
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr. , 04 January 2022
Sec. Pediatric Gastroenterology, Hepatology and Nutrition
Volume 9 - 2021 | https://doi.org/10.3389/fped.2021.810173
 Jae Young Choe1,2†
Jae Young Choe1,2† Sujin Choi1†
Sujin Choi1† Ki Hwan Song3
Ki Hwan Song3 Hyo-Jeong Jang4
Hyo-Jeong Jang4 Kwang-Hae Choi5
Kwang-Hae Choi5 Dae Yong Yi6
Dae Yong Yi6 Suk Jin Hong7
Suk Jin Hong7 Jun Hyun Hwang8
Jun Hyun Hwang8 Seung-Man Cho9
Seung-Man Cho9 Young Jin Kim10
Young Jin Kim10 Byung-Ho Choe1
Byung-Ho Choe1 Ben Kang1* on behalf of the Crohn's and Colitis Association in Daegu-Gyeongbuk (CCAiD)
Ben Kang1* on behalf of the Crohn's and Colitis Association in Daegu-Gyeongbuk (CCAiD)Background and Aim: There is paucity of data regarding the epidemiology of pediatric IBD in Asia compared to that of Western countries. We aimed to investigate the incidence and prevalence trends of pediatric inflammatory bowel disease (IBD) in the Daegu-Kyungpook province of South Korea from 2017 to 2020.
Methods: This study was a multicenter, retrospective study conducted in eight IBD referral centers located in the Daegu-Kyungpook province. Children and adolescents of ≤18 years who were initially diagnosed with IBD between 2017 and 2020 were included. The annual number of children and adolescents newly diagnosed with IBD and the annual resident population of children and adolescents ≤18 years of age in the Daegu-Kyungpook province were investigated to calculate the annual incidence and prevalence in the region.
Results: A total 304 children and adolescents that had been diagnosed with IBD were included in this study. Among these patients, 71.4% had been diagnosed with Crohn's disease (CD), and 28.6% with ulcerative colitis (UC). The population based annual incidences of IBD from 2017 to 2020 were each 7.24, 6.82, 10.27, and 13.33 per 100,000, respectively (P for trend <0.001), 4.48, 5.26, 7.39, and 9.8 per 100,000, respectively, for CD (P for trend <0.001), and 2.76, 1.56, 2.88, and 3.53 per 100,000, respectively, for UC (P for trend = 0.174).
Conclusion: Pediatric IBD, especially CD has significantly increased recently in the Daegu-Kyungpook province. Epidemiology studies from other regions of Asia are required to better elucidate this trend of increase in Asia.
The prevalence and incidence of pediatric inflammatory bowel disease (IBD) have increased rapidly worldwide over the past two decades. As the pathophysiology of IBD is yet to be elucidated, it is important to understand the epidemiology of IBD to understand the genetic and environmental factors (1). While the incidence of adult IBD is stagnant in some Western countries, the incidence in Asian countries, such as Japan, Korea and Singapore, is still on a rise (2–5). This difference in incidence trends between countries according to geographical location in adults has also been observed in children with IBD (6–8).
Various changes have occurred in the incidence trends of pediatric diseases due to the recent coronavirus infectious disease 2019 (COVID-19) pandemic. The increase of childhood obesity and decrease of infection-related systemic diseases is associated with compliance with the quarantine rules and changes in living patterns including increased activities at home (9–12).
In this study, we aimed to investigate the incidence and prevalence trends of pediatric IBD from 2017 to 2020 in the Daegu-Kyungpook province of South Korea.
This study was a multicenter, retrospective study conducted in eight IBD referral centers located in the Daegu-Kyungpook province: Kyungpook National University Children's Hospital affiliated with Kyungpook National University Chilgok Hospital, Keimyung University Dongsan Medical Center, Yeungnam University Medical Center, Kyungpook National University Hospital, Daegu Catholic University Medical Center, Dongguk University Gyeongju Hospital, Koo Hospital, and Daegu Fatima Hospital. These eight centers are the only pediatric IBD referral centers in the Daegu-Kyungpook province (Figure 1). Children and adolescents of ≤18 years who were initially diagnosed with IBD between January 1, 2017 and December 31, 2020 were included.
