
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Pediatr. , 05 August 2021
Sec. Neonatology
Volume 9 - 2021 | https://doi.org/10.3389/fped.2021.691146
Left posterior fascicular ventricular tachycardia (LPFVT) is extremely rare in neonates. We described a 17-day-old girl with LPFVT who was initially misdiagnosed as supraventricular tachycardia (SVT). Eventually, she was successfully treated by amiodarone infusion followed by oral amiodarone with propranolol for 9 months, and LPFVT spontaneously resolved after a 1-year follow-up. This case report illustrated the basic principles and caveats in differential diagnosis of LPFVT in the neonatal age group. With proper diagnosis and therapy, neonatal LPFVT might regress in the first year of life.
Left posterior fascicular ventricular tachycardia (LPFVT) is extremely rare in newborns. To the best of our knowledge, only three neonatal cases have been reported in the literature since LPFVT was firstly described by Belhassen et al. in 1981 (1–4). LPFVT is frequently misdiagnosed as supraventricular tachycardia (SVT) in clinical practice because the QRS duration is slightly prolonged during tachycardia, particularly in infants. In this case report, we described a 17-day-old girl with recurrent LPFVT, focusing on the electrocardiogram (ECG) recognition, management, and prognosis of this type of arrhythmia in neonatal age group.
A premature female newborn was delivered at a gestational age of 35+4 weeks in a local hospital, with birth weight of 2,410 g. She was transferred to NICU in our institution. On the 17th day after birth, tachycardia was identified by the monitor. A 12-lead electrocardiogram (ECG) demonstrated a regular tachycardia with a heart rate of 210 beats per minute (bpm), a slightly wide QRS duration of 72 ms, a superior QRS axis of 223°, and a right bundle branch block pattern (RBBB) (Figure 1). She was initially presumed to have SVT. The echocardiography showed a structurally normal heart with a patent foramen ovale and normal cardiac function. Ice dunking followed by three boluses of adenosine triphosphate (ATP) injection to a maximum dose of 0.5 mg/kg was unsuccessful in terminating the tachycardia. Thereafter, electrical cardioversion was tried and failed to revert the rhythm to sinus. She remained hemodynamically stable, and intravenous amiodarone infusion at a full dose of 15 mcg/kg/min was started. During continuous amiodarone infusion, ECG revealed atrioventricular (AV) dissociation, occasional capture beats, and fusion beats (Figure 2). The sinus rhythm with normal AV conduction and narrow QRS duration of 62 ms was achieved 6 h later (Figure 3). By then, a diagnosis of LPFVT was established by reviewing all ECG strips. Non-sustained tachycardia recurred when intravenous amiodarone was gradually weaned off. The patient was discharged on oral amiodarone (5 mg/kg/day) with propranolol (2 mg/kg/day), despite that non-sustained episodes of LPFVT were documented by Holter. At 2 months of age, the girl was admitted to the emergency room for sustained LPFVT over 1 h. Tachycardia was successfully terminated by electrical cardioversion, and the medication dose for prophylaxis arrhythmia was increased proportionally to her weight increment. She was closely followed up by Holter every 4–8 weeks, and there was no recurrence of LPFVT after 6 months. Anti-arrhythmia medications were discontinued at 9 months. Her liver function and thyroid function were assessed every 3 months prior to discontinuation of medication and were within the normal range. Her last Holter evaluation at 13 months of age was completely normal. The timeline of diagnosis and therapy of LPFVT in this neonatal case are set out in Table 1.
