
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr. , 16 February 2022
Sec. Pediatric Infectious Diseases
Volume 10 - 2022 | https://doi.org/10.3389/fped.2022.832694
Background: To establish the sensitivity of the diagnostic criteria published by Marais and co-workers in 2010 for childhood tuberculous meningitis (TBM), a retrospective study on children with confirmed TBM was conducted.
Methods: Between January 2006 and December 2019, children consecutively diagnosed with TBM were recruited retrospectively at our center. TBM was defined in cases where any of the following criteria were met: the presence of acid-fast bacilli (AFB) in cerebrospinal fluid (CSF) microscopy, CSF nucleic acid amplification test (NAAT, +), or M.tuberculosis cultured from CSF. The demographic and clinical features of all enrolled patients were recorded including clinical characteristics, CSF findings, cerebral imaging features, and other evidence of TB.
Results: A total of 30 children with confirmed diagnosis of TBM over an 14-year period were recruited. The mean age of patients was 7.2 ± 5.1 years and 16 (53.3%) were male. The estimated mean diagnostic score was 12.7 ± 2.4. Twenty-three (76.7%; 95% CI: 59.1–88.2%) patients were classified as “probable TBM” according to the Marais criteria and 7 (23.3%; 95% CI: 11.8–40.9%) as “possible TBM.” Further statistical analysis revealed significant differences in CSF scores between probable and possible TBM groups. Other variables reported at a relatively low frequency, such as symptoms and imaging features, made little contribution to TBM diagnosis according to the Marais criteria.
Conclusion: Childhood TBM could be effectively identified by the criteria defined by Marais et al. However, further revision is required to ensure that the system is more sensitive and easier to perform in practice.
Tuberculous meningitis (TBM) is an ongoing serious threat to child health. In China, 9.4% of children with tuberculosis (TB) are diagnosed with TBM, with 14.7% showing poor outcomes, such as death and transferred to a high care center (1, 2). Diagnostic delay is an important contributor to mortality in childhood-associated TBM (3). It was reported that about one-fifth of TBM children were asymptomatic on admission, and the sensitivities of Ziehl–Neelsen staining, culture, and polymerase chain reaction (PCR) for detection of childhood TBM were 25, 58, and 66.3%, respectively (4). Furthermore, in childhood TB, interferon-gamma release assay (IGRA) has a good sensitivity (83.3%) and few indeterminate results (2.5%) were reported (5). However, in childhood TBM, a relative low sensitivity of 71.7% was reported and indeterminate results (17.0%) were common (6). Moreover, limited techniques for effective TBM diagnosis in children, such as Xpert Ultra, are currently available (7). Two key factors are responsible for the diagnostic limitations in childhood TBM: (1) cerebrospinal fluid (CSF) is a paucibacillary specimen type and (2) TB in children is often paucibacillary. In addition, TBM is difficult to treat and often responds poorly to conventional TB treatment (8, 9).
TBM infection is easy to confirm, usually based on microbiological evidence in CSF samples. Routine microbiological methods include acid-fast bacilli (AFB) smear, culture, and nucleic acid amplification test (NAAT). However, during the past few decades, the definitions of “possible” and “probable” TBM have varied widely among studies. These inconsistencies induce selection bias and have a significant impact on the accuracy of systematic reviews (10). In 2010, a standardized set of diagnostic criteria for TBM was introduced by Marais et al. (11). Since then, this diagnostic scoring system has been widely used in the corresponding field and cited in numerous clinical studies. The Marais classification criteria are based on Thwaites' Index, which has previously shown good performance (12–14). However, these criteria are associated with a number of disadvantages that need to be addressed: (1) the difference between childhood and adult TBM is not fully considered, (2) the scoring system is presented as a personal view and lacks sufficient data to support its efficiency, and (3) insufficient information is available on the utility of the criteria in China.
This retrospective study aimed to evaluate the efficiency of the diagnostic scoring system in confirmed childhood TBM. Our findings should aid in improving application of the criteria for childhood TBM and providing further evidence to tailor the scoring system for more accurate diagnosis of TBM in children.
This study was conducted at the Shandong Provincial Chest Hospital in keeping with the Declaration of Helsinki. The study protocol was approved by the Ethical Committee of Shandong Provincial Chest Hospital (approval No. 2020XKYYEC-29). Due to the retrospective nature of this study and the anonymous nature of data analyzed, written informed consent was waived by the Ethical Committee of Shandong Provincial Chest Hospital.
