
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Pediatr., 30 June 2022
Sec. Pediatric Gastroenterology, Hepatology and Nutrition
Volume 10 - 2022 | https://doi.org/10.3389/fped.2022.915085
Background: Hepato-pancreato-biliary (HPB) disease has different causes and types between children and adults, which has been increasingly diagnosed in the pediatric group. Endoscopic retrograde cholangiopancreatography (ERCP) has been gradually considered as a therapeutic method in adults, while in pediatric patients, there are not many reports of its usage. This systematic review and meta-analysis aims to assess the use condition of therapeutic ERCP in the management of pediatric HPB diseases.
Methods: This systematic literature search was conducted in the PubMed, Embase, Web of Science, and Cochrane library databases to identify all relevant articles published from inception to February 2022 that evaluated therapeutic ERCP in pediatric patients with HPB diseases. The researchers included studies in which patients were less than 18 years old and underwent therapeutic ERCP procedures. A random-effects model was used to analyze the usage rate of therapeutic ERCP procedures, procedural success rates, adverse event rates, and the rate of different therapeutic procedures. Subgroup analysis, sensitivity analysis, and meta-regression were conducted to analyze the source of heterogeneity.
Results: A total of 33 articles were included. After homogenization, the overall use of therapeutic interventions accounts for 77% [95% confidence interval (CI) 74–81%] of all ERCP procedures. After excluding outlier studies, the estimation success rate of the therapeutic procedure is 74% (95% CI 69–79%), and adverse event rate is 8% (95% CI 6–10%). In our study, stent placement is the most common procedure, which makes up 75% (95% CI 65–86%) of all therapeutic procedures. In addition, the usage proportion of sphincterotomy (ST), stone extraction/removal, bougienage/balloon dilation is, respectively, 46% (95% CI 39–53%), 34% (95% CI 31–38%), and 26% (95% CI 22–29%).
Conclusion: The ERCP procedure is gradually considered a therapeutic technique in pediatric patients, the proportion of therapeutic ERCP is 77% of total usage, which is increasing every year. Meanwhile, its success rate is relatively high. It reflects that this operation modality is promising in the treatment of HPB disorders and is gradually expanded as more branch technologies are being used. A variety of operations can be achieved through ERCP procedures, and more functions should be developed in the future.
Systematic Review Registration: [https://www.crd.york.ac.uk/prospero/], identifier [CRD42022302911].
Hepato-pancreato-biliary (HPB) disease refers to the condition that affects the liver, pancreas, and biliary system. For adults, most are caused by chronic damage to the organ tissues, while in children, most have various genetic or hereditary causes. Traumatic HPB disruption and severe biliary complications (BC) after liver transplantation have a comparatively lower incidence rate in pediatric patients. Endoscopic retrograde cholangiopancreatography (ERCP) has traditionally been performed to diagnose adult HPB diseases. It has unique effectiveness in delineating ductal anatomy, which is especially beneficial in those patients with pancreaticobiliary maljunction (PBM) (1). With significant advancements in endoscopic techniques, many non-invasive diagnostic methods have replaced ERCP in pediatric populations (2). ERCP today is mainly restricted to therapeutic performance, which includes any interventional procedure performed in addition to a cholangiopancreatogram. Because of the difference in disease types, the indications of therapeutic ERCP between children and adults are significantly different. Children with HPB disease often experience acute abdominal pain, obstructive jaundice, abnormal liver function, and other fatal conditions. Prophylactic surgeries may lead to high-risk post-operative complications, and therapeutic ERCP can improve digestive juice drainage and resolve complications relatively safely. This requires pediatric surgeons to make efforts on establishing specific clinical and technical indications, preparing for the use of minimal invasive equipment as well as an effective procedure for children. Minimal invasive techniques including endoscopic surgery are gradually replacing invasive interventions such as bile duct exploration surgery.
Compared with the adult population, the therapeutic option of ERCP is relatively rare in most children’s hospitals. The usage of therapeutic ERCP specifically in pediatric HPB diseases has not been systematically evaluated. We carry out this systematic review and meta-analysis to comprehensively assess the use condition of therapeutic ERCP in the management of pediatric HPB diseases up to now. Specifically, this will expand the awareness of pediatric surgeons in the use of various minimally invasive techniques through ERCP to treat HPB diseases instead of surgery. What is more, it will contribute to the improvement of these therapeutic methods and enhance the utilization rate in this field.
This systematic review protocol was prospectively registered (PROSPERO ID: CRD42022302911). The review is reported according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement (3).
This systematic literature search was conducted in the PubMed, Embase, Web of Science, and Cochrane library database to identify all relevant articles published from inception to February 2021 that evaluated therapeutic ERCP in pediatric patients with HPB diseases. Trial registry websites such as ClinicalTrials.gov and WHO ICTRP were also searched. The following terms were searched: (“Pediatrics”[Mesh] OR “Child”[Mesh] OR “Adolescent”[Mesh] OR “Infant”[Mesh] AND “Cholangiopancreatography, Endoscopic Retrograde”[Mesh] AND “Therapeutics”[Mesh]). HPB diseases were included in the search results. To be as comprehensive as possible, the search was not restricted to any study types. We also hand-searched the reference lists of candidate articles to find the articles that might have been missed during the literature search. Our whole search strategy for all databases is described in the Supplementary Material.
Study inclusion criteria included the following: (1) the patients were less than 18 years old; (2) the patients underwent therapeutic ERCP procedures; (3) the patients all had HPB diseases; (4) the procedural success rate and adverse event rate were assessed in the studies; (5) they have detailed description and statistics of various specific treatment methods; and (6) they were randomized controlled trials, case-control studies, or cohort studies.
We excluded the studies that were (1) case reports and case series, which particularity cannot represent the general outcome, and their sampling population is too small to perform meta-analysis; (2) editorial letters, expert opinions, review papers, and meta-analysis as to avoid erroneous weighting toward more frequently cited articles; (3) conference abstracts which could not obtain their full study reports as their scientific rigorousness had not been peer-reviewed; (4) endoscopic nasobiliary drainage (ENBD) or endoscopic ultrasound-guided biliary drainage (EUS-BD) were the only therapeutic methods (If ERCP had been included in these studies, the data about ERCP alone was extracted); (5) pertinent data (such as the percentage of therapeutic interventions in all ERCP procedures, procedural success rates, and adverse event rates) were not available; (7) the cases included were not HPB diseases; and (6) not English-language articles.
If similar articles containing the same population or duplicate cases from a single center were available, we included the article that (1) contains the most comprehensive detail of study characteristics; (2) whose data set has the largest sample; (3) is the most recently published one for our review.
All articles searched through the four databases were imported into Endnote for screening. Two independent reviewers (RS and XX) screened all articles relevant to therapeutic ERCP for pediatric HPB diseases for methodological validity, and a third reviewer (QZ) resolved the discordance during the study. Titles, abstracts, and keywords were evaluated firstly, and full texts of the articles were retrieved and evaluated for eligibility after the initial screening. Two reviewers (RS and QZ) assessed the quality measures of the included studies, and discrepancies were adjudicated via consensus or referral to a third reviewer (XX).
