- 1Department of Gastroenterology, The Second Xiangya Hospital of Central South University, Changsha, China
- 2Research Center of Digestive Disease, Central South University, Changsha, China
Background: Peroral endoscopic myotomy (POEM) has shown promising short-term safety and efficacy in pediatric patients, while long-term outcomes are largely unknown. This study aimed to assess the clinical effects of POEM for pediatric achalasia who had a follow-up of at least 5 years.
Methods: Pediatric patients from a single center who underwent a POEM between October 2011 and November 2016 were, respectively, collected and analyzed for long-term clinical outcomes. Patients were contacted to evaluate their current symptoms and encouraged repeat endoscopy and manometry. The clinical success, procedure-related parameters, adverse events, gastroesophageal reflux disease after POEM, and quality of life were evaluated.
Results: A total of twenty-four patients who underwent POEM in our center were studied, with a mean age of 14.42 ± 2.65. Two of the 24 patients (8.3%) had previous treatment. The mean of the procedure time was 58.67 ± 19.10 min, 8.3% (2/24) of patients experienced perioperative adverse events. The current symptom scores were obtained from 21 patients at a mean follow-up of 92.57 months, the remainder were lost to follow-up after a mean of 38 months. Eckardt scores were significantly improved from preoperative baseline (preoperative 7.67 ± 1.62 vs. current 0.86 ± 1.28, P < 0.001). Long-term overall success was achieved in 95.8% of patients and none required retreatment for symptoms. 12.5% of patients were suffered from clinical reflux. 76.2% of patients expressed satisfaction with POEM. No severe adverse events were observed during the operation and the 5-years follow-up.
Conclusion: POEM resulted in successful symptomatic mitigation in a majority of pediatric patients after 5 years. A multi-center large-scale, prospective study is necessary for a confirmed conclusion.
Introduction
Achalasia is a rare esophageal motility disorder in pediatric, characterized by esophageal dysmotility and defective relaxation of the lower esophageal sphincter (LES). Its incidence in children is estimated to be 0.02–0.31 per 100,000 children per year (1–3). The pronounced symptoms of pediatric achalasia are dysphagia, regurgitation, vomiting, chest pain, weight loss, and respiratory symptoms (nocturnal cough, aspiration). If not appropriately treated, achalasia in children may lead to recurrent pneumonia, malnutrition, even intellectual and developmental disability. The symptoms may proceed into adulthood and impact quality of life.
Traditionally, achalasia in children has been treated with medical therapy, botulinum toxin injections, or balloon dilation, which do not have a long-lasting efficacy and often require additional interventions (4–8). Heller myotomy was recommended as first-line therapy for childhood achalasia, superior to balloon dilatation or botulinum injection (9, 10). After Inoue et al. described the first series of patients who received peroral endoscopic myotomy (POEM) in 2010 (11), POEM became a minimally invasive, rapid recovery, and preferred relatively novel procedure for achalasia in adults (12, 13). Multiple studies have also confirmed its efficacy and safety in children and adolescent patients (14–21). However, the long-term follow-up study in children, notably more than 5 years, is unclear.
In the present study, we investigated the clinical data of patients with pediatric achalasia who were at least 5 years out from their POEM procedure in our institution. We attempted to assess the endurance of symptom relief after POEM, as well as the outcomes of repeated esophagogastroduodenoscopy (EGD) and manometry, to understand the long-term outcome of the operation better.
Materials and Methods
Patients
The study was approved by the ethics committee of the Second Xiangya Hospital of Central South University. All the pediatric patients with achalasia who underwent POEM in our department between October 2011 and November 2016 were retrospectively collected. The inclusion criteria in this study included: (1) Achalasia diagnosed by Eckardt score ≥ 4 and further confirmed by esophagogastroduodenoscopy (EGD), barium esophagram, and/or esophageal manometry; and excluding others secondary to tumor, autoimmune diseases, etc. (2) patients with age ≤ 17 when performing POEM; (3) patients received POEM as a treatment more than 5 years. Those patients with severe cardiopulmonary disease, blood coagulation disorders, or other underlying diseases were excluded from this study. Demographics, presentation, clinical history, operation records, postoperative adverse events were retrieved from the medical records. Written informed consent was obtained from all patients’ parents or caregivers before the procedure was performed. All of them were informed of possible adverse events and other possible treatment options.
Peroral Endoscopic Myotomy Procedure
Pediatric POEMs were performed by three experienced endoscopists with more than 30 adult POEMs (DLL, LL, HYZ). The patients were required to fast for 12 h before their procedures. POEM was performed under general anesthesia via tracheal intubation using a standard single-channel endoscopy (GIF-Q260J; Olympus, Tokyo, Japan) with a transparent cap (D-201-11,802, Olympus) attached to the front. A carbon dioxide insufflator (UCR, Olympus) was used as the air supply from the endoscopy. Other equipment and accessories included a high-frequency generator (ICC 200; Erbe, Tübingen, Germany), argon plasma coagulation unit (APC300; Erbe), injection needle (NM-4L-1; Olympus), hybrid knife (Erbe), dual knife (KD-650L; Olympus), and hemostatic clips (HX-600-135; Olympus).
The POEM procedure was performed as previously reported (16, 17): Briefly, this procedure included five major steps: (1) A submucosal injection was made using mixed solution (100 ml saline + 2 ml indigo carmine + 1 mg epinephrine), (2) A longitudinal mucosal incision (about 2–3 cm long) was made using a dual or hybrid knife; (3) A submucosal tunneling was created passing over the esophagogastric junction (EGJ); (4) Myotomy was started from 2 to 3 cm below tunnel entry, (5) After careful hemostasis, closure of mucosal incision was finished with metal clips. The right posterior approach at 6–10 cm above EGJ was generally applied except for some complicated cases, such as fibrosis of the posterior location. For patients who have previously undergone endoscopic or surgical treatment, tunneling and myotomy were performed in areas of normal tissue to avoid fibrosis or adhesions caused by previous treatment. Figure 1 describes the procedure of POEM.
