- 1Pediatric Orthopedics Department, Wuxi 9th People's Hospital Affiliated to Soochow University, Wuxi, China
- 2Department of Orthopaedic, Wuhan Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
- 3Department of Orthopaedics and Trauma Surgery, Karama Medical Center, Dubai, United Arab Emirates
Background: Supracondylar humeral fractures (SHF) are the most common type of fracture occurring at the distal humerus in children. In patients with delayed presentation of SHF, closed reduction is challenging to achieve with traditional reduction maneuvers. This study aimed to report the clinical results of pediatric SHF delayed over 14 days treated by closed reduction with a minimally invasive technique and external fixation and evaluate the efficacy of this technique.
Methods: Between October 2010 and September 2018, children with delayed presentation of SHF over 14 days were retrospectively included in this study. The patients received closed reduction with a minimally invasive technique followed by external fixation. The demographics and radiographic data were collected. The Mayo Elbow Performance Score (MEPS) and the Flynn criteria were used to evaluate the clinical outcomes of treatments.
Results: A total of 11 children (aged 4–13 years) with delayed presentation (range, 14–22 days) were recruited. They received surgery using closed reduction with a minimally invasive technique followed by external fixation. None of the surgery was done with the open method. After surgery, the patients' carrying angle returned to normal. The radiological union was evident in 8 to 12 weeks in all fractures without complications. Every patient had a good to excellent score on the MEPS and the Flynn criteria.
Conclusions: The results of this series indicated a satisfactory outcome in children with delayed more than 14 days of supracondylar humeral fractures. The closed reduction with a minimally invasive technique followed by external fixation is an alternative treatment for such injury.
Introduction
Supracondylar humeral fracture (SHF) is an extra-articular fracture that passes through the olecranon fossa, encompasses the distal humeral condyles, and is one of the most common elbow injuries in children (1). Delayed presentation of SHF is defined if the patient presents to the hospital after 2 days of injury (2, 3). Patients with delayed presentation (>1 week) may present with callus formation, union, nonunion and/or malunion with varying degrees of elbow deformity and dysfunction (4).
Treatment of delayed SHF aims to attain anatomic reduction, stable fixation, comprehensive function and good cosmetic results. However, there is no consensus regarding the appropriate treatment method for delayed SHF among orthopedic surgeons (5). Treatment includes closed reduction or open reduction with fixation. Closed reduction and percutaneous fixation has become the preferred treatment option for pediatric SHF but usually fails in patients presenting more than 7 days after injury (4). On the other hand, open reduction and internal fixation may cause iatrogenic neurovascular injury, wound infection, elbow stiffness and other complications (6).
This study aimed to report the clinical results of pediatric SHF delayed over 14 days treated by closed reduction with a minimally invasive technique and external fixation and evaluate the efficacy of this technique.
Patients and methods
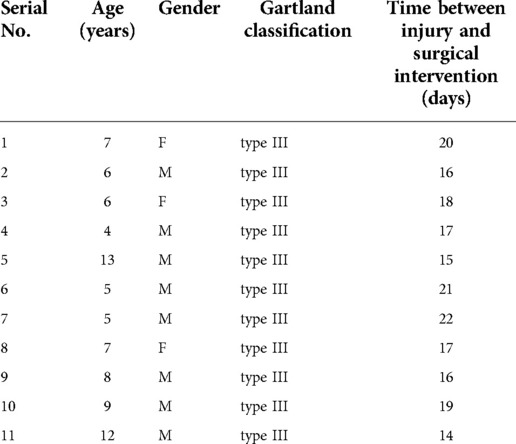
Children diagnosed with delayed SHF between October 2010 and September 2018 at the authors' hospital were retrospectively reviewed. The inclusion criteria were: (1) patients with delayed SHF more than 14 days after injury, (2) visible callus formation on the radiographs with failed manual reduction, (3) carrying angle of more than −15°, (4) availability of the complete clinical and radiological data, and (5) minimum follow up of 24 months. The exclusion criteria were: (1) patients with metabolic bone disease and (2) concomitant neurovascular injury needing exploratory surgery. Demographic data included age, gender, Gartland classification and time between injury and surgical intervention. All the patients' parents or legal guardians were fully informed of the surgical procedure and gave consent to be included in the study. It was informed that closed reduction might not be achieved and minimally invasive incision might be necessary. All patients were operated on by the same surgical team as per the standard protocol. This study was approved by the ethical review board of the corresponding author's institution.
