- 1Ministry of Education Key Laboratory of Child Development and Disorders, Chongqing Key Laboratory of Pediatrics, National Clinical Research Center for Child Health and Disorders, Children's Medical Big Data Intelligent Application Chongqing University Engineering Research Center, Department of Emergency, Children's Hospital of Chongqing Medical University, Chongqing, China
- 2Ministry of Education Key Laboratory of Child Development and Disorders, Chongqing Key Laboratory of Pediatrics, National Clinical Research Center for Child Health and Disorders, Children's Medical Big Data Intelligent Application Chongqing University Engineering Research Center, Department of Hematology and Oncology, Children's Hospital of Chongqing Medical University, Chongqing, China
Objective: Acute poisoning in children is characterized by regional differences. This study described the basic situation of childhood poisoning in southwest China based on hospitalized cases.
Data and Methods: A total of 1,076 acute poisoning cases among hospitalized children admitted to Children's Hospital of Chongqing Medical University from January 2012 to December 2020 were included in this study. Clinical data such as gender, age, living environment, poisonous substance, and cause of poisoning were statistically described. Trends of length of hospital stay, population distribution, poisonous substances, and causes of acute poisoning in the hospitalized children were compared over time.
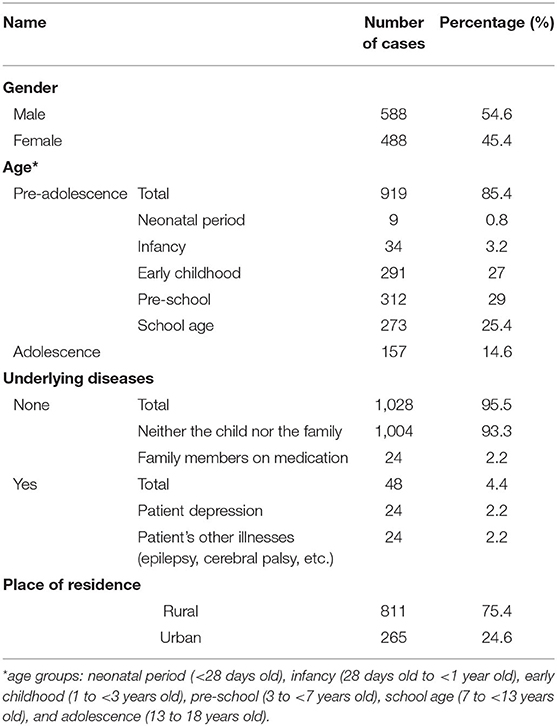
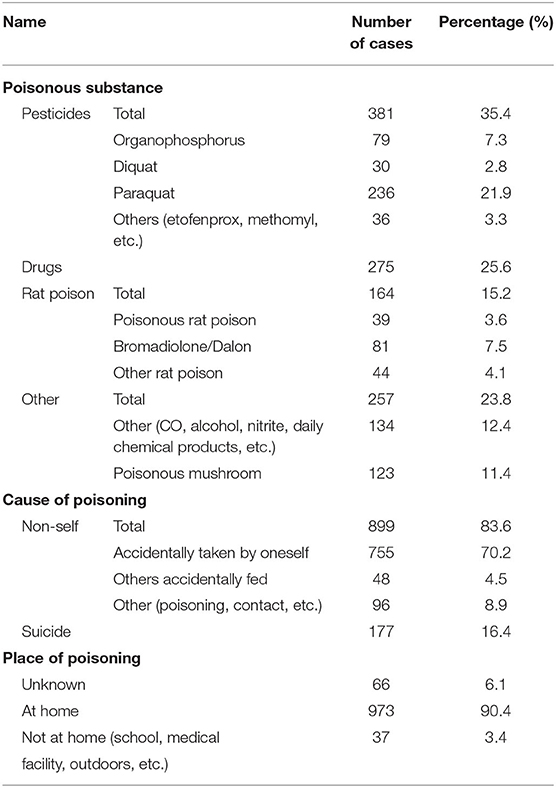
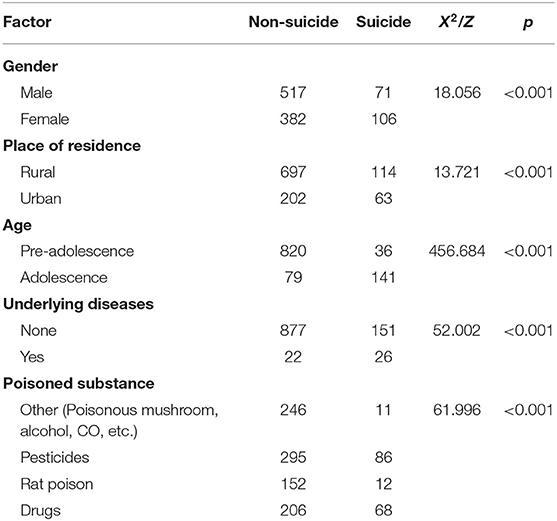
Results: The cohort comprised 588 males and 488 females; 811 cases lived in rural areas and the rest resided in urban areas. Most cases were between early childhood and school age. Poisoning usually occurred at home (973 cases, 90.4%). Pesticides (381 cases, 35.4%) and drugs (275 cases, 25.6%) were the two most common poisonous substances. Two main causes of poisoning were accidental taking (755 cases, 70.2%) and suicide (177 cases, 16.4%). The results of univariate analysis of suicide showed significant correlations among gender, place of residence, age, poisonous substance, and place of suicide (P < 0.001), while living environment (town), age (adolescence), and poisonous substance (pesticide, drug) were independent risk factors (P < 0.05). There was no significant change in the length of hospital stay for poisoning over time. The overall number of hospitalizations presented a decreasing trend, while the number of urban children gradually increased. The proportion of adolescent poisoned children and suicidal children increased in the last 3 years.
