
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr., 02 December 2022
Sec. Pediatric Hematology and Hematological Malignancies
Volume 10 - 2022 | https://doi.org/10.3389/fped.2022.1064038
This article is part of the Research TopicNon-Infection Complications Post-HSCTView all 4 articles
 Irina Zaidman1,2*†
Irina Zaidman1,2*† Tamar Shaziri1,†
Tamar Shaziri1,† Dina Averbuch1,3
Dina Averbuch1,3 Ehud Even-Or1,2
Ehud Even-Or1,2 Yael Dinur-Schejter2
Yael Dinur-Schejter2 Adeeb NaserEddin2
Adeeb NaserEddin2 Rebecca Brooks1,4
Rebecca Brooks1,4 Bella Shadur5,6
Bella Shadur5,6 Aharon Gefen7,8,‡
Aharon Gefen7,8,‡ Polina Stepensky1,2,‡
Polina Stepensky1,2,‡
Background: Allogeneic hematopoietic stem cell transplantation (HSCT) is an efficient treatment for numerous malignant and nonmalignant conditions affecting children. This procedure can result in infectious and noninfectious neurological complications (NCs).
Objective: The objective of the study is to examine the incidence, risk factors, and outcomes of NCs in pediatric patients following allogeneic HSCT.
Methods: We performed a retrospective study of 746 children who underwent 943 allogeneic HSCTs in two large pediatric hospitals in Israel from January 2000 to December 2019.
Results: Of the pediatric patients 107 (14.3%) experienced 150 NCs. The median follow-up was 55 months. Noninfectious NCs were more common than infectious NCs (81.3% vs. 18.7%). Factors significantly associated with type of NC (infectious vs. noninfectious) were underlying disease (immunodeficiency vs. malignant and metabolic/hematologic disease) (p-value = 0.000), and use of immunosuppressive agent, either Campath or ATG (p-value = 0.041). Factors with a significant impact on developing neurological sequelae post-NC were number of HSCT >1 (p-value = 0.028), the use of alemtuzumab as an immunosuppressive agent (p-value = 0.003), and infectious type of NC (p-value = 0.046). The overall survival rate of whole NC-cohort was 44%; one-third of all mortality cases were attributed to the NC. The strongest prognostic factors associated with mortality were older age at HSCT (p-value = 0.000), the use of alemtuzumab as an immunosuppressive agent (p-value = 0.004), and the existence of neurological sequelae (p-value = 0.000). Abnormal central nervous system imaging (p-value = 0.013), the use of alemtuzumab as an immunosuppressive agent (p-value = 0.019), and neurological sequelae (p-value = 0.000) had statistically significant effects on neurological cause of death.
Conclusion: Infectious and noninfectious NCs are a significant cause of morbidity and mortality following allogeneic HSCT in children. Further research is required to better understand the risk factors for different NCs and their outcomes regarding sequelae and survival.
Hematopoietic stem cell transplantation (HSCT) is an efficient treatment for numerous pediatric malignant and nonmalignant disorders. In preparation for the transplant, patients receive high-dose chemotherapy with or without irradiation (conditioning regimen), to destroy diseased cells and to reduce immunologic resistance. Following allogeneic HSCT, patients receive immunosuppressive medications to prevent graft-vs.-host disease (GVHD) (1).
The intensive conditioning, transplantation itself, and immunosuppressive therapy may lead to severe complications in many organs, including the nervous system, and cause neurological complications (NCs)—seizures, stroke, meningitis, and encephalitis—associated with morbidity and mortality (2).
The reported incidence of post-HSCT NCs ranges from 6.5% to 65% (3–12) and varies widely between different centers due to the heterogeneity of study groups and the criteria of NCs (5). NCs can occur secondary to a range of infectious and noninfectious causes, including medication-induced, metabolic, vascular, immune-mediated, or disease-related neurotoxicity (including relapse) (5, 13). Prevalence of infectious NCs is less than that of noninfectious NCs (1, 3, 7, 8, 10, 14). Many factors affect the incidence and severity of NC after HSCT including allogeneic transplantation (1, 4, 5, 9, 11), mismatched donor (3, 4, 9, 12), radiation-based conditioning regimen (1, 8), and GVHD (3–5, 9, 12).
NCs after HSCT can be divided into three groups according to onset (15): early complications during the first month after HSCT, such as seizures and posterior reversible encephalopathy syndrome (PRES) as a consequence of neurotoxic conditioning agents, or infections and bleeding secondary to conditioning-induced pancytopenia (16); intermediate-onset complications, between 1 and 6 months after HSCT, with central nervous system (CNS) infections; and late complications, >6 months after HSCT, like CNS relapse, late chemo-radiotherapy related neurotoxicity, and neurological manifestations of GVHD (1).
The survival rates of patients who develop NCs, both children and adults, are reduced (8, 9, 12, 17); mortality could be attributed to the NCs in more than half of the cases (8, 11); and 27%–43% (5, 7, 18) suffer from long-term neurological sequelae. NCs are often accompanied by neuroimaging changes such as brain edema, intracranial hemorrhage, ring-enhancing lesions or abscess, and cortical dysplasia (19–21).
Our goal was to study a large cohort of pediatric patients from two large pediatric medical centers who underwent allogeneic HSCT and developed NCs, over a period of 20 years. We aimed to examine the rate and risk factors of infectious and noninfectious NCs and their impact on outcomes such as survival and long-term neurological sequelae.
We performed a retrospective study in two tertiary pediatric hospitals, analyzing the incidence, risk factors, and outcomes of pediatric patients who developed NCs following allogeneic HSCT, between January 2000 and December 2019. All patients younger than 21 years at the time of HSCT, who experienced at least one neurological event during follow-up, were included. We excluded from this study pediatric patients that underwent autologous HSCTs and patients with brain tumors.
The study was approved by the Institutional Review Boards of both centers.
