
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Pediatr., 11 January 2023
Sec. Neonatology
Volume 10 - 2022 | https://doi.org/10.3389/fped.2022.1063387
Objectives: This meta-analysis evaluated and compared the efficacy and safety of noninvasive high-frequency oscillatory ventilation (NHFOV) and nasal intermittent positive-pressure ventilation (NIPPV) for preterm newborns after extubation.
Methods: We searched the PubMed, Cochrane Library, EMBASE, Web of Science, CNKI, Wanfang and VIP databases from inception to August 28, 2022. Randomized controlled trials (RCTs) that evaluated and compared the efficacy and safety of NHFOV and NIPPV in newborns were included in the review and meta-analysis, which followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guidelines.
Results: Eight studies involving 1,603 patients were included. Compared with NIPPV, NHFOV could reduce the reintubation rates (RR = 0.68, 95% CI 0.53, 0.86, P = 0.002). Subgroup analysis showed that the significant difference was found in reintubation rates within 72 h (RR = 0.48, 95% CI 0.32, 0.73, P = 0.0005). NHFOV also could decrease the duration of non-invasive ventilation (standard mean difference (SMD) = −1.52, 95% CI −2.58, −0.45, P = 0.005). However, all included studies had a high risk of bias, and the overall quality of the evidence of the outcomes was low or very low.
Conclusion: In our study, compared with NIPPV, NHFOV seems to reduce the reintubation rates without increasing adverse outcomes. Nevertheless, definite recommendations cannot be made based on the quality of the published evidence.
Preterm infants are prone to various conditions because of their immature organs. Respiratory failure related to organ immaturity is the most common cause of death in preterm infants. Invasive mechanical ventilation (IMV), which has been widely used in past decades to support preterm infants with respiratory diseases. Although lifesaving, IMV is an important risk factor in the development of many complications such as air leaks, ventilator-associated lung injury, and bronchopulmonary dysplasia (BPD) (1). In the past decade, the practice of prompt weaning and early extubation to non-invasive respiratory support has been the focus and ultimate goal (2). However, some preterm infants need to be reintubated after a trial of extubation. An international survey found that 43% of experts believed that extubation failure is an independent risk factor for increased mortality and morbidity (3).
Continuous positive airway pressure (CPAP) is the most commonly used respiratory support in clinical practice. CPAP significantly reduced the need for IMV, but failure rates of almost 50% have prompted neonatologists to seek more effective noninvasive ventilation modalities (4). The latest Cochrane systematic review (5) suggest that nasal intermittent positive pressure ventilation (NIPPV) reduces the incidence of extubation failure and the need for re-intubation within 48 h to one week more effectively than nasal CPAP, but does not substantially reduce chronic lung disease and mortality. The synchronisation may be important in delivering effective NIPPV. In practice, however, synchronization is difficult to achieve due to leaks, high respiratory rate, low tidal volume, and irregular breathing pattern. Noninvasive high-frequency oscillatory ventilation (NHFOV) is an unconventional noninvasive ventilation mode, which theoretically provides the advantages of HFOV (no need for synchronization, high CO2 removal, lower volume/barotrauma) and nasal continuous positive airway pressure (noninvasive, increased in functional residual capacity allowing oxygenation to improve) (6). Therefore, this method is regarded as a possible improvement over continuous positive airway pressure. Recent several systematic reviews and meta-analyses (7, 8) have shown that the relative risk of intubation was decreased with NHFOV in comparison with nasal CPAP in preterm infants with respiratory distress syndrome. Both NIPPV and NHFOV produced significantly greater improvements in respiratory support of preterm newborns than CPAP. However, to date, evidence for effectiveness between NHFOV and NIPPV at reducing the rate of reintubation was still unknown, and there is no relevant meta-analysis at present.
Hence, we chose to meta-analyze the impact of the NHFOV and NIPPV on respiratory support among preterm neonates after extubation. This may help clinicians determine the best strategy for respiratory support of preterm newborns while identifying knowledge gaps requiring further research.
