
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
PERSPECTIVE article
Front. Pediatr., 06 July 2022
Sec. Pediatric Pulmonology
Volume 10 - 2022 | https://doi.org/10.3389/fped.2022.891616
As wildfires increase in prevalence and intensity across California and globally, it is anticipated that more children will be exposed to wildfire smoke, and thus face associated adverse health outcomes. Here, we provide a concise summary of the respiratory effects of California's wildfires on pediatric healthcare utilization, examine global examples of wildfire smoke exposure within the pediatric population and associated physiological effects, and assess the efficacy of metrics used to measure and communicate air quality during wildfires within the United States and elsewhere.
Climate change has been increasing wildfire activity in California (1). In 2021 alone, wildfires burned across ~2.6 million acres in California, damaging over 3,000 structures and resulting in three fatalities (2). In addition to such impacts, wildfire smoke severely affects air quality by increasing the concentration of air pollutants. PM2.5, airborne particles with a diameter of ≤2.5 μm, are of particular concern since they are small enough to penetrate the deepest recesses of the lungs and enter the bloodstream, thus adversely affecting human health in the immediate surroundings and in areas downwind of wildfires (3). Currently, most studies on the adverse respiratory impact of wildfires focus on adults while fewer specifically consider impacts of wildfire smoke exposure on children's developing lungs (4).
Wildfire smoke is currently a major source of PM2.5 pollution in regions like the Western United States (5), and this source of pollution is projected to increase in the context of climate change and variability (6). Wildfire smoke is also a growing concern for public health after studies performed in mice observed that wildfire PM produced more oxidative stress and a greater inflammatory response when compared to other sources of PM (7). Other studies have found that concentrations of gas phase organic compounds and fine particle carbons measured during a wildfire episode were significantly higher than concentrations originating from urban air pollution (8). Although wildfire smoke appears to be more harmful than urban air pollution on human health (9), metrics used to communicate air quality to the public in the US, i.e., the Air Quality Index (AQI; https://www.airnow.gov/aqi/), fail to communicate current knowledge regarding the health impacts associated with PM2.5 emitted directly from wildfires (10) nor consider specific vulnerability to such impacts among subgroups such as children. Two gaps in knowledge we have identified concern are: (1) A paucity of short- and long-term respiratory impact data in the pediatric population; (2) How to best communicate air quality related to PM2.5 exposure to the public during wildfire episodes.
Children are particularly vulnerable to detrimental health impacts of wildfire smoke (11). During childhood respiratory development, lungs are more prone to injury and damage (11). Inhaling chemicals and other irritants, including PM2.5, are expected to yield more severe damage in children than in adults, via oxidative stress and inflammation (11, 12). In addition, children's smaller airway sizes, when compared to those of adults, raise their sensitivity to airborne pollutants in wildfire smoke by increasing particle deposition in children's lungs (13). Lastly, the increased respiratory rate of children compared to adults increases the dose of wildfire smoke (or any airborne pollutant) inhaled, thus putting children at a greater risk of detrimental respiratory outcomes such as lung damage (11, 14).
Although limited research has been conducted on how exposure to wildfire smoke impacts children's lungs, animal research provides insight into the physiological impact of wildfire smoke exposure on developing lungs. In 2008, a group of researchers in Northern California unintentionally exposed a colony of infant rhesus macaque monkeys to high levels of PM2.5 originating from a nearby wildfire. A colony of monkeys born the year after, and thus not exposed to wildfire smoke during infancy, were used by researchers as a control group. After evaluating both groups of monkeys during their adolescence, researchers determined that exposure to wildfire smoke as infants resulted in impaired lung function during adolescence. Although researchers concluded that exposure to wildfire smoke resulted in pulmonary damage that persisted with time, it is unknown whether said damage was detectable immediately following exposure. Animals exposed to wildfire smoke as infants tended to have a lower total lung volume when they reached adolescents (15).
