- 1Department of Pediatrics, Dezhou People's Hospital, Dezhou, China
- 2Department of Pediatrics, Laoling People's Hospital, Laoling, China
- 3Department of Pediatrics, Xiajin County People's Hospital, Dezhou, China
Introduction: Undernutrition, defined as stunting, wasting, and underweight, still implicates millions of infants and children worldwide. Micronutrients have pivotal effects on growth rate. The outcomes of vitamin D deficiency on undernutrition indices have stayed controversial. The object of current study is to answer this question: is there any association between vitamin D status and undernutrition indices?
Methods: The international databases were used for a systematic search to identify relevant observational studies in English up to January 2021. A random-effect model was applied to combine the results of included essays.
Results: Among 3,400 citations, 7 observational studies (4 cohorts and 3 cross-sectional) were eligible to enter in meta-analysis. Analysis of the lowest 8,295 children indicated that low vs. high serum level of vitamin D is directly associated with a higher risk of wasting (Summary Risk Estimate: 1.30; 95% CI: 1.04, 1.62; I2 = 0%). However, there is no significant association between vitamin status and risk of stunting (Summary Risk Estimate: 1.10; 95% CI: 0.72, 1.70; I2 = 81.6%) and underweight (Summary Risk Estimate: 1.12; 95% CI: 0.81, 1.56; I2 = 49.2%).
Conclusion: When comparing low and high serum vitamin D concentration categories, there is an inverse link between vitamin D status and wasting, but no relationship with stunting as well as underweight. However, further prospective and trial studies are required to deepen our understanding of these associations.
Introduction
Children undernutrition (including wasting, stunting, and underweight) is still a serious challenge and puts medical, social, and economic burden, particularly in developing countries. It is estimated that the number of stunted and wasted children are 144 (21.3%) and 47 (6.9%) million worldwide, respectively. Notably, the prevalence of undernutrition is roughly double in low and middle-income countries (1–3). The risk of morbidity and mortality is more significant in children with undernutrition so that the etiology of about 45% of children mortality could be attributed to undernutrition (1, 4). These children usually experience cognitive and motor impairments, growth retardation, and weaker school performance (4, 5). Widespread factors contribute to malnutrition, such as genetic agents, political position, low socioeconomic status, infections, and inadequate dietary intake (5, 6).
Several former studies established the role of some micronutrients such as vitamin A, zinc, iron, and vitamin D in growth rates (7, 8). Although vitamin D's role in the metabolism of calcium and phosphorous and, consequently, skeletal growth has been proven in previous studies (9, 10), recent research has found biological functions. For example, there is an interaction between vitamin D and growth hormone (9, 10). Vitamin D inadequacy as a common nutritional deficiency is rarely diagnosed (11). The increase of vitamin D deficiency has been a big problem for global public health (12, 13).
Several investigations have explored the association of vitamin D status with undernutrition indices in children but have announced incongruous results (14–20). For instance, a survey on undernutrition indices in a cohort of HIV-exposed, uninfected infants concluded that vitamin D deficiency might increase the chance of wasting, while it did not observe any association with stunting and underweight (20).
Due to no research has elucidated this controversy, this systematic review and meta-analysis of published observational papers were performed to summarize findings regarding the association between vitamin D status and risk of wasting, stunting, and underweight in children.
Method
This meta-analysis was conducted on essays that evaluated the link between serum vitamin D status and undernutrition as stunting, wasting, and underweight, among infants and children. The serum level of 25(OH) vitamin D was considered as a biomarker. This review was reported based on the Preferred Reporting Items of Systematic Reviews and Meta-Analysis (PRISMA) statement guidelines (21).
Search Strategy
The databases of PubMed and Scopus were searched to identify relevant articles published up to January 2021. The studies with an observational design that met inclusion criteria were enrolled to be analyzed. The search terms [Medical Subject Heading (MeSH) and non-MeSH terms] were the following items: Vitamin D OR Cholecalciferol OR ergocalciferol OR 25-hydroxyvitamin D OR 25(OH)D OR 1-alpha hydroxyvitamin D3 OR 1,25 dihydroxyvitamin D3 OR 1,25 dihydroxycholecalciferol OR 25 hydroxycholecalciferol OR 25 hydroxyvitamin D OR calcitriol in combination with stunting OR wasting OR underweight OR thinness OR leanness OR stunted growth. If there was missing data in included studies, we contacted the author by email. Google Scholar databases and references of included essays and relevant reviews were also checked to find any missed study.
Inclusion and Exclusion Criteria
Studies that had an observational design (cohort, cross-sectional, or case-control studies), conducted on children aged under 12 years, and reported sufficient data [hazard ratio (HR), relative risk (RR), and odds ratio (OR) with corresponding 95% CIs] regarding the association of serum vitamin D status and risk of wasting, stunting, and underweight were included. Studies with the following features were excluded: (1) adult population; (2) dietary vitamin D intake; (3) animal studies; (4) no English essays; (5) review articles, commentary, editorial, or letter; (6) intervention studies; (7) studies that had subjects with chronic diseases such as cancer, cystic fibrosis, and other conditions; (8) reporting the correlation coefficient instead of estimate risk.