Baseline demographics including gender, birth date, diagnosis date, diagnosis age, and type of IBD were retrieved from electronic medical charts by searching for diagnosis codes of 555.X and K50.XX for CD and 556.X and K51.XX for UC according to the ICD-9 and ICD-10 codes, respectively. Patients residing outside the Daegu-Kyungpook province at diagnosis were excluded from the incidence analysis, and those who had moved outside the Daegu-Kyungpook province were excluded from the next particular year of the prevalence analysis.
The annual number of children and adolescents newly diagnosed with IBD at the centers and the annual resident population of children and adolescents ≤18 years in the Daegu-Kyungpook province were investigated to calculate the population based annual incidence and prevalence of pediatric IBD in the region. By utilizing data from the Statistics Korea which is a government organization for statistics under the Ministry of Economy and Finance, the population based per 100,000 incidence and prevalence of IBD, Crohn's disease (CD), and ulcerative colitis (UC) were each calculated, respectively.
In addition, annual trends were analyzed according to the type of disease, gender, and age groups according to the Paris classification (13). Comparison of demographic factors was also conducted between patients diagnosed in the pre-COVID-19 (2017–2019) and the post-COVID-19 era (2020).
For statistical comparison between two groups, chi square test or Fisher's exact test was used for categorical variables, while Student's t-test were used for statistical comparison of continuous variables. Comparative data for continuous variables are expressed as medians with interquartile range (IQR) or means with standard deviation (SD). To test the statistical significance of the fluctuations of annual incidence, 95% confidence intervals (CIs) calculated by the Clopper-Pearson method (14) for incidence were compared among years. The Cochran-Armitage test was used to evaluate the incidence trend of IBD. Data were considered to be statistically significantly different if P < 0.05. Statistical analyses were conducted using R version 3.2.3 (http://www.r-project.org).
This study was conducted with approval from the Institutional Review Board (IRB) of Daegu Joint (IRB No. 2021-02-023), and informed consent was waived due to the retrospective nature of the study. We conducted this study in compliance with the principles of the Declaration of Helsinki.
A total of 304 incidence cases and 1,065 prevalence cases were analyzed in this study. Of the 304 incidence cases, 217 were diagnosed with CD (71.4%) and 87 were diagnosed with UC (28.6%). The mean ratio of CD to UC was 2.5:1. There were 150 males, and 67 females for CD, and 59 males and 28 females for UC. The ratio of male to female was 2.2:1. The mean ± SD age at diagnosis was 14.6 ± 3.4 for CD and 15.3 ± 4.1 for UC.
Annual incidences of IBD from 2017 to 2020 were each 63, 57, 82, and 102, respectively. Annual incidences of CD from 2017 to 2020 were each 39, 44, 59, and 75, respectively, while that of UC were each 24, 13, 23, and 27, respectively. Comparison of demographic factors between years are shown in Table 1. The annual number of newly diagnosed cases divided according to the Paris classification age is shown in Table 2.
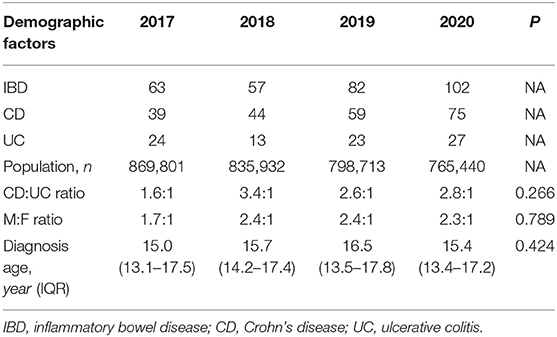
Table 1. Annual newly diagnosed cases, population, and comparison of demographic factors between years.
Comparison was conducted between patients diagnosed in the pre-COVID-19 (2017–2019) and the post-COVID-19 era (2020). Comparison of demographic factors are shown in Table 3.