A similar study, examined the consequences of early pregnancy exposure to wildfire smoke from the 2018 Camp Fire within rhesus macaque monkeys (16). The Camp Fire originated in Butte County California and resulted in elevated PM2.5 concentrations from November 9 to November 22 2018 (17, 18). The monkeys conceived before or on November 22 2018, were deemed by the researchers to be exposed to high levels of wildfire smoke, including high concentrations of PM2.5, during early pregnancy. A colony of monkeys conceived after November 22, 2018, and thus evaded exposure to wildfire smoke, were used by the team as a control group. Capitanio et al. (16) concluded that the animals exposed to wildfire smoke displayed elevations in a marker of inflammation and a varied physiological response to stress.
Researchers have been documenting the impact of wildfire PM2.5 exposure on health care utilization since the early 2000s. During a series of wildfire events in 2003 in Southern California, Delfino et al. (21) found that asthma admissions in children aged 0–4 years increased by 8.3% per 10 μg/m3 increase in PM2.5 concentration, while admissions in adults increased by 4.1%. During the post-wildfire period, children aged 0–4 saw a 51% increase in admissions for acute bronchitis and bronchiolitis and a 46% increase in pneumonia admissions (21). Künzli et al. (20) examined the same devastating events in 2003 and observed that during the wildfire episode elementary school-aged children were almost twice as likely to visit a doctor for respiratory symptoms than their high school-aged counterparts.
In another study in Southern California, Hutchinson et al. (3) estimated a mean of 89.1 μg/m3 PM2.5 concentration in the San Diego area during a series of several wildfires burning in October 2007. During this period, visits to emergency departments (ED) increased significantly for respiratory diagnosis, asthma, upper respiratory infections, acute bronchitis, and other respiratory symptoms for children aged 0–4 (3). Children aged 0–1 had the greatest increase in the presentations of symptoms identified in an ED for respiratory diagnoses (3).
After accessing pediatric health care utilization during the Lilac Fire in 2017, Leibel et al. (4) found that exposure to PM2.5 associated with wildfire smoke resulted in an increase in children aged 0–19 seeking medical treatment for respiratory symptoms, with children aged 0–5 reporting the most additional visits per day. While the Lilac Fire was active, the mean daily respiratory visits to pediatric hospital and urgent care facilities, jumped from 55 visits the week before the fire to 75.1 visits during the fire (4). Children aged 6 to 12 years old had an increase of 3.4 daily visits and children aged 0–5 years old had an increase of 7.3 visits per day (4).
Researchers across the globe have determined that wildfire episodes result in increased reports of respiratory symptoms (20, 22, 23, 25). By assessing respiratory symptoms via questionnaires, Künzli et al. (20) and Mirabelli et al. (22) determined that increases in wildfire specific PM10 resulted in an increase in respiratory symptoms across the pediatric population. Researchers assessing the impact of wildfires in Spain and Chile have also concluded that during wildfire episodes, reports of respiratory symptoms increase across the pediatric population (23, 25).
In addition to increased ED admissions and increased reports of respiratory outcomes, preliminary studies suggest that increase in the concentration of wildfire specific PM, increases the use of albuterol inhalers (an inhaler used to treat asthma (31)); a 2004 study assessing the impact of the 1994 bushfire episode in Sydney, Australia, found that during the brushfire reports of inhaled beta-agonist (another inhaler used for asthma (32)) increased to 13.2 from 9.2% and reports of inhaled corticosteroid use increased to 20.8 from 13.8% (19).
Although researchers have known that wildfire episodes increase pediatric healthcare utilization and respiratory symptoms for decades, recent studies suggest that PM originating from wildfires may be more harmful than PM from non-wildfire sources (9). After assessing pediatric health outcomes in San Diego County from 2011 to 2017, Aguilera et al. (9) determined that non-smoke PM2.5 resulted in a 3.7% increase in pediatric respiratory visits, while wildfire specific PM2.5 resulted in a 30.0% increase in pediatric respiratory visits. The authors concluded that PM2.5 from wildfires can be about 10 times more harmful as PM 2.5 from non-wildfires sources (9).