Data from the included studies were extracted into a standard form, detailing the first author(s), publication year, country, study design, study population, number of therapeutic ERCP procedures, procedural success rates, and adverse event rates. The number or rate of different therapeutic procedures was also extracted. We contacted the authors of articles for confirmation or correction when there was missing or unclear information in the paper. Data extraction was carried out using Microsoft Excel (Microsoft, Redmond, WA, United States).
On account of variations in study design and reporting among the included publications, we precluded the use of a standard definition for procedural success and post-ERCP adverse events in some specific studies to make a more comprehensive assessment of the outcome. In our review, procedural success was defined as the successful completion of the determined treatment of the desired endoscope therapeutic intervention (cannulation via the papilla to perform certain treatments successfully), and clinical condition improvement [relief of symptoms or improvement of biochemical tests: such as the decrease of total bilirubin, alanine transaminase, and γ-glutamyltranspeptidase (p < 0.01) in liver function tests (LFT)]. Adverse events were defined as overall complications (such as pancreatitis, perforation, and bleeding). In these cases, patients’ treatment should be altered, which means more diagnostic investigation, prescription of antibiotics, prolonged hospitalization, readmission, or even subsequent surgery was needed (4). Death is one of the extremes included.
The probability of publication bias was assessed through the visual inspection of funnel plots and Egger’s regression intercept.
This is a meta-analysis of proportions, which was performed using the Metan program with STATA Version 16 (StataCorp LP, College Station, TX, United States). We provide an overall estimate of the usage percentage of therapeutic interventions in all ERCP procedures, success rates of therapeutic procedures, adverse event rates, and the distribution of different therapeutic interventions. Due to the significant variability between studies, a random-effects meta-analysis was chosen over a fixed-effects meta-analysis using the restricted maximum likelihood method. A total of 95% confidence intervals (CIs) were calculated initially for the rate of each statistical result from the studies. The I2 statistic was used to evaluate the variance attributable to heterogeneity between individual studies. I2 < 25% was considered no heterotrophy, I2 between 25 and 50% was defined as low heterotrophy, I2 between 50 and 75% was defined as moderate heterotrophy, and I2 > 75% was defined as high heterotropy (5).
To find out the source of high heterogeneity, secondary analyses were performed to further investigate the influencing factors. A subgroup analysis was performed based on various countries, types of diseases, the year of publication, and design of the study. A sensitivity analysis of all studies was also performed to exclude papers deemed to be outliers. Outlier papers were identified based on the findings from the inclusive overall estimation.
The quality of all 33 included non-randomized studies was assessed according to the Newcastle–Ottawa scale (NOS) (Table 1). The NOS assessment tool is based on a star grading system, which includes three categorical criteria. According to this standard scoring algorithm, prospective and cross-sectional studies can award a maximum of nine scores and case-control studies can award a maximum of 10 scores. Studies that received a score of above six were deemed as high quality. Two reviewers (RS and XX) independently assessed the study quality using this format, and disagreements were solved by another author (JZ).
We initially searched for 3,897 results, the process was revealed in the PRISMA flow diagram (Figure 1). The search retrieved 2,061 results from Pubmed, 283 results from the Web of Science, 1,512 results from Embase, 36 results from Cochrane, and five results from Registers. All articles were imported into Endnote 20 (Clarivate Analytics) for screening after removing 653 duplicate records. After the first round by reviewing the title and abstracts, 3,244 studies were removed. Of the 294 reports sought for retrieval, one was not retrieved. In the second round, 293 reports were assessed for eligibility, 74 results were reviews, systematic reviews, and meta-analysis, 182 results were case reports, and four results were not published in English. Finally, 33 articles were included in the review.
A total of 33 articles were included (Table 2), the included studies were retrospective studies and prospective studies, which involve two multicenter studies. In the included literature, not all patients undergoing ERCP were treated with endoscopy simultaneously. Some of them are just diagnostic, and others are followed by other treatments such as surgery after diagnosis. In contrast, some of the patients underwent multiple endoscopic therapeutic procedures during one treatment. Therefore, a total of 13,053 therapeutic ER were performed in 14,162 children. The median patient number in each study is 396, and it ranges from 12 to 11,060. Most studies were conducted on minimally invasive therapy for the HPB system, whose indications include all pediatric hepatic, pancreatic, and biliary diseases. Other studies were only conducted on a single condition, such as pancreatic diseases, symptomatic PBM, and complications after liver, intestine, or composite abdominal organ transplantation. The studies cover Occident (the United States, France, Belgium, etc.) and Orient (China, Japan, South Korea, etc.) countries. A total of 20 studies have been conducted in the last decade, and the other 13 studies were performed before that. Seven articles did not report the total number of ERCP procedures, eight articles did not report the procedural success rates, and three articles did not report the adverse events rates. A total of 24 papers present the classification of specific therapeutic methods, and only 10 of them clarify the percentage of each treatment in all therapeutic procedures (Table 3). Due to the diversity of disease classification and complexity of specific treatment, sex and age stratification were not included in the study.
