- 1Division of Neonatology, Paediatric Intensive Care & Neuropaediatrics, Department of Paediatrics and Adolescent Medicine, Comprehensive Center for Paediatrics, Medical University of Vienna, Vienna, Austria
- 2Division of Neonatology, Department of Paediatrics and Adolescent Medicine, Medical University of Graz, Graz, Austria
Introduction
The increasing number of publications regarding neonatal lung ultrasound and its use will have a positive impact on the clinical care for our small patients, since lung ultrasound—as a point-of-care ultrasound (POCUS) exam—has proved its worth as a safe, quick, and reliable diagnostic tool (1). However, there is an ongoing discussion on who should perform ultrasound exams in which situations. We read with great interest the recent review article by Nestaas, who accomplished to thoroughly summarize the main aspects of neonatologist performed echocardiography (NPE) in the newborn (2), a term that was firstly introduced in 2016 by the European Society for Paediatric Research (ESPR) and the European Society for Neonatology (ESN) (3). On the other hand, we followed the discussion that evolved around Andronikou et al. and van Rijn et al. after expressing their concerns regarding non-radiologist POCUS, a term that we will also use in this statement (4–7).
Neonatal lung ultrasound
In recent years, more and more literature focused on the application of ultrasound for specific patient groups, interventions, or clinical problems. In the pediatric field, neonatal lung ultrasound has been one of the most thoroughly studied applications in the last several years and as a result, it is now included in a recently published POCUS guideline issued by the European Society of Paediatric and Neonatal Intensive Care (ESPNIC) (8).
Neonatal lung ultrasound has not only been proven to be safe and relatively easy to learn, but by now enables us to guide and refine our therapies. In particular, evidence shows that many of the main reasons for respiratory distress in the newborn, including pneumothorax, pleural effusion, respiratory distress syndrome, transient tachypnoea of the newborn, pneumonia and atelectasis can be diagnosed by lung ultrasound (1, 9, 10). Another prominent application is the use of a lung ultrasound score, a semiquantitative method to assess the neonatal lung (11). Based on this score, strong evidence allows us to identify infants who need surfactant, or even a second dose of surfactant (11, 12), infants who are very likely to develop bronchopulmonary dysplasia (13), or infants who suffer from lung edema after cardiac surgery (14). In our opinion, these insights are not only highly relevant for the clinician, but they also have an immediate clinical consequence and are therefore primarily performed by the attending neonatologist. The direct positive impact of these applications reflects what makes POCUS so powerful in clinical practice.
NPLUS—neonatologist performed lung ultrasound
Based on these developments and discussions, we would like to submit a proposal concerning the terminology of the lung ultrasound examination in newborn patients. In accordance with the well-established term NPE, we changed the terminology in our units to “Neonatologist Performed Lung Ultrasound” (NPLUS). This abbreviation, which was first introduced in one of our most recent publications, allows for a proper classification of the investigation (10). The term NPLUS emphasizes the functional and integrative character of the examination as a POCUS technique, as it is performed at the bedside by the involved neonatologist, who interprets the results in consideration of the patient's clinical condition.
Some authors, including Lichtenstein, who invented the concept of lung ultrasound and is recognized as the “father” of lung ultrasound, argued that the abbreviation LUS should only be used for “lung ultrasound score”, and the abbreviation LU should be used for “lung ultrasound” (12, 15, 16). However, use of LU and LUS appears to be inconsistent among dozens of publications, which again demonstrates the need for a discussion regarding the nomenclature by special interest groups and scientific societies.
In our opinion, the term NPLUS (or alternatively NPLU) helps differentiate a lung POCUS examination from a possibly more standardized and thorough assessment of the lung performed by a radiologist. This terminology may be extended to further applications of neonatologist performed ultrasound (abdominal, cranial, spinal ultrasound) allowing for a harmonization of ultrasound terminology and communication in neonatology (see Figure 1). The introduction of consistent terminology facilitates the difficult but inevitable process of standardization.