While we are unable to identify any studies that investigate the long-term effects of acute PM2.5 exposure from wildfire on children's respiratory outcomes, preliminary studies suggest that exposure to smoke specific PM2.5 may impair lung function later in life. A 2020 study by Shao et al. concluded that 3 years after the initial exposure to PM2.5 from a coal mine fire in 2014 in Australia there remained an association between exposure to high concentrations of PM2.5 and impaired lung function. After assessing the lung function of children who were exposed to fire-specific air population while under 2 years of age, the authors detected a small association between PM2.5 exposure and impaired lung function (12).
Another study by Shao et al. (13), analyzed the association between PM2.5 exposure (from the same coal mine fire above) during infancy and frequency of general practitioner visits and medication use during the year following the fire. The team found that children who were exposed to PM2.5 while under 2 years of age displayed increased use of antibiotics when compared to children who were not exposed; the exposed group had an average of 1.5 prescriptions per child per year for antibiotics in the year following the fire, while the non-exposed group had an average of 0.8 prescriptions per child per year (13).
Willis et al. (24) analyzed the long-term effects on health outcomes 2–4 years after the above coal fire episode and concluded that exposure to increased concentrations of PM2.5 from the coal fire while in utero was associated with impaired respiratory health and increased health care utilization 2–4 years after exposure. Table 1 summarizes the studies assessing pediatric health care outcomes during wildfires.
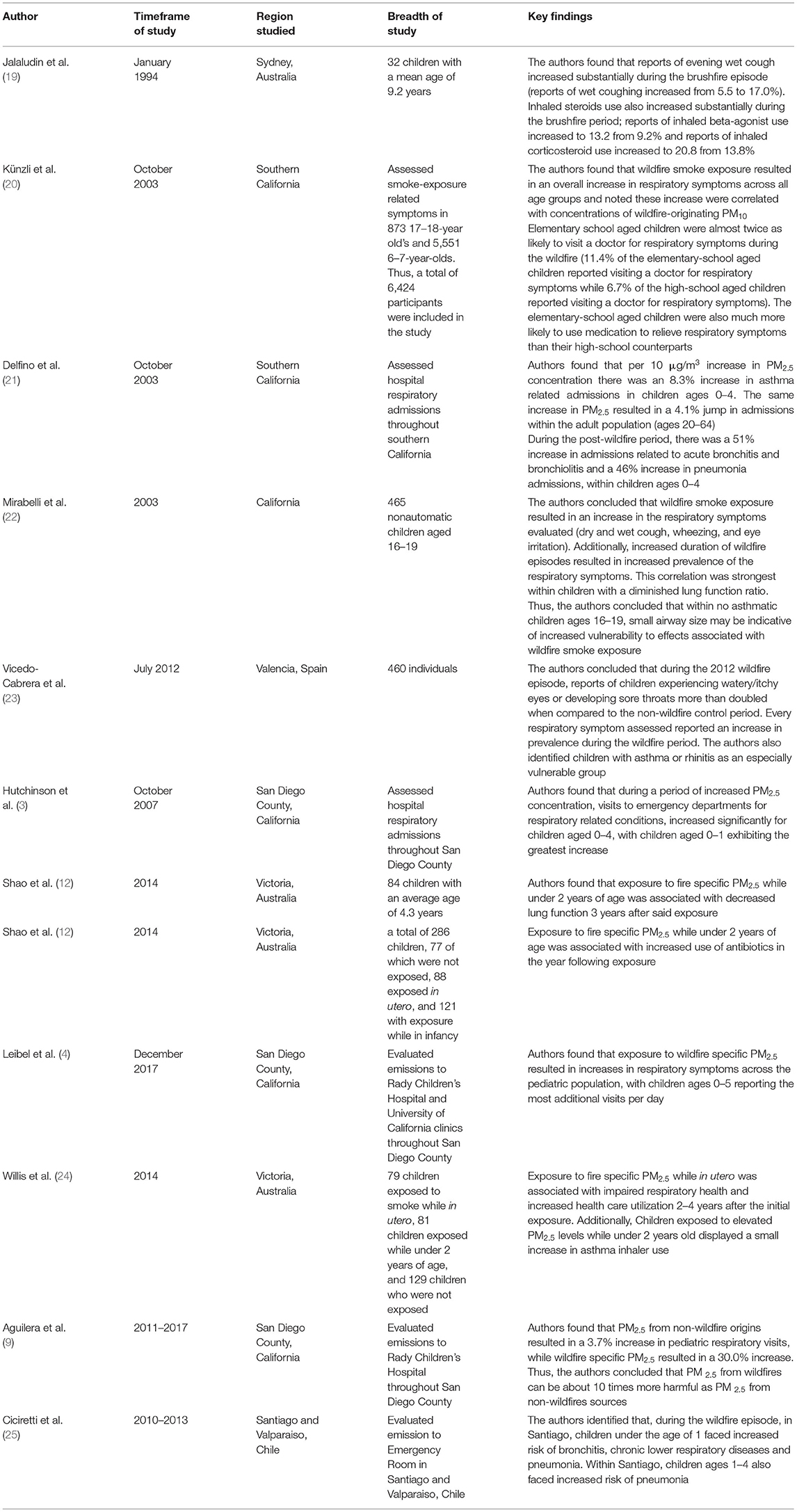
Table 1. Summary of wildfire and PM2.5 pediatric respiratory impact studies reviewed (organized chronologically by year published).
