
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr. , 05 January 2022
Sec. Pediatric Infectious Diseases
Volume 9 - 2021 | https://doi.org/10.3389/fped.2021.752993
 Melissa Lucero Tanaka1†
Melissa Lucero Tanaka1† Carolyn Jennifer Marentes Ruiz1†
Carolyn Jennifer Marentes Ruiz1† Sanchi Malhotra1
Sanchi Malhotra1 Lauren Turner1
Lauren Turner1 Ariana Peralta1
Ariana Peralta1 Yesun Lee1
Yesun Lee1 Jaycee Jumarang1
Jaycee Jumarang1 Stephanie E. Perez1
Stephanie E. Perez1 Jocelyn Navarro1
Jocelyn Navarro1 Jennifer Dien Bard2
Jennifer Dien Bard2 Aubree Gordon3
Aubree Gordon3 E. Kaitlynn Allen4
E. Kaitlynn Allen4 Paul G. Thomas4
Paul G. Thomas4 Pia S. Pannaraj1,5*
Pia S. Pannaraj1,5*Objectives: Studies of household transmission of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) focused on households with children are limited. We investigated household secondary attack rate (SAR), transmission dynamics, and contributing factors in households with children.
Materials and Methods: In this prospective case-ascertained study in Los Angeles County, California, all households members were enrolled if ≥1 member tested positive for SARS-CoV-2 by polymerase chain reaction (PCR). Nasopharyngeal PCRs, serology, and symptom data were obtained over multiple visits.
Results: A total of 489 individuals in 105 households were enrolled from June to December 2020. The majority (77.3%) reported a household annual income of <$50,000, and most (92.9%) were of Hispanic/Latinx ethnicity. Children <18 years old accounted for 46.9% index cases, of whom 45.3% were asymptomatic. Household index cases were predominantly children during low community transmission and adults during the high community transmission period (χ2 = 7.647, p = 0.0036. The mean household SAR was 77.0% (95% CI: 69.4–84.6%). Child and adult index cases both efficiently transmitted SARS-CoV-2 within households [81.9%, (95% CI: 72.1–91.9%) vs. 72.4% (95% CI: 59.8–85.1%), p = 0.23]. Household income and pets were significantly associated with higher SAR in the multivariable analysis of household factors (p = 0.0013 and 0.004, respectively).
Conclusions: The SAR in households with children in an urban setting with a large ethnic minority population is much higher than previously described. Children play important roles as index cases. SAR was disproportionately impacted by household income. Vaccination and public health efforts need special focus on children and vulnerable communities to help mitigate SARS-CoV-2 spread.
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) has continued to spread rapidly worldwide, leading to over 4.2 million deaths globally (1). Although travel and work exposure dominated initial SARS-CoV-2 spread, household exposure quickly became the principal source of transmission (2, 3). Households are high-risk settings for the spread of SARS-CoV-2 via respiratory droplets, aerosols, and fomites due to sustained close contact in enclosed indoor settings (4, 5). Published studies show a household attack rate of 47% and a secondary attack rate (SAR) ranging from 6 to 53 percent among household contacts (5–14), with a mean SAR of 16.6% on a meta-analysis of 44 studies by Madewell et al. (5). Previous studies suggest that children under 18 years old are unlikely to be index cases and result in a lower attack rate, that secondary attack rates are higher in adults than children, and that asymptomatic index cases have a limited role in household transmission (5, 15–18). The number of Coronavirus disease 2019 (COVID-19) cases in children, however, has been on the rise since summer 2020, paralleling trends among adults (19).
Many household studies are limited by evaluation of only a few members of the household, focusing primarily on adults in the household, using a cross-sectional or retrospective approach, studying a short period of time, or lacking serologic data. Here we describe a prospective, case-ascertained study of household SARS-CoV-2 transmission in Los Angeles, California. This is the largest household study in North America to our knowledge, the first to report findings over multiple phases of the pandemic, and one of few studies to focus primarily on households with children in an urban setting. Los Angeles County has been a hot spot of disease burden during this pandemic, with the highest COVID-19 positivity rate and the most daily new cases per 100,000 residents nationwide for most of the winter. Understanding transmission and characteristics of urban households, especially among ethnic minority populations disproportionately affected by COVID-19, will help in the development of COVID-19 prevention and mitigation measures.
Households in Los Angeles County, California were prospectively enrolled into the Household Exposure and Respiratory Virus Transmission and Immunity Study (HEARTS) if at least one household member tested positive for SARS-CoV-2 within 2 weeks prior to enrollment and at least two members living in the household agreed to participate. We recruited households of patients who tested positive for SARS-CoV-2 at Children's Hospital Los Angeles (CHLA) using a convenience recruitment strategy. These individuals had presented for testing due to COVID-19 symptoms, known exposure, or in preparation for a routine procedure or hospital admission. Recruitment fliers were also posted at CHLA and at community testing sites near the hospital. We defined a household as all people who occupy a housing unit; the household may include related family members and unrelated individuals (20).
At enrollment, a designated household representative responded to a questionnaire detailing household information including the number of household members, type of housing, number of bedrooms and bathrooms, pets, smokers, and household income in the last year. In addition, each consented household member answered an individual questionnaire that included demographic information, co-morbidities, and exposure history. Co-morbidities included pre-existing lung, heart, renal, liver, or neurologic disease, diabetes, cancer or other immunosuppression. Participants logged illness symptoms in a daily symptom diary for 28 days. Parents recorded symptoms for their children. COVID-19 associated symptoms were defined as at least one of the following: fever, chills, headache, runny nose, congestion, cough, sore throat, shortness of breath, wheeze, altered smell or taste, muscle aches, or gastrointestinal symptoms. Data was recorded in the Research Electronic Data Capture (REDCap Consortium, Vanderbilt, Tennessee, USA).
