
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr. , 22 December 2022
Sec. Pediatric Infectious Diseases
Volume 10 - 2022 | https://doi.org/10.3389/fped.2022.1017386
Background: Pneumonia, which is a form of acute lower respiratory tract infection, affects the lung parenchyma and destructs alveolar air space. Pneumonia is the leading cause of morbidity and mortality in under-five children. It was estimated that pneumonia kills 900,000 under-five children each year worldwide. Approximately 172 deaths per 1,000 live births occur in sub-Saharan African countries, with pneumonia being the major cause. This study aimed to assess the prevalence and determinant factors of pneumonia inunder-five children in southern Ethiopia.
Methodology: An institutional cross-sectional study was employed. A total of 239 child–caregiver pairs were included. Data were collected by trained nurses using a semi-structured questionnaire. The collected data were checked for completeness, coded and entered into EPI data version 4.6, and exported to SPSS version 25 for analysis. Results were reported as the mean, frequency, and percentile. Logistic regression was employed to assess statistically significant predictors of pneumonia. Variables with a p-value <0.05 were considered statistically significant factors of pneumonia.
Result: The prevalence of pneumonia in the study area was 30%. Among the factors assessed, place of food cooking—inside the living room [adjusted odd ratio (AOR) = 5.79, 95% confidence interval (CI): 2.47–13.58], nonexclusive breastfeeding (AOR = 3.26, 95% CI: 1.42–7.52), vitamin A supplementation status (AOR = 5.62, 95% CI: 2.65–11.94), and vaccination status (AOR = 3.59, 95% CI: 1.49–8.66) were significantly associated with the occurrence of pneumonia in under-five children.
Conclusion: This study showed that the prevalence of pneumonia was relatively higher in Arba Minch town than other parts of the country. Place of food cooking, nonexclusive breastfeeding, vitamin A supplementation status, and vaccination status of children were significant factors of pneumonia among under-five children. Enhancing caregivers’/mothers’ awareness of predicted factors was needed to reduce the incidence of childhood pneumonia and to enhance children's quality of health.
Pneumonia is a acute lower respiratory tract infection that affects the lung parenchyma and destructs alveolar air space (1). Pneumonia is the leading cause of morbidity and mortality in under-five children. In 2016, it was estimated that 900,000 under-five children died of pneumonia worldwide (2). From these, sub-Saharan African countries took the lion's share with 50% of the burden of worldwide under-five children mortality rate due to pneumonia. Approximately 172 deaths per 1,000 live births occur in sub-Saharan African countries, mainly due to pneumonia (3, 4). Between 2000 and 2019, the global under-five children mortality rate decreased by about 50%, but progress is still slower, and 65 (32%) of 204 countries, primarily in sub-Saharan Africa and south Asia, are not on course to fulfil either sustainable development goal (SDG) 3.2 targeted by 2030 (5). Nearly half of all under-five deaths in 2019 occurred in just five countries: Nigeria, India, Pakistan, the Democratic Republic of Congo and Ethiopia. Globally, infectious diseases, including pneumonia, diarrhea, and malaria, remain a leading cause of under-five deaths (6). Children with compromised immune systems like malnutrition, especially those not exclusively fed under-five children, are at a higher risk of developing pneumonia (7).
In developing countries like Ethiopia, the risk factors for pneumonia in under-five children are numerous. Among factors, nonexclusive breastfeeding, lack of/incomplete immunization, environmental conditions, outdoor/indoor air pollution, micronutrients, and vitamin deficiencies are predominantly reported (8–10).
The World Health Organization's Integrated Management of Childhood Illness (IMNCI) recommendations have been used in Ethiopia, which has done so since 2001 (11). Additionally, Ethiopia made a policy breakthrough by introducing community-based treatment of pneumonia through health extension workers in 2010. This was done to increase access to lifesaving interventions. Since then, integrated community case management has been used to treat pneumonia in the community by health extension workers over the whole health posts in the country. Even though child mortality due to pneumonia decreased, progress among under-five children is still slow (12).
