- 1Department of General Surgery, Beijing Children's Hospital, Capital Medical University, National Center for Children's Health, Beijing, China
- 2Department of Biomedical Engineering, The Fourth Military Medical University, Xi'an, China
Background: Acquired rectourethral (RUF) or rectovaginal fistulas (RVF) in children are rare conditions in pediatric surgery. Prior literature are retrospective studies and based on a small number of patients. The managements and outcomes vary widely across different studies. No standard or recommended management has been universally adopted. The goal was to systematically summarize different causes, provide an overlook of current clinical trend and to derive recommendation from the literature regarding the etiology, managements, and outcomes of pediatric acquired RUF and RVF.
Methods: PubMed, Embase, Cochrane databases were searched using terms: rectourethral fistula, recto-urethral fistula, urethrorectal fistula, urethro-rectal fistula, rectovaginal fistula. All studies were retrospective, in English, and included patients under the age of 18 years. Any series with congenital cases, adult (>18 years), <2 fistula cases less and obstetric related causes were excluded. The Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guideline was followed.
Results: Of the 531 records identified, 26 articles with 163 patients (63 RUF and 100RVF) were fully analyzed. Most RUF resulted from trauma, most RVF were from infection of HIV. About 92 patients underwent 1 of 3 categories of definitive repair, including transanal (4.3%), trans-sphincteric (48.9%), and transperineal (30.4%). Tissue interposition flaps were used in 37.6% patients, while temporary fecal diversions were used in 63.9% patients. Fistula was successfully closed in 50.3% patients (98.4% RUF and 20% RVF). 89.1 and 79.7 % of surgical repair patients had optimal fecal and urinary functions, respectively. In the inflammatory bowel disease and HIV infection related RVF patient group, the closure rate was prohibitive poor.
Conclusions: Most RVF are a sign of systematic diseases like HIV-infection or IBD and are associated with poor general conditions. While conservative treatment is recommended, stable patients can benefit from surgery. Further investigation is recommended if RVF are encountered without trauma or surgical history. RUF are likely to result from trauma or surgery, and transperineal or trans-sphincter approach can lead to closure and optimal function results. Fecal diversion and/or urinary diversion are helpful in some cases, while interposition technique may not be necessary. An objective scoring system for long-term follow-up and reporting consensus is needed to address treatment inconsistence.
Background
Acquired rectourethral (RUF) or rectovaginal fistulas (RVF) in children are rare conditions but a Gordian knot for pediatric surgeons (1). They may occur as a manifestation of HIV infection (2), in the setting of inflammatory bowel disease (IBD) (3), or resulting from trauma (4), iatrogenic fistulas because of colorectal surgery for congenital anorectal malformation (ARM) (5), or Hirschsprung's disease (6). Despite various reasons leading to acquired RUF and RVF, reported incidence is low and mishandled cases are frequent.
Conservative treatments are attempted by using draining seton, contemporary fecal diversion (FD) and/or urinary diversion (UD). However, irrespective of etiology, most children with RUF and RVF do not respond well to FD alone and require further treatments (7, 8). Various repair procedures: transperineal, trans-sphincteric (i.e., York-Mason, PSARP), transanal, transabdominal, or a combination of the above, have been described. Rarely, fibrin glue therapy or collagen plug are used, but outcomes are prohibitively poor (9).
Definitive repairs for children are considered more difficult than adults. The underdeveloped structure between primitive gut and urogenital sinus leads to two systems intimately attached to each other, leaving a narrow space to repair. The transperineal approach is favored by urologists as it provides a direct view and access to the posterior urethra (10), and allows for muscle flap interposition and concomitant urethroplasty. The trans-sphincteric approach (i.e., York-Mason, PSARP) (1, 4) involves midline sagittal division of posterior and anterior anorectal walls along with the corresponding sphincteric musculature. Fecal and urinary functions can be largely preserved. Flap interposition was once considered impossible or difficult through trans-sphincter incision (11), but recent research provides a new thought (1). The transanal approach (i.e., Latzko) has limited use because of narrow exposure (12). Obstructions of urinary and/or alimentary tract are commonly seen with acquired fistulas and may inhibit wound healing (13). Simultaneous end-to-end urethral anastomosis (14) and pull-through (PT) (15) are used to address these pathologic defects.
In summary, acquired RUF and RVF in children are heterogeneous; managements, and surgical approaches have been proposed. There is no established convention at present. Narrative review reflects the uncertainty and confusion, and fails to provide evidence-based knowledge. In this article, we aimed to systematically review literatures on pediatric acquired RUF and RVF to provide an overlook of current clinical trends and, when possible, outline suggestions for evaluation and treatment.
Methods
Protocol
This article is in accordance to the preferred reporting items for systematic reviews and meta-analyses (PRIMSA) guideline (16) and registered on INPLASY (INPLASY202110078).
Search Strategy and Sources
Two reviewers (Huang and Tan) screened PubMed and Embase from inception to Jan 2021 and searched records by title and abstract and reviewed eligible articles. A MEDLINE and Embase search was performed using three key terms with no date limits: (1) “rectourethral fistula” OR “recto-urethral fistula,” (2) “urethrorectal fistula” OR “urethro-rectal fistula,” (3) “rectovaginal fistula.” These three key terms were then narrowed: (1) English, (2) Human, (3) Child (<18 years). Ovid and the Cochrane library databases were searched using two key terms: (1) “rectourethral fistula” and (2) “rectovaginal fistula.” Pertinent references were searched manually. Five articles (9, 12, 17–19) were also reviewed for backgrounds but not used for qualitative analysis.
Enrolled Criteria
The studies were included using the following criteria: (1) Child <18y; (2) related to rectourethral or rectovaginal fistulas treatments.
