- 1Pharmacoepidemiology and Drug Safety Unit, Department of Pharmacology, Faculty of Medicine, Universiti Kebangsaan Malaysia Medical Centre, Cheras, Malaysia
- 2Nutritional Science Program and Centre for Healthy Ageing and Wellness, Faculty of Health Sciences, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia
- 3Pro Vice-Chancellor’s Office, Health Campus, Cheras, Malaysia
- 4Department of Pharmacology, Faculty of Medicine, Universiti Teknologi MARA, Sungai Buloh, Malaysia
The prevalence of childhood obesity in Malaysia has doubled in less than a decade. Moreover, being overweight and obese have been associated with immediate and later comorbidities, thus emphasizing the need to prevent obesity from an early age. This cross-sectional study involved 923 multi-ethnic Malaysian adolescents aged between 15 and 17 years old. Body composition was estimated using bioelectrical impedance analysis. Body mass index (BMI) classification was based on the World Health Organization (WHO) growth reference and the International Obesity Task Force (IOTF) cut-off. Meanwhile, the Child Growth Foundation (CGF) body fat reference was used to classify adolescents’ adiposity. Lifestyle indices including physical activity, sedentary behavior, supplement intake, smoking and alcohol status were assessed via questionnaires. A high prevalence of overweight/obesity among the adolescents was observed according to the CGF (26%), followed by that of the WHO (24%) and then the IOTF (23%) cut-off, with high concordance values between each pair. After adjustment, a significant association was found between physical activity (PAQ score) and lean mass (p = 0.027). No lifestyle determinant was found to be a significant predictor of fat percentage. A high sedentary level increased the likelihood of obesity (OR 3.0, p < 0.01), while antioxidant-rich supplements were found to protect against obesity (OR 0.4, p < 0.05). The lifestyle predictors identified in this study may be considered when designing interventions that integrate lifestyle modifications targeting adolescents.
Introduction
Obesity refers to excessive fat accumulation that might threaten a person's health (1). The rate of obesity has doubled in more than 70 countries since 1980 and has increased continuously to reach pandemic levels (2). In 2016, over 650 million adults and 124 million children and adolescents aged 5–19 (6% of girls and 8% of boys) were obese (3). In just four decades, childhood obesity has surpassed adult obesity tenfold (2). Many low- and middle-income countries (LMICs) are now facing the dual-burden of malnutrition, since obesity and overweight rates are rising parallel to the existing burden of undernutrition (4). Included in the affected countries is Malaysia, where the prevalence of overweight and obesity has risen exponentially, with half of the population (50.1%) being classified as overweight and obese in 2019 (5). Alarmingly, the obesity prevalence among Malaysian children under 18 has doubled in less than a decade (6, 7), hitting a record high of 14.8% in 2019 (5).
For many countries, the steep upsurge in obesity has been attributed to rapid nutritional transition (8). The fundamental cause of obesity is a long-term energy imbalance between the calories consumed (increased energy intake) and calories expended (reduced energy expenditure) (9, 10). The overconsumption of calorie-dense food and beverages, accompanied by physical inactivity and sedentary lifestyle preferences that lead to obesogenic environments, plays a pivotal role in the prevalence of obesity (11). Hence positive lifestyle changes are likely to be major factors in the prevention of obesity.
Obesity trends in children and adolescents are of particular concern for the predictions of how the burden of obesity might soon affect the population (9). Overweight and obese children/adolescents are more likely to become obese adults (12) and are highly associated with the risk of developing other non-communicable diseases (NCDs) such as cardiovascular disease, type 2 diabetes, and dyslipidemia, which eventually contribute to mortality and premature death (9, 8, 11, 13). Obesity is the fifth leading cause of global mortality (14), of which over 80% of premature deaths before the age of 70 occur in LMICs (15). Accordingly, obesity is now classified as a chronic progressive disease, distinct from being a risk factor for other diseases (16). In that regard, the prevention of childhood obesity is one of the key strategies for early intervention for NCDs.
Several local studies have been conducted to examine the lifestyle predictors of obesity risk among school-going adolescents living in certain states of Malaysia. Lifestyle determinants including low physical activity and smoking status have been associated with greater odds of obesity (17, l8). In an earlier study, lower physical activity and amount of moderate to vigorous physical activity (MVPA) in males, and high sedentary behavior (measured as screen time) in females have been linked with higher odds of obesity in adolescents (19). The available findings, mainly conducted among adolescents in the sub-urban regions of Malaysia, are relatively insufficient and warrant further studies. In recent years, concerns have arisen about the changes in adolescents’ physical activity following the COVID-19 pandemic (20, 21). Thus, it is crucial to revisit the classical (physical activity) and emerging lifestyle predictors, such as sedentary behavior. This study aims to evaluate the lifestyle indices associated with obesity risk and body composition (body fat and lean mass) among multi-ethnic adolescents in Malaysia and to compare the difference between international references when classifying adolescents' weight status. Monitoring childhood obesity and understanding the factors that contribute to this global epidemic may help public health efforts to formulate policies and implement culturally appropriate programs (22).
Materials and methods
Study design and sampling
This population-based, cross-sectional study was conducted among 15–17 years old Malaysian adolescents attending their fourth year (Form 4) of government secondary school education. A stratified random sampling technique was used to select six secondary schools [daily school-urban, daily school-rural, boarding, daily-vernacular, sports school, and Orang Asli (indigenous population) dominated school] to represent the national school system, locations, and heterogeneity of the population using computer-generated random number lists. The adolescents were recruited from three regions: the Federal Territory of Kuala Lumpur (metropolitan area), Selangor (central region), and Pahang (eastern region), based on discussions with the Ministry of Education (MOE) of Malaysia (23, 24). All the fourth-year students in the selected secondary schools were eligible to participate and be included in the current study if they were healthy and had no chronic disease that could prevent them from being physically active. The subjects were informed of the study and their participation was voluntary. Written informed consent was obtained from the participants and their legal guardians before the inception of this study. In summary, of the 1,078 adolescents invited, 960 adolescents returned with a signed consent form and had a complete data set, while 37 were excluded because 22 adolescents were not in the age range and 15 were non-Malaysians/non-residents of Peninsular Malaysia. Hence, 923 adolescents were included in the final analysis.
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Ethics Committee of the University Kebangsaan Malaysia Medical Center (UKMMC) (UKM 1.5.3.5/244/FF-2014). Formal approvals were also obtained from the Ministry of Education (MOE), the Department of State Education (JPN), the Department of Orang Asli Development (JAKOA), and the school authorities.
