- 1Life Perspectives, San Diego, CA, United States
- 2Counseling and Testing Center, University of Akron, Akron, OH, United States
Background: The demands on healthcare professionals caring for families grappling with a life-limiting condition in an unborn or newly born child can be overwhelming. Clinicians working in emergency/trauma, hospice, and pediatric settings are already at high risk for burnout and compassion fatigue, which can leave healthcare institutions increasingly vulnerable to poor retention, absenteeism, and waning quality of care. The provision of exemplary palliative care requires a cohesive interdisciplinary team of seasoned professionals resilient to daily challenges. In September 2019, the American College of Gynecology, in a committee opinion, published standard of care guidelines for perinatal palliative care. This has created an impetus for exceptional caregiving and a greater demand for both physician and interdisciplinary healthcare provider education, training, and ongoing support that promotes truly beneficent care for pregnant patients confronted with life-limiting fetal conditions.
Methods: A scoping review of the research literature was conducted in order to distinguish the barriers and facilitators of professional resiliency in perinatal palliative care. PubMed, Medline, CINAHL, and EBSCO Psychology & Behavioral Sciences Collections were systematically reviewed. Because of the paucity of studies specific to perinatal palliative care, several interviews of nurses and physicians in that field were conducted and analyzed for content distinctly pertaining to personal practices or workplace factors that support or hinder professional resiliency.
Results: The research indicated that medical professionals often cite a lack of knowledge, inexperience using effective communication skills related to perinatal palliative care and bereavement, challenges with interdisciplinary collaboration, misconceptions about the role and function of palliative care in the perinatal or neonatal settings, moral distress, and workload challenges as encumbrances to professional satisfaction. Strategic implementation of facility-wide bereavement care training, effective communication modalities, and evidenced-based practical applications are critical components for a thriving perinatal palliative care team. Authentic formal and informal debriefing, peer mentoring, adequate caseloads, robust provider self-care practices, exceptional relational efficacy, and cultural and spiritual humility can foster personal growth and even vicarious resilience for perinatal palliative care professionals.
Conclusions: Support should be strategic and multifaceted. The onus to implement salient measures to cultivate resilience in the perinatal palliative caregiver should not be only upon the individuals themselves but also upon prevailing regulatory governing bodies and healthcare institutions.
Introduction
Perinatal palliative care professionals have an integral role in the decision making and care delivery for many families encountering uncertain perinatal outcomes, some of which may have a reverberating and lasting impact. Palliative care champion Byock (1), in his 1997 book Dying Well, described how the time preceding a death can be a time of personal and spiritual growth for many. Researchers Côté-Arsenault et al. [(2), p. 12] said that “contrary to common societal reaction where focus is on what is wrong with the baby, [the study participants] focused on everything positive about their babies.” The parents also said that their participation in the research study was a positive experience and added meaning to their children's short lives (2). Nurses in a study that explored their reactions to perinatal death revealed that when adequately supported, “growth and transformation” emerged from “the anguish and grief” (3). This article will systematically explore ways that professional caregivers can glean a fecundate resilience and vicarious personal growth sojourning with their patients who are enduring a life-limiting fetal diagnosis.
The loss of a child in infancy can be a profoundly traumatic experience. Psychologists Jaffe and Diamond (4) described in their 2011 book, Reproductive Trauma: Psychotherapy with Infertility and Pregnancy Loss Clients, the hopes and dreams that individuals envision for their future family long before conception. They also portrayed the trauma that can occur when those hopes and dreams go awry. The psychological ramifications when one's fundamental beliefs about themselves and their offspring are disrupted by a life-limiting antenatal diagnosis can be devastating. Lang et al. (5) demonstrated in their research that the death and dying of unborn or newly born children, though culturally disenfranchised, is as emotionally painful as the loss of an older child or adult family member. The researchers also concluded that because of the lack of social support, intrinsic to disenfranchised losses, parents' emotional reactions to perinatal losses tend to be particularly traumatic compared to more traditional types of losses (5). Doka [(6), p. 5] described disenfranchised grief as an experience that “is not openly acknowledged, socially validated, or publicly observed.” The birth and/or untimely death of an infant and the associated grief reaction is outside of typical grieving norms, and parents can find themselves on an unworn path of bereavement.