The studies were excluded using the following criteria: (1) studies focusing on radiographic diagnosis of RUF/RVF; (2) case series/studies involving only congenital conditions; (3) reported cases focused on fistula repair with <2 patients (regardless of age); (4) case report; (5) studies focusing on obstetric related conditions; (6) review articles not reporting repairs and outcomes at the author's institution; (7) editorial letters/comments; (8) inadequate documentation of techniques or outcomes; (9) presentation abstracts; (10) others (adult patients, article not found, irrelevant).
Data Collection Process
Two reviewers (Huang and Tan) independently read all full articles and complied pertinent data as follows: (1) author and publication year, (2) number of RUF and/or RVF patients, (3) mean or median age, (4) etiology, (5) number of RUF and/or RVF patients who underwent surgical interventions, (6) number of patients who had temporary FD and/or UD, (7) type of surgical repair, (8) tissue flap usage, (9) treatment outcomes, (10) follow-up period, (11) prognosis. Types of surgical repair were organized into four categories: (1) trans-sphincteric, (2) transperineal, (3) transanal, and (4) others. Combined techniques such as laparotomy or endorectal pull-through were categorized as others. The trans-sphincteric category included York-Mason, PSARP as well as other sphincter-dividing operations. Temporary FD via colostomy or ileostomy alone was categorized as surgical interventions. Temporary UD defined as invasive drainage techniques was categorized as surgical interventions, i.e., suprapubic cystostomy. Use of transurethral Foley catheter was excluded.
Primary treatment outcomes were classified as follows: (1) successful fistula closure, (2) fistula recurrence or persistence; (3) others, i.e., patient refused treatment or died. Functional outcomes regarding fecal and urinary continence were defined as function after surgical repair closure within the study follow-up period and was based on description per respective authors. Successful fistula closure was defined as absence of clinical symptoms and radiographic confirmation of closure within the study follow-up period. Fistula recurrence was defined as a new fistula emerged after an attempt repair and a period absence of clinical symptoms, fistula persistence was defined as failed closure after surgical or conservative treatment within the study follow-up period. The follow-up period was defined as the mean or median time when patients were followed within the study. Prognosis included postoperative complications (i.e., anatomic pathologic features or impaired functional continence) and patient living status within the study follow-up period.
Bias Among Individual Studies
Given the rarity of pediatric acquired RUF and RVF, all studies were retrospective case series from single center with a small number of patients, and all were classified as level 4 evidence. Within some series, the surgical approach details were vague and heterogeneous, and the descriptions of outcomes were varied, which makes it difficult to compare within and between institutions. As with many retrospective studies, there is no control group, medical records are not consistent and accurate, and there is personal bias regarding surgical approaches.
Results
Study Selection
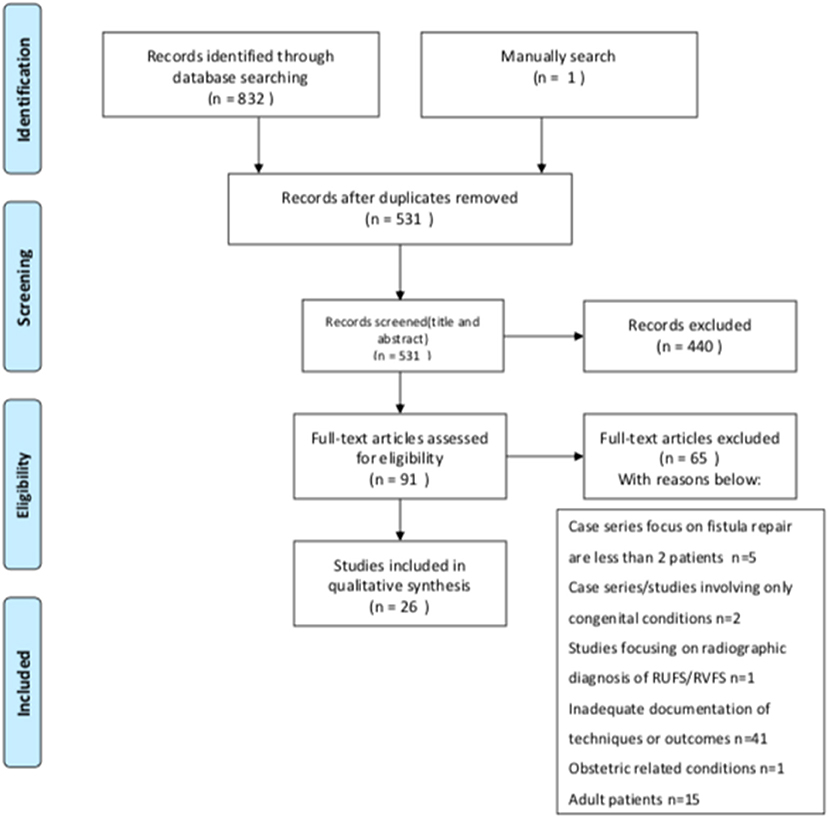
As shown in the PRISMA flow diagram for study selection process (Figure 1), 1,561 titles were generated with three key terms (451 “rectourethral fistula” OR “recto-urethral fistula,” 106 “urethrorectal fistula” OR “urethro-rectal fistula,” 1,004 “rectovaginal fistula.). The Ovid database search under the two key terms generated 2,544 titles (531 “rectourethral fistula”, 2,013 “rectovaginal fistula”). A total of 832 results were identified by using previously described limits. One article was added from the manual reference research. Three hundred and two duplicates were removed, leaving 531 citations for screening. After citations were screened, 440 were excluded, leaving 91 articles for full review. After 91 full-articles were reviewed, 65 were removed, leaving 26 articles for qualitative synthesis. No record was identified in the Cochrane Library.