Anthropometric and body composition
The heights and weights of the participants were measured in triplicate by the same trained personnel in each respective school. Height was measured using a portable Stadiometer to the nearest 0.1 cm (Seca 213, Germany). Body weight was measured in light clothing to the nearest 0.1 kg using a segmental body composition analyzer BC-420 MA (Tanita Corporation, Japan). Age- and gender-specific BMI-z scores were calculated based on the least mean square method (LMS) (25, 26). Body fat percentage (BF%) and lean mass were estimated using the same body composition analyzer, which integrates a validated bio-impedance analysis method developed for an age range of 5–99 years old (27). The individual measurements were automatically converted to z-scores using the formula incorporated in the instrument (27). Three international cut-offs were applied to classify the weight status. The BMI classification was based on the World Health Organization (WHO) growth reference (25) and the updated International Obesity Task Force (IOTF) cut-off (26). The body fat reference established for segmental BIA by the Child Growth Foundation (CGF) was used to classify the adolescents' adiposity (28). The following cut-offs are used to define obesity, according to each reference: the z-score ≥+2 standard deviations by the WHO (25); the percentile curve passing through the BMI = 30 kg/m2 at age 18 by the IOTF (26), and the BF% ≥ 95th percentile by the CGF (28).
Physical activity and sedentary behavior
Self-reported physical activity and sedentary behavior were assessed using a validated Malay version of the physical activity questionnaire for older children (PAQ-C), known as PAQ-C (M) (29). The questionnaire was adapted (30), modified, and validated among the 10–17 years old Malaysian students, with an acceptable validity of Spearman's correlation coefficient r = 0.6 (29). The subjects were required to complete questions related to their activities during leisure time, physical education (PE) classes, recess, lunchtime, after school, evenings, and weekends. They were also asked to provide a self-perception of their physical activity over the course of the seven days, with the final item asking the frequency with which they had participated in daily physical activity in the previous week. A five-point Likert scale ranging from low (score = 1) to high (score = 5) was used for each item. The physical activity score (PAQ score) is the average total score from these nine questions. A higher score indicates a greater physical activity level. Based on the PAQ score, each subject was categorized as having either low (PAQ score ranging from 1.00–2.33), moderate (PAQ score 2.34–3.66), or high (PAQ score 3.67–5.00) physical activity levels (31). For the current analysis, those with moderate or high physical activity levels were regarded as active, while adolescents with low physical activity were deemed inactive.
Regarding sedentary behavior, the adolescents were asked to report their daily sedentary activities (sitting or lying down) over the previous week, which included the number of hours usually spent per day during school days and on the weekend watching television, playing video games, surfing the internet/using the computer, doing homework/revision, attending extra classes (not within regular school hours), reading, and sitting while playing. Then, the average duration of total sedentary time was calculated for every subject. Due to the insufficient evidence available to specify time limits on sitting in children and adolescents, the recommended sitting time of not more than eight hours per day for adults was applied to classify the duration of sedentary behavior (32).
Other lifestyle variables
The intake of specific types of dietary supplements—including fatty acids, growth/protein formula, and antioxidant-rich supplements—was extracted using a dietary supplement questionnaire (DiSQ) with a substantial kappa correlation coefficient (k = 0.62) (33). In brief, the questionnaire inquires about the consumption of vitamins/minerals and nutraceutical or natural products over the past year (using yes/no questions). The adolescents were then required to provide the product names. Sociodemographic information such as gender, date of birth, ethnic group, and type of school, as well as smoking and alcohol intake status, was obtained via the same questionnaire. Regarding antioxidant supplements, those known to have antioxidant properties are vitamin C, vitamin E, multi-vitamin, B-carotene, selenium, zinc, phenols, ubiquinone/co-enzyme Q10, and Ginkgo Biloba (34, 35). For the current analysis, the adolescents were identified as either occasional drinkers (defined as drinking at most once a month) or non-drinkers (defined as never, or tried once or twice). Meanwhile, smoking status was categorized as either regular smokers (at least one puff a day) or non-smokers (tried once, sometimes, or never) (23).
Statistical analysis
At the initial stage, all the variables were tested for non-normality based on histograms and skewness values larger than two or an absolute kurtosis larger than seven (36). Continuous variables were presented using means and confidence intervals (CI), while categorical variables were presented using frequency statistics (the count and percentage). Gender-specific analysis was performed to assess the differences between the sexes. Analysis of covariance (ANCOVA) was conducted after taking into account age as a potential confounding factor. Meanwhile, an independent t-test was applied for age. Differences in proportions (percentages) were carried out using the χ2 test.
The strength of agreement/degree of concordance between each pair of cut-offs was calculated using the kappa (k) coefficient. Cohen's k coefficient values of less than 0.20 are described as poor agreement, values of 0.21–0.40 as fair agreement, values of 0.41–0.60 as moderate agreement, values of 0.61–0.80 as substantial agreement, and values of 0.81–1.00 as almost perfect agreement (37).
A multivariate linear regression model was generated to determine the best combination of lifestyle predictors for body fat percentage and lean mass, while a multivariate logistic regression model was created to determine the risk of obesity after controlling for confounding factors. Potential confounders were predetermined via the univariate analysis. Only significant variables in the univariate analysis were entered into the multivariate model. The variance inflation factor (VIF) was calculated for each regression model and detected no severe multicollinearity issues (>10) that warranted corrective measures.
Statistical analyses were performed using the SPSS for Windows version 24.0 (IBM Corp. Armonk, NY). A p-value of <0.05 is considered significant.
