding infant is thirsty, and therefore requires water (16–19).
The world is warming due to climate change. The International Panel on Climate Change (IPCC) estimates that global mean temperature increase will exceed 1.5–2°C by end of the century compared to the period 1850–1900 (20). Climate change is likely to increase impacts from more frequent and more intense heat waves. Observations confirm that the frequency and intensity of heatwaves has increased in Africa (21), while climate modeling has projected severe changes in both wet and dry extremes across Africa in the future (22).
This review is part of the CHAMNHA project that aims to understand how climate change may affect the health of pregnant women, newborns and infants in Africa (23). Despite increasing international attention on climate risks to maternal and neonatal health, no existing systematic review on heat impacts on infant feeding practices could be identified. Therefore, this review was conducted to explore how hot weather and/or climate conditions might affect perception of infant thirst and rates of non-EBF.
Methods
Objectives
To understand how hot weather conditions may impact infant feeding practices by identifying and appraising evidence that exclusively breastfed infants can maintain hydration levels under hot weather conditions, and by examining available literature on infant feeding practices in hot weather.
Search strategy
Four medical science databases were searched: MEDLINE, EMBASE, and Global Health from Ovid, plus Web of Science. Search terms were scoped for the weather and climate exposures by researching existing systematic reviews involving ambient heat exposures, drought, and hot climates (24–26), and search terms for “infant feeding practices” were scoped by researching an existing systematic review of breastfeeding and other infant feeding practices (27).
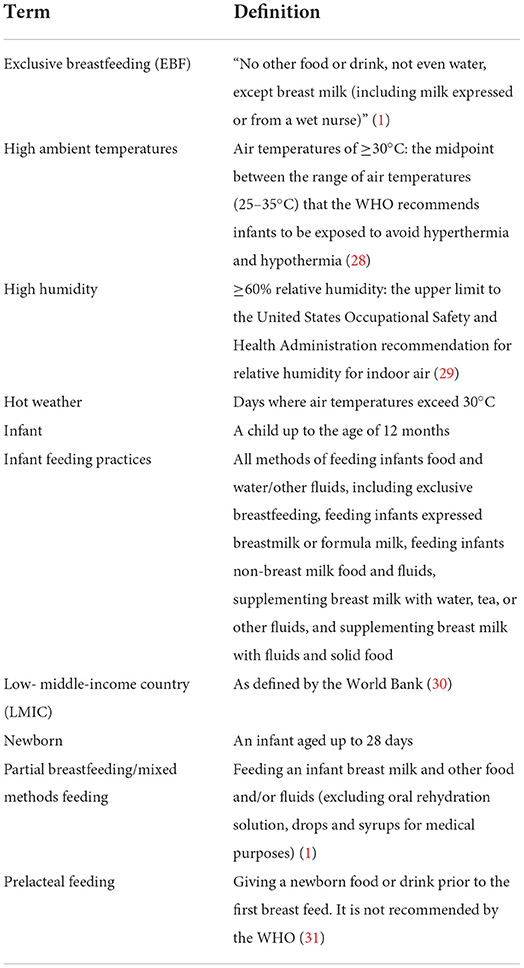
See Table 1 for definitions used in this review.
Inclusion and exclusion criteria for studies were defined prior to running the search in a PICO format:
• Population: infants up to the age of 1 year living in LMICs.
• Interventions/Exposures: ambient temperature, ambient humidity, hot weather, hot climate, hot season. Also, socio-cultural beliefs/medical advice relating to infant feeding in hot weather/climate conditions, EBF.
• Comparators: the same study sample under different weather/temperature conditions, the same study sample not breastfeeding exclusively, a control group from the same or very similar population.
• Outcome: weight loss, dehydration, infant feeding practices.
Articles were excluded if they:
• Reported heat exposures from heat sources unrelated to weather, unless heat exposures were controlled in order to simulate weather conditions.
• Referred to feeding practices of animals.
• Not in English.
• Were not published in peer-reviewed journals.
• Were reviews or commentaries.
• Examined feeding practices of children older than 1 year.
• Only report a study population in a high-income country.
• Were published prior to 1970.