Participants presented to our drive-thru respiratory testing center for nasopharyngeal (NP) swabs performed by trained study staff every 3–7 days for up to 4 weeks or until two consecutive negative SARS-CoV-2 real-time reverse transcription polymerase chain reaction (RT-PCR) results were produced. Blood was collected at the enrollment visit and a convalescent visit after 4 weeks from resolution of the last symptomatic household member. The study was approved by the Institutional Review Board at Children's Hospital Los Angeles.
We tested for SARS-Cov-2 using the CDC protocol that was approved by the Food and Drug Administration (FDA) for emergency use authorization (EUA) (21). RT-PCR was performed using primers and probes that targeted the N1, N2, and RnaseP (RNP, internal control) genes (Integrated DNA Technologies, Coralville, IW). A positive result was defined as cycle threshold (CT) value <40 for both N1 and N2. A valid result for SARS-CoV-2 detection was determined by RNP using a cut-off of CT value < 32. An inconclusive result was defined as either N1 or N2 gene detected only with RNP detection.
Serum SARS-CoV-2 receptor binding domain (RBD) and spike IgG antibody was measured using an ELISA, as previously described (22). A positive cut-off OD490 value of 0.2 was used for RBD based on the published protocol and the mean of the negative control values plus 3 standard deviations (SD) from 20 blood samples collected between 2017 and 2019. IgG against the spike protein was used to confirm RBD IgG positivity.
The attack rate of individuals per household was defined as the number of COVID-19 positive cases during the testing time period divided by the total number of household members. SAR in each household was defined as the number of new cases divided by the total number of at-risk members after subtracting out the index case. We used the earliest date between symptom onset and first positive RT-PCR result for each individual to determine the order of infection within a household. The index case was defined as the individual with the earliest onset date for symptoms or positive test in the household. If two members had the same earliest date for symptoms or positive test, they were considered co-index cases. If infection order could not be determined (e.g., asymptomatic case determined by acute/convalescent serology) for any household member, that household was excluded from the SAR analyses.
Comparisons of categorical variables were calculated using Pearson chi-square. Independent sample T-tests were used for comparison of continuous variables. Multiple linear regression analysis using the forward selection method was used to determine predictors of household attack rate and SAR. Variables were checked for multicollinearity; if found, only one variable was included in the multivariable model. All remaining factors with p ≤ 0.10 in the univariate analysis were included in the multivariable analysis. Statistical analyses were performed using SPSS Version 27.0 (IBM Corp., Armonk, NY). All tests were 2-tailed with p < 0.05 considered significant.
We enrolled 105 households with 489 individuals from June 17 to December 31, 2020, prior to COVID-19 vaccination roll-out to the general population. Three households were excluded from the analysis because only one member presented for PCR testing. One household was excluded because all members except for the index case had documented COVID-19 infection >3 months earlier. The 101 remaining households were included. Of those, 99 enrolled all individuals currently living in the household, two households each missed one individual, and one had two household members excluded due to prior diagnosed COVID-19 infection >3 months earlier. Therefore, we included 101 households with 477 individuals in the analysis.
Characteristics of the households are shown in Table 1. Households ranged from 2 to 11 members living together. All except five households had at least one child under 18 years of age. Almost half (46.5%) of the households had more than two persons per bedroom, meeting the definition for overcrowding based on the U.S. Department of Housing and Urban Development (20). The majority (77.3%) reported an annual household income of <$50,000 in the last year.
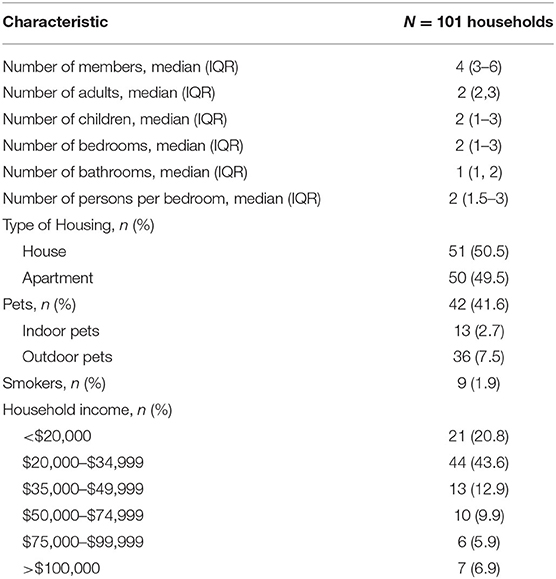
Table 1. Characteristics of households enrolled in a prospective study of SARS-CoV-2 household transmission—Los Angeles, California, USA, June–December 2020.
SARS-CoV-2 PCR testing of NP swabs in all 477 (100%) individuals and serology in 407 (85.3%) individuals were completed at the first visit. Individuals followed up for a median of three visits (IQR, 2–4) over 15 days (IQR, 7–27). Convalescent serology was obtained in 257 (53.9%) individuals. Overall, 393 (82.4%) tested positive for COVID-19 by PCR and/or serology at least one time point, six (1.3%) tested inconclusive by PCR with negative serology, and 78 (16.4%) tested negative for both at all time points. The COVID-19 positive individuals included 216 adults (55.0%) and 177 (45.0%) children. A little over half (233 [59.3%]) of the subjects who tested positive reported COVID-19 associated symptoms; 160 (72.7%) tested positive for SARS-CoV-2 after presenting with symptoms, 21 (9.2%) tested positive on the same day of illness onset, and 48 (21.0%) tested positive before developing symptoms. The majority of patients managed their symptoms at home, but two participants required hospitalization for COVID-19, and three participants were hospitalized for unrelated reasons. Fewer children were symptomatic compared with adults [91 (51.4%) vs. 142 (65.7%), p = 0.004].