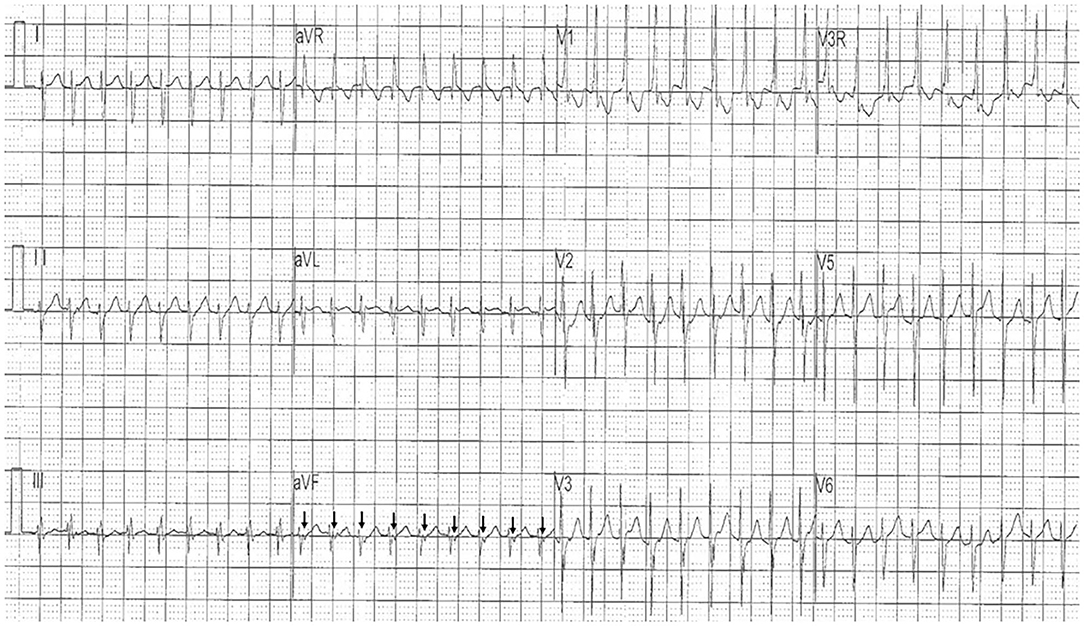
Figure 1. The initial 12-lead electrocardiogram showed regular tachycardia with a heart rate of 210 bpm, a slightly wide QRS duration of 72 ms, a superior QRS axis of 223°, and a right bundle branch block (RBBB) pattern. Reverse P′ waves (arrow) were identified in lead aVF, indicating the presence of 1:1 ventriculoatrial (VA) retrograde conduction.
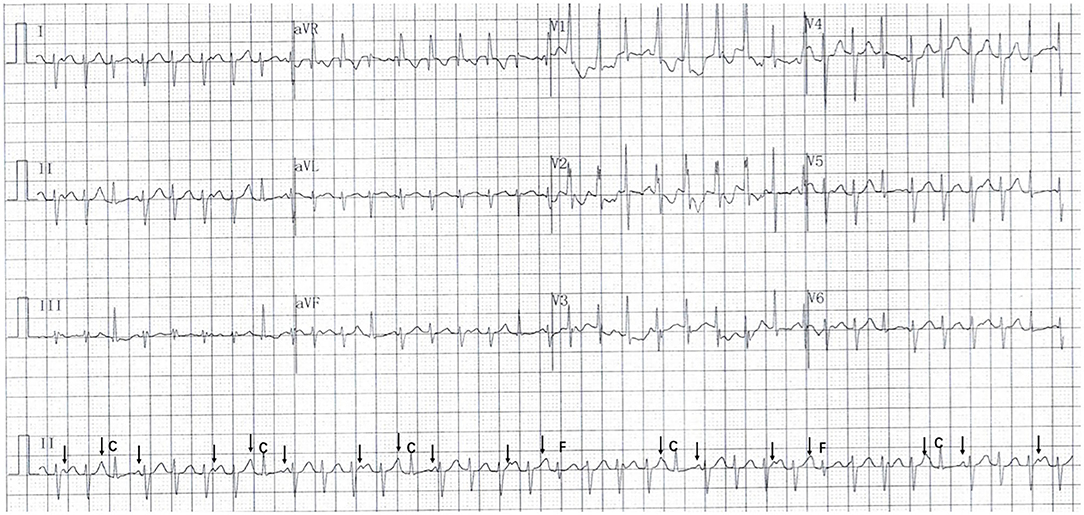
Figure 2. The electrocardiogram following amiodarone infusion revealed atrioventricular (AV) dissociation (arrow), capture beats (C), and fusion beats (F).
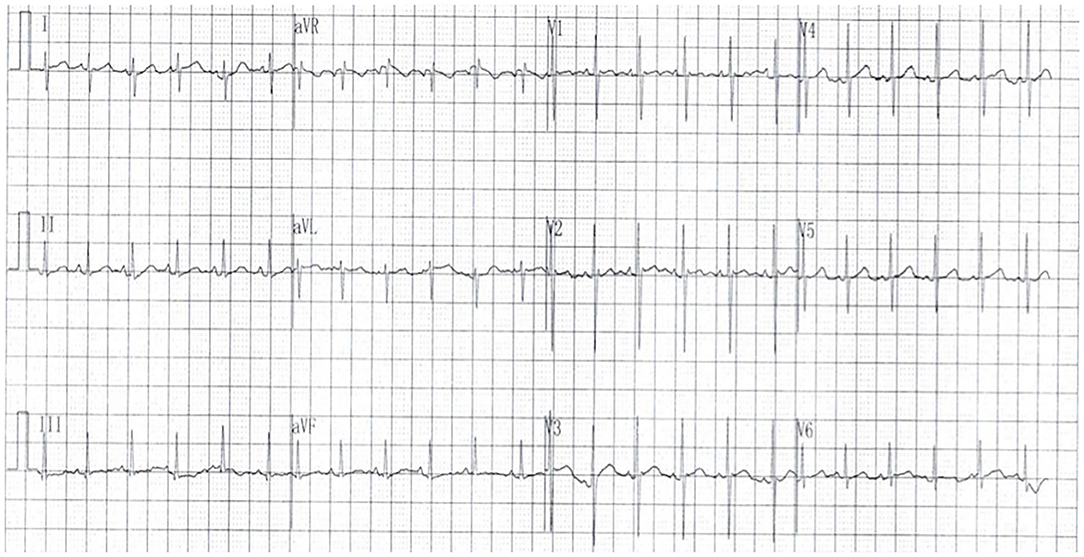
Figure 3. The 12-lead electrocardiogram showed sinus rhythm with a normal QRS duration of 62 ms, and a QRS axis of 72°.