We conducted a systematic review and meta-analysis following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (9).
Two authors independently searched the PubMed, Cochrane Library, EMBASE, Web of Science from inception to August 28, 2022, using the following search terms: ((Infant OR newborn OR neonat* OR premature OR very low birth weight OR low birth weight OR VLBW OR LBW) AND (Noninvasive High-Frequency Oscillatory Ventilation OR Noninvasive High Frequency Oscillation Ventilation OR Non-invasive high-frequency oscillatory ventilation OR NHFOV OR nHFV) AND (nasal intermittent positive pressure ventilation OR NIPPV OR nasal intermittent mandatory ventilation OR NIMV OR non-invasive positive pressure ventilation)). At the same time, two authors also searched the most commonly used and comprehensive Chinese scientific literature databases (CNKI, Wanfang and VIP databases). No language restrictions were applied. A third author was consulted for the authors' differences in opinion during the study selection process.
All included studies met the following criteria: (1) randomized controlled trial (RCT); (2) the intervention group was given NHFOV and the comparison group was given NIPPV as post-extubation respiratory support; And (3) at least one of the following outcome parameters was reported. The primary outcome was the rate of reintubation. The secondary outcomes included: (i) the duration of non-invasive ventilation, (ii) total oxygen therapy time, (iii) length of hospital stay (LOS), and (v) adverse outcomes, including air leak, abdominal distension, BPD, intraventricular hemorrhage (IVH), retinopathy of prematurity (ROP), necrotizing enterocolitis (NEC), nasal injury, periventricular leukomalacia, and apnea. The exclusion criteria were as follows: (1) non-clinical studies, (2) research protocols, (3) duplicated reports or secondary or post-hoc analyses of the same study population, or (4) lack of sufficient information related to baseline or outcome data.
Two authors used pre-designed tables to extract data independently from each of the eligible studies. Disagreements between the two investigators were resolved by discussion or consensus with a third author. We extracted the characteristics of each study and recorded the following data: first author, year of publication, study design, characteristics of the study population, sample size, and details related to the methodological quality and results. The numeric results, statistics used and p values were extracted for each outcome. We attempted to contact the author of the original report to obtain further details when any of the above information was unclear.
We assessed the quality of the included trials based on the information in the methods section and supplementary materials about them. The quality of the RCTs was assessed using the Cochrane Collaboration's risk-of-bias tool for randomized trials (RoB) (10), which consists of six domains and allowances for any other bias, with risk-of-bias judgments for RCTs ranging from “high,” “unclear” to “low”. Two authors independently assessed the studies' quality and resolved disagreements through consensus.
We used funnel plots to assess publication bias, which was calculated using RevMan 5.3 software. The Egger regression test was used to measure funnel plot asymmetry and was calculated using Stata 12.0 (StataCorp LP, College Station TX, United States).
Review Manager (RevMan) version 5.3 (Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014) was used to calculate the pooled estimates. Risk Ratio (RR) for dichotomous outcomes, the standardized mean difference (SMD) for continuous data and corresponding 95% confidence intervals (CI) were used for the analyses. The I2 statistic was used to evaluate the effect of heterogeneity on the pooled results (I2 > 50% indicated substantial heterogeneity). A fixed-effects model was used to pool data when the heterogeneity was not significant and a random-effects model was used when significant heterogeneity was identified. We conducted sensitivity analyses by omitting studies one by one in order to probe the impact of an individual study. A p-value < 0.05 was considered statistically significant.
Two authors assessed the certainty of the evidence (also known as the quality of the evidence) using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) (11) approach at the outcome level for each comparison between interventions. The certainty in the evidence could be high, moderate, low, or very low.