Conclusion: Optimizing the package and distribution channels of pesticides and drugs, raising safety awareness of children to avoid accidental injuries, and paying attention to children's mental health are measures that are necessary to prevent poisoning in children.
Introduction
Poisoning has been an important global public health issue, and acute poisoning is an important cause of unintentional injuries in children (1). Acute poisoning refers to a series of pathophysiological changes and relevant clinical manifestations in a short period of time after exposures to toxic substances or toxic doses of drugs. The consequences of acute poisoning are complex and change rapidly. Multiple organ dysfunction or failure can be observed in serious poisoning cases, which can be life-threatening (2). The World Health Organization (WHO) states that poisoning is one of the top five causes of death from unintentional injuries in children (3), and surveys from China also show that poisoning is one of the leading causes of death in Chinese children, ranking as high as the 3rd cause of accidental death (4). Despite numerous educational and public health campaigns aimed at avoiding childhood poisoning, poisoning remains the most common medical emergency among children. Children are more susceptible to serious injuries relative to adults due to their immature psychological and physical systems, lack of hazard awareness, and poor safety awareness and defense against poisons.
Acute childhood poisoning varies greatly from a global epidemiological perspective, with geography being a major factor for poisonous substances and risk factors (5). Some national epidemiological studies have been established in western countries, such as the European Association of Poisons Centers and Clinical Toxicologists (EAPCCT), Extracorporeal Treatments in Poisoning Work group (EXTRIP), National Poison Data System (NPDS), and the American Academy of Clinical Toxicology (AACT). Unfortunately, there remains a lack of large-scale, multicenter epidemiological data about the incidence of poisoning in Chinese populations, especially among children.
Children's Hospital of Chongqing Medical University is one of five national regional children's medical centers in China and the largest national tertiary class A children's specialty hospital in southwest China. Therefore, the acute poisoning cases from hospitalized children in this hospital are regionally representative. In this study, we included hospitalized children diagnosed with acute poisoning at the Children's Hospital of Chongqing Medical University from January 2012 to December 2020. We retrospectively analyzed their clinical characteristics, including length of hospital stay, poisoning population, poisoned substances, and causes of poisoning over time. This study is of significance for the prevention and control of acute poisoning in children.
Data and Methods
Selection of Research Subjects
Medical information of 1,101 hospitalized children diagnosed with acute poisoning from January 2012 to December 2020 at the Children's Hospital of Chongqing Medical University was collected from the hospital information management system. Twenty-five cases were excluded based on the following criteria: lack of clinical information, milder outpatient acute poisoning, non-acute poisoning, infectious poisoning, and poisonous insect and snake bites. All included subjects were <18 years old.
Research Method Design
The clinical data of 1,076 hospitalized children with acute poisoning were statistically described, including basic characteristics (age, gender, underlying diseases, distribution of residential area), place of poisoning, poisonous substances, and causes of poisoning. Univariate analysis and multivariate logistic regression analysis were used to analyze the poisoning characteristics of suicidal children. Trends in length of hospital stay, population distribution, poisonous substances, and causes of poisoning in hospitalized children with acute poisoning over the past 9 years were further compared.
Statistical Analysis
Data were analyzed using SPSS 22.0. Categorical variables are presented as cases/%. Ordinal and nominal categorical data were evaluated using rank sum test and Chi-square test, respectively. Enumeration variables are expressed as mean ± standard deviation. An independent sample t-test was used to compare two groups. One-way ANOVA was applied to compare differences among multiple groups assuming normal distribution, or the Kruskal-Wallis test was used when necessary. Bonferroni post-hoc test was performed for pair-wise comparisons. Univariate analysis was used for correlation factor analysis, followed by multi-factor logistic regression analysis. All results were considered statistically different at P < 0.05.
Results
Basic Characteristics of Hospitalized Children With Acute Poisoning
The basic characteristics of children enrolled in this study are summarized in Table 1. There were 588 males and 488 females, and the gender ratio was 1.2:1. The top three age groups of poisoning were early childhood, preschool, and school ages (291, 312, and 273 cases, respectively). Forty-eight cases were characterized by past history of underlying diseases, including 11 cases of depression and epilepsy. The number of children in rural areas was much higher than in urban areas.
