
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Pediatr. , 23 December 2022
Sec. General Pediatrics and Pediatric Emergency Care
Volume 10 - 2022 | https://doi.org/10.3389/fped.2022.1065957
Objective: To assess the knowledge, attitudes, and practices (KAP) towards artificial intelligence (AI) among young pediatricians in France.
Methods: We invited young French pediatricians to participate in an online survey. Invitees were identified through various email listings and social media. We conducted a descriptive analysis and explored whether survey responses varied according to respondents’ previous training in AI and level of clinical experience (i.e., residents vs. experienced doctors).
Results: In total, 165 French pediatricians participated in the study (median age 27 years, women 78%, residents 64%). While 90% of participants declared they understood the term “artificial intelligence”, only 40% understood the term “deep learning”. Most participants expected AI would lead to improvements in healthcare (e.g., better access to healthcare, 80%; diagnostic assistance, 71%), and 86% declared they would favor implementing AI tools in pediatrics. Fifty-nine percent of respondents declared seeing AI as a threat to medical data security and 35% as a threat to the ethical and human dimensions of medicine. Thirty-nine percent of respondents feared losing clinical skills because of AI, and 6% feared losing their job because of AI. Only 5% of respondents had received specific training in AI, while 87% considered implementing such programs would be necessary. Respondents who received training in AI had significantly better knowledge and a higher probability of having encountered AI tools in their medical practice (p < 0.05 for both). There was no statistically significant difference between residents’ and experienced doctors’ responses.
Conclusion: In this survey, most young French pediatricians had favorable views toward AI, but a large proportion expressed concerns regarding the ethical, societal, and professional issues linked with the implementation of AI.
Artificial intelligence (AI) pioneer Marvin Minsky defined AI as “the science of making machines do things that would require intelligence if done by men” (Box 1) (1). The use of AI tools is rapidly increasing in clinical medicine, thanks to the generalized availability of powerful computers and large datasets (2). So far, AI has been mainly used to develop diagnostic tools for various medical conditions (3). For example, with image recognition techniques such as convolutional neural networks, AI may help clinicians detect fractures on x-rays (4), diabetic retinopathy on digital fundus images (5), skin cancer (6), and genetic diseases on facial images (7). Beyond convolutional neural networks, other AI-enabled diagnostic applications include, for instance, improvement in diagnosing autism (8), identification of child abuse from medical records (9), and natural language processing systems to assist clinicians with detecting rare conditions (10). AI also has many non-diagnostic applications, including support for managing chronic diseases such as diabetes (11), decision support and hospital monitoring systems, drug discovery pipelines, and surgical robots (12).
Box 1 Definition of key terms used in artificial intelligence literature.
• Artificial intelligence (AI): AI is a broad term that refers to the ability of a digital computer or computer-controlled robot to perform tasks commonly associated with human intelligence.
• Machine learning (ML): ML is a subfield of AI. ML is a method to train a computer to learn from its raw input to perform complex regression and classification tasks.
• Neural network (NN): A NN is an ML program that operates in a manner inspired by the organization of neurons in the human brain.
• Deep learning (DL): DL is a class of NN that uses a high number of neuron-type units and layers to hierarchically extract features from the raw input. Popular applications of DL are in image and speech recognition.
AI-based healthcare technologies are promising, but they rely on complex statistical methods and concepts, thus generating high expectations but also fears among clinicians. Several studies have investigated the knowledge, attitudes, and practices (KAP) of young healthcare professionals towards AI. For example, Sit et al. conducted an online survey via social media among 484 medical students in the UK (13). This study aimed to identify their KAP towards AI and the potential impact of AI on choosing radiology as a specialization (13). While 49% of students stated that they were less willing to specialize in radiology out of fear of AI, 88% of participants believed AI would play an important role in medicine, and 89% claimed that AI training would benefit their career. Participants who had received theoretical training in AI were significantly more inclined to specialize in radiology and felt more confident using AI-based tools in their future practice.