Individual characteristics of all household participants, 113 index cases, and 214 secondary cases are shown in Table 2. Hispanic/Latinx ethnicity was associated with a higher individual SAR compared to non-Hispanic/Latinx ethnicity (80.0 vs. 47.4%, p = 0.002). This analysis excluded 18 households with 26 asymptomatic cases detected by positive SARS-CoV-2 serology only for whom infection order could not be determined.
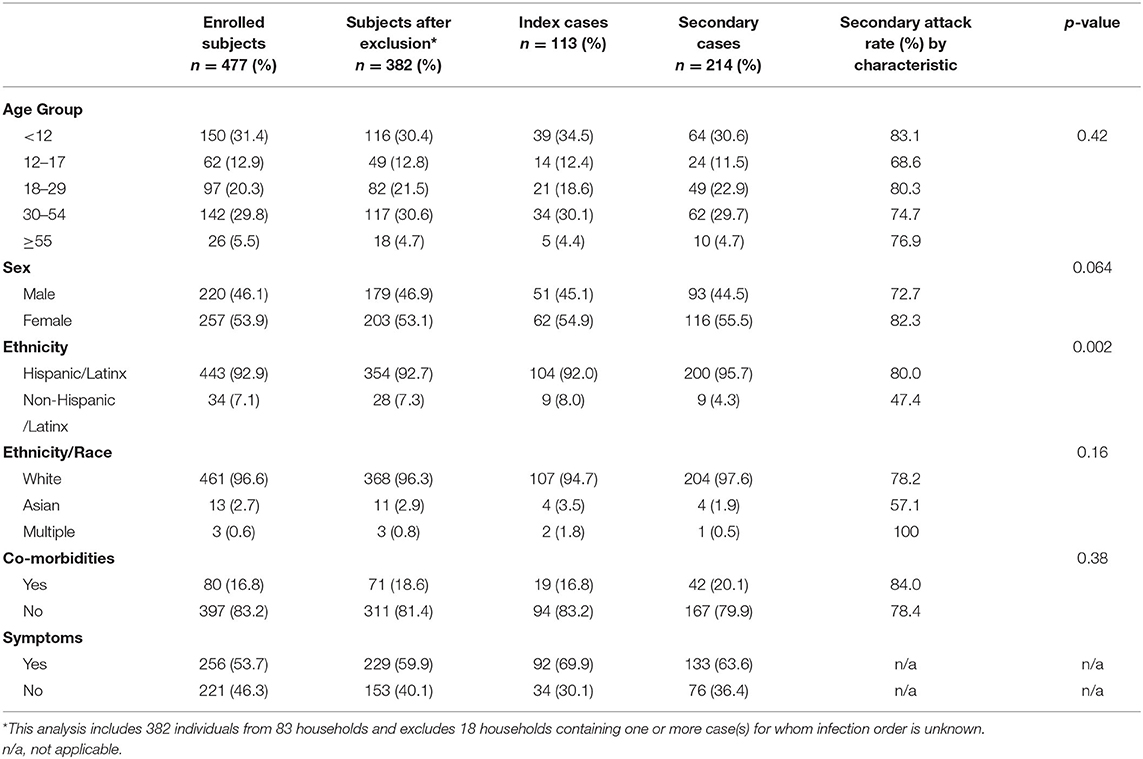
Table 2. Characteristics of all enrolled subjects, index cases, and secondary cases and individual secondary attack rate of laboratory-confirmed SARS-CoV-2 infections among those at risk by characteristics, in household members enrolled in a prospective study of SARS-CoV-2 household transmission—Los Angeles, California, June–December 2020.
Overall, children under 18 years of age accounted for 53 (46.9%) index cases, of whom 24 (45.3%) were asymptomatic. Children index cases were associated with periods of lower community case rates while adult index cases were associated with periods of high community transmission and rapid incidence rise of COVID-19 cases (p = 0.006, Figure 1 and Supplementary Table 1). Substantial secondary transmission occurred whether the index patient was an adult or a child [81.9%, (95% CI: 72.1–91.9%) vs. 72.4% (95% CI: 59.8–85.1%), p = 0.23]. Symptomatic and asymptomatic index cases both transmitted SARS-CoV-2 efficiently within the household [SAR: 76.7% (95% CI: 68.2–85.2%) vs. 78.2% (95% CI: 59.3–97.2%), p = 0.87]. Individuals reported last face-to-face contact with confirmed COVID-19 positive household members a median of 0 days (IQR, 0–0) prior to the day of study enrollment, i.e. on the same day, suggesting very close contact in the household.
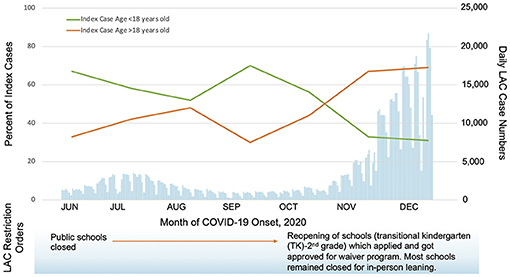
Figure 1. Laboratory-confirmed index cases by age group in participating households compared to Los Angeles County (LAC) daily case numbers, June-December 2020 (23). Household index cases were predominantly children during low community transmission (before November 1, 2020) and adults during the high community transmission period (after November 1, 2020), χ2 = 7.647, p = 0.006.