Results
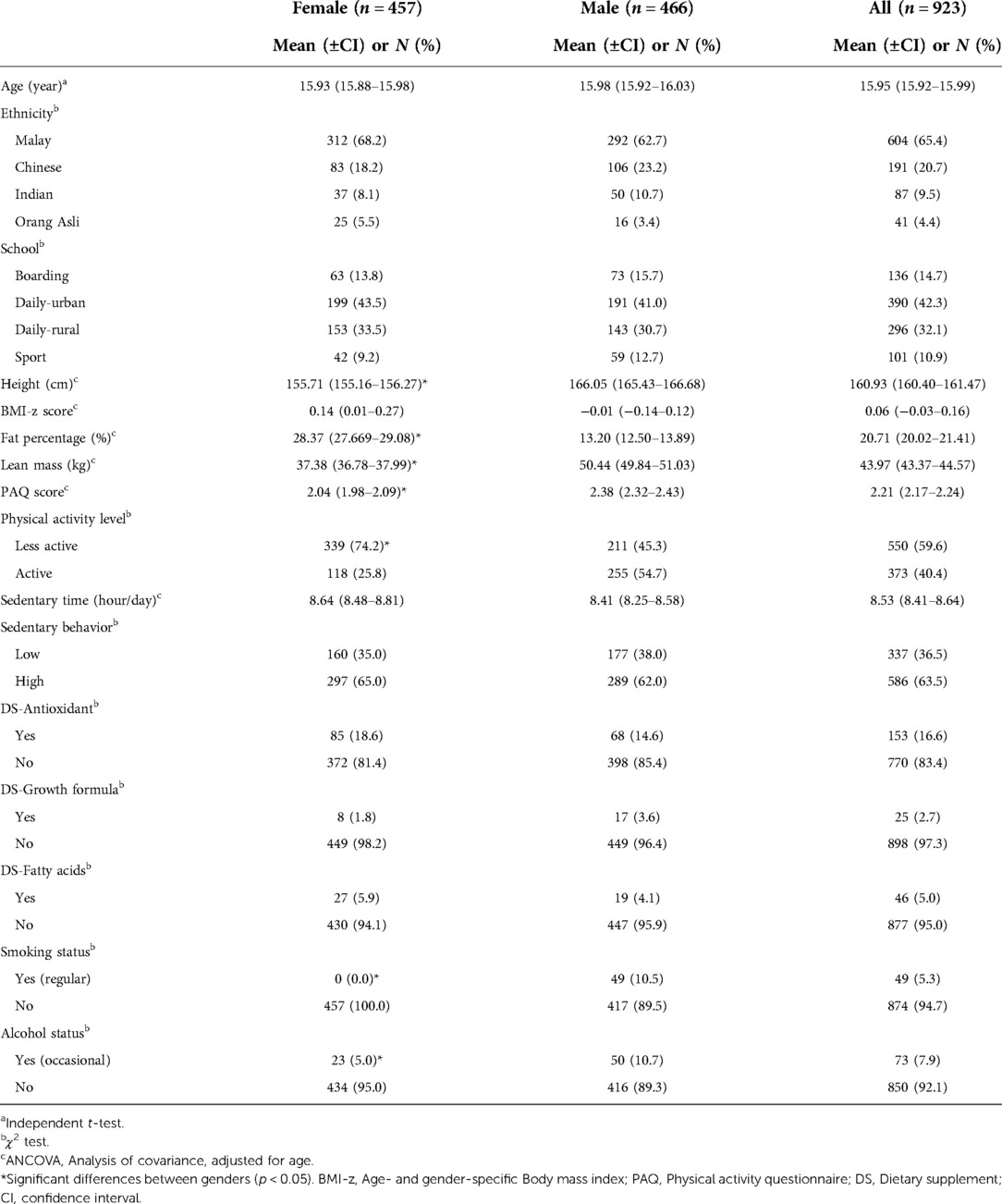
Table 1 shows the distribution of the subjects by gender and overall (n = 923). A total of 49.5% (457) participants were female adolescents, while 50.5% (466) were males. The overall composition was 65.4% Malays, 20.6% Chinese, 9.5% Indians, and 4.4% Orang Asli of the Semai tribe (the most prominent tribal group in Peninsular Malaysia). More than half of the sample population reported low levels of physical activity (60%), with 64% being identified as sedentary. In regard to gender, male and female adolescents did not differ by ethnicity, school type, sedentary level, or any type of dietary supplement intake. Female adolescents were less active than males (p < 0.05). Male adolescents reported higher proportions of smoking and alcohol consumption compared to female adolescents (p < 0.05). Male adolescents had higher mean lean mass and PAQ scores (p < 0.005), while female adolescents had a higher mean fat percentage than male adolescents (p < 0.05). There were no significant differences between the genders regarding the mean age, BMI-z scores, and sedentary time.
Table 2 displays the prevalence of nutritional status based on the three international references. The prevalence of overweight/obese was 24.3% for the WHO, 22.5% for the IOTF, and 26.3% for the CGF. Meanwhile, the prevalence of normal weight was 69.6% for the WHO, 61.8% for the IOTF, and 51.9% for the CGF. No statistical differences were identified between the genders except for the CGF classification, where male adolescents had a greater prevalence of underfat (41%) than females (2%) (p < 0.05).
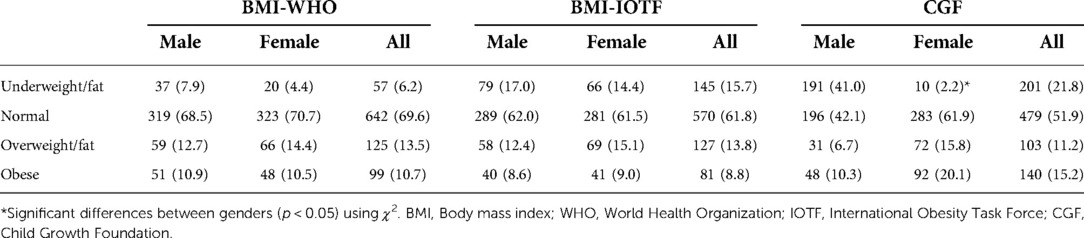
Table 2. Prevalence of nutritional status [N (%)] based on the three international references (n = 923).
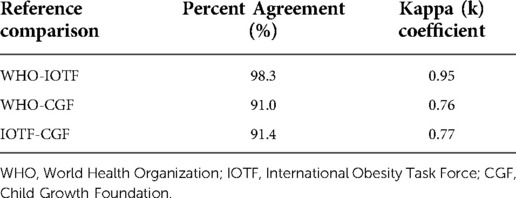
Table 3 exhibits a comparison of the overweight/obese prevalence between the three international references. The agreement between WHO-IOTF was very good (k = 0.95), while the agreement between WHO-CGF (k = 0.76) and IOTF-CGF (k = 0.77) was good. A good to very good agreement between the three references allowed any subsequent analysis to employ only one reference.