The last search was conducted on 11th July 2020. The reference lists of included papers and review papers were examined for relevant articles. Google Scholar was also used to find more recent papers by searching for articles that cited those already identified. Search results were screened by one reviewer (JE) by title. Abstracts were then screened by the same reviewer and excluded if irrelevant. The full text versions of the remaining articles were downloaded and assessed against inclusion and exclusion criteria.
Study quality
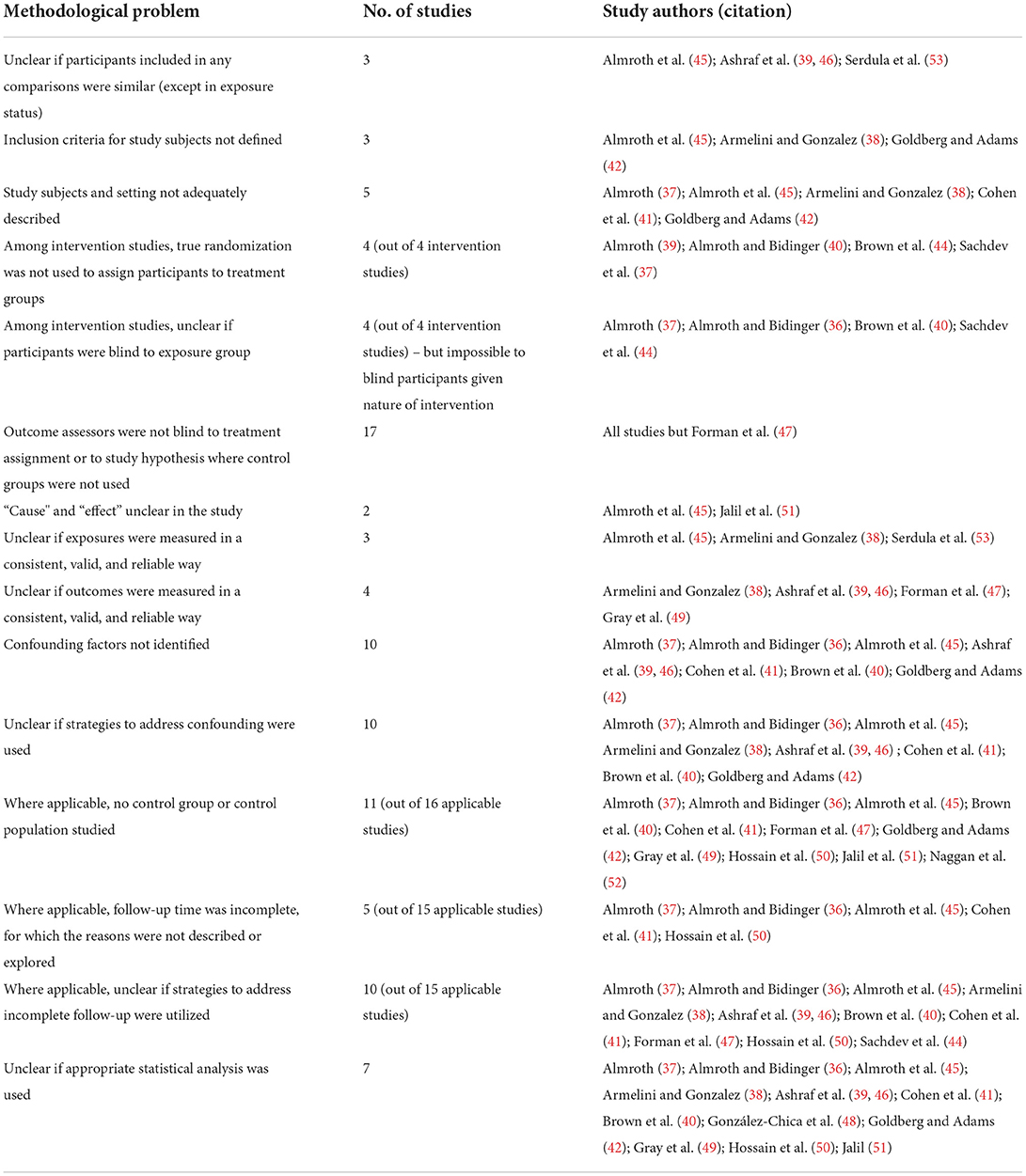
To appraise the quality of each article, the study designs for all articles were assessed according to predetermined quality criteria checklists adapted from the Joanna Briggs Institute critical appraisal tools for analytical cross-sectional studies (32), cohort studies (32), randomized controlled trials (33), and quasi-experimental studies (33) (for the purposes of this review, intervention studies that did not meet all of the methodological criteria of randomized controlled trials were designated quasi-experimental studies). These checklists were used to inform the rating of the quality of each study, which was either “poor,” “fair,” or “good” (details can be found in the Tables 4 and 5).
Data extraction
For this review, data were extracted from each study on the study setting, population, sample size, methods, exposure measures, outcome measures, results, authors' conclusions, and potential sources of bias.
Data synthesis
Findings were described using a narrative synthesis (34). Due to heterogeneity in study designs, a meta-analysis was not appropriate. The included studies were divided into two categories and findings compared within each group:
1. Studies that investigated the association between EBF and ambient temperature and/or humidity on infant hydration, including:
i. Associations between EBF and indices of infant hydration (e.g., urine specific gravity, urine volume etc.).
ii. Associations between temperature and indices of infant hydration;
iii. Associations between EBF and indices of infant hydration modified by temperature.
2. Studies that investigated how weather factors influence infant feeding practices, including:
i. Associations between ambient temperatures or the heat season and infant feeding practices;
ii. Explanations for these associations, including reports whether infant water supplementation was perceived to be necessary in hot conditions.
For studies in the first group, descriptive data was summarized in tables (34). For studies in the second category, a thematic analysis of the key findings was conducted to identify pathways by which hot weather and climate exposures might impact infant feeding. Methodological robustness and study quality are described in the results and discussion.
Results
Eighteen studies met the inclusion criteria. The full texts for three of these articles could not be located. Bibliography searching of already identified papers yielded two additional included articles and searching for articles which cited already selected papers in Google Scholar identified one additional article (see Figure 1).
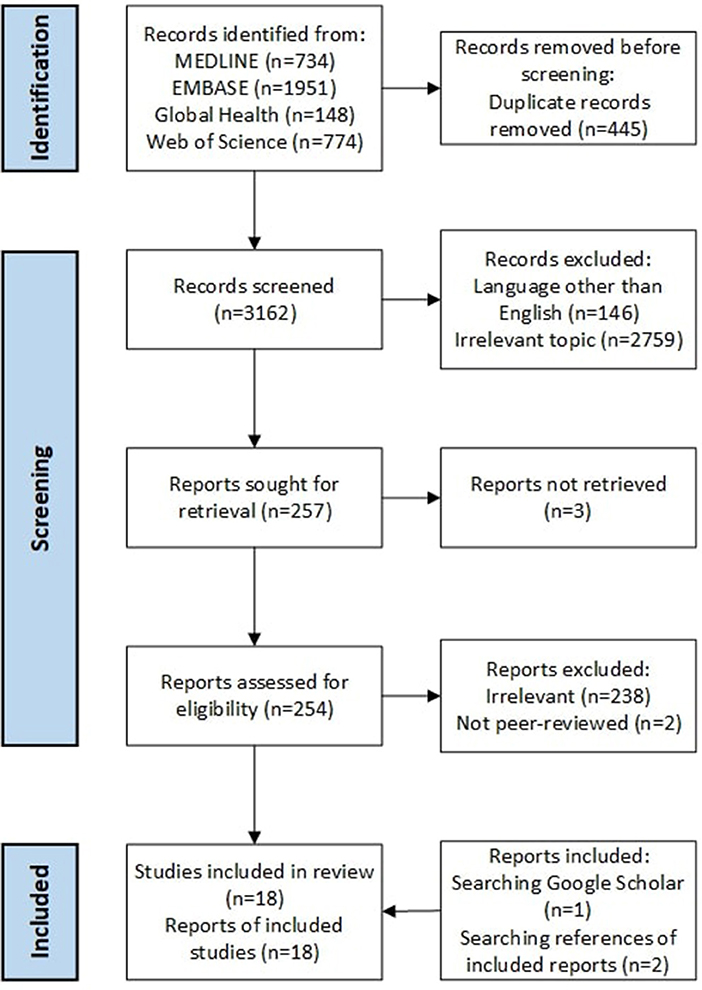
Figure 1. PRISMA flow diagram of included and excluded records [adapted from (35)].