Data were collected from medical records and entered directly into password-protected Microsoft Excel spreadsheets (Redmond, WA, United States). Data included gender, age at HSCT, diagnosis, number of HCSTs, type of donor, conditioning regimen and immunosuppression, type of GVHD, type and timing of NC, investigations of infectious and noninfectious NCs [laboratory, imaging (computed tomography, CT, and magnetic resonance imaging, MRI), and electroencephalography], and neurotoxic potential of medications. To determine if neurological sequelae are present, patients were followed from the time of their initial NC, date of last follow-up, overall survival (OS), and date and cause of death (neurological vs. non-neurological). Patients were evaluated by senior physicians specialized in pediatric HSCTs and pediatric neurologist. Cause of death was determined by senior physicians after reviewing the medical records. Clinical and neurological evaluation at last follow-up of living patients were conducted in HSCT late effects clinics.
We defined three groups underlying diseases: malignant diseases [acute lymphoblastic leukemia (ALL), myelodysplastic syndrome (MDS)/acute myeloid leukemia (AML), chronic myeloid leukemia (CML), juvenile myeloid leukemia (JMML), and Hodgkin and non-Hodgkin lymphomas]; nonmalignant-immunodeficiency [severe combined immunodeficiency (SCID), leukocyte adhesion deficiency (LAD), Wiskott–Aldrich syndrome, Kostmann syndrome, hemophagocytic lymphohistiocytosis (HLH), X-linked lymphoproliferative disease (XLP), Griscelli syndrome, and other rare primary immunodeficiencies]; nonmalignant-other [metabolic: metachromatic leukodystrophy (MLD), adrenoleukodystrophy (ALD), osteopetrosis, and hematological diseases: bone marrow failures: severe aplastic anemia (SAA), pure red cell aplasia, dyskeratosis congenita, Fanconi anemia, and hemoglobinopathies—sickle cell anemia, thalassemia major].
Conditioning regimens were divided into four groups: myeloablative with radiation (total body irradiation with etoposide or cyclophosphamide), myeloablative without radiation (busulfan-based regimen with cyclophosphamide, or melphalan), myeloablative reduced toxicity (treosulfan-based protocol with fludarabine and thiotepa), and reduced-intensity conditioning (RIC) (busulfan/fludarabine; treosulfan/fludarabine).
Serotherapy usage in conditioning regimen was classified as none, anti-thymocyte globulin (ATG), and alemtuzumab.
Donor types were divided into three groups based on HLA-compatibility: matched (10/10), mismatched (8–9/10), and haploidentical (related donors <8/10). Both matched and mismatched groups included related and unrelated donors.
Acute and chronic GVHD (AGVHD and CGVHD, respectively) were graded according to the modified Glucksberg criteria (22) and the revised Seattle criteria (23), respectively.
The etiology of the NCs was determined by signs and symptoms, medications, and microbiological and radiological characteristics. NCs were defined as “infectious” if a pathogen was identified by culture, serology, or polymerase chain reaction (PCR) in tissue of brain or cerebrospinal fluid (CSF) and as “noninfectious” if the patient displayed no clinical symptoms of infection, no organism was identified, and another cause was found.
Neurological sequelae were defined as residual neurological symptoms or damage after the NC, such as persistent convulsive disorder, paresis and plegia, aphasia, brain or optic nerve atrophy, cognitive deterioration, and coma.
To test the association between two categorical variables, χ2 test and the Fisher's exact test were used. The comparison of a quantitative variable between two independent groups was carried out by the two-sample t-test or the nonparametric Mann–Whitney test. The nonparametric test was used for quantitative variables that were not normally distributed. The logistic regression multivariate model was applied to simultaneously assess the effect of several variables on a dichotomous dependent variable. The Kaplan–Meier model with the log-rank test for the comparison of survival curves was used for testing the effect of categorical variables on survival. The Cox regression model was used to test the effect of quantitative variables on survival. This model was also used as the multivariate model that simultaneously assesses the effect of several variables on survival. Both the Cox regression multivariate model and the logistic regression model were carried out using the stepwise, forward, likelihood ratio method. All tests applied were two-tailed, and a p-value of 0.05 or less was considered statistically significant.
Statistical analysis was conducted by SPSS software (Chicago, IL, United States).
From January 2000 to December 2019, 746 pediatric patients underwent 943 allogeneic HSCTs in two tertiary pediatric hospitals in Israel. Detailed characteristics of study population are shown in Table 1. One hundred and seven of these patients experienced 150 neurological events, an incidence of 14.34%. Of 107 patients, 57 were transplanted for malignant and 50 for nonmalignant diseases. Median ages at transplant were 7.8 and 9.96 years in infectious and noninfectious group, respectively. Median times from HSCT to NC were 74.5 and 70.5 days in infectious and noninfectious group, respectively (Table 1). Median follow-up period after at least one neurological event was 55 months (range 0.2–199).
Most NCs were noninfectious, 81.3% (122 out of 150), vs. infectious, 18.7% (28 out of 150) (Table 1). In the noninfectious group, the common causes of NCs were PRES, convulsions, and encephalopathy secondary to multiorgan failure (33.6%, 15.6%, and 15.6%, respectively), followed by CNS relapse and hemorrhage (11.5% and 9.8%) (Table 2). In the infectious group, most common causes for neurological complications were fungal/protozoal infections (mostly toxoplasmosis; 39.3%), followed by viral (35.7%) and bacterial infections (25%) (Table 3).
The underlying disease was significantly correlated (p-value = 0.000) with the type of NC: while patients with malignant diseases and patients with metabolic/hematological diseases had more noninfectious NCs (89.3% and 85.5%, respectively), children with immunodeficiencies experienced mostly infectious NCs (60%).
The type of NC was also associated with the conditioning regimen used: noninfectious NCs were significantly more frequent in patients treated by myeloablative protocol, with or without radiation (86% and 89.6%, respectively), compared with those in patients who received either reduced toxicity or intensity regimens (46.2% and 69.2%, respectively; p-value = 0.002).
The immunosuppressive agent was another factor associated with the type of NC. When no immunosuppressive was used, patients had the lowest percentage (8.7%) of infectious NCs, compared with patients treated with alemtuzumab or ATG (30% and 21.7%, respectively). Although the significance of this difference was borderline by univariate analysis (p-value = 0.069), it reached a significant level when entered into the multivariate model.
We found no correlation between the type of NC (infectious/noninfectious) and sex, age at HSCT, number of HSCT, type of donor, AGVHD or CGVHD, and age at NC and time from HSCT to NC.