In France, a qualitative survey conducted by Laï et al. focused on the perception of AI among various healthcare workers (14). Forty individuals were interviewed: 13 physicians, 7 individuals involved in the industry, 5 researchers in the field of AI, 7 members of regulatory agencies, and 8 people who were not directly involved in the development of AI but had previously written about the challenges of implementing AI in medicine. Healthcare professionals appeared focused on providing their patients with the best and safest care. The responses revealed that AI seemed a true breakthrough for healthcare industrial partners, but legal difficulties in accessing individual health data could hamper its development. Institutional players were aware of their significant role in regulating the use of AI tools. Healthcare researchers specializing in AI had a more pragmatic point of view and hoped for a better translation from research to practice.
Other studies focusing on medical AI surveyed radiologists (15, 16), psychiatrists (17), and dermatologists (18). However, to our knowledge, no study focused specifically on the KAP towards AI among young pediatricians. In this context, we invited young French pediatricians to participate in an online survey.
This is a cross-sectional online study using several regional (i.e., Ile de France, the Paris area) and national mailing lists and social media. We aimed at including young pediatricians registered on the Facebook groups “Internes de France” (n = 17,096), “Association des Juniors en Pédiatrie” (AJP; n = 1,267), “Promo 2019 de Pédiatrie” (n = 87), “Pédiatrie Paris Promo socle” (n = 88), “Pédiatrie Paris Promo 2020” (n = 93) as well as on AJP-Paris’ mailing lists, regrouping Ile-de-France pediatrics residents from 2016 to 2021 (n = 465; Appendix 1). The survey was anonymous. Only pediatricians were eligible; young physicians from other specialties were excluded. There were no strict age limits, but most social media groups we used were targeted at residents and fellows. AJP's mailing list includes young pediatricians, mostly below 30 years old, all below 40. Data collection was conducted from January 12 to February 16, 2022. We followed the CHERRIES statement for reporting (Appendix 2).
The online questionnaire was developed and administered via Google Form. Consent, age, sex, faculty of origin, level of experience, and any additional training were gathered from the initial seven questions. The survey was then structured into four parts: (1) knowledge about AI (5 questions), (2) expected benefits of AI (13 questions), (3) fears toward AI (8 questions), and (4) practices regarding AI (6 questions). Responses to closed questions were collected on a 5-point Likert scale (i.e., “totally disagree”, “rather disagree”, “neutral”, “rather agree”, “totally agree”). Answers to questions expecting a numerical entry were offered a range of plausible values. Each social media and mailing list received a separate questionnaire, and the response files were merged for analysis. There was no need to answer all the questions of the survey to be included in the study, and partial responses were kept in the analysis. Because questionnaires were anonymous, it was not possible to detect and exclude duplicates, but we believe it is very unlikely that respondents took the survey several times.
The “residents” category included residents from the first to the eighth semester of residency training. The “experienced doctors” category included chief residents (“Docteur Junior” status), physicians working under a resident contract (“Faisant Fonction d’Interne” status), fellows (“Assistant/Chef de Clinique” status), attending physicians, professors (assistant, associate, and full), and private practitioners. We considered the responses “totally agree” and “rather agree” as positive, and the responses “rather disagree” and “totally disagree” as negative. Neutral responses were considered a third response category.
We first performed a descriptive analysis of study participants and survey responses. Descriptive statistics included means and medians for qualitative variables. Survey responses were summarized as percentages. In an exploratory approach, we used Chi-square tests and Fisher's exact tests (if n < 5) to compare proportions and assess if responses varied according to whether respondents had received (specific or non-specific) training in AI. We also compared residents’ and experienced doctors’ responses. All analyses involved the use of R software (R Foundation, Austria, Vienna). The significance threshold was set at 0.05. There was no specific sample size calculation for this survey.
