
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
POLICY AND PRACTICE REVIEWS article
Front. Pediatr. , 05 April 2022
Sec. Pediatric Nephrology
Volume 10 - 2022 | https://doi.org/10.3389/fped.2022.833611
This article is part of the Research Topic Insights in Pediatric Nephrology: 2021 View all 4 articles
 Franca M. Iorember1*†
Franca M. Iorember1*† Oluwatoyin F. Bamgbola2†
Oluwatoyin F. Bamgbola2†The population of children living in poverty and lacking healthcare insurance has increased in the United States of America in the last decade. Several factors have been responsible for this trend including illegal immigration, socioeconomic deprivation, young age, racial segregation, environmental degradation, and discriminatory housing policies. These systemic barriers have contributed to the exclusion of families from essential healthcare services. They are also contributory to the development of chronic illnesses (such as dialysis-dependent kidney disease) that are debilitating and frequently require considerable therapeutic resources. This unfortunate scenario creates a never-ending vicious cycle of poverty and diseases in a segment of society. For pediatric nephrologists, the challenges of caring for uninsured children with chronic kidney disease are all too familiar. Federally funded healthcare programs do not cover this patient population, leaving them the option of seeking care in emergency healthcare settings. Presentation with a critical illness often necessitates urgent placement of vascular catheters and the choice of acute hemodialysis. Adverse social environment influences the need for protracted chronic hemodialysis and a delay in kidney transplantation. Consequently, there is greater comorbidity, recurrent hospitalization, and a higher mortality rate. New policies should address the deficit in health insurance coverage while promoting social programs that will remove structural barriers to health care resources for undocumented children and young adults.
The last decade has seen an increase in the number of people including children and young adults living in poverty and consequently without health insurance coverage in the United States of America. A report released by the United States Census Bureau in September 2020 showed a 1% increase in the number of persons living in poverty between the years 2019 and 2020. The largest increase was seen in the Black and Hispanic populations (1). Similarly, there was a 0.1-point increase in the number of uninsured people from 2018 to 2020. Amongst the poor, the percentage of uninsured children, rose from 7.8% in 2018 to 9.3% in 2020. The largest increase was again seen in Black, Hispanic, foreign-born and non-citizen children (1). In a report by the Georgetown Center for Children and Families, there was an increase of more than 400,000 in the number of uninsured children between 2016 and 2018, with the largest increase observed in Latino and White children (2). Access to specialty healthcare has been shown to be directly linked to health insurance status of children, with uninsured children having poorer access to specialty care, compared to insured children (3).
Federal and State health insurance programs are intentionally designed for children and adults who are documented and lawfully residing in the United States (4). These programs do not make provision for undocumented families, the majority of whom are immigrant families. This increases the likelihood that children in these families will seek care in emergency care settings (5–9). The authors are all too familiar with children presenting to the emergency room with kidney failure and a late diagnosis of kidney disease. In nearly all cases, these children have not been seen by a primary care physician in many years. The principal objective of this article is to enhance community awareness on the scope of health care disparities among children and young adults with chronic kidney disease (CKD). We shall explore the social, cultural, and economic determinants of inadequate access to optimal kidney health care services. We shall also discuss the role of lack of health insurance on the promotion of CKD and offer recommendations on meaningful strategies to improve access to kidney health services in this population.
Lack of health insurance is detrimental to health and has been shown in adult studies to be associated with increased odds of dying (10). In children, a recent study examining the sociodemographic risk factors for pediatric acute kidney injury [AKI] showed that children who lacked insurance were more likely to be admitted to hospital with AKI (11). It is well established that children with AKI are at risk for the development of CKD later on. Disadvantaged socioeconomic status in early childhood, and by implication, a higher likelihood of being uninsured, translates to a higher risk of kidney disease and end stage kidney disease [ESKD] in later life (12). Lack of insurance means that children are more likely to experience delays in seeking medical care and a higher likelihood of presentation to the emergency department for needed healthcare services (13). Anecdotal reports suggest that children with kidney disease who do not have health insurance coverage often present to the emergency department in kidney failure. Adult literature is robust with reports of patients with kidney failure depending on the emergency department for chronic hemodialysis services and the resultant implications on cost and mortality (14–16). Moreover, the higher cost of care in the emergency department translates to higher individual and national healthcare costs which drives poverty at the individual level and promotes national disparities in healthcare delivery (17, 18). Health problems associated with lack of insurance in childhood could lead to delays in the attainment of developmental milestones, which impacts productivity later in life.