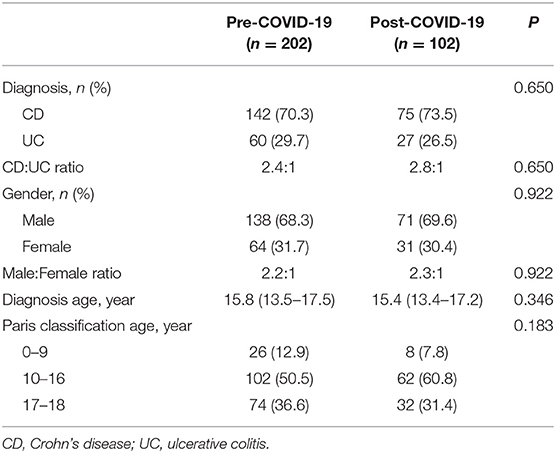
Table 3. Comparison of demographic factors between patients diagnosed in the pre- and post-COVID-19 era.
Compared to the pre-COVID-19 era, increases of incidences in the post-COVID-19 era for both pediatric CD and UC were observed only in the age group of 10–16 years (Figure 2). Although a statistical significance was not observed, the proportion of patients 10–16 years had increased from 50.5% in 2019 to 60.8% in 2020 among IBD patients (P = 0.183). The proportion of patients in the age group of 10–16 years had increased from 56.3% in 2019 to 64.0% in 2020 among patients diagnosed with CD (P = 0.243). The proportion of patients in the age group of 10–16 years had also increased from 36.7% in 2019 to 51.9% in 2020 among patients diagnosed with UC (P = 0.352).
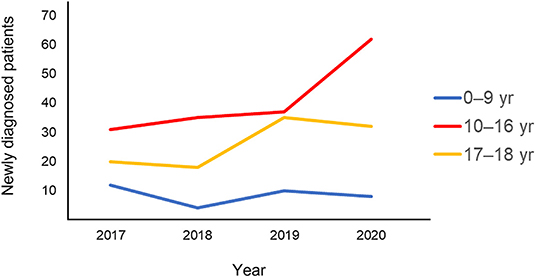
Figure 2. Annual changes in pediatric IBD, CD, and UC incidence according to age. IBD, inflammatory bowel disease; CD, Crohn's disease; UC, ulcerative colitis.
The population based annual incidences of IBD from 2017 to 2020 were each 7.24, 6.82, 10.27, and 13.33 per 100,000, respectively (P for trend <0.001). The population based annual incidences of CD from 2017 to 2020 were each 4.48, 5.26, 7.39, and 9.8 per 100,000, respectively (P for trend <0.001). The population based annual incidences of UC from 2017 to 2020 were each 2.76, 1.56, 2.88, and 3.53 per 100,000, respectively (P for trend = 0.174) (Figure 3). Pediatric CD showed a continuous increase from 4.48 (95%, CI, 3.19–6.13) per 100,000 in 2017 to 9.8 (7.71–12.28) per 100,000 in 2020, but pediatric UC showed a temporary decrease to 1.56 (95%, CI, 1.83–4.32) in 2018, followed by a continuous increase to 3.53 (95%, CI, 2.32–5.13) in 2020 (Figure 4; Table 4).
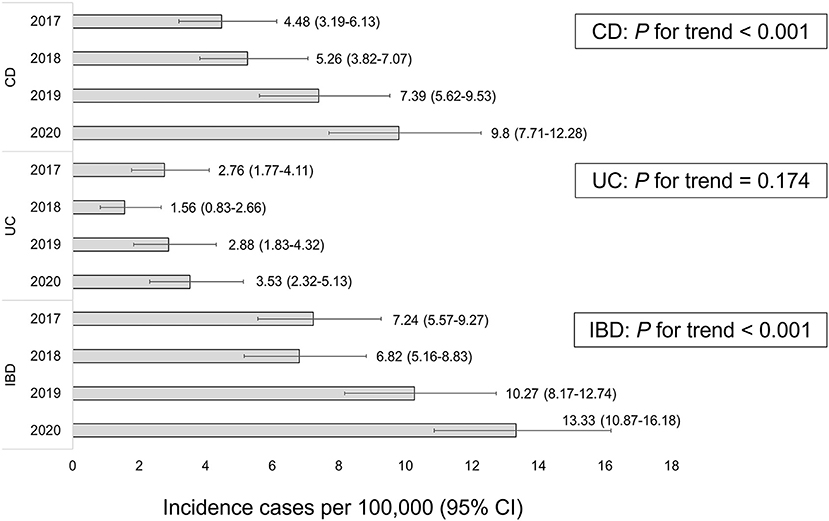
Figure 3. Population based incidence of pediatric CD, UC, and IBD per year. CD, Crohn's disease; UC, ulcerative colitis; IBD, inflammatory bowel disease.
