
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr., 22 February 2022
Sec. Pediatric Critical Care
Volume 10 - 2022 | https://doi.org/10.3389/fped.2022.826294
This article is part of the Research TopicPre-Hospital and Post-Resuscitation Care for Pediatric Cardiac ArrestView all 6 articles
 Kate McKenzie1*
Kate McKenzie1* Saoirse Cameron1
Saoirse Cameron1 Natalya Odoardi2
Natalya Odoardi2 Katelyn Gray1
Katelyn Gray1 Michael R. Miller1,3
Michael R. Miller1,3 Janice A. Tijssen1,3
Janice A. Tijssen1,3Background: Survival after pediatric out-of-hospital cardiac arrest is poor. Paramedic services provide critical interventions that impact survival outcomes. We aimed to describe local pediatric out-of-hospital cardiac arrest (POHCA) events and evaluate the impact of the paramedic service response to POHCA.
Methods: The Canadian Resuscitation Outcomes Consortium and corresponding ambulance call records were used to evaluate deviations from best practice by paramedics for patients aged 1 day to <18 years who had an atraumatic out-of-hospital cardiac arrest between 2012 and 2020 in Middlesex-London County. Deviations were any departure from protocol as defined by Middlesex-London Paramedic Services.
Results: Fifty-one patients were included in this study. All POHCA events had at least one deviation, with a total of 188 deviations for the study cohort. Return of spontaneous circulation (ROSC) was achieved in 35.3% of patients and 5.8% survived to hospital discharge. All survivors developed a new, severe neurological impairment. Medication deviations were most common (n = 40, 21.3%) followed by process timing (n = 38, 20.2%), vascular access (n = 27, 14.4%), and airway (n = 27, 14.4%). A delay in vascular access was the most common deviation (n = 25, 49.0%). The median (IQR) time to epinephrine administration was 8.6 (5.90–10.95) min from paramedic arrival. Cardiac arrests occurring in public settings had more deviations than private settings (p = 0.04). ROSC was higher in events with a deviation in any circulation category (p = 0.03).
Conclusion: Patient and arrest characteristics were similar to other POHCA studies. This cohort exhibited high rates of ROSC and bystander cardiopulmonary resuscitation but low survival to hospital discharge. The study was underpowered for its primary outcome of survival. The total deviations scored was low relative to the total number of tasks in a resuscitation. Epinephrine was frequently administered outside of the recommended timeframe, highlighting an important quality improvement opportunity.
Out-of-hospital cardiac arrest is rare in children and is associated with extremely poor outcomes (1, 2). The survival rate of pediatric out-of-hospital cardiac arrest (POHCA) is 10.2% in North America, and survivors often have a new, severe neurological impairment (2). The survival rates following POHCA vary depending on age, etiology, initial rhythm, bystander cardiopulmonary resuscitation (CPR), and other factors (1, 2).
Paramedic services play a critical role in the survival outcomes for POHCA (3–5). However, paramedics' lack of exposure to POHCA due to infrequent occurrence may contribute to a variable response. It is common for paramedics to prioritize extrication and transportation, which have been shown to be associated with worse outcomes (5, 6). Previous research has demonstrated that early on-scene management such as high-quality CPR and the time of medication administration are associated with improved survival (4, 5, 7); as such, resuscitation protocols prioritize these interventions (8). However, Kirves et al. discovered that only 40% of adult patients who experienced out-of-hospital cardiac arrest received care in accordance with the resuscitation recommendations (9). Deviations from hospital protocols for care of pediatric in-hospital cardiac arrests are also associated with worse outcomes (10). In addition, in a POHCA simulation study with non-shockable arrests, many key resuscitation tasks were not routinely performed in line with Pediatric Advanced Life Support guidelines (11). However, deviations from protocols during on-scene management for POHCA events have not been evaluated.
The purpose of this study was to describe the paramedic response to local POHCA events and to assess its impact on patient outcomes. We hypothesized that the paramedic response to POHCA is variable and that deviations from resuscitation protocols are negatively associated with survival.