Of the 101 households, 94 (93.1%) had at least one secondary laboratory-confirmed SARS-CoV-2 infection among household members. All members tested positive in 61 (60.4%) households. The mean household SAR was 77.0% (95% CI: 69.4–84.6%) when looking at PCR and serology data together, after excluding those households with any individuals with unknown infection order. If the SAR per household was calculated solely by PCR data, it would be underestimated at 63.2% (95% CI: 55.3–71.2). Because of the risk of misclassification of asymptomatic cases and varying incubation periods (24), we performed additional analyses after reclassifying cases within 1–5 days of the index case as a sensitivity analysis (Supplementary Table 2). The SAR remained high above 63%, even with reclassification. In a univariate analysis including all households, income, ethnicity, having multiple index cases, and pets were possible predictors (p ≤ 0.10) of a higher household SAR. In the multivariable analysis, only household income and pets remained significant factors associated with higher household SAR (Table 3). The mean attack rate in all households was 83.9 (95% CI: 79.4–88.3%). The number of bedrooms, bathrooms, household income, multiple index cases, and Hispanic/Latinx ethnicity were each associated with a higher attack rate in univariate analyses (Table 4). However, in the multivariable analysis after removing variables with multicollinearity, only the number of bedrooms was found to be a significant predictor of higher attack rates in the household.
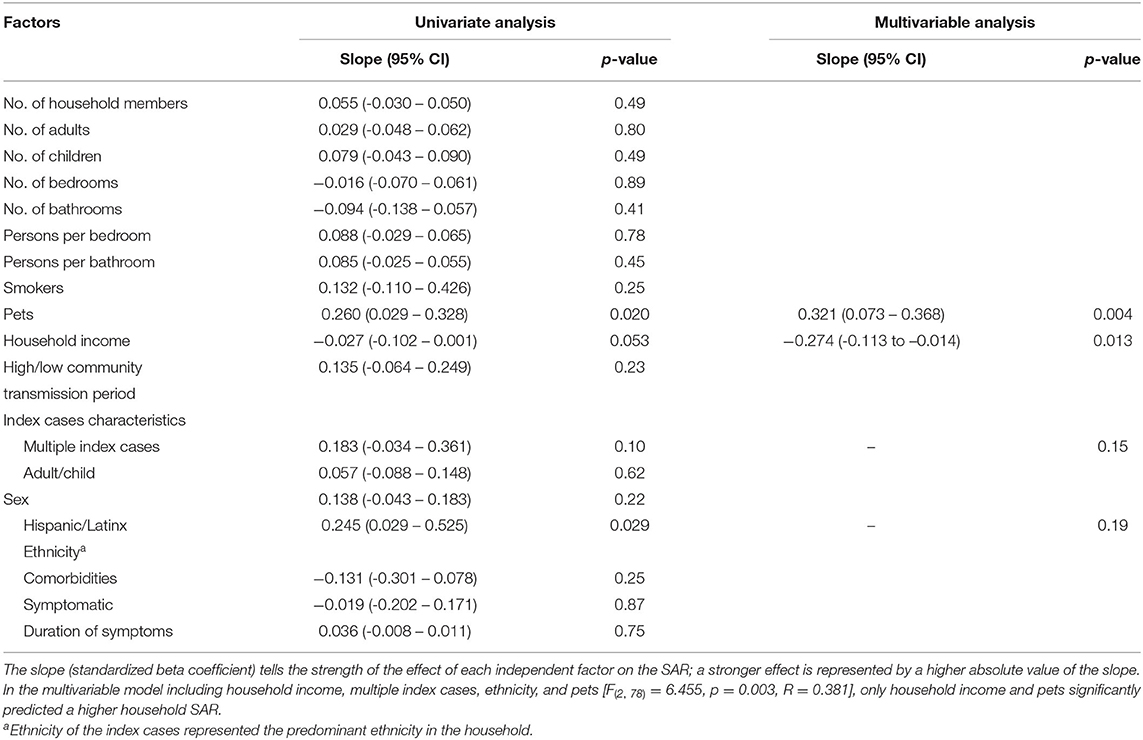
Table 3. Univariate and multivariable linear regression analysis of predictors of the household secondary attack rate (SAR).
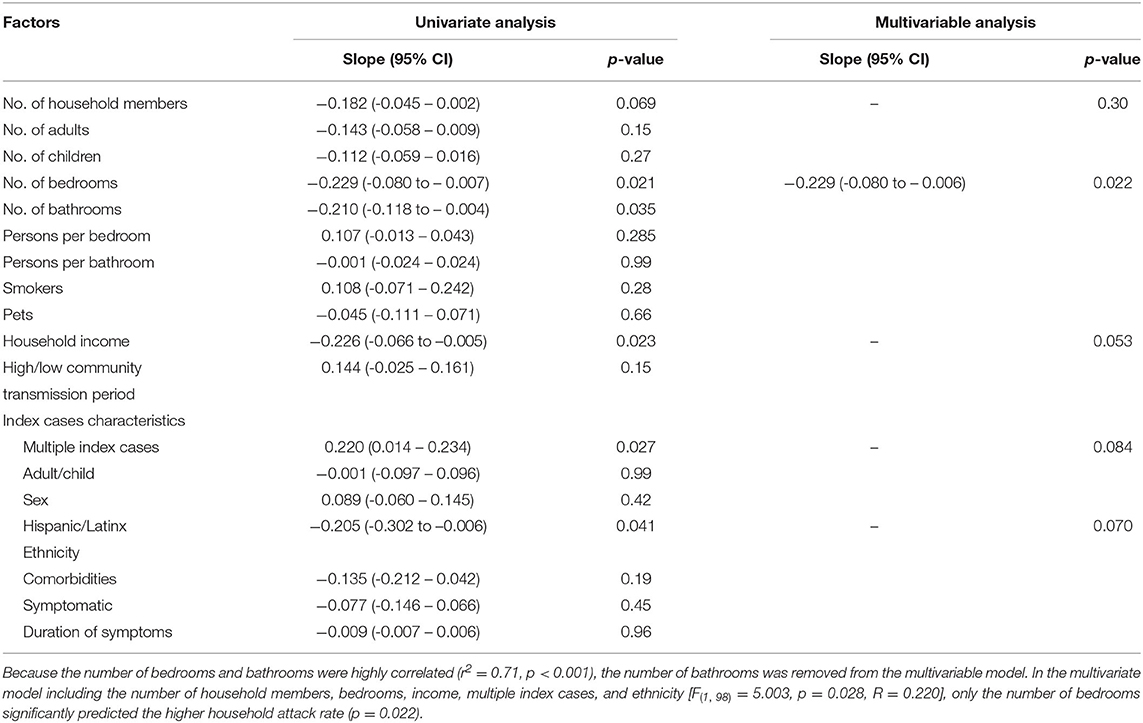
Table 4. Univariate and multivariable linear regression analysis of predictors of the household attack rate (includes index cases).
