- Division of Pulmonology and Sleep Medicine, Nemours Children's Hospital, Wilmington, DE, United States
Background: Children with Trisomy 21 (T21) are at an increased risk of sleep-disordered breathing (SDB), which can impact daily functioning and cause other health complications. Accordingly, it is imperative to diagnose and treat SDB in this population. Current guidelines recommend screening polysomnogram by age 4 or sooner if clinically indicated. There are limited published studies describing characteristics of SDB in children with T21, particularly in infants and young children.
Objective: The objective of this study is to characterize SDB and treatment modalities in infants and young children with T21.
Methods: This is a retrospective review of a cohort of children (≤60 months of age) with T21 who completed a polysomnogram (PSG) between 2015 and 2020 at a pediatric referral center. Demographic information, relevant medical history, polysomnography parameters, and treatment details of these children were collected from EMR. Descriptive and comparative statistics were calculated for the cohort; additional subgroup analysis was completed by age 0–35 months and 36–60 months.
Results: Most of the cohort met criteria for sleep apnea (84.1%), and airway surgery was the most common treatment modality (71.4%). The mean AHI was high (21.4 events/hour) with a trend towards hypoventilation (mean EtCO2 = 55.9 mmHg; mean percentage of TST with EtCO2 > 50 mmHg 20.8%). Mean arousal index was elevated (32 events/hour). There were no significant differences in SDB by age when we compared children 0–35 months and 36–60 months.
Conclusions: This cohort of referred children with T21 showed high prevalence of SDB with a trend towards hypoventilation and disrupted sleep quality with no significant differences by age. These data highlight the importance of maintaining a high index of suspicion for SDB in young patients with T21 and obtaining PSG testing to characterize sleep and breathing.
Introduction
Sleep disordered breathing (SDB) ranges from primary snoring to obstructive sleep apnea (OSA) and may cause disruptions in sleep quality as well as gas exchange abnormalities. Multiple studies have reported high prevalence rates of SDB including Obstructive Sleep Apnea (OSA) in children with Trisomy 21 (T21) ranging from 43% to 96% (1–4). This prevalence is much higher compared with the general pediatric population (5, 6). There are several anatomical features and associated comorbidities in children with T21 which predispose this population to SDB. Multiple anatomic features including glossoptosis, enlarged lingual tonsils, midface hypoplasia, relative macroglossia and hypotonia are associated with SDB (7, 8). Children with T21 also are more likely to have co-morbidities including obesity, hypothyroidism, and gastrointestinal and cardiac co-morbidities, which infer increased risk for SDB (8–10).
Undiagnosed and untreated SDB is associated with consequent fatigue, neurocognitive issues, cardiac conditions, and failure to thrive. The neurocognitive sequelae include behavioral difficulties, problems with executive dysfunction, difficulty planning, poor memory, lowered verbal IQ, and limited cognitive flexibility (11–16). The cardiac consequences may include pulmonary hypertension and heart failure (16).
Current guidelines recommend screening polysomnogram (PSG) for children with T21 at the age of 4 years or earlier if there are clinical signs and symptoms (17). There are limited studies evaluating SDB in younger children (≤5 years old) with T21. Few studies done in younger children with T21 have found high rates of OSA; other studies report not only higher rates of prevalence of OSA but also a more severe degree of OSA in infants with T21 (1, 18).
The goal of this retrospective study is to describe clinical characteristics, PSG data, comorbid conditions, and treatment modalities in young children with Trisomy 21 (<60 months old) who had an initial baseline PSG performed at a single referral institution. Additional subgroup analysis separated the data by age group (0–35 months and 36–60 months).
Methods
Patient population
This IRB-approved, retrospective review examined children with T21 who were 60 months old or younger at the time of first PSG between 2015 and 2020 and included both symptomatic and asymptomatic patients. Eligible patients were identified via review of EMR (electronic medical record) with problem list containing ICD code for Trisomy 21 (Q90.0) at the time of the PSG and confirmed via manual chart review by a member of the research team.