Place of Poisoning, Poisonous Substances, and Cause of Poisoning
Poisoning accidents mainly occurred at home (90.4%), followed by other places, including schools (9 cases), health care facilities (10 cases), and outdoors (18 cases). The three most common poisonous substances were pesticides, drugs, and rat poisons. Paraquat poisoning (236 cases) was the most prominent, accounting for 21.9% of pesticide poisonings. Rodenticides were dominated by anticoagulants (dallon and bromadiolone). The most common cause of poisoning was accidental ingestion of poisonous substances. According to the characteristics of children, accidental ingestion was classified as self-inflicted and accidentally fed by others. Suicide was another cause of poisoning (Table 2).
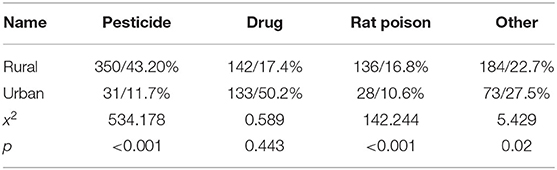
Pesticides and rodenticides were significantly higher in rural areas compared to urban areas (P < 0.001). The highest rates of pesticide poisoning were observed in rural areas, while the highest rates of drug poisoning were found in urban areas (Table 3).
Univariate analysis of poisoning characteristics of the 177 suicidal children showed that gender, residential area, age, previous history, and poisonous substances were all significantly associated with suicide (P < 0.001). The rate of suicide was higher in females than in males and increased with age. The rate of suicide was higher among those living in urban areas. Cases with basic/underlying diseases were characterized by a higher rate of suicide. Drugs and pesticides were the most prevalent poisonous substances (Table 4).
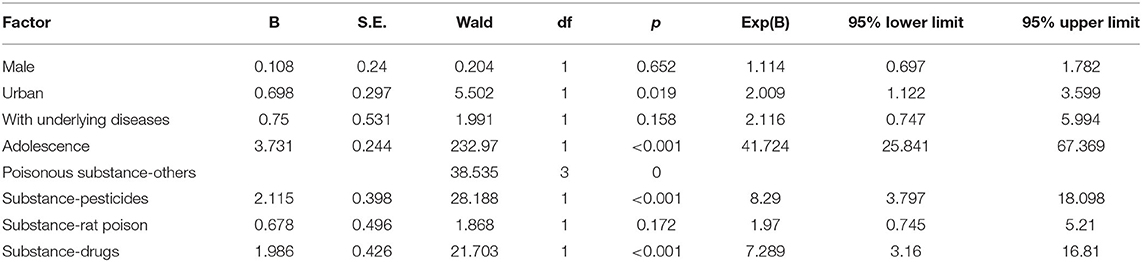
By performing the binary multifactorial logistic regression analysis of the poisoning characteristics of children who committed suicide, we found that residential areas (urban), age (adolescence), and poisonous substances (pesticides, drugs) were independent risk factors for suicide (Table 5).
Trends in Poisoning Characteristics From 2012 to 2020
Hospitalization Days
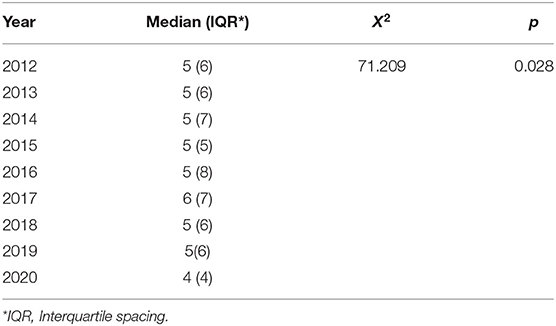
The number of hospitalization days is summarized in Table 6. The length of hospitalization stay from 2012 to 2020 was significantly different (P < 0.05).