The emotional impact on families confronted with a life-limiting fetal illness is often complex. At the time of diagnosis, parents may experience a variety of emotions including fear, shock, anger, anxiety, sadness, guilt, and even jealousy of other parents with healthy babies (7). The risk for severe psychological distress including depression, anxiety, and obsessive-compulsive behaviors was shown to be as much as five times higher in parents with a very low birth weight infant in comparison to parents with normal birth weight babies (8). In addition, some families have to cope with financial strain, time away from other family members, long commutes, and travel expenses (8). Furthermore, a couple planning a delivery or termination of a fetus with a life limiting condition is likely to encounter disagreements about their decision from healthcare professionals, family members, and friends. In the absence of multidisciplinary planning and support, the antenatal and postpartum bereavement has the potential to be fraught with ambivalence, shame, secrecy, and isolation. Those involved in the care provision may also find that, in the absence of personal resiliency practices, the persistent emotional strain is unsustainable (9, 10).
Palliative care teams, comprised of multidisciplinary professionals serving inpatient and home environments, are a relatively new concept in medical practice, particularly in pediatrics, and perinatal care. The team usually consists of two or more interdisciplinary professionals with complementary skills who collaborate and move toward common focused goals in the delivery of care (11). Team members often depend on and hold each other accountable for different complex and mutable aspects of palliative care. Perinatal teams are structured like adult and pediatric palliative care teams, which usually include medical care providers, social workers, chaplains, respiratory therapists, and lactation consultants. It is recommended that nurses and physicians in these teams be trained in obstetrics and neonatology (12). Because of