The standard measure of air quality in the United States, the Air Quality Index (AQI), provides guidance about air pollution to healthcare providers as well as the general public, including schools and parents (33). Based on the AQI during a wildfire, schools and healthcare providers may make decisions affecting children regarding masking and limiting outdoor activities (34). The AQI, however, does not include updated information regarding the impact of PM2.5 exposure according to particle chemical composition, sources of emissions nor growing evidence supporting exacerbated impacts among children and subgroups of the population. Specifically, the AQI communicates the dangers associated with six different air pollutants: ozone (O3), particle pollution (PM2.5 and PM10), carbon monoxide (CO), sulfur dioxide (SO2), and nitrogen dioxide (NO2). When calculating air quality associated with PM2.5, the AQI only considers the concentration of PM2.5 , disregarding the source of emission of PM2.5 (35), i.e., whether pollution is emitted from traffic or industrial activities, or wildfires.
In other regions such as Canada, researchers have raised concerns about the efficacy of standard measurement of air quality (Air Quality Health Index (AQHI)) during wildfire episodes (27). The AQHI is calculated based on the concentrations of O3, NO2, and PM2.5 and conveys air quality via a 1–10 scale (with 1 being low risk and 10 being high risk). Because AQHI considers risk associated with O3, NO2 and PM2.5, increased concentrations of PM2.5 during wildfire episodes may fail to push AQHI into the moderate/high risk category. Additionally, the AQHI value that is reported each hour is based on a 3-h average of each pollutant considered, and thus may fail to communicate risk associated with rapid increases in PM2.5 concentrations during wildfire episodes (26, 36). For instance, as noted by Yao et al. (27) during a 2014 wildfire episode in British Columbia, the highest AQHI value recorded was during a period of high O3 concentration. However, during peak PM2.5 concentrations, a lower AQHI value was recorded (27).
The AQHI has since been updated to reflect current knowledge regarding the risks of PM2, 5 exposure. The region of British Columbia implemented an addendum to the AQHI which ensured that if the PM2.5 concentration exceeded 60 μg/m3, the Trump & Hold AQHI-Plus value would be reported as 7, regardless of if the AQHI value was less than 7. The Trump & Hold AQHI-Plus value would remain as 7 for the following 5 h if the PM2.5 concentration was greater than 25 μg/m3 during the hour following the initial 60+ μg/m3 PM2.5 concentration (27).
