- 1The Second Clinical Medical College, Yangtze University, Jingzhou, China
- 2Department of Pediatrics, The Second People's Hospital of Jingmen, Jingmen, China
Objective: This study aimed to investigate whether the ventilation duration for children undergoing invasive mechanical ventilation (IMV) in pediatric intensive care unit (PICU) is correlated with pediatric sequential organ failure (pSOFA) score, white blood cell (WBC) count, blood lactate level, and duration of fever.
Methods: Retrospectively reviewed that the medical records of patients who received IMV in the PICU of Jingzhou Central Hospital between January 2018 and December 2020. According to the duration of IMV in diagnosis-related groups, these patients were divided into two groups: group A, ventilation duration <96 h, and group B, ventilation duration ≥96 h. Each group's pSOFA scores, WBC counts, blood lactate levels, and durations of fever were compared. Logistic regression analysis was used to analyze the clinical risk factors of ventilation duration ≥96 h, and the receiver operator characteristic (ROC) curve was drawn.
Results: A total of 42 patients were included, including 23 in group A and 19 in group B. The difference in pSOFA score between group A and group B was statistically significant (P < 0.05), while the differences in blood lactate level, duration of fever, and WBC count between the two groups were not statistically significant (P > 0.05). Logistic regression analysis was conducted to analyze the influencing factors of mechanical ventilation duration ≥96 h. An ROC curve was drawn with pSOFA score as a test variable and duration of mechanical ventilation ≥96 h as a state variable, revealing that the area under the curve was 0.76 (SE = 0.075, 95% CI: 0.614–0.906, P = 0.005). The sensitivity and specificity were 68.4 and 73.9%, respectively, and the corresponding pSOFA score was 7.5.
Conclusion: When the pSOFA score ≥8, the risk of mechanical ventilation duration ≥96 h increases.
Introduction
In PICU, ventilation is widely used and recognized as an important auxiliary treatment method. The duration of mechanical ventilation refers to the time patients receive invasive respiratory support through tracheal intubation. However, ventilator use also increases the risk of complications, such as ventilator-associated pneumonia (VAP), right ventricular dysfunction, and respiratory muscle injury (1), prolonging a patient's hospital stay and increasing both medical costs (2) and mortality rates. VAP is the second most common hospital-acquired infection resulting from PICU hospitalization (3). Previous research has found that the longer the duration of mechanical ventilation, the higher the risk of VAP (4). A previous study identified mechanical ventilation duration >96 h as a risk factor of VAP (5), and ventilator-related events have been found to be common in ICU patients with mechanical ventilator duration ≥96 h (6).
With the 2016 release of Sepsis 3.0, which is based on SOFA scores, there was a lack of a scoring system for children. An age-adaptive sequential failure scoring system for children has since been developed based on the SOFA score, in which the scoring of the liver and kidney function, circulatory system, and nervous system of children of different ages were standardized to provide criteria for the diagnosis and severity of sepsis in children. The aim of this system is to address the deficiency in children's diagnosis (7). As of 2018, there are three pSOFA scoring systems: one proposed by Schlapbach et al. (8), one proposed by Matics et al. (9), and one proposed by Shime et al. (10). The first two systems have been verified (11), and the second is widely used in clinical practice, leading to more accurate prediction of mortality rates (12–14).
In the present study, the clinical data of 42 children who received IMV in the PICU of Jingzhou Central Hospital between January 2018 and December 2020, were collected and retrospectively analyzed to identify differences between pSOFA score, WBC count, blood lactate level (within 6 h before intubation), and duration of fever. The objective was to investigate whether the duration of IMV for children in PICUs is correlated with pSOFA score.
Information and Methods
Subjects
Eligible children with mechanical ventilation admitted to the PICU of Jingzhou Central Hospital from January 2018 to December 2020 were selected. Inclusion criteria: (1) clear diagnosis of primary disease; (2) duration of mechanical ventilation ≥24 h; (3) patients with complete data. Exclusion criteria: (1) age < 31 days or > 12 years; (2) patients with surgical disease or surgical operation; (3) patients with midway transfer, abandonment of treatment, or death; (4) patients with incomplete case data.