improved technology and the earlier diagnoses of genetic anomalies and lethal malformations over the past four decades, expectant couples are now being counseled about the health of their unborn child earlier in the pregnancy. Since the onset of antenatal prognostication, the option of pregnancy termination was initially purported as the only measure to avoid suffering, and comfort-focused alternatives were not developed nor presented as a modality of care (13). Now, couples are being offered a broader spectrum of care that includes palliative and hospice provisions for their unborn (14). Thus, frequent acquiescence of the palliative professional's approach to varied patient care situations is essential, and enduring occupational resiliency is indispensable.
Methods
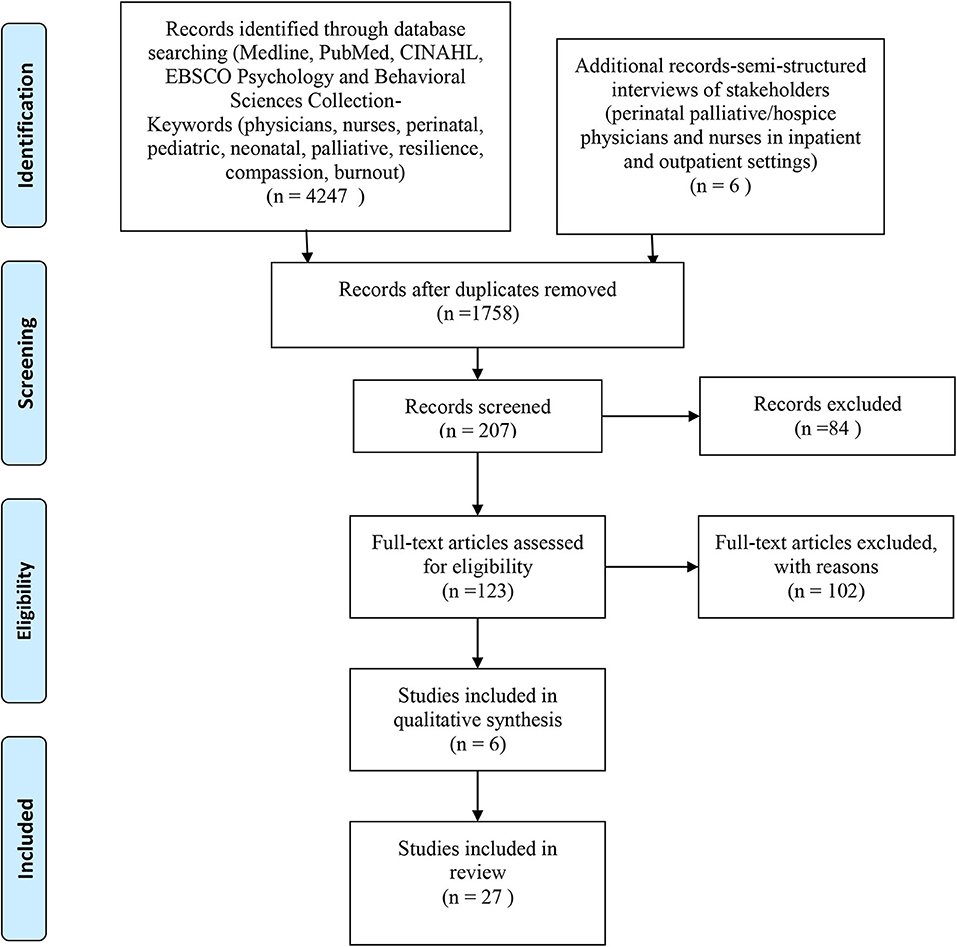
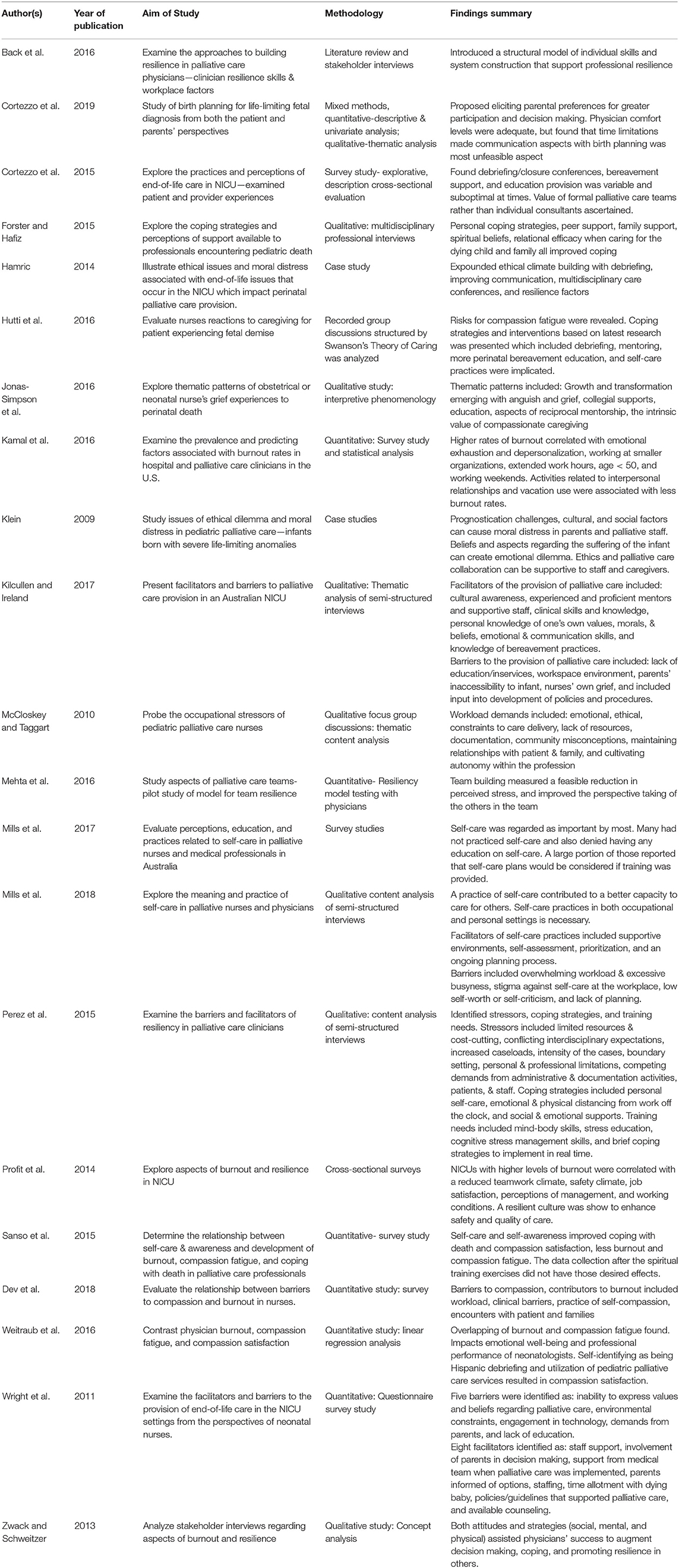
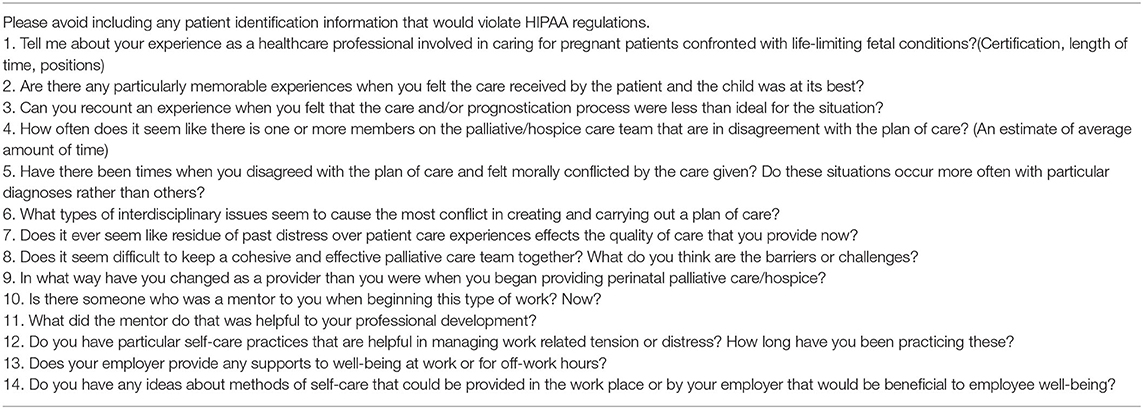
A scoping review according to the methods described by (15) was used to explore and amplify the key factors necessary for promoting professional stability in the perinatal palliative setting (Figure 1). The scope of practice for perinatal palliative care is still evolving, but for the purposes of this study the field of reference was that outlined by the American College of Gynecology (14). There is a body of research that explores various aspects of self-care and supportive measures to prevent compassion fatigue and burnout in healthcare providers in pediatric and palliative settings, but there is a paucity of studies specific to perinatal palliative care. The search included systematic reviews, qualitative case studies, and quantitative survey studies that had been published in the past 11 years (January 2009–January 2020) (Figure 1). Searches were made in PubMed, Medline, CINAHL, and an EBSCO Psychology & Behavioral Sciences Collection. Search words included perinatal, neonatal, and/or palliative combined with the words burnout, compassion fatigue, or resilience. Relevant studies were identified from screening summary and abstracts. Full articles were analyzed