Surgical technique
All the procedure was performed under general anesthesia. The patient was positioned supine with the injured extremity close to the edge of the operating table. The fracture line with the callus was located under fluoroscopy (Figure 1A). A 5 mm skin incision was made from the medial aspect of the humerus, closed to the fracture line with callus and guided by the intraoperative fluoroscopy. A hemostat was inserted, and soft tissue was mobilized away from the callus. Lateral, anterior, and posterior calluses were removed from the humerus horizontally along the fracture line with the hemostat in order to loosen the fracture (Figure 1B). Manual reduction of fractures was performed in order to correct the abnormal carrying angle, rotation and shortening after the fracture was loosened (Figure 1C).
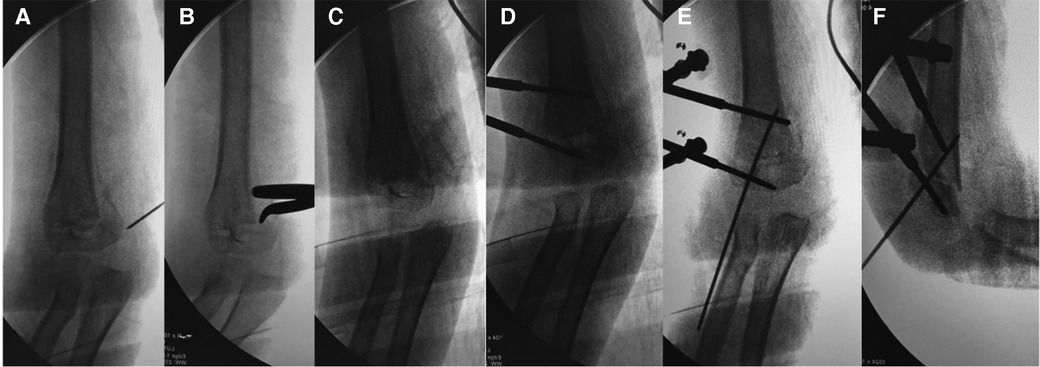
Figure 1. C-arm image during the surgical procedure of a 5-year-old boy with delayed supracondylar fracture of right humerus: (A) the fracture line with callus was located with a needle; (B) lateral, anterior, and posterior calluses were removed from the humerus horizontally along the fracture line with the hemostat; (C) manual reduction of fractures was performed to correct the abnormal carrying angle; (D) external fixation with two schanz pins was used; (E) placement of K-wire was served as a de-rotational wire to stabilize the fracture; (F) lateral view of the elbow after fixation.
External fixation was used for patients as per the technique reported by Slongo T et al. (7) The first Schanz pin (3.0–4.0 mm) was placed perpendicular to the longitudinal axis of the proximal humerus and buried in the medial cortex, keeping 2 cm above the fracture line. The second pin was placed perpendicular to the longitudinal axis of the distal fragment and parallel to the elbow joint, keeping 1–2 cm below the fracture line (Figure 1D). It was regarded as an adequate and stable reduction without malrotation following manual reduction when these 2 pins became parallel. A 1.5–2.0 mm K-wire was passed retrograde from the lateral epicondyle crossing the fracture line as a de-rotational wire (Figure 1E,F). The stability of the fixation was then tested in maximum flexion and extension, and a check x-ray was obtained. The surgical procedure of a typical case is presented in Figure 1.