Fascicular ventricular tachycardia (VT) is a form of idiopathic and Purkinje-related arrhythmia and is rarely reported in newborns. LPFVT is the most common form of fascicular VT, originating in the left posterior fascicle (5, 6).
The typical ECG pattern of LPFVT is characterized by right bundle branch block and superior axis deviation. The QRS morphology is mildly widened during tachycardia. It is often misdiagnosed as SVT with RBBB and left anterior hemiblock aberrancy. In the published literatures, the initial misdiagnosis rate of LPFVT in young infants is as high as 40% (2–4, 7–11). Therefore, we would like to demonstrate the basic principles and caveats in differential diagnosis of LPFVT in the neonatal age group by reviewing the present case. Firstly, VT in neonates is rare but does occur. It is important to bear in mind that the upper limit of normal QRS duration is 65 ms in neonates (12). In the present case, QRS duration during tachycardia was 72 ms, which exceeded the normal range. The diagnosis of VT should therefore be assumed. Secondly, AV dissociation, capture beats, and fusion beats during tachycardia are diagnostic markers of VT, but these studies are not usually present in neonates due to the rapid ventricular rate and presence of ventriculoatrial (VA) retrograde conduction. In reviewing the initial ECG strip of this case, the reverse P′ wave during VT was recognized, which indicated VA retrograde conduction. AV dissociation, capture beats, and fusion beats were identified during amiodarone infusion. Thirdly, LPFVT does not respond to adenosine (2, 8, 13), while other types of wide QRS tachycardia, which need to be differentiated from VT, including SVT with bundle branch block and SVT with anterograde conduction across an accessory pathway, can usually be terminated by adenosine. Thus, if adenosine injection is not effective in reverting presumed SVT, possibility of LPFVT should be considered.
The experience in management of infantile LPFVT is very limited. Verapamil is most commonly used in older children and has been shown to terminate tachycardia in 93% of children with LPFVT (13). However, its use in infants is widely considered to be contraindicated due to the risk of hemodynamic collapse (14). Beta blockers, amiodarone, and electrical cardioversion are usually recommended. Electrical cardioversion could achieve termination of LPFVT in 62% of children, and the effective rate of amiodarone infusion is not clearly known (13–15). In our neonatal case, LPFVT did not respond to electrical cardioversion, while it was reverted to sinus rhythm by amiodarone infusion. Oral amiodarone with propranolol had been given for 9 months to prevent recurrence until LPFVT regressed. Verapamil has recently been used for arrhythmia in infants (2, 16, 17). Slow intravenous infusion at a dose of 0.1 mg/kg over at least 10 min appeared to be safe and efficient in terminating infantile LPFVT, but only one newborn was enrolled (2, 7, 9, 11).
LPFVT is often considered to be a type of idiopathic VT with good prognosis, but delayed diagnosis and therapy can result in severe cardiac dysfunction (8). The eventual resolution of LPFVT in our neonatal case is consistent with the previous report by Collins et al., which showed that LPFVT occurring in the first year of life may resolve spontaneously (13).
This illustrative case report describes a neonate with LPFVT that was initially misdiagnosed as supraventricular tachycardia. The clinical course highlights the caveats of differential diagnosis in neonatal ECG evaluation and the favorable outcome of LPFVT. With proper diagnosis and treatment, LPFVT may regress over time within the first year of life.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Written informed consent was obtained from the minor(s)' legal guardian/next of kin for the publication of any potentially identifiable images or data included in this article.
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We are grateful to Thomas Yang from The Graduate School of Biomedical Sciences, Icahn School of Medicine at Mount Sinai, New York, NY, USA, who helped us edit and polish the English grammar for this article.