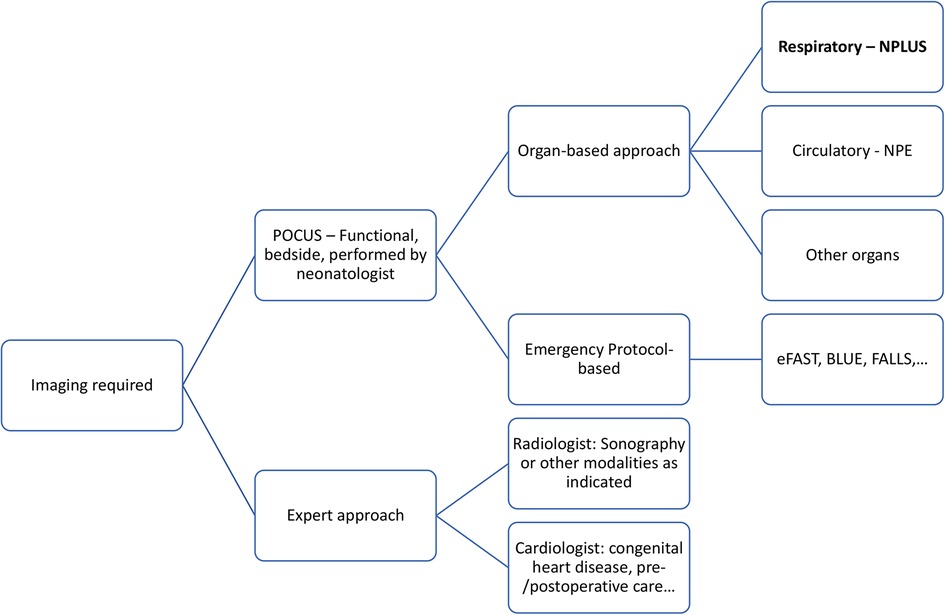
Figure 1. Decision tree for sonographic imaging of neonates. Two approaches (POCUS and expert approach) are further investigated. At the bedside, POCUS may provide quick answers regarding specific, organ-related questions by scanning the corresponding region or by application of an emergency protocol (e.g., respiratory insufficiency, intracranial haemorrhage, cardiac tamponade). In analogy to NPLUS and NPE, other organ-based exams might follow this nomenclature. Expert approach allows for a more thorough and sophisticated diagnostic evaluation, but might be more time-consuming and depends on the availability of skills and resources.
Discussion
The introduced distinction might calm down the discussion about who should perform lung ultrasound and who should not. It is of particular importance for the clinician in pediatrics to appreciate the value of expert radiologists and acknowledge the limitations of non-radiologist ultrasonography in order to avoid errors whenever possible, and subsequently provide the best care for our patients. We could not agree more with the main points of Arthurs et al., who emphasize the importance of experience, training, and establishment of a learning environment to increase the quality of ultrasound examinations (7).
The increasing use of lung ultrasound was initiated primarily by intensivists, leading to a majority of publications in pediatric journals. As Tomà states in his 2020 review, “fewer than 10% of the articles on lung ultrasonography, in the last 10 years, have been published in radiologic journals” (17). Of course, the possible differences in peer-review processes between radiologic and pediatric journals are obvious and must not be ignored. However, both radiologists and pediatricians acknowledge the need for standardized training and guidelines (18–20).
Concerns regarding non-radiologist POCUS were raised as soon as medical specialties recognized the potential of ultrasound (US) for different applications, most prominently seen in adult emergency care, but later also in pediatrics and other fields, possibly “undermining the role of the radiologist” (4, 21). However, we believe that both neonatologist- and radiologist performed ultrasound contribute to the care of our small patients, while each approach has various strengths and limitations in different situations, as the previous authors who are mentioned above correctly stated.
Furthermore, in our experience, POCUS training is often provided without radiologists being involved. Hence, special attention on understanding the limitations of non-radiologist POCUS or—maybe even more important –training programs held jointly involving radiologists and various clinical specialists seem crucial.