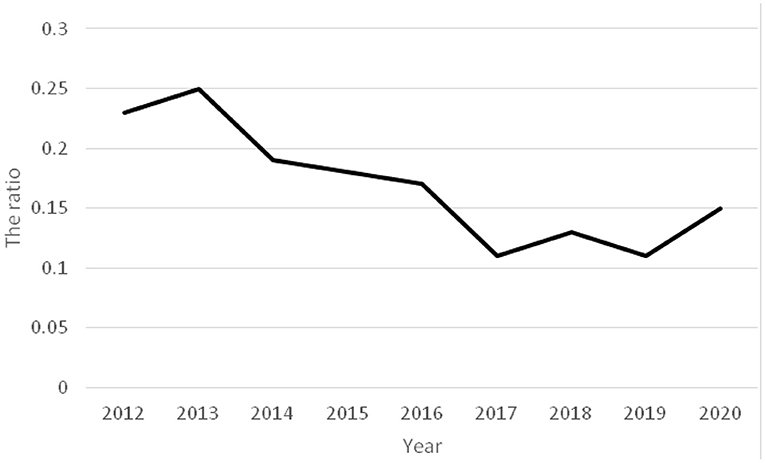
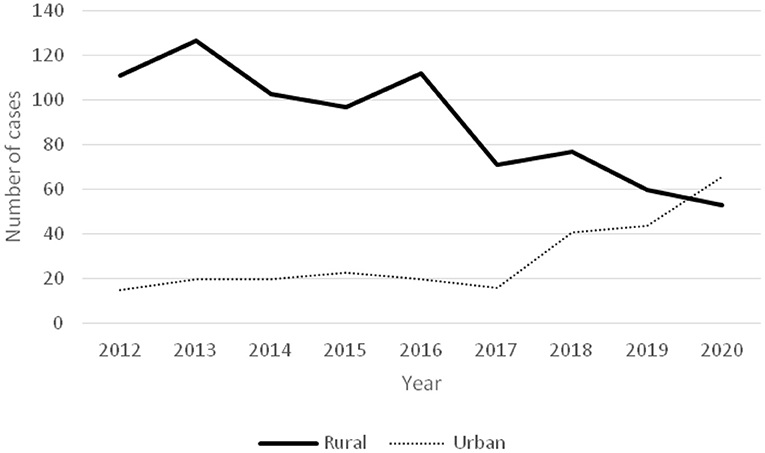
Number of Cases
The ratios of acute poisoning cases to total hospitalized children showed a decreasing trend from 2012 to 2020 (Figure 1). A gradual increase in the number of poisoning in children from urban areas was observed, while the number of cases in rural area decreased (Figure 2).
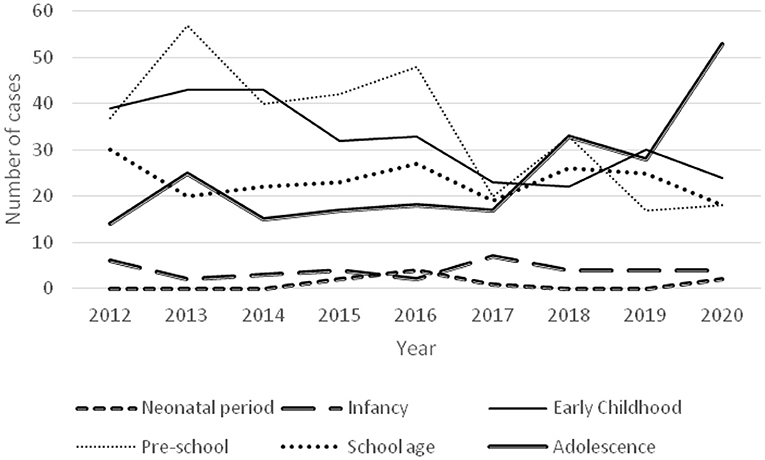
Age Group Distribution
The age distribution of poisoning was not significantly different from 2012 to 2017, but the proportion of poisoning in adolescent children increased from 2018 to 2020 (Figure 3).
Poisonous Substances
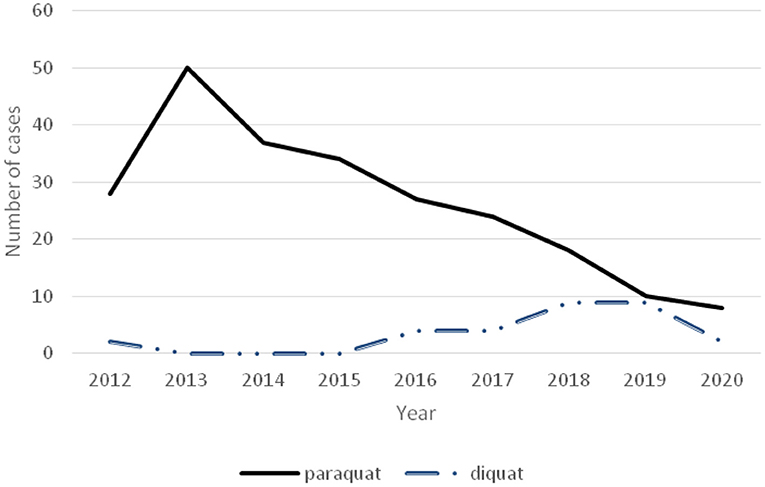
Pesticide poisoning showed a downward trend (Figure 4), accompanied by a decrease in the number of paraquat poisonings in recent years but an increasing number of diquat poisonings (Figure 5).