Multivariate analysis deemed only immunosuppressive agent (p-value = 0.041) and underlying disease (p-value = 0.000) as significantly correlated with the type of NC; children treated without immunosuppressive agent (compared with those treated with alemtuzumab) were 7.624 times more prone to develop a noninfectious NC (p-value=0.011). Children with metabolic/hematological diseases, and children with malignant diseases, were 14.102 and 16.711 times more likely to develop a noninfectious NC (p-value=0.000) (Table 4).
Neurological sequelae were developed in 36.4% of children with NCs (Table 5).
The underlying disease had a statistically significant effect on developing neurological sequelae (p-value = 0.019). The highest incidence (65%) was seen in patients in the nonmalignant-immunodeficiency group, to compare with 38.2% and 30.7% in the malignant and nonmalignant-other groups, respectively.
An association was seen between the number of HSCTs and neurological sequelae (p-value = 0.028). The highest percentile (63.2%) of sequelae was seen in patients that underwent two transplants, and the lowest percentile (33.6%) of sequelae was seen in patients that underwent one transplant. Half of patients that underwent a third transplant developed neurological sequelae, but the numbers were too small for statistical analysis.
We also found a correlation between the immunosuppressive agent used and neurological sequelae (p-value = 0.011). The highest percentile of neurological sequelae (65%) was seen in patients treated with alemtuzumab, compared with 37.3% among those treated with ATG, and 26.1% in patients not receiving any serotherapy.
The type of NC had a significant impact on whether they developed neurological sequelae: 60% of patients with infectious NCs suffered neurological sequelae compared with 32.8% of patients with noninfectious NCs (p-value = 0.006).
A correlation was seen between abnormal CNS imaging and sequelae (p-value = 0.021). In patients with abnormalities seen in both brain CT and MRI, the incidence of neurological sequelae was 43.2%, vs. 20% in patients with abnormalities only in MRI.
We found no association between developing a neurological sequelae and sex, conditioning regimen, type of donor, CGVHD, age at HSCT, and time from HSCT to NC.
Multivariate analysis of variables associated with neurological sequelae demonstrated that only a number of HSCTs more than 1 [odds ratio (OR) = 5.29, p-value = 0.007], alemtuzumab as serotherapy (OR = 6.515, p-value = 0.003), and infectious NC (OR = 2.58, p-value = 0.046), remained statistically significant (Table 4).
The OS of our cohort was 44%. Among patients who developed NCs during or after HSCT, 47 survived with median follow-up period 55 months (range 0.2–199).
Out of the 60 patients who did not survive, 20 died due to neurological causes and 40 died due to other reasons. The mortality rate from neurological reason in our study was 33% of all mortality cases of patients diagnosed with NCs.
There was an association seen between age of patients at HSCT and/or at the NC and survival. The survival period was shorter as the patient was older at the transplant (p-value = 0.003) and at the NC (p-value = 0.004). The death rate increased by a factor of 1.066 for every year older at the age of HSCT.
The immunosuppressive agent used had a significant effect on patient's survival (p-value = 0.000). The shortest survival was seen in patients treated with alemtuzumab—median 0.77 months, vs. a median of 84.37 months when no immunosuppressive agent was used and 40.87 months in patients treated with ATG (Figure 1A).
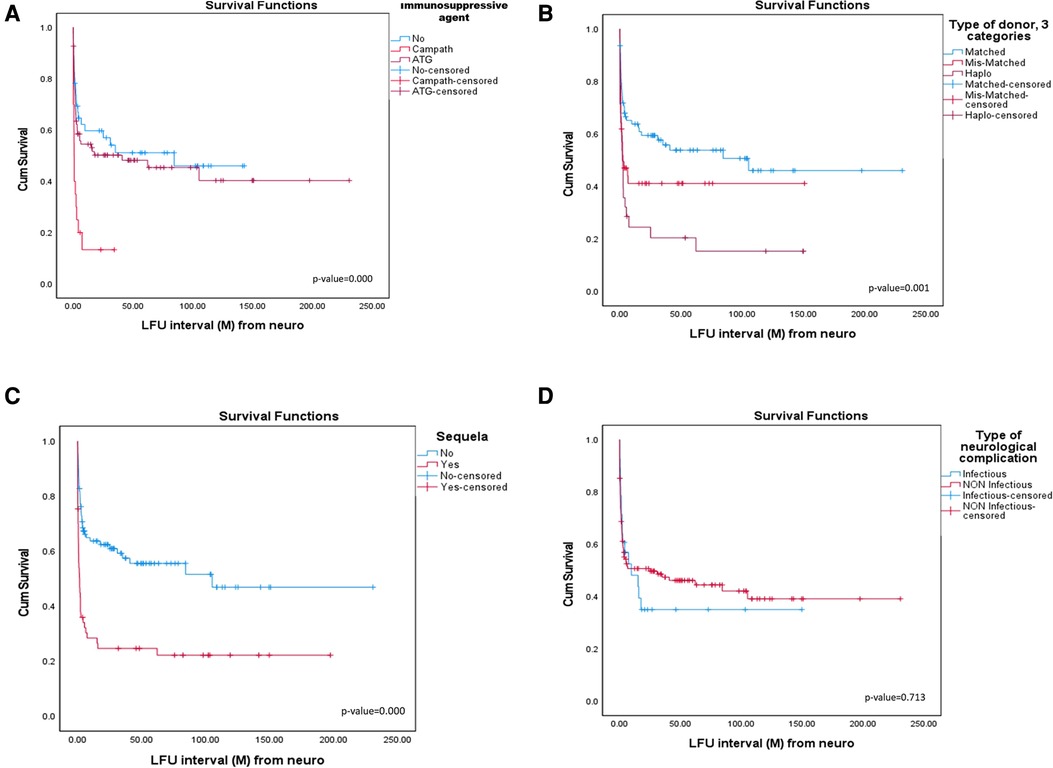
Figure 1. (A) Survival according to immunosuppressive agent. (B) Survival according to type of donor. (C) Survival according to neurological sequelae. (D) Survival according to type of neurological complication.