Patients with CKD have extensive healthcare needs and significant financial burdens (19, 20). While it is difficult to accurately estimate the cost of care of non-dialysis dependent CKD, expenses associated with dialysis and kidney transplant services are traceable and enormous, and without insurance coverage, patients are likely to suffer serious adverse outcomes. A recent retrospective analysis of children undergoing conventional hemodialysis showed mean monthly cost estimates of $3,500, adding up to $87,000 in 40 months. For children who have undergone kidney transplantation, mean monthly costs were estimated at $1,900, adding up to $48,000 in 50 months (21). The 2021 United States Renal Data System (USRDS) annual report provides information on spending associated with pre-dialysis care. For commercially insured children, the cost of caring for children with CKD was $20,764 per person per year (PPPY), compared to $2,092 for children without CKD (19). These estimates do not account for self-pay and other forms of payment for services. In 2018, the USRDS estimates of the Medicare spending for beneficiaries of non-dialysis dependent CKD younger than 66 years exceeded $ 11 billion. For all patients with ESKD, a total spending estimate of $ 49 billion was reported for the same year (19).
Although Medicare pays for dialysis and transplant services for children with ESKD, coverage is dependent upon meeting certain eligibility criteria. This includes being the dependent child of a parent who is eligible for social security benefits, who has worked the required time under social security, or who is a government employee and by implication, lawfully residing in the United States. Until recently, coverage for children who received a kidney transplant ended after 36 months, leaving families and patients with the financial burden of paying for vital immunosuppressive medications. However, in December 2020, the law was changed to provide lifetime Medicare coverage for post kidney transplant immunosuppressive coverage (22).
The costs associated with CKD care may vary depending on the state and the healthcare facility where treatment is received. For patients who do not have insurance coverage, such as undocumented patients, public hospitals and emergency departments become the only access to healthcare services, and costs associated with these services are high (23). While some State Medicaid programs extend coverage to uninsured and undocumented individuals, many States do not. Currently, California, Illinois, Oregon, Massachusetts, New York, and Washington States extend healthcare coverage using state funds to income-eligible children regardless of their immigration status (24, 25).
As a result of the huge costs associated with CKD care, the majority of uninsured and poor patients are less likely to receive crucial pre-dialysis care, presenting late with severe azotemia, requiring urgent initiation of dialysis (23, 26). Moreover, available data shows that immigrant, black and Hispanic children are more likely to receive hemodialysis as a chronic dialysis modality, as compared to their white counterparts (19, 27, 28). Hemodialysis is associated with a lower quality of life in both children and adults compared to peritoneal dialysis (29, 30). Furthermore, uninsured patients are often not eligible for kidney transplantation due to a lack of funding, which means a longer time on dialysis and an increased risk for morbidity and mortality (31). Moreover, when uninsured children receive kidney transplantation out of compassionate care, payment for immunosuppressive medications becomes a challenge, predisposing them to premature graft loss (32, 33).
Multiple structural barriers exist in the American political, socioeconomic and healthcare systems that hinder access to optimal healthcare (Table 1; Figure 1). We shall discuss the permissive role of these factors in the promotion of health disparity and CKD, as well as the adverse consequences on community life.
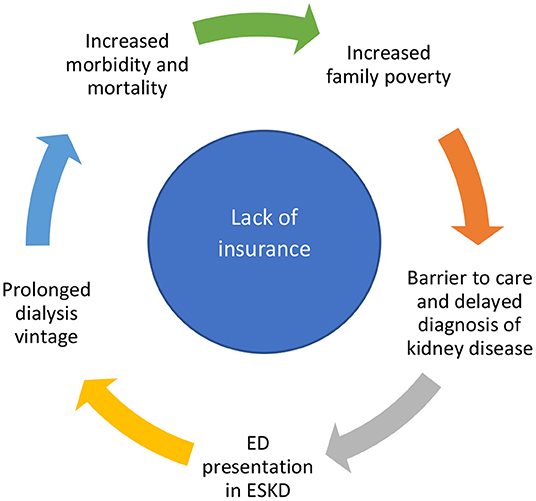
Figure 1. The circle of burden of the uninsured with chronic kidney disease. ED, emergency department; ESKD, end stage kidney disease.