This study focused on a high predominance of low-income Hispanic/Latinx households with children in an urban setting, a vulnerable group disproportionately affected by the pandemic in the United States. We report the highest recorded mean attack rate of 83.9% within our households and SAR of 77.0% compared with previous household studies (5–14). Only a few studies have found household SAR over 50% (25, 26). All members tested positive in 60.4% of our households, showing intense clustering of SARS-CoV-2 infections within households during periods of low and high community transmission.
The number of bedrooms was a significant factor in predicting the overall household attack rate in the multivariable analysis. Fewer bedrooms likely decreased the ability to properly quarantine within the living space. Indeed, most participants reported daily face-to-face contact with a known COVID-19 positive household member, supporting decreased ability to isolate from other household members. Medical sheltering facilities or temporary housing using hotels and motels may be useful for COVID-19 positive patients for the purpose of isolation to decrease household clusters of infection (27, 28).
Lower household income was significant in the multivariable analysis to predict a higher household SAR. This is most plausibly a reflection of the combination of challenges faced by households with low socioeconomic status such as decreased access to care, an obligation to work and interact with the community, different housing patterns, neighborhood interactions, and neighborhood childcare which we did not capture in our study. Although presence of pets were also associated with higher household SAR and it seems theoretically possible that pets could briefly carry the virus and spread it throughout the household, most studies to-date do not show evidence of pet-to-human transmission (29, 30). Hispanic/Latinx ethnicity was associated with higher individual SAR. This may be due to the large Hispanic/Latinx cohort in our study. Ethnic minority populations are currently at the highest risk of infection, hospitalization, and death from COVID-19 (31, 32). Multiple data sources have shown a disproportionately high case rate amongst the Hispanic/Latinx population, with a death rate 2.3 times higher than the non-Hispanic/Latinx White population (31, 33). The higher attack rates in these communities reinforces the need for vaccination efforts specifically focused on the lower income and disproportionately affected ethnic minority populations to overcome this large disparity (34, 35).
By following our patients over the pandemic, we found that both adults and children are responsible for bringing SARS-CoV-2 to the household as the index case. A recent population-based cohort study in Canada also found that younger children were more likely to transmit SARS-CoV-2 infection compared with older children (36). During the period with lower case numbers in the community (23), we observed that the index cases were most frequently children, despite public school closures. We did not ask households about adherence to community restrictions or childcare practices during school closure, but it is possible that public health measures were not followed as strictly when children were not in school in our study population (37). A study in Spain found that children were less likely to be index cases, but higher SAR occurred when children were out of school (25). Further studies are needed to determine if children will be important drivers of transmission similar to influenza (38) during periods without community restrictions. So far, school reopenings have not been associated with a significant increase in COVID-19 community transmission (39, 40); risk must be weighed against the significant benefit of in-person schooling (41). During the largest peak of COVID-19 cases when community restrictions intensified in Los Angeles, adults 18–54 years of age comprised the highest proportion of index cases. Los Angeles County restriction orders at this time included no in-person dining, decreased capacity for essential and non-essential establishments, and no private or public gathering. Adults in that age group were the most mobile individuals within the household and at the highest risk to acquire SARS-CoV-2 from work or social contacts outside of the family.
Substantial secondary transmission occurred from both child and adult index cases in our households. Other studies have shown a significantly lower SAR when the index case is a child (16, 42); fewer studies have found a higher SAR from child index cases compared with adults (42). Almost a third of our index cases were asymptomatic overall. Of the child index cases, almost half were asymptomatic. Unlike previous studies (5, 11, 42, 43), we found that asymptomatic index cases were important transmitters of SARS-CoV-2 similarly to symptomatic index cases. Individuals who are asymptomatic or have only mild symptoms generally remain active and are thus in greater contact with others, increasing the possibility of transmission to the household and community (44, 45).
Strengths of the study include capturing and testing entire households including all children, prospectively and repeatedly performing PCR testing on NP swabs over multiple visits to identify cases, and incorporating serologic data into the analysis to catch asymptomatic individuals who may have missed the PCR positivity window. However, the findings are subject to limitations. The convenience sampling strategy, especially during the pandemic, may cause selection bias. We were unable to determine the infection order in 26 (5.5%) participants who were serologically positive but asymptomatic, which may underestimate the number of asymptomatic index cases. Misclassification of index cases is a challenge for SARS-CoV-2 transmission studies, due to the possibility of different incubation time periods and asymptomatic presentation (24). We did not perform contact tracing outside of the household to capture the source of infection outside of the household. Only half of the participants returned for convalescent serology; therefore, we may have missed individuals who developed COVID-19 immediately before enrollment or during the follow-up period and missed by the NP swab. We could not definitively differentiate second cases from subsequent cases in the households; all were included in the SAR definition. Almost all patients who were enrolled only had mild illness, and this may underestimate the SAR in households where the index patient was more severely symptomatic. A possibility exists that some of the subsequent household cases were actually acquired outside the household rather than from household transmission, the SAR did not increase during the period of increased community transmission. Viral sequencing was not performed. Cultural practices may play a role in the transmission dynamics for which we did not assess.
