
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr., 04 April 2022
Sec. Pediatric Critical Care
Volume 10 - 2022 | https://doi.org/10.3389/fped.2022.834746
This article is part of the Research TopicPre-Hospital and Post-Resuscitation Care for Pediatric Cardiac ArrestView all 6 articles
In the pediatric intensive care unit (PICU), cardiac arrest (CA) is rare but results in high rates of morbidity and mortality. A retrospective chart review of 223 patients who suffered from in-PICU CA was analyzed from January 2017 to December 2020. Outcomes at discharge were evaluated using pediatric cerebral performance category (PCPC). Return of spontaneous circulation was attained by 167 (74.8%) patients. In total, only 58 (25%) patients survived to hospital discharge, and 49 (21.9%) of the cohort had good neurologic outcomes. Based on multivariate logistic regression analysis, vasoactive–inotropic drug usage before CA, previous PCPC scale >2, underlying hemato-oncologic disease, and total time of CPR were risk factors associated with poor outcomes. Furthermore, we determined the cutoff value of duration of CPR in predicting poor neurologic outcomes and in-hospital mortality in patients caused by in-PICU CA as 17 and 23.5 min respectively.
Cardiac arrest (CA) is uncommon in children, and the epidemiology of pediatric CA is different from adults. CA is a critical cause of death in children in the hospital especially in the pediatric intensive care unit (PICU). CA is reported in 2–6% of children in the PICU, which is much higher than out-of-hospital arrest (about 8 to 20 annual cases per 100,000 pediatric population) (1–3). Previous studies reported that return of spontaneous circulation (ROSC) after cardiopulmonary resuscitation (CPR) for in-hospital CA (IHCA) is about half of these patients, and ~30% survived to hospital discharge (1, 4, 5).
Previous studies had analyzed the cause and prognostic factors associated with outcomes after IHCA, which included the initial rhythm, duration of CA and CPR, the underlying disease, and where the event attacked (6). Patients in PICU are more likely to develop CA because they are more critically ill. Information on factors associated with prognosis of in-PICU CA can promote improvement in PICU care, which means improving survival with good neurologic outcomes. Analyzing the epidemiological variables and risk/prognostic factors of in-PICU CA is of great importance in developing the better therapeutic strategy and deciding appropriate preventive measures. The aim of the study was to analyze the clinical characteristics and prognostic factors associated with mortality and neurologic outcomes of in-PICU CA.
The study was conducted in the PICU of Chang Gung Hospital in Taiwan. Chang Gung Hospital is a tertiary medical center that received patients transferred from regional hospitals. These data were retrospectively analyzed from January 2017 to December 2020. All records of children aged from 1 month to 18 years who suffered in-PICU CA were included. As defined by the American Heart Association and the American College of Cardiology, CA is the sudden cessation of cardiac activity with clinical presentation, such as unresponsiveness to stimuli, apnea, or bradycardia with heart rate <60 bpm with poor perfusion that required external cardiac compressions and ventilation. The need for informed consent was waived by the Chang Gung Medical Foundation Institutional Review Board. This study was approved by the Ethics Committee of Chang Gung Memorial Hospital (approval no. 202000797B0).
Clinical data include age, birth weight, sex, previous history of CA and neurologic status based on the pediatric cerebral performance category (PCPC), underlying diseases, previous treatment, initial ECG rhythm, time to initiation of CPR, and total time of CPR.
Outcomes including return of spontaneous circulation (ROSC) and PCPC score were collected and analyzed. ROSC was defined as restoration of perfusion and heart rhythm in the absence of external chest compressions for over 20 min. The PCPC scores, ranging from 1 (normal) to 6 (brain dead), were validated to quantify a child's cognitive function after a critical illness or an injury. The investigators judged the PCPC score by reviewing the discharge summaries and outpatient records with the consensus of the pediatric neurologist. Categories 1 to 2 were viewed as good neurological outcomes.
The main outcomes for this study were mortality and neurologic outcomes at hospital discharge.
Univariate analyses were performed using the chi-square test, Fisher's exact test, or Mann–Whitney U-test, as appropriate. Multivariate logistic regression analysis with stepwise selection was conducted to identify independent predictors of main outcomes (mortality and neurologic outcomes). Finally, receiver operating characteristic (ROC) curve analysis was used to define the optimal cutoff values for the clinical parameters that may contribute to the main outcomes. A p-value < 0.05 was considered to be statistically significant. The IBM SPSS Statistics software (version 20.0; SPSS Statistics for Windows, Armonk, NY, USA) was used for all statistical calculations.