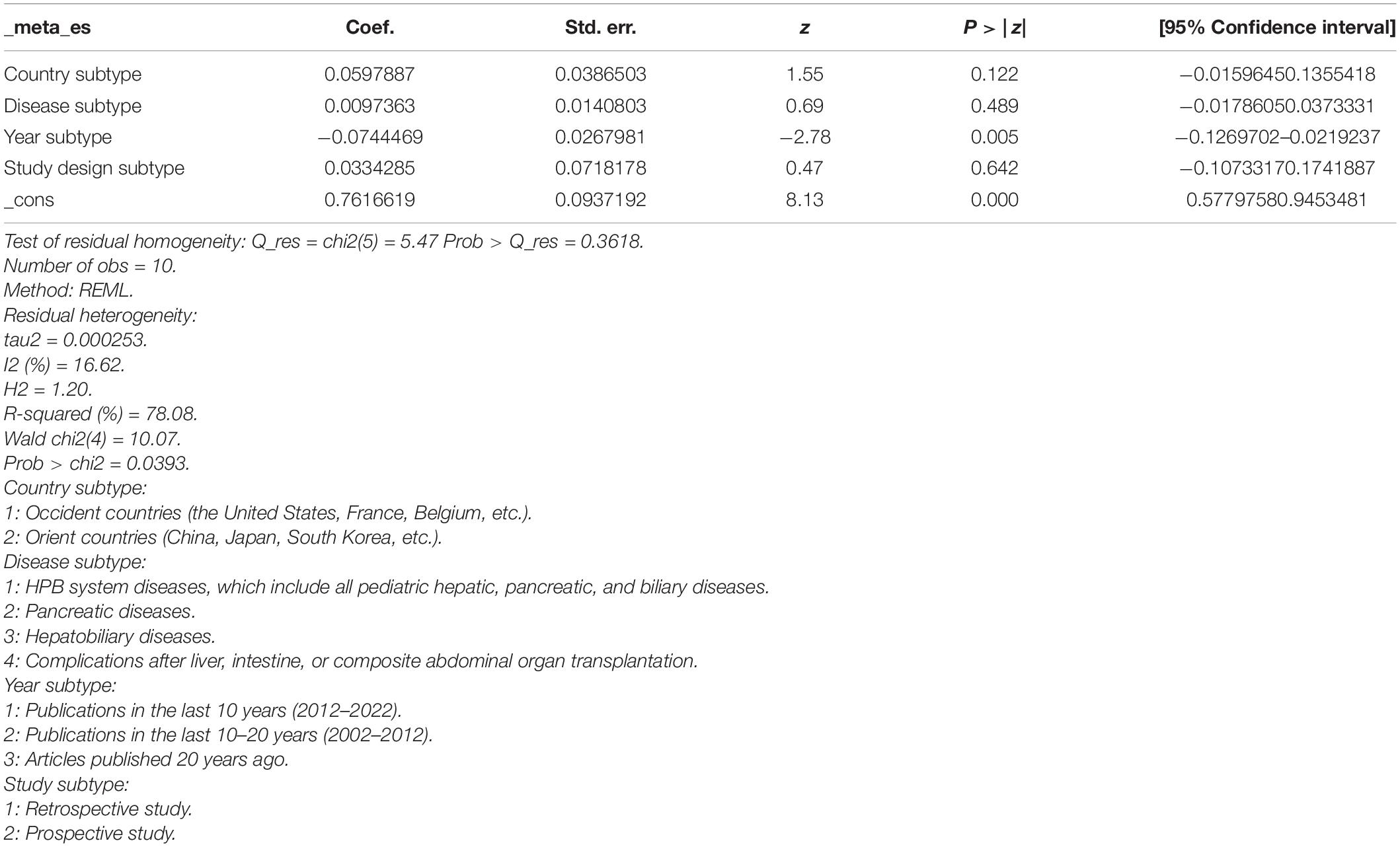
Table 3. Random-effects meta-regression to investigate the reason for heterogeneity of the percentage of therapeutic interventions in all endoscopic retrograde cholangiopancreatography (ERCP) procedures.
To explore the use ratio of ERCP as a minimal interventional therapy, 26 studies were initially included. After sensitivity analysis, we excluded articles with high heterogeneity, and 10 articles were included finally in the result. The usage rate of therapeutic ERCP is 77% (95% CI 74–81%) (Figure 2). A good symmetry can be roughly seen from the funnel plot, suggesting that there is no significant publication bias. However, some points fall outside the funnel plot, indicating that heterogeneity still exists (Figure 3). Regression-based Egger test for small-study effects shows that p = 0.6654, representing no significant publication bias and no small-study effects. This analysis is a confirmation of the stability of our result. Although heterogeneity has been minimized to 49.35%, which is a low heterogeneity, we conduct a meta-regression to investigate the reason for the difference, and the grouping method is shown in Table 3. The results show that the time of publication (year subtype p = 0.005) is the cause of heterogeneity. We divided the studies into three subgroups according to publication time: articles published in the last 10 years (2012–2022), articles published in the last 10–20 years (2002–2012), and articles published 20 years ago. We then performed a subgroup analysis on the year of publication and found that heterogeneity was indeed reduced in all groups. The usage rate of therapeutic ERCP is 80% (95% CI 77–83%) in the last decade (2012–2022), which is higher than the other two groups (Figure 4).
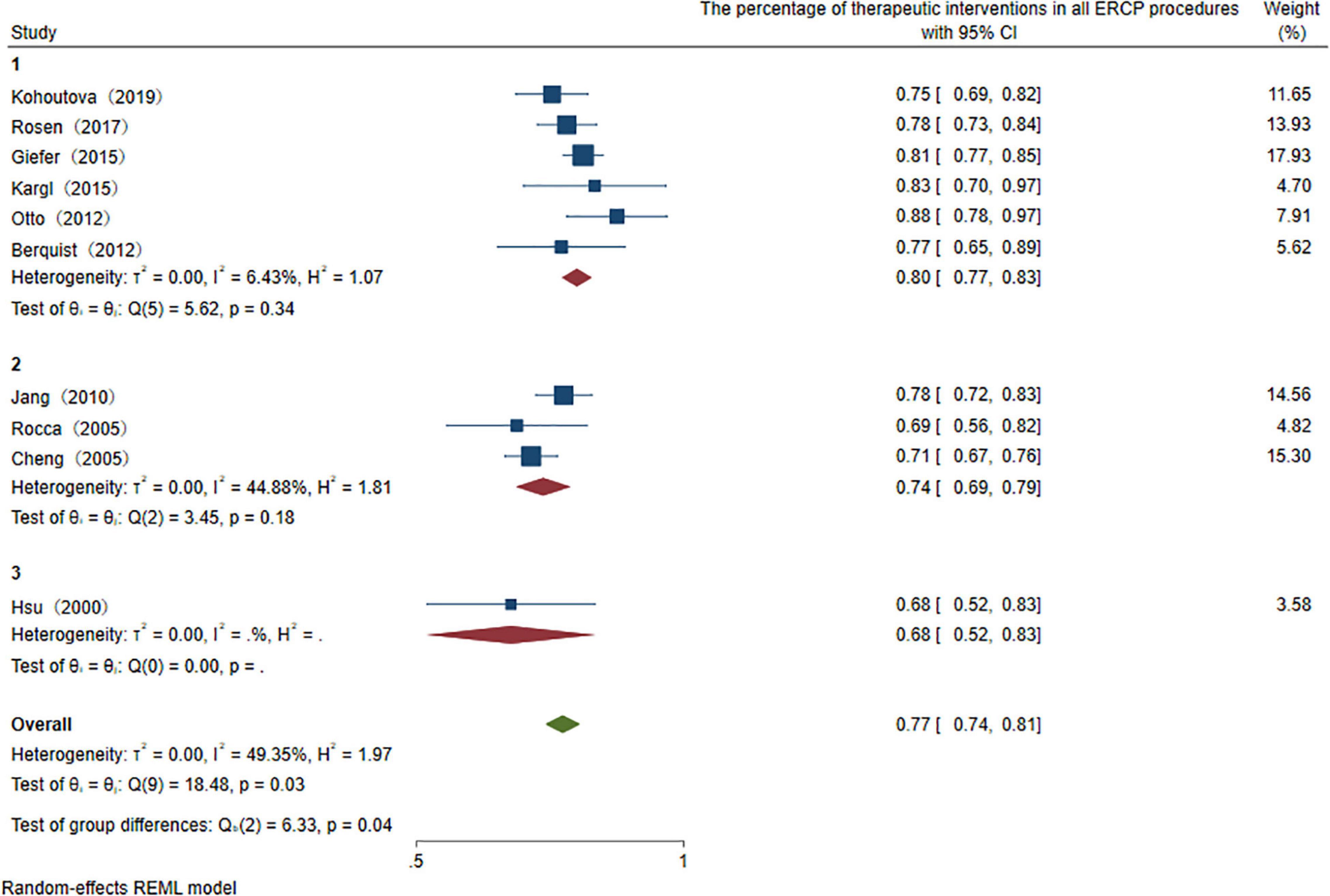
Figure 4. Subtype analysis of publication year of the percentage of therapeutic interventions in all ERCP procedures.