Between January 2006 and December 2019, consecutive patients (≤15 years old) with confirmed diagnosis of TBM were retrospectively recruited for study. TBM was defined in cases where any of the following criteria were met: acid-fast bacilli (AFB) in cerebrospinal fluid (CSF) microscopy, CSF NAAT (+) or M.tuberculosis cultured from CSF. The demographic characteristics and clinical features of all enrolled patients were recorded using standardized questionnaires developed on the basis of four criteria, including clinical, CSF and cerebral imaging features, and other evidence of TB (Table 1). Subsequently, a diagnostic score was calculated and patients were divided as probable and possible TBM based on the Marais criteria (11). Probable TBM is defined if a diagnostic score is ≥ 12 (with imaging) or ≥ 10 (without imaging). Possible TBM is defined if a diagnostic score is 6–11 (with imaging) or 6–9 (without imaging).
Continuous data were presented as mean ± standard deviation (SD) and categorical data as counts (percentages). In addition, 95% confidence interval (CI) was calculated whenever appropriate. Student's t-test was used to compare mean values of diagnostic scores (including total diagnostic score and scores for clinical criteria, CSF criteria, cerebral imaging criteria, and evidence of tuberculosis elsewhere) between two groups and P < 0.05 considered statistically significant.
A total of 149 childhood TBM cases diagnosed over the past 14 years were included for analysis, 30 of which were confirmed based on CSF culture (+, n = 24), CSF AFB (+, n = 2), and NAAT (+, n = 16). Among the 30 children, one patient has a positive result of CSF AFB smear, 5 have positive results of CSF PCR, 12 have positive results of CSF culture, one has positive results of CSF smear and culture, and 11 have positive results of CSF culture and PCR. The mean age was 7.2 ± 5.1 years and 16 (53.3%) were male. Clinicopathological characteristics were divided into four sets, shown in Table 2.
The mean symptom duration was 27.0 ± 34.2 days, with all symptoms recorded for over 5 days. Ten patients had a history of close TB contact and 12 were confirmed with TB infection via tuberculin skin test (TST) or interferon gamma release assay (IGRA). Common TB symptoms, such as weight loss (n = 1, 3.3%), night sweats (0, 0%), and cough (>2 weeks; n = 6, 20%), were reported in a minority of patients. In addition, focal neurological deficits (excluding cranial nerve palsy) and altered consciousness were recorded in 5 and 4 patients, respectively.
Clear appearance of CSF was reported in 25 cases (25/30, 83.3%). Among these, 19 patients (19/28, 67.9%) showed lymphocyte-predominant CSF accumulation (lymphocyte proportion: 64.5 ± 25.5%), 27 (90%) had cell numbers between 20 and 500/μL (mean level of 201.1 ± 174.2/μL), and 26 (86.7%) presented with a low CSF/plasma glucose ratio (<50%) or CSF glucose (<2.2 mmol/L; mean, 1.64 ± 0.88 mmol/L). However, CSF protein content above 1 g/L (concentration, 1,240 ± 1,048 mg/L) was observed in only half of the patients.
Twenty-four patients underwent radiological examinations. Hydrocephalus, basal meningeal enhancement, tuberculoma, infarct, and pre-contrast basal hyperdensity were reported in 7 (29.2%), 1 (4.2%), 13 (54.2%), 0 (0%), and 5 (20.8%) patients, respectively.
Twenty-seven patients were subjected to chest radiography, which revealed TB signs and miliary TB in 10 (37.0%) and 13 (48.2%) patients, respectively. Extra-neural specimens were subjected to microbiological tests. Overall, two patients were smear-positive, two were culture-positive, and two were NAAT-positive.
The diagnostic score was calculated for all patients as follows: 10 (n = 6), 11 (n = 4), 12 (n = 8), 13 (n = 2), 14 (n = 3), 15 (n = 1), 16 (n = 5), and 19 (n = 1). The mean score was subsequently estimated as 12.7 ± 2.4. Twenty-three patients (76.7%; 95% CI: 59.1–88.2%) were classified as probable TBM according to the Marais criteria (with imaging, >12; without imaging, >10) and 7 (23.3%; 95% CI: 11.8–40.9%) as possible TBM. Further statistical analysis showed significant differences in CSF scores between probable and possible TBM groups (Table 3). The collective data clearly indicate that more attention should be paid to improvement of diagnostic criteria based on CSF findings.