1. Belhassen B, Rotmensch HH, Laniado S. Response of recurrent sustained ventricular tachycardia to verapamil. Br Heart J. (1981) 46:679–82. doi: 10.1136/hrt.46.6.679
2. Kehr J, Binfield A, Maxwell F, Hornung T, Skinner JR. Fascicular tachycardia in infancy and the use of verapamil: a case series and literature review. Arch Dis Child. (2019) 104:789–92. doi: 10.1136/archdischild-2018-315617
3. Yilmaz FH, Oflaz MB, TarakÇI N, GÜLtekIN ND, Altunhan H. A rare arrhythmia in the newborn: posterior fascicular ventricular tachycardia. Eur Res J. (2020) 6:362–4. doi: 10.18621/eurj.592503
4. Young M-L, Flores L. Asymptomatic idiopathic belhassen ventricular tachycardia in a neonate detected using ‘smart sock’ wearable smartphone-enabled cardiac monitoring. Am J Case Reports. (2020) 21:e921092-1. doi: 10.12659/ajcr.921092
5. Kapa S, Gaba P, DeSimone CV, Asirvatham SJ. Fascicular ventricular arrhythmias: pathophysiologic mechanisms, anatomical constructs, and advances in approaches to management. Circ Arrhythm Electrophysiol. (2017) 10:e002476. doi: 10.1161/CIRCEP.116.002476
6. Kobayashi Y. Idiopathic ventricular premature contraction and ventricular tachycardia: distribution of the origin, diagnostic algorithm, and catheter ablation. J Nippon Med Sch. (2018) 85:87–94. doi: 10.1272/jnms.2018_85-14
7. Wang JD, Fu YC, Jan SL, Chi CS. Verapamil sensitive idiopathic ventricular tachycardia in an infant. Jpn Heart J. (2003) 44:667–71. doi: 10.1536/jhj.44.667
8. Snyder C, Bishara J, Darling R, Lucas V. Verapamil-sensitive ventricular tachycardia in an infant. Congenit Heart Dis. (2006) 1:124–6. doi: 10.1111/j.1747-0803.2006.00020.x
9. Hiremath G, Li W, Foltz R, Roy-Burman A, Cocalis M, Tanel RE. Verapamil-sensitive idiopathic left ventricular tachycardia in a 6-month-old: unique considerations in diagnosis and management in an infant. Pediatr Emerg Care. (2015) 31:50–3. doi: 10.1097/PEC.0000000000000307
10. Sriram CS, Gonzalez MD, Aggarwal S. Left posterior fascicular ventricular tachycardia in a young infant with a structurally normal heart: clinical course and caveats to electrocardiographic diagnosis. J Electrocardiol. (2020) 64:85–90. doi: 10.1016/j.jelectrocard.2020.12.003
11. Verma S, Gouthami V, Rao HB. Incessant fascicular ventricular tachycardia in an infant with heart failure. Ann Pediatr Cardiol. (2020) 13:153–6. doi: 10.4103/apc.APC_82_19
12. Galli MA, Danzi GB. Normal parameters of pediatric ECGs. In: A Guide to Neonatal and Pediatric ECGS. Springer: Science & Business Media (2013). p. 57. doi: 10.1007/978-88-470-2856-2_2
13. Collins KK, Schaffer MS, Liberman L, Saarel E, Knecht M, Tanel RE, et al. Fascicular and nonfascicular left ventricular tachycardias in the young: an international multicenter study. J Cardiovasc Electrophysiol. (2013) 24:640–8. doi: 10.1111/jce.12105
14. Brugada J, Blom N, Sarquella-Brugada G, Blomstrom-Lundqvist C, Deanfield J, Janousek J, et al. Pharmacological and non-pharmacological therapy for arrhythmias in the pediatric population: EHRA and AEPC-Arrhythmia Working Group joint consensus statement. Europace. (2013) 15:1337–82. doi: 10.1093/europace/eut082
15. Pfammatter J-P, Paul T. Idiopathic ventricular tachycardia in infancy and childhood. J Am Coll Cardiol. (1999) 33:2067–72. doi: 10.1016/s0735-1097(99)00105-9
16. LaPage MJ, Bradley DJ, Dick M. Verapamil in infants: an exaggerated fear? Pediatr Cardiol. (2013) 34:1532–4. doi: 10.1007/s00246-013-0739-8
Keywords: neonate, infant, arrhythmia, tachycardia, fascicular ventricular tachycardia
Citation: Zhao L, Wu L, Zhao Q-m and Liang X-c (2021) Case Report: Recurrent Left Posterior Fascicular Ventricular Tachycardia in a Newborn. Front. Pediatr. 9:691146. doi: 10.3389/fped.2021.691146
Received: 05 April 2021; Accepted: 05 July 2021;
Published: 05 August 2021.
Edited by:
Anne Lee Solevåg, Oslo University Hospital, NorwayReviewed by:
Stefan Kurath-Koller, Medical University of Graz, AustriaCopyright © 2021 Zhao, Wu, Zhao and Liang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lin Wu, d3VsaW4wNjA5QGZveG1haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.