In Ethiopia, pneumonia is one the leading causes of death in under-five children, with an estimated contribution of more than 40,000 deaths annually (13, 14). These deaths could be prevented by cost-effective interventions like immunization, health education, good nutrition, exclusive breastfeeding, and sanitary management (9). Reports showed that the prevalence of pneumonia among under-five children in Ethiopia reached 20.68% (14). According to a study conducted in Wondo Genet, southern Ethiopia, the magnitude of pneumonia in under-five children visiting health centers was reported to be 33.5% (15). Globally, Ethiopia ranks sixth among the top 15 countries in morbidity and mortality from pneumonia (16). Predictive factors of pneumonia need to be studied to better inform healthcare providers and other stakeholders/policymakers to consider additional pneumonia prevalence reduction strategies. Although studies are conducted in Ethiopia, the determinant factors for pneumonia differ in different societies and study populations (17). Taking the high burden of pneumonia and the variability of risk factors into account, this study aimed to identify the predicted factors of pneumonia among under-five children. Furthermore, there is no previous study in the area that could show the current status of pneumonia and its determinant factors.
All under-five children visiting the Pediatrics Outpatient Department of Arba Minch General Hospital.
All under-five children visiting the Pediatrics Outpatient Department of Arba Minch General Hospital during the data collection period.
The study included children who were under 5 years of age, those who were residents of Arba Minch town for a minimum of 6 months, and those who visited the pediatric unit of Arba Minch referral Hospital during the study period. Children with the following conditions were excluded from the study: cough that lasted for more than 15 days, cough because of the recent history of aspiration of liquid or foreign body, cardiac disease, and caregiver who did not have any information about the child during the time of data collection.
The study utilized the single population proportion formula technique to determine the study population sample size
where n is the desired sample size,
P is the population of under-five pneumonia children, which is 28.1% (18), have taken from previously published study from jimma town
Zα/2 is the critical value at the 95% confidence interval level of certainty (1.96), and
d is the margin of error between the sample and population (5%)
where source population (N)= 728, which was a monthly plan on the proportion of under-five children visiting the outpatient department in Arba Minch General Hospital. Because the source population was less than 10,000, we can use the correction formula to get the actual sample size of the study population:
where
nf = final sample size,
n = first calculated sample size,
N = source population.
. By adding 10% of the nonresponse rate, the total sample size of this study was 217 + 22 = 239.
A total of 239 participants were enrolled in this study. The study participants were selected by using the simple random sampling technique from under-five children outpatient registration book of Arba Minch General Hospital. The first study participant was selected by using K-value. That is
The first was selected from 1 − k (that is, from 1 to 3) by using the lottery method on the first day of data collection.
Dependent variables: Pneumonia among under-five children.
Independent variables:
Sociodemographic factors: Age, sex, and residence.
Health facility and childcare factors: Low birth weight, prematurity, exclusive breastfeeding, breastfeeding duration, vaccination status, and vitamin “A” supplementation.
Cook food inside the living room, home aeration, hand washing practice, domestic smoking, and carrying baby during cooking.
The data collection tool was developed after reviewing previously published relevant literature (14, 18, 19). The adopted structured questionnaire included sociodemographic factors, environmental factors, and health facility and childcare factors. Before data collection was started, the questionnaire was pretested on a 5% sample size at Chencha Primary Hospital to ensure the validity and reliability of the study tool. After collecting the pretest data, it was checked for potential problems related to the tool, such as any difficult question that was not easily understandable and unclear to reply, and corrective measures were taken. The data were collected through face-to-face interviews and medical chart reviews. Charts were reviewed to collect information about the diagnosis, pre-existing or comorbidities, and anthropometric data. Data were collected by four diploma nurses and one first-degree nurse who received 2 days of training on the objective and contents of the study.