Participation in the survey was voluntary. A short paragraph was included at the beginning of the questionnaire to inform participants of the study's objectives and of the confidentiality of their responses. Consent was considered obtained by virtue of questionnaire completion. Data were collected anonymously, and participants had the right to access and cancel their answers. In accordance with French legal regulations, ethical approval was not required for this study.
One hundred and sixty-five pediatricians responded to the survey (Figure 1) The participation rate was difficult to estimate due to potential redundancies across social media groups and mailing lists. Respondents’ median age was 27 years (interquartile range 25–30 years), and 78% of respondents were women. In total, 75% of the participants attended medical school in Ile-de-France (Paris V, Paris VI, Paris VII, UPEC, Paris-Sud, Paris 13, Versailles-Saint-Quentin Universities). Regarding clinical experience, 64% of respondents were classified as residents, while 36% of included pediatricians were “experienced doctors”.
In total, 90% of the participants stated that they understood the term “artificial intelligence”, compared to 65% for “machine learning”, 54% for “neural network” and only 40% for “deep learning”. Only 31% of the participants reported that they knew the difference between these different terms, while half of them (49%) did not. From a regulatory perspective, 58% of the respondents declared they were familiar with the General Data Protection Regulation (GDPR) framework.
The majority of the surveyed pediatricians seemed to have a favorable view of AI (Table 1). The participants appeared to think that AI could lead to major improvements in medicine, particularly in terms of medical training (88%), better access to healthcare in settings where experts are not available (80%), diagnostic assistance (71%), better compliance with treatment and patient follow-up (91%), and help for choosing among various therapeutic options (73%). More than half (60%) of respondents agreed with the statement that AI would “revolutionize medicine” while a quarter (24%) preferred to stay neutral on this question. A majority (86%) declared that they would favor the implementation of AI tools in pediatrics.
More than half of respondents (59%) saw AI as a threat to medical data security and 35% as a threat to the ethical and human dimensions of medicine (Table 2). Regarding their practice of medicine, 39% feared skill loss induced by task delegation to AI, but only 6% of the pediatricians stated that they feared losing their job because of AI.
Only 5% of the pediatricians stated that they had received specific teaching in AI, and 29% of pediatricians declared having been in contact with AI through specific or non-specific training (Table 3). In total, 42% of the participants declared that they had encountered at least one AI tool in their clinical practice. The vast majority of respondents considered that it would be necessary to implement specific training and courses about AI (87%).
Forty-eight physicians (29%) declared they had contact with AI through (specific or non-specific) training. These respondents significantly more often stated: (i) to know the difference between the terms “artificial intelligence”, “machine learning”, “neural network”, and “deep learning” (44% vs. 26%, p = 0.027), (ii) to know what the General Data Protection Regulation (GDPR) is (73% vs. 51%, p = 0.009), and (iii) to have encountered AI tools in their medical practice (65% vs. 33%, p < 0.001). We found no statistically significant difference between residents’ and experienced doctors’ responses (Appendix 3).
In this nationwide online survey of 165 young French pediatricians, we assessed their KAP towards AI in healthcare. We found insufficient knowledge in the lexical field and core concepts of AI, as, for example, 49% of the participants did not know the differences between the terms “artificial intelligence”, “machine learning”, “neural network” and “deep learning”. We also observed that the majority of respondents seemed to have a positive view of AI and were in favor of implementing AI tools in pediatrics. In contrast, more than half of respondents saw AI as a threat to medical data security and one-third as a threat to the ethical and human dimensions of medicine. Forty-two percent of the participants declared that they had encountered at least one AI tool in their medical practice, whereas only 5% of the pediatricians stated that they had received specific teaching about AI in medical school. Respondents who received training in AI had significantly better knowledge and a higher probability of encountering AI tools in their medical practice (Appendix 3).
To our knowledge, this is the first study focusing on the KAP towards AI among pediatricians in France. Similar studies have been conducted in other fields of medicine, including radiology (15, 16), psychiatry (17), and dermatology (18), but not in pediatrics, while several AI applications are being implemented in this specialty (3, 12).