Health disparity occurs in the context of systematic exclusion from adequate access to essential social and clinical services that are often based on racial, ethnic, socioeconomic, political, and religious differences. Other discriminatory factors of historical importance are cognitive dysfunction, physical disability, immigration status, rural geographical location, a younger or older age group, and gender identity or sexual orientation. As a result of expensive but required healthcare services, disparities in the treatment of CKD are particularly profound in marginalized communities. Genetic predisposition (as in APOL1 mutation) and socioeconomic disadvantage may account for the greater risk of developing CKD in Blacks compared with the White population (34, 35). Trend analysis between the year 2005–2014 showed a greater prevalence of diabetic CKD in Blacks and Hispanics compared to the White population (36). Moreover, poverty often leads to poor dietary choices which in turn promotes exogenous obesity and diabetic mellitus (37, 38). The latter is a leading cause of dialysis-dependent CKD in the USA. In a recent report, uninsured children were shown to be more likely to suffer AKI when compared to children with any health insurance (11). Furthermore, apart from promoting socio-economic deprivation, discriminatory housing policies may increase family exposure to environmental kidney toxins such as lead, mercury, cadmium, and arsenic heavy metals (39). Pregnancy may be complicated by adverse psychosocial and biological events including poor prenatal care, nutritional insufficiency, and premature delivery (leading to low nephron mass) that may produce permanent impairment in structural or functional programming of the fetal organs and result in the later development of cardiorenal morbidities (12, 40).
Unfavorable health insurance policy limits access of the socially disadvantaged to kidney subspecialists. Available evidence shows that marginalized population groups (including Blacks, Hispanics, and Asians, some of whom are undocumented) are less likely to receive kidney care in the last 12 months preceding the initiation of chronic dialysis due to lack of insurance coverage (41). Even when they have insurance coverage, the majority of these patients depend on primary care providers (PCP) for kidney-related care as a result of limited access to nephrologists. Unfortunately, there is often suboptimal quality of CKD education during encounters with PCP in the localities in which marginalized populations live (42–44). It is, therefore, necessary to work with community PCP to enhance their knowledge about the nature and complications associated with kidney disease. Our efforts should focus on preventative strategies such as avoiding the use of nephrotoxic medications as much as possible, prompt assessment and treatment of dehydration and infections. Early diagnosis and prompt therapeutic interventions to address morbidity in children living with CKD could also help preserve their kidney function and delay progression to ESKD. In rural areas with limited access to healthcare services, it may be necessary for PCP to share clinical responsibility with kidney specialists who are frequently located in urban environments. The recently available telemedicine resources may facilitate such engagements.
Although lack of health insurance coverage is the single most important barrier to accessing healthcare services, there are other salient contributory factors. The cost of healthcare services is often prohibitive and is mostly unaffordable for low-income families. Insurance plans are offered through a variety of programs including federal coverage through Medicaid and Medicare, employer-based plans, the Veteran's health administration and free- market plans. An understanding of this insurance structure takes concerted efforts and provision of quality education. A profile of the uninsured shows lower educational attainment, poor health literacy, and poverty (1, 45). These adverse social characteristics may be particularly profound among marginalized populations as depicted in Figure 1 (46). The significance of adequate health insurance coverage was demonstrated by a study that examined the impact of the Medicaid expansion program on the risk of kidney disease (47). There was a 3% reduction in the incidence of CKD among young adults in the first 3 years in the States that adopted Medicaid expansion in the USA. The largest benefit of this insurance practice was observed in the non-Hispanic White population. Similar studies looking at the impact of Medicaid expansion have shown improved access to kidney health services (48). The number of children and young adults covered by health insurance has also improved with Medicaid expansion (49, 50). Despite these gains in outcomes, universal health insurance coverage may not be enough to eradicate the disparity in the care of CKD. For instance, although the health insurance policy provided to the United States veterans regardless of ethnicity or social background helped improve access to renal physicians, it did not succeed in erasing the disparities and higher incidence of advanced kidney disease in the marginalized populations (51). Policies targeted at improving health literacy, and eradicating poverty and racism are also necessary.
In October 2018, the Trump administration expanded the definition of “public charge” (defined as an immigrant who has received one or more public benefits for more than 12 months within any 36-month period) to include any immigrant who was likely to receive public benefits in the future. If they were found likely to receive public benefit in the future, they were excluded from getting a green card or visa to the United States. This rule posed a threat to healthcare coverage for immigrants and their families (52). A simulation of the potential harms that would be caused by this rule showed that millions of children would lose healthcare coverage including many with specific medical needs that, if left untreated, could contribute to child deaths and future disability (53). Thankfully, the new public charge regulation was reversed by the Biden administration, in March, 2021, protecting many immigrant children from losing health insurance coverage.
Globalization in the twenty-first century has seen an exponential rise in the transnational migration of people, resulting in changes in socio-economic, political, cultural, and healthcare structures of various geographical regions around the world. Immigrant families are often of ethnic minority and lower socioeconomic status and may therefore endure discriminatory health care policies (54–58). Illegal immigration status has been linked to a lack of insurance policy and a limited ability to access a comprehensive healthcare service (59, 60). Immigrant children are more likely to be uninsured and lack access to healthcare, which increases the likelihood of delays in the diagnosis of their medical conditions, including kidney disease (1, 61). Language disparities also constitute a barrier to accessing healthcare services amongst non-English speaking immigrant families (Table 1). Such ineffective communication invariably compromises the quality of health care delivery, ability to adhere to medical recommendations, and even return for follow-up visits (61–64).