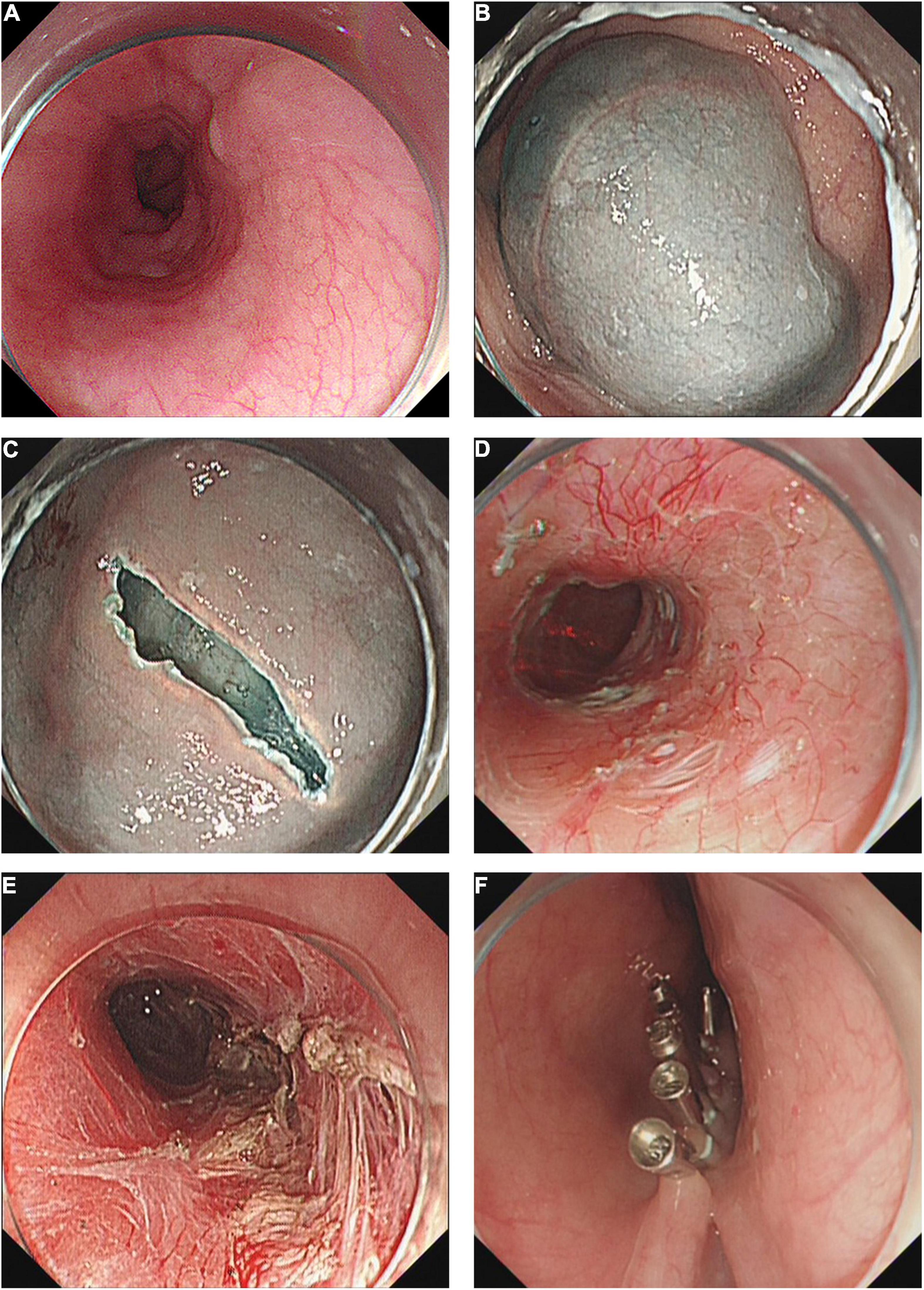
Figure 1. Technique of peroral endoscopic myotomy. (A) A dilated esophagus. (B) Submucosal injection. (C) Create tunnel entry. (D) Submucosal tunnel. (E) Circular myotomy. (F) Close the tunnel entry with metal clips.
Patients were fasted for 24 h after POEM, a liquid diet for 3 days, and returning gradually to a regular diet within 2 weeks. Intravenous proton pump inhibitor (PPI) and antibiotics were continued for 3 days. At Day 2 post-procedure, thoracoabdominal X-ray, or sometimes a chest CT, was performed to check for the occurrence of emphysema, pneumothorax, pneumoperitoneum and pleural effusion, etc.
The Primary Outcomes
The primary outcome was clinical success defined as a post-treatment Eckardt score reduced to ≤ 3 and freedom from re-intervention for persistent or recurrent symptoms (12, 22). The Eckardt score is a sum of the symptoms for dysphagia, regurgitation, chest pain, and weight loss. The maximum score is 12, suggesting the most pronounced symptoms.
The Secondary Outcomes
The secondary outcomes included technical success, procedure-related parameters, rate of adverse events, length of postoperative hospital stay, gastroesophageal reflux disease after POEM, and quality of life.
Technical success was defined as the completion of the whole POEM procedure. Mild perioperative adverse events (AEs) were defined as insufflation-related AEs, mucosal injuries, bleeding, pain requiring analgesics, and aspiration pneumonia; severe AEs were defined as delayed mucosal barrier failure, esophageal leaks, POEM related cardiopulmonary disease, intensive care unit admission, and conversion to a laparoscopic or open procedure (23). Length of postoperative hospital stay was defined as the number of days from procedure to hospital discharge. A GerdQ score of gastroesophageal reflux disease with a score of > 7 was defined as symptomatic reflux (18, 24–26). Reflux esophagitis was diagnosed and graded by EGD based on Los Angeles (LA) Classification. Clinical reflux was diagnosed if both symptomatic reflux and reflux esophagitis were positive. Quality of life (QoL) was assessed by Urbach scale questionaries, which is a 10-item measure of disease-specific health-related QoL that sampled the concepts of food tolerance, dysphagia-related behavior modifications, pain, heartburn, distress, lifestyle limitation, and satisfaction (27).
Follow Up
Children with achalasia received follow up postoperatively at 6, 12, 24, and 36 months, and then every 2 years. Eckardt score was regularly obtained to assess clinical symptomatic response or recurrence via telephone or face-to-face visit. At 6 months postoperatively, EGD, esophageal manometry, and barium esophagram were recommended for outcome evaluation.