Dates of publication ranged from 1978 to 2012 with most papers more than 10 years old. The review found a wide range of study designs:
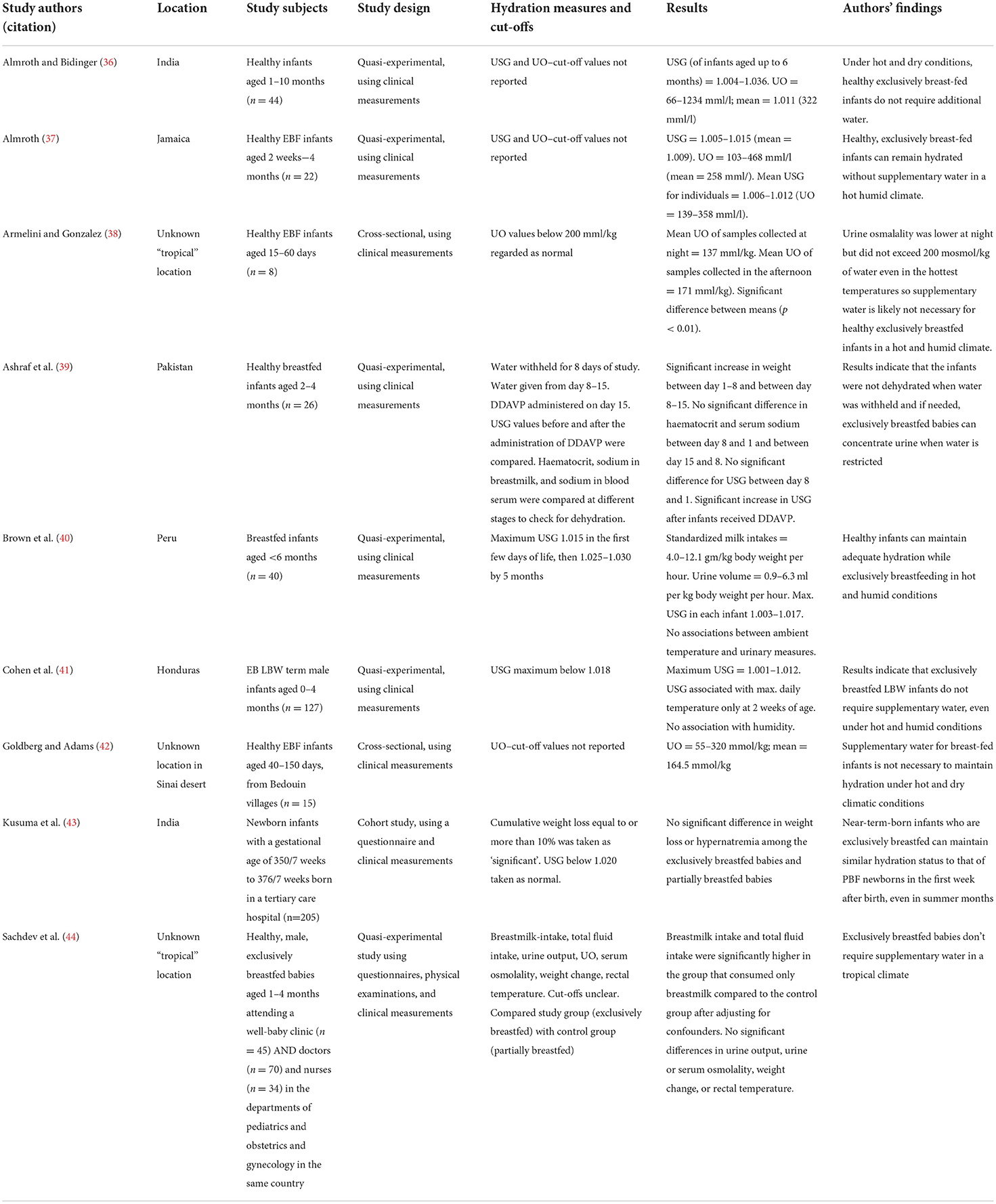
1. Studies investigating the effect of EBF and ambient temperature and humidity on infant hydration (summarized in Table 2):
° Quasi-experimental studies (n = 6).
° Cross-sectional studies (n = 2).
° Cohort study (n = 1).
2. Studies investigating factors (specifically including weather/season/climate exposures) affecting infant feeding practices (summarized in Table 3):
° Cohort studies (n = 7).
° Cross-sectional study (n = 1).
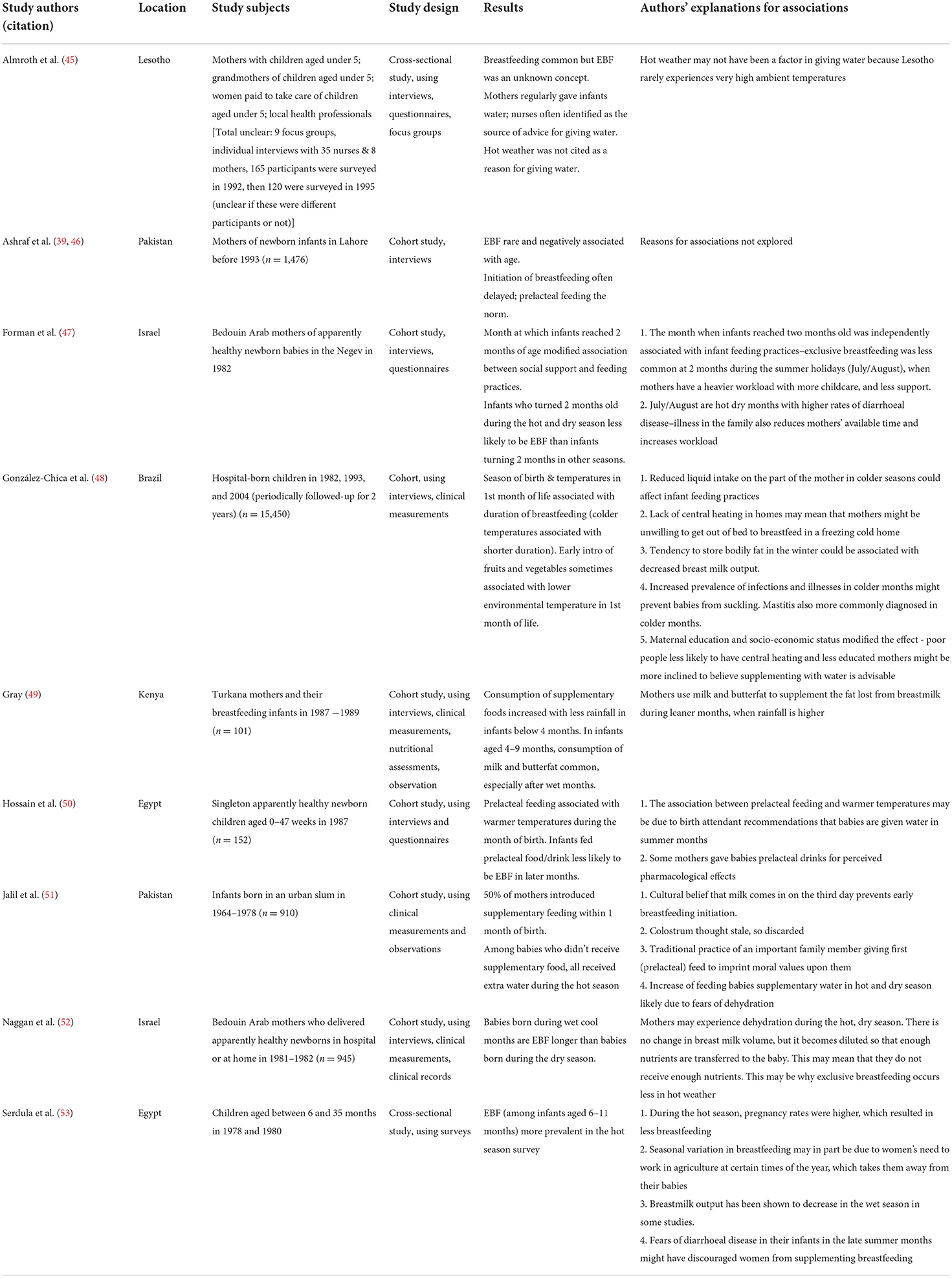
Table 3. Summary of studies investigating determinants of infant feeding practices relating to hot seasons and high ambient temperatures.