The underlying disease had a significant effect on patient's survival (p-value = 0.037). The shortest survival was seen in the malignant and nonmalignant-immunodeficiency groups, median 4.4 months, vs. nonmalignant-metabolic and hematologic patients, 84.37 months.
Type of donor had a significant effect on patients' survival (p-value = 0.001). The shortest median survival seen in the haploidentical group was 1.87 months, and in the mismatched group was 2.3 months, compared with 105.1 months after matched-donor HSCTs (Figure 1B).
Development of neurological sequelae after NC had a significant impact on patient survival (p-value = 0.000). Median survival for patients who developed sequelae was shorter at 1.8 months, compared with those without sequelae at 84.3 months (Figure 1C).
Survival was not correlated with abnormal imaging, conditioning regimen, time from HSCT to neurological complication, type of NC (Figure 1D), sex, underlying disease, AGVHD, and CGVHD.
A multivariable analysis that included all correlated variables demonstrated that age at NC (HR = 1.082, p-value = 0.000), neurological sequelae (HR = 2.693, p-value = 0.000), and the use of alemtuzumab as an immunosuppressive agent (HR = 2.696, p-value = 0.004) had the strongest impact on survival (Table 4).
An association was seen between number of HSCTs and the cause of death (p-value = 0.048). The highest percentiles (100% and 50%) of a neurological cause of death were seen in patients that underwent three or two transplants, respectively, vs. 27.1% in patients after one transplant.
Another association was seen between abnormal imaging and cause of death (p-value = 0.000): 47.3% of children with abnormal imaging had a neurological cause of death, compared with 3.7% in patients with normal imaging.
Developing neurological sequelae had a statistically significant impact on the cause of death (p-value = 0.000); 64.3% of a neurological cause of death was seen in patients who developed sequelae, vs. 6.3% in patients who did not.
Type of NC was significantly correlated with the cause of death (p-value 0.011), with 58.8% of the infectious group having a neurological cause of death vs. 26.2% of the noninfectious group.
The immunosuppressive agent used had a significant effect on patient's cause of death (p-value = 0.003). The highest incidence (64.7%) of a neurological cause of death was seen in patients treated with alemtuzumab, compared with patients treated without immunosuppressant or with ATG (33.3% and 18.6%, respectively).
Type of donor was also associated with cause of death. The highest incidence (47.8%) of a neurological cause of death was seen in the haploidentical donor group, compared with matched and mismatched donors (20.0% and 37.5%, respectively).
A correlation was seen between the interval from the patient's first NC to death, and the mortality cause (p-value = 0.002), with shorter interval in patients that died due to neurological reason: in the neurological cause of death group, the median NC to death interval was 16 days, while for the non-neurological cause of death group, this interval was 59 days.
We found no correlation between cause of death and sex, underlying disease, conditioning regimen, number of HSCT, age at HSCT, age at neurological complication, and time from HSCT to neurological complication.
Multivariate analysis demonstrated that out of all the statistically significant variables, only abnormal imaging (OR = 19.38, p-value = 0.013), sequelae (OR = 24.162, p-value = 0.000), and the use of alemtuzumab as an immunosuppressive agent (OR 7.768, p-value = 0.019) were statistically significant as risk factors for neurological cause of death (Table 4).
NCs in children who underwent allogeneic HSCT are an important cause of mortality and morbidity, including long-term neurological sequelae. These complications are due to various etiologies: infections (bacterial, fungal/protozoal, or viral encephalitis) or noninfectious (e.g., medication-induced neurotoxicity, metabolic, vascular, immune-mediated, or related to the underlying disease including relapse malignancy) (5, 13). However, research regarding prognostic factors for infectious and noninfectious NCs and sequelae is scarce, especially in children.
The aim of our study was to identify the characteristics, risk factors, and outcomes (neurological sequelae and survival) of pediatric patients who developed infectious and noninfectious NCs during and after allogeneic HSCT.
In our study, we analyzed a large cohort of pediatric patients consisting of 943 allogeneic HSCTs from two major pediatric centers, between the years 2000 and 2019. The incidence of NCs in our cohort was 14.34%. The reported incidence of NCs among children after HSCT varies greatly and ranges from 6.5% to 65% (3–12), which could be attributed to patients' heterogeneity and different definitions of NCs. The incidence of abnormal findings in autopsies is up to 90% (24). A recent Chinese study assessing 196 children (8) found the incidence to be 17%, comparable with our results (and similar to the 14.8% incidence in a recent study on 888 adult allo-transplanted patients) (17). The incidence of NCs after HSCT is higher than in children treated with chemotherapy only (10).
Noninfectious NCs were more than four times frequent than infectious NCs in our cohort. The reported incidence of CNS infections after allogeneic HSCT ranges from 7.5% to 27%, a smaller part from the overall incidence of NCs as described previously (1, 3, 7, 8, 10, 14); our findings are within that range.
Maffini et al. (25) reviewed the timing of NCs in adults after allogeneic HSCT. Early posttransplantation complications were noninfectious, associated mainly with calcineurin inhibitors toxicity (around 50% of all early noninfectious NCs) (1, 5) or with the conditioning regimen, whereas later complications were infectious and associated with immunosuppression status. In our pediatric cohort, the onset of infectious or noninfectious NCs was not statistically different (median 77 and 70 days, respectively). Moreover, in the literature, most NCs tend to occur earlier than 3 months post-HSCT (5, 7–9, 11, 12).
Risk factors for posttransplant pediatric NCs were described, and some of them have conflicting results. Most studies analyzed allogeneic HSCTs, but those that included also autologous transplants found a significant higher incidence in the allogeneic setting (1, 9, 11). Regarding pretransplant factors, underlying malignant diseases, especially leukemia or lymphoma (8, 12) or diseases already involving the CNS (8), radiation-based conditioning (1, 8, 20), and mismatched donor (9, 12) (in earlier works, but not in the recent ones, probably due to better matching processes), were associated with higher risk. GVHD was found to be correlated with NCs (9, 12); a recent retrospective analysis revealed statistically significant correlations between noninfectious NCs and GVHD, specifically between PRES or seizures, and acute GVHD, as well as seizures or stroke, and chronic GVHD; but causal relationships could not be established (4). The above-mentioned large adult study found increased age as the only significant risk factor (17).