The collected data were checked for completeness, coded and entered into Epi Info version 6, and exported to SPSS version 25 for analysis. Then, data were cleaned for consistency and the extent of outliers. Different statistical assumptions and appropriate corrections were made prior to analysis. Descriptive analyses were made for each independent variable. Bivariate and multivariate binary logistic regression analyses were used to test the association between the independent and dependent variables. Bivariate analysis was performed for each of the independent variables with the outcome variable. Variables with a p-value of <0.25 on bivariate analysis were taken as candidates for multivariate binary logistic regression model analysis to identify predictors of the outcome variable. Variables with a p-value of <0.05 on multivariate binary logistic regression analysis were considered predictive factors for pneumonia among under-five children. The strength of the association between the outcome variable and independent variables was expressed using an adjusted odd ratio (AOR) with 95% confidence intervals (CIs).
A total of 239 children's mothers/caregivers have participated in the current study, which made a response rate of 100%. About 125 (52.3%) of the children were boys. The highest proportions (41%) of participating children were in the age group of 12–36 months. In the current study, 75% of the respondents (children's mothers/caregivers) had formal education. Regarding the marital status of children's mothers/caregivers, 230 (96.2%) of the participants were married. The occupational profile of children's mothers/caregivers showed that the majority (189, 79%) were self-employed and 30 (12.5%) were civil servants. More than half (54.8%) of the study participants were residing in rural parts of the study area (shown in Table 1).
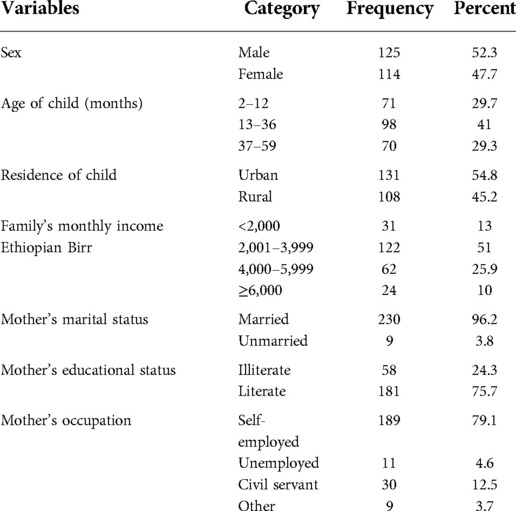
Table 1. Sociodemographic characteristics of children and mothers/caregivers studied at the Arba Minch General Hospital, southern Ethiopia (2021).
From the total participating children, 38% had a history of cough, 18% had difficulty breathing, and 34% had fast breathing at the time of the study. In addition to these signs and symptoms, 169 (70.7%) had a fever, and 35 (14.6%) had chest in-drawing. Our study showed that the overall prevalence of pneumonia among under-five children during the study period in Arba Minch General Hospital was 30% (73) (as shown in Figure 1). Among the children diagnosed with pneumonia, 21 (28.8%) had severe pneumonia and 15 (71.4%) had moderate to severe respiratory distress (as shown in Figure 2).
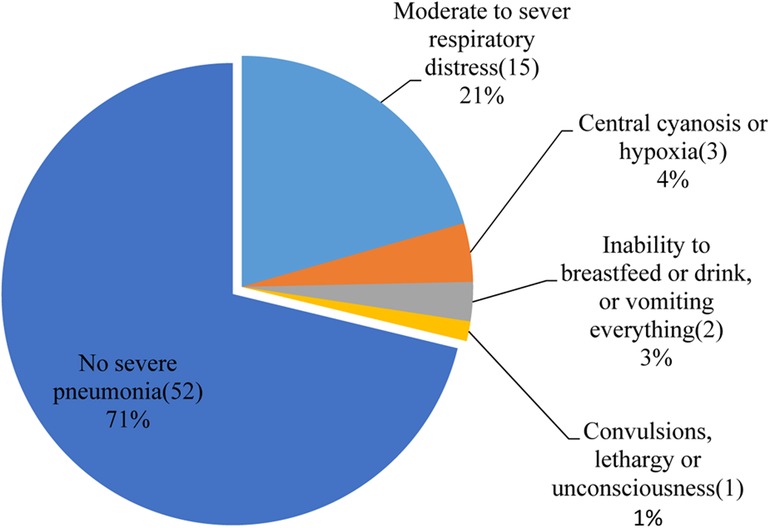
Figure 2. Severe pneumonia among under-five children visiting the Arba Minch General Hospital in 2021.
