
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr. , 26 March 2021
Sec. Pediatric Urology
Volume 9 - 2021 | https://doi.org/10.3389/fped.2021.654015
 Margaret Ekstein1
Margaret Ekstein1 Avi A. Weinbroum1
Avi A. Weinbroum1 Jacob Ben-Chaim2
Jacob Ben-Chaim2 Eyal Amar3
Eyal Amar3 Reut Schvartz1
Reut Schvartz1 Yifat Klein1
Yifat Klein1 Yuval Bar-Yosef2*
Yuval Bar-Yosef2*Objectives: Penile surgery is commonly performed in pediatric surgical centers. There is no consensus regarding which analgesic method is most effective in controlling pain in these children.
Methods: Consecutive children between 4 months and 16 years of age who underwent elective penile surgery were recruited. After inhaled induction of anesthesia, children were randomized to one of three methods of intraoperative analgesia: caudal block, IV fentanyl titrated to surgical response and spontaneous respiration, or dorsal penile nerve block (DPNB). All patients were given inhaled agents; fentanyl was added if either block was insufficient. Demographic data, analgesic use and pain scores were recorded by a blinded investigator in the PACU and ward. Pain scores, analgesic requirement, and recovery parameters of returning to normal activity level, eating, and voiding post-operatively for up to 4 days, were compared.
Results: 116 children were recruited. Pain scores in the post anesthesia care unit were significantly lower in the DPNB and caudal block groups compared to the fentanyl group for the first 30 postoperative min. Pain scores and analgesic use were subsequently similar among the three groups for the rest of the study period. There was no statistical difference in time to eat, return to normal activity or in parental satisfaction scores among the groups. There was a trend toward earliest time to void in the DPNB group.
Conclusions: Regional blocks most effectively controlled pain for 30 min after surgery. The choice of intra-operative analgesia protocol had no effect on later pain and recovery parameters.
Penile surgery, including circumcision, revision of circumcision and repair of penile torsion, chordee or hypospadias, is commonly performed in pediatric surgical centers. Analgesic methods include caudal, penile, pudendal and ring blocks, opioid and non-opioid systemic analgesics, as well as application of topical agents. Despite the importance of pain control in these patients, there is no consensus regarding which analgesic method is most effective and safe in controlling perioperative pain in these children (1, 2). Regional anesthesia provides effective pain relief with minimal effects on respiratory drive or hemodynamic stability; however, it is associated with occasional but significant complications, especially in infants, and has not been shown to be consistently superior to systemic analgesia in prospective studies (3). Literature asserts that regional anesthesia in infants, while considered safe, should be used with caution (4). Recent retrospective studies have compared different forms of analgesia in children undergoing penile surgery (5); however, prospective studies are rare and few evaluate outcome parameters longer than the immediate post-operative period. Hence, there is a need to clarify which anesthesia option is most effective for post-operative pain relief while providing lasting enhanced recovery after penile surgery in children. The study hypothesis was that blocks, specifically caudal and dorsal penile nerve block (DPNB), are effective in reducing intra-operative and post-operative pain.
We studied children between 4 months and 16 years of age who underwent elective penile surgery under general inhaled anesthesia using three different methods of analgesia: caudal block, intravenous fentanyl or dorsal penile nerve block (DPNB). The primary aim of this prospective, randomized double blind study was to compare pain scores and need of supplemental analgesics in the immediate post-operative period. The secondary aim was to compare recovery parameters up to 4 days post-operatively, as well as overall parental satisfaction scores.