Households with children in low income, urban communities have an extremely high household SAR. Strategies to decrease household transmission, particularly in ethnic minority communities and low socioeconomic settings, remains crucial to controlling the SARS-CoV-2 pandemic. It is imperative to increase access to resources to make infection prevention, COVID-19 testing, and following quarantine guidelines possible and less challenging for these populations. Children, both symptomatic and asymptomatic, are important contributors to household spread. Children could be drivers of continued low level community SARS-CoV-2 circulation in vulnerable populations without vaccination. Future vaccination efforts must include special focus on children and ethnic minority populations, including the households with low income who are disproportionately affected.
The raw data supporting the conclusions of this article will be made available by the authors upon request, without undue reservation.
The studies involving human participants were reviewed and approved by Children's Hospital Los Angeles Institutional Review Board. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
PP conceptualized and designed the study, analyzed the data, and reviewed and revised the manuscript. MT and CM collected data, carried out the initial analyses, and drafted the initial manuscript. SM helped carry out the initial analysis and draft the initial manuscript. LT and AP designed the data collection instruments, collected data, and reviewed and revised the manuscript. JN helped design the data collection instruments and reviewed and revised the manuscript. YL, PT, and AG helped design the study and reviewed and revised the manuscript. JJ and SP collected data and reviewed and revised the manuscript. EA and JD reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
This work was supported by the National Institute of Allergy and Infectious Diseases at the National Institutes of Health [U01AI144616-02S1] and a grant from Open Philanthropy.
PP has received consultant fees from Sanofi-Pasteur and Seqirus and also receives research funding from AstraZeneca and Pfizer for unrelated studies. AG has received consultant fees from Janssen.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We wish to thank the dedicated participants who contributed to this study. We would like to thank Florian Krammer and Ali Ellebedy for sharing constructs SARS-CoV-2 antigen and antibody constructs and Janet Smith, Melanie Ohi, Clay Brown, Jennifer Meagher, Brad Carlson, and Rebecca Tutino for providing the antibodies and antigens used in the ELISAs.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2021.752993/full#supplementary-material
CHLA, Children's Hospital Los Angeles; CI, Confidence Interval; CT, Cycle threshold; COVID-19, Coronavirus disease 2019; ELISA, Enzyme-linked immunosorbent assay; FDA, Food and Drug Administration; IQR, Interquartile range; NP, Nasopharyngeal; RBD, Receptor binding domain; RNP, RnaseP; RT-PCR, Reverse Transcriptase-Polymerase Chain Reaction; SAR, Secondary attack rate; SARS-CoV-2, Severe acute respiratory syndrome coronavirus-2; SD, Standard deviations.
1. World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. (2021). Available online at: https://covid19.who.int (accessed February 8, 2021).
2. Gudbjartsson DF, Helgason A, Jonsson H, Magnusson OT, Melsted P, Norddahl GL, et al. Spread of SARS-CoV-2 in the Icelandic Population. N Engl J Med. (2020) 382:2302–15. doi: 10.1056/NEJMoa2006100
3. Wang Z, Ma W, Zheng X, Wu G, Zhang R. Household transmission of SARS-CoV-2. J Infect. (2020) 81:179–82. doi: 10.1016/j.jinf.2020.03.040
4. Centers for Disease Control and Prevention. Scientific Brief: SARS-CoV-2 and Potential Airborne Transmission. (2020). Available online at: https://www.cdc.gov/coronavirus/2019-ncov/more/scientific-brief-sars-cov-2.html (accessed October 5, 2020).