Bivariate analysis showed that cooking food inside the living room, nonexclusive breastfeeding in the first 6 months, vitamin A supplementation status, caring for child on mothers’/caregivers’ back or beside the mother during food cooking, kitchen without a window, and children's contact history of a family with acute respiratory tract infection were significantly associated with pneumonia among under-five children (shown in Table 2). Variables with a p-value of <0.25 in the bivariate analysis were candidates for multivariate analysis. Multivariate analysis showed that the kitchen not being separated from the main house for food cooking, nonexclusive breastfeeding, vitamin A supplementation status, and vaccination status of children were statistically significant factors to be considered as independent causes of pneumonia in under-five children (shown in Table 3).
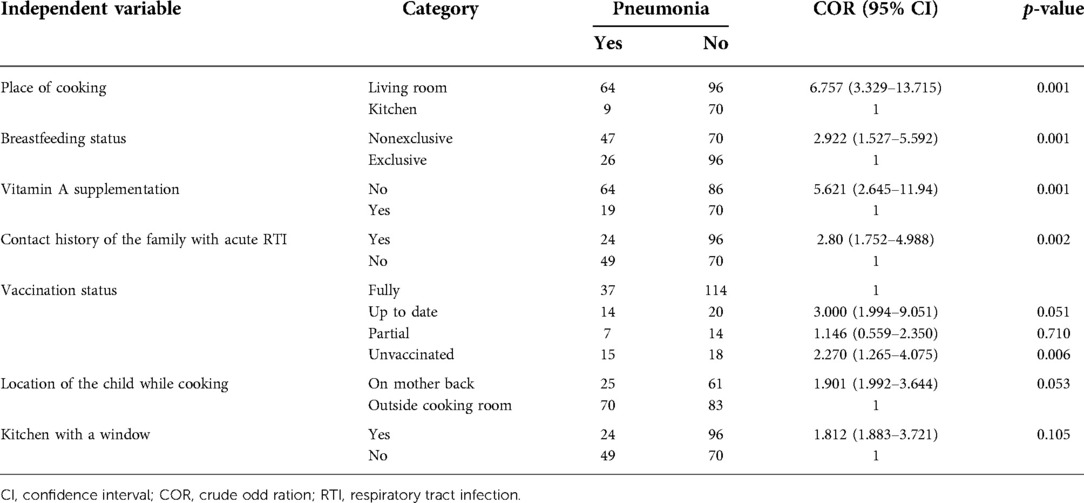
Table 2. Bivariate logistic regression analysis of independent variables and occurrence of pneumonia in under-five children in the Arba Minch General Hospital, 2021.
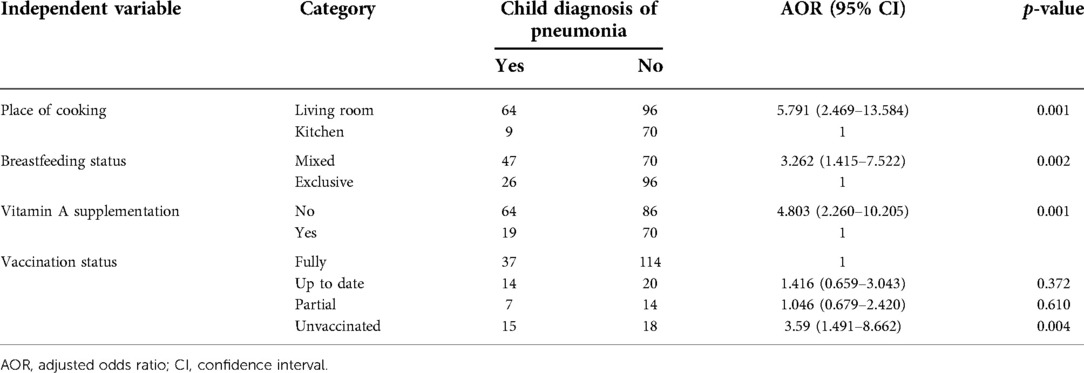
Table 3. Logistic regression analysis of independent variables and occurrence of pneumonia in under-five children in the Arba Minch General Hospital, 2021.