Postoperative care and follow-up
All patients were discharged 2–3 days after surgery without a cast. Free range of motion with non-weight-bearing was allowed 48 h post-operation. The external fixation was removed 6 weeks postoperatively. Every patient returned for clinical and radiographic evaluations at 6 weeks, 12 weeks, 6 months, 12 months and 24 months. The elbow joint function was evaluated with the Mayo Elbow Performance Score (MEPS) and the criteria of Flynn at the last follow-up (8, 9). The typical case in fellow up was presented in Figure 2.
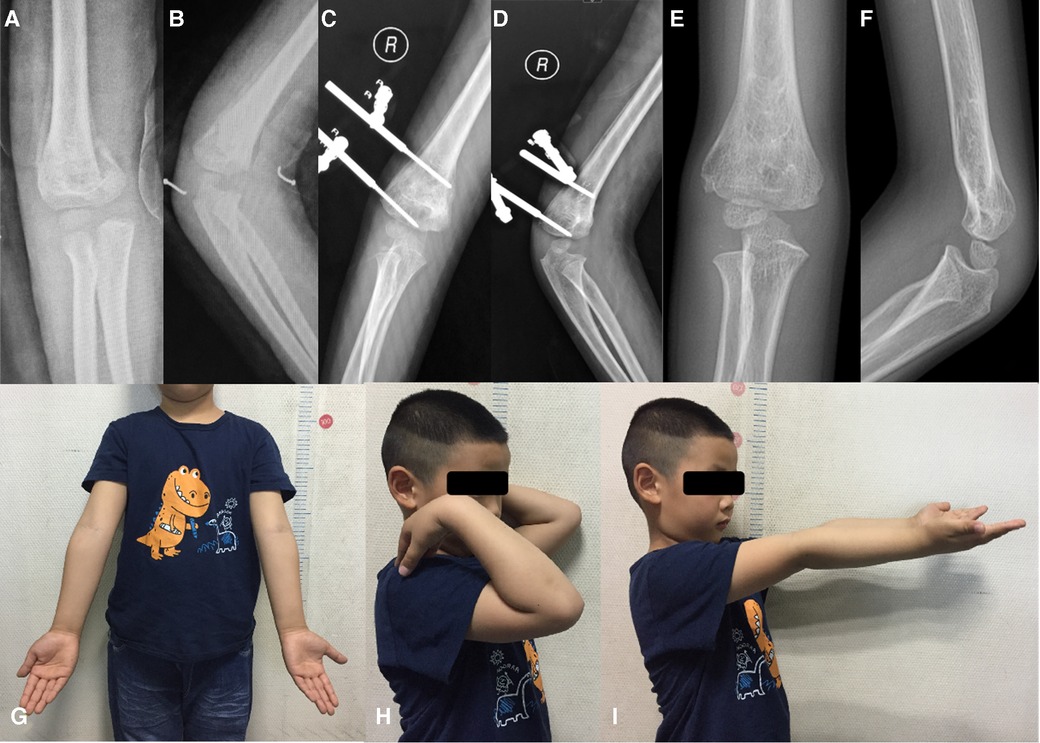
Figure 2. (A) anteroposterior and (B) lateral radiographs of the 5-year-old boy with delayed supracondylar fracture of right humerus; (C) anteroposterior and (D) lateral radiographs at 6 weeks post-operation; (E) anteroposterior and (F) lateral radiographs at 12 months post-operation; and the follow-up in 24 months after surgery show excellent cosmetic results (G) and the functional appearance (H,I).