This study was designed as a randomized, double blind, prospective clinical trial, with three arms, and was conducted in accordance with the CONSORT guidelines (Figure 1). After obtaining approval from the local IRB as well as the State Ministry of Health, we recruited consecutive children between the ages of 4 months (at least 60 weeks post conceptual age) and 16 years, undergoing various penile surgeries. Informed consent was obtained in each case from parents or guardians. Exclusion criteria were ASA status >II, a history of bleeding disorder, spinal cord disease, obstructive sleep apnea, developmental delay, behavior disorder, allergy to any of the protocol's medications, or chronic cardio/pulmonary disease which resulted in chronic hypoxemia. Patients were also excluded if their penile surgery was part of a combined procedure with another operation (e.g., hernioraphy, hydrocelectomy, etc.) or if surgery was expected to include intervention at another site (e.g., buccal mucosa for hypospadias repair). All children received general anesthesia. Following anesthesia induction, the patients were randomized to one of the three groups as described below.
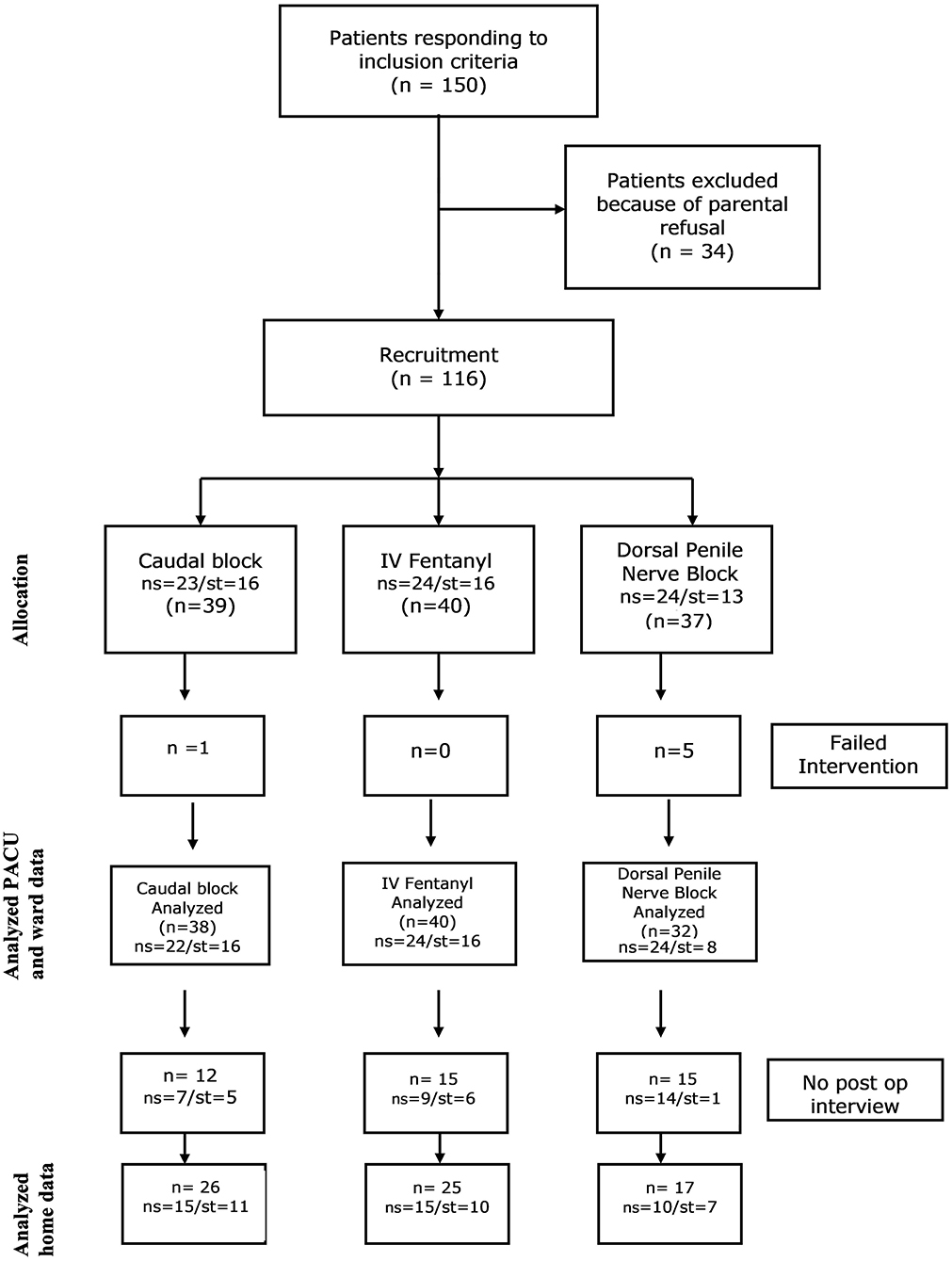
Figure 1. Flow diagram of the study cohort. ns, no penile stent placed; st, penile stent placed; PACU, post anesthesia care unit.