Quality Assessment
The valid tool of the Newcastle–Ottawa Scale (NOS) was used to ascertain the risk of bias of included essays (22). The total score of NOS is in the range of 0–9. If one study gets a score of ≥6, it is considered as high quality. The process of study qualification was performed by two independent researchers. If there was any discrepancy, researchers made the final decision by consultation and consensus.
Data Extraction and Abstraction
A pre-made form was used by two researchers independently to extract the required data. The following data were extracted: name of the first author, date of publication, study design, follow-up duration (in prospective cohort studies), sample size, age, gender, geographic situation, serum vitamin D assessment method, and outcome evaluating approach.
Statistical Analysis
The random-effects model was used to calculate estimated risk with 95% CIs to compare the highest and lowest serum level of vitamin D. The inverse variance method was applied to compute the standard error (SE) value of the logarithmic OR/HR/RR for each essay, and the estimated variance of the logarithmic RR was used to assess the weight of each study. I2 test was applied to assess heterogeneity between included studies. The I2 values of 25–50%, 50–75%, and >75% were considered as low, moderate, and high between-study heterogeneity, respectively (23). Subgroup analysis was conducted to identify source of heterogeneity according to the following variables: study design, participant age range, number of cases, and serum vitamin D assessment tool. For evaluating publication bias, the funnel plot and egger test were used (24). To examine the effect of one by one of the included studies on overall results, a sensitivity analysis was applied. All statistical analyses were done using STATA software version 15.1 (Stata Corporation, College Station, Texas, USA). The P-value under 0.05 was presumed as significant.
Results
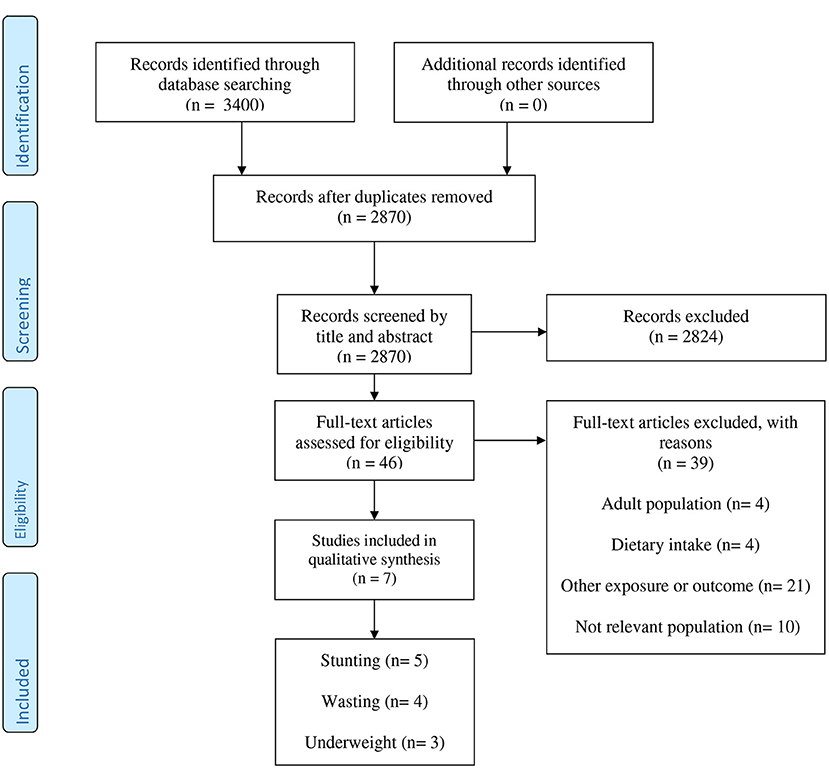
A total of 3,400 records were found by a systematic search that 2,870 remained after removing duplicates (Figure 1). After evaluating essays based on the title and abstract, 2,824 publications were excluded. Among 46 remained publications, 39 papers were excluded for the following reasons: adult population (n = 4), dietary intake (n = 4), assessing other exposure or outcome (n = 21), and not relevant population (n = 10).
Finally, seven observational studies (4 cohort and 3 cross-sectional studies) were opted for the systematic review and meta-analysis (14–20). The demographic information of eligible studies has been featured in Table 1. The studies were published between 2015 and 2020 and they were carried out in Tanzania (17, 20), Iran (15, 16), India (18, 19), and Ecuador (14). A total number of 7,624 persons participated in the studies, some of who were stunted (n = 1,349), wasted (n = 505), and underweight (n = 417). Two studies were conducted in infants (5–7 weeks) (17, 20) and five studies were performed in children between 6 months and 9 years old (14–16, 18, 19). Serum vitamin D was assessed by HPLC tandem MS (n = 2) (17, 20), and chemiluminescence immunoassay (n = 5) (14–16, 18, 19). The studied defined different cut-points for vitamin D deficiency, so that three of them considered serum 25(OH)D <10 ng/ml (15, 16, 18, 20), one considered 25(OH)D <12 ng/ml (19), one considered 25(OH)D <20 ng/ml (17), and other one 25(OH)D <17 ng/ml (20) as vitamin D deficiency. Stunting, wasting, and underweight was defined as a Length-for-age z score (LAZ), weight-for-length z score (WLZ), and weight-for-age z score (WAZ) of 2 or more SDs below the WHO population median, respectively. However, in one study, wasting was defined as BMI-for-age Z-score < −1 SD (15), and in another study, stunting considered as a Height-for-age Z-score of < -1 SD (16). All of the included essays had high methodological quality (score ≥ 6) (Supplementary Table 1).