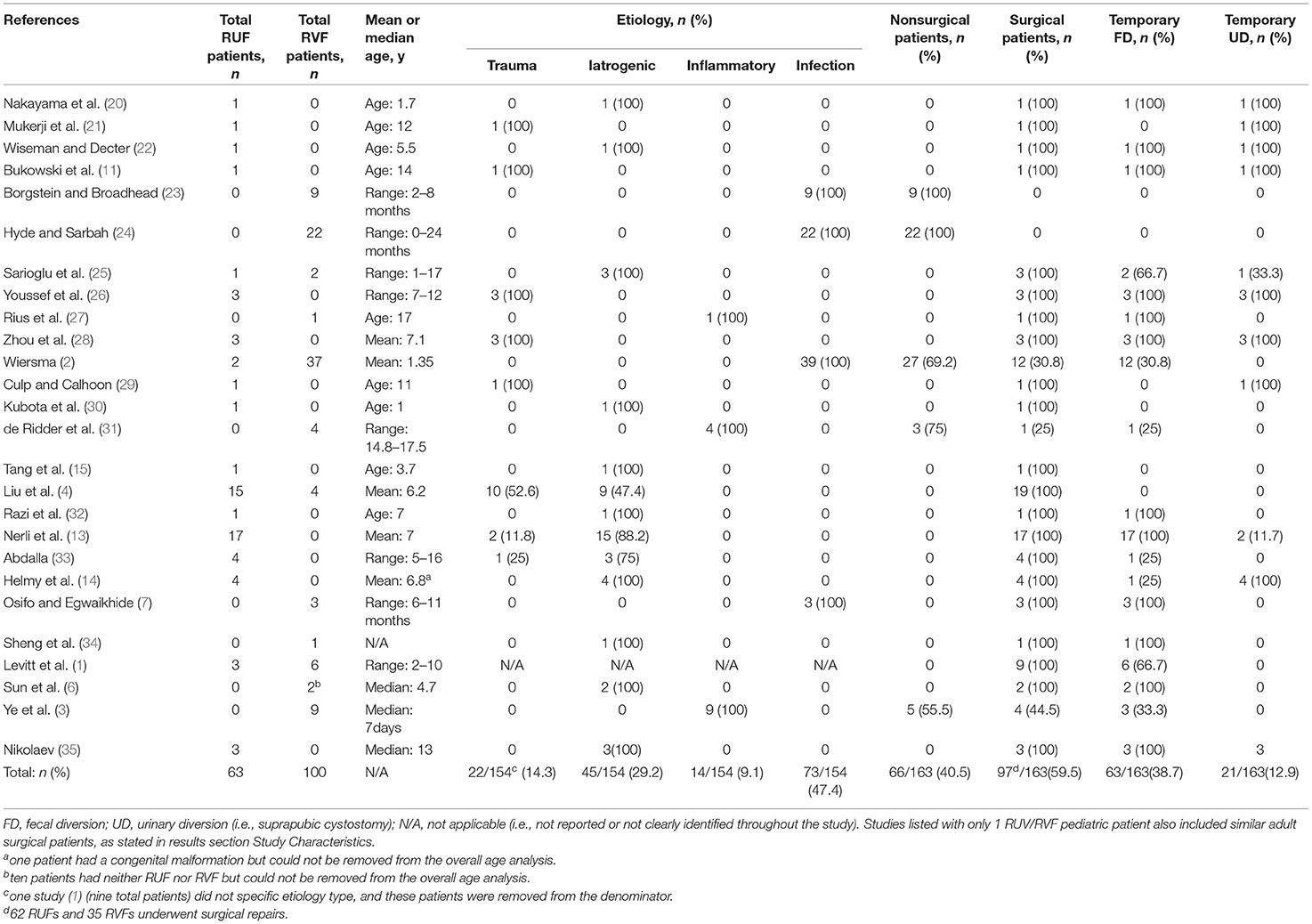
Study Characteristics
Overall patient-specific data are reported in Table 1. Surgical repairs, interposition flap usage, outcomes, follow-up, and prognosis are reported in Table 2. We identified 163 patients in 26 studies selected for qualitative analysis, including 63 RUF patients, and 100 RVF patients. Many case series written by urologists, describing both children and adult cases together. This was especially so for articles describing surgical techniques. This portion of surgeons and pediatric urologists would have accumulated substantial experience in treatment of fistulas. We tried to include these relatively more reliable articles in our analysis. Some of these case series only included one pediatric RUF/RVF case, but this nonetheless fulfilled our enrolment criteria. The mean or median age per study ranged from 7 days to 17.5 years. No studies met criteria for quantitative analysis.