We do recognize that a standardization of the term should be discussed and implemented by a joint discussion led by scientific societies. Two recent publications in this field can be considered as examples for such joint efforts, namely the “International evidence-based recommendations for point-of-care lung ultrasound” by the International Liaison Committee on Lung Ultrasound (ILC-LUS) and the “International evidence-based guidelines on Point of Care Ultrasound (POCUS) for critically ill neonates and children” issued by the POCUS Working Group of the European Society of Paediatric and Neonatal Intensive Care (ESPNIC) (8, 9). In our opinion, the latter organization can serve as a suitable forum to come to a decision in this matter. From a radiological standpoint, however, the European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB), which regularly publishes guidelines and recommendations, also offers a platform for joint sessions and discussions regarding innovations in sonography, hence there might be a significant participation by the organization in the discussion evolving around this proposal (22). Lastly, the P2Network published consensus papers regarding application and training in Pediatric Emergency Medicine Ultrasound and is a platform of clinical experts in POCUS (23).
We would endorse a harmonization of the terminology by establishing “NPLUS” in research papers in this field.
Author contributions
LA: drafted and revised the manuscript; EK and BS: critically revised the manuscript, added important intellectual content and approved of the final version to be published. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Raimondi F, Yousef N, Migliaro F, Capasso L, De Luca D. Point-of-care lung ultrasound in neonatology: classification into descriptive and functional applications. Pediatr Res. (2021) 90:524–31. doi: 10.1038/s41390-018-0114-9
2. Nestaas E. Neonatologist performed echocardiography for evaluating the newborn infant. Front Pediatr. (2022) 10:853205. doi: 10.3389/fped.2022.853205
3. Groves AM, Singh Y, Dempsey E, Molnar Z, Austin T, El-Khuffash A, et al. Introduction to neonatologist-performed echocardiography. Pediatr Res. (2018) 84:1–12. doi: 10.1038/s41390-018-0076-y
4. Van Rijn RR, Stafrace S, Arthurs OJ, Rosendahl K. Non-radiologist-performed point-of-care ultrasonography in paediatrics — european society of paediatric radiology position paper. Pediatr Radiol. (2021) 51:161–7. doi: 10.1007/s00247-020-04843-6
5. Györgyi Z, de Luca D, Singh Y. The European society of paediatric Radiology's Position statement on point-of-care ultrasound. Pediatr Radiol. (2022) 52:608–9. doi: 10.1007/s00247-021-05184-8
6. Andronikou S, Otero HJ, Belard S, Heuvelings CC, Ruby LC, Grobusch MP. Radiologists should support non-radiologist point-of-care ultrasonography in children: a case for involvement and collaboration. Pediatr Radiol. (2022) 52:604–7. doi: 10.1007/s00247-021-05185-7
7. Arthurs OJ, van Rijn RR, Stafrace S, Rosendahl K. Point-of-care ultrasound: reply to andronikou et al. And györgyi et al. Pediatr Radiol. (2022) 52:610–1. doi: 10.1007/s00247-021-05183-9
8. Singh Y, Tissot C, Fraga MV, Yousef N, Cortes RG, Lopez J, et al. International evidence-based guidelines on point of care ultrasound (POCUS) for critically ill neonates and children issued by the POCUS working group of the European society of paediatric and neonatal intensive care (ESPNIC). Crit Care. (2020) 24:65. doi: 10.1186/s13054-020-2787-9
9. International Liaison Committee on Lung Ultrasound (ILC-LUS) for the International Consensus Conference on Lung Ultrasound (ICC-LUS), Volpicelli G, Elbarbary M, Blaivas M, Lichtenstein DA, Mathis G, et al. International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. (2012) 38:577–91. doi: 10.1007/s00134-012-2513-4