In the initial literature search (up to 28, August 2022), 370 studies were yielded. After removing duplicates, we screened the titles and abstracts of 334 studies and excluded 295 that did not meet our eligibility criteria. After evaluating the full text of the remaining 39 studies, we included 8 studies (12–19) in our meta-analysis (Figure 1). In total 1,603 participants of whom 799 received NHFOV for respiratory support, were included in our meta-analysis (Table 1). The publication dates of the RCTs ranged from 2019 to 2022, and 87.5% of the RCTs were done in China. Although, synchronized (patient-triggered) NIPPV seems more effective than NIPPV in improving the success of extubation, with a reassuring absence of relevant side effects. Synchronization is difficult to achieve and is often unavailable, so all RCTs included in our meta-analysis used non-synchronous NIPPV. All RCTs were compared at baseline, and there were no significant differences between the two groups in gestational age and birth weight.
The RCTs were assessed using the Cochrane Collaboration risk of bias (RoB) tool. Adequate sequence generation was reported in eight studies (12–19), for them, a randomization sequence was generated using a computer-based random number generator. The method of allocation concealment was adequately reported in four studies. In the study of Soutrik Seth (16) and Yan Li (17), allocation concealment was done by using an opaque sealed envelope. In the study of Xingwang Zhu (12), allocation concealment was performed using a dedicated and secured website. The website generated the randomization, but the sequence was concealed from investigators at each of the participating sites. In the study of Yan Zhuan (12), the allocation was performed by a non-involved person. The infants and personnel could not be blinded due to the nature of the intervention and three studies were judged to have a high risk of bias due to performance bias; however, the outcome assessor was blinded, resulting in a low risk of bias due to detection bias. Three Studies demonstrated adequate follow-up of patients and accounted for any missing participants (12, 16, 17). In the remaining five studies, there were no reports of dropout of cases from randomization to the ascertainment, resulting in an unclear risk of bias due to attrition bias. In three studies (13, 14, 17), the definitions of some of the outcomes were not clear, the incidence of outcomes such as BPD can vary widely based on the definition. Therefore, they were considered to have a high risk of other biases. (Figure 2).
Eight RCTs (12–19) that reported the reintubation rates. Significant difference was found in the reduction of reintubation rates between NHFOV and NIPPV (RR = 0.68, 95% CI 0.53, 0.86, I2 = 42%, P = 0.002; very low-quality evidence; Figure 3). Among them, one RCT that reported reintubation rates within 48 h found no significant differences between NHFOV and NIPPV (RR = 0.78, 95% CI 0.54, 1.14, P = 0.20; very low-quality evidence; Figure 3). Five RCTs that reported reintubation rates within 72 h found significant differences between NHFOV and NIPPV (RR = 0.48, 95% CI 0.32, 0.73, I2 = 0%, P = 0.0005; very low-quality evidence; Figure 3). Two RCTs that reported reintubation rates within 7 days found no significant differences (RR = 0.74, 95% CI 0.19, 2.89, I2 = 80%, P = 0.67; very low-quality evidence; Figure 3).
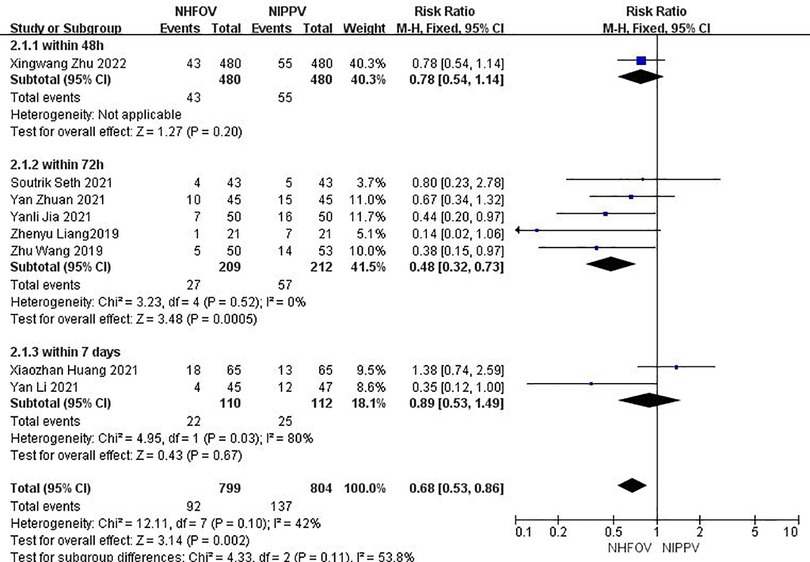
Figure 3. Results of the meta-analysis of reintubation rates; NHFOV, noninvasive high-frequency oscillatory ventilation; NIPPV, nasal intermittent positive-pressure ventilation.