Patients who underwent POEM for more than 5 years at the current study were contacted via telephone to obtain a current Eckardt score, GerdQ score, and Urbach scale questionaries. Those symptoms were recorded from the patient’s self-report or their parents and caretakers. Meanwhile, Patients were encouraged to have a repeat EGD, barium esophagram, and esophageal manometry at the current study time in our hospital. Patients or caretakers who lived far from our hospital or were unwilling to return for follow-up were followed through detailed telephone interviews to assess for AEs and obtain a current physical condition, including questionaries about their symptoms and examinations and treatments at other hospitals.
During the follow-up, orally PPIs were only used in those with symptoms of reflux and/or endoscopy-proven reflux esophagitis.
Statistical Analysis
The data were analyzed using SPSS 24.0 (Chicago, United States). Quantitative variables were presented as mean ± SD or medians and range. They were compared using a t-test or Mann-Whitney U-test. Categorical variables were expressed as absolute or relative frequencies. Those data were calculated using Chi-square or Fisher’s tests. A two-sided p < 0.05 was considered statistically significant.
Results
Patient Characteristics and Perioperative Outcomes
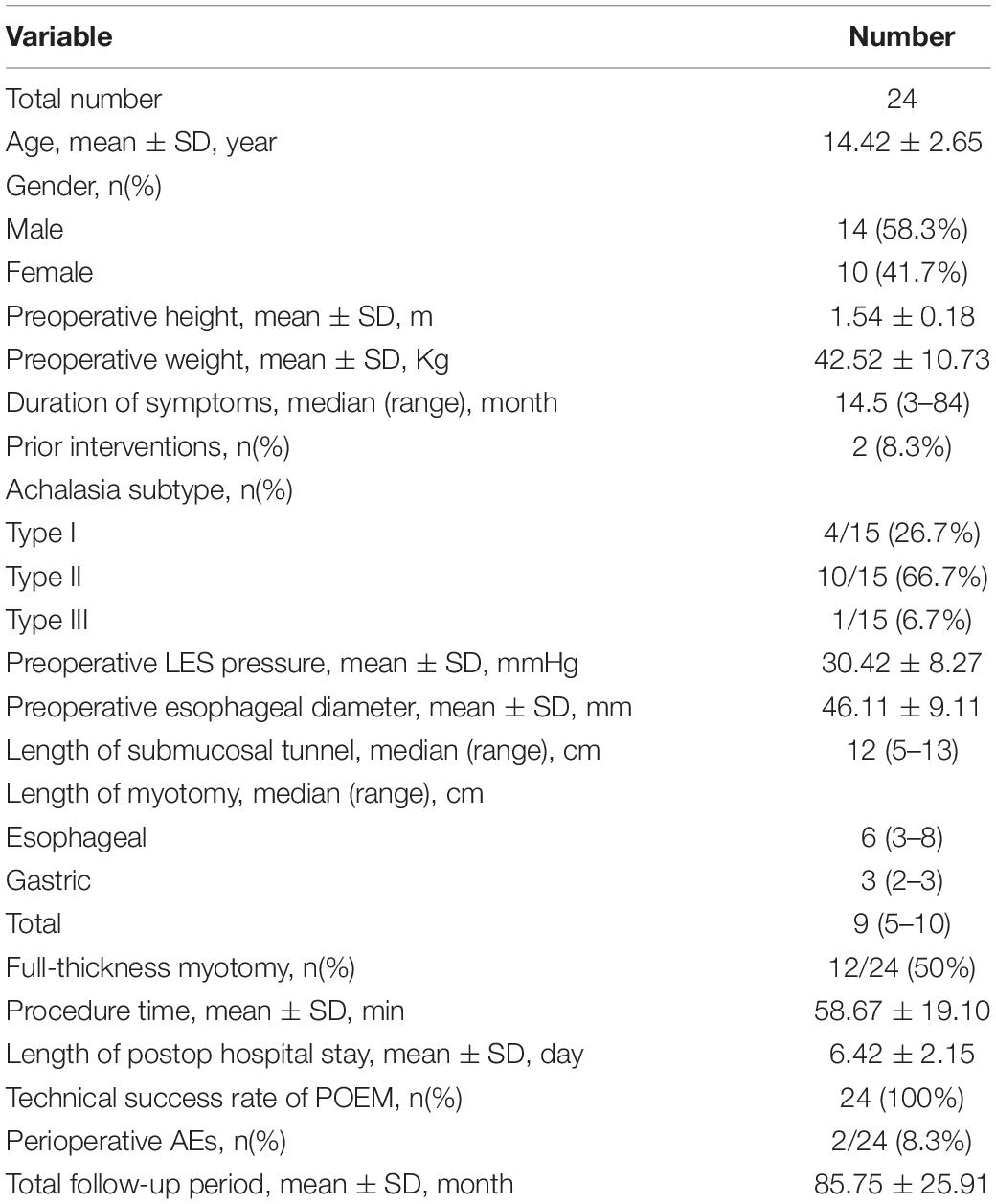
A total of 24 patients were collected during the specified duration. Fourteen of them were male and ten were female, with a mean age of 14.42 ± 2.65 year-old. The mean preoperative height is 1.54 ± 0.18 m and the mean preoperative weight is 42.52 ± 10.73 Kg. The median duration of symptoms is 14.50 (range 3–84) months. Two patients (8.3%) had received prior treatment, including 1 Heller myotomy and 1 balloon dilation. Fifteen patients underwent preoperative manometry. According to the Chicago classification of Esophageal Motility Disorders, the subtypes were type I 4 (26.7%), type II 10 (66.7%), and type III 1 (6.7%). The mean LES pre-POEM pressure was 30.42 ± 8.27 mmHg. The mean pre-POEM esophageal diameter was 46.11 ± 9.11 mm. One child who had a history of balloon dilation performed an anterior approach. Twenty-three children performed a right posterior approach. The median length of the submucosal tunnel is 12 (range 5–13) cm. The median incision length of esophageal, gastric and total is 6 (range 3–8) cm, 3 (range 2–3) cm, and 9 (range 5–10) cm, respectively. Full-thickness myotomy was performed in 50% (12/24) of the children. The mean operative time was 58.67 ± 19.10 min. The mean length of postoperatively hospital stay was 6.42 ± 2.15 days and the technical success of POEM is 100%(24/24). Two (8.3%) children developed perioperative subcutaneous emphysema. One children’s CT showed retroperitoneal, abdominal, and esophageal gas accumulation; another showed chest subcutaneous emphysema. Their gas-related AEs were spontaneously absorbed without any intervention. No severe perioperative adverse events occurred in those patients. The mean of total follow-up time was 85.75 ± 25.91 months (Table 1).