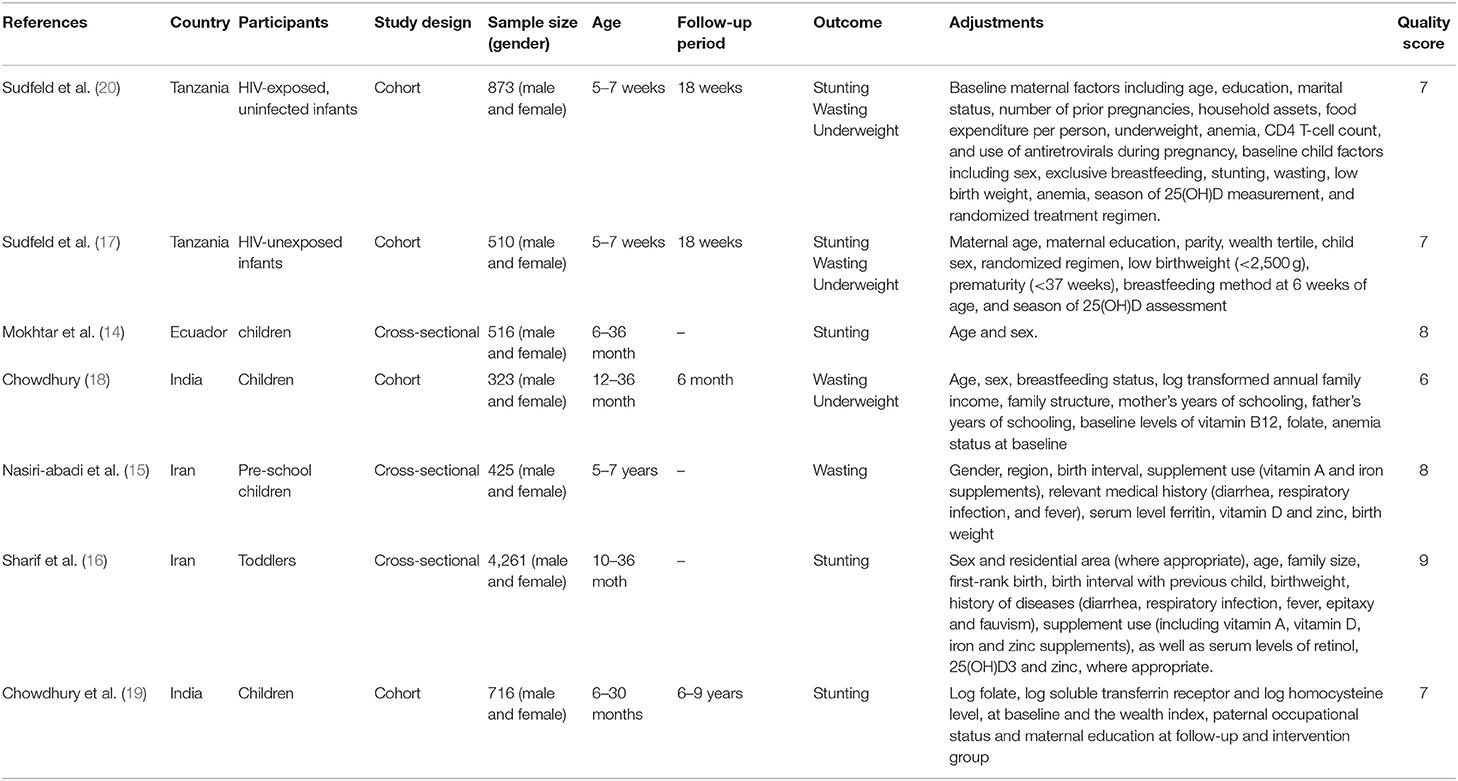
Table 1. Characteristics of observational studies eligible in the systematic review and meta-analysis.
Meta-Analysis
The Association of Serum Vitamin D Status With Risk of Wasting
Four studies were included in the analysis of lowest vs. highest serum vitamin D concentrations and risk of wasting (15, 17, 18, 20). Participants with the lowest serum vitamin D concentrations showed a significantly elevated risk of wasting compared to participants in the lowest group (Summary Risk Estimate: 1.30; 95% CI: 1.04, 1.62; I2 = 0%) (Figure 2). We conducted subgroup analyses based on study design, participant age range, number of cases, and serum vitamin D assessment tool. We also found a significant association between low vs. high serum vitamin D concentrations in cohort studies, those conducted in infants, and studies assessed serum vitamin D by HPLC-MS tool (P = 0.036 for all) (Table 2).