In this retrospective observational cohort study, we enrolled patients aged from 1 month to 18 years who suffered in-PICU CA between January 2017 and December 2020. Our PICU is a tertiary intensive care unit with 29 beds for patients aged from 1 month to 18 years. During the study period, there were 2,540 patients admitted in our PICU and a total of 223 (8.7%) in-PICU CA cases were retrieved. The return of spontaneous circulation was attained by 167 (74.8%) patients. In total, only 58 (25%) patients survived to hospital discharge, and 49 (84.4%) of the survivors had a good neurologic outcomes (Figure 1).
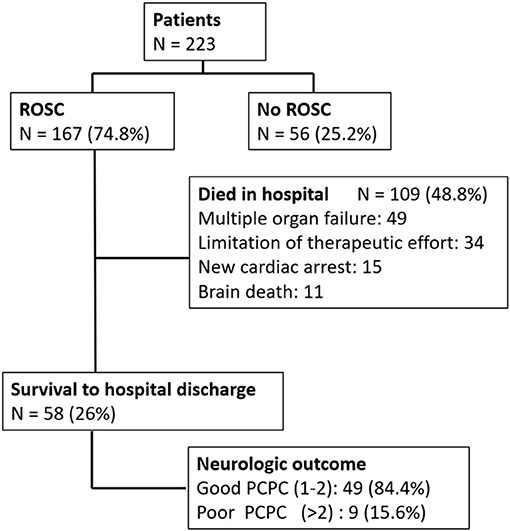
Figure 1. Algorithm of in-PICU CA. ROSC, return of spontaneous circulation; PCPC, pediatric cerebral performance category.
Table 1 reports the patients' neurologic outcomes and mortality rate of different characteristics. Most patients are aged from 1 to 12 months old (65.5% of the cohort). In all, 79.8% of these patients had an underlying disease. Patients with hemato-oncology disease had higher mortality, and patients with respiratory and neurological disease presented lower mortality.
One hundred ninety-three patients (86.5%) have good neurologic status (PCPC score of 1 or 2) prior to CA. After the CA event, 74.6% of the 193 patients developed to poor neurologic outcomes.
As for previous treatment, the patients who received vasoactive–inotropic and bicarbonate had significantly higher mortality rate than those who did not receive such drugs.
The two main etiology of CA were respiratory and cardiac disease. The rate of poor outcome was significantly higher in patients caused by sepsis.
In 90.5% of the cohort, CPR was initiated within 1 min after CA developed. Bradycardia (69%) was the most common cardiac rhythm, and only 13 patients (5.8%) presented with shockable rhythm.
CPR < 5 min accounted for the most proportion, and the longer CPR duration is associated with higher mortality.
Multivariate logistic regression analysis was performed to investigate the impact of multiple risk factors in predicting poor neurologic outcome at discharge and in-hospital mortality. In the final model, only vasoactive–inotropic drug usage before CA, total time of CPR, and previous PCPC scale >2 remained as the independent predictors of poor neurologic outcome at discharge (Table 2). As for the risk factors of in-hospital mortality, only vasoactive–inotropic drug usage before CA, total time of CPR, and underlying hemato-oncologic disease remained as the independent predictors (Table 2).
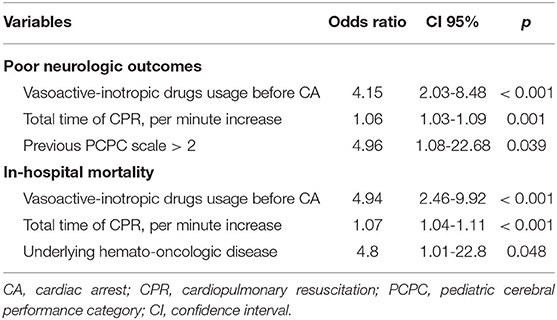
Table 2. Multivariate logistic regression analysis for poor neurologic outcomes and in-hospital mortality.
Figures 2A,B show the area under the ROC curve (AUC) of total time of CPR (min) for predicting poor neurologic outcome and in-hospital mortality. The AUC of total time of CPR (min) was 0.702 (95% CI, 0.627–0.778, p < 0.001) for poor neurologic outcome, and 0.738 (95% CI, 0.669–0.807, p < 0.001) for in-hospital mortality. The best cutoff values of total time of CPR (min) in predicting poor neurologic outcomes and in-hospital mortality are shown in Table 3. We identified total time of CPR (min) of 17 min for predicting poor neurologic outcome and 23.5 min for in-hospital mortality. Furthermore, the specificity was 99% for poor neurologic outcome after CPR for 29.5 min and was 99% for in-hospital mortality after CPR for 30.5 min.