Six RCTs (12–14, 16–18) that enrolled 1,471 neonates reported the duration of non-invasive ventilation, and found a significant decrease in the duration of non-invasive ventilation using NHFOV (standard mean difference (SMD) = −1.52, 95% CI −2.58, −0.45, I2 = 98%, P = 0.005; very low-quality evidence; Figure 4).
Five RCTs (12, 13, 15, 17, 18) with 1,345 neonates that reported the total oxygen therapy time found no significant differences between the NHFOV and NIPPV groups (SMD = −0.01, 95% CI −0.37, 0.35, I2 = 84%, P = 0.95; low-quality evidence; Figure 5).
Two RCTs (15, 17) with 182 neonates that reported LOS showed no significant difference in the decreased LOS (SMD = −0.18, 95% CI −0.47, 0.11, I2 = 0%, P = 0.22; low-quality evidence; Figure 6).
No significant differences in the likelihood of adverse outcomes were observed, including air leaks (Four RCTs (12, 13, 16, 18), RR = 0.74, 95% CI 0.34, 1.60, I2 = 36%, P = 0.45, low-quality evidence; Supplementary Figure S1), apnea (Two RCTs (13, 18), RR = 0.67, 95% CI 0.33, 1.36, I2 = 0%, P = 0.26, low-quality evidence; Supplementary Figure S2), abdominal distention (Two RCTs (15, 19), RR = 0.85, 95% CI 0.41, 1.73, I2 = 0%, P = 0.65, low-quality evidence; Supplementary Figure S3), BPD (Six RCTs (12–14, 16–18), RR = 0.88, 95% CI 0.75, 1.02, I2 = 0%, P = 0.09, low-quality evidence; Supplementary Figure S4), NEC (Three RCTs (14, 17, 19), RR = 0.75, 95% CI 0.26, 2.18, I2 = 0%, P = 0.59, low-quality evidence; Supplementary Figure S5), IVH (Four RCTs (14, 16–18), RR = 0.72, 95% CI 0.28, 1,86, I2 = 0%, P = 0.50, low-quality evidence; Supplementary Figure S6), nasal injury (Five RCTs (12, 13, 17–19), RR = 1.01, 95% CI 0.63, 1,63, I2 = 0%, P = 0.96, low-quality evidence; Supplementary Figure S7), ROP (Three RCTs (14, 17, 18), RR = 0.75, 95% CI 0.39, 1,46, I2 = 0%, P = 0.40, low-quality evidence; Supplementary Figure S8), and periventricular leukomalacia (Three RCTs (13, 14, 18), RR = 0.88, 95% CI 0.29, 2.67, I2 = 0%, P = 0.81, low-quality evidence; Supplementary Figure S9).
We only evaluated publication bias among the reintubation rates, which was the primary outcome parameter. The results suggested that the reintubation rates funnel plots we assessed were symmetrical, and the results of Egger's test were not significant, indicating the absence of publication bias (Supplementary Figure S10).
In sensitivity analysis, based on the stepwise omission of one study at a time, we found no significant difference in the duration of non-invasive ventilation in post-extubation respiratory support when the Zhu Wang et. al (18). study was excluded (Supplementary Figure S11). Exclusion of the Zhu Wang et al. (18) study led to reducing the total oxygen therapy time (Supplementary Figure S12). There was no significant change in other outcome parameters.