Among the studies which reported success rates of the therapeutic procedure, the heterogeneity among the originally included studies is significant. To investigate the source of heterogeneity, we performed several studies. We divided the countries into Occident and Orient countries. We divided diseases into overall HPB diseases, pancreatic diseases, biliary diseases, and HPB complications after organ transplantation. The year of publication was divided into the last decade, two decades, and two decades ago. Univariate random-effects meta-regression analysis shows that country (p = 0.821), disease (p = 0.453), and publication year (p = 0.596) are not the source of heterogeneity, multiple meta-regression analyses show that R2 (%) < 0.001, which indicate that the model constructed by these three variables is invalid. The subgroup analysis showed the same result because the heterogeneity was not well reduced according to the outcome of these three classifications. Non-parametric trim-and-fill analysis of publication bias indicates that after input five studies, the therapeutic procedural success rate is 87.4% (95% CI 79.4–95.4%) (Figure 5). Sensitivity analysis results show that the study has a significant effect on the heterogeneity. Based on the above analysis, five studies were deemed as outlier studies (Figure 6). After the exclusion of the relevant studies, the overall pooled estimates that the therapeutic procedural success rate is 74% (95% CI 69–79%), I2 = 18.08% (Figure 7).
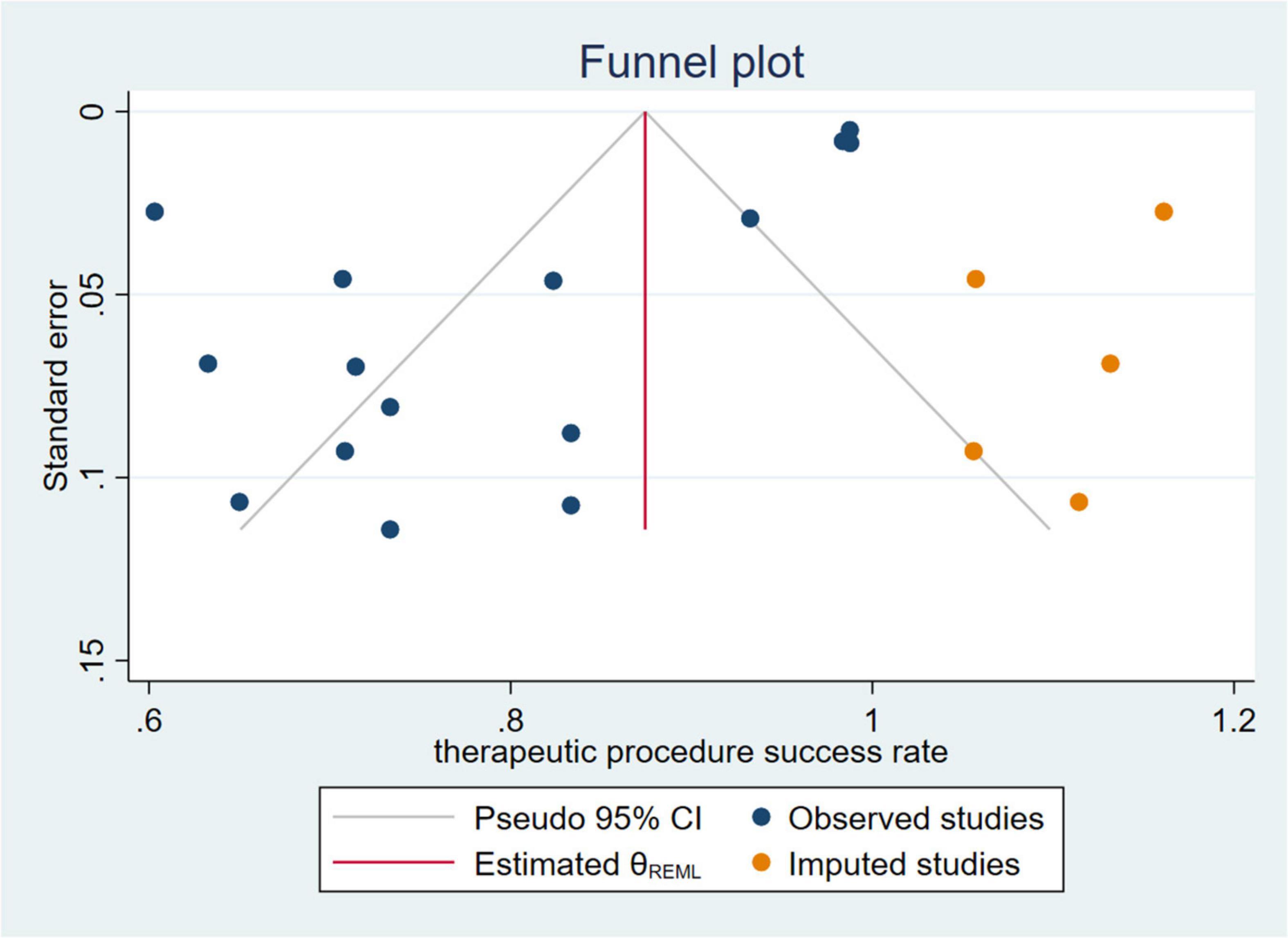
Figure 5. Non-parametric trim-and-fill analysis of publication bias of therapeutic procedure success rate.
Of the studies which represent the adverse rates, regression-based Egger test for small-study effects shows that p = 0.001, which represents the existence of publication bias. Non-parametric trim-and-fill analysis of publication bias indicates that after input seven studies, adverse rates of the therapeutic procedure are 5.6% (95% CI 2.1–9.1%). After sensitivity analysis, 10 outlier studies were excluded. The overall pooled therapeutic adverse event rate is 8% (95% CI 6–10%), I2 = 20.25% (Figure 8).
With the advancement of endoscopic manipulation techniques, more different treatments are performed in the therapeutic process (Table 4). We analyzed several main treatment methods. The results of three studies reveal that the pooled overall usage rate of stent placement is 75% (95% CI 65–86%), I2 = 0.00% (Figure 9). Similarly, when pooling studies after excluding papers with high heterogeneity, the usage rate of sphincterotomy (ST), stone extraction/removal, bougienage/balloon dilation was found to be, respectively, 46% (95% CI 39–53%), I2 = 56.5%, 34% (95% CI 31–38%), I2 = 0.01%, and 26% (95% CI 22–29%), I2 = 0.01% (Figures 10–12), as demonstrated in the forest plot.