Children were kept fasting according to institutional guidelines. In the holding area they were premedicated with oral midazolam 0.5 mg/kg, not to exceed 15 mg.
Anesthesia was induced in all children with O2, N2O and sevoflurane. Routine monitors (pulse oximeter, three lead ECG, non-invasive blood pressure cuff and gas analyzer) were used. A laryngeal mask airway (LMA) was then placed while the patient was breathing spontaneously and was sufficiently anesthetized; an intravenous (IV) line was then placed. All patients were given 10 cc/kg IV lactated ringers solution (LR) over the first h of surgery and maintenance fluid for the subsequent hours of surgery. If blood losses exceeded an estimate of 2 cc/kg, they were replaced with LR at a ratio of 3:1.
Anesthesia was maintained with 40% O2 in N2O and isoflurane at inspired fractions of 0.6–1% under spontaneous ventilation with pressure support 7–10 cmH2O. If apnea occurred, or end tidal pCO2 rose above 65 mmHg, or if O2 saturation dropped below 94%, controlled ventilation was started via the LMA. Intubation was performed if ventilation or oxygenation did not improve the latter. No muscle relaxants were given unless needed as an emergency treatment of laryngospasm. At the end of surgery, inhaled agents were discontinued, the LMA was removed, and the patient was allowed to awaken breathing 100% O2 via a face mask. The patients were brought to the PACU while breathing room air.
After induction, patients were randomized via slips of paper pulled from an envelope by the circulating OR nurse to one of three methods of analgesia: (1) caudal block using 0.6 cc/kg of 0.25% bupivacaine (group C); (2) IV fentanyl of 1 mcg/kg increments titrated to lack of movement or hemodynamic response to surgical stimuli, and targeted to a spontaneous respiratory rate of 12–24/min according to patient's age (group F); (3) dorsal penile nerve block injection of 0.25 cc/kg (not to exceed 8 cc) of 0.5% bupivacaine, using the landmark technique (group P). A block was considered a “failed block” if the patient responded (by movement or changes of hemodynamic parameters) to incision, despite 15 min having elapsed from time of block placement to skin incision (during which the patient was repositioned on the surgical table, prepped, and draped). These children were diverted to receive general anesthesia with IV fentanyl as needed and their data were eliminated from that time onward; only their demographic data were included. The same anesthesiologist (ME) performed all intraoperative anesthetics but was not involved in the later data collection or analyses.
A dedicated PACU nurse, blinded to the method of each child's analgesia, followed patients' recovery in the PACU. She/he recorded oxygen saturation on room air, heart rate, respiratory rate every 15 min, as well as any untoward events (including nausea/vomiting) and medications given. In addition, the blinded nurse assessed pain using two scores: (1) Objective scale: FLACC score (scale of 0–10 based on the child's Face, Arm movement (substituted for Leg movement), Activity, Crying and Consolability, each graded between 0 and 2 points, and (2) the subjective numerical rating scale (NRS) as assessed by the parents on a scale of 0 = no pain to 10 = the worst pain possible. The nurse also recorded the sedation status of the child on a four point sedation scale of 0–3, in which 0 = completely awake; 1 = responds to voice; 2 = responds to touch, 3 = does not respond to touch.