The evidence was judged to be of low quality of the outcome of total oxygen therapy time, hospitalization time, air leak, abdominal distension, BPD, IVH, ROP, NEC, nasal injury, periventricular leukomalacia, and apnea. Evidence for the outcome of the rate of reintubation and duration of noninvasive ventilation was judged to be very low quality (online Supplementary Table S1).
This meta-analysis of the findings from eight trials, including 1,603 participants compared the efficacy and safety of post-extubation respiratory support for neonates using NHFOV and NIPPV. The results showed that significant difference was found in the reduction of reintubation rates between NHFOV and NIPPV. Compared with NIPPV, NHFOV could decrease the duration of non-invasive ventilation. But there were no significant differences between the two groups for the adverse outcomes. It is worth noting that some of the results were found to have changed in sensitivity analysis, and the overall quality of the evidence of the outcomes was low or very low. Therefore, the results should be interpreted with caution.
Reintubation within 72 h of initial extubation in very low or extremely low birth weight infants was independently associated with increased risk of BPD/death and death in a retrospective cohort study (20). This result is consistent with a multicenter observational study (21) that demonstrated that for preterm infants, reintubation after elective extubation was an independent risk factor for death or moderate to severe BPD, especially reintubation within 48 h of extubation. For a successful transition from invasive to noninvasive ventilation, the mode choice of noninvasive ventilation is critical to avoid reintubation. In our study, the reduction in reintubation favored NHFOV over NIPPV, and the difference between the two groups was statistically significant. The reintubation rates of NHFOV and NIPPV were 11.51% (92/799) and 17.04% (137/804), respectively. However, the analysis should be considered with caution given the heterogeneity of criteria of reintubation and settings of NHFOV among included studies. In the study by Xingwang Zhu (12) and Yan Li et al. (17), the reintubation rates in the NHFOV group were 8.96% and 8.89%, respectively, lower than average, despite their reintubation criteria were broader, including severe respiratory acidosis, hypoxemia, severe apnea, or pulmonary hemorrhage, etc. We believe this discrepancy is caused by the difference of the NHFOV settings. In the study by Xingwang Zhu (12) and Yan Li et al. (17), the amplitude could be adjusted from 25 to 50 cmH2O, which is higher than the range of 12 to 16 cmH2O and 25 to 35 cmH2O specified in other studies. Using lower frequency and higher amplitude in the NHFOV device increases tidal volume and promotes CO2 removal (22). In addition, high mean airway pressure (MAP) may also play a role, as low MAP in NHFOV probably failed to recruit the lung effectively. Xingwang Zhu et al. (12) set MAP at 5 to 16 cmH2O, and Yan Li et al. (17) set MAP at 6 to 12 cmH2O. They were able to adjust MAP to a higher level than other studies that set MAP at 6 to 8 cmH2O and 8 to 10 cmH2O.
NHFOV holds promise as a non-invasive mode of ventilation that may help reduce the risk of reintubation in selected high-risk patients. Czernik et al. (23) have investigated the feasibility of NHFOV immediately after extubation in preterm infants at high risk of extubation failure. Of the 20 infants,14 remained extubated and were transitioned to another noninvasive ventilation mode, after remaining on NHFOV for a minimum of 32 h. A multiple institution North American Retrospective case series study (24) reported that about 58% of all NHFOV instances (rescue or prophylactic) resulted in a successful transition to another noninvasive ventilation mode, thus preventing intubation in the majority of this high-risk patient group. Wang et al. (25) also suggested that NHFOV can be used as a treatment after failure of other non-invasive assisted ventilation support, or as a preventive treatment for children at high risk of extubation failure, avoiding endotracheal intubation and mechanical ventilation. However, these were relatively small observational studies without a control group, and it is difficult to predict how many infants would have remained extubated even without the use of NHFOV. Due to limitations in the published data, our study was unable to perform subgroup analyses for the preterm infants at high risk, such as less than 28 weeks and less than 1000 g. Future rigorously designed prospective randomized clinical trials are needed to provide definitive answers regarding the role of NHFOV in preterm infants at high risk of extubation.