Advances in treatment technology and appropriately sized special endoscopes contribute to the expanded utilization in pediatric HPB diseases. More and more cohort studies and case reports on children have been described in this field. However, data on ERCP therapy is still scarce due to the technical difficulty of performing the intervention in pediatric cohorts and there is no comprehensive study due to the historical limitation of the research. Therefore, the efficacy and safety are still contentious. To guide the further development of clinical work, the therapeutic role of ERCP in children should be demonstrated. ERCP is generally accepted as a therapeutic technique, the proportion of therapeutic ERCP in all procedures is 77% demonstrated in our study. Subtype analysis shows that the proportion of use is increasing every year. In the last decade, it is roughly 80% of total usage, 74% in the last 10–20 years, and only 68% 20 years ago. It reflects that this operation modality has a unique clinical value and is being used by more clinical centers in treating pancreaticobiliary disorders in children.
There is a significant difference between children and adults in the type of anesthesia and the type of duodenoscope (6). ERCP in small children was often performed under general anesthesia with endotracheal intubation, to guarantee satisfaction of this population (7). With technological improvements in non-invasive imaging studies, it is gradually replaced by magnetic resonance cholangiopancreatography (MRCP). Though this cross-sectional imaging modality has no ionizing radiation and does not need intravenous contrast, it still has limitations. For example, it has a complementary lower resolution to discern detailed information such as minor ductal anatomy and abnormalities compared with ERCP, especially in pediatric patients (8). Currently, ERCP is mostly chosen as a therapeutic approach allowing the direct visualization of a biliary pancreatic duct structure. Specialized fiber-optic duodenoscopes are generally used in patients younger than 1 year (6). A systematic review and meta-analysis of single-balloon enteroscopy- (SBE-) assisted ERCP on adult biliary interventions reported that pooled procedural success rate was 75.8% (95% CI 71.0–80.3%) (9). Its feasibility in pediatric patients with surgically altered gastrointestinal anatomy has also been reported recently (10). Therapeutic ERCP procedures may be a beneficial and alternative treatment for HPB diseases, whose success rate in our study is 74% (95% CI 69–79%), especially for pediatric patients, because there are considerable risks for them during surgical operations. By analyzing the influencing factors, country, disease, and publication year did not affect the rate of therapeutic success. Using sensitivity analysis, we found that most of the studies that improve heterogeneity have a larger sample size. The study by Mercier et al. (11), which has the greatest heterogeneity, is a recently published large sample multicenter cohort study. In this study, ERCP was therapeutic in 90% of the included cases, and the overall complication rate was 19% (11). Compared with other included studies, it may have represented the rapid development of the therapeutic ERCP technique, the comprehensive results of multiple diseases, and the proficiency of doctors in French and Belgian children’s medical centers.
In the process of discussing the heterogeneity of procedural success rate by disease subtype analysis, we found I2 of HPB complications after the organ transplantation group is only 23.87%. This suggests that there may be a subgroup of diseases that benefit similarly from therapeutic ERCP. BC remain relatively common in the pediatric population after liver transplantation, with a wide range of 6–40% (12). Despite a progress in surgical procedures, anastomotic biliary strictures (ABS), leaks, and other complications often cause graft loss and high morbidity. The type of liver graft or abdominal organ transplant may cause different complications. Endoscopic biliary stenting (EBS) drainage with fully covered self-expandable metal stents (FC-SEMSs) or plastic stent (PS) has been reported to be potentially efficient for ABS after liver transplantation in adults (12), and approximately 10–20% of patients require surgical revision in the long run (13). When access to strictures in the peripheral biliary tree is not possible with ERCP, the Rendezvous technique (PTBD + ERCP) may be useful to insert the stent through the stricture (14). Patients with clinical symptoms initially receive an abdominal ultrasound to evaluate the sign of the presence of biliary tract strictures, then a cholangiogram by PTC can demonstrate the presence of caliber changes. During PTC dilation, the stent placement can be performed. If this is not successful, dilation and stent placement can be performed by ERCP.
The adverse event rate of ERCP is higher when the procedure includes a therapeutic intervention than when it is used for diagnostic purposes. In our study, the pooled therapeutic adverse event rate is 8%, which is higher than the overall complication rate of 6% (15). ERCP is less invasive than surgical therapy for the reason that the treatment is less traumatic, and the admissions were shorter, which did not impair school attendance or other activities. However, some patients still required surgical interventions after therapeutic ERCP, these malpractice cases after ERCP manifest that this treatment was not indicated. In these cases, patients suffered a secondary operation injury, and were at risk of adverse events, hence direct surgery would become less invasive and more time-saving. Reasons for subsequent surgery after therapeutic ERCP are: technical or endoscopic therapy failure (failure of cannulation via the minor papilla or failure of pancreatic duct stone extractions), unsatisfactory results of therapy (intractable and recurrent pain), significant comorbidities (intestinal perforation, duodenal hematoma, acute liver failure, progressive graft injury, etc.), complications (refractory bile duct stricture, bile duct obstruction, significant stenosis of the pancreatic duct, etc.), and specific primary diseases (choledocholithiasis, acute gallstone pancreatitis, chronic idiopathic pancreatitis, biliary atresia, etc.) (Table 5). Pre-operative ERCP before surgery may benefit patients with HPB, it can serve as a transitional step to definitive surgery by relieving clinical symptoms (16, 17). Therapeutic management of HPB diseases by ERCP before laparoscopy is effective in many conditions. It provides a more precise visualization of the anatomical structure, which can help during surgical excision. However, surgery is preferred as an effective modality in certain cases, such as established cystic dilation, because chronic inflammation of the bile duct due to reciprocal pancreaticobiliary reflux is a suspicion of malignancy. Although endoscopic treatment can be considered for most symptomatic patients and the cancelation rate was the lowest (23.0%) in adult patients (18), most pediatric surgeons would recommend surgery. For cases where primary pathology needs to be identified and cases with an unknown underlying cause, surgery is also necessary.