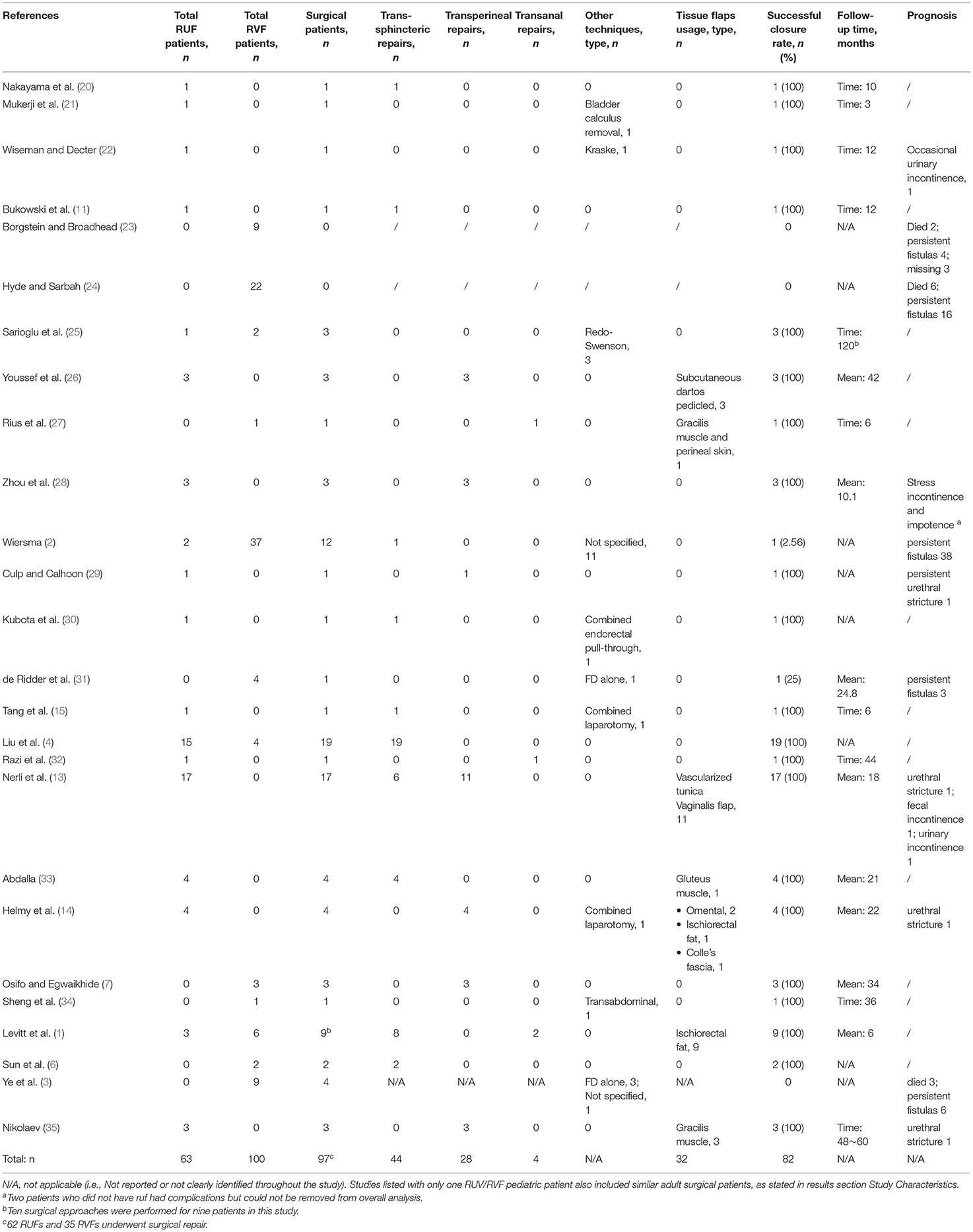
Table 2. Summary statistics for types of surgical repair, tissue flap usage, primary outcomes, follow-up period, and prognosis.
Etiology
Of 163 patients, 73 (47.4%) were caused by HIV infection in African since 1990s. Fistulas reported in those literature (2, 7, 23, 24) were predominantly RVF; HIV infection is the major cause of acquired RVF in the pediatric population. Second to retroviral infection, 45 (29.2%) iatrogenic fistulas were a complication of invasive operations, with rates as follows: 13.6% rectal surgery, 9.7% Hirschsprung's disease, 4.5% anorectal malformation, and 1.3% urethroplasty. Trauma-related fistulas were the third leading cause and the major cause of RUF, with over 80% of RUF (18 cases). The main types of trauma-related fistulas arose from pelvic fracture (14 patients), traffic accidents (six patients) and blunt/penetrating injuries (two patients). Although, they can present at any age, children beyond school-age are most affected (Table 1). There remained a small subset (14 patients, 9.1%) of RVF patients who were associated with inflammatory bowel disease (IBD). These patients are not many, but there is a trend of growing and early onset of symptoms.
Interventions
In total, 97 patients (59.5%) in 24 studies underwent surgical interventions, comprising of 98.4% (62/63) RUF and 35% (35/100) RVF patients. Among them, 92 patients had definitive surgical repairs, four RVF patient had FD alone with one healed spontaneously, one RUF patient healed after prolonged recovery followed removal of bladder calculus and UD. The remaining 66 patients (65 RVF and one RUF) were all exclusively in the IBD and HIV-infection group. Among them, nine patients died, 54 patients' fistulas persisted, three patients were lost to follow-up. Non-surgical treatments for these patients were anti-retroviral drugs, infliximab, broad spectrum antibiotics, supportive treatments, umbilical cord blood stem cell transplantation (three patients), or declined medical care (three patients).
Urinary and Fecal Diversions
Sixty two patients (63.9%) had temporary FD and 20 patients (20.6%) had temporary UD before or during definitive repair. Most studies (19/26) performed FD, among them 11 studies suggested that the variable time interval between effective FD and fistula repair ranged from 3 months to 8 years (data not shown). The indication of FD varied considerably across different etiology group. Patients in infection and inflammation groups exhibited (1) severe and advanced perianal infection or sepsis (2, 24, 27); (2) perforation (3). Patients in trauma and iatrogenic groups (1) were hopeful for spontaneous closure (4, 11); (2) had to prevent infection and maximize chance of closure (4, 13, 20, 22, 35); (3) classified as recurrent fistulas (11, 34). In general, temporary FD was closed 3 to 6 months after confirmation of closure, and temporary UD was removed 2–4 weeks postoperatively if there was no sign of leakage or infection.
Definitive Repairs
The number of definitive repairs (total 93) in 92 patients [one study (1) reported 10 surgical approaches for nine patients] for each surgical category is as follows: (1) four transanal (4.3%), (2) 45 trans-sphincteric (48.9%), (3) 28 transperineal (30.4 %), (4) three redo-Swenson procedure (3.2%), (5) one transabdominal (1.1%), (6) 12 non-specific (13.0%). One patient (14) required additional laparotomy to harvest the omentum for interposition and to create a FD at the same time. Another author (15) claimed that laparotomy was required because of severe pelvic fibrous adhesion. Some (30) advocated combined endorectal pull-through (PT) technique to prevent refistulization.
Tissue Interposition Flaps
Tissue interposition flaps were used in a little over one-third repairs (32/85, 37.6%) (Table 2). Vascularized tunica vaginalis flap were the most common (11/85, 12.9%) but were used in only one study (13), followed by ischiorectal fat (10/85, 11.8%), gracilis muscle (4/85, 4.7%), dartos (3/85, 3.5%), omentum (2/85, 2.4%), gluteus muscle (1/85, 1.2%), and Colle's fascia (1/85, 1.2%). Only seven literature performed tissue interposition, predominantly (28/31, 90.3%) via transperineal approach. Levitt et al. (1) and Abdalla et al. (33) used flap via trans-sphincteric or transanal approach. However, it is notable that across all definitive surgery repairs, there was no obvious advantage in flap usage regarding closure rate (all were 100%).