In this study, the kitchen not being separated from the main house for food cooking, nonexclusive breastfeeding, vitamin A supplementation status, and vaccination status of children were found to be significant risk factors associated with the occurrence of pneumonia among under-five children. This study also showed a high prevalence of pneumonia, with 30% among under-five children (as shown in Figure 1). Our finding was in agreement with a study done in other parts of Ethiopia (15, 18). However, the result of this study was greater than that of the study conducted by Merkeb and Fentahun(20.68%) (14) and lower than that of a study conducted in Uganda (53.7%) (20). This difference may be due to the study design (Merkeb and Fentahun conducted a systematic review and meta-analysis) and socioeconomic status variations and health service facility accessibility in the study area for the study in Uganda. Although the magnitude of pneumonia is reduced from time to time due to different health policies and strategies, pneumonia remains the leading cause of death in under-five children in sub-Saharan and developing countries. Utilization of effective strategies for the sustainable reduction of pneumonia in under-five children was hindered by many different factors (4). Our current study showed that under-five children from the household who used the main house for a place of cooking were 5.8 times (AOR = 5.791, 95% CI: 2.469–13.584, p = 0.001) more likely to develop pneumonia than those from the family having a separated kitchen (as shown in Table 3). Our study result was in line with other studies conducted in Wondo Genet, southern Ethiopia (15), a study conducted in Estie town Northwest Ethiopia (21), a study by Markos et al. (19), and a study conducted in central India and Dominican Republic (22, 23). The association between pneumonia and cooking environment might be due to the use of wood as a fuel produces irritants in the form of smoke. Inhalation of this smoke results in the impairment of alveolar cells and macrophages of the lung. This study indicated that unvaccinated under-five children were 3.5 times [AOR = 3.59, 95% CI: 1.491–8.662, p = 0.004] more vulnerable to suffering from pneumonia as compared to those children who completed their vaccination (as shown in Table 3). This result was supported by different studies conducted on predictors of pneumonia (14, 18, 24). This association could be due to the loss of strong enough immunity for causative agents. Concerning breastfeeding in the first 6 months of the children's age, the odds of being vulnerable to developing pneumonia was 3.3 times (AOR = 3.262, 95% CI: 1.415, 7.522, P = 0.002) more likely among children who were not exclusively breastfed as compared to those under-five children who were exclusively breastfed (Table 3). The finding was supported by Ramezani et al.’s report on the predictors of pneumonia (10) and was nearly similar to the UNICEF 2012 report on pneumonia predictors (24). This study also found that under-five children who were not supplemented by vitamin A were nearly five times (AOR = 4.803, 95% CI: 2.260–10.205, p = 0.001) more likely to suffer from pneumonia as compared to children who had vitamin A supplementation (Table 3). Studies in Rwanda also reported similar results (25). This association could be explained by the fact that vitamin A is an essential micronutrient that governs many biological processes and a deficiency of vitamin A will cause an imbalance between pro- and anti-inflammatory factors and excessive immune response (26).
Because this study was institution-based research with data gathered from a single hospital in Ethiopia, conclusions may not be easily extrapolated to patients admitted to other areas. Second, even though the cases of pneumonia were classified by physicians using 2014 WHO standard clinical and integrated management of newborn child illness, this study did not use chest x-ray, blood cultures, and other cultures to confirm pneumonia. We merely used physician's diagnosis from patient cards. Hence, this may not be as reliable as pneumonia confirmation using laboratory diagnostic methods.