5. Madewell ZJ, Yang Y, Longini IM Jr, Halloran ME, Dean NE. Household transmission of SARS-CoV-2: a systematic review and meta-analysis. J Am Med Assoc Netw Open. (2020) 3:e2031756. doi: 10.1001/jamanetworkopen.2020.31756
6. Lewis NM, Chu VT, Ye D, Conners EE, Gharpure R, Laws RL, et al. Household transmission of SARS-CoV-2 in the United States. Clin Infect Dis. (2020) 73:1805–13. doi: 10.1093/cid/ciaa1166
7. Jing QL, Liu MJ, Zhang ZB, Fang LQ, Yuan J, Zhang AR, et al. Household secondary attack rate of COVID-19 and associated determinants in Guangzhou, China: a retrospective cohort study. Lancet Infect Dis. (2020) 20:1141–50. doi: 10.1016/S1473-3099(20)30471-0
8. Viner RM, Mytton OT, Bonell C, Melendez-Torres GJ, Ward J, Hudson L, et al. Susceptibility to SARS-CoV-2 infection among children and adolescents compared with adults: a systematic review and meta-analysis. J Am Med Assoc Pediatr. (2021) 175:143–56. doi: 10.1001/jamapediatrics.2020.4573
9. Wu J, Huang Y, Tu C, Bi C, Chen Z, Luo L, et al. Household transmission of SARS-CoV-2, Zhuhai, China, 2020. Clin Infect Dis. (2020) 71:2099–108. doi: 10.1093/cid/ciaa557
10. Grijalva CG, Rolfes MA, Zhu Y, McLean HQ, Hanson KE, Belongia EA, et al. Transmission of SARS-COV-2 infections in households - Tennessee and Wisconsin, April-September 2020. Morb Mortal Wkly Rep. (2020) 69:1631–4. doi: 10.15585/mmwr.mm6944e1
11. Fung HF, Martinez L, Alarid-Escudero F, Salomon JA, Studdert DM, Andrews JR, et al. The household secondary attack rate of SARS-CoV-2: a rapid review. Clin Infect Dis. (2020) 73:S138–45. doi: 10.1093/cid/ciaa1558
12. Kuwelker K, Zhou F, Blomberg B, Lartey S, Brokstad KA, Trieu MC, et al. Attack rates amongst household members of outpatients with confirmed COVID-19 in Bergen, Norway: a case-ascertained study. Lancet Reg Health Eur. (2021) 3:100014. doi: 10.1016/j.lanepe.2020.100014
13. Goh DL-M, Lee BW, Chia KS, Heng BH, Chen M, Ma S, et al. Secondary household transmission of SARS, Singapore. Emerg Infect Dis J. (2004) 10:232. doi: 10.3201/eid1002.030676
14. Ng OT, Marimuthu K, Koh V, Pang J, Linn KZ, Sun J, et al. SARS-CoV-2 seroprevalence and transmission risk factors among high-risk close contacts: a retrospective cohort study. Lancet Infect Dis. (2021) 21:333–43. doi: 10.1016/S1473-3099(20)30833-1
15. Kim J, Choe YJ, Lee J, Park YJ, Park O, Han MS, et al. Role of children in household transmission of COVID-19. Arch Dis Child. (2020) 106:709–11. doi: 10.1136/archdischild-2020-319910
16. Posfay-Barbe KM, Wagner N, Gauthey M, Moussaoui D, Loevy N, Diana A, et al. COVID-19 in children and the dynamics of infection in families. Pediatrics. (2020) 146:1576. doi: 10.1542/peds.2020-1576
17. Li X, Xu W, Dozier M, He Y, Kirolos A, Lang Z, et al. Uncover. The role of children in the transmission of SARS-CoV2: updated rapid review. J Glob Health. (2020) 10:021101. doi: 10.7189/jogh.10.0201101
18. Lugon P, Fuller T, Damasceno L, Calvet G, Resende PC, Matos AR, et al. SARS-CoV-2 infection dynamics in children and household contacts in a slum in Rio de Janeiro. Pediatrics. (2021) 148:e2021050182. doi: 10.1542/peds.2021-050182
19. Leidman E, Duca LM, Omura JD, Proia K, Stephens JW, Sauber-Schatz EK. COVID-19 trends among persons aged 0-24 years - United States, March 1-December 12, 2020. Morb Mortal Wkly Rep. (2021) 70:88–94. doi: 10.15585/mmwr.mm7003e1
20. U.S. Census Bureau. U.S. Census Bureau Subject Definitions. (2020). Available online at: https://www.census.gov/programs-surveys/cps/technical-documentation/subject-definitions.html#household (accessed August 27, 2020).
21. Centers for Disease Control and Prevention. CDC 2019-Novel Coronavirus (2019-nCoV) Real-Time RT-PCR Diagnostic Panel. (2020). Available online at: https://www.fda.gov/media/134922/download (accessed 2020 February 1).
22. Stadlbauer D, Amanat F, Chromikova V, Jiang K, Strohmeier S, Arunkumar GA, et al. SARS-CoV-2 seroconversion in humans: a detailed protocol for a serological assay, antigen production, and test setup. Curr Protoc Microbiol. (2020) 57:e100. doi: 10.1002/cpmc.100
23. Los Angeles County Department of Public Health. LA County COVID-19 Surveillance Dashboard. (2021). Available online at: http://dashboard.publichealth.lacounty.gov/covid19_surveillance_dashboard/ (accessed February 15, 2021).
24. Accorsi EK, Qiu X, Rumpler E, Kennedy-Shaffer L, Kahn R, Joshi K, et al. How to detect and reduce potential sources of biases in studies of SARS-CoV-2 and COVID-19. Eur J Epidemiol. (2021) 36:179–96. doi: 10.1007/s10654-021-00727-7
25. Soriano-Arandes A, Gatell A, Serrano P, Biosca M, Campillo F, Capdevila R, et al. Household severe acute respiratory syndrome coronavirus 2 transmission and children: a network prospective study. Clin Infect Dis. (2021) 73:e1261–9. doi: 10.1093/cid/ciab228
26. Buonsenso D, Valentini P, De Rose C, Pata D, Sinatti D, Speziale D, et al. Seroprevalence of anti-SARS-CoV-2 IgG antibodies in children with household exposure to adults with COVID-19: preliminary findings. Pediatr Pulmonol. (2021) 56:1374–7. doi: 10.1002/ppul.25280
27. Chen S, Zhang Z, Yang J, Wang J, Zhai X, Barnighausen T, et al. Fangcang shelter hospitals: a novel concept for responding to public health emergencies. Lancet. (2020) 395:1305–14. doi: 10.1016/S0140-6736(20)30744-3
28. Gomez J, Albaiceta GM, Cuesta-Llavona E, Garcia-Clemente M, Lopez-Larrea C, Amado-Rodriguez L, et al. The Interferon-induced transmembrane protein 3 gene (IFITM3) rs12252 C variant is associated with COVID-19. Cytokine. (2021) 137:155354. doi: 10.1016/j.cyto.2020.155354
29. Lauzi S, Stranieri A, Giordano A, Lelli D, Elia G, Desario C, et al. Do dogs and cats passively carry SARS-CoV-2 on hair and pads? Viruses. (2021) 13:71357. doi: 10.3390/v13071357
30. Drozdz M, Krzyzek P, Dudek B, Makuch S, Janczura A, Paluch E. Current state of knowledge about role of pets in zoonotic transmission of SARS-CoV-2. Viruses. (2021) 13:61149. doi: 10.3390/v13061149
31. Lopez L 3rd, Hart LH 3rd, Katz MH. Racial and ethnic health disparities related to COVID-19. J Am Med Assoc. (2021) 325:1049–52. doi: 10.1001/jama.2020.26443
32. Galea S, Abdalla SM. COVID-19 pandemic, unemployment, and civil unrest: underlying deep racial and socioeconomic divides. J Am Med Assoc. (2020) 324:227–8. doi: 10.1001/jama.2020.11132
33. Centers for Disease Control Prevention. Risk for COVID-19 Infection, Hospitalization, and Death By Race/Ethnicity. (2021). Available online at: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html (accessed February 17, 2021).