In our work, infectious NCs were more frequent in patients who received myeloablative reduced toxicity (53.8%) or RIC (42.3%) regimens, vs. those who were treated with myeloablative protocols, with or without radiation (16.3% and 17.9%, respectively). A possible explanation is that the goal of reduced toxicity/intensity conditioning is tumor eradication and/or destruction of host hematopoiesis via immune-mediated effects (using serotherapy such as alemtuzumab or ATG), rather than cytotoxic effect (26). RIC protocols are thus related to higher prevalence of infectious complications.
As expected, infectious type of complications was more frequent in patients who received immunosuppressive agent, either alemtuzumab or ATG. Moreover, some negative outcomes were more frequent in those treated with alemtuzumab: prevalence of neurological sequelae and mortality, as well as neurological cause of death. Alemtuzumab is a monoclonal antibody against the CD52 antigen, expressed in both B and T lymphocytes (27); ATG, however, affects only T lymphocytes (28); immune recovery is slower after treatment with alemtuzumab rather than ATG (29). Avivi et al. (30) showed that adult patients treated with alemtuzumab-based RIC may have a lower risk of developing regimen-related/noninfectious NCs and are more susceptible to infectious NC. We did not find pediatric studies that described the association between the type of conditioning regimen and usage alemtuzumab/ATG and higher incidence of infectious NCs.
We observed the highest incidence (60%) of infectious NCs in the nonmalignant-immunodeficiency group. One reason could be the pretransplant poor immunological status of these patients that increases their susceptibility to infections. Another possible explanation is the prevalent use of RIC regimens used in these patients.
On the other hand, in our study, myeloablative conditioning protocols, with or without radiation, were risk factors for noninfectious NCs. Usually, myeloablative protocols put less emphasis on immunosuppressive effects; however, myeloablative medications such as busulfan and thiotepa, and the exposure to radiation, are known to be toxic to the brain tissue and cerebral vasculature. The incidence of neurotoxicity after busulfan-based conditioning is up to 7% in children (31), and includes seizures, PRES, altered consciousness, and headaches (32). Thiotepa is reported to cause chronic encephalopathy with progressive decline in cognitive and behavioral functions (33). As for radiation, CNS toxicity includes focal cerebral necrosis, neurocognitive deficits, cerebrovascular disease, myelopathy, and secondary neoplasms (34).
Another risk factor for developing noninfectious NCs was the patient's underlying disease being metabolic and hematological. This could be attributed to the neurotoxicity of the busulfan-based myeloablative protocols that are required for most patients with these diseases (31, 32).
Many survivors develop long-term neurological sequelae, including a wide range of neurological deficits, from severe leukoencephalopathy, long-lasting convulsion disorders, to more subtle and mild dysfunction such as learning disorders. Some of these sequelae are accompanied by imaging abnormalities (33). The presence of sequelae reported to be 27%–43% (5, 9, 18). Shin et al. demonstrated the following risk factors to be associated with neurological sequelae: malignancy as the underlying disease, infectious NC occurring after day 100 post-HSCT, and severe MRI abnormalities. Neither radiation nor the intensity of conditioning regimen nor the type of immunosuppressant affected the neurological prognosis (7). We found higher rates of neurological sequelae among patients who suffered an infectious NC rather than noninfectious, 56.8% vs. 31.9%, respectively. This may be explained by the reversible nature of some of the causes of noninfectious NCs post-HSCT, like hydroelectrolytic abnormalities and cyclosporine-associated PRES (35). Like us, Shin et al. (7) demonstrated that in their poor outcome group, there were more instances of malignancy as the underlying disease and infection as the cause of the neurological symptoms. Moreover, treatment with alemtuzumab was found to be a risk factor for developing neurological sequelae, compared with treatment with ATG or without immunosuppressive agent, by the same mechanism of delayed immunological reconstitution as discussed previously. Literature is scarce regarding neurological sequelae following post-HSCT NCs, especially among children; there is no consensus regarding risk factors for sequelae. Kang et al. reported in their pediatric study that 42.5% of neurological episodes had remaining neurological sequelae, 13.7% of them were severe. When they analyzed the sequelae according to etiology, 22.9% of calcineurin inhibitor-related (noninfectious) neurotoxicity had neurological sequelae, vs. 50% of infectious NCs (5).
Developing NCs after a second HSCT was associated with higher rates of neurological sequelae, 5.1 times more likely than after first HSCT. Generally, second transplants are associated with increased toxicity and poorer outcomes than the first HSCT (36, 37), which could be attributed to increased toxicity of a prolonged peritransplant treatment and a more resistant underlying disease. There is not much research regarding NC following second HSCT; however, Shah et al. reported a decreased neurocognitive function after a second HSCT (38). In their study, Mori et al. showed a higher incidence of HHV6-associated encephalitis/myelitis in recipients who underwent two or more HSCTs (39).
In the literature, OS of patients with NCs is inferior to those without NCs (3, 6, 8, 9, 12, 17). OS in our study group was 44%, comparable with current literature that depicts 30%–52.1% rate (3, 5, 6, 8, 9, 11, 17). Uckan et al. (12) found very dismal survival rate of 9% for children presented with life-threatening NCs.
In our cohort, the morality due to a neurological cause was 33% of mortality among NCs cases. In the literature, this rate is higher: 50%–61% (8, 11). Kang et al. found that extended chronic GVHD and the presence of neurological sequelae were associated with increased risk of mortality (HR 5.98 and 4.37, respectively) (5). On the other hand, the CNI-associated neurotoxicity was transient, not affecting either the survival outcome (3) or the occurrence of late neurological sequelae (1). We confirmed, in multivariate analysis, that older age at HSCT and the existence of neurological sequelae were significant risk factors for mortality. The death rate increased by a factor of 1.062 for every year older at the age of HSCT. There are conflicting results regarding the effect of age at transplant on mortality in literature. Socié et al. demonstrated lower mortality in patients younger than 15 years at HSCT (40), while Martin et al. did not identify a relationship between age at transplant and late mortality (41). Older age at transplant was also associated with a worse health-related quality of life (42). However, these studies do not discuss the relation between age at HSCT and mortality specifically after NCs. Regarding neurological sequelae, we suppose that developing sequelae indicates a more severe and irreversible CNS damage, increasing the risk of mortality.