This was a historical cohort study of POHCA events from an out-of-hospital cardiac arrest registry between January 1, 2012, and June 30, 2020. This study was approved by Western University Research Ethics Board (Project ID: #115304).
This study included children aged 1 day to <18 years old who experienced atraumatic out-of-hospital cardiac arrest in Middlesex-London County, Ontario, Canada. All children who had emergency medical services called to the scene and attempts at chest compressions and/or external defibrillation by Middlesex-London Paramedic Services (MLPS) were included. MLPS services a population of ~450,000 people. Patients were excluded if MLPS did not treat for cardiac arrest, if patients were not transported to hospital following identification of cardiac arrest, or if the primary outcome variable was missing. All patients were divided into age groups: infants (1 day to 12 months), children (1 year to 11 years), and adolescents (12 years to <18 years). The primary outcome for this study was survival to hospital discharge. Secondary outcomes included return of spontaneous circulation (ROSC), survival to hospital admission, neurological status at hospital discharge, and survival to 90 days post-cardiac arrest. Baseline, 6-month, and 12-month Pediatric Cerebral Performance Category (PCPC) post-POHCA scores were collected and reported as per the Pediatric Core Outcome Set for Cardiac Arrest guidelines (12). Events that were excluded were not included in the analysis of the primary or secondary outcomes.
Ambulance call records (ACR) for all POHCA events in Middlesex-London County from January 1, 2012, to June 30, 2020, were collected using study identification numbers through the Canadian Resuscitation Outcomes Consortium (CanROC) registry, a national de-identified out-of-hospital cardiac arrest registry. The registry includes all documentation required for reporting cardiac arrest for research as per the Utstein criteria (13). The researchers were not blinded to the outcomes of the events during data extraction. There was only one data extractor for the study. The deviation score definitions were objective and agreed on by the study team. The data collected from ACRs and the CanROC registry were combined, along with patient hospital records to create the POHCA database for our study. If there was any discrepancy between CanROC and ACR data, ACR data (as source data) were used.
All MLPS protocols were collated. When local protocols were non-specific, the Heart and Stroke Foundation of Canada's Pediatric Advance Life Support guidelines were used. The protocols guide Primary Care and Advanced Care Paramedics. Primary Care Paramedics can perform CPR and administer limited medications orally or through intramuscular routes. Advanced Care Paramedics have more training which allows them to insert advanced airways, secure IV and IOs, and administer intravascular medications such as epinephrine. Deviations were defined a priori as departure from “best practice” (8, 14–16). We used current protocols to define “best practice” when evaluating deviations across the study period. A deviation was not scored if a Primary Care Paramedic did not administer epinephrine as it is not in their scope of practice. It would be scored a deviation if an Advanced Care Paramedic delayed epinephrine administration as this is within their scope. Adapted from Wolfe et al., we modified eight categories of deviations for the POHCA population: (1) Airway management, (2) Medications, (3) Vascular access, (4) Chest compressions/CPR, (5) Defibrillation, (6) Equipment function, (7) Alerting, and (8) Process timing (10). Each deviation category was subdivided into specific actions for scoring, with the possible data entries of: Yes (deviation occurred), No (deviation did not occur), or Unknown (missing information). An example of a deviation would be delayed epinephrine administration. Epinephrine should be administered directly after IV or IO is secured, and before advanced airway is placed. If epinephrine is administered after another step after the IV is secured or if an advanced airway is placed prior, a deviation was scored. Each patient event was analyzed for deviations. Deviation frequencies were measured as a proportion of the total number of deviations scored. Secondary variables were also defined. “Circulation process of care deviation” (C-DEV) was defined as a deviation from the CPR/chest compression, defibrillation, medication, and vascular access categories (10). Others included “Airway deviation” (A-DEV), defined as any airway deviation that could include delayed advanced airway placement such as multiple attempts, or inappropriate advanced airway placement, and “Process deviation” (P-DEV), defined as any deviation in equipment function, process timing, and alerting categories. There were 83 predefined deviations that could occur, and the number of potential deviations was calculated as all deviations multiplied by the number of events.