Public anti-immigrant rhetoric limits access to healthcare by instilling fear of deportation, anxiety, and even depression in undocumented immigrants. This scenario frequently results in significant delays in seeking and receiving healthcare services, greater risk for more rapid progression of the disease and an earlier need for initiation of renal replacement therapy in patients with kidney disease (65).
Lower socioeconomic status is a determinant of health problems and has been linked to increased morbidity and mortality, reduced access to healthcare, and poorer health outcomes. Moreover, the absence of medical homes, sedentary lifestyles and poor nutritional quality, invariably promote exogenous obesity, hyperlipidemia, hypertension, diabetes mellitus, and ultimately cardio-renal morbidity (66, 67). A recent meta-analysis showed there was a predictive relationship between a low socioeconomic status and a decline in glomerular filtration rate (GFR) (OR = 1.4; 95% CI = 1.2–1.6), degree of albuminuria (OR = 1.5; 95% CI = 1.2–1.8) and ESKD (OR = 1.5; 95% CI = 1.4–1.7) (68). In another study, families with housing insecurity were shown to have a three-fold greater likelihood of developing incidental kidney disease (69). With reduced access to healthcare services, these individuals are more likely to experience delays in seeking medical intervention.
A remarkable example of how a reversal of adverse social environment (enhanced nutrition and physical exercise) could produce a favorable clinical outcome was demonstrated in the indigenous American community. Introduction of comprehensive indigenous health services to prevent and optimize the care of diabetes mellitus resulted in a 50% reduction in the incidence of ESKD. This intervention led to a decline in the prevalence of ESKD from the highest rate observed in 1996 to a level below that of Black and Hispanic populations by the year 2013 (70).
In summary, there is need for policymakers to re-examine the implications of leaving out certain population groups from insurance coverage. Lack of health insurance may be associated with significant cost implications and put a strain on healthcare expenditures (71). Studies on emergency department (ED) utilization in children show that uninsured children, some of whom may have CKD, are more likely to depend on the ED for their healthcare needs (13). Emergency care services are invariably expensive and contribute to greater financial burden in the healthcare system. Moreover, children with CKD who rely on ED care are more likely to present in severe kidney failure. This late presentation often means that patients are sicker and need more intense and expensive care. A comparison of scheduled vs. emergency-only dialysis in adult undocumented immigrants with ESKD has shown substantial cost savings when dialysis is provided in a planned and scheduled manner (15). Moreover, extending insurance coverage to undocumented immigrants and those who cannot afford to purchase insurance might lead to state and federal cost savings and improve the health of all U.S residents (72–74). Withholding kidney transplantation in children and young adults on dialysis due to an unfunded status is not only unethical but also increases morbidity and mortality. Similarly, providing chronic hemodialysis via a catheter instead of a fistula is fraught with access complications that increase the economic burden of dialysis care.
The root cause of health disparities in CKD in the United States is complex and includes modifiable social determinants such as poverty, poor nutrition, and racial segregation. Policymakers need to address the deficit in essential social programs by providing economic empowerment, improved educational standard, affordable quality food, access to a safe neighborhood, optimal recreational program, and reduction of environmental pollution. In this regard, the recent award of a $500,000 grant by the U.S. Department of Health and Human Services Office of Minority Health to support the collection of health data on community social determinants to address health disparities is a step in the right direction. A universal health insurance policy will minimize delay in seeking medical intervention, reduce the use of vascular catheters, decreases hospitalization rate, promotes the utilization of peritoneal dialysis, and enhance the opportunity for pre-emptive kidney transplantation. The summative effect is a substantial saving in health care cost, increase in human productivity, and a better quality of life for the citizens.
Both authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Bureau UC. Uninsured Rates for Children in Poverty Increased 2018–2020. (2021). Available from: https://www.census.gov/library/stories/2021/09/uninsured-rates-for-children-in-poverty-increased-2018-2020.html (cited 2021 Oct 10).