for components associated with professional caregiver burnout, compassion fatigue, resilience, and satisfaction (Table 1). In addition, semi-structured interviews were conducted (Table 2). The participants included four registered nurses and two physicians involved in various perinatal palliative and hospice care programs in the following US cities: San Diego, CA; New York, NY; Denver, CO; and Flagstaff, AZ. The interview questions were emailed to the perinatal palliative professionals who had agreed to participate. They either composed and returned written responses or answered the questions in a phone call conducted by the primary author, which were then transcribed. The responses were aggregated and then the content was analyzed for facilitators and barriers to professional resilience by two coders who have graduate level education in nursing or psychology (Table 3). There was no specific funding utilized for the conduction of this study.
Results
Database searches revealed 4,247 studies. Initial review and removal of duplicates, unavailable full-text article, marginal relevance to perinatal palliative care, and language barriers reduced to the search to 123 articles. Another 102 were removed because they did not report primary research. Therefore, 21 articles were selected. The literature review process and content analysis of the interviews yielded the following factors that contribute to distress in neonatal and palliative care professionals: challenges associated with both multi- and interdisciplinary collaboration, gaps in training, moral and ethical issues, misconceptions about the role and function of palliative care in the acute setting, and unfeasible workloads. Alternatively, components that supported resilience and career satisfaction included more comprehensive and interdisciplinary bereavement care training, formal and informal debriefing, supportive measures to strengthen teams and care delivery models, individualized self-care measures, and a humble approach to care provision that included both cultural and spiritual humility.