Studies were conducted in Africa, Asia, and South America: Pakistan (n = 3), India (n = 2), Egypt (n = 2), Israel (n = 2), Brazil (n = 1), Honduras (n = 1), Lesotho (n = 1), Peru (n = 1), Kenya (n = 1), and Jamaica (n = 1). The country locations of three studies were not identified in the journal articles, but since these articles specified the locations were “tropical,” it was inferred that the settings were more likely to be in LMICs than in HICs.
Effect of EBF on infant hydration in hot weather/climate conditions
The 6 quasi-experimental studies (see Table 2) involved requesting participating mothers to exclusively breastfeed their infants and investigating the effect of this on infant health and hydration status. Two studies were cross-sectional (38, 42) and a cohort study (43). The intervention group (in which mothers were requested to exclusively breastfeed) was compared to a control group (where mothers followed their usual feeding regime). It would not be possible to randomize for heat exposures. The studies were published between the 1970's and the 2000's. The most recent study was published in 2009 (43) but the findings of the quasi-experimental studies are likely to still be relevant.
Measures of infant hydration included urine specific gravity (USG), urine osmolality (UO), urine volume, total fluid intake, and infant weight change. USG and UO are two (correlated) measures of urine concentration and can be used to diagnose abnormal hydration levels when the subject's maximal urine concentration ability is known (54). There is no cut-off value for either USG or UO in the medical literature that distinguishes normal hydration from dehydration, as urine concentration ability is affected by many variables, including sex and age (55). In order to interpret USG or UO values, therefore, many studies also used additional health measures (e.g., identified participants' likely maximal urine concentration abilities) or compared with baseline values from start of study. Two studies used a cut-off value for “normal” USG; ≥ 1.020 (43) and ≥ 1.018 (41), but neither cited sources supporting these thresholds.
Nearly all the studies measured USG and/or UO and showed a high level of variance, reflecting the natural high variability in USG and UO levels, and also known variation in subgroups (infants of low birthweight and infants born near-term (with a gestational age of 350/7−376/7 weeks) (41, 43). In several studies, additional measures were also used to validate assigned outcome status or to investigate risk factors for the primary outcome, including USG, infant weight, fluid and/or breast milk intake, blood serum sodium, haematocrit, concentration of sodium in the mother's breast milk, rectal temperature, and blood serum osmolality. Increased haematocrit is a consequence of water loss and can therefore indicate dehydration (56–58). It is worth noting that there is no formal measurement methodology for dehydration in infants (59). Weight loss has traditionally been used as a “gold standard” measure of infant dehydration (59), but it is not always possible to obtain pre-dehydration weight for comparison (60, 61). A mix of measures has been shown to be most reliable for assessing dehydration (59–61).
As far as can be ascertained, temperatures and relative humidity levels measured during the studies ranged from 11–41°C to 10–96%, respectively. The average range of temperatures was 26.5–34.8°C and the average range of relative humidity levels was 38.8–69.2%. For the studies that recorded it, the average mean temperature was 29.7°C and the average mean level of relative humidity was 61%. Almost all studies that reported weather conditions reported mean temperatures above 30°C (36, 40–44) and most studies reported relative humidity to be 60% or above (37–41, 43).
All studies reported that even under hot conditions, exclusively breastfed infants maintained normal hydration levels without concentrating urine to maximal levels and concluded that supplementary water was therefore not necessary. Several studies concluded that exclusively breastfed infants could maintain normal levels of hydration in hot and humid conditions (37, 38, 41, 44). Only one study investigated hydration levels of exclusively breastfed infants in hot and dry conditions (42); these authors also concluded that the lack of water supplementation did not provoke abnormal dehydration. Furthermore, supplementary water did not appear necessary for exclusively breastfed infants that were low birthweight (41) or born near-term (43). No studies investigated or measured hydration levels or any other health indicators in the mothers.
Comparing exclusively breastfed and partially breastfed infants, no significant difference in incidence of weight loss or hypernatraemia was found (43), nor were there significant differences in urine output, urine or serum osmolality, weight change, or rectal temperature between exclusively breastfed infants and a control group (44). Even when infants who had been partially breastfed previously were breastfed exclusively for a week, observed levels of haematocrit and sodium in blood serum and USG did not change, suggesting that withholding water did not cause dehydration (39). In one study, infants were injected with desmopressin, which is a type of medication that limits the amount of water that is eliminated into urine (62). The infants then experienced a significant increase in USG, suggesting that exclusively breastfed babies can concentrate their urine when water is restricted and do not experience dehydration (39).
Effects of weather and climate exposures on infant feeding practices
Most of the included studies of infant feeding practices in hot weather were cohort studies (see Table 3) (46–52); the remaining two studies had a cross-sectional design (45, 53).
Studies investigating how factors relating to the weather or season affect infant feeding practices reported very different strengths and directions of associations. A cohort study conducted in Brazil (48) and a cross-sectional study conducted in Egypt (53) found that prevalence and duration of EBF increased in the warmer months. Conversely, four cohort studies, all conducted in either Pakistan (46, 51) or Israel (47, 52), found the opposite - that prevalence and duration of EBF decreased in the warmer months. In Kenya, a cohort study found that rainfall was also associated with lower rates of EBF (49).