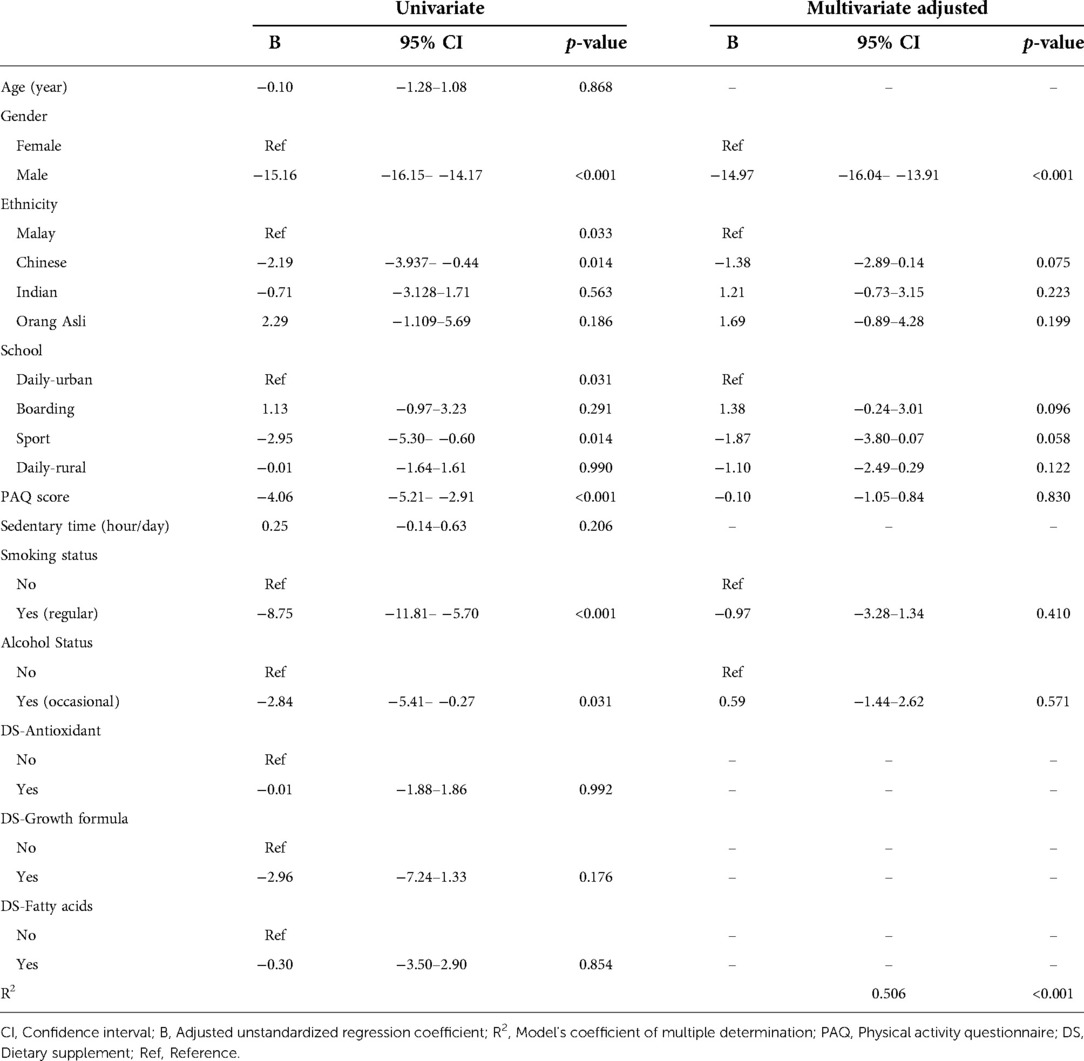
Table 4 demonstrates the univariate and multivariate linear regression models for body fat percentage. After adjusting for significant confounders (gender, race, and school type), no lifestyle determinant was found to be a significant predictor of fat percentage (R2 = 0.506, p < 0.001).
Table 5 shows the univariate and multivariate linear regression models for lean mass. After adjusting for selected demographic factors (gender, race, and school type), only one lifestyle indices, namely the physical activity scores, was found to be significant as a positive predictor of lean mass (p = 0.027). This model accounted for 53% of the variation in the adolescent lean mass (R2 = 0.531, p < 0.001).
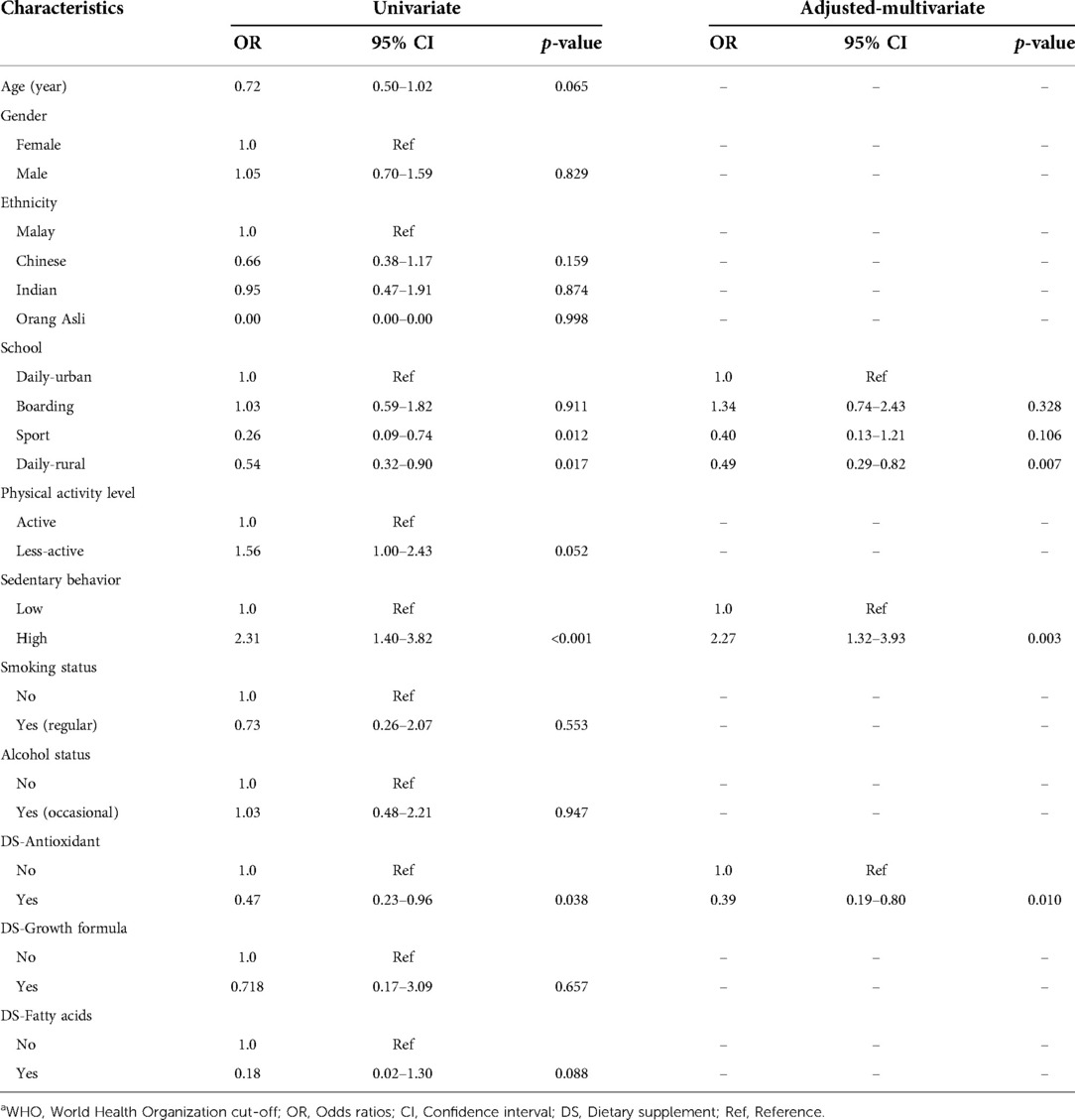
Table 6 displays the univariate and multivariate logistic regression models for obesity risk. After adjusting for a significant demographic confounder (school type), adolescents who sat for more than eight hours a day had obesity odds 2.3 times higher than those who sat for less than eight hours a day (p = 0.003), while adolescents who took antioxidant-type supplements had obesity odds 0.4 times lower than their non-intake counterparts (p = 0.010).