Discussion
Palliative Care Collaboration
Professionals agree that initiating palliative care and education to the family as soon as possible after the devastating diagnosis procures more salient comfort measures, which, in turn, enhances the significance of the care received (16). Care demonstrated to be effective and relevant can improve caregiver satisfaction and resilience. A registered nurse and clinical coordinator of the Neonatal Comfort Care program at New York's Presbyterian Morgan Stanley Children's hospital, Fran McCarthy, recalled a recent case involving a mother who had just received the initial introduction with the comfort care program and staff when she delivered prematurely. A birth plan and end-of-life options and procedures had not yet been reviewed, nor had there been time to develop a trusting alliance. Consequently, the attending medical resident and nurses were distressed about the despondent mother's demands for continued and prolonged resuscitation measures that were not typically indicated for an infant born in the presented condition. The difficult timing issues resulted in a knowledge gap that, in turn, caused parental and staff distress. In contrast, McCarthy recalled that some of the cases she considered to be most optimal had been those in which the staff and the families had adequate time to prepare and nurture a reciprocal relationship prior to the birth of the child. Karen Christie, Registered Nurse Pediatric/Perinatal Case Manager at The Elizabeth Hospice in San Diego, also recalled that more affirming bereavement experiences occurred for families who had received maximum in-depth training and antepartum palliative care planning. In regard to one memorable encounter, Christie said, “I appreciated having continuity and the experience of being part of a spiritually uplifting situation observing the parents' joy in the life, albeit short, of their son.”
Bereavement care initiated soon after an ominous prenatal diagnosis can address the anticipatory grief that parents often experience and help them cope with a loss that is typically multifaceted (17, 18). Perinatal palliative care teams aim to mitigate the trauma of disenfranchised grief through supportive modalities, ongoing education, and active care for patients and their families throughout the perinatal and bereavement periods (12, 19). In several studies (2, 20–22), Côté-Arsenault demonstrated how professionals providing effective family-centered palliative support can potentially optimize the parents' adjustment to the painful event. Many parents also reported feeling fulfilled and even joyful to have had the short time to parent and love their severely ill children (2, 21).
Moral, Ethical Issues, and Misconceptions
Palliative, neonatal, and obstetric care teams have had to become increasingly flexible to varying patient values and desires for the trajectory of their pregnancy. The increasing scope in the range of care delivery options has not occurred in the absence of moral distress experienced by those providing the care (23–25). When interviewed about the barriers and challenges to keeping a cohesive and effective palliative care team together, the medical director of the Perinatal/Pediatric Hospice Program at The Elizabeth Hospice and a family practice in San Diego, Dr. George Delgado, said the “challenges include emotional stress, compassion fatigue, ethical dilemmas, and cost-cutting across healthcare.” From his experience most of the conflicts are ethical, extending from contrasting societal philosophical axioms influencing healthcare, which can leave professionals in an ideological betwixt and between in the delivery of care. Ethical dilemmas not only surround the termination of a live fetus but also accompany the initiation and continuation of life-sustaining treatments that can be perceived as a prolongation of suffering and an exercise in futility for an infant bound to die (24, 26, 27). Both options are indicated as palliative options on the spectrum of services for those diagnosed with life-limiting fetal malformations by the American College of Obstetrics and Gynecology (14). Emerging perinatal palliative care programs are involved in the provision of comfort care to the neonate that neither aims to hasten death nor aggressively prolong life.
Additionally, moral distress can occur when professionals experience reluctance advocating the interests of their patients for fear of discord with the parental prerogative or institutional constraints (28, 29). Practitioners delivering direct patient care in acute situations are more vulnerable to moral distress, which can lead to burnout and staff retention issues (30, 31). Strategies for addressing and alleviating moral distress include frequent communication with the family, clarifying patient understanding of diagnosis/prognosis, engaging in ongoing goal setting, discussing the ethical issues, increasing team collaborative efforts, and using a skilled ethics facilitator for high levels of distress (23, 32).