Figure 2. Receiving operating characteristic curve of total time of cardiopulmonary resuscitation (min) for predicting poor neurologic outcome (A) and in-hospital mortality (B).
The occurrence of pediatric CA is rare even in the relatively predictable settings, such as PICU. Previous studies have demonstrated the different rates of ROSC, in-hospital mortality, and neurologic outcome at discharge (Table 4) (7–9). The current study identified that in-PICU CA is associated with high mortality rate (73.9%), which is comparable with a previous study (1, 5, 7, 10). The purpose of the current study was to identify the independent risk factors associated with outcomes after in-PICU CA.
Sustained ROSC attained by 74.8% of patients and 26% of survivors were discharged with 21.9% of patients with good neurologic outcomes. The outcomes of in-PICU CA were better than the CA attacked in other areas, such as CA in the emergency department (6). Our previous study reported that only 4.6% of CA in the ED had a good neurologic outcome at discharge (11). Patients in the PICU received more intensive vital sign monitoring and readiness to recognize CA, then can immediately respond. ED has relative insufficient ability to monitor and stabilize patients competently. Training the medical team and improving the facility to identify and rescue CA quickly outside the PICU can improve the outcome (12, 13).
Previous studies had reported that several underlying diseases of patients before CA had impact on the outcome (7, 14, 15). The current study reported that respiratory patients have better neurologic outcome than those suffering from other disease. Most of the respiratory patients who suffered from CA were caused by obstruction of the airway, usually caused by sputum impaction of the airway or smaller size of the tracheal tube. Therefore, intensive care of the respiratory tract is very important for critically ill patients. Furthermore, patients with hemato-oncology disease had a significantly higher rate of poor neurologic outcome and in-hospital mortality, which was comparable with previous study (14). As for the etiology of CA, respiratory and cardiac diseases were most common, but the etiology of sepsis was the main cause of CA with increased poor neurologic outcome and higher in-hospital mortality in the current study. Sepsis is one of the main causes of admitting in PICU, so, it is important to build protocol for the early detection and resuscitation of sepsis.
Patients who received mechanical ventilation before CA did not suffer from higher morbidity and mortality. It may be because those in-PICU CA patients progress rapidly and did not need further respiratory exercise during CPR. Additionally, vasoactive–inotropic drug usage before CA was the independent risk factor associated with poor neurologic outcome and in-hospital mortality (16–19). Patients who need vasoactive–inotropic drugs indicating critical illness and hemodynamic disturbances, despite receiving intensive care, still had significantly higher morbidity and mortality.
Longer CPR duration after CA was a well-established risk factor associated with poor outcome, and previous studies identified CPR for more than 10 min as a prognostic risk factor (14, 15, 17, 18). Despite CPR for more than 10 min indicating poor prognosis, discontinuing resuscitation after CPR for 10 min seems to be too short. Deciding on the adequate duration of CPR before stopping resuscitation efforts in-PICU CA is a difficult subject, which needs the balancing of capability of the medical team, the family members' feelings, especially the probability of yielding extra morbidity. Therefore, we determined the cutoff value of the duration of CPR in predicting poor neurologic outcomes and in-hospital mortality in patients caused by in-PICU CA as 17 and 23.5 min, respectively, based on the ROC analysis. Furthermore, CPR for 29.5 and 30.5 min had about a 99% probability of poor neurologic outcome and in-hospital mortality, respectively. This information about CPR duration associated with poor prognosis can be used as a reference for some patients with extremely poor prognosis whether the resuscitation should be continued or stopped. Extracorporeal life support may be premediated for some patients with possible reversible disease, while they were not sustained ROSC (20–22). Further prospective studies are warranted to establish the guidelines.
1The current study has several limitations. First, this study was conducted at a single center with a retrospective design. Therefore, there is a risk of information bias, but we included a relative large patient number within the recent 3 years, which may be able to reduce the bias potentially. Second, the current study did not analyze the initial severity of illness at admission in the PICU, but other studies reported that there was no association between the initial severity of illness and the outcome of in-PICU CA (23). Third, rescue with extracorporeal membrane oxygenation (ECMO) during CPR was seldom performed in our PICU. Only two patients received ECMO CPR rescue caused by cardiac disease with a 50% mortality. ECMO CPR rescue may be considered for some patients with reversible disease but are insensitive to conventional CPR (18, 22). Further prospective studies are warranted to establish guidelines. Fourth, the quality of CPR performance is associated with prognosis that a high-quality of CPR is associated with better outcomes (24). A high-quality of CPR involves appropriate chest compression rate, proper chest compression depth, complete chest recoil, and minimization of compression interruptions, which were not analyzed in the current study.