Symptomatic Outcomes
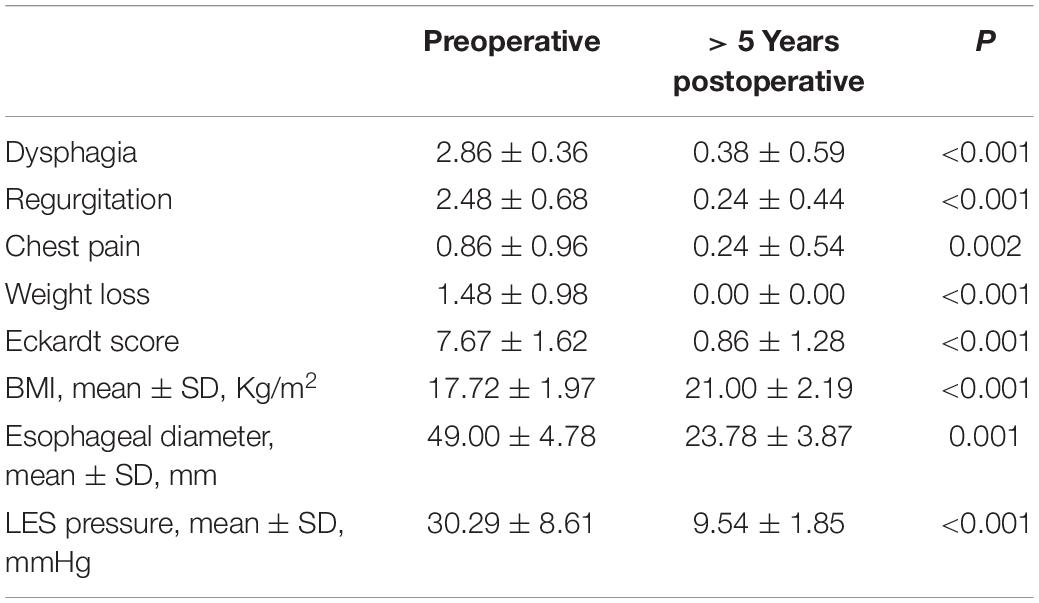
Of a mean follow-up period of 85.75 ± 25.91 months, 3 patients were lost for long-term follow-up. None of them had a history of prior treatment for achalasia. They were similar in age (14.29 ± 2.81 vs. 15.33 ± 0.58, p = 0.534), sex (57.1 vs. 66.7% of male, p = 1.000), and Eckardt Score at baseline (7.67 ± 1.62 vs. 7.67 ± 3.22, p = 1.000) compared to those who remained under study. With a mean follow-up duration of 38 ± 7.55 months, the mean Eckardt score at the last follow-up was 0.67 ± 0.58. These three patients were considered to be a clinical success at the previous follow-up. All patients have a 95.8%(23/24) clinical success rate, none underwent operational intervention again. With a mean follow-up time of 92.57 ± 19.38 months, the Eckardt score after 5 years of follow-up was significantly declined compared with the score before POEM (7.67 ± 1.62 vs. 0.86 ± 1.28, p < 0.001). Table 2 shows the change in each symptom component of the Eckardt score. One of the patients (Eckardt score = 4) suffered from mild dysphagia and chest pain from 39 months post-POEM. He needed to drink water when swallowing hard food most of the time, but still within tolerable limits. The chest pain can be alleviated by oral PPIs. The recent upper endoscopy showed multiple esophageal polyps (POEM related). Currently, he is undergoing symptoms and physiologic surveillance. The mean weight and height gain in patients are 17.41 ± 9.75 Kg and 0.15 ± 0.12 m in 5 years follow-up, respectively. At 5-year follow-up, the BMI was significantly increased from pre-POEM (preoperative 17.72 ± 1.97 vs. current 21.00 ± 2.19, p < 0.001). Additionally, Urbach scale questionaries were obtained from 21 patients to evaluate their quality of life. The median score was 14 (range 11–22). The outstanding symptoms reported by patients were the need to drink water while eating (14/21, 66.7%), bothered by the eating time (17/21, 81.0%). 71.4%(15/21) patients reported no limitation of lifestyle because of achalasia, 9.5% (2/21) of patients are very satisfied and 66.7%(14/21) are satisfied with their health as for achalasia.
Objective Outcomes
A total of 4 patients had paired barium esophagram results, the esophageal diameter is significantly decreased at 5 years post-POEM compared with the pre-POEM (49.00 ± 4.78 mm vs. 23.78 ± 3.87 mm, p = 0.001). A total of 10 patients had paired manometry results, and the LES pressure is significantly decreased at 5 years post-POEM compared with the pre-POEM (30.29 ± 8.61 vs. 9.54 ± 1.85 mmHg, p < 0.001) (Table 2). None of the children developed severe adverse events during the follow-ups, such as delayed bleeding, gastrointestinal fistulas, and secondary mediastinal or abdominal infections.