Besides efficacy, safety was another important focus when NHFOV was used. The European survey (26) described that abdominal distention and upper airway obstruction due to viscous secretions were the most frequently reported side effects of NHFOV. However, these were only surveyed as physicians' opinions. Soutrik Seth et al. (16) did not find such alarming side effect as viscous secretions, which they attributed to good nursing care and maintenance of oral hygiene. And in our study, it was found that there was no significant difference in the risk of abdominal distension between NIPPV and NHFOV.
Ventilator-induced lung injury is a major, potentially modifiable, risk factor implicated in BPD causation. Attenuation of intra-tracheal pressure in NHFOV lowered alveolar pressure, thereby maintaining the end-expiratory volume at a normal level without atelectasis trauma to the lung parenchyma, thus reducing the risk for BPD (27). Our results showed that the reduction of the risk of BPD tended to favor NHFOV over NIPPV, although this result did not reach statistical significance. Fang Zou et al. (28) demonstrated that in the initial respiratory support, compared with NIPPV, NHFOV could reduce the risk of BPD for infants with gestational age less than 31 weeks and birth weight less than 1500 g (23% vs. 41%, P < 0.05). Therefore, the benefits of NHFOV in populations at high risk for BPD, especially very preterm and ultra-preterm infants, require further high-quality research.
Undoubtedly, some limitations in our meta-analysis may have affected the interpretation of the findings. Firstly, the trials analyzed the differences in research design and clinical characteristics of the subjects. The heterogeneity in the characteristics of the participants and interventions and the lack of a standardized assessment of reintubation and BPD were additional limitations. Secondly, subgroup analyses based on gestational age or birth weight could not be performed due to the lack of individual patient data. Finally, although the search was not limited by language or publication source, most included studies were from China. We were unable to generalize the current findings to other ethnic groups. The present survey in five European countries showed that neonatologists in 17% of 172 European NICUs used NHFOV for various indications (26), but studies in European-American countries were retrospective case series with relatively small sample sizes.
In conclusion, despite some limitations, this meta-analysis demonstrates that NHFOV could decrease the reintubation rates and shorten the duration of non-invasive ventilation compared with NIPPV. In addition, NHFOV was safe, and no significant difference in the occurrence of adverse outcomes between the two groups. While NHFOV may be of some benefit for post-extubation respiratory support in preterm neonates, definite recommendations cannot be made due to the quality of the published evidence. Further multicenter randomized controlled trials are warranted to recommend using NHFOV as post-extubation respiratory support in the management of preterm neonates.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Protocol development: all authors; literature search and assessing for eligibility: YZ, ZFW; Data extraction: LM, ZJM; analysis: LM, ZJM; critical review and approval of the manuscript: all authors. All authors contributed to the article and approved the submitted version.
We thank all the authors whose studies were included in this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2022.1063387/full#supplementary-material.