Proposed or investigated mechanisms behind these associations were varied. A cohort study conducted in Egypt (48) found that prelacteal feeding was associated with both warmer temperatures during the month of birth and with lower rates of EBF in later months of life. The authors proposed that birth attendants were advising mothers to give infants water, particularly in summer months. A cross-sectional study in Lesotho (45) reported advice from healthcare providers also encouraging mothers to feed their infants supplementary water, although hot weather was not the justification for this recommendation. Studies of communities in Pakistan (51) and Israel (46) reported beliefs among mothers that dehydration was a risk for their babies in the hot and dry season, and so supplemented their breast milk with water more frequently during these periods.
Some associations between weather and infant feeding practices were found to be modified or confounded by other variables. For example, a cohort study of Bedouin women in Israel found that the relationship between mothers' experience of social support and infant feeding practices was modified by the infant's season of birth (47). School holidays took place during the hot, dry months, placing more childcare responsibilities on breastfeeding mothers, therefore higher temperatures seemed to affect rates of EBF only by their coinciding with the end of the school term. Similarly, research in Egypt indicated that associations between hot weather and reduced rates of EBF could be in part explained by higher pregnancy rates in the hot season, rather than temperatures themselves (53). In some settings, breastfeeding while pregnant is believed to cause the breast milk to become poisonous, therefore mothers stop breastfeeding as soon as they become aware of pregnancy (17), although it is not clear from the report if this is the case in the Egyptian study population. It was also proposed that Egyptian women's participation in seasonal agriculture might take them away from their infants and limit breastfeeding, which could also explain why EBF was less prevalent in summer (53). Furthermore, lower rates of diarrhoeal disease occurred in the early summer months–women were less inclined to supplement breastfeeding when there was a high risk of diarrhoeal disease, for fear of giving infants contaminated water (53).
Some studies found associations in the opposite direction: reduced rates of EBF were associated with cooler or wetter weather. It was reported that in the leaner, wetter months, Kenyan Turkana mothers would feed infants milk and butterfat to supplement fat perceived to have been lost from breast milk (49). Studying Brazilian mothers, researchers proposed that reduced liquid intake on the part of the mother in colder seasons could cause real or perceived maternal dehydration, which might encourage supplementing breast milk with fluids to prevent dehydration transferring to the infant (48). Alternatively, the authors proposed that a lack of central heating in homes could mean that mothers were unwilling to get out of bed to breastfeed in a cold home, while increased prevalence of infections and illnesses in infants during colder months could prevent babies from suckling. These hypotheses have not been fully investigated by scientific means, however.
Discussion
All studies investigating hydration in exclusively breastfed infants reported that even under hot conditions, exclusively breastfed infants maintained normal hydration levels, and concluded that supplementary water was therefore not necessary.
The methodological quality of most of these studies was fair (38–41) or poor (36, 37, 42) (see Tables 4, 5). Study designs often did not account for biases or confounding, which weakened the strength of their findings. Many also did not include a control group or any comparisons for the study infants, which meant that it was difficult to isolate any associations, or lack thereof, between EBF and dehydration in hot conditions. With all of this in mind, both of the studies rated “good” (43, 44) also concluded that exclusively breastfed infants do not require supplementary water or fluids in hot conditions, and their findings were found to be less susceptible to bias. Given this and that no study provided any evidence for increased risk of dehydration in exclusively breastfed babies in hot conditions, it would be reasonable to agree with the WHO and UNICEF guidelines that recommend healthy infants up to the age of 6 months are fed exclusively with breast milk, regardless of weather conditions.
Studies investigating how factors relating to the weather, season, or climate affect infant feeding practices were largely rated “fair” (47, 49, 51, 53) or “good” (48, 50, 52) and reported a wide variety of findings. No conclusive general relationship between weather and/or seasonal changes and infant feeding practices could be ascertained–rather, relationships were often context specific, mediated by other distal factors.
Despite no evidence supporting the need (as established by this review), several studies investigating infant feeding practices in LMICs reported that mothers supplemented breast milk because they believed that their infants were at risk of dehydration in hot weather (49–51). This concern has been proposed elsewhere in the literature as a potential reason why women are not breastfeeding exclusively in many LMICs (17, 18, 63–68).
However, fear of infant dehydration in hot conditions is not the only mechanism by which weather can influence infant feeding practices. Time spent taking part in agricultural labor can vary according to weather conditions (69) and was identified in one of the included studies as potentially affecting breastfeeding duration (53). Similarly, a study in Ethiopia indicated that rainfall during the primary agricultural season in a child's first year of life had a significant impact on EBF duration due to mothers increased hours worked in farming (70).
While some of the studies included in this review (51, 52) found that grandmothers, aunts, or the mother's own beliefs influenced infant feeding practices, others (44, 45, 50) reported that it was healthcare providers who advised mothers to give infants below the age of six months supplementary water. Similar findings have been reported elsewhere in the literature (64, 68)–they were not included as studies in this systematic review as they did not match the inclusion criteria. Healthcare providers have an important role to play in encouraging optimal breastfeeding, being one of the main sources of breastfeeding advice and knowledge in many communities. A study of infant feeding practices in Tanzania found that women who received advice on EBF were five times more likely to breastfeed exclusively (18). In communities that are both more vulnerable to climate risks and where access to formal healthcare is limited, increasing heatwaves could increase concerns regarding infant hydration.
Limitations
Only one reviewer screened, selected, assessed, and summarized the included studies, which means that these stages of the review process may have been affected by bias. However, the other co-authors were consulted during these processes to reduce bias. Secondly, this review included studies published as early as 1978, due to the limited number of available studies matching the inclusion criteria. There may be a higher chance of such studies containing outdated information or knowledge, or their findings being less relevant to current practices and/or trends. This review also only included studies published in English, with relevant studies published in other languages probably missed. The literature search was not conducted in regional databases such as Africa-wide, which may have also led to missed records. Other limitations include the lack of detail in included studies on hot weather exposures (so it was not possible to directly compare temperature exposures) and lack of information on the hydration status of the mother. It is reasonable to assume that the mothers in studies were well-hydrated but, in some settings, mothers may be dehydrated with poor nutrition.