Descriptive analyses were performed on patient and cardiac arrest characteristics, interventions, deviations, and outcomes; continuous variables were summarized using medians and interquartile ranges, and categorical variables were summarized using frequencies and percentages. Deviations were analyzed as categories and as individual deviations. Bivariate analyses were completed on total deviation categories, composite deviation categories, and demographic characteristics for all outcome variables. A prognostic score for survival likelihood was calculated for each patient using patient and arrest characteristics and known predictors of survival. Each predictor was scored as a +1 or a−1. Positive predictors included adolescent age, witnessed arrest, bystander CPR, shockable rhythm, and drowning as an etiology (17–21). Negative predictors included unwitnessed arrest, no bystander CPR, asystole as an initial rhythm, sudden infant death syndrome as an etiology, baseline PCPC >1, do not attempt resuscitation status, and a severe underlying condition (e.g., Cardiomyopathy, Trisomy 18) (18, 20, 22).
Between January 1, 2012, and June 30, 2020, there were 52 pediatric patients who experienced an atraumatic POHCA in Middlesex-London County. One patient was excluded as they did not receive CPR by paramedics and were not transported to hospital. Patient and event characteristics are listed in Tables 1, 2, respectively. Patient characteristics were not associated with deviations. ROSC was achieved in 18 (35.3%) patients with 15 (29.4%) surviving to hospital admission. Survival to hospital discharge occurred in 3 (5.8%) patients. Survivors had a new, severe neurological impairment with PCPC scores of 4 at both 6 and 12 months post-POHCA.
Deviations were not associated with the primary survival outcome (p > 0.05). A total of 188 deviations were scored. We calculated that there were 4,233 potential deviations based on our cohort of 51 patients and the number of potential deviations per unique event. Therefore, 188 deviations represent a small fraction (4.4%) of total possible deviations. All events had at least one deviation, with a median (IQR) of 3 (2–5) deviations per event. Deviations occurred most frequently in the medication category (n = 40, 21.3%), but as for individual deviations, a delay to vascular access (n = 25, 49%) was the most common. Following medication, the categories with more frequent deviations are process timing (n = 38, 20.2%), followed by vascular access (n = 27, 14.4%) and airway (n = 27, 14.4%), defibrillation (n = 26, 13.8%), alerting (n = 17, 9.0%), chest compressions/CPR (n = 10, 5.3%), and equipment function (n = 3, 1.6%). The most common deviations per category are presented in Table 3.
As previously mentioned, delay to vascular access was the most common individual deviation scored (49.0%). The majority of patients had intraosseous (IO) access as the successful method for vascular access (n = 33, 64.7%), with an initial attempt success rate of 96.7% compared to the intravenous (IV) initial attempt success rate of 61.5%. The median (IQR) time from MLPS arrival on scene to epinephrine administration was 8.6 min (5.9–10.9). The number of events that had the first dose of epinephrine administered after 5 and 10 min from MLPS arrival on scene was 43 (84.3%) and 15 (29.4%), respectively. MLPS did not administer epinephrine in 11 (21.5%) events. Delay to vascular access and delay to epinephrine administration in each group are reflected in Figure 1. The delay to epinephrine administration could be attributed to a deviation at several decision points during an event. Delayed epinephrine administration caused by a delay in vascular access occurred in 29 (49.0%) events. Delayed epinephrine administration after vascular access was achieved occurred in eight events (15.7%). Primary care paramedics do not administer epinephrine as it does not fall within their scope of practice. Therefore, when only primary care paramedics were on-scene (n = 7, 13.7%), a deviation in the sub-category of delay to epinephrine administration was not scored. These events were included in the total number of events with epinephrine administration delay (n = 43, 84.3%), regardless of the reason for the delay as described above.