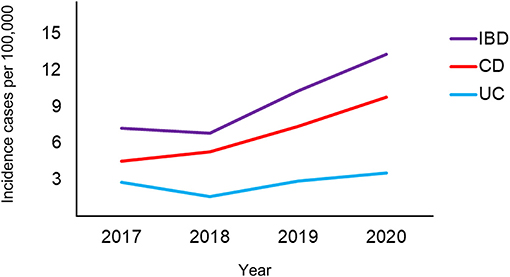
Figure 4. Annual changes in the population based incidence of pediatric IBD, CD, and UC. IBD, inflammatory bowel disease; CD, Crohn's disease; UC, ulcerative colitis.
The prevalence of pediatric IBD from 2017 to 2020 showed a steady increase, which was 28.3, 29.9, 32.8 and 40.1 per 100,000 each year respectively in the Daegu-Kyungpook province. The prevalence of pediatric CD was 21.4, 23.0, 25.5, and 30.8 per 100,000, while the prevalence of pediatric UC was 6.9, 6.9, 6.9, and 9.3 per 100,000 each year, respectively, from 2017 to 2020.
In this study, we identified a significant increase in the incidence and prevalence of pediatric IBD, CD, and UC, respectively, in the Daegu-Kyungpook province of South Korea from 2017 to 2020.
The metropolitan city of Daegu is the fourth largest city in Korea located in the southeast with a population of ~2.5 million (Figure 1). The combined population of Daegu-Kyungpook province accounts for 9.8% of the total Korean population as of 2020, and 15.1% of the total population of children under the age of 18 (15). Seven centers participating in this study are located in Daegu, while one center is located in the city of Gyeongju of Kyungpook province. These eight centers are the only referral centers capable of care for pediatric IBD patients in the Daegu-Kyungpook province. Therefore, it is likely that the incidence and prevalence in this study represents that of the general population in this age group in the region.
Unlike the plateau in pediatric IBD incidence in Western countries, the incidence of pediatric IBD is on a sharp rise in Asia (6, 8, 16). According to a recent systematic review, the incidence of IBD, CD, and UC were each 0.5–11.4, 0.3–3.7, and 0.2–3.9 per 100,000 person-years, respectively, from 1968 to 2012 (8). However, when compared to the adult data on IBD epidemiology, there are still very few studies from Asian countries with relatively high population such as China, India, and Central Asia (17–20). Owing to the limited data regarding pediatric IBD epidemiology in Asia, this study may be an important piece of the puzzle to define the epidemiology of pediatric IBD in the region.
CD to UC ratio may vary according to factors such as age, region, and also over time (2, 21). In a study conducted in Japan, pediatric UC dominated pediatric CD (22). Meanwhile, a study conducted in Singapore showed a CD dominance over UC in the pediatric age group, which is comparable of the results in this study (23). Globally, CD predominates over UC in regions of high IBD incidence (8). Recent data have shown higher rates of pediatric CD than UC in Europe and North America (8). Meanwhile, similar to the ratio of Japan, UC incidence is higher than that of CD in northern California, Finland, and Italy (24–26). The reason for these differences between regions is yet to be elucidated.
In our previous study that investigated the incidence of pediatric IBD from 2011 to 2016 in the Daegu-Kyungpook province, mean pediatric CD to UC ratio was 4.1:1 (27). However, in this study, mean pediatric CD to UC ratio was reduced to 2.5:1. Compared to our previous study, the annual number of pediatric CD cases increased 3.3-fold, while the number of pediatric UC cases showed a sharp increase of 5.4-fold. Thus, the relatively higher increase rate in pediatric UC cases compared to CD cases may have contributed to this result.
Several studies have reported that the age at diagnosis of IBD is decreasing with time (28–32). A recent study conducted in Israel showed that there was an average decrease in age at diagnosis from 15.0 ± 2.8 in 2002–2008 to 14.3 ± 3.1 in 2009–2016 (P < 0.001). Although we were unable to identify such statistically significant difference due to the short study period, we were able to observe that the median diagnosis age in 2020 had decreased compared to 2019. The decrease in diagnosis age may hypothetically result from the change in disease biology, known as the concept of genetic anticipation (30). Although genetic anticipation is well-established in some monogenic disorders, there are controversies regarding its relevance to polygenic disorders, such as IBD (30).