Successful Closure
In total, 82 (50.3%) patients had successful closure, 67 patients had persistent fistulas, 11 patients died because of underlying diseases and three patients missed follow-up. Successful closure rate in RUF was 98.4% (62/63), and 20% (20/100) in RVF. In surgical group, 82 patients had successful closure, 13 fistulas persisted and two died. The ultimate successful closure rate was optimal across all surgical repair cases (82/97, 84.5%) (Table 2), among them delayed closure was observed in four patients (4, 20, 21) (4/97, 4.1%) after adequate drainage of postoperative infection. At least seven studies (1, 15, 22, 27–29, 35) reported 18 patients who had 35 failed attempts of repair before ultimate closure, mainly via transperineal approach. Fistulas persisted in 67 patients (67/163, 41.1%), who were almost exclusively RVF patients (66/67, 98.5%) (Table 2). The definition of successful fistula closure varied in 23 studies as follows: (1) absence of clinical symptoms alone (14, 22, 28, 32); (2) radiographic confirmation of closure alone (6, 7, 13, 20, 26, 29, 30, 33, 35) (i.e., retrograde urethrogram or contrast enema); (3) evidence of radiographic closure and absence of symptoms (21); or (4) not specified (1, 2, 4, 11, 15, 25, 27, 31, 34).
Follow-Up
In 15 studies with a total of 64 definitive surgical repair, follow-up for postoperative function demonstrated that good fecal continence was preserved in 57 patients (57/64, 89.1%) and urinary continence was preserved in 51 patients (51/64, 79.7%). Ten studies (7, 11, 13, 14, 22, 26, 32–35) claimed to have mean or median follow-up period over one-year. Major postoperative anatomic and/or incontinence complications were rare, and only observed in six patients as follows: urethral stricture in four, urinary incontinence in two, fecal incontinence in one, urinary incontinence in one, and impotence in one (Table 2). Most functional results were based on description per authors. High mortality rate was observed in RVF (Table 2), all were secondary to underlying pathologic infection disease.
Discussion
Main Findings
Most RVF manifest as signs of systematic diseases including HIV-infection and IBD, which are associated with poor general conditions. While conservative treatment is recommended, stable patients can benefit from surgery. Further, investigation is recommended if RVF is encountered without trauma or surgical history. RUF are likely to result from trauma or surgery, and transperineal or trans-sphincter approach can lead to closure and optimal function results. Fecal diversion and/or urinary diversion is helpful in some cases, while interposition technique may not be necessary. An objective scoring system for long-term follow-up and reporting consensus is needed to address treatment inconsistence.
Interpretation
Acquired RUF and RVF are more common in adults and are rarely encountered in pediatric population. In children, infection with HIV is becoming an important and rapidly increased cause of acquired RUF. It is estimated that about 3 per 2.8 million women of reproductive age had babies with HIV-related RVF in Africa (7). The underlying pathophysiology, although, not yet fully-understood, shares a consistent clinical pattern (17): there is a significantly higher female prevalence (23, 24), but the few male patients (2) showed more complex fistulas. Most affected children were diagnosed within 1 year of age due to observation of abnormal feces discharge following a period of diarrhea. Presumably caused by anal gland abscess, fistula tended to arise from the dentate line, but biopsy showed non-specific inflammatory features (2).
Second to HIV-related fistulas, iatrogenic fistulas are also prevalent causes of RUF. Re-do Hirschsprung's disease (36) or re-do ARM repair (5) are two major sources of acquired fistulas in pediatric surgical practice. Fistulas in re-do Hirschsprung's disease are considered to be totally preventable and unacceptable (36), regardless of initial operations (6, 15, 20, 30, 34) (i.e., Duhamel, Soave, Swenson). These fistulas can be prevented by improving basic surgical skills. In re-do ARM repair patients, acquired fistulas are thought to occur when lacking the benefit of urethral Foley catheter, or when the anterior rectal wall is damaged (5). Trauma-related fistulas are frequently accompanied by pelvic fracture and complicated by urethroplasty (4, 28, 33), which highlights the need for cooperation between urologists and pediatric surgeons. Nerli et al. (13) suggested such pathologic defects should be cured before definitive fistula repair.
A small portion of acquired RVF patients are also diagnosed in the setting of IBD, particularly Crohn's disease. Most pediatric IBD are teenagers (37), and <1% are neonatal or infantile on-set. In the early 20th century, IBD related RVF (27, 31) was only noticed during adolescence but awareness has recently been raised for infantile-onset IBD related RVF (3). The increased diagnosis rate in younger age children (38) can be attributed to growing awareness in physicians (18) and advancing diagnosis techniques, which would explain a recent report (3) about acquired RVF in infantile onset IBD patients. It is reasonable to presume that this trend will continue in the future. Underlying pathology begins with small colonic mucosal ulcerations, followed by transmural penetration, and fistula formation (39). It is noteworthy that infantile onset patients had more severe clinical presentations and a very high mortality (3). Predisposing genetic mutation may play a critical role.