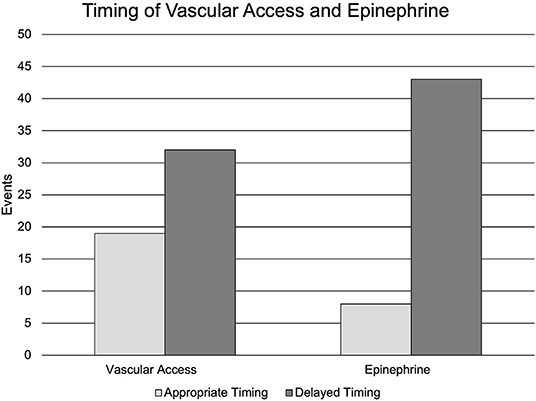
Figure 1. Timing of vascular access and epinephrine. Nineteen (37.2%) events had appropriate vascular access. Thirty-two (62.7%) events had a delay in vascular access. Eight (15.7%) events had appropriately timed epinephrine administration. Forty-three (84.3%) events had a delay in epinephrine administration.
Time on scene (as a continuous variable) was positively associated with total deviations and C-DEV (p = 0.01), but there was no significant association with categorical time on-scene. Suboptimal scene time outside of 10–35 min occurred in 24 (47.1%) events. Time on-scene was <10 min in 18 (35.3%) events. POHCA events that occurred in a public setting had significantly more deviations compared to a private setting (p = 0.04). ROSC was higher in events with at least one C-DEV (p = 0.03).
There were 18 (35.3%) events with Positive Prognostic Scores indicating a higher likelihood of survival based on patient and arrest characteristics prior to MLPS arrival (Table 4). Only 1 (5.5%) of these patients survived to hospital discharge. The number of deviation and the type of deviations in this group were comparable to the whole study cohort; the most common deviations were delay in vascular access (n = 9, 50.0%), suboptimal time on scene (n = 7, 38.9%), and incorrect rhythm check intervals (n = 7, 38.9%).
We described local POHCA events and evaluated paramedic response. Our main findings were: (1) the local POHCA population was similar to other jurisdictions, but the survival rate was lower, (2) deviations from best practice occurred in every event, and (3) we identified important deviations known to be associated with survival, including delay to epinephrine administration and suboptimal time on scene, which are potentially modifiable through quality improvement initiatives.
The patient and arrest characteristics of the local POHCA population in Middlesex-London County are comparable to other studies. The most common initial rhythm was asystole (n = 30, 58.8%) and the most common etiology was no obvious cause (n = 32, 62.7%), consistent with the current literature (20). The cardiac arrest was witnessed in 31.3% of cases. Our cohort had high rates of bystander CPR (n = 40, 78.4%), a factor known to positively influence survival outcomes (2, 5, 23, 24). Our cohort had high rates of ROSC (n = 18, 35.3%), double the North American reported average (2), but lower rates of survival to hospital discharge (n = 3, 5.8%) and all survivors had new, severe neurological impairments. Our study was underpowered for our primary outcome of survival.
POHCA events are rare, unique, and complex (20). In our cohort, every event had at least one deviation from protocol, with the median (IQR) score of 3 (2–5) deviations per event, highlighting the variability in on-scene management. We considered a deviation rate of 4.4% of all potential deviations to be low. We were not surprised that more deviations occurred when more time was spent on scene. We were intrigued to learn that more deviations occurred for public POHCA events than private (p = 0.04). This may be explained by the potential for increased distractions and pressure during a resuscitation where there are more bystanders present.
The common types of deviations that occurred in our study are known to be associated with lower survival (8, 16), and are comparable to those that occurred in a previous simulation study (11). Achieving vascular access through IV or IO is associated with survival in POHCA (5) but this was frequently delayed in our study. Optimal time on scene has been described to be between 10 and 35 min, but this not happen almost half the time, with most scene time deviations of <10 min (5). During pediatric in-hospital cardiac arrest resuscitation, deviating from hospital protocols, particularly care involving medications, CPR, defibrillation, and vascular access, is associated with decreased survival (10). Adherence to protocols during in-hospital cardiac arrest in adults has been shown to increase 30-day survival and lead to more favorable neurological outcomes (25). Though our study was underpowered to show an association between deviations and survival, deviations from protocols are known to influence survival and should be considered as modifiable risk factors to improve survival.