Over a period of eight wildfire seasons from 2010 to 2017, Yao et al. (27) examined the relative effectiveness of AQHI, Trump & Hold AQHI-plus and three other metrics, placing particular emphasis on the ability of the evaluations of air quality to predict the prevalence of adverse health impact due to wildfire smoke. The 1-h PM2.5 Only AQHI-Plus method of accessing air quality, one of the other metrics evaluated by Yao et al., was developed in order to better communicate the impact that gradual increases in PM2.5 has on air quality. Like the Trump & Hold AQHI-Plus , the 1-h PM2.5 Only AQHI-Plus method ensures that when concentration of PM2.5 reaches 60 μg/m3, the AQHI-plus value will be reported as 7, however, the 1-h PM2.5 Only method also ensures that when concentrations of PM2.5 are over 30 μg/m3 the AQHI-plus value will be reported as 4. Yao et al. (27), concluded that this measurement of air quality was the best predictor of the respiratory-related health impacts, especially for individuals with asthma, during high intensity wildfire episodes. Thus, the authors recommended that the 1-h PM2.5 Only AQHI - Plus mechanism be used to communicate air quality during wildfire season (27).
In an effort to combat the negative health outcomes of air pollution exposure, Gladson et al. (29), conducted a study to determine the best mechanism for respiratory risk among children (29). The team found that the most effective communicators of risk globally were indexes that adjusted for extreme pollution values while simultaneously considering the effect of co-pollutants (29).
In addition to updating the metric used to evaluate air quality, researchers have noted that smoke-forecasting systems and other prediction systems may aid in implementation of improved public health responses. A 2013 study by Yao et al. (26) assessed the utility of one such system, the BlueSky Western Canada Wildfire Smoke Forecasting Framework. This technology has provided the public with forecasts of PM2.5 concentrations up to 60 h in advance since 2010. After evaluating the technology's performance for a period of 35 days during fire season (from July 24 to August 29, 2010), the team concluded that there was modest agreement between the PM2.5 concentration predicted by BlueSky technology and the hourly measured PM2.5 concentrations (26). The authors also concluded that each 30 μg/m3 increase in BlueSky's PM2.5 prediction was correlated with an 8% increase in salbutamol (a common asthma prescription) dispensations and 5% increase in asthma-related physician visits (26, 31).
The efficacy of another prediction system, the British Columbia Asthma Prediction System (BCAPS), was assessed by Henderson et al. (30) during British Columbia's 2018 wildfire season. The BCAPS uses historical data on PM2.5 concentrations and subsequent health outcomes to predict the impact of PM2.5 exposure in the upcoming days. The inhaler dispensation forecasts made by the BCAPS during the study period were within 20% of the actual value in 71% of observed cases. The authors noted that BCAPS provided users with valuable insights regarding the impact of expected smoke exposure (30).
Within Australia, another modeling technique, Air Quality Visualization (AQVx), was trialed in Victoria, a region of south-eastern Australia plagued by both frequent wildfire episodes during the summer and large-scale prescribed burnings (28). The AQVx system incorporates air quality metrics, satellite imagery, radar, and crowd-sourced information (health symptoms, smoke sightings, etc.) into the final interface. According to Williamson et al. (28), the AQVx system provided the Department of Environmental, Land, Water, and Planning with information necessary to identify populations at risk of smoke exposure. Table 2 Summarizes the studies assessing efficacy of communicating air quality.
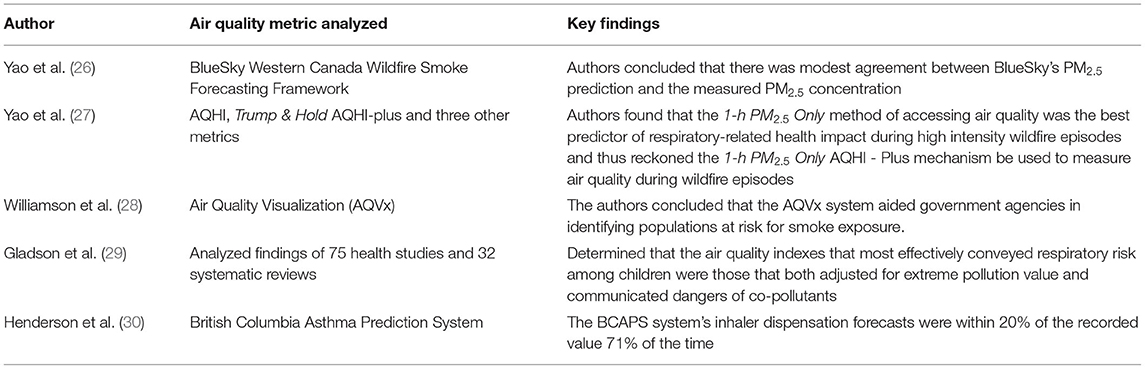
Table 2. Summary of air quality communication studies reviewed (organized chronologically by year published).