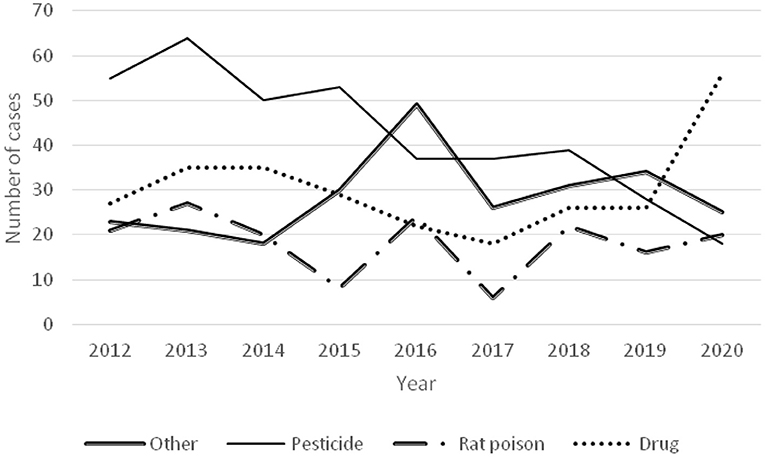
Figure 4. Time-varying curve of each poisoned substance and number of poisoned children in rural and urban areas.
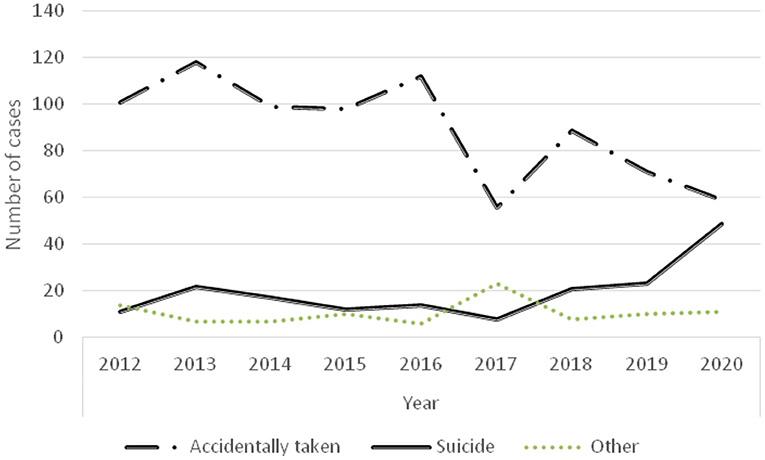
Causes of Poisoning
As shown in Figure 6, the number of children with accidental poisoning declined, but the number of poisoning cases by suicide increased in the last 3 years (Figure 6).
Discussion
Gender Ratio and Age Structure of Hospitalized Children With Acute Poisoning
There were 588 males and 488 females in hospitalized children with acute poisoning. This result may not only be related to the fact that boys are generally more curious and active, but also may be due to the higher proportion of males in hospitalized children (6). The traditional Chinese custom of giving preference to sons over daughters results in Chinese families paying more attention to the health of boys, especially in the poor rural areas where families are more willing prioritize treating males (7).
The age structure results showed that infants and preschoolers accounted for the highest numbers of poisoning, which is generally consistent with the literature (5). Children in these age groups are generally curious but lack the ability to judge hazards (8). Our findings show that the number of poisoning cases in adolescent children has been increasing, and poisoning in adolescent children was significantly associated with suicide.
Poisoning Caused by Pesticides, Drugs, and Other Products
The nature of substances causing acute poisoning in children varies in different countries and regions due to differences in national conditions, social status, and ethnicity. Drugs and household product poisoning are predominant in European and American countries (5). It has been documented that drug poisoning (chemical products and household cleaners) is most common in children aged 5 or younger, and there has been an increasing trend of opioids acute poisoning in children from 2005 to 2018 according to the US National Poison Data System (NPDS) (9). The Spanish Society of Pediatric Emergency Medicine Working Group on Poisoning evaluated 1,749 cases of poisoning children between 2008 and 2017, and the top three reported toxicants were drugs, household products, and alcohol (10). Drug poisoning is also the most predominant type of hospitalization for poisoning in aboriginal children in New South Wales (11). Acute poisoning in Iranian children aged 1–4 years old is predominantly drug-based (12). Pesticides are most commonly reported in developing agricultural countries such as India, China, South Africa, and Sri Lanka (13), which is consistent with the results of this study.
The number of poisoning cases was higher in children living in rural compared to urban areas. Pesticides have become the most common substance causing poisoning in rural areas, this is consistent with the relevant research results (4). Poisoning caused by herbicides and organophosphorus comprises the two major types of pesticide poisoning. Due to the ban of paraquat usage in China in 2016, the number of paraquat poisoning cases has sharply decreased. However, the number of poisoning caused by other types of herbicides has increased, such as diquat (which has a similar high toxicity and lethality rate as paraquat). Similar findings were reported in a Korean study (14). In addition, the number of cases of rat poisoning also increased. After the Chinese government explicitly banned the use of highly toxic rodenticides and promoted the use of anticoagulant rodenticides (bromadiolone and dalon), poisoning caused by anticoagulant rodenticides significantly increased compared with the previous ones. Reasons for poisoning could include poor economic and sanitary conditions in rural areas, low education of rural people, relatively weak safety awareness, and improper storage of pesticides. In our study, there were a few cases of children accidentally taking paraquat by pouring it into beverage bottles and storing it. There has also been an increase in the number of children in rural areas who lack parental care and supervision in recent years (15), which has greatly increased the risk of accidents. In several countries, it has been reported that there is a significant increase in accidental injuries among children who are cared for by someone other than their parents or those with low social status or level of education (13, 16–19). Moreover, Sri Lankan scholars found that the strongest risk factors for accidental poisoning of local children were improper supervision, working mothers, and improper storage of poisonous substances (13).