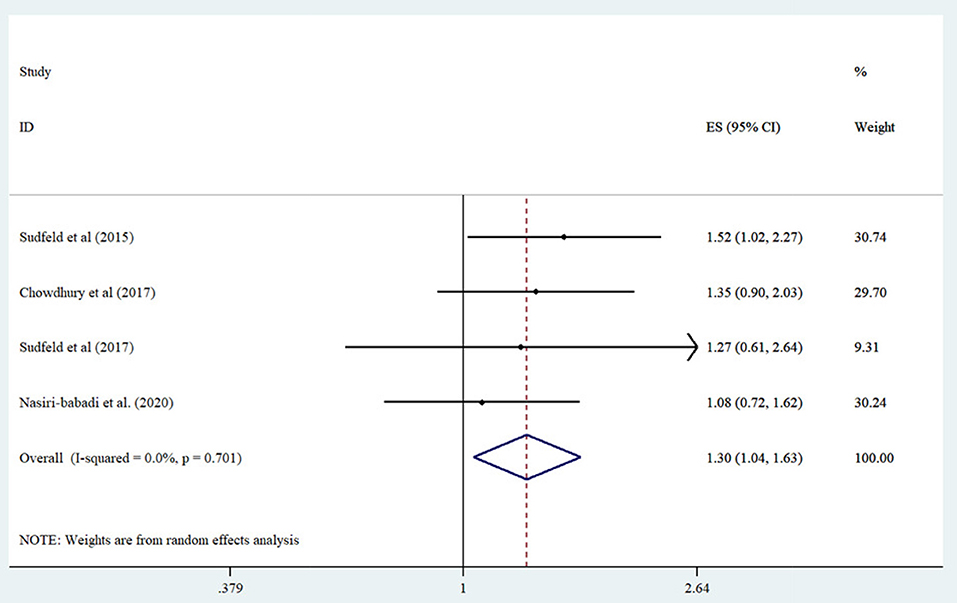
Figure 2. Forest plot derived from random-effects meta-analysis of studies investigating the association between low vs. high serum vitamin D concentration and wasting in children. CI, confidence interval; ES, effect size.
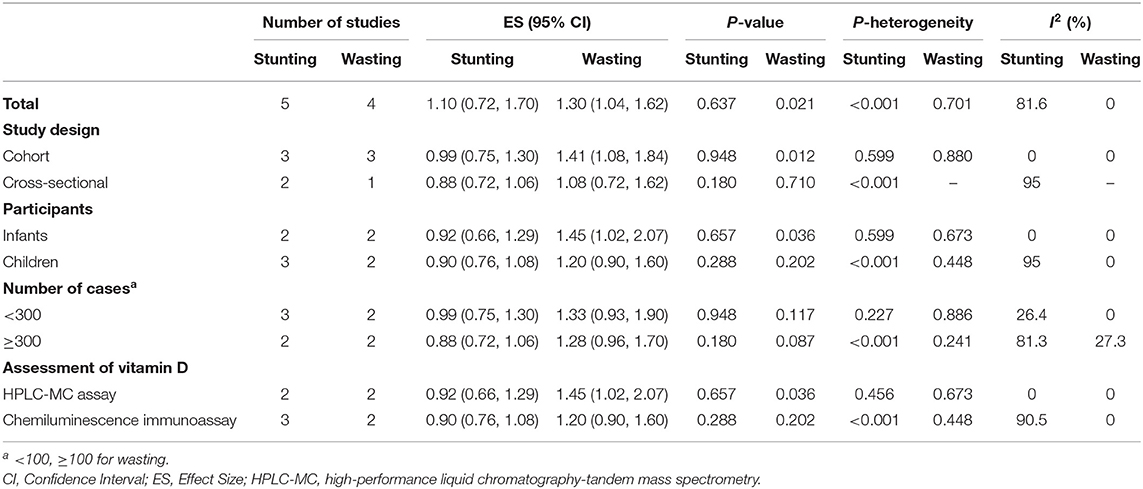
Table 2. Results of subgroup analysis for vitamin D status and risk of stunting and wasting in children.
The Association of Serum Vitamin D Status With Stunting Risk
Five studies were pooled in the meta-analysis comparing high vs. low serum level vitamin D categories (14, 16, 17, 19, 20). Comparing the lowest vs. highest serum vitamin D concentrations, no significant association was demonstrated between serum vitamin D level and stunting risk (Summary Risk Estimate: 1.10; 95% CI: 0.72, 1.70; I2 = 81.6%) (Figure 3). Subgroup analysis based on predefined factors including study design, participant age range, number of cases, and serum vitamin D assessment tool displayed that all of these items were the sources of heterogeneity (Table 2). Moreover, we failed to find any significant relationship between serum vitamin D status and stunting in subgroups.