Our finding that less than a third (31%) of pediatricians knew the difference between “artificial intelligence”, “machine learning”, “neural network”, and “deep learning” is in line with other studies that also questioned physicians on their understanding of AI [response rates: 24% among dermatologists (18) and 35% among radiologists (16)]. Only 5% of the pediatricians in our survey said they had received specific training in AI, but 42% had encountered AI solutions in their practice. In the study by Ooi et al. among radiologists (16), a similar proportion of only 5% of respondents stated that they had received training in AI. Still, the majority of them commonly used AI solutions in their practice (93% for voice recognition and 56% for image interpretation) (16). It appears that specific training on AI in medical studies is currently lacking. Hence, doctors may confront AI tools directly in their clinical practice without prior instruction about the concepts behind algorithms, how AI solutions are developed and evaluated, and their limitations and potential biases (19, 20). Accordingly, 87% of the pediatricians in our survey considered that it would be necessary to offer specific training in AI, as 80% of the dermatologists surveyed by Polesie et al. (18) and 89% of the radiologists in the Ooi study (16).
Regarding their attitudes toward AI in medicine, 60% of young French pediatricians believed that AI would “revolutionize medicine”. A greater proportion (89%) of radiologists surveyed in the Ooi study agreed that AI would “revolutionize the practice of their specialty” (16). This higher proportion could be because the vast majority (93%) of radiologists already commonly used AI solutions in their practice (16). In addition, radiology relies on advanced technologies, whereas pediatricians might be more focused on clinical skills. In the study surveying dermatologists (18), 69% of respondents believed that AI would “revolutionize dermatology”. However, the authors explained that “dermatologists with a special interest in dermatoscopy were more likely to have received the invitation [to participate in the survey]”, potentially shifting the results toward a positive perception of AI.
Regarding the potential negative attitudes toward AI, only 6% of pediatricians expressed their fear of losing their job because of AI. This low proportion was also found in dermatology (5.4%) (18). Also, in psychiatry, only 3.8% of responding physicians feared that AI would make their practice obsolete, but as high as 75% of them thought that AI could replace them in completing and updating medical records (17). Coppola's study among 1,032 radiologists reported that 11% of them were afraid of being replaced by an AI solution (15). This shows that most physicians across several specialties see AI as having the potential to help clinicians rather than replace them.
Attitudes towards AI were generally positive: 86% of French pediatricians in our survey favored implementing AI tools in their specialty, as were 77% of radiologists in Coppola's study (15). When asked whether increased use of AI would make their specialty more “exciting”, 63% of dermatologists (18) and 76% of radiologists agreed (16). AI thus seems generally perceived as a solution to enhance clinical practice.
Our study has limitations. First, there was probably a selection bias due to our distribution channels favoring access to young pediatricians trained in the Paris region (75%). This population of young pediatricians might be more exposed to research and innovation, including AI, in their training and clinical practice than in other regions. Furthermore, determining the exact response rate was not practicable because of the potential for user overlap between groups. Given that in 2022, France counted 1,635 residents training in Pediatrics, our best approximation of the response rate in this subgroup is around 6% (105/1,635). Hence, our collected responses may not represent the KAP of all young French pediatricians. Second, we opted for a relatively short and shallow questionnaire to maximize the completion rate. Qualitative and mixed-methods studies are needed to allow deeper investigations of barriers and facilitators of AI use in pediatrics.
While AI offers many promises in healthcare, it raises technical, professional, and ethical questions. The majority of young French pediatricians who responded to this survey had positive attitudes towards AI and emphasized the need to set up specific training programs in AI and the importance of ethical and societal issues linked with the implementation of AI in healthcare.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Participation in the survey was voluntary. A short paragraph was included at the beginning of the questionnaire to inform participants of the study's objectives and of the confidentiality of their responses. Consent was considered obtained by virtue of questionnaire completion. Data were collected anonymously, and participants had the right to access and cancel their answers. In accordance with French legal regulations, ethical approval was not required for this study.