Although a statically significant increase was not identified compared to the pre-COVID-19 era, the highest annual incidences for pediatric IBD, CD and UC in this study were all observed in the post-COVID-19 era of 2020. Although there have been studies investigating the changes incidence of other diseases or health conditions (9–12), no study in Asia has yet investigated the change of incidence in pediatric IBD patients after the COVID-19 pandemic. This study is the first in Asia to investigate the incidence in the pediatric population of IBD after the COVID-19 pandemic.
The increase of pediatric IBD incidence in the Daegu-Kyungpook province in the post-COVID-19 era may be attributable to several reasons. First, the increase may be merely on the same line of a continuous increase of pediatric IBD in Korea. The increase of pediatric IBD has been reported worldwide, especially in Asian countries (6, 19, 22, 23, 31). There have also been studies on the recent rapid increase in pediatric IBD incidence in Korea (27, 32, 33). Pediatric IBD incidences as high as 14.3–18.3 per 100,000 have been reported in regions from Western countries (34–38). Although the incidence of IBD remains highest in the northern populations of Europe and America, it has remained stable or even decreased (8). To our knowledge, the pediatric IBD incidence of 13.3 per 100,000 as of 2020 in this study is the highest in Asia, and shows that the incidence in the Daegu-Kyungpook province has nearly reached that of the highest regions in the world.
Second, the relative increase of pediatric IBD incidence I n the Daegu-Kyungpook province may be a result of a sharp decrease in the number of children in the region. During the study period, the total population in Daegu-Kyungpook province decreased by 1.1% from 5,133,000 to 5,074,000, while the number of children under the age of 18 decreased by 12.0% from 869,801 to 765,440 (14). As of 2020, Korea has the lowest birth rate in the world with a total fertility rate of 0.84 (39). The birth rate in Daegu-Kyungpook province is also continuously decreasing.
Third, the change in lifestyle in the post-COVID-19 era may have influenced this increase. The COVID-19 pandemic has led to increased time spent at home and reduced physical activity, which has caused an increase in childhood obesity (9). In addition, the increased time spent at home and the explosion of food delivery services have increased the frequency of exposure to processed food instead of homemade food. This change in eating habits and activity may have led to an increase of exposure to environmental risk factors. Changes in diet and consequent alteration in the composition of the intestinal microbiota may be associated with the increasing incidence of pediatric IBD (40).
There are some limitations of this study, and therefore results of this study should be interpretated with caution. First, this study was conducted in a particular region in Korea, and therefore the results may not represent that of the whole country. Second, there is a possibility that some pediatric IBD patients in the region follow up to centers outside the region. Therefore, there is a possibility that these patients were excluded from this analysis. However, because most patients are initially diagnosed at centers located at the administrative district of residence, we believe the number of these patients are extremely small to influence the results of this study. Third, 4 years may be rather short for investigating the incidence trend in a particular region. Fourth, we were unable to investigate the incidence of IBD-unclassified (IBD-U) due to the lack of a diagnostic code for IBD-U on ICD-9 and ICD-10. Last but not least, this study was a retrospective study.
In conclusion, we identified a significant increase in the incidence and prevalence of pediatric IBD in the Daegu-Kyungpook province of South Korea from 2017 to 2020. Unlike the decrease in pediatric infectious diseases or pediatric infection-related systemic diseases in the post-COVID-19 era, pediatric IBD has significantly increased in the Daegu-Kyungpook province. Epidemiology studies from other regions are required to better identify whether the COVID-19 pandemic has influenced pediatric IBD incidence or not.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Institutional Review Board (IRB) of Daegu Joint (IRB No. 2021-02-023). Written informed consent from the participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
JC, SC, H-JJ, SH, and S-MC contributed in the acquisition, analysis and interpretation of data, and drafting of the initial manuscript. KS, K-HC, DY, JH, YK, and B-HC contributed in the acquisition, analysis and interpretation of data, and critical revision for important intellectual content. BK contributed in the conception of the study, acquisition, analysis and interpretation of data, drafting of the initial manuscript, and critical revision for important intellectual content. All authors approved the final version of the manuscript and agreed to be accountable for all aspects of the work.