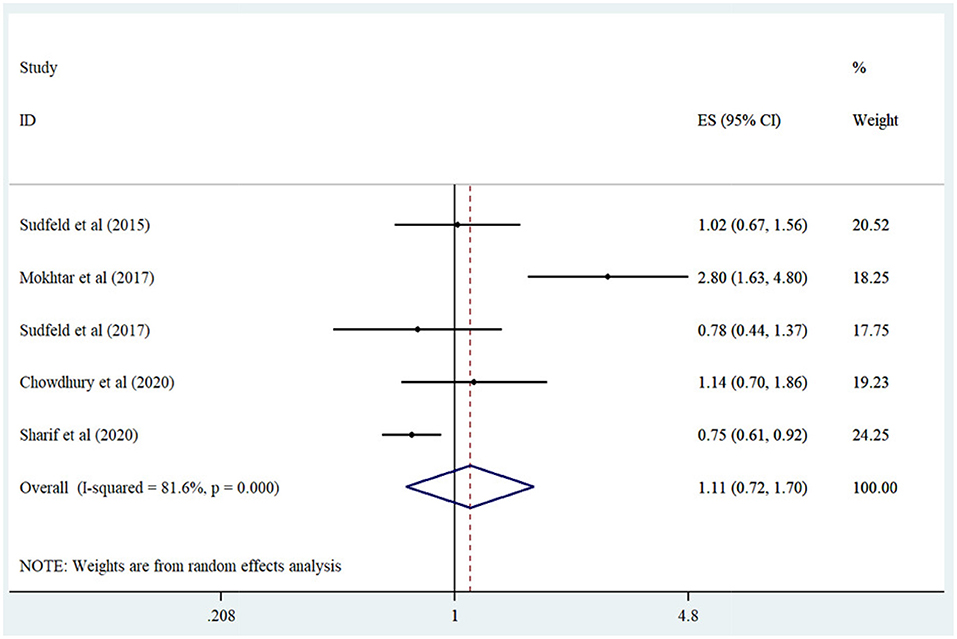
Figure 3. Forest plot derived from random-effects meta-analysis of studies investigating the association between low vs. high serum vitamin D concentration and stunting in children. CI, confidence interval; ES, effect size.
The Association of Serum Vitamin D Status With Risk of Underweight
Combining the risk estimates of three studies (17, 18, 20) regarding the association of lowest vs. highest serum vitamin D concentration and risk of underweight illustrated no significant relationship (Summary Risk Estimate: 1.12; 95% CI: 0.81, 1.56; I2 = 49.2%) (Figure 4).
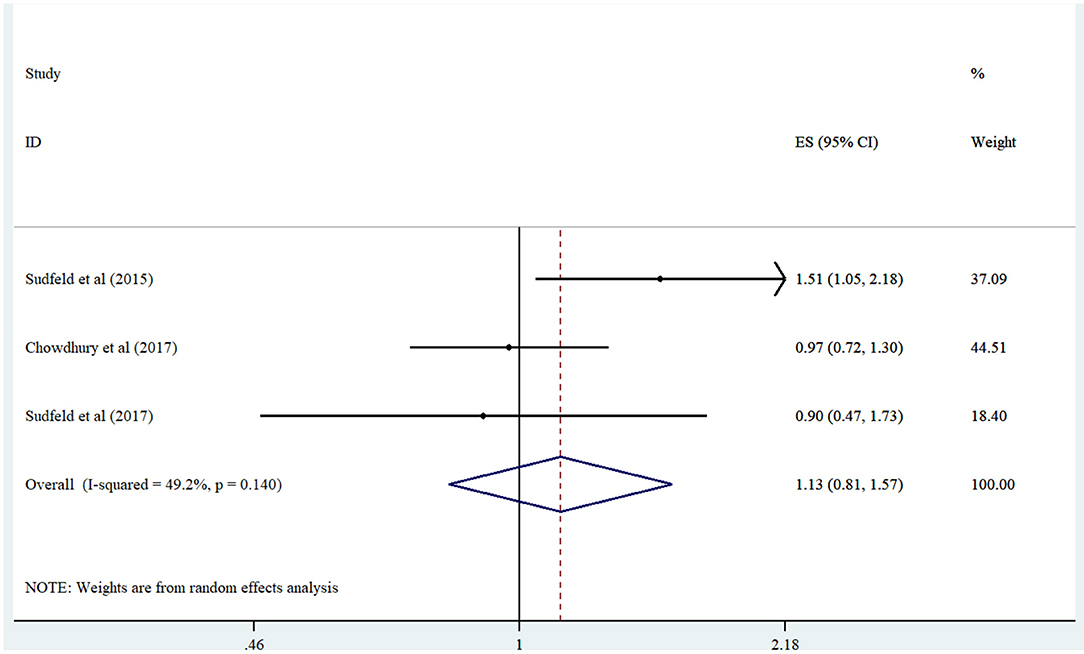
Figure 4. Forest plot derived from random-effects meta-analysis of studies investigating the association between low vs. high serum vitamin D concentration and underweight in children. CI, confidence interval; ES, effect size.
Publication Bias
Evidence of publication bias was not recognized in both the egger test and funnel plot for wasting (P = 0.93), stunting (P = 0.20), and underweight (P = 0.97) (Supplementary Figures 1–3).
Sensitivity Analysis
According to the sensitivity analysis test results, any studies could not significantly influence summary risk regarding the association of low vs. high serum concentrations of vitamin D and risk of wasting, stunting, and underweight (Supplementary Figures 4–6).
Discussion
The present meta-analysis assessed the association between vitamin D status and risk of wasting, stunting, and underweight using data from three cohort and four cross-sectional studies. Our findings demonstrated a significant association between lowest vs. highest serum vitamin D concentration and risk of wasting. However, serum vitamin D status (low vs. high) was not associated with an increased risk of stunting and underweight.