This study showed that the prevalence of pneumonia was higher in Arba Minch town compared to study reports from other parts of the country. Place of food cooking, nonexclusive breastfeeding, vitamin A supplementation status, and vaccination status of children were significant factors of pneumonia among under-five children. Enhancing caregivers’/mothers’ awareness of predicted factors needed to reduce the incidence of childhood pneumonia and to increase enhanced children's quality of health.
The original contributions presented in the study are included in the article/Supplementary Material; further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by Ethics Review Committee of Paramed Health Sciences and Business College. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
YS: data curation, formal analysis, investigation, methodology, and writing—review and editing. ZK: conceptualization, resources, software, supervision, methodology, and investigation. TF: data curation, methodology, resource, software, supervision, and writing. SE: formal analysis, resource, software, supervision, and data curation. All authors contributed to the article and approved the submitted version.
All of the funding for the research was covered by the authors.
The authors thank their study participants and data collectors for their priceless cooperation.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. UNICEF, WHO. Pocket book of hospital care for children 3rd ed. Guidelines for the management of common illnesses with limited resources. Geneva 27, Switzerland: World Health Organization (2015).
2. Hogan DR, Gretchen AS, Ahmad RH, Ties B. Monitoring universal health coverage within the sustainable development goals: development and baseline data for an index of essential health services. Lancet Global Health. (2018) 6(2):152–68. doi: 10.1016/S2214-109X(17)30472-2
3. Rudan I, Tomaskovic L, Boschi-Pinto C, Campbell H. Global estimate of the incidence of clinical pneumonia among children under five years of age. Bull World Health Organ. (2004) 82(12):895–903. PMID: 15654403, PMCID: PMC2623105.15654403
4. Black RE, Cousens S, Johnson HL. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet. (2010) 375(9730):1969–87. doi: 10.1016/S0140-6736(10)60549-1
5. GBD 2019 Under-5 Mortality Collaborators, Molokhia M, Wang Y. Global, regional, and national progress towards Sustainable Development Goal 3.2 for neonatal and child health: all-cause and cause-specific mortality findings from the Global Burden of Disease Study. Lancet. (2019) 398(10303):870–905. doi: 10.1016/S0140-6736(21)01207-1
6. United Nations Inter-Agency Group for Child Mortality Estimation. Levels and trends in child mortality. New York: UNICEF (2020).
7. Chisti MJ, Tebruegge M, Vincente SL, Graham SM, Duke T. Pneumonia in severely malnourished children in developing countries—mortality risk, aetiology and validity of WHO clinical signs: a systematic review. Trop Med Int Health. (2009) 14(10):1173–89. doi: 10.1111/j.1365-3156.2009.02364.x
8. Rudan I, Tomaskovic L, Bilogla Z, Holland K, Campbell H. Epidemiology and etiology of childhood pneumonia. Bull World Health Org. (2008) 86:408–16. doi: 10.2471/BLT.07.048769
9. Roomaney RA, Pillay-van Wyk V, Awotiwon OF, Dhansay A, Groenewald P, Joubert JD, et al. Epidemiology of lower respiratory infection and pneumonia in South Africa (1997–2015): a systematic review protocol. Br Med J. (2016) 6(9):e012154. doi: 10.1136/bmjopen-2016-012154
10. Ramezani M, Aemmi SZ, Emami Moghadam Z. Factors affecting the rate of pediatric pneumonia in developing countries: a review and literature study. Int J Pediatr. (2015) 3(6.2):1173–81. doi: 10.22038/ijp.2015.6179
11. UNICEF. The state of the world's children 2014 in numbers: every child counts revealing disparities, advancing children's right. New York: United Nations Children's Fund (2014).
12. Miller NP, Amouzou A, Tafesse M, Hazel E, Legesse H, Degefie T, et al.. Integrated community case management of childhood illness in Ethiopia: implementation strength and quality of care. The American journal of tropical medicine and hygiene, 91(2), 424–34. doi: 10.4269/ajtmh.13-0751
13. Central Statistical Agency. Ethiopian mini demography and health survey report. Addis Ababa: Central Statistical Agency (2016). p. 165.