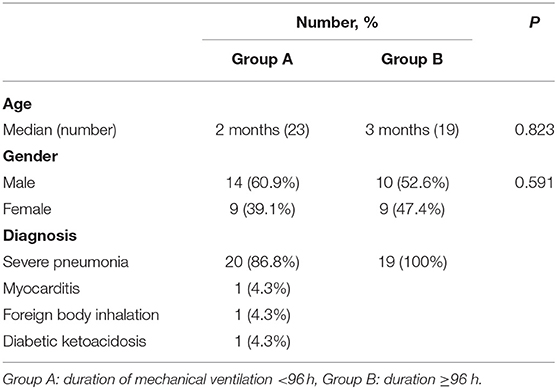
A total of 42 patients were included, including 23 in group A and 19 in group B, aged between 1 and 74 months. The median age of group A was 2 months, that of group B was 3 months, and the difference was statistically significant (P > 0.05). Of these children, 39 had severe pneumonia, 1 had myocarditis, 1 had undergone bronchial foreign-body removal, and 1 had diabetic ketoacidosis. Forty of the children had been given sedatives and analgesic drugs (see Table 1).
Observation Indices
The medical data collected included gender, age, IMV duration, blood lactate level (within 6 h before intubation), duration of fever (from admission to transferring out of PICU), Duration of stay, total bilirubin (within 24 h before intubation), creatinine (within 24 h before intubation), platelet count (within 24 h before intubation), PiO2/FiO2 value or SpO2/FiO2 value, Glasgow coma scale score, blood pressure, use of circulatory support drugs, WBC count (within 24 h before intubation), hospital stay and pSOFA score at the beginning of IMV. According to the duration of mechanical ventilation in diagnosis-related groups, the patients were divided into two groups: group A, ventilation duration <96 h, and group B, ventilation duration ≥96 h.
Statistical Analysis
Statistical analysis was conducted using statistical software SPSS 23.0. Normally distributed measurement data were expressed as mean ± standard deviation (x ± SD) and compared using an independent sample t-test, while non-normally distributed measurement data were expressed as the median and interquartile and compared using a non-parametric Mann–Whitney U test. Logistic regression analysis was conducted to analyze the influencing factors of mechanical ventilation duration ≥96 h. The receiver operator characteristic (ROC) curve method was used to analyze the best cut-off value, sensitivity, and specificity of a predictive exponential equation in predicting pSOFA scores in the case of IMV duration ≥96 h. P < 0.05 was considered statistically significant.
Results
Comparison of Clinical Indexes Between the Two Groups
The pSOFA score was significantly higher in group B than in group A (p < 0.05, Table 2). The differences in blood lactate level, duration of fever, hospital stay, and WBC count between the two groups were not statistically significant (P > 0.05).
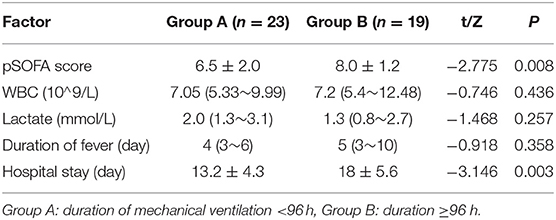
Table 2. Comparison of pSOFA score, lactate level, duration of fever, hospital stay and WBC count between two groups.
Univariate Analysis of Duration of Mechanical Ventilation ≥96 Hours
The related factors with statistical significance between the two groups were used for logistic regression analysis in order to identify the influencing factors of mechanical ventilation duration ≥96 h. The results of the analysis revealed that pSOFA score (OR = 1.694, 95% CI: 1.099–2.610) is an independent risk factor.
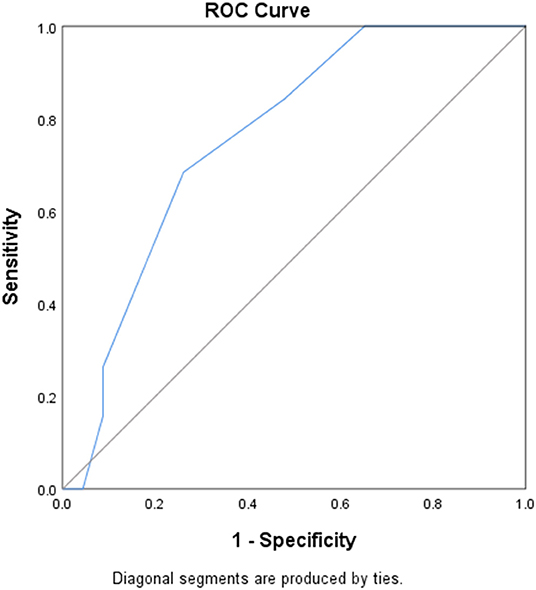
An ROC curve was drawn with pSOFA score as a test variable and duration of mechanical ventilation ≥96 h as a state variable. This revealed that the area under the curve was 0.76 (SE = 0.075, 95% CI: 0.614–0.906, P = 0.005), the sensitivity and specificity were 68.4 and 73.9%, respectively, the Youden's index was 0.423, and the corresponding pSOFA score was 7.5; that is, when pSOFA score ≥ 8, the risk of duration of mechanical ventilation ≥96 h is relatively higher (see Figure 1).