Comparison of Outcomes Between Short-Term and Long-Term Follow-up
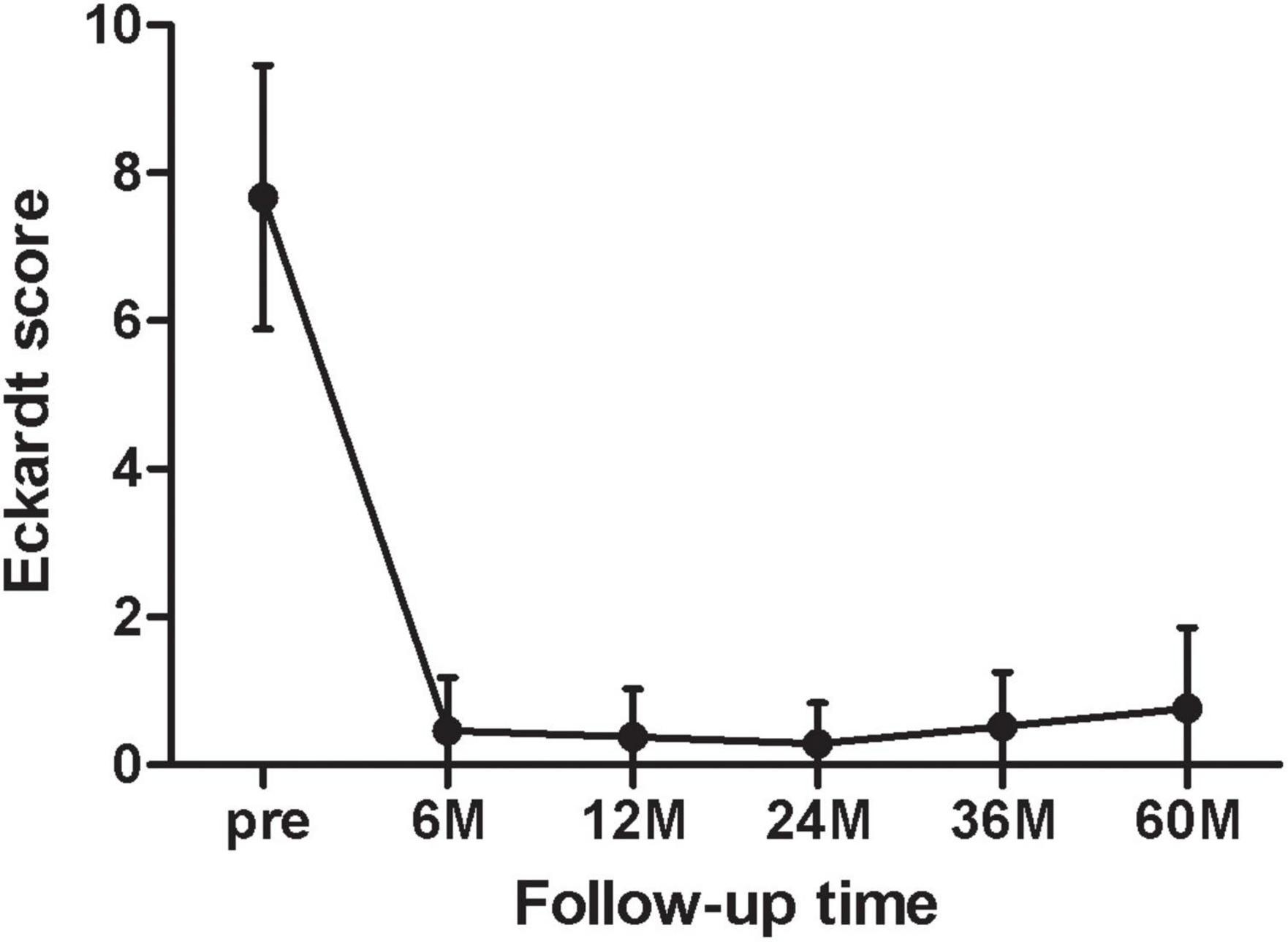
Figure 2 showed the mean of the Eckardt score at each follow-up point (6, 12, 24, 36, 60 months). At 6 months postoperatively, the Eckardt score was significantly decreased from baseline (pre 7.67 ± 1.79 vs. 6 months0.46 ± 0.72, p < 0.001, n = 24). However, the Eckardt score began to gradually deteriorate in the second year (24 months 0.19 ± 0.40 vs. 60 months 0.76 ± 1.09, p = 0.019, n = 21).
With 3 patients having paired barium esophagram results and 9 patients having paired esophageal manometry results, there were no significant differences in Eckardt score, LES pressure, and esophageal diameter between 6 months and 5 years postoperatively (Supplementary Table 1).
Post-peroral Endoscopic Myotomy Gastro-Esophageal Reflux
At 6 months follow-up, 3 children (3/24, 12.5%) showed esophagitis on EGD (2 Los Angeles Type A, 1 Los Angeles Type B), their symptoms relieved after a 4-week oral PPI therapy. At 5 years follow-up, five patients (5/21, 23.8%) were suffered from symptomatic reflux, three patients (3/16, 18.8%) showed reflux esophagitis (2 Los Angeles Type A, 1 Los Angeles Type B) on endoscopy, two patients (2/16, 12.5%) were suffered from clinical reflux (Figure 3). No cases of Barrett’s esophagus were found. One patient with Gerd Q > 7 didn’t perform endoscopy at the end of our study. Eight patients received oral PPI therapy for 4 or 8 weeks during the follow-up.
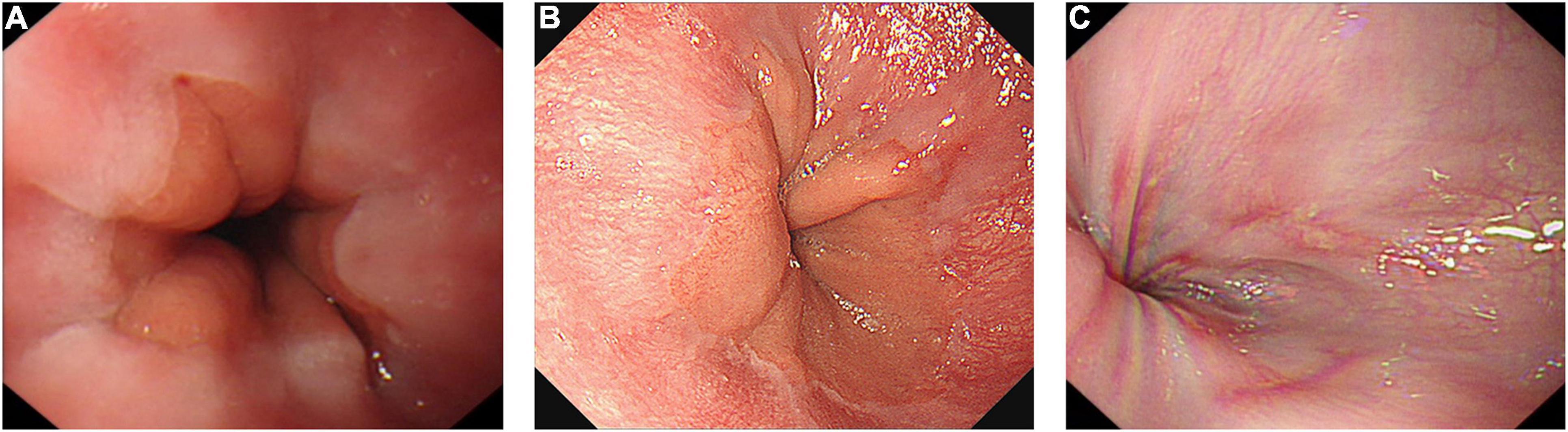
Figure 3. Postoperative endoscopy with a minimum follow-up of 5 years. (A) No abnormality. (B) Reflux esophagitis (Los Angeles Type A). (C) Reflux esophagitis (Los Angeles Type B).