Data collection
Data collected for this study consisted of demographic information, relevant medical history, PSG data, and treatment information. All data were extracted retrospectively from the EMR via chart review by a member of the research team. PSG data was collected via sleep study report available in the EMR. All patients included in this study completed a clinical office visit with a pediatric sleep specialist prior to the PSG which includes clinical exam and documentation of relevant medical and surgical history. These visits are typically completed <2 months prior to the PSG. Clinical and demographic data were collected for this project via review of the problem list and documentation in the EMR at the time of the office visit.
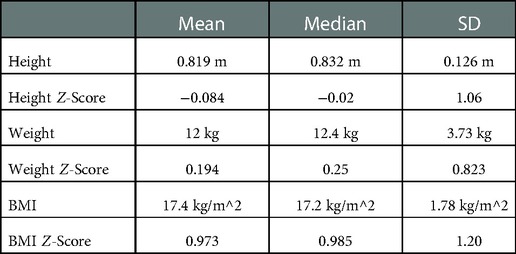
The demographic information consisted of age, sex, race, ethnicity, height, height z-score, weight, weight z-score, BMI, BMI z-score, medications at the time of the PSG, and tobacco smoke exposure. Z-scores for height and weight were determined using Trisomy 21 growth charts while z-scores for BMI were determined using WHO growth charts.
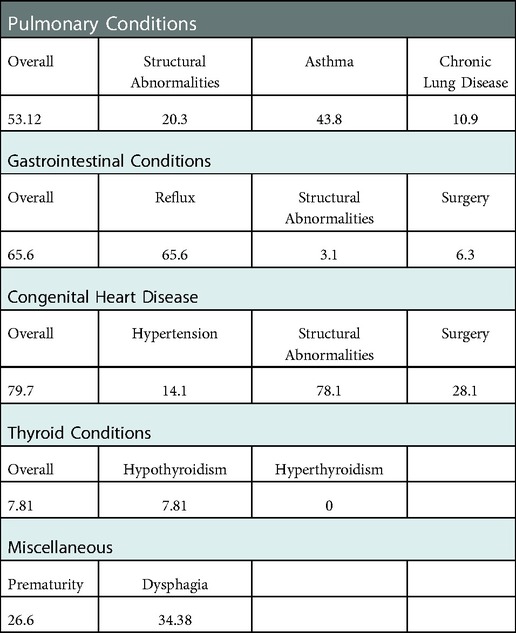
Relevant medications included nasal steroids, antihistamines, montelukast, melatonin and other non-prescription sleep aids, inhaled medications, histamine-2 antagonists (hist-2), and proton pump inhibitors (PPI). These data were collected from the EMR as documented in the medication review at the clinical encounter immediately prior to the PSG. Relevant medical history included the existence of relevant pre-existing conditions, feeding tube prior to the first PSG, ENT visits, ENT surgeries prior to the first PSG, ENT surgery at any time, prematurity, pulmonary conditions, dysphagia and other gastrointestinal conditions, cardiac disease, thyroid conditions, and neurodevelopmental conditions. The comorbidities were defined based on review of the problem list in the EMR at the time of the visit as well as documented in the clinical notes at the time of the clinical visit immediately prior to the PSG. Prematurity was defined as being born prior to gestational age of 37 weeks. Pulmonary conditions consisted of (1) history of asthma or recurrent wheezing that was diagnosed by a physician or for which the patient was prescribed pulmonary inhaled medications, (2) bronchopulmonary dysplasia (BPD) or chronic lung disease of prematurity, and (3) structural airway abnormalities, specifically oropharyngeal malformations, laryngomalacia, laryngeal clefts, vocal cord paralysis, tracheomalacia, bronchomalacia, and tracheoesophageal fistula (TEF). Gastrointestinal conditions consisted of (1) reflux that was diagnosed by a physician or for which the patient was prescribed reflux medications, (2) gastrointestinal surgical repair, and (3) structural GI anomalies, specifically duodenal atresia, duodenal stenosis, TEF, intestinal malrotation, and Hirschsprung's disease. Cardiac conditions consisted of (1) pulmonary hypertension, (2) surgical repair of structural heart defects, and (3) congenital structural heart defects, specifically ASD, VSD, AV canal, TOF, coarctation of aorta, and PDA. PFOs were not included as congenital structural heart defects. Thyroid conditions consisted of hypothyroidism and hyperthyroidism. Neurodevelopmental conditions consisted of autism and ADHD. ENT surgery included myringotomy tube placement, adenoidectomy, tonsillectomy, adenotonsillectomy, and supraglottoplasty.