Pain and sedation scores were recorded upon arrival to the PACU (time 0) and at 10, 20, 30 and 60 min later. If pain score by either scale was >3/10 and/or the parent requested medication for the child, 0.05 mg/kg of IV morphine was administered. Additional doses were available every 10 min, up to a total of 0.2 mg/kg. Ondansetron 0.15 mg/kg IV was available if there were signs of nausea or vomiting. The child was allowed to drink if fully awake, starting from 10 min after arrival to the PACU. Following existing directives, all children stayed in the PACU for a minimum of 60 min; they could stay longer if still sleepy or in pain.
After discharge from the PACU, patients were admitted to the pediatric surgery ward. Pain and sedation scores were recorded upon arrival (time 0), and 2, 4 and 6 h after arrival by the ward nurse, the parent being consulted every time. If pain score by either scale was >3/10, 10 mg/kg ibuprofen syrup was given to the child; if this was insufficient to control pain after 30 min, 0.2 mg/kg oxycodone syrup was added. Those who refused or were unable to drink 4 h after arriving to the ward were re-attached to IV fluids of 5% Dextrose in 0.45% normal saline for maintenance, until they started to drink. The time to first analgesic, time to drink, eat and stand/walk (age dependent), as well as time to first void, were recorded by a blinded research assistant. All medications given, and any untoward effects, were recorded by the ward nurse.
Those who did not have a urethral stent inserted during surgery, were discharged home the same day of surgery, provided they drank, were able to walk (age dependent), had adequate pain control on oral medications, and had voided spontaneously. Time to spontaneous voiding was recorded. Children who had a urethral stent inserted intraoperatively were discharged the next day, when meeting the same criteria except for voiding requirement.
On post-operative day (POD) 4, the blinded research assistant (YK) called the parent (or guardian) for a short interview. Number of doses of analgesics, and the times of their administration, were recorded. Recovery parameters, consisting of when the child returned to his normal eating pattern and to his normal level of activity, and an overall parental satisfaction score (0–10) were also recorded.
Data was collected by a blinded research assistant (YK) who followed each child once consent was obtained, throughout the perioperative period, including the telephone interview on POD 4. Data included demographics: age, weight, ASA status, surgical procedure, surgical time and total operating room time, as well as PACU and ward parameters as described. Patients were dropped out of the study if parents requested it at any time, if the procedure was canceled, or changed to one of those listed in the exclusion criteria after randomization was performed.
Statistical analysis of the data was carried out for categorical variables with the χ2 and Fisher exact test where appropriate, for comparison of mean of scale variables ANOVA was used and Tukey test was used for post hoc analysis. Kruskal-Wallis nonparametric test was used when appropriate. A significance level of .05 was used. All analyses were carried out using the IBM® SPSS® 21 for Windows.
Out of 150 children responding to inclusion criteria, due to last minute parental refusal, 116 children between the ages of 4 months and 15 years were recruited. 39 were blindly randomized to the caudal block group (group C), 40 to the fentanyl group (group F), 37 to the dorsal penile nerve block group (group P). Of the two block groups, six had failed blocks and were given fentanyl in the operating room; their pain and recovery data were excluded from analysis. Interviews on POD 4 were obtained in 68 patients (see consort statement, Figure 1).
There was no difference in the mean age, weight, ASA status, surgical or total OR time among the groups (Table 1). All patients were managed intra-operatively with LMA's; no child required intraoperative intubation. No child required PACU stay longer than the expected time, nor was anyone brought back to the OR within 4 days of surgery for revision of surgery.
Pain scores in the PACU were statistically (p < 0.001) lower in the DPNB and caudal block groups compared to the fentanyl group during the first 20 min postoperatively, as detected by the FLACC score and for the first 30 min by the NRS score (Table 2). Pain scores were the lowest in the caudal group during this time period. After the first 30 min, pain scores were not different among the three groups for the rest of their PACU stay and throughout their hospital stay.
The relative risk for patients requiring morphine in the PACU as well as the total morphine consumed (mg) was lowest in the caudal group (p < 0.001) (Table 2). The time elapsed in the PACU to first morphine dose administration among those who required additional analgesia was not different among all groups (Table 2).