Along the timeline of the neurological toxicity, the clinical picture could be accompanied by neuroimaging findings—starting from CT changes during the acute phase (19) to long-term alterations of the MRI (20, 21); the impact of these changes on the patients' outcomes is not fully elucidated. A recent study of Shin et al. (7) found that among 91 transplanted children with NCs, MRI changes were present in 56%. Zając-Spychała et al. described long-term imaging and functional outcomes of pediatric patients with acute lymphoblastic leukemia after radiation-based HSCT, compared with nontransplanted children, and found that the former had significant decline in both brain structures (as demonstrated by MRI) and cognitive performance tests (20). In our study, additional risk factor for a neurological cause of death included abnormal imaging. We assume that the existence of abnormalities seen in imaging is implying a more severe CNS damage, thus resulting in death due to a neurological cause. Regarding the imaging modality, there is a marked difference between abnormal findings seen in CT and in MRI. MRI shows functional changes in CNS, such as the mostly-reversible PRES, the main cause for NCs after pediatric allogeneic HSCT. CT however shows structural CNS damages (abscesses, cerebrovascular complications, etc.) that are more likely to leave permanent sequelae (43). That correlates with the higher percentile of a neurological cause of death among children with abnormalities seen on CT, in comparison to children with abnormalities seen on MRI.
Our study included symptomatic patients; a future research direction could be screening of all transplanted children for presymptomatic changes, both by imaging and cognitive tests, as described above for leukemic patients (20), and by newer neuro-electrophysiological tools like evoked potentials, as already done by Kroczka et al. (44–46) in leukemic patients (with emphasis on irradiated patients (45). With these modern tools, the group of patients presenting NCs would likely be larger.
Our study has some strengths. First, this is one of the largest and longest studies that analyzed the characteristics of pediatric patients with NCs following allogeneic HSCT, compared infectious vs. noninfectious NCs, and defined risk factors for developing complications, neurological sequelae, and the associated mortality.
In our study, we found and described the correlations between type of conditioning regimen and immunosuppressive agent, and type of NCs (infectious vs. noninfectious) in pediatric patients, which have not been noted before in literature. We also described that late-onset neurological sequelae are associated with alemtuzumab, and with infectious NCs.
We recognize the study's limitations, mainly its retrospective nature and involving only two centers.
In conclusion, infectious and noninfectious NCs are a significant cause of morbidity and mortality following allogeneic HSCT in the pediatric population. Further multicenter prospective research is required for a deeper understanding of the individual risk factors for different NCs and their different outcomes regarding sequelae and mortality. This knowledge could be implemented in clinical practice for developing preventing strategies and early detection.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
We would like to greatly thank Tali Bdolah-Abram, the statistician who accompanied this work, for her dedicated and meticulous work on this project. We thank our patients and their families for putting their trust in our care and allowing us to publish this manuscript. We thank the two departments' medical, nursing, and administrative staff for their devoted work.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
HSCT, hematopoietic stem cell transplantation; NCs, neurological complications; RIC, reduced-intensity conditioning; GVHD, graft-vs.-host disease; PRES, posterior reversible encephalopathy syndrome; CNS, central nervous system; CT, computed tomography; MRI, magnetic resonance imaging; OS, overall survival; ALL, acute lymphoblastic leukemia; AML, acute myeloid leukemia; MDS, myelodysplastic syndrome; CML, chronic myeloid leukemia; JMML, juvenile myeloid leukemia; MLD, metachromatic leukodystrophy; ALD, adrenoleukodystrophy; SAA, severe aplastic anemia; SCID, severe combined immunodeficiency; LAD, leukocyte adhesion deficiency; HLH, hemophagocytic lymphohistiocytosis; XLP, X-linked lymphoproliferative disease; ATG, anti-thymocyte globulin; CSF, cerebrospinal fluid; PCR, polymerase chain reaction.
1. Hierlmeier S, Eyrich M, Wölfl M, Schlegel PG, Wiegering V. Early and late complications following hematopoietic stem cell transplantation in pediatric patients: a retrospective analysis over 11 years. PLoS One. (2018) 13(10):1–16. doi: 10.1371/journal.pone.0204914
2. Rubin J, Wide K, Remberger M, Gustafsson B. Acute neurological complications after hematopoietic stem cell transplantation in children. Pediatr Transplant. (2005) 9:62–7. doi: 10.1111/j.1399-3046.2004.00277.x
3. Koh KN, Park M, Kim BE, Im HJ, Seo JJ. Early central nervous system complications after allogeneic hematopoietic stem cell transplantation in children. Korean J Hematol. (2010) 45:164–70. doi: 10.5045/kjh.2010.45.3.164
4. Azik F, Yazal Erdem A, Tavil B, Bayram C, Tunç B, Uçkan D. Neurological complications after allogeneic hematopoietic stem cell transplantation in children, a single center experience. Pediatr Transplant. (2014) 18(4):405–11. doi: 10.1111/petr.12265
5. Kang JM, Kim YJ, Kim JY, Cho EJ, Lee JH, Lee MH, et al. Neurologic complications after allogeneic hematopoietic stem cell transplantation in children: analysis of prognostic factors. Biol Blood Marrow Transplant. (2015) 21:1091–8. doi: 10.1016/j.bbmt.2015.02.007
6. Faraci M, Lanino E, Dini G, Fondelli MP, Morreale G, Dallorso S, et al. Severe neurologic complications after hematopoietic stem cell transplantation in children. Neurology. (2002) 59:1895–904. doi: 10.1212/01.WNL.0000036608.42104.B9
7. Shin H, Yum MS, Kim MJ, Suh JK, Im HJ, Kim H, et al. Hematopoietic stem cell transplantation-associated neurological complications and their brain MR imaging findings in a pediatric population. Cancers. (2021) 13:3090. doi: 10.3390/cancers13123090
8. Mak CYK, Cheuk DKL, Lee PPW, Chiang AKS, Ha SY, Liu APY, et al. Neurological complications in Chinese children undergoing hematopoietic stem cell transplantation. Childs Nerv Syst. (2021) 37:3753–67. doi: 10.1007/s00381-021-05235-3
9. Iguchi A, Kobayashi R, Yoshida M, Kaneda M, Watanabe N, Cho Y, et al. Neurological complications after stem cell transplantation in childhood. Bone Marrow Transplant. (1999) 24:647–52. doi: 10.1038/sj.bmt.1701969
10. Schmidt K, Schulz AS, Debatin KM, Friedrich W, Classen CF. CNS complications in children receiving chemotherapy or hematopoietic stem cell transplantation: retrospective analysis and clinical study of survivors. Pediatr Blood Cancer. (2008) 50:331–6. doi: 10.1002/pbc.21237
11. Zaucha-PraZmo A, Jasiński M, Drabko K, Choma M, Wójcik B, Kowalczyk JR. Neurologic complications in children after hemaopoietic stem cell transplantation: a single-center experience. Transplant Proc. (2007) 39:2905–7. doi: 10.1016/j.transproceed.2007.08.070
12. Uckan D, Cetin M, Yigitkanli I, Tezcan I, Tuncer M, Karasimav D, et al. Life-threatening neurological complications after bone marrow transplantation in children. Bone Marrow Transplant. (2005) 35:71–6. doi: 10.1038/sj.bmt.1704749
13. Duléry R. Neurological Complications. In: Carreras E, Dufour C, Mohty M, Kröger N, editors. The EBMT Handbook. Cham: Springer (2019). p. 403–407.