Original idea: EP, MR, AT. Study design: EP, MR, AT, CD, JC. Data collection: EP, MR, AT. Data analysis: EP, MR, AT, JC. Study supervision: JC. First draft of the manuscript: EP, MR, AT. Review of the manuscript for critical intellectual content: all authors. All authors contributed to the article and approved the submitted version.
Dubois and Cohen received research funding from “Sauver la Vie” (Fondation Université Paris Cité) for projects in the field of artificial intelligence in healthcare.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
AI, artificial intelligence; AJP, Association des Juniors en Pédiatrie (Young Pediatricians Association); GDPR, general data protection regulation; KAP, knowledge, attitudes, and practices.
2. Topol EJ. High-performance medicine: the convergence of human and artificial intelligence. Nat Med. (2019) 25(1):44–56. doi: 10.1038/s41591-018-0300-7
3. Hoodbhoy Z, Masroor Jeelani S, Aziz A, Habib MI, Iqbal B, Akmal W, et al. Machine learning for child and adolescent health: a systematic review. Pediatrics. (2021) 147(1):e2020011833. doi: 10.1542/peds.2020-011833
4. Kuo RY, Harrison C, Curran TA, Jones B, Cussons D, Freethy A, et al. Artificial intelligence in fracture detection: a systematic review and meta-analysis. Radiology. (2022) 304(1):50–62. doi: 10.1148/radiol.211785
5. Gulshan V, Peng L, Coram M, Stumpe MC, Wu D, Narayanaswamy A, et al. Development and validation of a deep learning algorithm for detection of diabetic retinopathy in retinal fundus photographs. JAMA. (2016) 316(22):2402–10. doi: 10.1001/jama.2016.17216
6. Esteva A, Kuprel B, Novoa RA, Ko J, Swetter SM, Blau HM, et al. Dermatologist-level classification of skin cancer with deep neural networks. Nature. (2017) 542(7639):115–8. doi: 10.1038/nature21056
7. Gurovich Y, Hanani Y, Bar O, Nadav G, Fleischer N, Gelbman D, et al. Identifying facial phenotypes of genetic disorders using deep learning. Nat Med. (2019) 25(1):60–4. doi: 10.1038/s41591-018-0279-0
8. Levy S, Duda M, Haber N, Wall DP. Sparsifying machine learning models identify stable subsets of predictive features for behavioral detection of autism. Mol Autism. (2017) 8:65. doi: 10.1186/s13229-017-0180-6
9. Annapragada AV, Donaruma-Kwoh MM, Annapragada AV, Starosolski ZA. A natural language processing and deep learning approach to identify child abuse from pediatric electronic medical records. PLoS One. (2021) 16(2):e0247404. doi: 10.1371/journal.pone.0247404
10. Liang H, Tsui BY, Ni H, Valentim CCS, Baxter SL, Liu G, et al. Evaluation and accurate diagnoses of pediatric diseases using artificial intelligence. Nat Med. (2019) 25(3):433–8. doi: 10.1038/s41591-018-0335-9
11. Piette JD, Mendoza-Avelares MO, Ganser M, Mohamed M, Marinec N, Krishnan S. A preliminary study of a cloud-computing model for chronic illness self-care support in an underdeveloped country. Am J Prev Med. (2011) 40(6):629–32. doi: 10.1016/j.amepre.2011.02.014
12. Shu LQ, Sun YK, Tan LH, Shu Q, Chang AC. Application of artificial intelligence in pediatrics: past, present and future. World J Pediatr. (2019) 15(2):105–8. doi: 10.1007/s12519-019-00255-1