Sedation scores were significantly (p < 0.05) higher in the caudal group (Group 1) for the first 30 min in the PACU compared to the fentanyl or the DPNB group (Table 2); this measure paralleled the lower pain scores in the caudal group. There was no difference among the fentanyl and DPNB groups in sedation scores. Past 30 min into the PACU time of stay, the abovementioned higher caudal sedation score disappeared for the rest of the duration of the PACU course.
Nausea and vomiting in the PACU was not different between the study groups (p = 0.09). Respiratory rates as well as oxygen saturation (while breathing room air), both on arrival and on discharge from the PACU, were not different among the three groups. There was no statistical difference in time to eat, void or return to normal activity among the groups (Table 3).
The telephone interview on POD 4 made with the designated parent, showed no differences in the patients' recovery: the time to normal eating, and the home activity patterns were not different in all groups. The number of children who required pain medications at home and their amounts were not different as well, as was the overall parental satisfaction scores (Table 4).
This was a single center, prospective, randomized and double-blinded trial comparing three anesthetic techniques for penile surgery in children: general anesthesia with fentanyl or combined with either caudal or dorsal penile nerve block. We aimed at identifying the technique which would best control post-operative pain and allow optimal return to normal function over the first 4 days after pediatric penile surgery.
We found that during the first 30 postoperative min, both the caudal and penile blocks were associated with lower pain scores and narcotic requirements than the fentanyl group. Recovery of spontaneous voiding was earliest in the penile block group; however, this did not reach statistical significance. There was no difference in parental satisfaction scores or in the child's return to normal activity over four post-operative days.
Many studies have compared different options for pain management after pediatric penile surgery; however, to our knowledge, this is the first that also investigated differences in parental satisfaction during four post-operative days. The Cochrane Database Systematic Review in 2008 concluded that differences in analgesic need could not be detected between caudal, parenteral and penile block methods for circumcision, but that there is a need for more trials (1). More recently, Baird reviewed analgesic methods for pediatric hernia repair; there too, similar to our findings, they found no difference in analgesic outcome between caudal and peripheral blocks by 1 h after surgery (6). Contrary to our finding, Panda showed more effective analgesia up to 8 h after penile surgery with a DPNB and earlier recovery of normal eating compared to general anesthesia with fentanyl (7). A retrospective analysis of caudal vs. penile blocks with and without ultrasound guidance for circumcisions found that fewest caudal patients required intra-operative narcotics and that they had the longest time before requesting supplemental analgesia; the ultrasound guided block was as effective as the caudal in the PACU, but the landmark penile blocks required significantly more narcotics peri-operatively. Similar to our study the differences were recorded through the PACU period only (8).
Caudal blocks are the most common pediatric regional anesthesia used because it is easily performed, reliable and safe (4). There is a perceived preference to caudal blocks in younger pediatric patients in retrospective reports, as the motor block is less of a hindrance to their recovery (8). We had only one failed caudal block and found no difference in age distribution in this randomized and prospective study. We also found that motor block associated with the caudal blocks did not impact on recovery parameters. The likelihood that caudal block is associated with surgical complications in hypospadias surgery, as suggested by Saavedra-Belaunde (9), has been refuted by different studies (10) and meta-analysis (11). Rarely, when DPNB is used, the analgesics may infiltrate the tissues of the dorsal aspect of the penis and distort anatomical planes, which may cause technical difficulties and theoretically affect the procedure's success and final penile appearance. These aspects of caudal block and DPNB were not evaluated in this prospective study which tracked recovery parameters for the first 4 post-operative days.