We found significant inverse relationship between vitamin serum vitamin D and wasting. In line with our result, a randomized clinical trial study in Pakistan showed supplementation with 200,000 IU twice/month vitamin D3 improved the mean WLZ in children aged 6–58 months with severe acute malnutrition (25). Another clinical trial on Canadian healthy mature infants who used at least 400 IU/d vitamin D supplement from 1 to 12 months of age found that elevated vitamin D concentrations from infancy to 3 years of age were related to leaner body composition (26). In contrast to our finding, a cross-sectional study in Uganda on 158 children aged 6–24 months observed no significant difference in vitamin D levels between the wasting and non-wasting children (27).
The chances are that differences in study design, age group, assessment method of serum vitamin D concentration, number of wasted children, defining different cut-points for vitamin D deficiency, and adjusted factors are the reasons for these contradictions. In this study, we also found similar findings in cohort studies, infants, studies with a higher number of cases, and studies that used HPLC-MS to evaluate vitamin D concentration. Needing follow-up assessments to examine the associations between vitamin- D status and growth, the findings of prospective cohort studies are more reliable than cross-sectional studies. Moreover, infants are more susceptible to vitamin D deficiency than children in higher ages due to low vitamin D intake during breastfeeding, confined exposure to sunlight, and inadequate vitamin D transmission through the placenta (28). Furthermore, 25(OH)D concentrations can be overestimated by the immunoassay method compared to HPLC-MS (29) due to its lipophilic nature, which makes it vulnerable to matrix effects in the protein binding assays (30).
We detected that risk of stunting and underweight did not elevated in low serum vitamin D. In line with our finding, a double-blind, placebo-controlled trial on 3,046 children ages 1–11 months from inner-city Kabul indicated that supplementation with 100,000 IU vitamin D3 for 18 months had no effect on weight age, weight for height, height for age (31). In contrast to our findings, Kumar et al., in a randomized clinical trial, investigated the effects of 35 μg/week vitamin D in low birth weight infants (1.8–2.5 kg) from birth up to 6 months of age in India. They indicated that vitamin D supplements raised weight, height, and arm circumference compared to placebo (32). Besides, maternal vitamin D3 supplementation (35,000 IU/wk) during the third trimester of pregnancy improved infants' linear growth during 1 year after birth compared to infants born from mothers who did not receive vitamin D supplementation (33).
Therefore, the lack of significant relationships between vitamin D status and stunting and underweight in our study may be unpredicted. One likelihood is that bone growth disorders in children occur after a severe vitamin D deficiency. Another explanation is that in addition to vitamin D shortage, other growth-related macro and micronutrient deficiencies such as animal-source protein, calcium, vitamin B12, and zinc may also involve low growth (34). Thus, the vitamin D impact on development could be trivial in the light of other growth-related nutrient deficiencies in children.
Vitamin-D plays several roles in the growth of children (14, 18). First, children need higher calcium intake than adults to provide adequate calcium for bone mineralization (35). Vitamin D is participated in bone mineralization by maintaining normal calcium and phosphate concentrations in the blood (36). Second, Vitamin D increases the growth plate cells' sensitivity to growth hormone, which has an important influence on linear growth in school-aged children (9). Third, vitamin D may help muscle growth through vitamin D receptors (VDR) (37). It conducts this role by stimulation of the production of new proteins involving in muscle cell proliferation, differentiation, and contractility and the regulation of calcium transport in the sarcoplasmic reticulum (38, 39).
Based on our knowledge, this study is the first systematic review and meta-analysis to investigate the association of vitamin D status with the risk of wasting, stunting, and underweight in children. Moreover, we did not identify any evidence of publication bias. The amount of heterogeneity was low regarding the association of vitamin D status with the risk of wasting and underweight. Finally, all of included essays had high quality score.
This study has several limitations. First, the small number of studies and sample size may have led to the disability to identify some significant associations. Second, although all included studies controlled different types of relevant confounders, it may be necessary to consider other residual confounding factors, including dietary and serum levels of other growth-limited nutrients, in future studies. Third, using cross-sectional studies may prevent us from detecting causal associations between vitamin D status and undernutrition factors. Finally, the number of studies that provided adequate data for dose-response analysis was so low that we could not perform this analysis.
In conclusion, we found that children with the lowest serum vitamin D concentration had a greater risk of wasting than children with the highest serum vitamin D level category. However, there was no significant relationship between serum vitamin D status and risk of stunting and underweight in children. More prospective cohort studies with larger sample size and longer duration of follow-up among various children populations, including those living in areas with a higher prevalence of vitamin D deficiency like tropical settings, are needed to confirm our findings.