1. Nasef N, Rashed HM, Aly H. Practical aspects on the use of non-invasive respiratory support in preterm infants. Int J Pediatr Adolesc Med. (2020) 7:19–25. doi: 10.1016/j.ijpam.2020.02.005
2. Masry A, Nimeri N, Koobar O, Hammoudeh S, Chandra P, Elmalik EE, et al. Reintubation rates after extubation to different non-invasive ventilation modes in preterm infants. BMC Pediatr. (2021) 21:281. doi: 10.1186/s12887-021-02760-7
3. Al-Mandari H, Shalish W, Dempsey E, Keszler M, Davis PG, Sant'Anna G. International survey on periextubation practices in extremely preterm infants. Arch Dis Child Fetal Neonatal Ed. (2015) 100:F428–31. doi: 10.1136/archdischild-2015-308549
4. Behnke J, Lemyre B, Czernik C, Zimmer KP, Ehrhardt H, Waitz M. Non-Invasive ventilation in neonatology. DTSCH ARZTEBL INT. (2019) 116:177–83. doi: 10.3238/arztebl.2019.0177
5. Lemyre B, Davis PG, De Paoli AG, Kirpalani H. Nasal intermittent positive pressure ventilation (NIPPV) versus nasal continuous positive airway pressure (NCPAP) for preterm neonates after extubation. Cochrane Database Syst Rev. (2017) 2:CD003212. doi: 10.1002/14651858.CD003212.pub3
6. De Luca D, Dell'Orto V. Non-invasive high-frequency oscillatory ventilation in neonates: review of physiology, biology and clinical data. Arch Dis Child Fetal Neonatal Ed. (2016) 101:F565–70. doi: 10.1136/archdischild-2016-310664
7. Li J, Chen L, Shi Y. Nasal high-frequency oscillatory ventilation versus nasal continuous positive airway pressure as primary respiratory support strategies for respiratory distress syndrome in preterm infants: a systematic review and meta-analysis. Eur J Pediatr. (2022) 181:215–23. doi: 10.1007/s00431-021-04190-0
8. Haidar SA. Non-invasive high flow oscillatory ventilation in comparison with nasal continuous positive pressure ventilation for respiratory distress syndrome, a literature review. J Matern Fetal Neonatal Med. (2021) 34:2900–9. doi: 10.1080/14767058.2019.1671332
9. Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. (2015) 4:1. doi: 10.1186/2046-4053-4-1
10. Zeng X, Zhang Y, Kwong JS, Zhang C, Li S, Sun F, et al. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evid Based Med. (2015) 8:2–10. doi: 10.1111/jebm.12141
11. Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. Br Med J. (2008) 336:924–6. doi: 10.1136/bmj.39489.470347.AD
12. Zhu X, Qi H, Feng Z, Shi Y, De Luca D. Noninvasive high-frequency oscillatory ventilation vs nasal continuous positive airway pressure vs nasal intermittent positive pressure ventilation as postextubation support for preterm neonates in China: a randomized clinical trial. Jama Pediatr. (2022) 176:551–9. doi: 10.1001/jamapediatrics.2022.0710
13. Yaoli J, Guanjun Z, kuangzhao Z. Comparison of different ventilation modes in premature infants with low body mass respiratory distress syndrome after extubation. China Pract Med J. (2021) 48:49–52.
14. Xiaozhan H, Yongxing L, Fangli Z. Comparison of the effect of non-invasive high frequency ventilation and nasal intermittent positive pressure ventilation in the treatment of neonatal respiratory distress syndrome after withdrawal. Clin Med. (2021) 41:69–70.
15. Yan Z, Xirong G, Yunqin W, Yuee X, Dunmin Z. Application of non-invasive high-frequency oscillatory ventilation after extubation and deuteration in premature infants with severe bronchopulmonary dysplasia. Chin J Neonatol. (2021) 36:42–7.
16. Seth S, Saha B, Saha AK, Mukherjee S, Hazra A. Nasal HFOV versus nasal IPPV as a post-extubation respiratory support in preterm infants—a randomised controlled trial. Eur J Pediatr. (2021) 180:3151–60. doi: 10.1007/s00431-021-04084-1
17. Li Y, Wei Q, Zhao D, Mo Y, Yao L, Li L, et al. Non-invasive high-frequency oscillatory ventilation in preterm infants after extubation: a randomized, controlled trial. J Int Med Res. (2021) 49:030006052098491. doi: 10.1177/0300060520984915
18. Wang Z, Gao W, Shen Y, Lin X, Shen Y, Zhou W, et al. Application of non-invasive high-frequency oscillatory ventilation after extubation in infants with very low birth weight respiratory distress syndrome. Guangdong Medical. (2019) 40:1391–5.
19. Zhenyu L, Na C, Wenjia W. Evaluation of non-invasive high frequency ventilation for respiratory support after withdrawal of neonatal acute respiratory distress syndrome. Chin Med Sci. (2019) 9:110–2.