Discussion
In the present study, our result mainly indicated that POEM provided satisfactory long-term safety and efficacy for pediatric patients with achalasia. These data add to a growing body of evidence, much of which comes from the adult population. In the 10 years since POEM was performed, many studies have shown POEM resulted in a durable long-term symptomatic relief for 83–93% of adult patients with achalasia (28, 29). Previous studies have indicated that POEM has a short-term benefit in children patients, with a median follow-up duration of about 13.2–40 months (14–20). Pediatric patients assume a longer life expectancy, the long-term therapeutic effect for them is particularly crucial. However, owing to the low incidence of pediatric achalasia, the long-term efficacy of POEM in children is vague. In our study, we retrospectively reviewed 21 pediatric patients and performed a follow-up with a mean duration of 92.57 months, ranging from 60 to 122 months. To the best of our knowledge, this is the first study to indicate the safety and efficacy of POEM for pediatric achalasia with a minimum follow-up of 5 years.
In our research, all the pediatric patients with preoperative dysphagia and regurgitation reported improved or resolved symptoms at 5-years follow-up. All of them were free from the further intervention for achalasia after POEM. The total long-term clinical success rate was 95.8%. This good outcome of POEM in children suggested superior to that in Heller’s myotomy and balloon dilatation (30, 31). Children tend to have better treatment outcomes than adults, compared with a 5-year long-term success rate of 80–83% for adults (28, 29). This may be attributed to persistent eating disorders that can cause developmental delays in children, they earned more attention than adults, and their LES structure may be more malleable. The mean Eckardt score at each follow-up point showed a gradual and slight worsening of symptoms in pediatric patients beginning in the second year. A similar trend can be seen in the long-term follow-up study of adult POEMs (28). Success rates for balloon dilation and Heller myotomy also showed a gradual decline in a randomized controlled study (32). All of these results indicate the progression of achalasia symptoms requires careful monitoring and evaluation. Noteworthy, besides weight loss, failure to gain weight is an important aspect in assessing the severity of achalasia in pediatrics. Therefore, we recommend that physicians pay attention to growth indicators in children with achalasia.
It is well known that prior treatment may induce submucosal fibrosis, increasing the technical difficulty of subsequent myotomy and thus increasing the time of surgery and the risk of severe AEs. For the patient with treatment history, we performed an opposite myotomy avoiding the previous myotomy site or cutting the fibrotic tissue; details have been elaborated in our earlier research (33). In the present study, two patients who received prior treatment had significant symptoms of remission and reduced LES pressure after performing POEM and were satisfied with their life quality at present. Although one patient who underwent previously Heller myotomy had reflux (Gerd Q = 12) and esophagitis on gastroscopy at 5 years follow-up, the symptoms were relieved with an 8-week oral PPI and Eckardt score was 3. This result extends those from previous studies (34) and provides additional evidence in children that POEM has an excellent long-term efficacy for more than 5 years as a remedial treatment.
Moreover, the POEM procedure is relatively complicated, and it is perhaps more difficult in the pediatric population. In our experience, there are several key points to the success of pediatric POEM. Above all, the operator should be an expert with rich experience in endoscopic submucosal dissection, who can skillfully operate endoscopes and deal with possible complications. It would be better the operator had experience in adult POEM before performing pediatric POEM. Secondly, the operation should be performed as early as possible before significant esophageal dilation or distortion develops. Thirdly, submucosal injection into the esophageal cavity with a mixed solution containing indigo can be used to preset tunnel routes to ensure a straight tunnel into the proximal stomach. Fourthly, intraoperative mucosal integrity should be maintained and metal clips would be used if necessary.
Gastroesophageal reflux disease (GERD) is the most concerning complication after POEM in consideration of it does not include antireflux procedure as is typically performed during Heller’s myotomy. In our study, the 5-year long-term consequences of clinical reflux, symptomatic reflux, and esophagitis arising after POEM are 12.5, 23.8, and 18.8%, respectively, which was comparable to Chen’s result, who found the overall clinical reflux adverse event rates were 19.2% in children (14). In a recent study, Nabi et al. found erosive esophagitis was detected in 55% of children at 3 months post-procedure (19). This difference may be related to GERD subjective and objective measurements. Additionally, pediatric patients are received more attention from parents and doctors. They were placed on medical therapy if they had evidence of GERD; thus, the incidence of GERD may be controlled in long-term follow-up. Long-term surveillance endoscopy after treatment for achalasia showed that those patients may develop erosive esophagitis, Barrett’s esophagus, and even esophageal adenocarcinoma (28, 35, 36). These results indicated routine surveillance for GERD after POEM should be recommended in pediatric achalasia as well. In our study cohort, no dysplasia or malignancy was identified yet. However, follow-up over decades, even life-long, is warranted in future studies.
At the study time, most patients were over 16 years old. Thence, the Urbach Scale was applied to assess patients’ long-term quality of life via face-to-face visits or phone contacts. The only adolescent patient had completed the QoL questionnaire with the help of parents. Majority of the patients in whom at least 5 years had elapsed since POEM are satisfied with their health regarding achalasia. POEM could result in a good adult quality of life for pediatric patients.