We defined block failure as the need for supplemental IV fentanyl because of patient's response to surgery. Failure rate was higher in the DPNB group (13.5%) than in the caudal group (2.5%). We performed the DPNB using landmark technique rather than an ultrasound guided technique. Nevertheless, a more recent prospective study by Teunken comparing analgesic outcome using DPNB for circumcision via either the landmark or ultrasound technique found no difference in pain scores or in needs for analgesic supplementations intraoperatively or 24 h postoperatively (12). The failure rate in their study was somewhat higher than ours, 26% in the landmark group; and 36% in the ultrasound-guided group. Sandeman retrospectively compared landmark and ultrasound guided DPNB to caudal blocks in 216 pediatric circumcisions and found that 63% of patients with landmark placed DPNBs required intraoperative narcotics, compared to 5.5% of the caudal-based anesthetics and just 1.7% of the ultrasound placed DPNB. He also found that the landmark placed penile block patients required more morphine in the PACU compared to those with either caudal of ultrasound guided penile blocks (8). Chan and coauthors' retrospective study of more than 700 pediatric penile surgeries reported, similar to our study, that 18% of children treated with dorsal penile blocks required intraoperative supplemental narcotics as compared to 2% of caudal block children and that they had nearly 2.7 times the odds to have a pain score >3/10 in the PACU compared to those with caudal blocks (5).
Our finding that patients with penile blocks had a trend toward earlier return of spontaneous micturition is supported by Metzelder et al. who found less impairment of micturition after hypospadias repair with a DPNB compared to a caudal block (13). Wang et al. as well-reported that an ultrasound-guided dorsal penile nerve block provided comparable analgesia to the caudal block for circumcisions and was associated with a shorter time to spontaneous voiding (14).
This study bears with it several limitations. These include the small number of patients, which is the probable cause for the near statistically significant results. Children from a broad age range were included in this study. It is plausible that blocks may have different effectiveness in different age groups, such as pre-pubertal vs. post-pubertal boys. The small number of participants is not sufficient for sub-analysis of age groups. In addition, the telephone interview (POD 4) was accomplished in approximately half of the cases because many parents did not answer the calls. Their eventual interview upon their postoperative visit (7–10 days after surgery) was discarded since real-time data could not be analyzed with delayed responses. Some of the studied children required urethral stents, while others did not; however, they were equally distributed among the groups, so that results appear not to be biased toward one subgroup. Finally, there were some children who, despite an apparently adequate block during surgery, came to the PACU and required analgesia within the first 0–30 min. Although all were premedicated with midazolam, some of these children might have been agitated or crying on arrival to the PACU because of emergence from the inhaled anesthetics. Due to their high FLACC and parental VAS score, they were therefore medicated with morphine. Analgesia is part of the initial treatment of emergence agitation in non-communicative children (15) and might have introduced an error when analyzing the results.
In conclusion, post-operative pain was initially better controlled with regional anesthesia; however, once immediate analgesics were administered (within the first 30 min after arrival to the PACU), pain scores, analgesia requirements and 4-day recovery, as expressed by time to start eating and the return to normal activity, as determined by parents, were not different among all penile surgery groups of children.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Tel-Aviv Medical Center ethics committee. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