Conclusion
A systematic review of studies investigating the ability of exclusively breastfed infants to stay hydrated in hot weather/climate conditions was conducted and found no evidence that exclusively breastfed infants required additional water or other liquids. A systematic review investigating hot weather and climate impacts on infant feeding practices in low- and middle-income settings was also conducted and found that multiple pathways exist by which temperatures and weather may influence infant feeding practices, including the belief that infants required water and/or other liquids alongside breast milk in hot weather or seasons. In addition, some factor, such as the demands on a woman's time (work or childcare), are highly seasonal and/or weather-dependent and linked to reduced time spent breastfeeding.
Global average temperatures are increasing, which means that populations everywhere will be exposed to higher daily temperatures. It has also been suggested that as LMICs economically transition, overall breastfeeding rates could decrease to similar levels to those of HICs (1). It is a concern that there has been a lack of studies conducted in the last two decades on infant feeding practices in hot weather. Future studies of infant feeding practices should use the WHO definition of ‘EBF' consistently, to improve the validity and compatibility of results. Many countries are already experiencing effects of climate change, so research in the worst-affected areas could be particularly relevant for determining intervention priorities for infant health as climate change progresses.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
JE undertook the screening and analyses and led on the drafting of the article. VF, SK, and BN contributed to the review designed and contributed to the drafting of the article. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Natural Environment Research Council (NERC) [Grant Numbers NE/T013613/1, NE/T01363X/1]; Research Council of Norway (RCN) [Grant Number 312601]; The Swedish Research Council for Health, Working Life and Welfare in collaboration with the Swedish Research Council (Forte) [Grant Number 2019-01570]; and the National Science Foundation (NSF) [Grant Number ICER-2028598]; coordinated through a Belmont Forum partnership.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. WHO. Breastfeeding: World Health Organization. (2019). Available online at: https://www.who.int/health-topics/breastfeeding#tab=tab_1 (accessed August 23, 2022).
2. Victora CG, Bahl R, Barros AJ, França GV, Horton S, Krasevec J, et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. (2016) 387:475–90. doi: 10.1016/S0140-6736(15)01024-7
3. Hair AB, Hawthorne KM, Chetta KE, Abrams SA. Human milk feeding supports adequate growth in infants ≤ 1250 grams birth weight. BMC Res Notes. (2013) 6:1–8. doi: 10.1186/1756-0500-6-459
4. Fund UNCs,. Children in an Urban World. New York, NY: UNICEF (2012). Available online at: https://www.unicef.org/media/89226/file/The%20State%20of%20the%20World%27s%20Children%202012.pdf (accessed August 23, 2022).
5. Development Initiatives. 2020 Global Nutrition Report: Action on Equity to End Malnutrition. Bristol, UK: Development Initiatives (2020).
6. Odeniyi AO, Embleton N, Ngongalah L, Akor W, Rankin J. Breastfeeding beliefs and experiences of African immigrant mothers in high-income countries: a systematic review. Matern Child Nutr. (2020) 16:e12970. doi: 10.1111/mcn.12970
7. Osman H, El Zein L, Wick L. Cultural beliefs that may discourage breastfeeding among Lebanese women: a qualitative analysis. Int Breastfeed J. (2009) 4:1–6. doi: 10.1186/1746-4358-4-12
8. Wanjohi M, Griffiths P, Wekesah F, Muriuki P, Muhia N, Musoke RN, et al. Sociocultural factors influencing breastfeeding practices in two slums in Nairobi, Kenya. Int Breastfeed J. (2016) 12:1–8. doi: 10.1186/s13006-016-0092-7
9. Balogun OO, Dagvadorj A, Anigo KM, Ota E, Sasaki S. Factors influencing breastfeeding exclusivity during the first 6 months of life in developing countries: a quantitative and qualitative systematic review. Matern Child Nutr. (2015) 11:433–51. doi: 10.1111/mcn.12180
10. de Jager E, Skouteris H, Broadbent J, Amir L, Mellor K. Psychosocial correlates of exclusive breastfeeding: a systematic review. Midwifery. (2013) 29:506–18. doi: 10.1016/j.midw.2012.04.009
11. Santana GS, Giugliani ERJ, Vieira TdO, Vieira GO. Fatores associados à manutenção da amamentação por 12 meses ou mais: revisão sistemática. J Pediatr. (2018) 94:104–22. doi: 10.1016/j.jped.2017.06.013
12. Kapil U, Verma D, Narula S, Nayar D, Sachdev H, Shah AD, et al. Breast-feeding practices in schedule caste communities in Haryana state. Indian Pediatr. (1994) 31:1227.
13. Marriott BM, Campbell L, Hirsch E, Wilson D. Preliminary data from demographic and health surveys on infant feeding in 20 developing countries. J Nutr. (2007) 137:518S−23S. doi: 10.1093/jn/137.2.518S
14. Mangrio E, Persson K, Bramhagen AC. Sociodemographic, physical, mental and social factors in the cessation of breastfeeding before 6 months: a systematic review. Scand J Caring Sci. (2018) 32:451–65. doi: 10.1111/scs.12489
15. Matsuyama A, Karama M, Tanaka J, Kaneko S. Perceptions of caregivers about health and nutritional problems and feeding practices of infants: a qualitative study on exclusive breast-feeding in Kwale, Kenya. BMC Public Health. (2013) 13:1–13. doi: 10.1186/1471-2458-13-525
16. Alade O, Titiloye MA, Oshiname FO, Arulogun OS. Exclusive breastfeeding and related antecedent factors among lactating mothers in a rural community in Southwest Nigeria. Int J Community Based Nurs Midwifery. (2013) 5:132–8. doi: 10.5897/IJNM2013.0111
17. Cosminsky S, Mhloyi M, Ewbank D. Child feeding practices in a rural area of Zimbabwe. Soc Sci Med. (1993) 36:937–47. doi: 10.1016/0277-9536(93)90085-I
18. Maonga AR, Mahande MJ, Damian DJ, Msuya SE. Factors affecting exclusive breastfeeding among women in Muheza District Tanga northeastern Tanzania: a mixed method community based study. Matern Child Health J. (2016) 20:77–87. doi: 10.1007/s10995-015-1805-z
19. Onah S, Osuorah DIC, Ebenebe J, Ezechukwu C, Ekwochi U, Ndukwu I. Infant feeding practices and maternal socio-demographic factors that influence practice of exclusive breastfeeding among mothers in Nnewi South-East Nigeria: a cross-sectional and analytical study. Int Breastfeed J. (2014) 9:1–10. doi: 10.1186/1746-4358-9-6
20. IPCC. Climate Change 2021: The Physical Science Basis. Contribution of Working Group I to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change: Cambridge University Press. (2021). Available online at: https://www.ipcc.ch/report/sixth-assessment-report-working-group-i/ (accessed August 23, 2022).