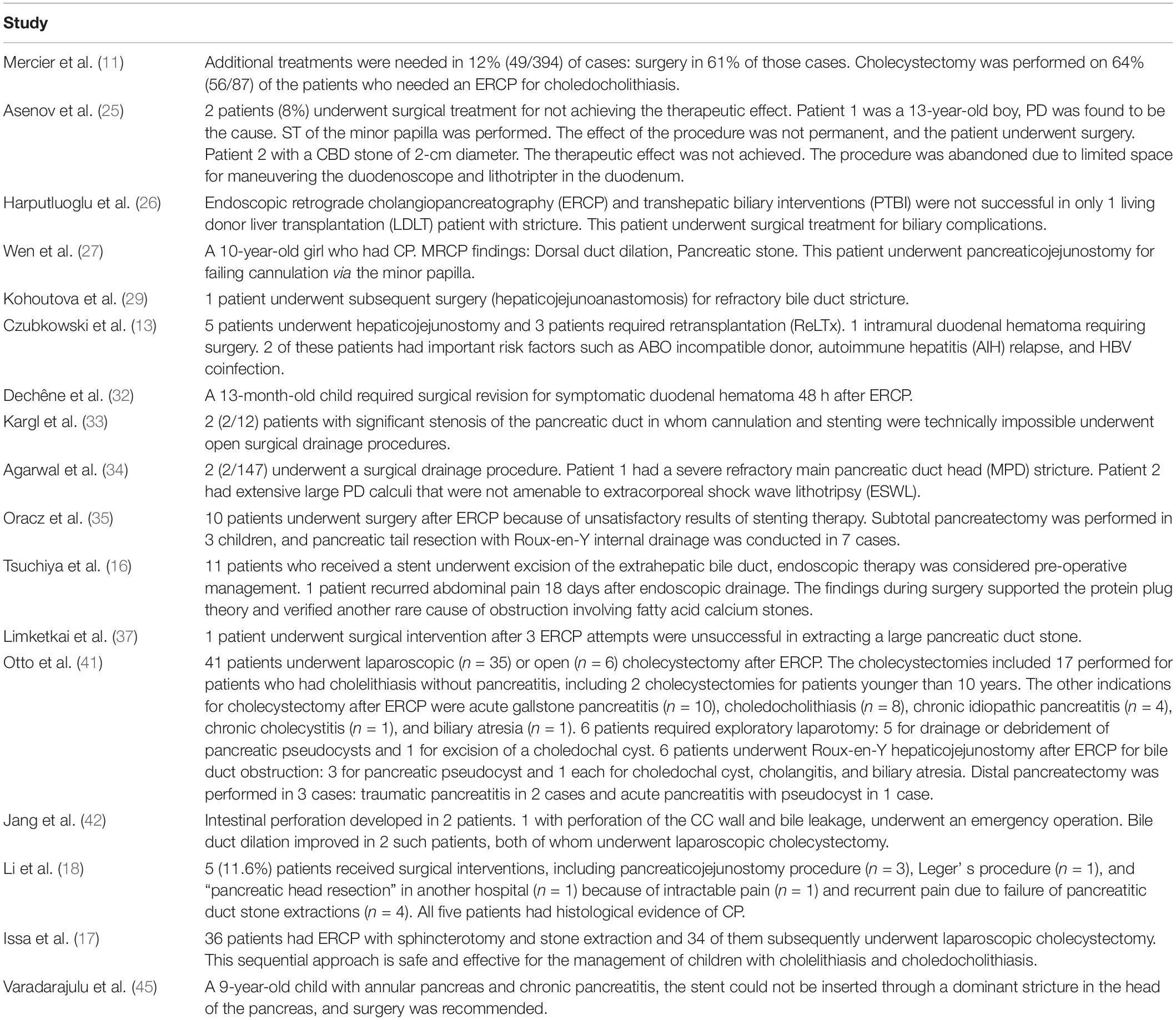
Table 5. Cases required surgical interventions after therapeutic endoscopic retrograde cholangiopancreatography (ERCP).
In our study, the pooled overall usage rate of stent placement is 75%. The usage rate of ST, stone extraction/removal, and bougienage/balloon dilation is, respectively, 46, 34, and 26%. EST or biliary drainage by ERCP is relatively minimal invasive and has a shorter operating duration. Ductal drainage is an effective method to redress elevated intra-organic pressure, which can reduce pain and recurrence. The goal of endoscopic interventions is to reduce pressure in the damaged biliary or pancreatic duct system, early drainage is the main prerequisite for spontaneous closure of the leak. Most patients benefit from ST, EPS, or stent placement through pancreaticobiliary duct decompression. Endoscopic drainage of pancreaticobiliary ducts is now accepted as a viable treatment option in a wide range of cases. Ductal obstruction and ductal disruption (pancreaticobiliary duct leak, ductal stricture, and residual stone diseases) can be treated by ERCP stent placement, especially in anatomically complex patients (19). Our study demonstrates that stent placement is the most common usage, which accounts for 75% of all therapeutic procedures. A recent study shows the temporary use of FC-SEMSs for recurrent benign main pancreatic duct (MPD) strictures in children is feasible and safe (20). In many other cases, such as post-traumatic duct disruption, it can also be managed by temporary stenting. Emergent excision may be dangerous under such particular circumstances, except when precise pancreaticobiliary anatomy is obtained (21). Although there are advantages, prophylactic or therapeutic stent placement may be associated with a higher rate of post-ERCP pancreatitis (PEP), which is demonstrated by a univariate analysis (11). Long-term management requires stent exchange.
It is important to make the proper choice of endoscopic therapy, surgery, and other treatments. More well-designed, large clinical controlled trials are necessary to be performed in this field. There should be evidence-based guidelines to recommend the therapeutic ERCP procedure, which will specifically benefit certain types of pediatric patients. Endoscopists and surgeons who specialized in evaluating pediatric patients usually function as members of a multidisciplinary team. To yield better outcomes and to decrease the number of hospitalizations and surgical interventions, every step of the process, from preparation to subsequent treatment, should be performed in close collaboration with anesthesiologists, pediatricians, pediatric surgeons, and gastroenterologists.
The limitations of our study should be acknowledged: the outcomes of pediatric ERCP performed by surgical vs. medical specialties are different. Small vs. large patient volume healthcare facilities should be compared. Robust volume outcomes should be obtained from a larger population. Pediatric ERCP had different roles in disparate age groups, so age stratification is also a potential influence factor (22). A comprehensive assessment of these data may help expand the awareness of doctors in the usage of minimally invasive techniques to treat HPB diseases and contribute to the improvement of therapeutic methods and enhance the utilization rate in this field.
Our analysis indicates that ERCP is an effective treatment option for pediatric HPB diseases. Given the above analysis, we deem it reasonable to perform therapeutic ERCPs under appropriate conditions to achieve long-term remission. Further study should be conducted to decipher the feasibility of therapeutic ERCP in children.
The original contributions presented in this study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
RS and XX made substantial contributions to the conception or design of the work and the acquisition, analysis, or interpretation of data for the work, and screened all articles relevant to therapeutic ERCP for Pediatric HPB diseases for methodological validity. QZ resolved the discordance during the study and drafted the work or revised it critically for important intellectual content. RS and QZ assessed the quality measures for included studies and discrepancies were adjudicated via consensus or referral to XX. JZ gave approval of the final version to be published. All authors evaluated firstly the titles, abstracts, and keywords and after the initial screening full texts of the manuscript were retrieved and evaluated for eligibility, agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved, contributed to the article, and approved the submitted version.