The Mean Duration of Hospital Stay in Children With SOFA Score of More Than or Less Than 8
The mean duration of hospital stay in children with SOFA score of more than 8 was 16.6 ± 5.6 days, that of <8 was 14.4 ± 5.2 days, the different was not statistically significant (P > 0.05, see Table 3).
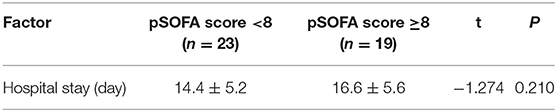
Table 3. The mean duration of hospital stay in children with SOFA score of more than or less than 8.
Discussion
The pSOFA score predicts the severity and prognosis of sepsis in children more accurately than pediatric risk score of mortality and pediatric critical illness score (12–15) and can also be used to predict the outcome of the general PICU population. Furthermore, it is more accurate than systemic inflammatory response syndrome (SIRS) in defining pediatric sepsis (16) and can better predict the new incidence rate or mortality rate of critically ill children within 3 years (17). Matics et al. found that the best threshold of pSOFA for differentiating mortality rate was >8 (9). In another single center study, a pSOFA Score >4 was associated with a significant increase in mortality (18).
In PICU, the use of ventilators is closely related to the occurrence of VAP and other complications. Prolonged mechanical ventilation has been found to increase the use of broad-spectrum antibiotics (19), lengthen the hospitalization duration for children due to longer recovery, and increase the risk of death in children with VAP (20).
In the present study, the best critical value of pSOFA for differentiating ventilation duration ≥96 h was eight points. This is also confirmed to a certain extent by the findings of Matics et al. and Lalitha et al. found that when pSOFA score was more than 8 on both days 1 and 3, the relative risk of prolonged duration of mechanical ventilation was increased (21). When the initial pSOFA score at the beginning of ventilator use is ≥8, the risk of mechanical ventilation duration ≥96 h is higher, so taking effective preventive measures in nursing and treatment can improve patient outcomes (22). For children with a score >8, chest radiographs should be performed 72 h after mechanical ventilation, so that VAP can be detected and treated early.
Blood lactate level is an indicator of hypoxia, cancer (23), and the body's response to an epinephrine infusion can also cause the lactate level to rise (24). Lactate clearance rate has certain significance to evaluate the prognosis and curative effect of critically ill patients, and a decrease in lactate clearance rate can cause a decrease in oxygen metabolism ability, leading to hypoxia and damage in the tissues and organs. Choi et al. found that blood lactate level and mechanical ventilation were significantly correlated with mortality rate (25), and a recent study revealed that 24-h lactate level was an independent predictor of mortality rate, which was positively correlated with pSOFA, indicating that 24-h lactate level into pSOFA score can lead to more accurate prediction (26). Six-hour lactate level has also been found to be better than 0-h lactate level for predicting mortality (13). In the present study, only 0-h lactate level was measured, and it was found that there was no correlation between 0-hlactate level and duration of mechanical ventilation. One study found that 6-h lactate level was associated with mortality and superior to 0-h lactate levels (13). This study did not measure 6-h lactate level and lactate clearance rate, however, so whether 6-h lactate level and lactate clearance rate are related to the duration of mechanical ventilation requires further study.
The present study was a retrospective study and had three limitations: (1) there may have been recall bias and selection bias; (2) the incidence of VAP was not analyzed; (3) the significance of blood lactate level in the judgment of duration of mechanical ventilation in critically ill children is still not clear, for which further research is required.
Conclusion
Logistic regression analysis was used to establish the ROC curve and predict the sensitivity and specificity of pSOFA scores at the beginning of mechanical ventilation, which is of great significance to the clinical development of individualized and standardized preventive treatment measures to reduce the risk of VAP and other mechanical ventilation complications. It was found that, when the pSOFA score ≥ 8, the risk of mechanical ventilation duration ≥96 h increased. Taking active preventive measures early may minimize the incidence of ventilator-associated pneumonia and other complications, shorten the length of the hospital stay for the patient, and reduce costs.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics Statement
The study was conducted in accordance with the Declaration of Helsinki (as was revised in 2013). The study was approved by Ethics Committee of Jingzhou Center Hospital-the Second Clinical Medical College of Yangtze University.