Attitudes toward conservative treatment as an initial plan varied considerably among different etiology groups. In fistulas induced by IBD or HIV infection, it is currently widely accepted (2, 9, 17, 19) that medicine is the first-line treatment; surgery is preserved as an adjunct therapy with very limited indications. One pivotal fact is that retroviral therapy (17) and antibiotics (40) have been proved effective to alleviate local effect. On the other hand, procedures performed to eliminate the fistula in the setting of active disease or infection are disappointing (2, 3, 27). However, with the advancement of conservative treatment to stable the general condition of patients, a potential change is emerging; surgery might only be needed if the RUV persists. More recent updates showed that patients could benefit from definitive repairs (1, 7), although, the timing and type of surgery needs further study. A careful small selection of patients (7) had a diverting fecal stoma to relieve infection and inflammatory process, which ultimately led to successful fistula closure. Yet as most authors (2, 3, 24) would agree, a FD is a last resort to control life-threating sepsis, advance perineal disease, or acute perforation, because poor healing will cause the situation to deteriorate. RUF induced by IBD or HIV infection were rarely reported (2), and special attention must be paid to their high infection risk, complex anatomy, and additional surgical needs. In summary, patients with asymptomatic RVF require no immediate surgical intervention, whereas, such intervention can be considered if their general conditions are stable.
In contrast with the above, among surgery or trauma induced fistula patients, debate about the need, timing, type of FD, and its role in protecting surgical repairs continue to be controversial. Two reports (11, 22) in this review mentioned spontaneous closure with FD in few patients, and two (11, 33) suggested diversion can be selectively adopted. One series (4) with a large volume of patients (n = 19) reported 100% successful closure rate via single stage surgery, but emphasized urethral stricture and secondary megacolon must be cured first. In many (13, 20, 22, 34), authors claimed that most patients did not respond well to FD alone and strongly advocated for FD to aid subsequent repair. Commonly, FD is considered based on the experience and opinions of the surgeons with conditions as follows: (1) recurrent fistulas; (2) severe urinary tract or perineum infection; (3) previous failed repairs; (4) dense scar and adhesion in fistula site. FD types are chosen to emphasize effective and complete diversion (20); an end ileostomy allows colon mobilization and coloanal anastomosis if needed, otherwise one can consider a colostomy. Most surgeons tended to wait 3 to 6 months before definitive repair, when scar may be soft and infections disappeared (4), but there is no clear census about appropriate timing at present. Notably, there are no data to support higher closure rates with FD, and <50% of patients in these two etiology groups had temporary FD before definitive repair. However, we believe that usage of FD must be individualized. FD is generally preferred in patients with large fistulas (>2cm), multiple failed repairs, poor general condition, and/or damaged sphincter function. Reversal of FD usually comes after radiologic confirmation of closure, while temporary UD is removed earlier if no clinical sign of leakage or infection.
The trans-sphincteric approach was used in half the patients and is a good initial approach to repair fistulas. The approach facilitates excellent exposure for the fistula and posterior urogenital structure, and provides a direct surgical field and preserves continence function. Successful closure was reported as 100% regardless of etiology. Two studies (15, 30) suggested to combine endorectal pull-through technique in the following situations: (1) extremely difficult fistula resection; (2) concomitant megacolon or anorectal stenosis; (3) large (>5mm), heavy scarred fistulas. Although, transperineal approach has a comparable closure rate (100%), it also involved multiple unspecified prior failures and postoperative urinary complications. Yet this approach is still favored by many urologists (26, 28, 29) to address concomitant urethra and/or vagina defects (i.e., stricture, atresia), and nearly 90% flap interposition was performed via this approach. Transanal approach (i.e., Latzko) is seldom used because of limited exposure to dissect and repair fistula. Large volume of blood loss and long surgical hours was also encountered (32). There remains a need for transabdominal approach for fistula proximal to bladder neck, dense pelvic adhesion, omental harvest. Tissue interposition flaps are not used as frequent as in adults (12). Adult fistulas tend to be large, complex and radiation-induced, requiring muscle flap (i.e., gracilis, dartos). Kubota et al. (30) and others (15) thought it was unnecessary and complicated, but Nikolaev et al. (35) claimed that accurate position of flap was the key to achieve success. No higher closure rate was observed with interposition technique in this review, which suggests that surgeons must carefully take all benefits and risks of interposition into account before repair.
Follow-up information suggested that acquired fistulas have substantial chance at healing with good fecal continence, particularly for RUF. RVF were associated with high mortality rate but this was mostly due to underlying pathology. However, follow-up rate in this study was not ideal (15/26) and length of follow-up was also subpar, with only 10 studies ranging over 1-year. Furthermore, aside from two studies (6, 34) that adopted the 2005 Krickenbeck classification to assess postoperative excretory function, all others were descriptive and therefore subjective. Current clinical guidelines for RVF does not include a scoring system to measure functional outcome, but the international continence society recommends using the ICS score (41) for urinary continence in RUF children. Long-term outcomes for RUF have also been studied using the bowel function score, an established qualitative scoring system for benign anorectal disorders (42), and evaluation of the overall success of RUF treatments has been carried out using the Pediatric Quality of Life Inventory (43). We believe that further use of these scoring systems, singularly or altogether, would provide a more detailed and reliable analysis of treatment success rates for both acquired RUF and RVF.
Limitations
The numerous conservative treatments and surgical repairs reflect the variability in surgeon preference and surgical skills, as well as the need for individualized treatment plan. Due to the heterogeneity of the trials and the limited amount of evidence, we were unable to perform any meta-analyses. A main limitation of this study is that all articles were retrospective studies from single institutions without a control group. The small number of patients and vague description of outcomes also precludes objective comparisons, but some conclusions can still be drawn from the existing information. Careful and extensive screening of the articles adds to the reliability of our conclusions, as lone case reports and articles without sufficient reliable information were excluded. The conclusions we have arrived at and the recommendations made for treatment of this rare disease should be but a stepping stone for further more detailed research.