2. Center For Children Families. The Number of Uninsured Children is on the Rise. (2019). Available from: https://ccf.georgetown.edu/2019/10/29/the-number-of-uninsured-children-in-on-the-rise-acs/ (cited 2022 Jan 08)
3. Skinner AC, Mayer ML. Effects of insurance status on children's access to specialty care: a systematic review of the literature. BMC Health Serv Res. (2007) 7:194. doi: 10.1186/1472-6963-7-194
4. Bojorquez GR, Fry-Bowers EK. Beyond Eligibility: Access to Federal Public Benefit Programs for Immigrant Families in the United States. J Pediatr Health Care. (2019) 33:210–3. doi: 10.1016/j.pedhc.2018.11.004
5. Russell EA, Tsai C, Linton JM. Children in immigrant families: advocacy within and beyond the pediatric emergency department. Clin Pediatr Emerg Med. (2020) 21:100779. doi: 10.1016/j.cpem.2020.100779
6. Samra S, Taira BR, Pinheiro E, Trotzky-Sirr R, Schneberk T. Undocumented patients in the emergency department: challenges and opportunities. West J Emerg Med. (2019) 20:791–8. doi: 10.5811/westjem.2019.7.41489
7. Ku L. Improving health insurance and access to care for children in immigrant families. Ambul Pediatr. (2007) 7:412–20. doi: 10.1016/j.ambp.2007.08.002
8. Hill I, Dubay L, Kenney GM, Howell EM, Courtot B, Palmer L. Improving coverage and access for immigrant Latino children: the Los Angeles healthy kids program. Health Aff (Millwood). (2008) 27:550–9. doi: 10.1377/hlthaff.27.2.550
9. Gushue C, Miller R, Sheikh S, Allen ED, Tobias JD, Hayes D, et al. Gaps in health insurance coverage and emergency department use among children with asthma. J Asthma. (2019) 56:1070–8. doi: 10.1080/02770903.2018.1523929
10. Woolhandler S, Himmelstein DU. The Relationship of Health Insurance and Mortality: Is Lack of Insurance Deadly? Ann Intern Med. (2017) 167:424–31. doi: 10.7326/M17-1403
11. Bjornstad EC, Marshall SW, Mottl AK, Gibson K, Golightly YM, Charles A, et al. Racial and health insurance disparities in pediatrie acute kidney injury in the USA. Pediatr Nephrol. (2020) 35:1085–96. doi: 10.1007/s00467-020-04470-1
12. Brophy PD, Shoham DA, Charlton JR, Carmody JB, Reidy KJ, Harshman L, et al. Early-life course socioeconomic factors and chronic kidney disease. Adv Chronic Kidney Dis. (2015) 22:16–23. doi: 10.1053/j.ackd.2014.06.006
13. Schlichting LE, Rogers ML, Gjelsvik A, Linakis JG, Vivier PM. Pediatric emergency department utilization and reliance by insurance coverage in the United States. Acad Emerg Med. (2017) 24:1483–90. doi: 10.1111/acem.13281
14. Cervantes L, Carr AL, Welles CC, Zoucha J, Steiner JF, Johnson T, et al. The experience of primary caregivers of undocumented immigrants with end-stage kidney disease that rely on emergency-only hemodialysis. J Gen Intern Med. (2020) 35:2389–97. doi: 10.1007/s11606-020-05696-3
15. Nguyen OK, Vazquez MA, Charles L, Berger JR, Quiñones H, Fuquay R, et al. Association of scheduled vs emergency-only dialysis with health outcomes and costs in undocumented immigrants with end-stage renal disease. JAMA Intern Med. (2019) 179:175–83. doi: 10.1001/jamainternmed.2018.5866
16. Raghavan R. Caring for undocumented immigrants with kidney disease. Am J Kidney Dis. (2018) 71:488–94. doi: 10.1053/j.ajkd.2017.09.011
17. Marwick C. Lack of health insurance costs up to $130bn in illness and premature death. BMJ. (2003) 326:1418. doi: 10.1136/bmj.326.7404.1418-f
18. National Academies Press (US). Hidden Costs, Values Lost: Uninsurance in America. Washington (DC) (2003).
19. National Institute of Diabetes and Digestive and Kidney Diseases (U.S.). USRDS Coordinating Center. U.S. Renal Data System … Annual Data Report, Researcher's Guide, Reference Tables, ADR Slides. Ann Arbor MI: National Institute of Diabetes and Digestive and Kidney Diseases U.S. Renal Data System Coordinating Center.
20. Honeycutt AA, Segel JE, Zhuo X, Hoerger TJ, Imai K, Williams D. Medical costs of CKD in the Medicare population. J Am Soc Nephrol. (2013) 24:1478–83. doi: 10.1681/ASN.2012040392
21. Camargo MF de., Barbosa Kd, Fetter SK, Bastos A, Feltran Ld, Koch-Nogueira PC. Cost analysis of substitutive renal therapies in children. J Pediatr (Rio J). (2018) 94:93–9. doi: 10.1016/j.jped.2017.05.004
22. National Kidney Foundation. Expanded Medicare Coverage of Immunosuppressive Drugs for Kidney Transplant Recipients. (2021). Available from: https://www.kidney.org/atoz/content/faq-expanded-medicare-coverage-immunosuppressive-drugs-kidney-transplant-recipients (cited 2022 Jan 09).