PSG was performed in an American Academy of Sleep Medicine-accredited sleep laboratory at Nemours Children's Hospital, Delaware. PSG is the gold standard for the diagnosis of OSA (17). Electroencephalography, electrooculography, electromyography, and electrocardiography were continuously recorded throughout the PSG. Respiratory effort was measured via respiratory inductance plethysmography and oxygen saturation was measured via a finger probe on a pulse oximeter. A nasal pressure cannula and a thermistor measured airflow, and snoring was measured via a microphone. The patients were monitored using by a polysomnographic technician during the entire duration of the study in a dark and comfortable environment. The raw data was reviewed and interpreted by a pediatric board-certified sleep medicine physician. Respiratory events were scored according to the American Academy of Sleep Medicine guidelines using pediatric scoring (19).
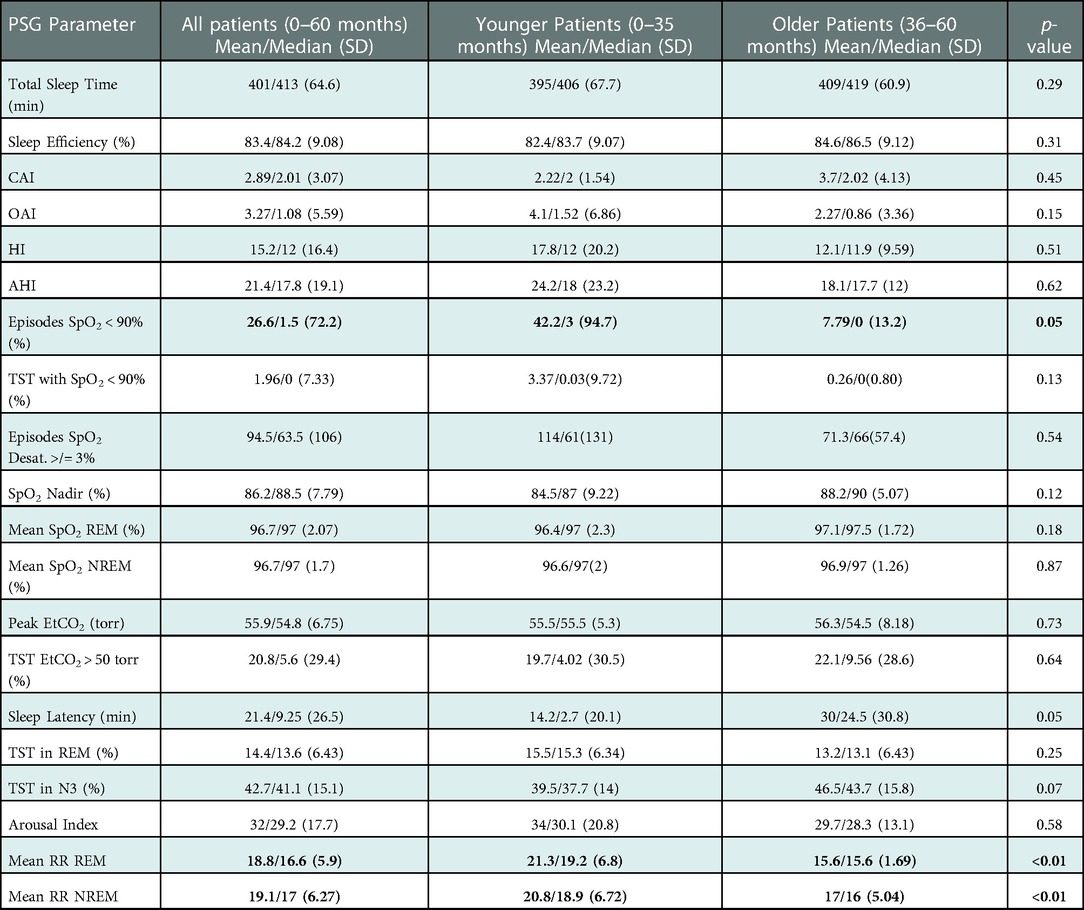
The PSG data collected included respiratory and sleep architecture data. The respiratory parameters consisted of the central apnea index (CAI), obstructive apnea index (OAI), hypopnea index (HI), apnea-hypopnea index (AHI), number of episodes of oxygen saturations less than 90% (# Episodes SpO2 < 90%), the percent of total sleep time spent below 90% saturation (TST with SpO2 < 90%), number of episodes of relative oxygen desaturations ≥3% (Episodes SpO2 desaturation ≥ 3%), SpO2 nadir, mean SpO2 in REM, mean SpO2 in NREM, peak End tidal CO2 (EtCO2) level, percent of total sleep time spent with a peak EtCO2 level above 50 torr (TST w/EtCO2 > 50 torr), periodic breathing time (PBT), percent of total sleep time spent with periodic breathing (TST with PBT), mean respiratory rate in REM (MRR REM), and mean respiratory rate in NREM (MRR NREM), periodic limb movements of sleep index (PLMI), periodic limb movements associated with arousals (PLM assoc. with arousals) for children above the age 2 years. Sleep architecture included the patient's total sleep time (TST), sleep efficiency (SE), sleep latency, percentage of TST in REM, percentage of TST in N3, and arousal index. Sleep efficiency was considered decreased if it was <90%. Severe sleep apnea was noted if the AHI was ≥10/hour. Potential treatment options were supplemental oxygen, airway surgery, positive airway pressure (PAP), intranasal corticosteroids, and other. Airway surgery consisted of adenoidectomy alone, adenotonsillectomy, and supraglottoplasty.