Accidental administration of drugs is the main cause of poisoning in children who live in towns or cities and have less chance of being exposed to pesticides. Our study showed that drug poisoning was predominantly caused by psychotropic, cardiovascular, and cold medicines. We also found that 72 children and/or families had chronic diseases requiring long-term drug use. These drugs can lead to accidental poisoning if they are placed where children can easily access them or if they are improperly administered.
Reducing poisoning from pesticides, drugs, and other products requires concerted efforts from many aspects. One aspect lies in strengthening regulation at the governmental and social levels. Others have reported serious poisoning cases caused by illegal sales of pesticides and drugs in small street stores (20–24). Therefore, relevant state departments should designate appropriate laws and regulations to emphasize design safety, control, and sales measures. For example, pesticide packaging should further emphasize its toxicity labeling, uses, and safe storage methods; food safety supervision should be strengthened to avoid the inflow of rat poison contaminated rice, noodles, and meat into the market; and “street pesticides” should be reduced by strengthening enforcement of illegal pesticides. However, there is limited evidence that environmental change interventions could reduce the risk of accidental poisoning in children (25, 26). Therefore, there is also a need to strengthen child safety awareness to avoid accidental poisoning.
With increased efforts to regulate highly toxic substances in China and improved medical care in primary care hospitals, the number of cases of hospitalized children who are poisoned has gradually decreased. The trend of changes in poisonous substances over the past 9 years showed that the number of children poisoned by pesticides decreased significantly and the number of children poisoned in rural areas also decreased. The reasons might be related to the strengthening of state regulation of pesticides and the improvement of people's knowledge about children's safety. The decreased number of children living in rural areas due to migration might also be contributing to the reduction of poisoning cases in rural areas (27).
Suicide Poisoning
In this study, the majority of suicide cases were adolescents and females, and the number of suicide cases was higher in urban areas. Some suicide cases had a history of depression, and all children had life or study disputes with family members, classmates, or teachers before committing suicide. The number of suicide poisonings increased over the last 3 years, including an increased number of adolescent poisoning (Figure 6). Previous researches have shown that heavy burden from study is very common in adolescents committed suicide by taking poison (28). The suicide rates of children are higher in urban areas compared to rural areas, which might be attributed to greater study pressure of urban children originated from more family educational investment. While problems surrounding the mental health of left-behind children are prominent among the poisoning children in rural areas, and it is more common for left-behind children who are lack of care and love for a long time become to be introverted, lonely, insecure, and easily go to extremes (15). Poisoning suicides among adolescent girls might be associated with an awakening of their sense of self, unstable emotions, increased pressure from studies, society, and even sexual relations. Meanwhile, females are more emotionally rich and less resistant to frustration than males (29). Scholars in Taiwan have reported that female adolescents are also at high risk of poisoning suicide (30). In this study, one female case committed suicide by taking medicine because of the long-term sexual abuse from her stepfather. This example emphasizes the need for more awareness of child sexual abuse and protecting underage females.
Chronic mental illnesses such as depression are more prominent among poisoning cases in children with underlying diseases, and some foreign scholars have suggested that chronic physical and mental illnesses are associated with an increased risk of self-harm and suicidal ideation. Measures to assess and intervene with this population should be developed to effectively prevent these poisoning outcomes (31, 32).
There are some limitations in our study. We only included hospitalized children who have suffered from acute poisoning who were severely ill. More statistical studies are needed for children who are non-severely ill in the outpatient setting and who are not hospitalized. In addition, this is only a 9-year retrospective study with a minority of missing or inaccurate data. Children's Hospital of Chongqing Medical University is the largest national 3A pediatric hospital in southwest China, so the data in this study is regional representative but may be different with data from primary medical institutions (33, 34).
Conclusions
Acute poisoning in children causes both familial and societal burdens. We call for state, school and family awareness of child poisoning to reduce risk of death and significant harm. First, we propose strengthening supervision at the governmental and social levels to reduce the unregulated circulation of pesticides and drugs. Secondly, we should reinforce the publicity of child safety knowledge and enhance the awareness of drug safety in families to protect children's health. Thirdly, there is an urgent call to focus on children's psychological safety, but there is a lack of professionals in child psychiatry in China who are qualified to treat the psychological defects of children with depression or suicide. In addition, the levels of medical care in primary hospitals vary, and the level of treatment for acute poisoning in children in some rural primary hospitals needs to be improved. These are key areas to address to reduce accidental poisoning in children in the future.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by the Institutional Review Board of Children's Hospital, Chongqing Medical University. Written informed consent from the participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author Contributions
ZL and LT designed the study. ZL, LX, LY, SL, and LT collected and analyzed the data. ZL, LX, and LT drafted the manuscript. Critically revising the article was done by ZL, LX, and LT. All authors read and approved the final manuscript.