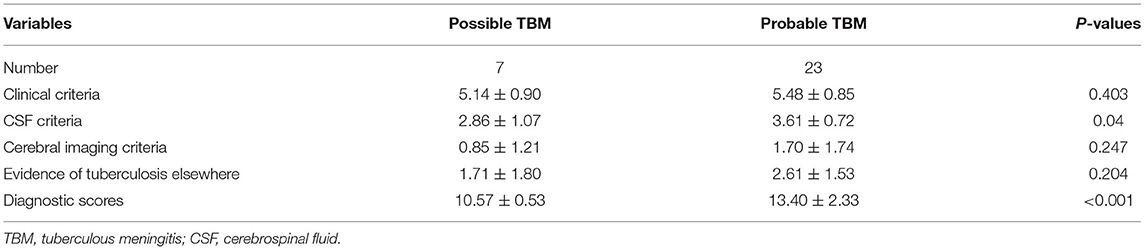
Table 3. Diagnostic scores of four sets of TBM diagnositc criteria between probable and possible TBM.
TBM is the most severe form of TB and a significant cause of morbidity and mortality worldwide. Clinical diagnosis of TBM remains a significant challenge in practice, since a definitive diagnosis is hard to establish and a uniform clinical case definition is absent. In 2010, a case definition of TBM was published by Marais et al. (11). Over the last decade, these criteria have been cited more than 700 times and performed well in clinical research. In the current study, we assessed the utility of the Marais criteria in classification of childhood TBM. Although further revisions are required, our data support the high efficiency and utility of the Marais criteria for definitive diagnosis of childhood TBM.
Fever should be introduced into the current guidelines and the scores of items of clinical criteria refined. In our study, fever was the most common symptom, reported in 29 patients (96.7%, data not shown). Previously, fever was identified as a protective factor for the treatment delay of TBM (15). Therefore, introduction of fever into the current criteria may improve diagnostic performance and improve management of childhood TBM. In addition, based on the observation that a high proportion of TBM subjects have prior TB diagnosis and long duration of illness but relatively low frequency of other clinical presentations, we conclude that items of clinical criteria should be optimized and score values further refined, especially for meningitis symptoms.
CSF features are widely utilized for classification as possible TBM but associated with a number of limitations. First, the variable CSF scores between probable and possible TBM cannot be explained by a single CSF biomarker, since no differences are evident between the groups for each CSF feature. Second, atypical CSF findings reflect an abnormal state and could be used to evaluate severity of TBM. Similarly, the diagnostic score may correlate with progression of childhood TBM. Third, lymphocytic predominance and CSF protein have a relatively poor performance in classification. In our experiments, patients with lymphocytic predominance accounted about 70% of the study group. Although this percentage appears lower than that of other studies (~80%) (11), variable distribution is reported (16–18). Additionally, the criterion for CSF protein level <1 g/L is easily met in clinical practice and other references (such as 0.45 g/L and 0.8 g/L) are additionally used in clinical research (19–21). Fourth, chloride should be considered in the revised version of diagnostic criteria, since high CSF chloride levels are associated with treatment delay of TBM (15). The utility of CSF chloride in diagnosis of TBM has been previously evaluated (22).
Hydrocephalus, basal meningeal enhancement, infarct, and tuberculoma are the four main characteristics of TBM and the presence of these features on neuroimaging enhances confidence in clinical diagnosis (23–25). Neuroimaging is considered invaluable for assessment of TBM (26). In our study, these four features showed no sensitivity in TBM diagnosis. In addition, although tuberculoma was the most common presentation (54.2%), diagnosis was mostly made based on positive responses to anti-TB therapy. Another major limitation of this study was that several cases were confirmed based on microbiological evidence and radiological assessment was thus waived at the initial evaluation stage, leading to lack of imaging data. Overall, 66.7% of the subjects had pulmonary involvement and half the patients had miliary TB. These findings support the significance of respiratory specimens and need for caution in cases of miliary TB for potential diagnosis of childhood TBM.
Our study has several limitations that should be taken into consideration. First, comparison between childhood TBM and controls was not performed, since the hospital was a referral TB setting and few meningitis cases of other etiologies were admitted. Moreover, few TBM cases were confirmed over the long-term period of analysis. Second, due to the retrospective nature of the study, some data were overlooked during collection, which would decrease the actual diagnostic score and result in misclassification. Third, the lack of TST and IGRAs is another limitation, since their use might change the performance of the Marais criteria. Therefore, our results should be interpreted with caution. Fourth, due to other study limitations, such as single center design, small sample size, and lack of controls, further research is required to revise the criteria and evaluate the efficiency of both primary and revised versions in diagnosis of suspected childhood TBM.