Perspectives and Implication
Acquired RUF and RVF are rare in children. Most RVF are a sign of systematic diseases whereas RUF are likely to result from trauma or surgery. Treatments for RVF focus on medicine but stable patients may benefit from surgery. Further, and thorough investigation of the timing and type of surgery is needed in acquired RUF. An objective function scoring system for long-term follow-up and reporting consensus are needed in the future to address current treatment inconsistence.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author Contributions
All authors conceptualized and wrote the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Levitt MA, King SK, Bischoff A, Alam S, Gonzalez G, Pena A. The Gonzalez hernia revisited: use of the ischiorectal fat pad to aid in the repair of rectovaginal and rectourethral fistulae. J Pediatr Surg. (2014) 49:1308–10. doi: 10.1016/j.jpedsurg.2013.10.020
2. Wiersma R. HIV-positive African children with rectal fistulae. J Pediatr Surg. (2003) 38:62–4; discussion 62–4. doi: 10.1053/jpsu.2003.50011
3. Ye Z, Zhou Y, Huang Y, Wang Y, Lu J, Tang Z, et al. Phenotype and management of infantile-onset inflammatory bowel disease: experience from a tertiary care center in China. Inflamm Bowel Dis. (2017) 23:2154–64. doi: 10.1097/MIB.0000000000001269
4. Liu GC, Xia HM, Wen YQ, Zhang LY, Li ZM. Considerations before repair of acquired rectourethral and urethrovaginal fistulas in children. World J Pediatr. (2008) 4:53–7. doi: 10.1007/s12519-008-0011-0
5. Pena A, Grasshoff S, Levitt M. Reoperations in anorectal malformations. J Pediatr Surg. (2007) 42:318–25. doi: 10.1016/j.jpedsurg.2006.10.034
6. Sun S, Chen G, Zheng S, Dong K, Xiao X. Usefulness of posterior sagittal anorectoplasty for redo pull-through in complicated and recurrent Hirschsprung disease: experience with a single surgical group. J Pediatr Surg. (2017) 52:458–62. doi: 10.1016/j.jpedsurg.2016.08.016
7. Osifo OD, Egwaikhide EA. Acquired rectovaginal fistula in babies of unknown and asymptomatic retroviral positive mothers. J Pediatr Adolesc Gynecol. (2011) 24:e79–82. doi: 10.1016/j.jpag.2010.08.013
8. Nyam DC, Pemberton JH. Long-term results of lateral internal sphincterotomy for chronic anal fissure with particular reference to incidence of fecal incontinence. Dis Colon Rectum. (1999) 42:1306–10. doi: 10.1007/BF02234220
9. Vogel JD, Johnson EK, Morris AM, Paquette IM, Saclarides TJ, Feingold DL, et al. Clinical practice guideline for the management of anorectal abscess, fistula-in-ano, and rectovaginal fistula. Dis Colon Rectum. (2016) 59:1117–33. doi: 10.1097/DCR.0000000000000733
10. Varma MG, Wang JY, Garcia-Aguilar J, Shelton AA, McAninch JW, Goldberg SM. Dartos muscle interposition flap for the treatment of rectourethral fistulas. Dis Colon Rectum. (2007) 50:1849–55. doi: 10.1007/s10350-007-9032-3
11. Bukowski TP, Chakrabarty A, Powell IJ, Frontera R, Perlmutter AD, Montie JE. Acquired rectourethral fistula: methods of repair. J Urol. (1995) 153(3 Pt. 1):730–3. doi: 10.1016/S0022-5347(01)67701-2
12. Hechenbleikner EM, Buckley JC, Wick EC. Acquired rectourethral fistulas in adults: a systematic review of surgical repair techniques and outcomes. Dis Colon Rectum. (2013) 56:374–83. doi: 10.1097/DCR.0b013e318274dc87
13. Nerli RB, Koura A, Prabha V, Patne P, Devaraju S, Amarkhed SS, et al. Acquired recto-urethral fistula in children: long-term follow-up. J Pediatr Urol. (2009) 5:485–9. doi: 10.1016/j.jpurol.2009.03.001
14. Helmy TE, Sarhan OM, Dawaba ME, Wadie BS. Urethrorectal fistula repair in children: urologic perspective. J Trauma. (2010) 69:1300–3. doi: 10.1097/TA.0b013e3181e7934f
15. Tang S, Dong N, Tong Q, Wang Y, Mao Y. Laparoscopic assisted endorectal pull-through with posterior sagittal approach to the repair of postoperative rectourethral and rectovaginal fistula. Pediatr Surg Int. (2007) 23:1077–80. doi: 10.1007/s00383-007-1995-6
16. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. (2009) 62:1006–12. doi: 10.1016/j.jclinepi.2009.06.005
17. Uba AF, Chirdan LB, Ardill W, Ramyil VM, Kidmas AT. Acquired rectal fistula in human immunodeficiency virus-positive children: a causal or casual relationship? Pediatr Surg Int. (2004) 20:898–901. doi: 10.1007/s00383-004-1285-5
18. Shim JO. Recent advance in very early onset inflammatory bowel disease. Pediatr Gastroenterol Hepatol Nutr. (2019) 22:41–9. doi: 10.5223/pghn.2019.22.1.41
19. Wilson DC, Russell RK. Overview of paediatric IBD. Semin Pediatr Surg. (2017) 26:344–8. doi: 10.1053/j.sempedsurg.2017.10.002
20. Nakayama DK, Templeton JM Jr, Ziegler MM, O'Neill JA, Walker AB. Complications of posterior sagittal anorectoplasty. J Pediatr Surg. (1986) 21:488–92. doi: 10.1016/S0022-3468(86)80218-4
21. Mukerji AC, Ghosh BC, Sharma MM, Taneja OP. Spontaneous urinary fistula caused by vesical calculus. Br J Urol. (1970) 42:208–12. doi: 10.1111/j.1464-410X.1970.tb10024.x
22. Wiseman NE, Decter A. The Kraske approach to the repair of recurrent rectourethral fistula. J Pediatr Surg. (1982) 17:342–6. doi: 10.1016/S0022-3468(82)80484-3
23. Borgstein ES, Broadhead RL. Acquired rectovaginal fistula. Arch Dis Child. (1994) 71:165–6. doi: 10.1136/adc.71.2.165
24. Hyde GA Jr, Sarbah S. Acquired rectovaginal fistula in human immunodeficiency virus-positive children. Pediatrics. (1994) 94(6 Pt. 1):940–1.