23. Douthit NT, Old C. Renal replacement therapy for undocumented immigrants: current models with medical, financial, and physician perspectives—a narrative review. J Gen Intern Med. (2019) 34:2246–53. doi: 10.1007/s11606-019-05237-7
24. KFF. Health Coverage of Immigrants. (2021). Available from: https://www.kff.org/racial-equity-and-health-policy/fact-sheet/health-coverage-of-immigrants/ (cited 2022 Jan 09).
25. Cervantes L, Johnson T, Hill A, Earnest M. Offering better standards of dialysis care for immigrants: the Colorado example. Clin J Am Soc Nephrol. (2020) 15:1516–8. doi: 10.2215/CJN.01190120
26. Williams ME. The ESRD uninsured matter. Adv Chronic Kidney Dis. (2007) 14:67–74. doi: 10.1053/j.ackd.2006.10.013
27. Furth SL, Powe NR, Hwang W, Neu AM, Fivush BA. Racial differences in choice of dialysis modality for children with end-stage renal disease. Pediatrics. (1997) 99:E6. doi: 10.1542/peds.99.4.e6
28. Schoenmaker NJ, Tromp WF, van der Lee JH, Adams B, Bouts AH, Collard L, et al. Disparities in dialysis treatment and outcomes for Dutch and Belgian children with immigrant parents. Pediatr Nephrol. (2012) 27:1369–79. doi: 10.1007/s00467-012-2135-7
29. Alhusaini OA, Wayyani LA, Dafterdar HE, Gamlo MM, Alkhayat ZA, Alghamdi AS, et al. Comparison of quality of life in children undergoing peritoneal dialysis versus hemodialysis. Saudi Med J. (2019) 40:840–3. doi: 10.15537/smj.2019.8.12747
30. Chuasuwan A, Pooripussarakul S, Thakkinstian A, Ingsathit A, Pattanaprateep O. Comparisons of quality of life between patients underwent peritoneal dialysis and hemodialysis: a systematic review and meta-analysis. Health Qual Life Outcomes. (2020) 18:191. doi: 10.1186/s12955-020-01449-2
31. Charnaya O, Verghese P, Goldberg A, Ladin K, Porteny T, Lantos JD. Access to transplantation for undocumented pediatric patients. Pediatrics. (2020). 146:e20193692. doi: 10.1542/peds.2019-3692
32. McEnhill ME, Brennan JL, Winnicki E, Lee MM, Tavakol M, Posselt AM, et al. Effect of immigration status on outcomes in pediatric kidney transplant recipients. Am J Transplant. (2016) 16:1827–33. doi: 10.1111/ajt.13683
33. Yu E, Wightman A. Pediatric kidney transplant in undocumented immigrants: an American perspectives. Pediatr Transplant. (2021) 25:e13788. doi: 10.1111/petr.13788
34. Freedman BI, Limou S, Ma L, Kopp JB. APOL1-Associated nephropathy: a key contributor to racial disparities in CKD. Am J Kidney Dis. (2018) 72:S8–S16. doi: 10.1053/j.ajkd.2018.06.020
35. Crews DC, Pfaff T, Powe NR. Socioeconomic factors and racial disparities in kidney disease outcomes. Semin Nephrol. (2013) 33:468–75. doi: 10.1016/j.semnephrol.2013.07.008
36. Dias JP, Shardell M, Golden SH, Ahima RS, Crews DC. Racial/ethnic trends in prevalence of diabetic kidney disease in the United States. Kidney Int Rep. (2018) 4:334–7. doi: 10.1016/j.ekir.2018.10.018
37. Mendenhall E, Kohrt BA, Norris SA, Ndetei D, Prabhakaran D. Non-communicable disease syndemics: poverty, depression, and diabetes among low-income populations. Lancet. (2017) 389:951–63. doi: 10.1016/S0140-6736(17)30402-6
38. Gaskin DJ, Thorpe RJ, McGinty EE, Bower K, Rohde C, Young JH, et al. Disparities in diabetes: the nexus of race, poverty, and place. Am J Public Health. 104:2147–55. doi: 10.2105/AJPH.2013.301420
39. Orr SE, Bridges CC. Chronic kidney disease and exposure to nephrotoxic metals. Int J Mol Sci. (2017). 18:1039. doi: 10.3390/ijms18051039
40. Chehade H, Simeoni U, Guignard J-P, Boubred F. Preterm birth: long term cardiovascular and renal consequences. Curr Pediatr Rev. (2018) 14:219–26. doi: 10.2174/1573396314666180813121652
41. Purnell TS, Bae S, Luo X, Johnson M, Crews DC, Cooper LA, et al. National trends in the association of race and ethnicity with predialysis nephrology care in the United States from 2005 to 2015. JAMA Netw Open. (2020). 3:e2015003. doi: 10.1001/jamanetworkopen.2020.15003