14. Schmidt-Hieber M, Zweigner J, Uharek L, Blau IW, Thiel E. Central nervous system infections in immunocompromised patients—update on diagnostics and therapy. Leuk Lymphoma. (2009) 50:24–36. doi: 10.1080/10428190802517740
15. Dulamea AO, Lupescu IG. Neurological complications of hematopoietic cell transplantation in children and adults. Neural Regen Res. (2018) 13:945–54. doi: 10.4103/1673-5374.233431
16. Noè A, Cappelli B, Biffi A, Chiesa R, Frugnoli I, Biral E, et al. High incidence of severe cyclosporine neurotoxicity in children affected by haemoglobinopaties undergoing myeloablative haematopoietic stem cell transplantation: early diagnosis and prompt intervention ameliorates neurological outcome. Ital J Pediatr. (2010) 36:14. doi: 10.1186/1824-7288-36-14
17. Mannina D, Berneking L, Both A, Timm W, Urbanowicz T, Wolschke C, et al. Major central nervous system complications after allogeneic stem cell transplantation: a large retrospective study on 888 consecutive adult patients. Eur J Haematol. (2020) 105:722–30. doi: 10.1111/ejh.13489
18. Hawkins MM, Lancashire ER, Winter DL, Frobisher C, Reulen RC, Taylor AJ, et al. The British childhood cancer survivor study: objectives, methods, population structure, response rates and initial descriptive information. Pediatr Blood Cancer. (2008) 50:1018–25. doi: 10.1002/pbc.21335
19. Ricci E, Toni F, Marra C, Masetti R, Porelli S, Balducci J, et al. Computed tomography in acute severe central nervous system complications in children treated for cancer: still a useful diagnostic tool in the emergency setting. J Child Neurol. (2021) 36:169–76. doi: 10.1177/0883073820962354
20. Zając-Spychała O, Pawlak MA, Karmelita-Katulska K, Pilarczyk J, Jończyk-Potoczna K, Przepióra A, et al. Long-term brain status and cognitive impairment in children treated for high-risk acute lymphoblastic leukemia with and without allogeneic hematopoietic stem cell transplantation: a single-center study. Pediatr Blood Cancer. (2020) 67:e28224. doi: 10.1002/pbc.28224
21. Sakaguchi Y, Natsume J, Kidokoro H, Tanaka M, Okai Y, Ito Y, et al. Change of white matter integrity in children with hematopoietic stem cell transplantation. Pediatr Neurol. (2020) 111:78–84. doi: 10.1016/j.pediatrneurol.2020.06.008
22. Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. 1994 Consensus conference on acute GVHD grading. Bone Marrow Transplant. (1995) 15(6):825–8. PMID: 7581076
23. Lee SJ, Vogelsang G, Flowers MED. Chronic graft-versus-host disease. Biol Blood Marrow Transplant. (2003) 9(4):215–33. doi: 10.1053/bbmt.2003.50026
24. Bleggi-Torres LF, De Medeiros BC, Werner B, Neto JZ, Loddo G, Pasquini R, et al. Neuropathological findings after bone marrow transplantation: an autopsy study of 180 cases. Bone Marrow Transplant. (2000) 25:301–7. doi: 10.1038/sj.bmt.1702140
25. Maffini E, Festuccia M, Brunello L, Boccadoro M, Giaccone L, Bruno B. Neurologic complications after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. (2017) 23:388–97. doi: 10.1016/j.bbmt.2016.12.632
26. Gratwohl A, Carreras E. Chapter 8: Principles of conditioning. In: Apperley J, Carreras E, Gluckman E, Masszi T, editors. EBMT-ESH handbook on haemopoietic stem cell transplantation 6th edition. Paris: European School of Hematology (2012). p. 122–36
27. Alinari L, Lapalombella R, Andritsos L, Baiocchi RA, Lin TS, Byrd JC. Alemtuzumab (Campath-1H) in the treatment of chronic lymphocytic leukemia. Oncogene. (2007) 26:3644–53. doi: 10.1038/sj.onc.1210380
28. Kekre N, Antin JH. ATG In allogeneic stem cell transplantation: standard of care in 2017? Counterpoint. Blood Adv. (2017) 1:573–6. doi: 10.1182/bloodadvances.2016001552
29. Willemsen L, Jol-van der Zijde CM, Admiraal R, Putter H, Jansen-Hoogendijk AM, Ostaijen-Ten Dam MM, et al. Impact of serotherapy on immune reconstitution and survival outcomes after stem cell transplantations in children: thymoglobulin versus alemtuzumab. Biol Blood Marrow Transplant. (2015) 21:473–82. doi: 10.1016/j.bbmt.2014.11.674
30. Avivi I, Chakrabarti S, Kottaridis P, Kyriaku C, Dogan A, Milligan DW, et al. Neurological complications following alemtuzumab-based reduced-intensity allogeneic transplantation. Bone Marrow Transplant. (2004) 34:137–42. doi: 10.1038/sj.bmt.1704538
31. Vassal G, Deroussent A, Hartmann O, Challine D, Benhamou E, Valteau-Couanet D, et al. Dose-dependent neurotoxicity of high-dose busulfan in children: a clinical and pharmacological study. Cancer Res. (1990) 50:6203–7. PMID: 2400986
32. De La Camara R, Tomas JF, Figuera A, Berberana M, Fernandez-Ranada JM. High dose busulfan and seizures. Bone Marrow Transplant. (1991) 7:363–4. PMID: 2070145
33. Shah AJ, Rosser T, Goodarzian F. Neurologic sequealae of hematopoietic stem cell transplantation (HSCT). In: Demirer T, editor. New advances in stem cell transplantation. London: IntechOpen (2012). p. 517–32.