Discussion
The present study estimated a high prevalence of overweight and obesity in adolescents aged 15–17. The prevalence of obesity in a national study among children and adolescents under 18 (15%) was slightly higher than that reported in this study (11%), probably due to the wider age range (5, 38).
Notably, a higher prevalence of overweight/obesity was discovered with the CGF cut-off (26%), followed by those of the WHO (24%) and IOTF (23%). A previous comparison study also found important differences between the cut-off points for BMI and body fat. The prevalence of overweight/obesity in children and adolescents aged 7–19 from Southern Europe (Italy and Spain) was 32.3% according to IOTF, 37.3% according to the WHO, and 39.8% according to the CGF references (39). The discrepancies suggest the importance of specifying the method and reference cut-off points used to classify a sample until a consensus is reached. Despite the differences, the concordance values between each pair were high. Currently, there is no recommended/standard cut-off for the evaluation of overweight or obesity. Therefore, the high concordance values allowed for the application of any cut-off.
Concerning the risk of obesity, the results from the multivariate analysis revealed elevated odds of obesity when sedentary levels were high. Sitting for more than eight hours per day increased the odds of obesity by 2.3 times. The findings of the current study corroborated those reported among adolescents in France (40), the USA (41), Southeast Asia (42, 43), and Lebanon (44, 45). Other studies also demonstrated a link between long screen time and obesity (44, 46). However, several studies have also reported no significant association between obesity and sedentary behavior/ long screen-time in adolescents (47–49). The reason for this contradictory result is still not entirely apparent but could be partly attributed to methodological differences. Sedentary behavior involves very low energy expenditure and severely limits the number of calories burnt. Prolonged sitting could suppress lipoprotein lipase (a protein important for controlling plasma triglyceride catabolism, HDL cholesterol, and other metabolic risk factors) activity due to the loss of contractile stimulation of weight-bearing muscle, which could contribute to the development of obesity in the long term (50, 51). Whether exercise can reverse the detrimental effects of prolonged sitting requires more high-quality control trial studies. However, the current recommendation is to interrupt long hours of sitting with light movements (52).
The protective role of physical activity against obesity may not be consistent among adolescents. Interestingly, the analysis of the components of body composition revealed that physical activity contributes significantly to an increase in lean mass. Muscle growth or muscle hypertrophy is linked to a physiological process known as muscle protein synthesis, in which protein is produced to repair the muscle damage caused by intense exercise (53). This recovery process occurs after exercise, when the body is at rest. Muscle hypertrophy occurs whenever the rate of muscle protein synthesis is greater than the rate of muscle protein breakdown (54). Thus, the impact of exercise when repeated over time eventually contributes to muscle hypertrophy (53, 54).
When comparing weight-loss intervention programs, which are widely accepted methods for dealing with obesity, physical activity interventions alone appear to be less effective than combined intervention programs that include a caloric-restriction/hypocaloric (diet) and exercise (either resistance or endurance) (55). Although diet-only interventions and combined intervention programs produced similarly increased weight loss (55–57), diet-induced weight loss alone may significantly decrease muscle mass (58, 59). On the other hand, diet and physical activity combined programs were found to be not only effective in reducing fat mass but also able to attenuate muscle loss (56–58). Moreover, physical activity, particularly resistance exercise, not only protects muscle tissue during weight loss but may also increase muscle strength (56, 59, 60). This information is important since compared to a normal-weight person, those who are obese have higher muscle mass but lower muscle quality. Maximum muscle hypertrophy can be achieved through a combination of physical activities (such as resistance training) and hyperaminoacidemia from protein intake (54). However, protein intake alone cannot increase muscle strength. Accordingly, participation in physical activity (or in conjunction with protein intake) is more advisable than simply taking protein supplements to increase muscle mass.
Of the three supplement categories explored, antioxidant supplements were found to protect against obesity. Research indicates that low circulatory concentrations of antioxidants in the blood are linked with increased body fat and BMI in children (61). Meanwhile, others have highlighted that overweight and obese individuals have lower concentrations of antioxidants in their blood than children and adolescents of normal weight (62–64). Excess body fat may enhance oxidative stress, which depletes endogenous and exogenous antioxidants via the increased indirect utilization of antioxidants, while the free radicals generated may play a major role in the etiology and development of obesity-related comorbidities. However, the proposed mechanism should consider the limitations of the existing studies (65). Based on the assumption that individuals with excess body fat have high oxidative stress, overweight/fat and obese individuals with low antioxidant levels in the body to act as direct antioxidants are advised to consume more antioxidants (as food, or supplements intake, or a combination of these) to attain the same serum-plasma levels as a normal-weight person (66). These observational studies in children demonstrate that antioxidants may have an impact on obesity, but causality can only be ascertained with clinical trials.
Several limitations of the present study should be acknowledged. Firstly, dietary patterns were not investigated. Other local studies have reported that a dietary pattern mainly characterized by high sugar and fat among adolescents was not associated with obesity (67, 68). The present study found no definitive association between physical activity and obesity. Similar findings have been reported by other studies (40, 41, 43, 44, 46, 47, 49). Meanwhile, some studies have noted a significant association between physical activity and obesity (17, 18, 19, 45, 48, 69). These discrepancies could be related to recall bias from self-reporting methods (although validated), hence the use of an objective measure is recommended, although this is impractical for large-scale epidemiological studies. Moreover, the PAQ-C is limited to measuring the level of physical activity and cannot discriminate between types of physical activity (e.g., endurance vs. resistance exercise). Additionally, no causal inferences could be made as the data were drawn from a cross-sectional study. Longitudinal studies are warranted to confirm any actual links. Despite these limitations, the present study not only represents multi-ethnic adolescents in Malaysia but also, most importantly, assessed the odds of being obese and other body composition parameters, including lean mass and fat percentage, which had not been reported previously. In the wake of the new norms, Malaysia is at high risk of widespread inactivity and an obesity pandemic. Moreover, many experts contend that early healthy lifestyle practices tend to be translated into adulthood and indirectly reduce the burden of disease throughout life (70, 71). Considering that, the current findings indicate that urgent action is needed, with extensive focus on strategies that can help adolescents to create and follow healthy lifestyles.