Funding
This work was supported by 2019 Annual Philosophy and Social Science Projects of Chongqing Medical University (No. X9842).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2021.727900/full#supplementary-material
References
1. Pawłowicz U, Wasilewska A, Olański W, Stefanowicz M. Epidemiological study of acute poisoning in children: a 5-year retrospective study in the Paediatric University Hospital in Białystok, Poland. Emerg Med J. (2013) 30:712–6. doi: 10.1136/emermed-2012-201376
2. Chinese Medical Doctor Association Emergency Medic, Chinese Chinese Society of Toxicology Poisoning and Treatment. Chinese expert consensus on diagnosis and treatment of acute poisonin. Chin Crit Care Med. (2016) 28:966. doi: 10.3760/cma.j.cn121430-20210305-00338
3. Peden M, Oyegbite K, Ozanne-Smith J, Hyder AA, Branche C, Rahman AKMF, et al. World Report on Child Injury Prevention. Switzerland: WHO (2008).
4. Zhu YM, Wu Q. The current situation of acute poisoning in children. Chin Pediatr Emerg Med. (2018) 25:81–3. doi: 10.3760/cma.j.issn.1673-4912
5. Mintegi S, Azkunaga B, Prego J, Qureshi N, Dalziel SR, Arana-Arri E, et al. International epidemiological differences in acute poisoning in Pediatric Emergency Departments. Pediatr Emerg Care. (2019) 35:50–57. doi: 10.1097/PEC.0000000000001031
6. Howells K, Caple A, Jones M. Are boys more physically active than girls during a primary school day? Prim Phys Educ Matt. (2010) 5:17–9.
7. Liao L, Zhang C. Does the Son Preference Harm Girls' Health? Evidence from China Family Panel Studies. Econ Rev. (2020) 2:139–54. doi: 10.19361/j.er.2020.02.09
8. David C S. Why “accidents” are not accidental: Using psychological science to understand and prevent unintentional child injuries. Am Psychol. (2019) 74:1137–47. doi: 10.1037/amp0000487
9. Land ME, Wetzel M, Geller RJ, Kamat PP, Grunwell JR. Analysis of 207,543 children with acute opioid poisonings from the United States National Poison Data System. Clin Toxicol. (2019) 19:1–8. doi: 10.1080/15563650.2019.1691731
10. Santiago P, Bilbao N, Martinez-Indart L, Mintegia S, Azkunaga B. Epidemiology of acute pediatric poisonings in Spain: a prospective multicenter study from the Spanish Society of Pediatric Emergency Medicine. Eur J Emerg Med. (2020) 27:284–9. doi: 10.1097/MEJ.0000000000000661
11. Lee C, Hanly M, Larter N, Zwi K, Jorm L. Demographic and clinical characteristics of hospitalised unintentional poisoning in Aboriginal and non-Aboriginal preschool children in New South Wales, Australia: a population data linkage study. BMJ Open. (2019) 9:e022633. doi: 10.1136/bmjopen-2018-022633
12. Feiz Disfani H, Kamandi M, Mousavi SM, Sadrzadeh SM, Farzaneh R, Doolabi N, et al. Risk factors contributing to the incidence and mortality of acute childhood poisoning in emergency department: a hospital base case-control study. Epidemiol Hea. (2019) 2019:e2019016. doi: 10.4178/epih.e2019016
13. Dayasiri K, Jayamanne SF, Jayasinghe CY. Accidental and deliberate self-poisoning with medications and medication errors among children in Rural Sri Lanka. Emerg Med Int. (2020) 2020:1–8. doi: 10.1155/2020/9872821
14. Ham S, Min YG, Chae MK, Kim HH. Epidemiology and regional differences of acute poisonings of eight cities in Gyeonggi-do province in Korea using data from the National Emergency Department Information System of Korea. Clin Exp Emerg Med. (2020) 7:43–51. doi: 10.15441/ceem.19.014
15. Fan Y, Liu H, Li Y, Chang X. On survival patterns of left-behind children in China based on field survey. J Chin Soc Educ. (2020) 3:51–6.
16. Xavier DM, Cezar-Vaz MR, Bonow CA, Schimith MD. Work accidents with children and youth in a rural environment in southern Brazil. Rev Lat Am Enfermagem. (2020) 28:e3243. doi: 10.1590/1518-8345.3188.3243
17. Tobaiqy M, Asiri BA, Sholan AH, Alzahrani YA, Alkatheeri AA, Mahha AM. Frequency and management of acute poisoning among children attending an emergency department in Saudi Arabia. Pharmacy. (2020) 8:189. doi: 10.3390/pharmacy8040189
18. Berta GN, Di Scipio F, Bosetti FM, Mognetti B, Romano F, Carere ME, et al. Childhood acute poisoning in the Italian North-West area: A six-year retrospective study. Ital J Pediatr. (2020) 46:83. doi: 10.1186/s13052-020-00845-0
19. Nevriana A, Pierce M, Dalman C, Wicks S, Hasselberg M, Hope H, et al. Association between maternal and paternal mental illness and risk of injuries in children and adolescents: nationwide register based cohort study in Sweden. BMJ. (2020) 369:m853. doi: 10.1136/bmj.m853
20. Gholami N, McDonald R, Farnaghi F, Hosseini Yazdi M, Zamani N, Hassanian-Moghaddam H. Fatal outcome in acutely poisoned children with hospitalization: a 10-year retrospective study from Tehran, Iran. Pediatr Emerg Care. (2021). doi: 10.1097/PEC.0000000000002429. [Epub ahead of print].