13. Sit C, Srinivasan R, Amlani A, Muthuswamy K, Azam A, Monzon L, et al. Attitudes and perceptions of UK medical students towards artificial intelligence and radiology: a multicentre survey. Insights Imaging. (2020) 11(1):14. doi: 10.1186/s13244-019-0830-7
14. Lai MC, Brian M, Mamzer MF. Perceptions of artificial intelligence in healthcare: findings from a qualitative survey study among actors in France. J Transl Med. (2020) 18(1):14. doi: 10.1186/s12967-019-02204-y
15. Coppola F, Faggioni L, Regge D, Giovagnoni A, Golfieri R, Bibbolino C, et al. Artificial intelligence: radiologists’ expectations and opinions gleaned from a nationwide online survey. Radiol Med. (2021) 126(1):63–71. doi: 10.1007/s11547-020-01205-y
16. Ooi SKG, Makmur A, Soon AYQ, Fook-Chong S, Liew C, Sia SY, et al. Attitudes toward artificial intelligence in radiology with learner needs assessment within radiology residency programmes: a national multi-programme survey. Singapore Med J. (2021) 62(3):126–34. doi: 10.11622/smedj.2019141
17. Doraiswamy PM, Blease C, Bodner K. Artificial intelligence and the future of psychiatry: insights from a global physician survey. Artif Intell Med. (2020) 102:101753. doi: 10.1016/j.artmed.2019.101753
18. Polesie S, Gillstedt M, Kittler H, Lallas A, Tschandl P, Zalaudek I, et al. Attitudes towards artificial intelligence within dermatology: an international online survey. Br J Dermatol. (2020) 183(1):159–61. doi: 10.1111/bjd.18875
19. Keane PA, Topol EJ. AI-facilitated health care requires education of clinicians. Lancet. (2021) 397(10281):1254. doi: 10.1016/S0140-6736(21)00722-4
20. James CA, Wachter RM, Woolliscroft JO. Preparing clinicians for a clinical world influenced by artificial intelligence. JAMA. (2022) 327(14):1333–4. doi: 10.1001/jama.2022.3580
a. Responses according to whether physicians declared they had contact with AI through (specific or non-specific) training.
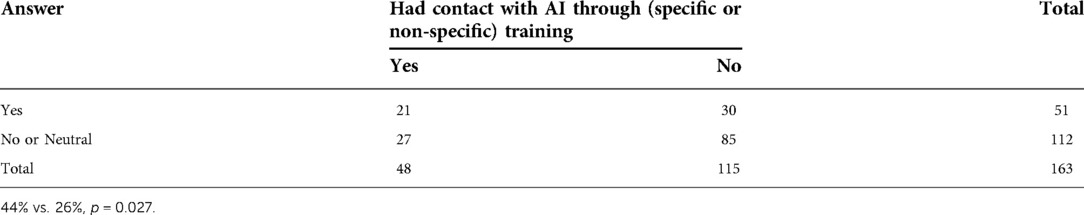
1. Do you know the difference between the terms “artificial intelligence”, “machine learning”, “neural network”, and “deep learning”?
b. Comparison of residents’ and experienced doctors’ responses.
Keywords: artificial intelligence, pediatrics, knowledge - attitude - behavior, survey, machine learning
Citation: Perrier E, Rifai M, Terzic A, Dubois C and Cohen JF (2022) Knowledge, attitudes, and practices towards artificial intelligence among young pediatricians: A nationwide survey in France. Front. Pediatr. 10:1065957. doi: 10.3389/fped.2022.1065957
Received: 10 October 2022; Accepted: 30 November 2022;
Published: 23 December 2022.
Edited by:
Joe Kossowsky, Boston Children's Hospital, Harvard Medical School, United StatesReviewed by:
Thiago Gonçalves dos Santos Martins, Federal University of São Paulo, Brazil© 2022 Perrier, Rifai, Terzic, Dubois and Cohen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jérémie F. Cohen amVyZW1pZS5jb2hlbjJAYXBocC5mcg==
†These authors have contributed equally to this work
‡ORCID Jérémie F. Cohen orcid.org/0000-0003-3572-8985
Specialty Section: This article was submitted to General Pediatrics and Pediatric Emergency Care, a section of the journal Frontiers in Pediatrics
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.