42. Cedillo-Couvert EA, Hsu JY, Ricardo AC, Fischer MJ, Gerber BS, Horwitz EJ, et al. Patient experience with primary care physician and risk for hospitalization in Hispanics with CKD. Clin J Am Soc Nephrol. (2018) 13:1659–67. doi: 10.2215/CJN.03170318
43. Greer RC, Cooper LA, Crews DC, Powe NR, Boulware LE. Quality of patient-physician discussions about CKD in primary care: a cross-sectional study. Am J Kidney Dis. (2010) 57:583–91. doi: 10.1053/j.ajkd.2010.08.027
44. Murphy KA, Greer RC, Roter DL, Crews DC, Ephraim PL, Carson KA, et al. Awareness and discussions about chronic kidney disease among African-Americans with chronic kidney disease and hypertension: a mixed methods study. J Gen Intern Med. (2020) 35:298–306. doi: 10.1007/s11606-019-05540-3
45. Novick TK, Diaz S, Barrios F, Cubas D, Choudhary K, Nader P, et al. Perspectives on kidney disease education and recommendations for improvement among Latinx patients receiving emergency-only hemodialysis. JAMA Netw Open. (2021). 4:e2124658. doi: 10.1001/jamanetworkopen.2021.24658
46. Leon JJ, Guthrie KK, Rueda C, La Cruz D de, Montoya-Williams D. Pediatric healthcare needs and barriers self-reported by a rural hispanic community. Cureus. (2020) 12:e11999. doi: 10.7759/cureus.11999
47. Thorsness R, Swaminathan S, Lee Y, Sommers BD, Mehrotra R, Nguyen KH, et al. Medicaid expansion and incidence of kidney failure among nonelderly adults. J Am Soc Nephrol. (2021) 32:1425–35. doi: 10.1681/ASN.2020101511
48. Harhay MN, McKenna RM, Boyle SM, Ranganna K, Mizrahi LL, Guy S, et al. Association between Medicaid expansion under the affordable care act and preemptive listings for kidney transplantation. Clin J Am Soc Nephrol. (2018) 13:1069–78. doi: 10.2215/CJN.00100118
49. Sanders SR, Cope MR, Park PN, Jeffery W, Jackson JE. Infants without health insurance: Racial/ethnic and rural/urban disparities in infant households' insurance coverage. PLoS ONE. (2020) 15:e0222387. doi: 10.1371/journal.pone.0222387
50. Griffith KN. Changes in insurance coverage and access to care for young adults in 2017. J Adolesc Health. (2019) 66:86–91. doi: 10.1016/j.jadohealth.2019.05.020
51. Suarez J, Cohen JB, Potluri V, Yang W, Kaplan DE, Serper M, et al. Racial disparities in nephrology consultation and disease progression among veterans with CKD: an observational cohort study. J Am Soc Nephrol. (2018) 29:2563–73. doi: 10.1681/ASN.2018040344
52. Perreira KM, Yoshikawa H, Oberlander J. A New threat to immigrants' health—the public-charge rule. N Engl J Med. (2018) 379:901–3. doi: 10.1056/NEJMp1808020
53. Zallman L, Finnegan KE, Himmelstein DU, Touw S, Woolhandler S. Implications of changing public charge immigration rules for children who need medical care. JAMA Pediatr. (2019). 173:e191744. doi: 10.1001/jamapediatrics.2019.1744
54. Beech BM, Ford C, Thorpe RJ, Bruce MA, Norris KC. Poverty, Racism, and the Public Health Crisis in America. Front Public Health. (2021). 9:699049. doi: 10.3389/fpubh.2021.699049
55. Williams DR, Cooper LA. Reducing racial inequities in health: using what we already know to take action. Int J Environ Res Public Health. (2019). 16:606. doi: 10.3390/ijerph16040606
56. Lee D-C, Liang H, Shi L. The convergence of racial and income disparities in health insurance coverage in the United States. Int J Equity Health. (2021) 20:96. doi: 10.1186/s12939-021-01436-z
57. Bignall ON, Crews DC. Stony the road we trod: towards racial justice in kidney care. Nat Rev Nephrol. (2021) 17:79–80. doi: 10.1038/s41581-020-00389-w
58. Nguyen AW, Hamler TC, Cobb RJ. Discrimination and chronic kidney disease among Caribbean blacks: the effects of immigration and social status. Race Soc Probl. (2018) 10:248–58. doi: 10.1007/s12552-018-9234-4
59. Rizzolo K, Cervantes L. Immigration status and end-stage kidney disease: role of policy and access to care. Semin Dial. (2020) 33:513–22. doi: 10.1111/sdi.12919