ME concept, design, analysis of data, and drafting of manuscript. YB-Y concept, design, interpretation of data, and drafting of manuscript. YK acquisition and analysis of data. RS interpretation and analysis of data. EA interpretation and analysis of data. JB-C concept, interpretation of data, and revision of manuscript. AW design, interpretation of data, and revision of manuscript. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Cyna AM, Middleton P. Caudal epidural block versus other methods of postoperative pain relief for circumcision in boys. Cochrane Database Syst Rev. (2008) 2008:CD003005. doi: 10.1002/14651858.CD003005
2. Everett T, Koyle M. Editorial comment. Urology. (2018) 118:169–70. doi: 10.1016/j.urology.2017.08.064
3. Bosenberg A. Benefits of regional anesthesia in children. Paediatr Anaesth. (2012) 22:10–8. doi: 10.1111/j.1460-9592.2011.03691.x
4. Walker BJ, Long JB, Sathyamoorthy M, et al. Complications in pediatric regional anesthesia. Anesthesiology. (2018) 129:721–32. doi: 10.1097/ALN.0000000000002372
5. Chan KH, Shah A, Moser EA, Szymansi K, Whittam BM, Misseri R, et al. Comparison of intraoperative and early postoperative outcomes of caudal vs dorsal penile nerve blocks for outpatient penile surgeries. Urology. (2018) 118:164–71. doi: 10.1016/j.urology.2017.08.062
6. Baird R, Guilbault MP, Tessier R, Ansermino JM. A systematic review and meta-analysis of caudal blockade versus alternative analgesic strategies for pediatric inguinal hernia repair. J Pediatr Surg. (2013) 48:1077–85. doi: 10.1016/j.jpedsurg.2013.02.030
7. Panda A1, Bajwa SJS, Sen S, Parmar SS. Penile block for paediatric urological surgery: a comparative evaluation with general anaesthesia. Indian J Urol. (2011) 27:457–64. doi: 10.4103/0970-1591.91432
8. Sandeman DJ, Reiner D, Dilley AV, Bennett MH, Kelly KJ. A retrospective audit of three different regional anaesthetic techniques for circumcision in children. Anaesth Intensive Care. (2010) 38:519–24. doi: 10.1177/0310057X1003800317
9. Saavedra-Belaunde JA, Soto-Aviles O, Jorge J, Escudero K, Vazquez-Cruz M, Perez-Brayfield M. Can regional anesthesia have an effect on surgical outcomes in patients undergoing distal hypospadia surgery? J Pediatr Urol. (2017) 13:45.e1–45.e4. doi: 10.1016/j.jpurol.2016.09.011
10. Splinter WM, Kim J, Kim AM, Harrison MA. Effect of anesthesia for hypospadias repair on perioperative complications. Paediatr Anaesth. (2019) 29:760–7. doi: 10.1111/pan.13657
11. Zhu C, Wei R, Tong Y, Liu J, Song Z, Zhang S. Analgesic efficacy and impact of caudal block on surgical complications of hypospadias repair: a Systematic review and meta-analysis. Reg Anesth Pain Med. (2019) 44:259–67. doi: 10.1136/rapm-2018-000022
12. Teunkens A, Van de Velde M, Vermeulen K, Van Loon P, Bogaert G, Fieuws S, et al. Dorsal penile nerve block for circumcision in pediatric patients: a prospective, observer-blinded, randomized controlled clinical trial for the comparison of ultrasound-guided vs landmark technique. Paediatr Anaesth. (2018) 28:703–9. doi: 10.1111/pan.13429
13. Metzelder ML, Kuebler JF, Glueer S, Suempelmann R, Ure BM, Petersen C. Penile block is associated with less urinary retention than caudal anesthesia in distal hypospadia repair in children. World J Urol. (2010) 28:87–91. doi: 10.1007/s00345-009-0420-2
14. Wang X, Dong C, Beekoo D, Qian X. Dorsal penile nerve block via perineal approach, an alternative to a caudal block for pediatric circumcision: a randomized controlled trial. Biomed Res Int. (2019) 2019:1–7. doi: 10.1155/2019/6875756
Keywords: anesthesia, penis (MeSH), pediatrics - children, surgery, pain
Citation: Ekstein M, Weinbroum AA, Ben-Chaim J, Amar E, Schvartz R, Klein Y and Bar-Yosef Y (2021) Comparison of Caudal Block vs. Penile Block vs. Intravenous Fentanyl Only in Children Undergoing Penile Surgery: A Prospective, Randomized, Double Blind Study. Front. Pediatr. 9:654015. doi: 10.3389/fped.2021.654015
Received: 15 January 2021; Accepted: 03 March 2021;
Published: 26 March 2021.
Edited by:
Ezekiel E. Young, University at Buffalo, United StatesReviewed by:
John Samuel Wiener, Duke University, United StatesCopyright © 2021 Ekstein, Weinbroum, Ben-Chaim, Amar, Schvartz, Klein and Bar-Yosef. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuval Bar-Yosef, eWJhcnlvc2VmQGdtYWlsLmNvbQ==; eXV2YWxieUB0bHZtYy5nb3YuaWw=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.