About one in five patients who suffered from in-PICU CA had good neurologic outcome, which had improved compared with previous studies. Several factors were associated with prognosis after in-PICU CA, such as vasoactive–inotropic drug usage before CA, previous PCPC scale >2, underlying hemato-oncologic disease, and total time of CPR. Furthermore, we determined the cutoff value of duration of CPR in predicting poor neurologic outcomes and in-hospital mortality in patients caused by in-PICU CA as 17 and 23.5 min, respectively.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by the Institutional Review Board and Ethics Committee of Chang Gung Memorial Hospital. Written informed consent from the participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
E-PL and H-PW conceived and designed the study. O-WC and J-JL participated in the data analysis. O-WC and S-HH gathered the data. E-PL drafted the manuscript. H-PW designed, oversaw the study, interpreted the data, and revised the manuscript. All authors have read and approved the final manuscript for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We thank the statistician in Chang-Gung Memorial Hospital for completing the statistical analysis.
1. Suominen P, Olkkola KT, Voipio V, Korpela R, Palo R, Räsänen J. Utstein style reporting of in-hospital paediatric cardiopulmonary resuscitation. Resuscitation. (2000) 45:17–25. doi: 10.1016/S0300-9572(00)00167-2
2. Young KD, Gausche-Hill M, McClung CD, Lewis RJ. A prospective, population-based study of the epidemiology and outcome of out-of-hospital pediatric cardiopulmonary arrest. Pediatrics. (2004) 114:157–64. doi: 10.1542/peds.114.1.157
3. Donoghue AJ, Nadkarni V, Berg RA, Osmond MH, Wells G, Nesbitt L, et al. CanAm pediatric cardiac arrest investigators: out-of-hospital pediatric cardiac arrest: an epidemiologic review and assessment of current knowledge. Ann Emerg Med. (2005) 46:512–22. doi: 10.1016/j.annemergmed.2005.05.028
4. Nadkarni VM, Larkin GL, Peberdy MA, Carey SM, Kaye W, Mancini ME, et al. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA. (2006) 295:50. doi: 10.1001/jama.295.1.50
5. Samson RA, Nadkarni VM, Meaney PA, Carey SM, Berg MD, Berg RA, et al. Outcomes of in-hospital ventricular fibrillation in children. N Engl J Med. (2006) 354:2328. doi: 10.1056/NEJMoa052917
6. Donoghue AJ, Nadkarni VM, Elliott M, Durbin D American Heart Association National Registry of Cardiopulmonary Resuscitation Investigators. Effect of hospital characteristics on outcomes from pediatric cardiopulmonary resuscitation: a report from the national registry of cardiopulmonary resuscitation. Pediatrics. (2006) 118:995–1001. doi: 10.1542/peds.2006-0453
7. Meaney PA, Nadkarni VM, Cook EF, Testa M, Helfaer M, Kaye W, et al. Higher survival rates among younger patients after pediatric intensive care unit cardiac arrests. Pediatrics. (2006) 118:2424–33. doi: 10.1542/peds.2006-1724
8. Moreno RP, Vassallo JC, Sáenz SS, Blanco AC, Allende D, Araguas JL, et al. Cardiopulmonary resuscitation in nine pediatric intensive care units of the Argentine Republic. Arch Argent Pediatr. (2010) 108:216–25. doi: 10.1590/S0325-00752010000300007
9. Berens RJ, Cassidy LD, Matchey J, Campbell D, Colpaert KD, Welch T, et al. Probability of survival based on etiology of cardiopulmonary arrest in pediatric patients. Paediatr Anaesth. (2011) 21:834–40. doi: 10.1111/j.1460-9592.2010.03479.x
10. Reis AG, Nadkarni V, Perondi MB, Grisi S, Berg RA. A prospective investigation into the epidemiology of in-hospital pediatric cardiopulmonary resuscitation using the international Utstein reporting style. Pediatrics. (2002) 109:200. doi: 10.1542/peds.109.2.200
11. Lee J, Yang WC, Lee EP, Huang JL, Hsiao HJ, Lin MJ, et al. Clinical survey and predictors of outcomes of pediatric out-of-hospital cardiac arrest admitted to the emergency department. Sci Rep. (2019) 9:7032. doi: 10.1038/s41598-019-43020-0