In conclusion, although childhood TBM could be effectively identified by the Marais criteria, further revision of these guidelines is essential to improve diagnostic performance, reliability, and ease of use.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
The study protocol was approved by the Ethical Committee of Shandong Provincial Chest Hospital. Due to the retrospective nature of this study and the anonymous nature of data analyzed, written informed consent was waived by the Ethical Committee of Shandong Provincial Chest Hospital.
X-JL and Y-AZ designed the study and supervised data collection. M-SW collected data, performed statistical analysis, and drafted the initial manuscript. J-LW revised the manuscript. All authors approved the final version of the report.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Wang MS, Zhao M, Liu XJ. Risk factors for poor outcome in childhood tuberculous meningitis. Sci Rep. (2021) 11:8654. doi: 10.1038/s41598-021-87082-5
2. Wang MS, Wang JL, Liu XJ. Epidemiological trends in the form of childhood tuberculosis in a referral tuberculosis hospital in Shandong, China. Biomed Res Int. (2020) 2020:6142567. doi: 10.1155/2020/6142567
3. Bang ND, Caws M, Truc TT, Duong TN, Dung NH, Ha DT, et al. Clinical presentations, diagnosis, mortality and prognostic markers of tuberculous meningitis in Vietnamese children: a prospective descriptive study. BMC Infect Dis. (2016) 16:573. doi: 10.1186/s12879-016-1923-2
4. Buonsenso D, Lancella L, Delogu G, Krzysztofiak A, Testa A, Ranno O, et al. A twenty-year retrospective study of pediatric tuberculosis in two tertiary hospitals in Rome. Pediatr Infect Dis J. (2012) 31:1022–6. doi: 10.1097/INF.0b013e3182615270
5. Buonsenso D, Delogu G, Perricone C, Grossi R, Careddu A, De Maio F, et al. Accuracy of QuantiFERON-TB gold plus test for diagnosis of mycobacterium tuberculosis infection in children. J Clin Microbiol. (2020) 58:e00272–20. doi: 10.1128/JCM.00272-20
6. Roy RB, Thee S, Blázquez-Gamero D, Falcón-Neyra L, Neth O, Noguera-Julian A, et al. Performance of immune-based and microbiological tests in children with tuberculosis meningitis in Europe: a multicentre paediatric tuberculosis network european trials group (ptbnet) study. Europ Respir J. (2020) 56:1902004. doi: 10.1183/13993003.02004-2019
7. Donovan J, Cresswell FV, Thuong NTT, Boulware DR, Thwaites GE, Bahr NC, et al. Xpert MTB/RIF ultra for the diagnosis of tuberculous meningitis: a small step forward. Clin Infect Dis. (2020) 71:2002–5. doi: 10.1093/cid/ciaa473
8. Buonsenso D, Serranti D, Valentini P. Management of central nervous system tuberculosis in children: light and shade. Eur Rev Med Pharmacol Sci. (2010) 14:845–53.