Analysis
All analysis was performed using group-generated R scripts. Descriptive statistics consisted of mean, median, standard deviation, and percentages where appropriate. In subgroup analysis, the younger (0–35 months) patients were compared to the older (36–60 months) patients using 2-sample Wilcoxon-rank sum test after tests for normality were performed using the Shapiro-Wilk test. A p value of ≤0.05 was considered statistically significant.
Results
68 children were found to fit all inclusion criteria; four were excluded due to incomplete PSG data. Therefore, the cohort analyzed consisted of a baseline PSG in 64 children with T21.
Demographic and clinical data
The full cohort was predominantly female (54.7%), white (61.9%), and non-Hispanic or Latino (71.9%). 14.3% of the cohort were black, and 22.2% were listed as “other.” The mean age of the participants was 30.8 months (median = 30.5, SD = 16.4). See Table 1 for descriptive statistics for height, weight, and BMI and z-scores for those parameters. 63.5% were taking relevant medications with the most common being inhaled respiratory therapies (39.7%). Roughly a quarter had a history of tobacco smoke exposure.
Comorbid conditions
The most prevalent comorbidities include congenital heart disease (78.1%) and asthma/wheezing history (43.8%). Table 2 details the percentage of patients with each comorbid condition.
Relevant medical and surgical history
In this cohort, many children were referred for PSG with history of airway concerns including enlarged tonsils (62.5%), snoring (81.2%), and restless sleep (59.4%). 18.8% were considered to be asymptomatic and referred due to age and history of Trisomy 21. Noisy breathing was present in approximately 25% of the population. Asthma or wheezing was present in 43.8% of patients of which most (89.3%) were treated with inhaled medications. Reflux was diagnosed in 64.6%, and 42.9% were treated with medical therapy. Roughly half of the patients had a feeding tube (either nasogastric tube or surgically-placed tube) at some point prior to the PSG.