Banerjee argues that time on scene may be less important than what actually happens on scene (7). This theory may also be supported by reports from Japan where scene time is routinely <10 min but survival is 9.8%, with unknown remaining neurological function (26). The majority of our study's events (84.3%) had a delay in epinephrine administration beyond 5 min from MLPS arrival and 29.4% beyond 10 min from MLPS arrival. Our results are better than reported across North America and Taiwan, where, on average, epinephrine was administered at >10 min in 54 and 97%, respectively (4, 24). A recent POHCA simulation study conducted in Oregon found the mean time from paramedic arrival to epinephrine administration was 9.2 min, with 59% of patients receiving either epinephrine after 10 min or no epinephrine at all (11). Our local median time of 8.6 min is less compared to 17.3 min after paramedic arrival in Taiwan and the recent simulation findings (11, 24). Rapid epinephrine administration, namely as soon as possible, is known to increase the chance of survival in pediatric cardiac arrest and it is now reflected in the PALS guidelines (27). For every 1 min delay in epinephrine administration, survival odds decrease by 9% for pediatric cardiac arrest patients and odds decrease 57% when epinephrine is administered after 10 min from paramedic arrival (4).
In our study, almost half of the events (49.0%) had a delay in vascular access. In order to administer epinephrine, vascular access needs to be achieved (20). In the pediatric population, obtaining vascular access can be problematic due to the limited exposure of pediatric resuscitation and challenging anatomy in the poorly perfused patient; thus, this task can be time-consuming, and may distract from high quality CPR. IOs are an alternative route to IVs that are easier and, therefore, quicker to secure but have not been shown to improve cardiac arrest outcomes (28–30). As mentioned previously, IOs had a higher initial success rate (96.7%) in our study compared to IV initial attempts (61.5%). Interestingly, the presence of a caregiver, which is common in POHCA, has been shown to delay the time to IO insertion (31). In our study, bystanders, who were often caregivers, were present for during paramedic resuscitation in 78.4% of events. Therefore, there is a need to investigate the barriers to epinephrine administration and create opportunities for other modes of rapid epinephrine delivery, such as an intramuscular route.
In our study, ROSC was higher in patients who had at least one C-DEV (p < 0.05), which we found to be mainly due to vascular access or medication deviations. If the deviation was due to a delay in vascular access or medication administration, this may have translated to reduced interruptions to high quality CPR. Bobrow et al. demonstrated a 4.0% increase in survival to hospital discharge when implementing a minimally interrupted cardiac resuscitation (32). Others have demonstrated that prolonged interruptions to chest compressions are negatively associated with survival (33). Our local ROSC rate is higher than reported in other studies (4, 5, 34), but this is unlikely to be entirely explained by the presumed focus on early high-quality CPR at the expense of vascular access and medication administration.
Although our local ROSC rate was higher than reported studies, the local survival rate was lower compared to Japan and other countries where paramedics do not administer epinephrine (26, 35). A nation-wide study conducted in Japan discovered that spending <5 min on scene for young children and <10 min on scene for older children was associated with higher rates of survival to hospital discharge, regardless of neurological status (26). Because epinephrine is administered 1% of the time on scene in Japan (26), a shorter scene time likely resulted in shorter time to epinephrine administration in the emergency department, which may explain this finding. Another study analyzed North American regional variation in POHCA survival to hospital discharge and discovered that regions with the greatest improvement in survival outcomes had increased bystander CPR, shockable rhythms, and EMS-witnessed cardiac arrest (2). The higher ROSC rate locally is more likely to be attributable to a combination of MLPS interventions such as epinephrine administration, early high-quality CPR, and regular rhythm checks. This group of interventions performed by paramedics may be more important than any individual intervention paired with bystander CPR; however, additional research into post-ROSC factors' impact on survival is required to evaluate the lower local survival rate.
This was a single paramedic agency study with a relatively small convenience sample. A larger sample size is needed to adequately determine whether a link between important deviations and survival exists. There are inherent limitations that occur in retrospective observational studies. Though ACR source data recording was inconsistent at times, the key Utstein variables were collected prospectively through the CanROC Registry in a consistent manner. Data were reviewed from multiple sources, which ensured a higher degree of accuracy and completeness. The definitions used for data collection were object, not subjective, to reduce bias.