Several factors could limit the extent to which the results can be generalized in our study. First of all, our sample size was small and the mean age was slightly older. This shortage is due to achalasia being less common in children than adults, and younger children tend to receive treatment in children’s hospitals in China. Besides, despite these operations being performed by our most experienced endoscopist, children included still present our initial experience with the procedure. According to the POEM learning curve (37), The results could change as the number of surgeries increases. Third, although we emphasized the importance of long-term monitoring for achalasia in children, some patients were not reviewed by endoscopy and manometry. None of them were willing to take a 24-h PH test. Therefore, the incidence of reflux esophagitis is likely to be misestimated.
In summary, peroral endoscopic myotomy could lead to a favorable long-term efficacy in most childhood achalasia and little need for renewed intervention. Future, a multi-center prospective study with a large sample size is required.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committee of the Second Xiangya Hospital of Central South University. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin. Written informed consent was obtained from the individual(s), and minor(s)’ legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author Contributions
DP designed the study protocol, and took part in the collection of data and writing the manuscript. YT shared in designing the study protocol, data collection, and manuscript revision. CJL shared in the collection of data and statistical analysis. LL, HZ, CBL shared in the description of detailed operation steps and picture collecting. RL and DL conceived the original idea, supervised the project, and contributed to all phases of the article. All authors contributed to the manuscript and approved the submitted version.
Funding
This work was supported by the National Natural Science Foundation of China (No. 81900501) and the Natural Science Foundation of Hunan Province (Nos. 2019JJ50868 and 2020JJ5812).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2022.845103/full#supplementary-material
References
1. Mayberry JF, Mayell MJ. Epidemiological study of achalasia in children. Gut. (1988) 29:90–3. doi: 10.1136/gut.29.1.90
2. Smits M, van Lennep M, Vrijlandt R, Benninga M, Oors J, Houwen R, et al. Pediatric achalasia in the Netherlands: incidence, clinical course, and quality of life. J Pediatr. (2016) 169:110–5.e3. doi: 10.1016/j.jpeds.2015.10.057
3. Marlais M, Fishman JR, Fell JME, Haddad MJ, Rawat DJ. UK incidence of achalasia: an 11-year national epidemiological study. Arch Dis Child. (2011) 96:192–4. doi: 10.1136/adc.2009.171975
4. Ip KS, Cameron DJ, Catto-Smith AG, Hardikar W. Botulinum toxin for achalasia in children. J Gastroenterol Hepatol. (2000) 15:1100–4.
5. Hurwitz M, Bahar RJ, Ament ME, Tolia V, Molleston J, Reinstein LJ, et al. Evaluation of the use of botulinum toxin in children with achalasia. J Pediatr Gastroenterol Nutr. (2000) 30:509–14. doi: 10.1097/00005176-200005000-00009
6. Di Nardo G, Rossi P, Oliva S, Aloi M, Cozzi DA, Frediani S, et al. Pneumatic balloon dilation in pediatric achalasia: efficacy and factors predicting outcome at a single tertiary pediatric gastroenterology center. Gastrointest Endosc. (2012) 76:927–32. doi: 10.1016/j.gie.2012.06.035
7. Franklin AL, Petrosyan M, Kane TD. Childhood achalasia: a comprehensive review of disease, diagnosis and therapeutic management. World J Gastrointest Endosc. (2014) 6:105–11. doi: 10.4253/wjge.v6.i4.105
8. Tashiro J, Petrosyan M, Kane TD. Current management of pediatric achalasia. Transl Gastroenterol Hepatol. (2021) 6:33. doi: 10.21037/tgh-20-215
9. Zagory JA, Golden JM, Demeter NE, Nguyen Y, Ford HR, Nguyen NX. Heller myotomy is superior to balloon dilatation or botulinum injection in children with achalasia: a two-center review. J Laparoendosc Adv Surg Tech A. (2016) 26:483–7. doi: 10.1089/lap.2015.0435
10. van Lennep M, van Wijk MP, Omari TIM, Salvatore S, Benninga MA, Singendonk MMJ, et al. Clinical management of pediatric achalasia: a survey of current practice. J Pediatr Gastroenterol Nutr. (2019) 68:521–6. doi: 10.1097/MPG.0000000000002221
11. Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. (2010) 42:265–71. doi: 10.1055/s-0029-1244080
12. Bechara R, Ikeda H, Inoue H. Peroral endoscopic myotomy: an evolving treatment for achalasia. Nat Rev Gastroenterol Hepatol. (2015) 12:410–26. doi: 10.1038/nrgastro.2015.87
13. Werner Y, Hakanson B, Martinek J, Repici A, von Rahden B, Bredenoord A, et al. Endoscopic or surgical myotomy in patients with idiopathic achalasia. N Engl J Med. (2019) 381:2219–29. doi: 10.1056/NEJMoa1905380
14. Chen WF, Li QL, Zhou PH, Yao LQ, Xu MD, Zhang YQ, et al. Long-term outcomes of peroral endoscopic myotomy for achalasia in pediatric patients: a prospective, single-center study. Gastrointest Endosc. (2015) 81:91–100. doi: 10.1016/j.gie.2014.06.035
15. Miao S, Wu J, Lu J, Wang Y, Tang Z, Zhou Y, et al. Peroral endoscopic myotomy in children with achalasia: a relatively long-term single-center study. J Pediatr Gastroenterol Nutr. (2018) 66:257–62. doi: 10.1097/MPG.0000000000001675
16. Tan Y, Zhu H, Li C, Chu Y, Huo J, Liu D. Comparison of peroral endoscopic myotomy and endoscopic balloon dilation for primary treatment of pediatric achalasia. J Pediatr Surg. (2016) 51:1613–8. doi: 10.1016/j.jpedsurg.2016.06.008
17. Li C, Tan Y, Wang X, Liu D. Peroral endoscopic myotomy for treatment of achalasia in children and adolescents. J Pediatr Surg. (2015) 50:201–5. doi: 10.1016/j.jpedsurg.2014.10.017
18. Liu Z, Wang Y, Fang Y, Huang Y, Yang H, Ren X, et al. Short-term safety and efficacy of peroral endoscopic myotomy for the treatment of achalasia in children. J Gastroenterol. (2020) 55:159–68. doi: 10.1007/s00535-019-01607-4
19. Nabi Z, Ramchandani M, Chavan R, Darisetty S, Kalapala R, Shava U, et al. Outcome of peroral endoscopic myotomy in children with achalasia. Surg Endosc. (2019) 33:3656–64. doi: 10.1007/s00464-018-06654-1
20. Choné A, Familiari P, von Rahden B, Desai P, Inoue H, Shimamura Y, et al. Multicenter evaluation of clinical efficacy and safety of per-oral endoscopic myotomy in children. J Pediatr Gastroenterol Nutr. (2019) 69:523–7. doi: 10.1097/MPG.0000000000002432
21. Zhong C, Tan S, Huang S, Peng Y, Lü M, Tang X. Clinical outcomes of peroral endoscopic myotomy for achalasia in children: a systematic review and meta-analysis. Dis Esophagus. (2021) 34:doaa112. doi: 10.1093/dote/doaa112
22. Eckardt VF. Clinical presentations and complications of achalasia. Gastrointest Endosc Clin N Am. (2001) 11:281–92, vi.