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (No. 2021R1A2C1011004).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Aniwan S, Park SH, Loftus EV. Epidemiology, natural history, and risk stratification of Crohn's disease. Gastroenterol Clin North Am. (2017) 46:463–80. doi: 10.1016/j.gtc.2017.05.003
2. Kaplan GG, Windsor JW. The four epidemiological stages in the global evolution of inflammatory bowel disease. Nat Rev Gastroenterol Hepatol. (2021) 18:56–66. doi: 10.1038/s41575-020-00360-x
3. Ng SC, Shi HY, Hamidi N, Underwood FE, Tang W, Benchimol EI, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. (2017) 390:2769–78. doi: 10.1016/S0140-6736(17)32448-0
4. Park SH, Kim YJ, Rhee KH, Kim YH, Hong SN, Kim KH, et al. A 30-year trend analysis in the epidemiology of inflammatory bowel disease in the Songpa-Kangdong District of Seoul, Korea in 1986–2015. J Crohns Colitis. (2019) 13:1410–7. doi: 10.1093/ecco-jcc/jjz081
5. Piovani D, Danese S, Peyrin-Biroulet L, Bonovas S. Inflammatory bowel disease: estimates from the global burden of disease 2017 study. Aliment Pharmacol Ther. (2020) 51:261–70. doi: 10.1111/apt.15542
6. Huang JG, Aw MM. Pediatric inflammatory bowel disease in Asia: epidemiology and natural history. Pediatr Neonatol. (2020) 61:263–71. doi: 10.1016/j.pedneo.2019.12.008
7. Roberts SE, Thorne K, Thapar N, Broekaert I, Benninga MA, Dolinsek J, et al. A systematic review and meta-analysis of paediatric inflammatory bowel disease incidence and prevalence across Europe. J Crohns Colitis. (2020) 14:1119–48. doi: 10.1093/ecco-jcc/jjaa037
8. Sýkora J, Pomahačová R, Kreslová M, Cvalínová D, Štych P, Schwarz J. Current global trends in the incidence of pediatric-onset inflammatory bowel disease. World J Gastroenterol. (2018) 24:2741–63. doi: 10.3748/wjg.v24.i25.2741
9. Kang HM, Jeong DC, Suh BK, Ahn MB. The impact of the coronavirus disease-2019 pandemic on childhood obesity and vitamin D status. J Korean Med Sci. (2021) 36:e21. doi: 10.3346/jkms.2021.36.e21
10. Nogueira-de-Almeida CA, Del Ciampo LA, Ferraz IS, Del Ciampo IRL, Contini AA, Ued FDV. COVID-19 and obesity in childhood and adolescence: a clinical review. J Pediatr (Rio J). (2020) 96:546–58. doi: 10.1016/j.jped.2020.07.001
11. Ahn SY, Park JY, Lim IS, Chae SA, Yun SW, Lee NM, et al. Changes in the occurrence of gastrointestinal infections after COVID-19 in Korea. J Korean Med Sci. (2021) 36:e180. doi: 10.3346/jkms.2021.36.e180
12. Hong SJ, Kang B, Hwang JH, Kim YB, Lee YM, Jang HJ, et al. The occurrence of infection-related systemic diseases in Korean children and adolescents has decreased after the spread of the COVID-19 pandemic: a multicenter retrospective study. Transl Pediatr. (2021) 10:2888–96. doi: 10.21037/tp-21-315
13. Levine A, Griffiths A, Markowitz J, Wilson DC, Turner D, Russell RK, et al. Pediatric modification of the Montreal classification for inflammatory bowel disease: the Paris classification. Inflamm Bowel Dis. (2011) 17:1314–21. doi: 10.1002/ibd.21493
14. Abraham J. Computation of CIs for Binomial Proportions in SAS its Practical Difficulties. (2013). Available at: https://www.semanticscholar.org/paper/Computation-of-CIs-for-Binomial-proportions-in-SAS-Abraham/e0f243f4e5ea664499bb1e0128c5ab8f4333114a (Accessed August 30, 2021).
15. Korea S. 2017–2021 Local population population density. (2021). Available at: http://www.index.go.kr/potal/stts/idxMain/selectPoSttsIdxSearch.do?idx_cd=1007&stts_cd=100701&freq=Y (Accessed August 26, 2021).