As climate change continues to promote hotter and drier conditions in California, exacerbating California's already notorious wildfire seasons (37), more children are expected to be exposed to and disproportionately affected by wildfire smoke (38). Within this paper, our group provided a summary of the existing knowledge regarding both short- and long-term exposure to smoke-specific PM2.5 and assessed the efficacy of air quality metrics during wildfire episodes.
Based on the above findings, we are concerned that the respiratory impacts of wildfire specific PM2.5 on children is currently being underestimated and needs to be investigated further regarding both short- and long-term health outcomes. Additionally, young children may be particularly at risk for increased respiratory healthcare utilization (4) because of physiologic aspects of lung development. Furthermore, PM2.5 from wildfire exposure may have more of a respiratory health impact than ambient PM2.5 as suggested by Aguilera et al. (9).
In order to protect children - our most vulnerable population - more specific analysis on the pediatric respiratory effects of PM2.5 during wildfires and bolder steps to incorporate the effects of wildfire PM2.5 into the USA's AQI, particularly in wildfire prone areas, are both needed.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
SN complied sources and wrote drafts of the manuscript. RA, AG, TB, and SL suggested sources to include and provided SN with comments on drafts. SL provided additional guidance to SN. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Williams AP, Abatzoglou JT, Gershunov A, Guzman-Morales J, Bishop DA, Balch JK, et al. Observed impacts of anthropogenic climate change on wildfire in California. Earth's Future. (2019) 7:892–910. doi: 10.1029/2019EF001210
2. California Department of Forestry Fire Protection (CAL FIRE). 2020 incident archive. Cal Fire Department of Forestry and Fire Protection. Avaible online at: https://www.fire.ca.gov/incidents/2020/ (accessed November 13, 2021).
3. Hutchinson JA, Vargo J, Milet M, French N, Billmire M, Johnson J, et al. The San Diego 2007 wildfires and Medi-Cal emergency department presentations, inpatient hospitalizations, and outpatient visits: an observational study of smoke exposure periods and a bidirectional case-crossover analysis. PLoS Med. (2018) 15:e1002601. doi: 10.1371/journal.pmed.1002601
4. Leibel S, Nguyen M, Brick W, Parker J, Ilango S, Aguilera R, et al. Increase in pediatric respiratory visits associated with santa ana wind-driven wildfire smoke and PM2.5 levels in San Diego County. Ann Am Thorac Soc. (2020) 17:313–20. doi: 10.1513/AnnalsATS.201902-150OC
5. McClure CD, Jaffe DA. US particulate matter air quality improves except in wildfire-prone areas. Proc Nat Acad Sci USA. (2018) 115:7901–6. doi: 10.1073/pnas.1804353115
6. Ford B, Val Martin M, Zelasky SE, Fischer EV, Anenberg SC, Heald CL, et al. Future fire impacts on smoke concentrations, visibility, and health in the contiguous United States. GeoHealth. (2018) 2:229–47. doi: 10.1029/2018GH000144
7. Wegesser TC, Franzi LM, Mitloehner FM, Eiguren-Fernandez A, Last JA. Lung antioxidant and cytokine responses to coarse and fine particulate matter from the great California wildfires of 2008. Inhal Toxicol. (2010) 22:561–70. doi: 10.3109/08958370903571849
8. Na K, Cocker DR. Fine organic particle, formaldehyde, acetaldehyde concentrations under and after the influence of fire activity in the atmosphere of Riverside, California. Environ Res. (2008) 108:7–14. doi: 10.1016/j.envres.2008.04.004