60. Mendu ML, Weiner DE. Health policy and kidney care in the United States: core curriculum 2020. Am J Kidney Dis. (2020) 76:720–30. doi: 10.1053/j.ajkd.2020.03.028
61. Jewers M, Ku L. Noncitizen children face higher health harms compared with their siblings who have US Citizen status. Health Aff (Millwood). (2021) 40:1084–9. doi: 10.1377/hlthaff.2021.00065
62. Pandey M, Maina RG, Amoyaw J, Li Y, Kamrul R, Michaels CR, et al. Impacts of English language proficiency on healthcare access, use, and outcomes among immigrants: a qualitative study. BMC Health Serv Res. (2021) 21:741. doi: 10.1186/s12913-021-06750-4
63. Cervantes L, Rizzolo K, Carr AL, Steiner JF, Chonchol M, Powe N, et al. Social and cultural challenges in caring for Latinx individuals with kidney failure in urban settings. JAMA Netw Open. (2021). 4:e2125838. doi: 10.1001/jamanetworkopen.2021.25838
64. Li J, Lowres N, Koo FK, Gallagher R. A systematic review of quantitative and qualitative literature on health professionals' experiences communicating with Chinese immigrants. Int J Nurs Pract. (2021) 27:e12960. doi: 10.1111/ijn.12960
65. Ornelas C, Torres JM, Torres JR, Alter H, Taira BR, Rodriguez RM. Anti-immigrant rhetoric and the experiences of Latino immigrants in the emergency department. West J Emerg Med. (2021) 22:660–6. doi: 10.5811/westjem.2021.2.50189
66. Seligman HK, Schillinger D. Hunger and socioeconomic disparities in chronic disease. N Engl J Med. (2010) 363:6–9. doi: 10.1056/NEJMp1000072
67. Crews DC, Kuczmarski MF, Grubbs V, Hedgeman E, Shahinian VB, Evans MK, et al. Effect of food insecurity on chronic kidney disease in lower income Americans. Am J Nephrol. (2014) 39:27–35. doi: 10.1159/000357595
68. Vart P, Gansevoort RT, Joosten MM, Bültmann U, Reijneveld SA. Socioeconomic disparities in chronic kidney disease: a systematic review and meta-analysis. Am J Prev Med. (2015) 48:580–92. doi: 10.1016/j.amepre.2014.11.004
69. Novick TK, Han D, Jacobs EA, Zonderman A, Evans MK, Crews DC. Health-related social needs and kidney risk factor control in an urban population. Kidney Med. (2021) 3:680–2. doi: 10.1016/j.xkme.2021.03.005
70. Bullock A, Burrows NR, Narva AS, Sheff K, Hora I, Lekiachvili A, et al. Vital signs: decrease in incidence of diabetes-related end-stage renal disease among American Indians/Alaska Natives—United States, 1996–2013. MMWR Morb Mortal Wkly Rep. (2017) 66:26–32. doi: 10.15585/mmwr.mm6601e1
71. Welles CC, Cervantes L. Barriers to providing optimal dialysis care for undocumented immigrants: policy challenges and solutions. Semin Dial. (2020) 33:52–7. doi: 10.1111/sdi.12846
72. Nguyen OK, Makam AN. Comparison of scheduled vs emergency-only dialysis in undocumented immigrants with end-stage renal disease-reply. JAMA Intern Med. (2019) 179:728–9. doi: 10.1001/jamainternmed.2019.0537
73. Pourat N, Martinez AE. Reducing access disparities in california by insuring low-income undocumented adults. Policy Brief UCLA Cent Health Policy Res. (2019) 2019:1–8.
Keywords: structural inequities, racial disparities, uninsured, insurance coverage, chronic kidney disease, immigration
Citation: Iorember FM and Bamgbola OF (2022) Structural Inequities and Barriers to Accessing Kidney Healthcare Services in the United States: A Focus on Uninsured and Undocumented Children and Young Adults. Front. Pediatr. 10:833611. doi: 10.3389/fped.2022.833611
Received: 11 December 2021; Accepted: 31 January 2022;
Published: 05 April 2022.
Edited by:
Michael L. Moritz, University of Pittsburgh, United StatesReviewed by:
Zubin Modi, University of Michigan, United StatesCopyright © 2022 Iorember and Bamgbola. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Franca M. Iorember, RnJhbmNhLmlvcmVtYmVyQGJjbS5lZHU=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.