Results
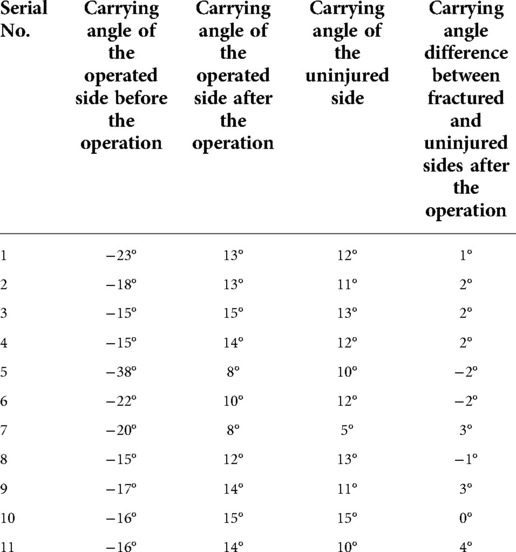
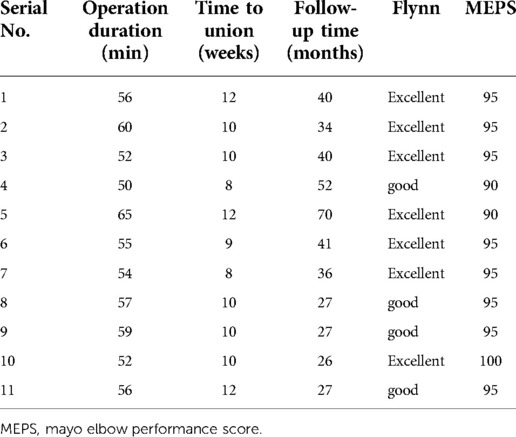
A total of 11 patients (8 boys and 3 girls) with an average age of 7 years (range, 4–13 years) were included in this study. Closed reduction with a minimally invasive technique achieved a satisfactory reduction in all patients. All cases were classified as Gartland type III and underwent surgery with an average of 17.7 days after injury (Table 1). The average duration of the surgery was 56 min (range, 50–65 min). The radiological union was evident in 8 to 12 weeks in all fractures. No complications such as Volkmann ischemic contracture, infection, nonunion, myositis ossificans, iatrogenic neurological injuries or residual vascular deficits were noted. The carrying angle difference between fractured and uninjured sides was less than 4°, and cosmetic results in all patients were excellent (Table 2). At the last follow-up, all patients reported 90 points or more on MEPS and good to excellent outcomes on Flynn criteria (Table 3). The therapeutic effect was satisfactory in all patients. Neither revision surgery after the initial fixation nor change in muscle power in the injured limb relative to the uninjured limb was reported at the last follow-up.
Discussion
To our best knowledge, this was the first study reporting the outcome of pediatric supracondylar humerus fractures treated with closed or mini-open reduction and external fixation after 14 days of injury. SHF accounts for 55% to 80% of total elbow fractures in children and up to two-thirds of pediatric elbow injuries require hospitalization (10). This type of fracture usually occurs as a result of a fall from height and the incidence is estimated to be 177.3 per 100,000 (11). Delayed presentation of SHF is defined if the patient presents to the hospital after 2 days of injury in developed countries (4). Prabhakar P et al. reported that surgical treatment of low-severity Gartland type III SHFs might be delayed without increasing surgical time and reduction difficulty, but only if the delay time was about 18.5 h, which was hardly a delay in developing countries (12). Silva M et al. showed that anatomic reduction of type II humeral supracondylar fractures could be achieved probably even when closed reduction and percutaneous pinning was performed 7 days after the original injury, but the risk of avascular necrosis of the humeral trochlea must be considered (13). In developing countries, the delayed duration always exceeds 7 days, and the reasons for a delay in interventions are quackery, lack of medical facilities, cost, poor economic status, lack of awareness, delayed referral from the rural hospital, fear of surgery, and various indigenous forms of treatment, which bring difficulty for closed reduction (14–16).