PSG respiratory parameters
Table 3 contains respiratory parameters of the PSG. In general, these patients had high rates of obstructive apnea and hypopnea events (mean = 21.4, median = 17.8, SD = 19.1). The hypopnea index is high (HI: mean = 15.2, median = 12, SD = 16.4). The SpO2 nadir was moderately reduced with a mean value of 86.2% (median = 88.5%, SD = 7.8%); however most had saturations above 90% for majority of the study (Duration of SpO2 below 90%; mean = 1.96% of TST, median = 0% of TST, SD = 7.33% of TST). Mean oxygen saturation recorded was 97% (median = 97%, SD = 2.1% in REM; 1.7% in NREM). In addition to experiencing frequent apnea and hypopnea episodes, the patients also demonstrated borderline abnormal ventilation an elevated mean peak EtCO2 (mean = 55.9 torr, median = 54.8 torr, SD = 6.75 torr) and percentage of time above 50 torr (mean = 20.8%, median = 5.6%, SD = 29.4%).
PSG sleep architecture
Table 3 includes all descriptive statistics for the cohort's sleep architecture. The majority (94%) had TST >300 min. 78.1% of studies showed decreased sleep efficiency of <90%. The sleep latency (mean = 21.4 min, median = 9.25 min, SD = 26.5 min) was within normal range, but the arousal index (mean = 32, median = 29.2, SD = 17.7) was elevated (20). The patients spent more time in N3 (mean = 42.7%, median = 41.1%, SD 15.1%) and less time in REM (mean = 14.4%, median = 13.6%, SD = 6.4%) than expected for the mean age (20).
Treatment modalities
A majority of the cohort was found to have OSA (84.1%), and 67.2% had severe sleep apnea (defined as AHI >10 events/hour). Airway surgery was the most common treatment choice (65.1%) followed by intranasal corticosteroids (11.1%), PAP therapy (6.4%), other (4.8%), and supplemental oxygen (3.2%). Many patients (12.5%) received more than one treatment modality. Approximately 30% of patients were followed with clinical observation after the baseline PSG.
Subgroup analysis by age
The entire cohort was sub-divided into younger (0–35 months of age) and older (36–60 months of age) cohorts with 35 and 29 patients, respectively. There were no significant differences in the majority of PSG parameters and specifically no differences in rates of OSA. See Table 3 for full comparison of all PSG parameters between the two groups. One notable difference between the two group's PSG parameters was in the number of desaturations less than 90% with the younger cohort having a mean of 42.2 compared to the older group having a mean of 7.8 (p = 0.05). As expected physiologically, the mean respiratory rates were higher in younger cohort in both REM (21.3 vs. 15.6; p < 0.01) and NREM (20.8 vs. 17; p < 0.01) Another important difference between the two cohorts was the diversity of treatment modalities. The older cohort almost exclusively underwent an AT or clinical observation with only 3.45% of patients receiving an alternative strategy. In comparison, 28.6% of the younger cohort received treatment other than an AT or clinical observation (including supplemental oxygen, CPAP).
Discussion
In this cohort of children <60 months with T21, a majority (84%) demonstrated OSA on baseline PSG. Of these, 67.2% met criteria for severe OSA, which is similar to prior studies showing high rates of SDB in this population (2, 4, 9, 21). The high rate of OSA was not age-dependent with high rates described in both the 0–35 month and 36–60 month subgroups.
Polysomnogram data in infants and younger children with T21 have not been well studied; however studies published in these young age groups show high prevalence of OSA (21, 22). In this study, not only were there high rates of OSA in the younger group, but also high rates of increased severity of OSA with a mean AHI of 24.2. The combined cohort had borderline abnormal gas exchange with a trend toward hypoventilation (peak EtCO2: mean = 55.9 torr, median = 54.8 torr, SD = 6.75 torr; TST with EtCO2 > 50 torr: mean = 20.8%, median = 5.6%, SD = 29.4%).
Sleep disturbances were also prevalent in this cohort. Similar to prior studies, this cohort demonstrated disrupted sleep with high mean arousal index and abnormal sleep architecture with increased duration of N3 sleep and reduced duration of REM. The mean sleep efficiency of the cohort was lower than expected. Testing procedures and other behavioral comorbidities may be potential underlying factors contributing to this finding. Notably, most children (94%) were able to sleep for >300 min.