Conclusion
The current study demonstrated a high prevalence of overweight and obesity among Malaysian adolescents aged 15–17. Although the prevalence of obesity differs based on the reference method employed, the degree of concordance between each pair was high. Excessive sedentary behavior was found to increase the odds of obesity, while antioxidant-rich supplements were found to protect against obesity. A high lean mass was positively associated with physical activity (PAQ score), while no lifestyle determinant was found to be a significant predictor of fat percentage. The lifestyle predictors identified in this study could be considered when designing interventions that integrate lifestyle modifications targeting adolescents.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving human participants were reviewed and approved by Institutional Ethics Committee of University Kebangsaan Malaysia Medical Center (UKMMC) (UKM 1.5.3.5/244/FF-2014). Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
Methodology, MSZ, RS and IN-M; validation, IN-M, RS and ANS; formal analysis, MSZ and IN-M; investigation, MSZ, RS, ANS and IN-M; data curation, MSZ and IN-M; writing—original draft preparation, MSZ; writing—review and editing, RS and IN-M; supervision, IN-M, RS, SAM and ANS; project administration, IN-M; funding acquisition, IN-M, SAM and ANS. All authors contributed to the article and approved the submitted version.
Funding
This research was financially supported by a university grant, Dana Impak Perdana (Premier Impact Grant) grant number DIP-2013-002.
Acknowledgments
The authors wish to express their gratitude to the participants and teachers from the participating schools; Nurul Huda Razalli from the Dietetics Program, Faculty of Health Sciences, UKM; and Tg Mohd Ikhwan Tg Abu Bakar Sidik from the Faculty of Medicine, UKM for statistical support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Prospective Studies Collaboration. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. (2009) 373:1083–96. doi: 10.1016/S0140-6736(09)60318-4
2. The GBD 2015 Obesity Collaborators, Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. (2017) 377:13–27. doi: 10.1056/NEJMoa1614362
3. World Health Organization. Obesity and overweight. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (Accessed September 8, 2020).
4. Tzioumis E, Adair LS. Childhood dual burden of under- and overnutrition in low- and middle-income countries: a critical review. Food Nutr Bull. (2014) 35:230–43. doi: 10.1177/156482651403500210
5. Institute for Public Health (IPH). National Health and Morbidity Survey (NHMS) 2019 (2019): Vol. I: NCDs—Non-Communicable Diseases: risk factors and other health problems.
6. Institute for Public Health (IPH). National health and morbidity survey 2011 (NHMS 2011) (2011). Vol. 2: non-communicable diseases.
7. Institute for Public Health (IPH). National health and morbidity survey 2015 (NHMS 2015) (2015). Vol. II: non-communicable diseases, risk factors & other health problems.
8. Heymsfield SB, Wadden TA. Mechanisms, pathophysiology, and management of obesity. N Engl J M. (2017) 376:254–66. doi: 10.1056/NEJMra1514009
9. Blüher M. Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol. (2019) 15:288–98. doi: 10.1038/s41574-019-0176-8
10. Gadde KM, Martin CK, Berthoud HR, Heymsfield SB. Obesity: pathophysiology and management. J Am Coll Cardiol. (2018) 71:69–84. doi: 10.1016/j.jacc.2017.11.011
11. Di Cesare M, Sorić M, Bovet P, Miranda JJ, Bhutta Z, Stevens GA, et al. The epidemiological burden of obesity in childhood: a worldwide epidemic requiring urgent action. BMC Med. (2019) 17:212. doi: 10.1186/s12916-019-1449-8
12. Guo SS, Wu W, Chumlea WC, Roche AF. Predicting overweight and obesity in adulthood from body mass index values in childhood and adolescence. Am J Clin Nutr. (2002) 76:653–8. doi: 10.1093/ajcn/76.3.653
13. Umer A, Kelley GA, Cottrell LE, Giacobbi P Jr, Innes KE, Lilly CL. Childhood obesity and adult cardiovascular disease risk factors: a systematic review with meta-analysis. BMC Public Health. (2017) 17:683. doi: 10.1186/s12889-017-4691-z
14. World Health Organization. Global health risks: Mortality and burden of disease attributable to selected major risks. Geneva: World Health Organization (2009).
15. World Health Organization. Global status report on noncommunicable diseases 2014. Geneva: World Health Organization (2014).
16. Bray GA, Kim KK, Wilding JPH, World Obesity Federation. Obesity: a chronic relapsing progressive disease process. A position statement of the World Obesity Federation. Obes Rev. (2017) 18:715–23. doi: 10.1111/obr.12551
17. Alagappan M, Rampal L, Zalilah MS. Prevalence of overweight/obesity and its associated factors among secondary school students in semi urban area in Malaysia. Med J Malaysia. (2019) 74:513–20.31929478
18. Lai WK, Mohd Sidik S, Lekhraj R, Gan WY, Ismail SIF. Prevalence and predictors of overweight and obesity among adolescents in Seremban, Negeri Sembilan, Malaysia. Cureus. (2022) 14(1):e21795. doi: 10.7759/cureus.21795
19. Teo PS, Nurul-Fadhilah A, Aziz ME, Hills AP, Foo LH. Lifestyle practices and obesity in Malaysian adolescents. Int J Environ Res Public Health. (2014) 11:5828–38. doi: 10.3390/ijerph110605828
20. Ruíz-Roso MB, de Carvalho Padilha P, Matilla-Escalante DC, Brun P, Ulloa N, Acevedo-Correa D, et al. Changes of physical activity and ultra-processed food consumption in adolescents from different countries during COVID-19 pandemic: an observational study. Nutrients. (2020) 12:2289. doi: 10.3390/nu12082289
21. Dunton GF, Do B, Wang SD. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U.S. BMC Public Health. (2020) 20:1351. doi: 10.1186/s12889-020-09429-3
22. Poskitt EM. Childhood obesity in low- and middle-income countries. Paediatr Int Child Health. (2014) 34:239–49. doi: 10.1179/2046905514Y.0000000147
23. Zulfarina MS, Sharif R, Syarifah-Noratiqah SB, Sharkawi AM, Aqilah-Sm ZS, Mokhtar SA, et al. Modifiable factors associated with bone health in Malaysian adolescents utilising calcaneus quantitative ultrasound. PLoS One. (2018) 13:e0202321. doi: 10.1371/journal.pone.0202321
24. Zulfarina MS, Sharif R, Sharkawi AM, Mokhtar SA, Shuid AN, Naina-Mohamed I. Quality of energy intake in Malaysian adolescents: prevalence, characteristics, determinants and impact of implausible reporters. Public Health Nutr. (2022):1–23. doi: 10.1017/S1368980022000726. [Epub ahead of print]35321764
25. de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. (2007) 85:660–7. doi: 10.2471/blt.07.043497
26. Cole TJ, Lobstein T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes. (2012) 7:284–94. doi: 10.1111/j.2047-6310.2012.00064.x
27. Merritt S, Ballinger D. Reliability and feasibility of Tanita body composition scale in high school physical education and health classes. Res. Q. Exerc. Sport. (2003) 74:A26.