This study was funded by Xinjiang Uygur Autonomous Region Science Foundation Project (2019D01A12 and 2021D01A38).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2022.915085/full#supplementary-material
1. Rocca R, Castellino F, Daperno M, Masoero G, Sostegni R, Ercole E, et al. Therapeutic ERCP in paediatric patients. Dig Liver Dis. (2005) 37:357–62. doi: 10.1016/j.dld.2004.09.030
2. Saito T, Terui K, Mitsunaga T, Nakata M, Kuriyama Y, Higashimoto Y, et al. Role of pediatric endoscopic retrograde cholangiopancreatography in an era stressing less-invasive imaging modalities. J Pediatr Gastroenterol Nutr. (2014) 59:204–9. doi: 10.1097/MPG.0000000000000399
3. Moher D, Liberati A, Tetzlaff J, Altman DG, Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. (2009) 339:b2535. doi: 10.1136/bmj.b2535
4. Cotton PB, Eisen GM, Aabakken L, Baron TH, Hutter MM, Jacobson BC, et al. lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc. (2010) 71:446–54. doi: 10.1016/j.gie.2009.10.027
5. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
6. Bang JY, Varadarajulu S. Pediatrics: ERCP in children. Nat Rev Gastroenterol Hepatol. (2011) 8:254–5. doi: 10.1038/nrgastro.2011.63
7. Chua GCC, Cyna AM. Satisfaction measures in pediatric anesthesia and perioperative care. Paediatr Anaesth. (2021) 31:746–54. doi: 10.1111/pan.14197
8. Kolodziejczyk E, Jurkiewicz E, Pertkiewicz J, Wejnarska K, Dadalski M, Kierkus J, et al. Versus ERCP in the evaluation of chronic pancreatitis in children: which is the better choice? Pancreas. (2016) 45:1115–9. doi: 10.1097/MPA.0000000000000644
9. Tanisaka Y, Ryozawa S, Mizuide M, Araki R, Fujita A, Ogawa T, et al. Status of single-balloon enteroscopy-assisted endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy: systematic review and meta-analysis on biliary interventions. Dig Endosc. (2021) 33:1034–44. doi: 10.1111/den.13878
10. Yokoyama K, Yano T, Kanno A, Ikeda E, Ando K, Miwata T, et al. The efficacy and safety of balloon enteroscopy-assisted endoscopic retrograde cholangiography in pediatric patients with surgically altered gastrointestinal anatomy. J Clin Med. (2021) 10:3936. doi: 10.3390/jcm10173936
11. Mercier C, Pioche M, Albuisson E, Ponchon T, Gonzalez JM, Barthet M, et al. Safety of endoscopic retrograde cholangiopancreatography in the pediatric population: a multicenter study. Endoscopy. (2021) 53:586–94. doi: 10.1055/a-1209-0155
12. Lee AY, Lehrman, Perito ER, Kerlan RK Jr., Kohi MP, Kolli KP, et al. Non-operative management of biliary complications after Liver Transplantation in pediatric patients: a 30-year experience. Pediatr Transplant. (2021) 25:e14028. doi: 10.1111/petr.14028
13. Czubkowski P, Pertkiewicz J, Markiewicz-Kijewska M, Kaliciński P, Rurarz M, Jankowska I, et al. Endoscopic treatment in biliary strictures after pediatric liver transplantation. Pediatr Transplant. (2018) 22:e13271. doi: 10.1111/petr.13271
14. Yoshiya S, Shirabe K, Matsumoto Y, Ikeda T, Soejima Y, Yoshizumi T, et al. Rendezvous ductoplasty for biliary anastomotic stricture after living-donor liver transplantation. Transplantation. (2013) 95:1278–83. doi: 10.1097/TP.0b013e31828a9450
15. Usatin D, Fernandes M, Allen IE, Perito ER, Ostroff J, Heyman MB. Complications of endoscopic retrograde cholangiopancreatography in pediatric patients; A systematic literature review and meta-analysis. J Pediatr. (2016) 179:160–5.e3. doi: 10.1016/j.jpeds.2016.08.046
16. Tsuchiya H, Kaneko K, Itoh A, Kawashima H, Ono Y, Tainaka T, et al. Endoscopic biliary drainage for children with persistent or exacerbated symptoms of choledochal cysts. J Hepatobiliary Pancreat Sci. (2013) 20:303–6. doi: 10.1007/s00534-012-0519-5
17. Issa H, Al-Haddad A, Al-Salem AH. Diagnostic and therapeutic ERCP in the pediatric age group. Pediatr Surg Int. (2007) 23:111–6. doi: 10.1007/s00383-006-1832-3
18. Li ZS, Wang W, Liao Z, Zou DW, Jin ZD, Chen J, et al. long-term follow-up study on endoscopic management of children and adolescents with chronic pancreatitis. Am J Gastroenterol. (2010) 105:1884–92. doi: 10.1038/ajg.2010.85
19. Perez-Miranda M. Combined ERCP and transhepatic endoscopic ultrasound-guided stent placement for biliary drainage in malignant hilar obstruction: not too good to be true. Endoscopy. (2021) 53:63–4. doi: 10.1055/a-1296-8207
20. Jeong IS, Lee SH, Oh SH, Park DH, Kim KM. Metal stents placement for refractory pancreatic duct stricture in children. World J Gastroenterol. (2018) 24:408–14. doi: 10.3748/wjg.v24.i3.408
21. Cho JM, Jeong IS, Kim HJ, Oh SH, Kim KM. Early adverse events and long-term outcomes of endoscopic sphincterotomy in a pediatric population: a single-center experience. Endoscopy. (2017) 49:438–46. doi: 10.1055/s-0043-103956
22. Keil R, Drábek J, Lochmannová J, Št’ovíček J, Koptová P, Wasserbauer M, Frýbová B. ERCP in infants, children, and adolescents-Different roles of the methods in different age groups. PLoS One. (2019) 14:e0210805. doi: 10.1371/journal.pone.0210805
23. Barakat MT, Cholankeril G, Gugig R, Berquist WE. Nationwide evolution of pediatric endoscopic retrograde cholangiopancreatography indications, utilization, and readmissions over time. J Pediatr. (2021) 232:159–65.e1. doi: 10.1016/j.jpeds.2020.11.019
24. Lin TK, Pathak SJ, Hornung LN, Vitale DS, Nathan JD, Abu-El-Haija M. Clinical outcomes following therapeutic endoscopic retrograde cholangiopancreatography in children with pancreas divisum. J Pediatr Gastroenterol Nutr. (2021) 72:300–5. doi: 10.1097/MPG.0000000000002996
25. Asenov Y, Akın M, Cantez S, Gün Soysal F, Tekant Y. Endoscopic retrograde cholangiopancreatography in children: retrospective series with a long-term follow-up and literature review. Turk J Gastroenterol. (2019) 30:192–7. doi: 10.5152/tjg.2018.18165
26. Harputluoglu M, Demirel U, Caliskan AR, Selimoglu A, Bilgic Y, Aladag M, et al. Endoscopic treatment of biliary complications after duct-to-duct biliary anastomosis in pediatric liver transplantation. Langenbecks Arch Surg. (2019) 404:875–83. doi: 10.1007/s00423-019-01804-y