21. Harrington LJ, Otto FE. Reconciling theory with the reality of African heatwaves. Nat Clim Chang. (2020) 10:796–8. doi: 10.1038/s41558-020-0851-8
22. Kendon EJ, Stratton RA, Tucker S, Marsham JH, Berthou S, Rowell DP, et al. Enhanced future changes in wet and dry extremes over Africa at convection-permitting scale. Nat Commun. (2019) 10:1–14. doi: 10.1038/s41467-019-09776-9
23. Roos N, Kovats S, Hajat S, Filippi V, Chersich M, Luchters S, et al. Maternal and newborn health risks of climate change: a call for awareness and global action. Acta Obstet Gynecol Scand. (2021) 100:566–70. doi: 10.1111/aogs.14124
24. Ahern M, Kovats RS, Wilkinson P, Few R, Matthies F. Global health impacts of floods: epidemiologic evidence. Epidemiol Rev. (2005) 27:36–46. doi: 10.1093/epirev/mxi004
25. Stanke C, Kerac M, Prudhomme C, Medlock J, Murray V. Health effects of drought: A systematic review of the evidence. PLoS Curr. (2013) 5. doi: 10.1371/currents.dis.7a2cee9e980f91ad7697b570bcc4b004
26. Xu Z, Sheffield PE, Su H, Wang X, Bi Y, Tong S. The impact of heat waves on children's health: a systematic review. Int J Biometeorol. (2014) 58:239–47. doi: 10.1007/s00484-013-0655-x
27. Harrison M, Brodribb W, Hepworth J. A qualitative systematic review of maternal infant feeding practices in transitioning from milk feeds to family foods. Matern Child Nutr. (2017) 13:e12360. doi: 10.1111/mcn.12360
28. World Health Organization M Newborn Health/Safe M. Thermal Protection of the Newborn: A Practical Guide. Geneva: World Health Organization (1997).
29. Fairfax RE,. Reiteration of Existing Osha Policy on Indoor Air Quality: Office Temperature/Humidity Environmental Tobacco Smoke: United States Department of Labor. (2003). Available online at: https://www.osha.gov/laws-regs/standardinterpretations/2003-02-24 (accessed August 23, 2022).
30. World Bank. How Does the World Bank Classify Countries? - World Bank Data Help Desk (2020). Available online at: https://datahelpdesk.worldbank.org/knowledgebase/articles/378834-how-does-the-world-bank-classify-countries (accessed July 29, 2022).
31. World Health Organization and the United Nations Children's Fund. Baby-Friendly Hospital Initiative: Revised, Updated and Expanded for Integrated Care. Section 3. Breastfeeding Promotion and Support in A Baby-Friendly Hospital: A 20-Hour Course for Maternity Staff. Geneva: World Health Organization (2009).
32. Moola S, Aromataris E, Sears K, Sfetcu R, Currie M, Qureshi R. Chapter 7: Systematic Reviews of Etiology Risk. JBI Manual for Evidence Synthesis. (2020). Available online at: https://jbi-global-wiki.refined.site/space/MANUAL. doi: 10.46658/JBIMES-20-08 (accessed August 23, 2022).
33. Tufanaru C, Campbell J, Hopp L. Chapter 3: Systematic Reviews of Effectiveness. JBI Manual for Evidence Synthesis. (2020). Available online at: https://jbi-global-wiki.refined.site/space/MANUAL
34. Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews: A Product From the ESRC Methods Programme. Version 1. (2006). Available online at: https://www.lancaster.ac.uk/media/lancaster-university/content-assets/documents/fhm/dhr/chir/NSsynthesisguidanceVersion1-April2006.pdf (accessed August 23, 2022).
35. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. (2020) 88:105906. doi: 10.1016/j.ijsu.2021.105906
36. Almroth S, Bidinger PD. No need for water supplementation for exclusively breast-fed infants under hot and arid conditions. Trans R Soc Trop Med Hyg. (1990) 84:602–4. doi: 10.1016/0035-9203(90)90056-K
37. Almroth SG. Water requirements of breast-fed infants in a hot climate. Am J Clin Nutr. (1978) 31:1154–7. doi: 10.1093/ajcn/31.7.1154
38. Armelini PA, Gonzalez CF. Breast feeding and fluid intake in a hot climate. Clin Pediatr. (1979) 18:424–5. doi: 10.1177/000992287901800709
39. Ashraf R, Jalil F, Aperia A, Lindblad B. Additional water is not needed for healthy breast-fed babies in a hot climate. Acta Paediatr. (1993) 82:1007–11. doi: 10.1111/j.1651-2227.1993.tb12799.x
40. Brown KH, de Kanashiro HC, del Aguila R, de Romana GL, Black RE. Milk consumption and hydration status of exclusively breast-fed infants in a warm climate. The J Pediatr. (1986) 108:677–80. doi: 10.1016/S0022-3476(86)81040-X
41. Cohen R, Brown K, Rivera L, Dewey K. Exclusively breastfed, low birthweight term infants do not need supplemental water. Acta Paediatr. (2000) 89:550–2. doi: 10.1111/j.1651-2227.2000.tb00336.x
42. Goldberg N, Adams E. Supplementary water for breast-fed babies in a hot and dry climate—not really a necessity. Arch Dis Child. (1983) 58:73. doi: 10.1136/adc.58.1.73
43. Kusuma S, Agrawal SK, Kumar P, Narang A, Prasad R. Hydration status of exclusively and partially breastfed near-term newborns in the first week of life. J Hum Lact. (2009) 25:280–6. doi: 10.1177/0890334408324453
44. Sachdev H, Krishna J, Puri R, Satyanarayana L, Kumar S. Water supplementation in exclusively breastfed infants during summer in the tropics. Lancet. (1991) 337:929–33. doi: 10.1016/0140-6736(91)91568-F
45. Almroth S, Mohale M, Latham MC. Unnecessary water supplementation for babies: grandmothers blame clinics. Acta Paediatr. (2000) 89:1408–13. doi: 10.1111/j.1651-2227.2000.tb02767.x
46. Ashraf R, Jalil F, Khan S, Zaman S, Karlberg J, Lindblad B, et al. Early child health in Lahore, Pakistan: V. Feeding patterns. Acta Paediatr. (1993) 82:47–61. doi: 10.1111/j.1651-2227.1993.tb12906.x
47. Forman MR, Hundt GL, Towne D, Graubard B, Sullivan B, Berendes HW, et al. The forty-day rest period and infant feeding practices among Negev Bedouin Arab women in Israel. Med Anthropol. (1990) 12:207–16. doi: 10.1080/01459740.1990.9966022
48. González-Chica DA, Gonçalves H, Nazmi A, Santos IS, Barros AJ, Matijasevich A, et al. Seasonality of infant feeding practices in three Brazilian birth cohorts. Int J Epidemiol. (2012) 41:743–52. doi: 10.1093/ije/dys002