In this retrospective observational study, we discovered that the local POHCA patient and arrest characteristics are comparable to other regions. The MLPS response to POHCA is variable. We reported a high rate of ROSC, but a low rate of survival to hospital discharge. Deviations from MLPS protocols were low relative to the number of potential deviations that can occur in a resuscitation. The study was underpowered for its primary outcome of survival. Although time to epinephrine administration was often delayed, it was better than other reported regions. Future studies should explore the modifiable barriers to rapid epinephrine administration, the optimization of scene time, and the local in-hospital management of POHCA to further investigate opportunities to improve health outcomes.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
KM, SC, NO, and JT contributed to the design of the study. SC and NO organized the database. KM and KG contributed to data collection. MM performed statistical analysis. KM wrote the first draft of the manuscript. All authors contributed to the article and approved the submitted version.
This project was partially funded by the Schulich School of Medicine Summer Research Training Program.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors would like to acknowledge the Middlesex-London Paramedic Services for their guidance. We also thank Schulich School of Medicine and Dentistry Summer Research Training Program for their funding support. The sponsors were not involved in the study design, data collection, analysis or interpretation, nor the writing of the manuscript.
1. Gerein RB, Osmond MH, Stiell IG, Nesbitt LP, Burns S. What are the etiology and epidemiology of out-of-hospital pediatric cardiopulmonary arrest in Ontario, Canada? Acad Emerg Med. (2006) 13:653–8. doi: 10.1197/j.aem.2005.12.025
2. Fink EL, Prince DK, Kaltman JR, Atkins DL, Austin M, Warden C, et al. Unchanged pediatric out-of-hospital cardiac arrest incidence and survival rates with regional variation in North America. Resuscitation. (2016) 2016:121–8. doi: 10.1016/j.resuscitation.2016.07.244
3. Moler FW, Donaldson AE, Meert K, Brilli RJ, Nadkarni V, Shaffner DH, et al. Multicenter cohort study of out-of-hospital pediatric cardiac arrest. Crit Care Med. (2011) 39:141–9. doi: 10.1097/CCM.0b013e3181fa3c17
4. Hansen M, Schmicker RH, Newgard CD, Grunau B, Scheuermeyer F, Cheskes S, et al. Time to epinephrine administration and survival from nonshockable out-of-hospital cardiac arrest among children and adults. Circulation. (2018) 137:2032–40. doi: 10.1161/CIRCULATIONAHA.117.033067
5. Tijssen JA, Prince DK, Morrison LJ, Atkins DL, Austin MA, Berg R, et al. Time on the scene and interventions are associated with improved survival in pediatric out-of-hospital cardiac arrest. Resuscitation. (2015) 94:1–7. doi: 10.1016/j.resuscitation.2015.06.012
6. Grunau B, Kime N, Leroux B, Rea T, Van Belle G, Menegazzi JJ, et al. Association of intra-arrest transport vs continued on-scene resuscitation with survival to hospital discharge among patients with out-of-hospital cardiac arrest. J Am Med Assoc. (2020) 324:1058–67. doi: 10.1001/jama.2020.14185
7. Banerjee PR, Ganti L, Pepe PE, Singh A, Roka A, Vittone RA. Early on-scene management of pediatric out-of-hospital cardiac arrest can result in improved likelihood for neurologically-intact survival. Resuscitation. (2019) 135:162–7. doi: 10.1016/j.resuscitation.2018.11.002
8. Duff JP, Topjian AA, Berg MD, Chan M, Haskell SE, Hoyner BL, et al. 2019 American Heart Association focused update on pediatric basic life support: an update to the American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. (2019) 140:915–21. doi: 10.1161/CIR.0000000000000736