Author Contributions
FL and HQ: conception and design of the research. HQ: acquisition of data. FL: analysis and interpretation of the data. A-ML: statistical analysis, obtaining financing, and critical revision of the manuscript for intellectual content. FL and A-ML: writing of the manuscript. All authors read and approved the final draft.
Funding
This study was funded by the Jingzhou Science and Technology Bureau (No. 2019CC54-03).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We are particularly grateful to all the people who have given us help on our article.
References
1. Withers A, Ching Man TC, D'Cruz R, de Vries H, Fisser C, Ribeiro C, et al. Highlights from the respiratory failure and mechanical ventilation 2020 conference. ERJ Open Res. (2021) 7:00752–2020. doi: 10.1183/23120541.00752-2020
2. Zenteno D, Torres-Puebla G, Navarro X, Rivas C, Tapia J, Rodríguez-Núñez I, et al. Experience in a pediatric prolonged mechanical ventilation unit from a public hospital in chile. Experiencia de una Unidad de Ventilación Mecánica Pediátrica Prolongada en un hospital público de Chile. Arch Argent Pediatr. (2021) 119:25–31. doi: 10.5546/aap.2021.25
3. Kohbodi GA, Rajasurya V, Noor A. Ventilator-Associated Pneumonia. StatPearls Treasure Island, FL: StatPearls Publishing (2020).
4. Chomton M, Brossier D, Sauthier M, Vallières E, Dubois J, Emeriaud G, et al. Ventilator-associated pneumonia and events in pediatric intensive care: a single center study. Pediatr Crit Care Med. (2018) 19:1106–13. doi: 10.1097/PCC.0000000000001720
5. Awasthi S, Tahazzul M, Ambast A, Govil YC, Jain A. Longer duration of mechanical ventilation was found to be associated with ventilator-associated pneumonia in children aged 1 month to 12 years in India. J Clin Epidemiol. (2013) 66:62–6. doi: 10.1016/j.jclinepi.2012.06.006
6. He Q, Wang W, Zhu S, Wang M, Kang Y, Zhang R, et al. The epidemiology and clinical outcomes of ventilator-associated events among 20,769 mechanically ventilated patients at intensive care units: an observational study. Crit Care. (2021) 25:44. doi: 10.1186/s13054-021-03484-x
7. Xiang L, Wang Y, Zhao LB. Pediatrics sequential organ failure assessment in predicting the severity and outcome of sepsis in children: a clinical study. Chin Pediatr Emerg Med. (2020) 27:887–92. Available online at: https://kns.cnki.net/kcms/detail/detail.aspx?FileName=LYYL202012002&DbName=ZHYX2020
8. Schlapbach LJ, Straney L, Bellomo R, MacLaren G, Pilcher D. Prognostic accuracy of age-adapted SOFA, SIRS, PELOD-2, and qSOFA for in-hospital mortality among children with suspected infection admitted to the intensive care unit. Intensive Care Med. (2018) 44:179–88. doi: 10.1007/s00134-017-5021-8
9. Matics TJ, Sanchez-Pinto LN. Adaptation and validation of a pediatric sequential organ failure assessment score and evaluation of the sepsis-3 definitions in critically ill children. JAMA Pediatr. (2017) 171:e172352. doi: 10.1001/jamapediatrics.2017.2352
10. Shime N, Kawasaki T, Nakagawa S. Proposal of a new pediatric sequential organ failure assessment score for possible validation. Pediatr Crit Care Med. (2017) 18:98–9. doi: 10.1097/PCC.0000000000001009
11. Kawasaki T, Shime N, Straney L, Bellomo R, MacLaren G, Pilcher D, et al. Paediatric sequential organ failure assessment score (pSOFA): a plea for the world-wide collaboration for consensus. Intensive Care Med. (2018) 44:995–7. doi: 10.1007/s00134-018-5188-7
12. Kwon R, Koutsogiannaki S, Staffa SJ, Yuki K. The outcomes of pediatric hematopoietic stem cell transplantation recipients requiring intensive care unit admission- a single center experience. Transl Perioper Pain Med. (2019) 6:75–80. doi: 10.31480/2330-4871/092
13. Jaiswal P, Dewan P, Gomber S, Banerjee BD, Kotru M, Malhotra RK, et al. Early lactate measurements for predicting in-hospital mortality in paediatric sepsis. J Paediatr Child Health. (2020) 56:1570–6. doi: 10.1111/jpc.15028