The higher rates of OSA may be attributed to a medically-complex referred population analyzed in our cohort. There were high rates of comorbidities with nearly all patients (95.3%) having one comorbid condition. Overall, congenital heart defects were the most common comorbidity (78.1%), but reflux (65.62%) and asthma/wheezing (43.8%) were also very prevalent in this cohort, both which may predispose to SDB. Compared to other published studies, this cohort includes large number of infants and children with T21 who are surgically naïve (with the exception of one child who had a prior supraglottoplasty). In addition, this study data adds to further characterize various comorbidities and sleep disordered breathing as well as detailing sleep architecture in younger children and infants with T21.
Overall, the prevalence of OSA was high in this cohort of referred children with T21, including younger children and infants aged 0–35 months. These results call for continued diligent screening for sleep disordered breathing children with T21 beginning in infancy and maintaining high level of clinical suspicion for sleep apnea in infants and younger toddlers, as it is known that parental report of sleep symptoms tend to underestimate PSG results. Also, given the high prevalence of associated Pulmonary, GI and Cardiac conditions in this cohort, there should be a high index of suspicion of SDB in patients with these comorbidities. Further studies are warranted to determine which comorbidities may cause highest risk of SDB in this unique population.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving human participants were reviewed and approved by Nemours, Wilmington, Delaware. Written informed consent from the participants’ legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
All authors contributed to data collection; data analysis; manuscript writing and edits. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Anand V, Shukla G, Gupta N, Gupta A, Sapra S, Gulati S, et al. Association of sleep apnea with development and behavior in down syndrome: a prospective clinical and polysomnographic study. Pediatr Neurol. (2021) 116:7–13. doi: 10.1016/j.pediatrneurol.2020.10.007
2. Nerfeldt P, Sundelin A. Obstructive sleep apnea in children with down syndrome - prevalence and evaluation of surgical treatment. Int J Pediatr Otorhinolaryngol. (2020) 133: 109968. doi: 10.1016/j.ijporl.2020.109968
3. Heubi CH, Knollman P, Wiley S, Shott SR, Smith DF, Ishman SL, et al. Sleep architecture in children with down syndrome with and without obstructive sleep apnea. Otolaryngol Neck Surg. (2021) 164(5):1108–15. doi: 10.1177/0194599820960454
4. de Miguel-Díez J, Villa-Asensi JR, Álvarez-Sala JL. Prevalence of sleep-disordered breathing in children with down syndrome: polygraphic findings in 108 children. Sleep. (2003) 26(8):1006–9. doi: 10.1093/sleep/26.8.1006
5. Nehme J, LaBerge R, Pothos M, et al. Predicting the presence of sleep-disordered breathing in children with down syndrome. Sleep Med. (2017) 36:104–8. doi: 10.1016/j.sleep.2017.03.032
6. Marcus CL. Sleep disordered breathing in children. Curr Opin Pediatr. (2000) 12(3):208–12. doi: 10.1097/00008480-200006000-00005
7. Donnelly LF, Shott SR, LaRose CR, Chini BA, Amin RS. Causes of persistent obstructive sleep apnea despite previous tonsillectomy and adenoidectomy in children with down syndrome as depicted on static and dynamic cine MRI. Am J Roentgenol. (2004) 183(1):175–81. doi: 10.2214/ajr.183.1.1830175
8. Basil JS, Santoro SL, Martin LJ, Healy KW, Chini BA, Saal HM. Retrospective study of obesity in children with down syndrome. J Pediatr. (2016) 173:143–8. doi: 10.1016/j.jpeds.2016.02.046