9. Kirves H, Skrifvars MB, Vähäkuopus M, Ekström K, Martikainen M, Castren M. Adherence to resuscitation guidelines during prehospital care of cardiac arrest patients. Eur J Emerg Med. (2007) 14:75–81. doi: 10.1097/MEJ.0b013e328013f88c
10. Wolfe HA, Morgan RW, Zhang B, Topjian AA, Fink EL, Berg RA, et al. Deviations from AHA guidelines during pediatric cardiopulmonary resuscitation are associated with decreased event survival. Resuscitation. (2020) 149:89–99. doi: 10.1016/j.resuscitation.2020.01.035
11. Bahr N, Meckler G, Hansen M, Guise J-M. Evaluating pediatric advanced life support in emergency medical services with a performance and safety scoring tool. Am J Emerg Med. (2021) 48:301–6. doi: 10.1016/j.ajem.2021.06.061
12. Topjian AA, Scholefield BR, Pinto NP, Fink EL, Buysse CM, Haywood K, et al. P-COSCA (pediatric core outcome set for cardiac arrest) in children. Circulation. (2020) 2020:1–16. doi: 10.1016/j.resuscitation.2021.01.023
13. Nolan JP, Berg RA, Andersen LW, Bhanji F, Chan PS, Donnino MW, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the utstein resuscitation registry template for in-hospital cardiac arrest: a consensus report from a task force of the International Liaison Committee on Resuscitation (American. Circulation. (2019) 140:e746–57. doi: 10.1161/CIR.0000000000000710
15. Emergency Health Regulatory Accountability Branch Ministry Ministry of Health Long-Term Care. Basic Life Support Patient Care Standards Version 3.2. (2019). Available online at: http://www.health.gov.on.ca/en/pro/programs/emergency_health/docs/basic_life_support_patient_care_standards_v3_2_en.pdf (accessed September, 2021).
16. Ministry of Health Long-Term Care. Advanced Life Support Patient Care Standards Comes into Force on Emergency Health Services Branch Ministry of Health and Long-Term Care. (2016). Available online at: https://www.hsnsudbury.ca/portalen/Portals/23/2015-04-20_AdvancedLifeSupportPatientCareStandardsVersion3.3_Comesintoforce-1Feb2016.pdf?ver=2015-05-04-150827-867#page=215 (accessed September, 2021).
17. Nitta M, Iwami T, Kitamura T, Nadkarni VM, Berg RA, Shimizu N, et al. Age-specific differences in outcomes after out-of-hospital cardiac arrests. Pediatrics. (2011) 128:e812–20. doi: 10.1542/peds.2010-3886
18. Donoghue AJ, Nadkarni V, Berg RA, Osmond MH, Wells G, Nesbitt L, et al. Out-of-hospital pediatric cardiac arrest: an epidemiologic review and assessment of current knowledge. Ann Emerg Med. (2005) 46:512–22. doi: 10.1016/j.annemergmed.2005.05.028
19. Naim MY, Burke RV, McNally BF, Song L, Griffis HM, Berg RA, et al. Association of bystander cardiopulmonary resuscitation with overall and neurologically favorable survival after pediatric out-of-hospital cardiac arrest in the United States a report from the cardiac arrest registry to enhance survival surveillance registry. J Am Med Assoc Pediatr. (2017) 171:133–41. doi: 10.1001/jamapediatrics.2016.3643
20. Atkins DL, Everson-Stewart S, Sears GK, Daya M, Osmond MH, Warden CR, et al. Epidemiology and outcomes from out-of-hospital cardiac arrest in children: the resuscitation outcomes consortium epistry-cardiac arrest. Circulation. (2009) 119:1484–91. doi: 10.1161/CIRCULATIONAHA.108.802678
21. Goto Y, Maeda T, Nakatsu-Goto Y. Decision tree model for predicting long-term outcomes in children with out-of-hospital cardiac arrest: a nationwide, population-based observational study. Crit Care. (2014) 18:cc13951. doi: 10.1186/cc13951
22. Michiels E, Quan L, Dumas F, Rea T. Long-term neurologic outcomes following paediatric out-of-hospital cardiac arrest. Resuscitation. (2016) 102:122–6. doi: 10.1016/j.resuscitation.2016.01.010