27. Wen J, Li T, Liu L, Bie LK, Gong B. Long-term outcomes of therapeutic ERCP in pediatric patients with pancreas divisum presenting with acute recurrent or chronic pancreatitis. Pancreatology. (2019) 19:834–41. doi: 10.1016/j.pan.2019.08.004
28. Zeng JQ, Deng ZH, Yang KH, Zhang TA, Wang WY, Ji JM, et al. Endoscopic retrograde cholangiopancreatography in children with symptomatic pancreaticobiliary maljunction: a retrospective multicenter study. World J Gastroenterol. (2019) 25:6107–15. doi: 10.3748/wjg.v25.i40.6107
29. Kohoutova D, Tringali A, Papparella G, Perri V, Boškoski I, Hamanaka J, et al. Endoscopic treatment of chronic pancreatitis in pediatric population: long-term efficacy and safety. United European Gastroenterol J. (2019) 7:270–7. doi: 10.1177/2050640618817699
30. Rosen JD, Lane RS, Martinez JM, Perez EA, Tashiro J, Wagenaar AE, et al. Success and safety of endoscopic retrograde cholangiopancreatography in children. J Pediatr Surg. (2017) 52:1148–51. doi: 10.1016/j.jpedsurg.2017.01.051
31. Giefer MJ, Kozarek RA. Technical outcomes and complications of pediatric ERCP. Surg Endosc. (2015) 29:3543–50. doi: 10.1007/s00464-015-4105-1
32. Dechêne A, Kodde C, Kathemann S, Treckmann J, Lainka E, Paul A, et al. Endoscopic treatment of pediatric post-transplant biliary complications is safe and effective. Dig Endosc. (2015) 27:505–11. doi: 10.1111/den.12420
33. Kargl S, Kienbauer M, Duba HC, Schöfl R, Pumberger W. Therapeutic step-up strategy for management of hereditary pancreatitis in children. J Pediatr Surg. (2015) 50:511–4. doi: 10.1016/j.jpedsurg.2014.05.016
34. Agarwal J, Nageshwar Reddy D, Talukdar R, Lakhtakia S, Ramchandani M, Tandan M, et al. in the management of pancreatic diseases in children. Gastrointest Endosc. (2014) 79:271–8. doi: 10.1016/j.gie.2013.07.060
35. Oracz G, Pertkiewicz J, Kierkus J, Dadalski M, Socha J, Ryzko J. Efficiency of pancreatic duct stenting therapy in children with chronic pancreatitis. Gastrointest Endosc. (2014) 80:1022–9. doi: 10.1016/j.gie.2014.04.001
36. Steen MW, Bakx R, Tabbers MM, Wilde JC, van Lienden KP, Benninga MA, et al. Endoscopic management of biliary complications after partial liver resection in children. J Pediatr Surg. (2013) 48:418–24. doi: 10.1016/j.jpedsurg.2012.10.075
37. Limketkai BN, Chandrasekhara V, Kalloo AN, Okolo PI III. Comparison of performance and safety of endoscopic retrograde cholangiopancreatography across pediatric age groups. Dig Dis Sci. (2013) 58:2653–60. doi: 10.1007/s10620-013-2691-0
38. Enestvedt BK, Tofani C, Lee DY, Abraham M, Shah P, Chandrasekhara V, et al. Endoscopic retrograde cholangiopancreatography in the pediatric population is safe and efficacious. J Pediatr Gastroenterol Nutr. (2013) 57:649–54. doi: 10.1097/MPG.0b013e31829e0bb6
39. Otto AK, Neal MD, Mazariegos GV, Slivka A, Kane TD. Endoscopic retrograde cholangiopancreatography is safe and effective for the diagnosis and treatment of pancreaticobiliary disease following abdominal organ transplant in children. Pediatr Transplant. (2012) 16:829–34. doi: 10.1111/j.1399-3046.2012.01771.x
40. Berquist WE. Endoscopy in the management of pancreaticobiliary complications after liver, intestine, or composite visceral transplantation in children. Pediatr Transplant. (2012) 16:815–7. doi: 10.1111/petr.12000
41. Otto AK, Neal MD, Slivka AN, Kane TD. An appraisal of endoscopic retrograde cholangiopancreatography (ERCP) for pancreaticobiliary disease in children: our institutional experience in 231 cases. Surg Endosc. (2011) 25:2536–40. doi: 10.1007/s00464-011-1582-8
42. Jang JY, Yoon CH, Kim KM. Endoscopic retrograde cholangiopancreatography in pancreatic and biliary tract disease in Korean children. World J Gastroenterol. (2010) 16:490–5. doi: 10.3748/wjg.v16.i4.490
43. Vegting IL, Tabbers MM, Taminiau JA, Aronson DC, Benninga MA, Rauws EA. Is endoscopic retrograde cholangiopancreatography valuable and safe in children of all ages? J Pediatr Gastroenterol Nutr. (2009) 48:66–71. doi: 10.1097/MPG.0b013e31817a24cf
44. Cheng CL, Fogel EL, Sherman S, McHenry L, Watkins JL, Croffie JM, et al. Diagnostic and therapeutic endoscopic retrograde cholangiopancreatography in children: a large series report. J Pediatr Gastroenterol Nutr. (2005) 41:445–53. doi: 10.1097/01.mpg.0000177311.81071.13
45. Varadarajulu S, Wilcox CM, Hawes RH, Cotton PB. Technical outcomes and complications of ERCP in children. Gastrointest Endosc. (2004) 60:367–71. doi: 10.1016/s0016-5107(04)01721-3
46. Pfau PR, Chelimsky GG, Kinnard MF, Sivak MV Jr., Wong RC, Isenberg GA, et al. Endoscopic retrograde cholangiopancreatography in children and adolescents. J Pediatr Gastroenterol Nutr. (2002) 35:619–23. doi: 10.1097/00005176-200211000-00006
47. Poddar U, Thapa BR, Bhasin DK, Prasad A, Nagi B, Singh K. Endoscopic retrograde cholangiopancreatography in the management of pancreaticobiliary disorders in children. J Gastroenterol Hepatol. (2001) 16:927–31. doi: 10.1046/j.1440-1746.2001.02545.x
48. Hsu RK, Draganov P, Leung JW, Tarnasky PR, Yu AS, Hawes RH, et al. Therapeutic ERCP in the management of pancreatitis in children. Gastrointest Endosc. (2000) 51:396–400. doi: 10.1016/s0016-5107(00)70437-8
Keywords: cholangiopancreatography, endoscopic retrograde, therapeutics, pediatrics, hepatobiliary, pancreas, meta-analysis
Citation: Sun R, Xu X, Zheng Q and Zhan J (2022) Therapeutic Endoscopic Retrograde Cholangiopancreatography for Pediatric Hepato-Pancreato-Biliary Diseases: A Systematic Review and Meta-Analysis. Front. Pediatr. 10:915085. doi: 10.3389/fped.2022.915085
Received: 07 April 2022; Accepted: 06 June 2022;
Published: 30 June 2022.
Edited by:
Radhika Chavan, Asian Institute of Gastroenterology, IndiaReviewed by:
Yuichi Okata, Kobe University Hospital, JapanCopyright © 2022 Sun, Xu, Zheng and Zhan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jianghua Zhan, emhhbmppYW5naHVhdGpAMTYzLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.