34. Painter EM, Ussery EN, Patel A, Hughes MM, Zell ER, Moulia DL, et al. Demographic characteristics of persons vaccinated during the first month of the COVID-19 vaccination program - United States, December 14, 2020-January 14, 2021. Morb Mortal Wkly Rep. (2021) 70:174–7. doi: 10.15585/mmwr.mm7005e1
35. McClung N, Chamberland M, Kinlaw K, Bowen Matthew D, Wallace M, Bell BP, et al. The advisory committee on immunization practices' ethical principles for allocating initial supplies of COVID-19 vaccine - United States, 2020. Morb Mortal Wkly Rep. (2020) 69:1782–6. doi: 10.15585/mmwr.mm6947e3
36. Paul LA, Daneman N, Schwartz KL, Science M, Brown KA, Whelan M, et al. Association of age and pediatric household transmission of SARS-CoV-2 infection. J Am Med Assoc Pediatr. (2021) 175:1151–8. doi: 10.1101/2021.03.29.21254565
37. Larcher V, Dittborn M, Linthicum J, Sutton A, Brierley J, Payne C, et al. Young people's views on their role in the COVID-19 pandemic and society's recovery from it. Arch Dis Child. (2020) 105:1192–6. doi: 10.1136/archdischild-2020-320040
38. Endo A, Uchida M, Kucharski AJ, Funk S. Fine-scale family structure shapes influenza transmission risk in households: Insights from primary schools in Matsumoto city, 2014/15. PLoS Comput Biol. (2019) 15:e1007589. doi: 10.1371/journal.pcbi.1007589
39. Somekh I, Boker LK, Shohat T, Pettoello-Mantovani M, Simões EAF, Somekh E. Comparison of COVID-19 incidence rates before and after school reopening in Israel. J Am Med Assoc Netw Open. (2021) 4:e217105. doi: 10.1001/jamanetworkopen.2021.7105
40. Falk A, Benda A, Falk P, Steffen S, Wallace Z, Hoeg TB. COVID-19 cases and transmission in 17 K-12 Schools - Wood County, Wisconsin, August 31-November 29, 2020. Morb Mortal Wkly Rep. (2021) 70:136–40. doi: 10.15585/mmwr.mm7004e3
41. Buonsenso D, Roland D, De Rose C, Vasquez-Hoyos P, Ramly B, Chakakala-Chaziya JN, et al. Schools closures during the COVID-19 pandemic: a catastrophic global situation. Pediatr Infect Dis J. (2021) 40:e146–50. doi: 10.1097/INF.0000000000003052
42. Zhu Y, Bloxham CJ, Hulme KD, Sinclair JE, Tong ZWM, Steele LE, et al. A meta-analysis on the role of children in SARS-CoV-2 in household transmission clusters. Clin Infect Dis. (2020) 72:e1146–53. doi: 10.1101/2020.03.26.20044826
43. Li F, Li YY, Liu MJ, Fang LQ, Dean NE, Wong GWK, et al. Household transmission of SARS-CoV-2 and risk factors for susceptibility and infectivity in Wuhan: a retrospective observational study. Lancet Infect Dis. (2021) 21:617–28. doi: 10.1016/S1473-3099(20)30981-6
44. Ip DK, Lau LL, Leung NH, Fang VJ, Chan KH, Chu DK, et al. Viral shedding and transmission potential of asymptomatic and paucisymptomatic influenza virus infections in the community. Clin Infect Dis. (2017) 64:736–42. doi: 10.1093/cid/ciw841
Keywords: COVID-19, SARS-CoV-2, secondary transmission, attack rate, households, children
Citation: Tanaka ML, Marentes Ruiz CJ, Malhotra S, Turner L, Peralta A, Lee Y, Jumarang J, Perez SE, Navarro J, Dien Bard J, Gordon A, Allen EK, Thomas PG and Pannaraj PS (2022) SARS-CoV-2 Transmission Dynamics in Households With Children, Los Angeles, California. Front. Pediatr. 9:752993. doi: 10.3389/fped.2021.752993
Received: 04 August 2021; Accepted: 30 November 2021;
Published: 05 January 2022.
Edited by:
Danilo Buonsenso, Catholic University of the Sacred Heart, ItalyReviewed by:
Eli Somekh, Mayanei Hayeshua Medical Center, IsraelCopyright © 2022 Tanaka, Marentes Ruiz, Malhotra, Turner, Peralta, Lee, Jumarang, Perez, Navarro, Dien Bard, Gordon, Allen, Thomas and Pannaraj. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Pia S. Pannaraj, cHBhbm5hcmFqQGNobGEudXNjLmVkdQ==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.