23. Nabi Z, Reddy DN, Ramchandani M. Adverse events during and after per-oral endoscopic myotomy: prevention, diagnosis, and management. Gastrointest Endosc. (2018) 87:4–17. doi: 10.1016/j.gie.2017.09.029
24. Jones R, Junghard O, Dent J, Vakil N, Halling K, Wernersson B, et al. Development of the GerdQ, a tool for the diagnosis and management of gastro-oesophageal reflux disease in primary care. Aliment Pharmacol Ther. (2009) 30:1030–8. doi: 10.1111/j.1365-2036.2009.04142.x
25. Jonasson C, Wernersson B, Hoff DA, Hatlebakk JG. Validation of the GerdQ questionnaire for the diagnosis of gastro-oesophageal reflux disease. Aliment Pharmacol Ther. (2013) 37:564–72. doi: 10.1111/apt.12204
26. Chiu JY, Wu JF, Ni YH. Correlation between gastroesophageal reflux disease questionnaire and erosive esophagitis in school-aged children receiving endoscopy. Pediatr Neonatol. (2014) 55:439–43. doi: 10.1016/j.pedneo.2014.01.004
27. Urbach DR, Tomlinson GA, Harnish JL, Martino R, Diamant NE. A measure of disease-specific health-related quality of life for achalasia. Am J Gastroenterol. (2005) 100:1668–76. doi: 10.1111/j.1572-0241.2005.50141.x
28. Teitelbaum EN, Dunst CM, Reavis KM, Sharata AM, Ward MA, DeMeester SR, et al. Clinical outcomes five years after POEM for treatment of primary esophageal motility disorders. Surg Endosc. (2018) 32:421–7. doi: 10.1007/s00464-017-5699-2
29. McKay SC, Dunst CM, Sharata AM, Fletcher R, Reavis KM, Bradley DD, et al. POEM: clinical outcomes beyond 5 years. Surg Endosc. (2021) 35:5709–16. doi: 10.1007/s00464-020-08031-3
30. Saliakellis E, Thapar N, Roebuck D, Cristofori F, Cross K, Kiely E, et al. Long-term outcomes of Heller’s myotomy and balloon dilatation in childhood achalasia. Eur J Pediatr. (2017) 176:899–907. doi: 10.1007/s00431-017-2924-x
31. Jarzebicka D, Czubkowski P, Sieczkowska-Golub J, Kierkus J, Kowalski A, Stefanowicz M, et al. Achalasia in children-clinical presentation, diagnosis, long-term treatment outcomes, and quality of life. J Clin Med. (2021) 10:3917. doi: 10.3390/jcm10173917
32. Moonen A, Annese V, Belmans A, Bredenoord AJ, Bruley des Varannes S, Costantini M, et al. Long-term results of the European achalasia trial: a multicentre randomised controlled trial comparing pneumatic dilation versus laparoscopic Heller myotomy. Gut. (2016) 65:732–9. doi: 10.1136/gutjnl-2015-310602
33. Tan Y, Li C, Yan J, Long L, Huo J, Liu D. Difficult peroral endoscopic myotomy: definition and management strategies. Expert Rev Gastroenterol Hepatol. (2019) 13:933–42. doi: 10.1080/17474124.2019.1674648
34. Nabi Z, Ramchandani M, Darisetty S, Kotla R, Reddy DN. Impact of prior treatment on long-term outcome of peroral endoscopic myotomy in pediatric achalasia. J Pediatr Surg. (2020) 55:1552–5. doi: 10.1016/j.jpedsurg.2019.07.010
35. Gossage JA, Devitt PG, Watson DI, Myers JC, Jamieson GG, Thompson SK. Surveillance endoscopy at five or more years after cardiomyotomy for achalasia. Ann Surg. (2014) 259:464–8. doi: 10.1097/SLA.0b013e318297ae28
36. Leeuwenburgh I, Scholten P, Caljé TJ, Vaessen RJ, Tilanus HW, Hansen BE, et al. Barrett’s esophagus and esophageal adenocarcinoma are common after treatment for achalasia. Dig Dis Sci. (2013) 58:244–52. doi: 10.1007/s10620-012-2157-9
Keywords: achalasia, pediatric, peroral endoscopic myotomy, POEM, long-term outcomes, endoscopic surgery
Citation: Peng D, Tan Y, Li C, Lv L, Zhu H, Liang C, Li R and Liu D (2022) Peroral Endoscopic Myotomy for Pediatric Achalasia: A Retrospective Analysis of 21 Cases With a Minimum Follow-Up of 5 Years. Front. Pediatr. 10:845103. doi: 10.3389/fped.2022.845103
Received: 29 December 2021; Accepted: 01 March 2022;
Published: 04 April 2022.
Edited by:
Jayanta Samanta, Postgraduate Institute of Medical Education and Research (PGIMER), IndiaReviewed by:
Zaheer Nabi, Asian Institute of Gastroenterology, IndiaShruti Mony, The Johns Hopkins Hospital, Johns Hopkins Medicine, United States
Copyright © 2022 Peng, Tan, Li, Lv, Zhu, Liang, Li and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rong Li, eHlsdWxyQGNzdS5lZHUuY24=; Deliang Liu, ZGVsaWFuZ2xpdUBjc3UuZWR1LmNu
 Dongzi Peng1,2
Dongzi Peng1,2 Liang Lv
Liang Lv Chengbai Liang
Chengbai Liang Rong Li
Rong Li Deliang Liu
Deliang Liu