Optimum treatment of SHF is essential in order to avoid serious complications. It is well recognized that the Gartland type III and type IV fractures should be treated surgically (17). To date, closed reduction and percutaneous pinning is the gold standard for all displaced fractures (10). The advantages of closed reduction are the preservation of blood supply to the fracture site, shortening of hospital stays and reduction of risk of infection (18). However, controversy remains with regard to the timing of emergency reduction, whether reduction can be safely delayed, the adequate reduction technique, the risk/benefit ratio of open reduction and the long-term consequences of a cubitus varus deformity (19). It is a challenge for surgeons to improve the success rate of closed reduction, especially for delayed supracondylar humeral fractures. Displaced supracondylar fractures had been traditionally treated as surgical emergencies for the reason that delayed surgery often required open reduction rather than closed reduction (20). In the case of delayed presentation, especially for Gartland type III fractures which is a statistically significant independent risk factor for closed reduction failure, the probability of fracture swelling is significantly increased, for which open reduction is needed to achieve better outcomes and avoid complications such as iatrogenic neurovascular injuries, stiffness, delayed union, malunion and nonunion (14, 15, 21, 22). A meta-analysis conducted by Farrow L et al. showed that there was no statistically significant difference in the risk of complications between immediate and 91-h delayed treatment for patients with SHFs undergoing open reduction (23). However, all the patients in this study were Gartland type III fractures and were delayed over 14 days. All achieved a satisfactory result with reduction with a minimally invasive technique.
The formation of intraperiosteal bone begins immediately after the fracture, but proliferative activity in the cells appears to cease before 2 weeks. By the time the endochondral process has reached the stage of chondrogenesis, a large number of woven bone forms near the fracture site. Once the fracture coalesces through the bone-bridging gap, the callus (composed entirely of woven bone) remodels to form a mechanically capable layered structure (24). Callus formation occurs even faster in children, which is why closed reduction over 14 days often fails and open reduction is the only option left. Close reduction avoids complications related to open reduction, such as wound infection or elbow stiffness (18, 25, 26). However, the closed reduction could not be achieved in a single patient presenting more than 7 days after injury in Tiwari A et al.'s study because closed reduction and cast fixation were not feasible in late-presenting SHFs. The injury is usually accompanied by severe swelling that prevents rapid and safe flexion, and soft tissue scabbed at the end of the first week precludes reduction of the fracture (4). All the patients achieved a satisfactory reduction using the minimally invasive technique in this study. Traditional K-wires fixation of SHF was not performed in this series because without removing the callus from the fracture site, the fixation could not be stable only by K-wires. Instead, the external fixator could provide better stability than K-wires. Sufficient stability following the use of an external fixator allowing an early functional exercise was indicated by good to excellent functional outcomes. Also, none of the cases underwent revision surgery in our series.
The carrying angle of the elbow is used to assess varus or valgus deformity (19). The patients' carrying angles in this study were over −15° pre-operation, with a high risk of cubitus varus deformity that might lead to a second corrective osteotomy. After the operation, the carrying angle difference between fractured and uninjured sides was less than 4°, indicating that the reduction of fracture by minimally invasive technique and application of external fixation corrected the preoperative cubitus varus effectively. Masumbuko CK et al. showed that delaying surgery for more than seven days resulted in reduced elbow range of motion (27). In contrast, midterm follow-up results of the elbow function were satisfactory in our study. The advantages of external fixation include stable fixation avoiding delayed healing and early mobilization, which may contribute to good functional results (7, 28). This method reduced the risk of complications of open reduction, such as neurovascular injury, elbow stiffness, wound infection and ugly scarring, as well as complications due to unsatisfactory closed reduction, including triceps fibrilization and limited elbow mobility.
Limitations of this study were the small number of cases, failure to follow-up until the closure of physes, and its retrospective nature. This case series could not provide a control group because none of the parents or guardians chose to wait for a long-term outcome with a high risk of cubitus varus. They all chose a one-stage procedure in view of carrying angle >−15°.