23. Ohashi-Fukuda N, Fukuda T, Doi K, Morimura N. Effect of prehospital advanced airway management for pediatric out-of-hospital cardiac arrest. Resuscitation. (2017) 114:66–72. doi: 10.1016/j.resuscitation.2017.03.002
24. Lee J, Yang WC, Lee EP, Huang JL, Hsiao HJ, Lin MJ, et al. Clinical survey and predictors of outcomes of pediatric out-of-hospital cardiac arrest admitted to the emergency department. Sci Rep. (2019) 9:1–9. doi: 10.1038/s41598-019-43020-0
25. Hessulf F, Herlitz J, Rawshani A, Aune S, Israelsson J, Sodersved-Kallestedt ML, et al. Adherence to guidelines is associated with improved survival following in-hospital cardiac arrest. Resuscitation. (2020) 155:13–21. doi: 10.1016/j.resuscitation.2020.07.009
26. Kiyohara K, Okubo M, Komukai S, Izawa J, Gibo K, Matsuyama T, et al. Association Between resuscitative time on the scene and survival after pediatric out-of-hospital cardiac arrest. Circ Rep. (2021) 3:CR-21-0021. doi: 10.1253/circrep.CR-21-0021
27. Lavonas E, Magid D, Aziz K, Berg KM, Cheng A, Hoover AV, et al. Highlights of the 2020 American Heart Association guidelines For CPR and ECC. Am J Hear Assoc. (2020) 53:1689–99. doi: 10.1161/CIR.0000000000000901
28. Clemency B, Tanaka K, May P, Innes J, Zagroba S, Blaszak J, et al. Intravenous vs. intraosseous access and return of spontaneous circulation during out of hospital cardiac arrest. Am J Emerg Med. (2017) 35:222–6. doi: 10.1016/j.ajem.2016.10.052
29. Chreiman KM, Dumas RP, Seamon MJ, Kim PK, Reilly PM, Kaplan LJ, et al. The intraosseous have it: a prospective observational study of vascular access success rates in patients in extremis using video review. J Trauma Acute Care Surg. (2018) 84:558–62. doi: 10.1097/TA.0000000000001795
30. Recher M, Baert V, Escutnaire J, Le Bastard Q, Javaudin F, Hubert H, et al. Intraosseous or peripheral IV access in pediatric cardiac arrest? Results from the French National Cardiac Arrest Registry. Pediatr Crit Care Med. (2021) 2021:286–96. doi: 10.1097/PCC.0000000000002659
31. Lee S, Frey M, Kerrey B, Zhang Y, Byczkowski T, Geis G, et al. Video-based, case-control study of factors associated with intraosseous catheterization during pediatric resuscitation. Ann Emerg Med. (2020) 75:755–61. doi: 10.1016/j.annemergmed.2019.09.005
32. Bobrow BJ, Clark LL, Ewy GA, Chikani V, Sanders AB, Berg RA, et al. Minimally interrupted cardiac resuscitation by emergency medical services for out-of-hospital cardiac arrest. J Am Med Assoc. (2008) 299:1158–65. doi: 10.1001/jama.299.10.1158
33. Brouwer TF, Walker RG, Chapman FW, Koster RW. Association between chest compression interruptions and clinical outcomes of ventricular fibrillation out-of-hospital cardiac arrest. Circulation. (2015) 132:1030–7. doi: 10.1161/CIRCULATIONAHA.115.014016
34. Matsuyama T, Komukai S, Izawa J, Gibo K, Okubo M, Kiyohara K, et al. Pre-hospital administration of epinephrine in pediatric patients with out-of-hospital cardiac arrest. J Am Coll Cardiol. (2020) 75:194–204. doi: 10.1016/j.jacc.2019.10.052
Keywords: pediatric, cardiac arrest, resuscitation, emergency medical services, deviations
Citation: McKenzie K, Cameron S, Odoardi N, Gray K, Miller MR and Tijssen JA (2022) Evaluation of Local Pediatric Out-of-Hospital Cardiac Arrest and Emergency Services Response. Front. Pediatr. 10:826294. doi: 10.3389/fped.2022.826294
Received: 30 November 2021; Accepted: 24 January 2022;
Published: 22 February 2022.
Edited by:
Yan Ren Lin, Changhua Christian Hospital, TaiwanReviewed by:
Javier Urbano, Hospital Universitario Gregorio Marañon, SpainCopyright © 2022 McKenzie, Cameron, Odoardi, Gray, Miller and Tijssen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kate McKenzie, a21ja2VuemllMjAyM0BtZWRzLnV3by5jYQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.