9. Aguilera R, Corringham T, Gershunov A, Leibel S, Benmarhnia T. Fine particles in wildfire smoke and pediatric respiratory health in California. Pediatrics. (2021) 147:e2020027128. doi: 10.1542/peds.2020-027128
10. Monteiro A, Vieira M, Gama C, Miranda AI. Towards an improved air quality index. Air Qual Atmos Health. (2016) 10:447–55. doi: 10.1007/s11869-016-0435-y
11. Holm SM, Miller MD, Balmes JR. Health effects of wildfire smoke in children and public health tools: a narrative review. J Expo Sci Environ Epidemiol. (2021) 31:1–20. doi: 10.1038/s41370-020-00267-4
12. Shao J, Zosky GR, Hall GL, Wheeler AJ, Dharmage S, Melody S, et al. Early life exposure to coal mine fire smoke emissions and altered lung function in young children. Respirology. (2019) 25:198–205. doi: 10.1111/resp.13617
13. Shao J, Zosky GR, Wheeler AJ, Dharmage S, Dalton M, Williamson GJ, et al. Exposure to air pollution during the first 1000 days of life and subsequent health service and medication usage in children. Environ Pollut. (2020) 256:113340. doi: 10.1016/j.envpol.2019.113340
14. Dietert RR, Etzel RA, Chen D, Halonen M, Holladay SD, Jarabek AM, et al. Workshop to identify critical windows of exposure for children's health: immune and respiratory systems work group summary. Environ Health Perspect. (2000) 108 Suppl 3(Suppl 3), 483–90. doi: 10.1289/ehp.00108s3483
15. Black C, Gerriets JE, Fontaine JH, Harper RW, Kenyon NJ, Tablin F, et al. Early life wildfire smoke exposure is associated with immune dysregulation and lung function decrements in adolescence. Am J Respir Cell Mol Biol. (2017) 56:657–66. doi: 10.1165/rcmb.2016-0380OC
16. Capitanio JP, Del Rosso LA, Gee N, Lasley BL. Adverse biobehavioral effects in infants resulting from pregnant rhesus macaques' exposure to wildfire smoke. Nat Commun. (2022) 13:1774. doi: 10.1038/s41467-022-29436-9
17. Fire name (cause) date county acres... - California. Available online at: https://www.fire.ca.gov/media/lbfd0m2f/top20_deadliest.pdf (accessed April 19, 2022).
18. Huttunen K, Siponen T, Salonen I, Yli-Tuomi T, Aurela M, Dufva H, et al. Low-level exposure to ambient particulate matter is associated with systemic inflammation in ischemic heart disease patients. Environ Res. (2012) 116:44–51. doi: 10.1016/j.envres.2012.04.004
19. Jalaludin BB, O'Toole BI, Morgan G, Leeder S. Acute Effects of bushfires on respiratory symptoms and medication use in children with wheeze in Sydney, Australia. Environ Health. (2004) 4:20–9. doi: 10.3316/informit.202856565301189
20. Künzli N, Avol E, Wu J, Gauderman WJ, Rappaport E, Millstein J, et al. Health effects of the 2003 Southern California wildfires on children. Am J Respir Crit Care Med. (2006) 174:1221–8. doi: 10.1164/rccm.200604-519OC
21. Delfino RJ, Brummel S, Wu J, Stern H, Ostro B, Lipsett M, et al. The relationship of respiratory and cardiovascular hospital admissions to the southern California wildfires of 2003. Occup Environ Med. (2009) 66:189–97. doi: 10.1136/oem.2008.041376
22. Mirabelli MC, Künzli N, Avol E, Gilliland FD, Gauderman WJ, McConnell R, et al. Respiratory symptoms following wildfire smoke exposure. Epidemiology. (2009) 20:451–9. doi: 10.1097/EDE.0b013e31819d128d
23. Vicedo-Cabrera AM, Esplugues A, Iñíguez C, Estarlich M, Ballester F. Health effects of the 2012 Valencia (Spain) wildfires on children in a cohort study. Environ Geochem Health. (2015) 38:703–12. doi: 10.1007/s10653-015-9753-5
24. Willis GA, Chappell K, Williams S, Melody SM, Wheeler A, Dalton M, et al. Respiratory and atopic conditions in children two to four years after the 2014 Hazelwood coalmine fire. Med J Aust. (2020) 213:269–75. doi: 10.5694/mja2.50719