49. Gray S. Butterfat feeding in early infancy in African populations: new hypotheses. Am J Hum Biol. (1998) 10:163–78.
50. Hossain MM, Radwan MM, Arafa SA, Habib M, DuPont HL. Prelacteal infant feeding practices in rural Egypt. J Trop Pediatr. (1992) 38:317–22. doi: 10.1093/tropej/38.6.317
51. Jalil F, Karlberg J, Hanson L, Lindblad B. Growth disturbance in an urban area of Lahore, Pakistan related to feeding patterns, infections and age, sex, socio-economic factors and seasons. Acta Paediatr. (1989) 78:44–54. doi: 10.1111/j.1651-2227.1989.tb11197.x
52. Naggan L, Forman MR, Sarov B, Lewando-Hundt G, Zangwill L, Chang D, et al. The Bedouin infant feeding study: study design and factors influencing the duration of breast feeding. Paediatr Perinat Epidemiol. (1991) 5:428–44. doi: 10.1111/j.1365-3016.1991.tb00729.x
53. Serdula MK, Seward J, Marks JS, Staehling N, Galal O, Trowbridge FL. Seasonal differences in breast-feeding in rural Egypt. Am J Clin Nutr. (1986) 44:405–9. doi: 10.1093/ajcn/44.3.405
54. Miles B, Paton A, De Wardener H. Maximum urine concentration. BMJ. (1954) 2:901. doi: 10.1136/bmj.2.4893.901
55. Perucca J, Bouby N, Valeix P, Bankir L. Sex difference in urine concentration across differing ages, sodium intake, and level of kidney disease. Am J Physiol Regul Integr Comp Physiol. (2007) 292:R700–R5. doi: 10.1152/ajpregu.00500.2006
56. Barley OR, Chapman DW, Abbiss CR. Reviewing the current methods of assessing hydration in athletes. J Int Soc Sports Nutr. (2020) 17:1–13. doi: 10.1186/s12970-020-00381-6
57. Oppliger RA, Bartok C. Hydration testing of athletes. Sports Med. (2002) 32:959–71. doi: 10.2165/00007256-200232150-00001
58. Zubac D, Marusic U, Karninčič H. Hydration status assessment techniques and their applicability among Olympic combat sports athletes: literature review. Strength Cond J. (2016) 38:80–9. doi: 10.1519/SSC.0000000000000236
59. Friedman JN, Goldman RD, Srivastava R, Parkin PC. Development of a clinical dehydration scale for use in children between 1 and 36 months of age. J Pediatr. (2004) 145:201–7. doi: 10.1016/j.jpeds.2004.05.035
60. Goldman RD, Friedman JN, Parkin PC. Validation of the clinical dehydration scale for children with acute gastroenteritis. Pediatrics. (2008) 122:545–9. doi: 10.1542/peds.2007-3141
61. Gorelick MH, Shaw KN, Murphy KO. Validity and reliability of clinical signs in the diagnosis of dehydration in children. Pediatrics. (1997) 99:e6. doi: 10.1542/peds.99.5.e6
62. Cuzzo B, Padala SA, Lappin SL. Physiology, Vasopressin. StatPearls: StatPearls Publishing (2020).
63. Agnarsson I, Mpello A, Gunnlaugsson G, Hofvander Y, Greiner T. Infant feeding practices during the first six month of life in the rural areas of Tanzania. East Afr Med J. (2001) 78:9–13. doi: 10.4314/eamj.v78i1.9104
64. Engebretsen IMS, Wamani H, Karamagi C, Semiyaga N, Tumwine J, Tylleskär T. Low adherence to exclusive breastfeeding in Eastern Uganda: a community-based cross-sectional study comparing dietary recall since birth with 24-hour recall. BMC Pediatr. (2007) 7:1–12. doi: 10.1186/1471-2431-7-10
65. Kamudoni P, Maleta K, Shi Z, De Paoli M, Holmboe-Ottesen G. Breastfeeding perceptions in communities in Mangochi district in Malawi. Acta Paediatr. (2010) 99:367–72. doi: 10.1111/j.1651-2227.2009.01603.x
66. Mgongo M, Mosha MV, Uriyo JG, Msuya SE, Stray-Pedersen B. Prevalence and predictors of exclusive breastfeeding among women in Kilimanjaro region, Northern Tanzania: a population based cross-sectional study. Int Breastfeed J. (2013) 8:1–8. doi: 10.1186/1746-4358-8-12
67. Qureshi AM, Oche OM, Sadiq UA, Kabiru S. Using community volunteers to promote exclusive breastfeeding in Sokoto State, Nigeria. Pan Afr Med J. (2011) 10:8. doi: 10.4314/pamj.v10i0.72215
68. Shirima R, Greiner T, Kylberg E, Gebre-Medhin M. Exclusive breast-feeding is rarely practised in rural and urban Morogoro, Tanzania. Public Health Nutr. (2001) 4:147–54. doi: 10.1079/PHN200057
69. Arora NK. Impact of climate change on agriculture production and its sustainable solutions. Environ Sustain. (2019) 2:95–6. doi: 10.1007/s42398-019-00078-w
Keywords: breastfeeding, climate, infant care, heat stress, dehydration, systematic review
Citation: Edney JM, Kovats S, Filippi V and Nakstad B (2022) A systematic review of hot weather impacts on infant feeding practices in low-and middle-income countries. Front. Pediatr. 10:930348. doi: 10.3389/fped.2022.930348
Received: 27 April 2022; Accepted: 18 August 2022;
Published: 06 September 2022.
Edited by:
Andrew S. Day, University of Otago, New ZealandReviewed by:
Getu Engida Wake, Debre Berhan University, EthiopiaMaria Oana Sasaran, George Emil Palade University of Medicine, Pharmacy, Sciences and Technology of Târgu Mureş, Romania
Copyright © 2022 Edney, Kovats, Filippi and Nakstad. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jessica M. Edney, amVzc2ljYS5lZG5leUB1a2hzYS5nb3YudWs=
 Jessica M. Edney
Jessica M. Edney Sari Kovats
Sari Kovats Veronique Filippi2
Veronique Filippi2 Britt Nakstad
Britt Nakstad