14. Kim K, Kim S, Lee JW, Yoon JS, Chung NG, Cho B. Prognostic factors of ICU mortality in pediatric oncology patients with pulmonary complications. J Pediatr Hematol Oncol. (2020) 42:266–70. doi: 10.1097/MPH.0000000000001616
15. Zhou LB, Chen J, DU XC, Wu SY, Bai ZJ, Lyu HT. Value of three scoring systems in evaluating the prognosis of children with severe sepsis. Zhongguo Dang Dai Er Ke Za Zhi. (2019) 21:898–903. doi: 10.7499/j.issn.1008-8830.2019.09.011
16. Mohamed El-Mashad G, Said El-Mekkawy M, Helmy Zayan M. La escala pediátrica de evaluación del fallo multiorgánico secuencial (pSOFA): una nueva escala de predicción de la mortalidad en la unidad de cuidados intensivos pediátricos [Paediatric sequential organ failure assessment (pSOFA) score: a new mortality prediction score in the paediatric intensive care unit]. An Pediatr. (2020) 92:277–85. doi: 10.1016/j.anpedi.2019.05.018
17. Matics TJ, Pinto NP, Sanchez-Pinto LN. Association of organ dysfunction scores and functional outcomes following pediatric critical illness. Pediatr Crit Care Med. (2019) 20:722–7. doi: 10.1097/PCC.0000000000001999
18. Humoodi MO, Aldabbagh MA, Salem MM, Al Talhi YM, Osman SM, Bakhsh M, et al. Epidemiology of pediatric sepsis in the pediatric intensive care unit of king Abdulaziz Medical City, Jeddah, Saudi Arabia. BMC Pediatr. (2021) 21:222. doi: 10.1186/s12887-021-02686-0
19. Chang I, Schibler A. Ventilator associated pneumonia in children. Paediatr Respir Rev. (2016) 20:10–16. doi: 10.1016/j.prrv.2015.09.005
20. Raymond J, Aujard Y. Nosocomial infections in pediatric patients: a European, multicenter prospective study. European Study Group. Infect Control Hosp Epidemiol. (2000) 21:260–3. doi: 10.1086/501755
21. Lalitha AV, Satish JK, Reddy M, Ghosh S, George J, Pujari C. Sequential organ failure assessment score as a predictor of outcome in sepsis in pediatric intensive care unit. J Pediatr Intensive Care. (2021) 10:110–7. doi: 10.1055/s-0040-1714705
22. de Neef M, Bakker L, Dijkstra S, Raymakers-Janssen P, Vileito A, Ista E. Effectiveness of a ventilator care bundle to prevent ventilator-associated pneumonia at the picu: a systematic review and meta-analysis. Pediatr Crit Care Med. (2019) 20:474–80. doi: 10.1097/PCC.0000000000001862
23. Singh M, Ajmeri AN, Suliman MS, Zaheer K, Al-Astal AK. A challenging case of coexisting type A and type B lactic acidosis: a case report. Cureus. (2019) 11:e3944. doi: 10.7759/cureus.3944
24. Wutrich Y, Barraud D, Conrad M, Cravoisy-Popovic A, Nace L, Bollaert PE, et al. Early increase in arterial lactate concentration under epinephrine infusion is associated with a better prognosis during shock. Shock. (2010) 34:4–9. doi: 10.1097/SHK.0b013e3181ce2d23
25. Choi SJ, Ha EJ, Jhang WK, Park SJ. Elevated central venous pressure is associated with increased mortality in pediatric septic shock patients. BMC Pediatr. (2018) 18:58. doi: 10.1186/s12887-018-1059-1
Keywords: duration of mechanical ventilation, pSOFA score, lactate, PICU, operator characteristic
Citation: Lu F, Qin H and Li A-M (2022) The Correlation Between Mechanical Ventilation Duration, Pediatric Sequential Organ Failure Assessment Score, and Blood Lactate Level in Children in Pediatric Intensive Care. Front. Pediatr. 10:767690. doi: 10.3389/fped.2022.767690
Received: 31 August 2021; Accepted: 21 January 2022;
Published: 14 March 2022.
Edited by:
Brenda M. Morrow, University of Cape Town, South AfricaReviewed by:
Başak Nur Akyildiz, Erciyes University, TurkeyThomas Vincent Brogan, Seattle Children's Hospital, United States
Copyright © 2022 Lu, Qin and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ai-Min Li, bGlhaW1pbmRyQDE2My5jb20=
†These authors have contributed equally to this work
 Fang Lu
Fang Lu Hua Qin2†
Hua Qin2† Ai-Min Li
Ai-Min Li