25. Sarioglu A, Senocak M, Hicsonmez A, Buyukpamukcu N. Management of uncommon complications of definitive operations of Hirschsprung's disease. Eur J Pediatr Surg. (1996) 6:358–61. doi: 10.1055/s-2008-1071015
26. Youssef AH, Fath-Alla M, El-Kassaby AW. Perineal subcutaneous dartos pedicled flap as a new technique for repairing urethrorectal fistula. J Urol. (1999) 161:1498–500. doi: 10.1016/S0022-5347(05)68937-9
27. Rius J, Nessim A, Nogueras JJ, Wexner SD. Gracilis transposition in complicated perianal fistula and unhealed perineal wounds in Crohn's disease. Eur J Surg. (2000) 166:218–22. doi: 10.1080/110241500750009311
28. Zhou FJ, Xiong YH, Zhang XP, Shen PF. Transperineal end-to-end anastomotic urethroplasty for traumatic posterior urethral disruption and strictures in children. Asian J Surg. (2002) 25:134–8. doi: 10.1016/S1015-9584(09)60161-5
29. Culp OS, Calhoon HW. A variety of rectourethral fistulas: experiences with 20 cases. J Urol. (1964) 91:560–71. doi: 10.1016/S0022-5347(17)64171-5
30. Kubota A, Kawahara H, Okuyama H, Oue T, Tazuke Y, Ihara Y, et al. Endorectal pull-through with posterior sagittal approach to the repair of postoperative rectourethral and rectovaginal fistula. J Pediatr Surg. (2003) 38:1775–7. doi: 10.1016/j.jpedsurg.2003.08.021
31. de Ridder L, Escher JC, Bouquet J, Schweizer JJ, Rings EH, Tolboom JJ, et al. Infliximab therapy in 30 patients with refractory pediatric crohn disease with and without fistulas in the Netherlands. J Pediatr Gastroenterol Nutr. (2004) 39:46–52. doi: 10.1097/00005176-200407000-00010
32. Razi A, Yahyazadeh SR, Gilani MA, Kazemeyni SM. Transanal repair of rectourethral and rectovaginal fistulas. Urol J. (2008) 5:111–4. doi: 10.22037/uj.v5i2.56
33. Abdalla MA. Posterior sagittal pararectal approach with rectal mobilization for repair of rectourethral fistula: an alternative approach. Urology. (2009) 73:1110–4. doi: 10.1016/j.urology.2008.11.061
34. Sheng Q, Lv Z, Xiao X. Re-operation for Hirschsprung's disease: experience in 24 patients from China. Pediatr Surg Int. (2012) 28:501–6. doi: 10.1007/s00383-012-3062-1
35. Nikolaev VV. Recurrent rectourethral fistula repair: a novel technique of gracilis muscle interposition. J Pediatr Surg. (2020) 55:1974–8. doi: 10.1016/j.jpedsurg.2020.05.028
36. Pena A, Elicevik M, Levitt MA. Reoperations in Hirschsprung disease. J Pediatr Surg. (2007) 42:1008–13; discussion 13–4. doi: 10.1016/j.jpedsurg.2007.01.035
37. Loftus EV Jr. Clinical epidemiology of inflammatory bowel disease: incidence, prevalence, and environmental influences. Gastroenterology. (2004) 126:1504–17. doi: 10.1053/j.gastro.2004.01.063
38. Benchimol EI, Manuel DG, Guttmann A, Nguyen GC, Mojaverian N, Quach P, et al. Changing age demographics of inflammatory bowel disease in Ontario, Canada: a population-based cohort study of epidemiology trends. Inflamm Bowel Dis. (2014) 20:1761–9. doi: 10.1097/MIB.0000000000000103
39. Coran AG, Caldamone A, Adzick NS, Krummel TM, Laberge J-M, Shamberger R. Pediatric Surgery, 2-Volume Set Expert Consult - Online and Print. Philadelphia, PA: Mosby Elsevier - Health Sciences Division (2012).
40. McKee RF, Keenan RA. Perianal Crohn's disease–is it all bad news? Dis Colon Rectum. (1996) 39:136–42. doi: 10.1007/BF02068066
41. Varma KK, Mammen A, Kolar Venkatesh SK. Mobilization of pelvic musculature and its effect on continence in classical bladder exstrophy: a single-center experience of 38 exstrophy repairs. J Pediatr Urol. (2015) 11:87.e1–5. doi: 10.1016/j.jpurol.2014.11.023
42. Kyrklund K, Pakarinen MP, Koivusalo A, Rintala RJ. Long-term bowel functional outcomes in rectourethral fistula treated with PSARP: controlled results after 4-29 years of follow-up: a single-institution, cross-sectional study. J Pediatr Surg. (2014) 49:1635–42. doi: 10.1016/j.jpedsurg.2014.04.017
Keywords: rectourethral fistula, rectovaginal fistula, acquired fistula, pediatric surgery, systematic review
Citation: Huang X, Tan SS, Chen Y and Li T (2021) Acquired Rectourethral and Rectovaginal Fistulas in Children: A Systematic Review. Front. Pediatr. 9:657251. doi: 10.3389/fped.2021.657251
Received: 25 January 2021; Accepted: 12 April 2021;
Published: 07 May 2021.
Edited by:
Ezekiel E. Young, University at Buffalo, United StatesReviewed by:
Rados P. Djinovic, Sava Perovic Foundation, SerbiaYuval Bar-Yosef, Dana-Dwek Children's Hospital, Israel
Nicole Alavi-Dunn, University at Buffalo, United States
Copyright © 2021 Huang, Tan, Chen and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yajun Chen, ZHIuY2hlbnlqX3BlZGlhdHJAYWxpeXVuLmNvbQ==; Tian Li, Zm1tdWx0QGZveG1haWwuY29t
 Xinjie Huang
Xinjie Huang Sarah Siyin Tan
Sarah Siyin Tan Yajun Chen
Yajun Chen Tian Li
Tian Li