Conclusions
The results of this series indicated a satisfactory outcome in children with delayed more than 14 days of supracondylar humeral fractures. The closed reduction with a minimally invasive technique followed by external fixation is an alternative treatment for such kind of injury.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving human participants were reviewed and approved by The Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology (IORG No: IORG0003571). Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin. Written informed consent was obtained from the individual(s), and minor(s)' legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author contributions
JTL, ZXO and ZZW were involved in data collection and follow-up assessments. XT, SR and WFL were responsible for literature search and study design, SL and YYP drafted the manuscript. XT, WFL and SR finalized the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Marquis CP, Cheung G, Dwyer J, Emery D. Supracondylar fractures of the humerus. Curr Orthop. (2008) 22:62–9. doi: 10.1016/j.cuor.2007.12.002
2. Devnani AS. Late presentation of supracondylar fracture of the humerus in children. Clin Orthop Relat Res. (2005) 431:36–41. doi: 10.1097/01.blo.0000152439.43810.11
3. Harwant S, Borhan TA. The efficacy of side arm traction in the reduction of supracondylar fracture humerus in children. Med J Malaysia. (2000) 55:311–7.11200710
4. Tiwari A, Kanojia RK, Kapoor SK. Surgical management for late presentation of supracondylar humeral fracture in children. J Orthop Surg. (2007) 15:177–82. doi: 10.1177/230949900701500211
5. Eren A, Guven M, Erol B, Cakar M. Delayed surgical treatment of supracondylar humerus fractures in children using a medial approach. J Pediatr Orthop. (2008) 2:21–7. doi: 10.1007/s11832-007-0072-y
6. Lal GM, Bhan S. Delayed open reduction for supracondylar fractures of the humerus. Int Orthop. (1991) 15:189–91. doi: 10.1007/BF00192291
7. Slongo T. Treatment of posttraumatic cubitus varus in children and adolescents. Supracondylar humeral osteotomy using radial external fixation. Oper Orthop Traumatol. (2015) 27:194–209. doi: 10.1007/s00064-015-0403-y
8. Cusick MC, Bonnaig NS, Azar FM, Mauck BM, Smith RA, Throckmorton TW. Accuracy and reliability of the mayo elbow performance score. J Hand Surg Am. (2014) 39:1146–50. doi: 10.1016/j.jhsa.2014.01.041
9. Fowler TP, Marsh JL. Reduction and pinning of pediatric supracondylar humerus fractures in the prone position. J Orthop Trauma. (2006) 20:277–81. doi: 10.1097/00005131-200604000-00008
10. Omid R, Choi PD, Skaggs DL. Supracondylar humeral fractures in children. J Bone Jt Surg, Am Vol. (2008) 90:1121–32. doi: 10.2106/JBJS.G.01354
11. Mulpuri K, Hosalkar H, Howard A. AAOS Clinical practice guideline: the treatment of pediatric supracondylar humerus fractures. J Am Acad Orthop Surg. (2012) 20:328–30. doi: 10.5435/JAAOS-20-05-328
12. Prabhakar P, Ho CA. Delaying surgery in type III supracondylar humerus fractures does not lead to longer surgical times or more difficult reduction. J Orthop Trauma. (2019) 33:e285–90. doi: 10.1097/BOT.0000000000001491
13. Silva M, Wong TC, Bernthal NM. Outcomes of reduction more than 7 days after injury in supracondylar humeral fractures in children. J Pediatr Orthop. (2011) 31:751–6. doi: 10.1097/BPO.0b013e31822f16e5
14. Qiu X, Deng HS, Zhao ZH, Zeng SD, Zeng YP, Wang XY, et al. Upper limb pediatric fractures in 22 tertiary children's Hospitals, China: a multicenter epidemiological investigation and economic factor analysis of 32,832 hospitalized children. J Orthop Surg Res. (2022) 17(300):17. doi: 10.1186/s13018-022-03159-5
15. Das R, Borthakur B, Agarwala V, Ghosh S. Evaluation of anterior approach in failed closed reduction and delayed presentation of supracondylar humerus fractures in children. J Orthop. (2022) 30:51–8. doi: 10.1016/j.jor.2022.02.006