28. McCarthy HD, Cole TJ, Fry T, Jebb SA, Prentice AM. Body fat reference curves for children. Int J Obes (Lond). (2006) 30:598–602. doi: 10.1038/sj.ijo.0803232
29. Zaki NAM, Sahril N, Omar MA, Ahmad MH, Baharudin A, Mohd Nor NS. Reliability and validity of the physical activity questionnaire for older children (PAQ-C) in malay language. Int J Public Health Res. (2016) 6:670–6.
30. Kowalski KC, Crocker PR, Donen RM. The physical activity questionnaire for older children (PAQ-C) and adolescents (PAQ-A) manual. Saskatoon, Canada: College of Kinesiology, University of Saskatchewan (2004). p. 1–38.
31. Crocker PR, Bailey DA, Faulkner RA, Kowalski KC, McGrath R. Measuring general levels of physical activity: preliminary evidence for the Physical Activity Questionnaire for Older Children. Med Sci Sports Exerc. (1997) 29:1344–9. doi: 10.1097/00005768-199710000-00011
32. van der Ploeg HP, Chey T, Korda RJ, Banks E, Bauman A. Sitting time and all-cause mortality risk in 222 497 Australian adults. Arch Intern Med. (2012) 172:494–500. doi: 10.1001/archinternmed.2011.2174
33. Zulfarina MS, Sharif R, Sharkawi AM, Tg Abu Bakar Sidik TMI, Mokhtar SA, Shuid AN, et al. Reliability of self-administered questionnaire on dietary supplement consumption in Malaysian adolescents. Nutrients. (2020) 12:2853. doi: 10.3390/nu12092853
34. Manzanares W, Dhaliwal R, Jiang X, Murch L, Heyland DK. Antioxidant micronutrients in the critically ill: a systematic review and meta-analysis. Crit Care. (2012) 16:R66. doi: 10.1186/cc11316
35. Evans JR, Lawrenson JG. Antioxidant vitamin and mineral supplements for preventing age-related macular degeneration. Cochrane Database Syst Rev. (2017) 7:CD000253. doi: 10.1002/14651858.CD000253.pub4
36. Kim HY. Statistical notes for clinical researchers: assessing Normal distribution (2) using skewness and kurtosis. Restor Dent Endod. (2013) 38:52–4. doi: 10.5395/rde.2013.38.1.52
37. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. (1977) 33:159–74. doi: 10.2307/2529310
38. Institute for Public Health (IPH). National health and morbidity survey (NHMS) 2017. Kuala Lumpur: Adolescent Nutrition Survey (2017).
39. López-Sánchez GF, Sgroi M, D'Ottavio S, Díaz-Suárez A, González-Víllora S, Veronese N, et al. Body composition in children and adolescents residing in Southern Europe: prevalence of overweight and obesity according to different international references. Front Physiol. (2019) 10:130. doi: 10.3389/fphys.2019.00130
40. Thibault H, Contrand B, Saubusse E, Baine M, Maurice-Tison S. Risk factors for overweight and obesity in French adolescents: physical activity, sedentary behavior and parental characteristics. Nutrition. (2010) 26:192–200. doi: 10.1016/j.nut.2009.03.015
41. Liu JH, Jones SJ, Sun H, Probst JC, Merchant AT, Cavicchia P. Diet, physical activity, and sedentary behaviors as risk factors for childhood obesity: an urban and rural comparison. Child Obes. (2012) 8:440–8. doi: 10.1089/chi.2012.0090
42. Pengpid S, Peltzer K. Overweight, obesity and associated factors among 13–15 years old students in the association of Southeast Asian nations member countries, 2007–2014. Southeast Asian J Trop Med Public Health. (2016) 47:250–62.27244964
43. Pengpid S, Peltzer K. Underweight and overweight or obesity and associated factors among school-going adolescents in five ASEAN countries, 2015. Diabetes Metab Syndr. (2019) 13:3075–80. doi: 10.1016/j.dsx.2019.11.002
44. Nasreddine L, Naja F, Akl C, Chamieh MC, Karam S, Sibai AM, et al. Dietary, lifestyle and socio-economic correlates of overweight, obesity and central adiposity in Lebanese children and adolescents. Nutrients. (2014) 6:1038–62. doi: 10.3390/nu6031038
45. El-Kassas G, Ziade F. Exploration of the risk factors of generalized and central obesity among adolescents in North Lebanon. J Environ Public Health. (2017) 2017:2879075. doi: 10.1155/2017/2879075
46. Musaiger AO, Al-Roomi K, Bader Z. Social, dietary and lifestyle factors associated with obesity among Bahraini adolescents. Appetite. (2014) 73:197–204. doi: 10.1016/j.appet.2013.11.002
47. Duncan S, Duncan EK, Fernandes RA, Buonani C, Bastos KD, Segatto AF, et al. Modifiable risk factors for overweight and obesity in children and adolescents from São Paulo, Brazil. BMC Public Health. (2011) 11:585. doi: 10.1186/1471-2458-11-585
48. Al-Hazzaa HM, Abahussain NA, Al-Sobayel HI, Qahwaji DM, Musaiger AO. Lifestyle factors associated with overweight and obesity among Saudi adolescents. BMC Public Health. (2012) 12:354. doi: 10.1186/1471-2458-12-354
49. Kerkadi A, Sadig AH, Bawadi H, Al Thani AAM, Al Chetachi W, Akram H, et al. The relationship between lifestyle factors and obesity indices among adolescents in Qatar. Int J Environ Res Public Health. (2019) 16:4428. doi: 10.3390/ijerph16224428
50. Hamilton MT, Etienne J, McClure WC, Pavey BS, Holloway AK. Role of local contractile activity and muscle fiber type on LPL regulation during exercise. Am J Physiol. (1998) 275:E1016–22. doi: 10.1152/ajpendo.1998.275.6.E1016
51. Hamilton MT, Hamilton DG, Zderic TW. Exercise physiology versus inactivity physiology: an essential concept for understanding lipoprotein lipase regulation. Exerc Sport Sci Rev. (2004) 32:161–6. doi: 10.1097/00003677-200410000-00007
52. Loh R, Stamatakis E, Folkerts D, Allgrove JE, Moir HJ. Effects of interrupting prolonged sitting with physical activity breaks on blood glucose, insulin and triacylglycerol measures: a systematic review and meta-analysis. Sports Med. (2020) 50:295–330. doi: 10.1007/s40279-019-01183-w