21. Vilaça L, Volpe FM, Ladeira RM. Accidental poisoning in children and adolescents admitted to a referral toxicology department of a Brazilian emergency hospital. Rev Paul Pediatr. (2019) 38:e2018096. doi: 10.1590/1984-0462/2020/38/2018096
22. Pascale A, Laborde A. Impact of pesticide exposure in childhood. Rev Environ Health. (2020) 35:221–7. doi: 10.1515/reveh-2020-0011
23. Chartier C, Penouil F, Blanc-Brisset I, Pion C, Descatha A, Deguigne M. Pediatric cannabis poisonings in France: more and more frequent and severe. Clin Toxicol. (2021) 59:326–33. doi: 10.1080/15563650.2020.1806295
24. Rice NC, Rauscher NA, Moffett MC, Myers TM. Organoleptic assessment and median lethal dose determination of oral aldicarb in rats. Ann N Y Acad Sci. (2020) 1480:136–45. doi: 10.1111/nyas.14448
25. Bhatta S, Mytton J, Deave T. Environmental change interventions to prevent unintentional home injuries among children in low-and middle-income countries: A systematic review and meta-analysis. Child Care Health Dev. (2020) 46:537–51. doi: 10.1111/cch.12772
26. Benaboud J, Elachour M, Oujidi J, Chafi A. Farmer's behaviors toward pesticides use: insight from a field study in Oriental Morocco. Environ Anal Health Toxicol. (2021) 36:e2021002. doi: 10.5620/eaht.2021002
27. Su H, Wei H. Immigration potential and urban growth. China Soft Sci. (2020) 8:78–90. doi: 10.3969/j.issn.1002-9753.2020.08.008
28. Ye M, Hu Y, He C, Dong C, Yang Y, Lu Z. The psychological experience of juvenile poisoning suicide patients: a qualitative study. Chin J Nurs. (2021) 56:250–4. doi: 10.3761/j.issn.0254-1769.2021.02.015
29. Silvia LL, Paula M, Vanesa SS. Exploring the relationship between interparental conflict and emotional security: What happens with adolescents in residential care compared to those living with their families? Child Youth Serv Rev. (2019) 101:123–30. doi: 10.1016/j.childyouth.2019.03.054
30. Lee J, Fan NC, Yao TC, Hsia SH, Lee EP, Huang JL, et al. Clinical spectrum of acute poisoning in children admitted to the pediatric emergency department. Pediatr Neonatol. (2019) 60:59–67. doi: 10.1016/j.pedneo.2018.04.001
31. Forte A, Vichi M, Ghirini S, Orri M, Pompili M. Trends and ecological results in suicides among Italian youth aged 10-25 years: A nationwide register study. J Affect Disord. (2021) 282:165–72. doi: 10.1016/j.jad.2020.12.142
32. Abdel Baseer KA, Gad EF, Abdel Raheem YF. Clinical profile and outcome of acute organophosphate poisoning in children of Upper Egypt: a cross-sectional study. BMC Pediatr. (2021) 21:98. doi: 10.1186/s12887-021-02563-w
33. Su Y, Liu L. Relationship between Family's socioeconomic status and parental investments in early learning: evidence from the China family panel studies. Peking U Educ Rew. (2020) 18:86–103. doi: 10.12088/pku671-9468.202003004
Keywords: children, acute poisoning, pesticides, drugs, suicide
Citation: Li Z, Xiao L, Yang L, Li S and Tan L (2021) Characterization of Acute Poisoning in Hospitalized Children in Southwest China. Front. Pediatr. 9:727900. doi: 10.3389/fped.2021.727900
Received: 20 June 2021; Accepted: 08 October 2021;
Published: 10 December 2021.
Edited by:
Rouhullah Dehghani, Kashan University of Medical Sciences, IranReviewed by:
Nihar Ranjan Mishra, All India Institute of Medical Sciences, Kalyani (AIIMS Kalyani), IndiaCihad Dundar, Ondokuz Mayis University, Turkey
Copyright © 2021 Li, Xiao, Yang, Li and Tan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Liping Tan, dGFubHAwODI1QGhvdG1haWwuY29t
 Zhu Li
Zhu Li Li Xiao2
Li Xiao2 Lin Yang
Lin Yang