10. Aichhorn L, Küng E, Habrina L, Werther T, Berger A, Urlesberger B, et al. The role of lung ultrasound in the management of the critically ill neonate—a narrative review and practical guide. Children. (2021) 8:628. doi: 10.3390/children8080628
11. Brat R, Yousef N, Klifa R, Reynaud S, Shankar Aguilera S, De Luca D. Lung ultrasonography score to evaluate oxygenation and surfactant need in neonates treated with continuous positive airway pressure. JAMA Pediatr. (2015) 169:e151797. doi: 10.1001/jamapediatrics.2015.1797
12. Raimondi F, Migliaro F, Corsini I, Meneghin F, Pierri L, Salomè S, et al. Neonatal lung ultrasound and surfactant administration. Chest. (2021) 160:2178–86. doi: 10.1016/j.chest.2021.06.076
13. Alonso-Ojembarrena A, Serna-Guerediaga I, Aldecoa-Bilbao V, Gregorio-Hernández R, Alonso-Quintela P, Concheiro-Guisán A, et al. The predictive value of lung ultrasound scores in developing bronchopulmonary dysplasia. Chest. (2021) 160:1006–16. doi: 10.1016/j.chest.2021.02.066
14. Girona-Alarcón M, Cuaresma-González A, Rodríguez-Fanjul J, Bobillo-Perez S, Inarejos E, Sánchez-de-Toledo J, et al. LUCAS (Lung ultrasonography in cardiac surgery) score to monitor pulmonary edema after congenital cardiac surgery in children. J Matern Fetal Neonatal Med. (2022) 35:1213–8. doi: 10.1080/14767058.2020.1743660
15. Lichtenstein DA. Current misconceptions in lung ultrasound. Chest. (2019) 156:21–5. doi: 10.1016/j.chest.2019.02.332
16. Rouby J-J, Arbelot C, Gao Y, Zhang M, Lv J, An Y, et al. Training for lung ultrasound score measurement in critically ill patients. Am J Respir Crit Care Med. (2018) 198:398–401. doi: 10.1164/rccm.201802-0227LE
17. Tomà P. Lung ultrasound in pediatric radiology—cons. Pediatr Radiol. (2020) 50:314–20. doi: 10.1007/s00247-019-04524-z
18. Pervaiz F, Hossen S, Chavez MA, Miele CH, Moulton LH, McCollum ED, et al. Training and standardization of general practitioners in the use of lung ultrasound for the diagnosis of pediatric pneumonia. Pediatr Pulmonol. (2019) 54:1753–9. doi: 10.1002/ppul.24477
19. Elsayed Y, Abdelmawla M, Narvey M, Wrogemann J. A model of integrated lung and focused heart ultrasound as a new screening examination in infants at risk of respiratory or hemodynamic compromise. J Pediatr Neonatal Individ Med. (2017) 6:e060131. doi: 10.7363/060131
20. Marini TJ, Rubens DJ, Zhao YT, Weis J, O’Connor TP, Novak WH, et al. Lung ultrasound: the essentials. Radiol Cardiothorac Imaging. (2021) 3:e200564. doi: 10.1148/ryct.2021200564
21. ESR Executive Council 2009, European Society of Radiology. ESR Position paper on ultrasound. Insights Imaging. (2010) 1:27–9. doi: 10.1007/s13244-009-0005-z
22. Dietrich CF, Rudd L, Saftiou A, Gilja OH. The EFSUMB website, a great source for ultrasound information and education. Med Ultrason. (2017) 19:102. doi: 10.11152/mu-938
Keywords: lung ultrasound, POCUS, neonatology, neonatologist performed lung ultrasound, NPE
Citation: Aichhorn L, Küng E and Schwaberger B (2023) Neonatologist performed lung ultrasound: NPLUS—proposal for a consistent ultrasound terminology. Front. Pediatr. 10:1007672. doi: 10.3389/fped.2022.1007672
Received: 30 July 2022; Accepted: 20 December 2022;
Published: 14 February 2023.
Edited by:
Minesh Khashu, University Hospitals Dorset NHS Foundation Trust, United KingdomReviewed by:
Shivani Shankar Aguilera, Assistance Publique Hopitaux De Paris, FranceMahmoud Montasser, Wishaw General Hospital, United Kingdom
© 2023 Aichhorn, Küng and Schwaberger. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lukas Aichhorn lukas.aichhorn@meduniwien.ac.at
Specialty Section: This article was submitted to Neonatology, a section of the journal Frontiers in Pediatrics
 Lukas Aichhorn
Lukas Aichhorn