These study report important public health implications particularly for populations with low socioeconomic status. Our findings propose that strategies to enhance vitamin D status in children by food fortification or supplementation could help the Ministry of Health's efforts to decrease undernutrition especially wasting.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
ChunhS, HL, and HS designed the work. BW and ChunlS extracted the data. ChunlS analyzed the data. HL wrote the manuscript and supervised the work. All authors critically revised and approved the final version of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2021.665749/full#supplementary-material
References
1. Gross R, Webb P. Wasting time for wasted children: severe child undernutrition must be resolved in non-emergency settings. Lancet. (2006) 367:1209-11. doi: 10.1016/S0140-6736(06)68509-7
2. Li Z, Kim R, Vollmer S, Subramanian SV. Factors associated with child stunting, wasting, and underweight in 35 low- and middle-income countries. JAMA Netw Open. (2020) 3:e203386. doi: 10.1001/jamanetworkopen.2020.3386
3. Ghosh-Jerath S, Singh A, Jerath N, Gupta S, Racine EF. Undernutrition and severe acute malnutrition in children. BMJ. (2017) 359:j4877. doi: 10.1136/bmj.j4877
4. Vaivada T, Akseer N, Akseer S, Somaskandan A, Stefopulos M, Bhutta ZA. Stunting in childhood: an overview of global burden, trends, determinants, and drivers of decline. Am J Clin Nutr. (2020) 112 (Suppl. 2):777s−91s. doi: 10.1093/ajcn/nqaa159
5. Black RE, Allen LH, Bhutta ZA, Caulfield LE, de Onis M, Ezzati M, et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. (2008) 371:243–60. doi: 10.1016/S0140-6736(07)61690-0
6. van Stuijvenberg ME, Nel J, Schoeman SE, Lombard CJ, du Plessis LM, Dhansay MA. Low intake of calcium and vitamin D, but not zinc, iron or vitamin A, is associated with stunting in 2- to 5-year-old children. Nutrition. (2015) 31:841–6. doi: 10.1016/j.nut.2014.12.011
7. Rivera JA, Hotz C, González-Cossío T, Neufeld L, García-Guerra A. The effect of micronutrient deficiencies on child growth: a review of results from community-based supplementation trials. J Nutr. (2003) 133:4010S−20S. doi: 10.1093/jn/133.11.4010S
8. DeBoer MD, Lima AA, Oría RB, Scharf RJ, Moore SR, Luna MA. Early childhood growth failure and the developmental origins of adult disease: do enteric infections and malnutrition increase risk for the metabolic syndrome? Nutr Rev. (2012) 70:642–53. doi: 10.1111/j.1753-4887.2012.00543.x
9. Esposito S, Leonardi A, Lanciotti L, Cofini M, Muzi G, Penta L. Vitamin D and growth hormone in children: a review of the current scientific knowledge. J Trans Med. (2019) 17:87. doi: 10.1186/s12967-019-1840-4
10. Caprio M, Infante M, Calanchini M, Mammi C, Fabbri A. Vitamin D: not just the bone. Evidence for beneficial pleiotropic extraskeletal effects. Eating Weight Disord. (2017) 22:27–41. doi: 10.1007/s40519-016-0312-6
11. Holick MF. Vitamin D: extraskeletal health. Rheum Dis Clin N Am. (2012) 38:141–60. doi: 10.1016/j.rdc.2012.03.013
12. Mithal A, Wahl DA, Bonjour JP, Burckhardt P, Dawson-Hughes B, Eisman JA, et al. Global vitamin D status and determinants of hypovitaminosis D. Osteoporosis Int. (2009) 20:1807–20. doi: 10.1007/s00198-009-0954-6
13. Villena-Esponera MP, Moreno-Rojas R, Molina-Recio G. Food insecurity and the double burden of malnutrition of indigenous refugee Épera Siapidara. J Immigr Minor Health. (2019) 21:1035–42. doi: 10.1007/s10903-018-0807-5
14. Mokhtar RR, Holick MF, Sempértegui F, Griffiths JK, Estrella B, Moore LL, et al. Vitamin D status is associated with underweight and stunting in children aged 6-36 months residing in the Ecuadorian Andes. Public Health Nutr. (2018) 21:1974–85. doi: 10.1017/S1368980017002816
15. Nasiri-babadi P, Sadeghian M, Sadeghi O, Siassi F, Dorosty A, Esmaillzadeh A, et al. The association of serum levels of zinc and vitamin D with wasting among Iranian pre-school children. Eating Weight Disord. (2020) 26:211–8. doi: 10.1007/s40519-019-00834-1
16. Sharif Y, Sadeghi O, Dorosty A, Siassi F, Jalali M, Djazayery A, et al. Association of vitamin D, retinol and zinc deficiencies with stunting in toddlers: findings from a national study in Iran. Public Health. (2020) 181:1–7. doi: 10.1016/j.puhe.2019.10.029
17. Sudfeld CR, Manji KP, Smith ER, Aboud S, Kisenge R, Fawzi WW, et al. Vitamin D deficiency is not associated with growth or the incidence of common morbidities among Tanzanian infants. J Pediatr Gastroenterol Nutr. (2017) 65:467–74. doi: 10.1097/MPG.0000000000001658
18. Chowdhury R, Taneja S, Bhandari N, Kvestad I, Strand TA, Bhan MK. Vitamin-D status and neurodevelopment and growth in young north Indian children: a secondary data analysis. Nutr J. (2017) 16:59. doi: 10.1186/s12937-017-0285-y
19. Chowdhury R, Taneja S, Kvestad I, Hysing M, Bhandari N, Strand TA. Vitamin D status in early childhood is not associated with cognitive development and linear growth at 6-9 years of age in North Indian children: a cohort study. Nutr J. (2020) 19:14. doi: 10.1186/s12937-020-00530-2
20. Sudfeld CR, Duggan C, Aboud S, Kupka R, Manji KP, Kisenge R, et al. Vitamin D status is associated with mortality, morbidity, and growth failure among a prospective cohort of HIV-infected and HIV-exposed Tanzanian infants. J Nutr. (2015) 145:121–7. doi: 10.3945/jn.114.201566
21. Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. (2015) 4:1. doi: 10.1186/2046-4053-4-1
22. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Euro J Epidemiol. (2010) 25:603–5. doi: 10.1007/s10654-010-9491-z
23. Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Chichester, England; Hoboken. NJ: Wiley-Blackwell (2008).
24. Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
25. Saleem J, Zakar R, Zakar MZ, Belay M, Rowe M, Timms PM, et al. High-dose vitamin D3 in the treatment of severe acute malnutrition: a multicenter double-blind randomized controlled trial. Am J Clin Nutr. (2018) 107:725–33. doi: 10.1093/ajcn/nqy027
26. Hazell TJ, Gallo S, Vanstone CA, Agellon S, Rodd C, Weiler HA. Vitamin D supplementation trial in infancy: body composition effects at 3 years of age in a prospective follow-up study from Montréal. Pediatr Obes. (2017) 12:38–47. doi: 10.1111/ijpo.12105
27. Nabeta HW, Kasolo J, Kiggundu RK, Kiragga AN, Kiguli S. Serum vitamin D status in children with protein-energy malnutrition admitted to a national referral hospital in Uganda. BMC Res Notes. (2015) 8:418. doi: 10.1186/s13104-015-1395-2
28. Wagner CL, Greer FR. Prevention of rickets and vitamin D deficiency in infants, children, and adolescents. Pediatrics. (2008) 122:1142–52. doi: 10.1542/peds.2008-1862
29. Costelloe SJ, Woolman E, Rainbow S, Stratiotis L, O'Garro G, Whiting S, et al. Is high-throughput measurement of 25-hydroxyvitamin D3 without 25-hydroxyvitamin D2 appropriate for routine clinical use? Ann Clin Biochem. (2009) 46 (Pt 1):86–7. doi: 10.1258/acb.2008.008157
30. Hollis BW. Editorial: the determination of circulating 25-hydroxyvitamin D: no easy task. J Clin Endocrinol Metab. (2004) 89:3149–51. doi: 10.1210/jc.2004-0682
31. Crowe FL, Mughal MZ, Maroof Z, Berry J, Kaleem M, Abburu S, et al. Vitamin D for growth and rickets in stunted children: a randomized trial. Pediatrics. (2021) 147:e20200815. doi: 10.1542/peds.2020-0815
32. Kumar GT, Sachdev HS, Chellani H, Rehman AM, Singh V, Arora H, et al. Effect of weekly vitamin D supplements on mortality, morbidity, and growth of low birthweight term infants in India up to age 6 months: randomised controlled trial. BMJ. (2011) 342:d2975. doi: 10.1136/bmj.d2975
33. Roth DE, Perumal N, Al Mahmud A, Baqui AH. Maternal vitamin D3 supplementation during the third trimester of pregnancy: effects on infant growth in a longitudinal follow-up study in Bangladesh. J Pediatr. (2013) 163:1605–11.e3. doi: 10.1016/j.jpeds.2013.07.030
34. Eaton JC, Rothpletz-Puglia P, Dreker MR, Iannotti L, Lutter C, Kaganda J, et al. Effectiveness of provision of animal-source foods for supporting optimal growth and development in children 6 to 59 months of age. Cochrane Database Syst Rev. (2019) 2:Cd012818. doi: 10.1002/14651858.CD012818.pub2
35. Shin YH, Shin HJ, Lee YJ. Vitamin D status and childhood health. Korean J Pediatr. (2013) 56:417–23. doi: 10.3345/kjp.2013.56.10.417
36. Bikle DD. Vitamin D metabolism, mechanism of action, and clinical applications. Chem Biol. (2014) 21:319–29. doi: 10.1016/j.chembiol.2013.12.016
37. Dirks-Naylor AJ, Lennon-Edwards S. The effects of vitamin D on skeletal muscle function and cellular signaling. J Steroid Biochem Mol Biol. (2011) 125:159–68. doi: 10.1016/j.jsbmb.2011.03.003
38. Garcia LA, King KK, Ferrini MG, Norris KC, Artaza JN. 1,25(OH)2vitamin D3 stimulates myogenic differentiation by inhibiting cell proliferation and modulating the expression of promyogenic growth factors and myostatin in C2C12 skeletal muscle cells. Endocrinology. (2011) 152:2976–86. doi: 10.1210/en.2011-0159
Keywords: vitamin D, undernutrition, stunting, wasting, underweight, meta-analysis
Citation: Song C, Sun H, Wang B, Song C and Lu H (2021) Association Between Vitamin D Status and Undernutrition Indices in Children: A Systematic Review and Meta-Analysis of Observational Studies. Front. Pediatr. 9:665749. doi: 10.3389/fped.2021.665749
Received: 08 February 2021; Accepted: 28 April 2021;
Published: 04 June 2021.
Edited by:
Mojtaba Heydari, Shiraz University of Medical Sciences, IranReviewed by:
Soheil Hassanipour, Gilan University of Medical Sciences, IranNimmathota Arlappa, National Institute of Nutrition (ICMR), India
Copyright © 2021 Song, Sun, Wang, Song and Lu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hongying Lu, aG9uZ3lpbmcubHUyMUBnbWFpbC5jb20=
 Chunhua Song1
Chunhua Song1 Hongying Lu
Hongying Lu