9. Simpson R, Oyekan AA, Ehsan Z, Ingram DG. Obstructive sleep apnea in patients with down syndrome: current perspectives. Nat Sci Sleep. (2018) 10:287–93. doi: 10.2147/NSS.S154723
10. Zhang M, Zhang W, Tan J, Zhao M, Zhang Q, Lei P. Role of hypothyroidism in obstructive sleep apnea: a meta-analysis. Curr Med Res Opin. (2016) 32(6):1059–64. doi: 10.1185/03007995.2016.1157461
11. Rosen D. Management of obstructive sleep apnea associated with down syndrome and other craniofacial dysmorphologies. Curr Opin Pulm Med. (2011) 17(6):431–6. doi: 10.1097/MCP.0b013e32834ba9c0
12. Breslin J, Spanò G, Bootzin R, Anand P, Nadel L, Edgin J. Obstructive sleep apnea syndrome and cognition in down syndrome. Dev Med Child Neurol. (2014) 56(7):657–64. doi: 10.1111/dmcn.12376
13. Joyce A, Elphick H, Farquhar M, Gringras P, Evans H, Bucks RS, et al. Obstructive sleep apnoea contributes to executive function impairment in young children with down syndrome. Behav Sleep Med. (2020) 18(5):611–21. doi: 10.1080/15402002.2019.1641501
14. Freezer NJ, Bucens IK, Robertson CF. Obstructive sleep apnoea presenting as failure to thrive in infancy. J Paediatr Child Health. (1995) 31(3):172–5. doi: 10.1111/j.1440-1754.1995.tb00779.x
15. Carskadon MA, Pueschel SM, Millman RP. Sleep-disordered breathing and behavior in three risk groups: preliminary findings from parental reports. Childs Nerv Syst. (1993) 9(8):452–7. doi: 10.1007/BF00393547
16. Lal C, White DR, Joseph JE, van Bakergem K, LaRosa A. Sleep-disordered breathing in down syndrome. Chest. (2015) 147(2):570–9. doi: 10.1378/chest.14-0266
17. Marcus CL, Chapman D, Ward SD. Clinical practice guideline: diagnosis and management of childhood obstructive sleep apnea syndrome. Pedatrics. (2002) 109(4):704–12. doi: 10.1542/peds.109.4.704
18. Shires CB, Anold SL, Schoumacher RA, Dehoff GW, Donepudi SK, Stocks RM. Body mass index as an indicator of obstructive sleep apnea in pediatric down syndrome. Int J Pediatr Otorhinolaryngol. (2010) 74(7):768–72. doi: 10.1016/j.ijporl.2010.03.050
19. Berry RB, Brooks R, Gamaldo CE, Harding SM, Lloyd RM, Quan SF, et al. The AASM manual for the scoring of sleep and associated events: rules, terminology, and technical specifications. Am Acad Sleep Med. (2015) 2:665–6. doi: 10.5664/jcsm.6576
20. Beck SE, Marcus CL. Pediatric polysomnography. Sleep Med Clin. (2009) 4(3):393–406. doi: 10.1016/j.jsmc.2009.04.007
21. Goffinski A, Stanley MA, Shepherd N, Duvall N, Jenkinson SB, Davis C, et al. Obstructive sleep apnea in young infants with down syndrome evaluated in a down syndrome specialty clinic. Am J Med Genet A. (2015) 167(2):324–30. doi: 10.1002/ajmg.a.36903
Keywords: trisomy 21 (Down syndrome), osa, breathing abnormalities, cardiac, pediatrics - children
Citation: Gaza K, Gustave J, Rani S, Strang A and Chidekel A (2023) Polysomnographic characteristics and treatment modalities in a referred population of children with trisomy 21. Front. Pediatr. 10:1109011. doi: 10.3389/fped.2022.1109011
Received: 27 November 2022; Accepted: 23 December 2022;
Published: 10 January 2023.
Edited by:
Simin Li, Southern Medical University, ChinaReviewed by:
Eliot S Katz, Harvard Medical School, United StatesOlivia J. Veatch, University of Kansas Medical Center, United States
© 2023 Gaza, Gustave, Rani, Strang and Chidekel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Abigail Strang QXN0cmFuZ0BuZW1vdXJzLm9yZw==
Specialty Section: This article was submitted to Pediatric Pulmonology, a section of the journal Frontiers in Pediatrics
 Kaelyn Gaza
Kaelyn Gaza Jodi Gustave
Jodi Gustave Abigail Strang
Abigail Strang