53. Witard OC, Wardle SL, Macnaughton LS, Hodgson AB, Tipton KD. Protein considerations for optimising skeletal muscle mass in healthy young and older adults. Nutrients. (2016) 8:181. doi: 10.3390/nu8040181
54. Stokes T, Hector AJ, Morton RW, McGlory C, Phillips SM. Recent perspectives regarding the role of dietary protein for the promotion of muscle hypertrophy with resistance exercise training. Nutrients. (2018) 10:180. doi: 10.3390/nu10020180
55. Johns DJ, Hartmann-Boyce J, Jebb SA, Aveyard P, Behavioural Weight Management Review Group. Diet or exercise interventions vs combined behavioral weight management programs: a systematic review and meta-analysis of direct comparisons. J Acad Nutr Diet. (2014) 114:1557–68. doi: 10.1016/j.jand.2014.07.005
56. Said MA, Abdelmoneem M, Almaqhawi A, Hamid Kotob AA, Alibrahim MC, Bougmiza I. Multidisciplinary approach to obesity: aerobic or resistance physical exercise? J Exerc Sci Fit. (2018) 16:118–23. doi: 10.1016/j.jesf.2018.11.001
57. Said MA, Abdelmoneem M, Alibrahim MC, Elsebee MA, Kotb AAH. Effects of diet versus diet plus aerobic and resistance exercise on metabolic syndrome in obese young men. J Exerc Sci Fit. (2020) 18:101–8. doi: 10.1016/j.jesf.2020.03.002
58. Chomentowski P, Dubé JJ, Amati F, Stefanovic-Racic M, Zhu S, Toledo FG, et al. Moderate exercise attenuates the loss of skeletal muscle mass that occurs with intentional caloric restriction-induced weight loss in older, overweight to obese adults. J Gerontol A Biol Sci Med Sci. (2009) 64:575–80. doi: 10.1093/gerona/glp007
59. Cava E, Yeat NC, Mittendorfer B. Preserving healthy muscle during weight loss. Adv Nutr. (2017) 8:511–9. doi: 10.3945/an.116.014506
60. Said MA, Abdelmoneim MA, Alibrahim MS, Kotb AAH. Aerobic training, resistance training, or their combination as a means to fight against excess weight and metabolic syndrome in obese students—which is the most effective modality? A randomized controlled trial. Appl Physiol Nutr Metab. (2021) 46:952–63. doi: 10.1139/apnm-2020-0972
61. de Souza Valente da Silva L, Valeria da Veiga G, Ramalho RA. Association of serum concentrations of retinol and carotenoids with overweight in children and adolescents. Nutrition. (2007) 23:392–7. doi: 10.1016/j.nut.2007.02.009
62. Sarni RO, Suano de Souza FI, Ramalho RA, Schoeps Dde O, Kochi C, Catherino P, et al. Serum retinol and total carotene concentrations in obese pre-school children. Med Sci Monit. (2005) 11:CR510–4.16258394
63. Marreiro DN, Fisberg M, Cozzolino SM. Zinc nutritional status and its relationships with hyperinsulinemia in obese children and adolescents. Biol Trace Elem Res. (2004) 100:137–49. doi: 10.1385/bter:100:2:137
64. Strauss RS. Comparison of serum concentrations of alpha-tocopherol and beta-carotene in a cross-sectional sample of obese and nonobese children (NHANES III). National Health and Nutrition Examination Survey. J Pediatr. (1999) 134:160–5. doi: 10.1016/s0022-3476(99)70409-9
65. Hosseini B, Saedisomeolia A, Allman-Farinelli M. Association between antioxidant intake/status and obesity: a systematic review of observational studies. Biol Trace Elem Res. (2017) 175:287–97. doi: 10.1007/s12011-016-0785-1
66. Vioque J, Weinbrenner T, Asensio L, Castelló A, Young IS, Fletcher A. Plasma concentrations of carotenoids and vitamin C are better correlated with dietary intake in normal weight than overweight and obese elderly subjects. Br J Nutr. (2007) 97:977–86. doi: 10.1017/S0007114507659017
67. Emi NA, Gan WY, Mohd Shariff Z, Anuar Zaini A, Shamsuddin NH, Appukutty M, et al. Associations of an empirical dietary pattern with cardiometabolic risk factors in Malaysian adolescents. Nutr Metab (Lond). (2020) 17:1–10. doi: 10.1186/s12986-020-00447-x
68. Garba JA, Rampal L, Hejar AR, Salmiah MS. Major dietary patterns and their associations with socio-demographic characteristics and obesity among adolescents in petaling district, Malaysia. Malays J Med Heal Sci. (2014) 10:13–21.
69. Andegiorgish AK, Wang J, Zhang X, Liu X, Zhu H. Prevalence of overweight, obesity, and associated risk factors among school children and adolescents in Tianjin, China. Eur J Pediatr. (2012) 171:697–703. doi: 10.1007/s00431-011-1636-x
70. Viner RM, Ross D, Hardy R, Kuh D, Power C, Johnson A, et al. Life course epidemiology: recognising the importance of adolescence. J Epidemiol Community Health. (2015) 69:719–20. doi: 10.1136/jech-2014-205300
Keywords: obese, body fat, LEAN MASS, physical activity, sedentary behavior, antioxidants
Citation: Zulfarina MS, Sharif R, Mokhtar SA, Shuid AN and Naina-Mohamed I (2022) Lifestyle indices of body composition and obesity risk and prevalence among multi-ethnic adolescents in Malaysia. Front. Pediatr. 10:899014. doi: 10.3389/fped.2022.899014
Received: 17 August 2022; Accepted: 10 October 2022;
Published: 1 November 2022.
Edited by:
Giulio Maltoni, Sant'Orsola-Malpighi Polyclinic, ItalyReviewed by:
Valentina Chiavaroli, Pescara Public Hospital, ItalyMohamed Ahmed Said, King Faisal University, Saudi Arabia
© 2022 Zulfarina, Sharif, Mokhtar, Shuid and Naina-Mohamed. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Isa Naina-Mohamed aXNhbmFpbmFAcHB1a20udWttLmVkdS5teQ==
Specialty Section: This article was submitted to Pediatric Obesity, a section of the journal Frontiers in Pediatrics
 Mohamed S. Zulfarina
Mohamed S. Zulfarina Razinah Sharif
Razinah Sharif Sabarul Afian Mokhtar3
Sabarul Afian Mokhtar3 Ahmad Nazrun Shuid
Ahmad Nazrun Shuid