16. Anjum R, Sharma V, Jindal R, Singh TP, Rathee N. Epidemiologic pattern of paediatric supracondylar fractures of humerus in a teaching hospital of rural India: a prospective study of 263 cases. Chin J Traumatol. (2017) 20:158–60. doi: 10.1016/j.cjtee.2016.10.007
17. Barton KL, Kaminsky CK, Green DW, Shean CJ, Kautz SM, Skaggs DL. Reliability of a modified Gartland classification of supracondylar humerus fractures. J Pediatr Orthop. (2001) 21:27–30. doi: 10.1097/00004694-200101000-00007
18. The RM, Severijnen RS. Neurological complications in children with supracondylar fractures of the humerus. Eur J Surg. (1999) 165:180–2. doi: 10.1080/110241599750007009
19. Gartland JJ. Management of supracondylar fractures of the humerus in children. Surg Gynecol Obstet. (1959) 109:145–54.13675986
20. Wilkins KE. Residuals of elbow trauma in children. Orthop Clin North Am. (1990) 21:291–314. doi: 10.1016/S0030-5898(20)31546-7
21. Beck JD, Riehl JT, Moore BE, Deegan JH, Sartorius J, Graham J, et al. Risk factors for failed closed reduction of pediatric supracondylar humerus fractures. Orthopedics. (2012) 35:e1492–6. doi: 10.3928/01477447-20120919-18
22. Li J, Fu D, Yu C, Wang S, Ze R, Tang X. Surgical management of delayed irreducible Gartland III supracondylar fractures in children: open reduction and internal fixation versus external fixation. J Shoulder Elbow Surg. (2017) 26:299–304. doi: 10.1016/j.jse.2016.10.006
23. Farrow L, Ablett AD, Mills L, Barker S. Early versus delayed surgery for paediatric supracondylar humeral fractures in the absence of vascular compromise: a systematic review and meta-analysis. Bone Joint J. (2018) 100-B:1535–41. doi: 10.1302/0301-620X.100B12.BJJ-2018-0982.R1
24. Einhorn TA. The cell and molecular biology of fracture healing. Clin Orthop Relat Res. (1998) 355:S7–21. doi: 10.1097/00003086-199810001-00003
25. Nayak AR, Natesh K, Bami M, Vinayak S. Is closed manipulative reduction and percutaneous Kirschner wiring of supracondylar humeral fracture in children as day-care surgery a safe procedure? Malays Orthop J. (2013) 7:1–5. doi: 10.5704/MOJ.1307.006
26. Savvidou OD, Zampeli F, Koutsouradis P, Chloros GD, Kaspiris A, Sourmelis S, et al. Complications of open reduction and internal fixation of distal humerus fractures. EFORT Open Rev. (2018) 3:558–67. doi: 10.1302/2058-5241.3.180009
27. Masumbuko CK, Mutheke EG, Mbindyo B, Hawkes MT. Delayed surgery leads to reduced elbow range of motion in children with supracondylar humeral fractures managed at a referral hospital in sub-saharan Africa. Afr Health Sci. (2019) 19:2565–70. doi: 10.4314/ahs.v19i3.32
Keywords: close reduction, minimally invasive technique, external fixation, delayed presentation, supracondylar humeral fracture, children
Citation: Liu S, Peng Y, Liu J, Ou Z, Wang Z, Rai S, Lin W and Tang X (2022) Small incision reduction and external fixation for the treatment of delayed over fourteen days supracondylar humeral fractures in children. Front. Pediatr. 10:1039704. doi: 10.3389/fped.2022.1039704
Received: 8 September 2022; Accepted: 14 October 2022;
Published: 2 November 2022.
Edited by:
Federico Canavese, Centre Hospitalier Regional et Universitaire de Lille, FranceReviewed by:
Weibin Du, Zhejiang Chinese Medical University, ChinaYuan Zhang, Children's Hospital of Chongqing Medical University, China
© 2022 Liu, Peng, Liu, Ou, Wang, Rai, Lin and Tang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xin Tang ZHJfeGludGFuZ0BodXN0LmVkdS5jbg==
†These authors have contributed equally to this work and share first authorship
‡These authors have contributed equally to this work and share last authorship
Specialty Section: This article was submitted to Pediatric Orthopedics, a section of the journal Frontiers in Pediatrics
 Shuai Liu
Shuai Liu YingYing Peng
YingYing Peng JiaTong Liu2
JiaTong Liu2 Saroj Rai
Saroj Rai Xin Tang
Xin Tang