9. Buonsenso D, Serranti D, Focarelli B, Chiaretti A, Calzedda R, Valentini P. How to manage TB in children? Problems and solutions in four cases. Open Med. (2015) 10:63–9. doi: 10.1515/med-2015-0012
10. Kay AW, Gonzalez Fernandez L, Takwoingi Y, Eisenhut M, Detjen AK, Steingart KR, et al. Xpert MTB/RIF and Xpert MTB/RIF Ultra assays for active tuberculosis and rifampicin resistance in children. Cochrane Database Syst Rev. (2020) 8:CD013359. doi: 10.1002/14651858.CD013359.pub2
11. Marais S, Thwaites G, Schoeman JF, Torok ME, Misra UK, Prasad K, et al. Tuberculous meningitis: a uniform case definition for use in clinical research. Lancet Infect Dis. (2010) 10:803–12. doi: 10.1016/S1473-3099(10)70138-9
12. Saavedra JS, Urrego S, Toro ME, Uribe CS, Garcia J, Hernandez O, et al. Validation of Thwaites Index for diagnosing tuberculous meningitis in a Colombian population. J Neurol Sci. (2016) 370:112–8. doi: 10.1016/j.jns.2016.09.007
13. Zhang YL, Lin S, Shao LY, Zhang WH, Weng XH. Validation of thwaites' diagnostic scoring system for the differential diagnosis of tuberculous meningitis and bacterial meningitis. Jpn J Infect Dis. (2014) 67:428–31. doi: 10.7883/yoken.67.428
14. Pehlivanoglu F, Yasar KK, Sengoz G. Tuberculous meningitis in adults: a review of 160 cases. ScientificWorldJournal. (2012) 2012:169028. doi: 10.1100/2012/169028
15. He Y, Han C, Chang KF, Wang MS, Huang TR. Total delay in treatment among tuberculous meningitis patients in China: a retrospective cohort study. BMC Infect Dis. (2017) 17:341. doi: 10.1186/s12879-017-2447-0
16. Karande S, Gupta V, Kulkarni M, Joshi A. Prognostic clinical variables in childhood tuberculous meningitis: an experience from Mumbai, India. Neurol India. (2005) 53:191–5; discussion 195–6. doi: 10.4103/0028-3886.16407
17. Youssef FG, Afifi SA, Azab AM, Wasfy MM, Abdel-Aziz KM, Parker TM, et al. Differentiation of tuberculous meningitis from acute bacterial meningitis using simple clinical and laboratory parameters. Diagn Microbiol Infect Dis. (2006) 55:275–8. doi: 10.1016/j.diagmicrobio.2006.01.027
18. Kumar R, Singh SN, Kohli N. A diagnostic rule for tuberculous meningitis. Arch Dis Child. (1999) 81:221–4. doi: 10.1136/adc.81.3.221
19. van Well GT, Paes BF, Terwee CB, Springer P, Roord JJ, Donald PR, et al. Twenty years of pediatric tuberculous meningitis: a retrospective cohort study in the western cape of South Africa. Pediatrics. (2009) 123:e1–8. doi: 10.1542/peds.2008-1353
20. Wang JL, Han C, Yang FL, Wang MS, He Y. Normal cerebrospinal fluid protein and associated clinical characteristics in children with tuberculous meningitis. Ann Med. (2021) 53:885–89. doi: 10.1080/07853890.2021.1937692
21. Solari L, Soto A, Agapito JC, Acurio V, Vargas D, Battaglioli T, et al. The validity of cerebrospinal fluid parameters for the diagnosis of tuberculous meningitis. Int J Infect Dis. (2013) 17:e1111–5. doi: 10.1016/j.ijid.2013.06.003
22. Wang SS. An assessment on the concentration of fluorescein sodium and chloride in cerebrospinal fluid for the diagnosis of tuberculous meningitis. Zhonghua Jie He He Hu Xi Za Zhi. (1987) 10:218–20, 254–5.
23. Botha H, Ackerman C, Candy S, Carr JA, Griffith-Richards S, Bateman KJ. Reliability and diagnostic performance of CT imaging criteria in the diagnosis of tuberculous meningitis. PLoS One. (2012) 7:e38982. doi: 10.1371/journal.pone.0038982
24. Christensen AS, Andersen AB, Thomsen VO, Andersen PH, Johansen IS. Tuberculous meningitis in Denmark: a review of 50 cases. BMC Infect Dis. (2011) 11:47. doi: 10.1186/1471-2334-11-47
25. Andronikou S, Smith B, Hatherhill M, Douis H, Wilmshurst J. Definitive neuroradiological diagnostic features of tuberculous meningitis in children. Pediatr Radiol. (2004) 34:876–85. doi: 10.1007/s00247-004-1237-1
Keywords: children, tuberculous meningitis, diagnosis, criteria, diagnostic score
Citation: Wang M-S, Wang J-L, Liu X-J and Zhang Y-A (2022) The Sensitivity of Diagnostic Criteria of Marais S, et al. in Confirmed Childhood Tuberculous Meningitis. Front. Pediatr. 10:832694. doi: 10.3389/fped.2022.832694
Received: 13 December 2021; Accepted: 11 January 2022;
Published: 16 February 2022.
Edited by:
Danilo Buonsenso, Catholic University of the Sacred Heart, ItalyReviewed by:
Francesca Raffaelli, Fondazione Policlinico Universitario A. Gemelli IRCCS, ItalyCopyright © 2022 Wang, Wang, Liu and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xin-Jie Liu, bGl1eGluamllQHNkdS5lZHUuY24=; Yan-An Zhang, emhhbmd0Ymdyb3VwQDE2My5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.