12. Sharek PJ, Parast LM, Leong K, Coombs J, Earnest K, Sullivan J, et al. Effect of a rapid response team on hospital-wide mortality and code rates outside the ICU in a children's hospital. JAMA. (2007) 298:2267–74. doi: 10.1001/jama.298.19.2267
13. Tibballs J, Kinney S. Reduction of hospital mortality and of preventable cardiac arrest and death on introduction of a pediatric medical emergency team. Pediatr Crit Care Med. (2009) 10:306–12. doi: 10.1097/PCC.0b013e318198b02c
14. Del Castillo J, López-Herce J, Cañadas S, Matamoros M, Rodríguez-Núnez A., Rodríguez-Calvo A, et al. Cardiac arrest and resuscitation in the pediatric intensive care unit: a prospective multicenter multinational study. Resuscitation. (2014) 85:1380–6. doi: 10.1016/j.resuscitation.2014.06.024
15. López-Herce J, Del Castillo J, Matamoros M, Cañadas S, Rodriguez-Calvo A, Cecchetti C, et al. Factors associated with mortality in pediatric in hospital cardiac arrest: a prospective multicenter multinational observational study. Intensive Care Med. (2013) 39:309–18. doi: 10.1007/s00134-012-2709-7
16. Rodríguez-Núñez A, López-Herce J, García C, Carrillo A, Domínguez P, Calvo C, et al. Effectiveness and long-term outcome of cardiopulmonary resuscitation in paediatric intensive care units in Spain. Resuscitation. (2006) 71:301–9. doi: 10.1016/j.resuscitation.2005.11.020
17. De Mos N, van Litsenburg RR, McCrindle B, Bohn DJ, Parshuram CS. Pediatric in-intensive-care-unit cardiac arrest: incidence, survival, and predictive factors. Crit Care Med. (2006) 34:1209–15. doi: 10.1097/01.CCM.0000208440.66756.C2
18. Wu ET, Li MJ, Huang SC, Wang CC, Liu YP, Lu FL, et al. Survey of outcome of CPR in pediatric in hospital cardiac arrest in a medical center in Taiwan. Resuscitation. (2009) 80:443–8. doi: 10.1016/j.resuscitation.2009.01.006
19. Tian J, Kaufman DA, Zarich S, Chan PS, Ong P, Amoateng-Adjepong Y, et al. Outcomes of critically ill patients who received cardiopulmonary resuscitation. Am J Respir Crit Care Med. (2010) 182:501–6. doi: 10.1164/rccm.200910-1639OC
20. Alsoufi B, Al-Radi OO, Nazer RI, Gruenwald C, Foreman C, Williams WG, et al. Survival outcomes after rescue extracorporeal cardiopulmonary resuscitation in pediatric patients with refractory cardiac arrest. J Thorac Cardiovasc Surg. (2007) 134:952–59. doi: 10.1016/j.jtcvs.2007.05.054
21. Thiagarajan RR, Laussen PC, Rycus PT, Bartlett RH, Bratton SL. Extracorporeal membrane oxygenation to aid cardiopulmonary resuscitation in infants and children. Circulation. (2007) 116:1693–700. doi: 10.1161/CIRCULATIONAHA.106.680678
22. Huang SC, Wu ET, Chen YS, Chang CI, Chiu IS, Wang SS, et al. Extracorporeal membrane oxygenation rescue for cardiopulmonary resuscitation in pediatric patients. Crit Care Med. (2008) 36:1607–13. doi: 10.1097/CCM.0b013e318170b82b
23. Serrano M, Rodríguez J, Espejo A, del Olmo R, Llanos S, Del Castillo J, et al. Relationship between previous severity of illness and outcome of cardiac arrest in hospital. An Pediatr (Barc). (2013) 81:9–15. doi: 10.1016/j.anpedi.2013.09.018
Keywords: resuscitation, mortality, pediatric intensive care unit, cardiac arrest, neurologic outcome
Citation: Lee E-P, Chan O-W, Lin J-J, Hsia S-H and Wu H-P (2022) Risk Factors and Neurologic Outcomes Associated With Resuscitation in the Pediatric Intensive Care Unit. Front. Pediatr. 10:834746. doi: 10.3389/fped.2022.834746
Received: 13 December 2021; Accepted: 01 February 2022;
Published: 04 April 2022.
Edited by:
Yan Ren Lin, Changhua Christian Hospital, TaiwanReviewed by:
Guoping Lu, Fudan University, ChinaCopyright © 2022 Lee, Chan, Lin, Hsia and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Han-Ping Wu, YXJ0aHVyMTIyNkBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.