34. Dropcho EJ. Neurotoxicity of radiation therapy. Neurol Clin. (2010) 28:217–34. doi: 10.1016/j.ncl.2009.09.008
35. Saillard C, Blaise D, Mokart D. Critically ill allogeneic hematopoietic stem cell transplantation patients in the intensive care unit: reappraisal of actual prognosis. Bone Marrow Transplant. (2016) 51:1050–61. doi: 10.1038/bmt.2016.72
36. Yaniv I, Krauss AC, Beohou E, Dalissier A, Corbacioglu S, Zecca M, et al. Second hematopoietic stem cell transplantation for post-transplantation relapsed acute leukemia in children: a retrospective EBMT-PDWP study. Biol Blood Marrow Transplant. (2018) 24:1629–42. doi: 10.1016/j.bbmt.2018.03.002
37. Lund TC, Ahn KW, Tecca HR, Hilgers MV, Abdel-Azim H, Abraham A, et al. Outcomes after second hematopoietic cell transplantation in children and young adults with relapsed acute leukemia. Biol Blood Marrow Transplant. (2019) 25:301–6. doi: 10.1016/j.bbmt.2018.09.016
38. Shah AJ, Kapoor N, Weinberg KI, Crooks GM, Kohn DB, Lenarsky C, et al. Second hematopoietic stem cell transplantation in pediatric patients: overall survival and long-term follow-up. Biol Blood Marrow Transplant. (2002) 8:221–8. doi: 10.1053/bbmt.2002.v8.pm12014811
39. Mori Y, Miyamoto T, Nagafuji K, Kamezaki K, Yamamoto A, Saito N, et al. High incidence of human herpes virus 6-associated encephalitis/myelitis following a second unrelated cord blood transplantation. Biol Blood Marrow Transplant. (2010) 16:1596–602. doi: 10.1016/j.bbmt.2010.05.009
40. Socié G, Stone J V, Wingard JR, Weisdorf D, Henslee-Downey PJ, Bredeson C, et al. Long-term survival and late deaths after allogeneic bone marrow transplantation. Late effects working committee of the international bone marrow transplant registry. N Engl J Med. (1999) 341:14–21. doi: 10.1056/NEJM199907013410103
41. Martin PJ, Counts GW, Appelbaum FR, Lee SJ, Sanders JE, Deeg HJ, et al. Life expectancy in patients surviving more than 5 years after hematopoietic cell transplantation. J Clin Oncol. (2010) 28:1011–6. doi: 10.1200/JCO.2009.25.6693
42. Brice L, Weiss R, Wei Y, Satwani P, Bhatia M, George D, et al. Health-related quality of life (HRQoL): the impact of medical and demographic variables upon pediatric recipients of hematopoietic stem cell transplantation. Pediatr Blood Cancer. (2011) 57:1179–85. doi: 10.1002/pbc.23133
43. Bonardi M, Turpini E, Sanfilippo G, Mina T, Tolva A, Thyrion FZ. Brain imaging findings and neurologic complications after allogenic hematopoietic stem cell transplantation in children. Radiographics. (2018) 38:1223–38. doi: 10.1148/rg.2018170139
44. Kroczka S, Stepien K, Witek-Motyl I, Kwiecinska K, Kapusta E, Biedron A, et al. Clinical utility of complex assessment with evoked potentials in acute lymphoblastic leukemia survivors: comparison of various treatment protocols. BMC Cancer. (2021) 21(1):150. doi: 10.1186/s12885-021-07873-x
45. Kroczka S, Stepien K, Witek-Motyl I, Klekawka T, Kapusta E, Biedron A, et al. Polyneuropathy in acute lymphoblastic leukemia long-term survivors: clinical and electrophysiological characteristics with the impact of radiotherapy. Front Pediatr. (2021) 8:526235. doi: 10.3389/fped.2020.526235
Keywords: neurological complications, hematopoietic stem cell transplantation, survival, neurological sequelae, abnormal imaging, pediatric malignant and nonmalignant diseases
Citation: Zaidman I, Shaziri T, Averbuch D, Even-Or E, Dinur-Schejter Y, NaserEddin A, Brooks R, Shadur B, Gefen A and Stepensky P (2022) Neurological complications following pediatric allogeneic hematopoietic stem cell transplantation: Risk factors and outcome. Front. Pediatr. 10:1064038. doi: 10.3389/fped.2022.1064038
Received: 7 October 2022; Accepted: 1 November 2022;
Published: 2 December 2022.
Edited by:
Tomasz Szczepanski, Medical University of Silesia, PolandReviewed by:
Szymon Skoczen, Jagiellonian University Medical College, Poland© 2022 Zaidman, Shaziri, Averbuch, Even-Or, Dinur-Schejter, NaserEddin, Brooks, Shadur, Gefen and Stepensky. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Irina Zaidman emFpZGlyaW5AZ21haWwuY29t
†These authors have contributed equally to this work and share first authorship
‡These authors have contributed equally to this work and share last authorship
Specialty Section: This article was submitted to Pediatric Hematology and Hematological Malignancies, a section of the journal Frontiers in Pediatrics
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.