14. Merkeb AY, Fentahun A. Magnitude and predictors of pneumonia among under-five children in Ethiopia: a systematic review and meta-analysis. J Environ Public Health. (2020) 1606783. doi: 10.1155/2020/1606783
15. Teshome A. Prevalence of pneumonia and factors associated among children 2-59 months old in Wondo Genet district, Sidama zone, SNNPR, Ethiopia. Curr Pediatr Res. (2017).
16. Hailemariam S, Gebeyehu Y, Loha E, Johansson KA, Lindtjørn B. Inadequate management of pneumonia among children in South Ethiopia: findings from descriptive study. BMC Health Serv Res. (2019) 19(1):426. doi: 10.1186/s12913-019-4242-7
17. Horta BL, Victoria CG. World Health Organization. Short-term effects of breastfeeding: a systematic review on the benefits of breastfeeding on diarrhoea and pneumonia mortality. Geneva: World Health Organization. (2013). Available from: https://apps.who.int/iris/handle/10665/95585
18. Lema K, Murugan R, Tachbele E. Prevalence and associated factors of pneumonia among under-five children at public hospitals in Jimma zone, South West of Ethiopia. J Pulmonol Clin Res. (2018) 2(1):25–31.
19. Markos Y, Dadi AF, Demisse AG, Ayanaw Habitu Y, Derseh BT, Debalkie G. Determinants of under-five pneumonia at Gondar University hospital, Northwest Ethiopia: an unmatched case-control study. J Environ Public Health. (2019) 9790216. doi: 10.1155/2019/9790216
20. Nantanda R, Tumwine JK, Ndeezi G, Ostergaard MS. Asthma and pneumonia among children less than five years with acute respiratory symptoms in Mulago Hospital, Uganda: Evidence of under-diagnosis of asthma. PLoS ONE (2013) 8(11): e81562. doi: 10.1371/journal.pone.0081562
21. Fekadu GA, Terefe MW, Alemie GA. Prevalence of pneumonia among under-five children in Este Town and the surrounding rural Kebeles, Northwest Ethiopia: a community based cross sectional study. Sci J Public Health. (2014) 2(3):150–5. doi: 10.11648/j.sjph.20140203.12
22. Taksande AM, Yeole M. Risk factors of acute respiratory infection in under-five in a rural hospital of central India. J Pediatr Neonatal Ind Med. (2016) 5(1):e050105. doi: 10.7363/050105
23. Bautista LE, Correa A, Baumgartner J, Breysse P, Matanoski GM. Indoor charcoal smoke and acute respiratory infections in young children in the Dominica Republic. Am J Epidemiol. (2008) 169:572–80. doi: 10.1093/aje/kwn372
24. UNICEF, WHO. Pneumonia and diarrhoea. In: Tackling the deadliest diseases for the world’s poorest children. New York: United Nations Children's Fund (2012).
25. Cancedda C, Coot P, Shema J. Health professional training and capacity strengthening through international academic partnership: the first five years of the human resources for health program in Rwanda. Int J Health Policy Manag. (2018) 7(11):1024–39. doi: 10.15171/ijhpm.2018.61
Keywords: pneumonia, childhood illness, Arba Minch, Gamo, under-five
Citation: Solomon Y, Kofole Z, Fantaye T and Ejigu S (2022) Prevalence of pneumonia and its determinant factors among under-five children in Gamo Zone, southern Ethiopia, 2021. Front. Pediatr. 10:1017386. doi: 10.3389/fped.2022.1017386
Received: 11 August 2022; Accepted: 17 November 2022;
Published: 22 December 2022.
Edited by:
Gönül Tanır Dr Sami Ulus Child Health and Diseases Training and Research Hospital, TurkeyReviewed by:
Mohammed Ahmed Haramaya University, Ethiopia© 2022 Solomon, Kofole, Fantaye and Ejigu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yerukneh Solomon eWVydWtuZXNvbG9tb25AZ21haWwuY29t
Specialty Section: This article was submitted to Pediatric Infectious Diseases, a section of the journal Frontiers in Pediatrics
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.