16. Benchimol EI, Fortinsky KJ, Gozdyra P, Van den Heuvel M, Van Limbergen J, Griffiths AM. Epidemiology of pediatric inflammatory bowel disease: a systematic review of international trends. Inflamm Bowel Dis. (2011) 17:423–39. doi: 10.1002/ibd.21349
17. Srivastava A, Sathiyasekharan M, Jagadisan B, Bolia R, Peethambaran M, Mammayil G, et al. Paediatric inflammatory bowel disease in India: a prospective multicentre study. Eur J Gastroenterol Hepatol. (2020) 32:1305–11. doi: 10.1097/MEG.0000000000001859
18. Cui G, Yuan A. A systematic review of epidemiology and risk factors associated with Chinese inflammatory bowel disease. Front Med. (2018) 5:183. doi: 10.3389/fmed.2018.00183
19. Wang XQ, Zhang Y, Xu CD, Jiang LR, Huang Y, Du HM, et al. Inflammatory bowel disease in Chinese children: a multicenter analysis over a decade from Shanghai. Inflamm Bowel Dis. (2013) 19:423–8. doi: 10.1097/MIB.0b013e318286f9f2
20. Poddighe D, Telman A, Tuleutayev E, Ibrayeva A. Pediatric ulcerative colitis in Kazakhstan: first case series from Central Asia and current clinical management. Gastroenterol Insights. (2020) 11:27–35. doi: 10.3390/gastroent11020006
21. Ng SC, Kaplan GG, Tang W, Banerjee R, Adigopula B, Underwood FE, et al. Population density and risk of inflammatory bowel disease: a prospective population-based study in 13 countries or regions in Asia-Pacific. Am J Gastroenterol. (2019) 114:107–15. doi: 10.1038/s41395-018-0233-2
22. Ishige T, Tomomasa T, Hatori R, Tatsuki M, Igarashi Y, Sekine K, et al. Temporal trend of pediatric inflammatory bowel disease: analysis of national registry data 2004 to 2013 in Japan. J Pediatr Gastroenterol Nutr. (2017) 65:e80–2. doi: 10.1097/MPG.0000000000001547
23. Ong C, Aw MM, Liwanag MJ, Quak SH, Phua KB. Rapid rise in the incidence and clinical characteristics of pediatric inflammatory bowel disease in a South-East Asian cohort in Singapore, 1994–2015. J Dig Dis. (2018) 19:395–403. doi: 10.1111/1751-2980.12641
24. Abramson O, Durant M, Mow W, Finley A, Kodali P, Wong A, et al. Incidence, prevalence, and time trends of pediatric inflammatory bowel disease in Northern California, 1996 to 2006. J Pediatr. (2010) 157:233–239.e1. doi: 10.1016/j.jpeds.2010.02.024
25. Virta LJ, Saarinen MM, Kolho KL. Inflammatory bowel disease incidence is on the continuous rise among all paediatric patients except for the very young: a nationwide registry-based study on 28-year follow-up. J Crohns Colitis. (2017) 11:150–6. doi: 10.1093/ecco-jcc/jjw148
26. Castro M, Papadatou B, Baldassare M, Balli F, Barabino A, Barbera C, et al. Inflammatory bowel disease in children and adolescents in Italy: data from the pediatric national IBD register (1996–2003). Inflamm Bowel Dis. (2008) 14:1246–52. doi: 10.1002/ibd.20470
27. Hong SJ, Cho SM, Choe BH, Jang HJ, Choi KH, Kang B, et al. Characteristics and incidence trends for pediatric inflammatory bowel disease in Daegu-Kyungpook Province in Korea: a multi-center study. J Korean Med Sci. (2018) 33:e132. doi: 10.3346/jkms.2018.33.e132
28. Henderson P, Hansen R, Cameron FL, Gerasimidis K, Rogers P, Bisset WM, et al. Rising incidence of pediatric inflammatory bowel disease in Scotland. Inflamm Bowel Dis. (2012) 18:999–1005. doi: 10.1002/ibd.21797
29. Benchimol EI, Manuel DG, Guttmann A, Nguyen GC, Mojaverian N, Quach P, et al. Changing age demographics of inflammatory bowel disease in Ontario, Canada: a population-based cohort study of epidemiology trends. Inflamm Bowel Dis. (2014) 20:1761–9. doi: 10.1097/MIB.0000000000000103