25. Ciciretti R, Barraza F, De la Barrera F, Urquieta L, Cortes S. Relationship between wildfire smoke and children's respiratory health in the metropolitan cities of Central-Chile. Atmosphere. (2021) 13:58. doi: 10.3390/atmos13010058
26. Yao J, Brauer M, Henderson SB. Evaluation of a wildfire smoke forecasting system as a tool for public health protection. Environ Health Perspect. (2013) 121:1142–7. doi: 10.1289/ehp.1306768
27. Yao J, Stieb DM, Taylor E, Henderson SB. Assessment of the Air Quality Health Index (AQHI) and four alternate AQHI-Plus amendments for wildfire seasons in British Columbia. Can J Public Health. (2020) 111:96–106. doi: 10.17269/s41997-019-00237-w
28. Williamson GJ, Lucani C. AQVx-an interactive visual display system for air pollution and Public Health. Front Public Health. (2020) 8:85. doi: 10.3389/fpubh.2020.00085
29. Gladson LA, Cromar KR, Ghazipura M, Knowland KE, Keller CA, Duncan B. Communicating respiratory health risk among children using a global air quality index. Environ Int. (2022) 159:107023. doi: 10.1016/j.envint.2021.107023
30. Henderson SB, Morrison KT, McLean KE, Ding Y, Yao J, Shaddick G, et al. Staying ahead of the epidemiologic curve: evaluation of the British Columbia Asthma Prediction System (BCAPS) during the unprecedented 2018 wildfire season. Front Public Health. (2021) 9:499309. doi: 10.3389/fpubh.2021.499309
31. NHS. Salbutamol inhaler. NHS choices (2021). Available online at: https://www.nhs.uk/medicines/salbutamol-inhaler/ (accessed April 30, 2022).
32. NHS. Overview -Bronchodilators. NHS choices (2019). Available online at: https://www.nhs.uk/conditions/bronchodilators/#:~:text=Beta%2D2%20agonists%20are%20used,also%20be%20injected%20or%20nebulised (accessed April 30, 2022).
33. System alerts. Air Quality Flag Program Main Page | AirNow.gov. Available online at: https://www.airnow.gov/air-quality-flag-program/ (accessed November 13, 2021).
34. McBride DL. Protecting children from wildfire smoke. J Pediatr Nurs. (2021) 60:300–2. doi: 10.1016/j.pedn.2021.08.015
35. EPA. (2018). Technical assistance document for the reporting ... - airnow. https://www.epa.gov/. Available online at: https://www.airnow.gov/sites/default/files/2020-05/aqi-technical-assistance-document-sept2018.pdf (accessed April 29, 2022).
36. Yao J, Eyamie J, Henderson SB. Evaluation of a spatially resolved forest fire smoke model for population-based epidemiologic exposure assessment. J Expo Sci Environ Epidemiol. (2016) 26:233–40. doi: 10.1038/jes.2014.67
37. Goss M, Swain DL, Abatzoglou JT, Sarhadi A, Kolden CA, Williams AP, et al. Climate change is in creasing the likelihood of extreme autumn wildfire conditions across California. Environ Res Lett. (2020) 15:094016. doi: 10.1088/1748-9326/ab83a7
Keywords: PM2.5 exposure, pediatric, respiratory, California wildfires, Air Quality Index (AQI) efficiency
Citation: Naughten SM, Aguilera R, Gershunov A, Benmarhnia T and Leibel S (2022) A Perspective on Pediatric Respiratory Outcomes During California Wildfires Due to Smoke and PM2.5 Exposure. Front. Pediatr. 10:891616. doi: 10.3389/fped.2022.891616
Received: 08 March 2022; Accepted: 13 June 2022;
Published: 06 July 2022.
Edited by:
Bülent Taner Karadag, Marmara University, TurkeyReviewed by:
Fabienne Reisen, CSIRO Oceans and Atmosphere, AustraliaCopyright © 2022 Naughten, Aguilera, Gershunov, Benmarhnia and Leibel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sydney Leibel, c2xlaWJlbEBoZWFsdGgudWNzZC5lZHU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.