20. Li J, Zhang J, Hao Q, Shen Z, Du Y, Chen H, et al. The impact of time interval between first extubation and reintubation on bronchopulmonary dysplasia or death in very low birth weight infants. FRONT PEDIATR. (2022) 10:867767. doi: 10.3389/fped.2022.867767
21. Shalish W, Kanbar L, Kovacs L, Chawla S, Keszler M, Rao S, et al. The impact of time interval between extubation and reintubation on death or bronchopulmonary dysplasia in extremely preterm infants. J Pediatr. (2019) 205:70–76.e2. doi: 10.1016/j.jpeds.2018.09.062
22. Li J, Li X, Huang X, Zhang Z. Noninvasive high-frequency oscillatory ventilation as respiratory support in preterm infants: a meta-analysis of randomized controlled trials. Respir Res. (2019) 20:58. doi: 10.1186/s12931-019-1023-0
23. Czernik C, Schmalisch G, Bührer C, Proquitté H. Weaning of neonates from mechanical ventilation by use of nasopharyngeal high-frequency oscillatory ventilation: a preliminary study. J Matern Fetal Neonatal Med. (2012) 25:374–8. doi: 10.3109/14767058.2011.580401
24. Mukerji A, Singh B, Helou SE, Fusch C, Dunn M, Belik J, et al. Use of noninvasive high-frequency ventilation in the neonatal intensive care unit: a retrospective review. Am J Perinatol. (2015) 30:171–6. doi: 10.1055/s-0034-1381317
25. Wang CH, Shi LP, Ma XL, Lin HJ, Xu YP, Du LZ. [Use of noninvasive high-frequency oscillatory ventilation in very low birth weight infants]. Zhonghua Er Ke Za Zhi. (2017) 55:177–81. doi: 10.3760/cma.j.issn.0578-1310.2017.03.003
26. Fischer HS, Bohlin K, Bührer C, Schmalisch G, Cremer M, Reiss I, et al. Nasal high-frequency oscillation ventilation in neonates: a survey in five European countries. Eur J Pediatr. (2015) 174:465–71. doi: 10.1007/s00431-014-2419-y
27. Null DM, Alvord J, Leavitt W, Wint A, Dahl MJ, Presson AP, et al. High-frequency nasal ventilation for 21 d maintains gas exchange with lower respiratory pressures and promotes alveolarization in preterm lambs. PEDIATR RES. (2014) 75:507–16. doi: 10.1038/pr.2013.254
Keywords: noninvasive high-frequency oscillatory ventilation, nasal intermittent positive-pressure ventilation, preterm infants, respiratory support, meta-analysis
Citation: Mei Z, Ming L, Wu Z and Zhu Y (2023) Use of NHFOV vs. NIPPV for the respiratory support of preterm newborns after extubation: A meta-analysis. Front. Pediatr. 10:1063387. doi: 10.3389/fped.2022.1063387
Received: 7 October 2022; Accepted: 21 December 2022;
Published: 11 January 2023.
Edited by:
Christoph Bührer, Charité Universitätsmedizin Berlin, GermanyReviewed by:
Manoj Biniwale, University of Southern California, United States© 2023 Mei, Ming, Wu and Zhu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yong Zhu Y3FtdXpodXlvbmdAMTYzLmNvbQ== Zhifeng Wu d3V6aGlmZW5ndmlwQDEyNi5jb20=
†These authors have contributed equally to this work and share first authorship
Specialty Section: This article was submitted to Neonatology, a section of the journal Frontiers in Pediatrics
AbbreviationsIMV, invasive mechanical ventilation; BPD, bronchopulmonary dysplasia; NHFOV, noninvasive high-frequency oscillatory ventilation; NIPPV, nasal intermittent positive pressure ventilation; LOS, length of hospital stay; IVH, intraventricular hemorrhage; ROP, retinopathy of prematurity; NEC, necrotizing enterocolitis; RRV, Risk Ratio; SMD, standardized mean difference (SMD); CI, confidence intervals; MAP, mean airway pressure.
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.