30. Ghersin I, Khteeb N, Katz LH, Daher S, Shamir R, Assa A. Trends in the epidemiology of inflammatory bowel disease among Jewish Israeli adolescents: a population-based study. Aliment Pharmacol Ther. (2019) 49:556–63. doi: 10.1111/apt.15160
31. Shen YM, Wu JF, Chen HL, Hsu HY, Chang MH, Hsieh TK, et al. Characteristics and incidences of pediatric Crohn's disease in the decades before and after 2000. Pediatr Neonatol. (2011) 52:317–20. doi: 10.1016/j.pedneo.2011.08.003
32. Kim BJ, Song SM, Kim KM, Lee YJ, Rhee KW, Jang JY, et al. Characteristics and trends in the incidence of inflammatory bowel disease in Korean children: a single-center experience. Dig Dis Sci. (2010) 55:1989–95. doi: 10.1007/s10620-009-0963-5
33. Shin DH, Sinn DH, Kim YH, Kim JY, Chang DK, Kim EJ, et al. Increasing incidence of inflammatory bowel disease among young men in Korea between 2003 and 2008. Dig Dis Sci. (2011) 56:1154–9. doi: 10.1007/s10620-010-1403-2
34. Grieci T, Bütter A. The incidence of inflammatory bowel disease in the pediatric population of Southwestern Ontario. J Pediatr Surg. (2009) 44:977–80. doi: 10.1016/j.jpedsurg.2009.01.038
35. Benchimol EI, Bernstein CN, Bitton A, Carroll MW, Singh H, Otley AR, et al. Trends in epidemiology of pediatric inflammatory bowel disease in Canada: distributed network analysis of multiple population-based provincial health administrative databases. Am J Gastroenterol. (2017) 112:1120–34. doi: 10.1038/ajg.2017.97
36. Sjöberg D, Holmström T, Larsson M, Nielsen AL, Holmquist L, Ekbom A, et al. Incidence and natural history of ulcerative colitis in the Uppsala Region of Sweden 2005-2009—results from the IBD cohort of the Uppsala Region (ICURE). J Crohns Colitis. (2013) 7:e351–7. doi: 10.1016/j.crohns.2013.02.006
37. Lehtinen P, Pasanen K, Kolho KL, Auvinen A. Incidence of pediatric inflammatory bowel disease in Finland: an environmental study. J Pediatr Gastroenterol Nutr. (2016) 63:65–70. doi: 10.1097/MPG.0000000000001050
38. Fernández A, Hernández V, Martínez-Ares D, Sanromán L, de Castro ML, Pineda JR, et al. Incidence and phenotype at diagnosis of inflammatory bowel disease. Results in Spain of the EpiCom study. Gastroenterol Hepatol. (2015) 38:534–40. doi: 10.1016/j.gastrohep.2015.03.001
39. Statistics Korea. 2020 Birth Death Trends. (2021). Available at: http://www.index.go.kr/potal/main/EachDtlPageDetail.do?idx_cd=1011 (Accessed August 26, 2021).
Keywords: COVID-19, inflammatory bowel disease, Crohn's disease, Korea, Asia, child
Citation: Choe JY, Choi S, Song KH, Jang H-J, Choi K-H, Yi DY, Hong SJ, Hwang JH, Cho S-M, Kim YJ, Choe B-H and Kang B (2022) Incidence and Prevalence Trends of Pediatric Inflammatory Bowel Disease in the Daegu-Kyungpook Province From 2017 to 2020. Front. Pediatr. 9:810173. doi: 10.3389/fped.2021.810173
Received: 06 November 2021; Accepted: 13 December 2021;
Published: 04 January 2022.
Edited by:
Dimitri Poddighe, Nazarbayev University School of Medicine, KazakhstanReviewed by:
Iago Rodríguez-Lago, Galdakao University Hospital, SpainCopyright © 2022 Choe, Choi, Song, Jang, Choi, Yi, Hong, Hwang, Cho, Kim, Choe and Kang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ben Kang, YmVua2FuZ0BrbnUuYWMua3I=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.