Misconceptions surrounding the goals and spectrum of palliative care are often the most challenging aspects of its provision and collaboration amid the dominant curative culture of medicine. Caregivers may also deduce that their service efforts are marginalized when the modality of palliation is disparaged within the healthcare system. Despite decades of research, misunderstandings and erroneous beliefs surrounding the value of palliative care, particularly in the inpatient setting, have been pervasive. Grunauer and Mikesell [(33), p. 3] listed the more prevalent misconceptions regarding the implementation of palliative care in intensive care units as:
[It] is (1) ineffective and unimportant for most ICU patients, (2) synonymous with hospice and hopeless on the part of the family, patients, and/or clinician, (3) equivalent to the “soft skills” that health-care professionals already innately have, and (4) wasteful in that it absorbs valuable time and resources from intensivists.
However, they went on to state that none of these misconceptions were supported by research. In fact, multiple studies show that initiation of palliative care in a timely manner can improve symptom control, professional communication, the patient's perception of their quality of life, and even lengthen survival times (33). Dispelling the myths about palliative care and holistic care for neonates and infants with life limiting conditions and their families can be accomplished with ongoing education provided to the entire caregiving staff within each unit (18, 33, 34). More research and widespread education can enhance the appreciation of palliative care, which can foster a benevolent environment. Dr. Elvira Parravicini, M.D., neonatologist from Columbia University Irving Medical Center, said that “most obstetricians have come along to supporting us after seeing the benefits and appreciation from the patient of what we have done for them.”
Professional Strength
Professional caregivers experiencing distress and high levels of stress have been associated with the development of cynicism, depersonalization of patients, diminished professional satisfaction, impaired decision making, medical errors, increased rates of adverse events, and higher mental and physical morbidities (9, 10, 35). Compassion fatigue or secondary traumatic stress disorder can also occur when empathetic caregivers experience, through a phenomenon known as countertransference, the trauma of their patients. Figley (36) coined the term compassion fatigue when he examined his own reaction to caring for military veterans debriefing from their traumatic combat experiences. He (36) said this regarding the personal anguish he encountered: “We feel the feelings of our clients. We experience their fears. We dream their dreams. Eventually, we lose a certain spark of optimism, humor and hope. We tire. We aren't sick, but we are not ourselves.”
Palliative and hospice professionals have higher rates of burnout and compassion fatigue than most other specialists with rates averaging as much as 61% in some studies (9, 37). Increased levels of distress and burnout can lead to absenteeism and negatively impact the palliative care team (38). Efforts to mitigate burnout and compassion fatigue are not without significant benefits for both the patient and the caregiver (39). Long-term job satisfaction can also flourish from relational efficacy (40).
Fostering Resilience
Hernandez et al. (41) revealed that vicarious resilience occurs when professional caregivers experience their own growth through the provision of care and witness of patients enduring and recovering from traumatic experiences. Author van Dernoot Lipsky [(42), p. 11] wrote, “Those who support trauma stewardship believe that joy and pain are realities of life, and that suffering can be transformed into meaningful growth and healing when a quality of presence is cultivated and maintained even in the face of great suffering.” Therefore, a self-assessment to determine one's level of compassion fatigue or professional satisfaction is essential. The Professional Quality of Life Measure (ProQol) is a tool found to be useful for this appraisal (43). Self-care has been found to be a key aspect in developing resilience and maintaining an instrumental presence in the midst of suffering and loss (10, 35, 44, 45).
Resilience is an individual's ability to cope with adversity and maintain a healthy response to stressors (46). Effective coping and resilience can be nurtured by participation in a variety of self-care practices such as physical activity, mindful focusing, meditation, breathing exercises, and positive interactions with colleagues and friends (47). Hutti [(48), p. 25] found that “nurses reported strength to cope primarily from three sources: faith, relationships with fellow health care providers, and their own families.” Active involvement in a range of personal and employer organized supportive care strategies can augment coping, effective decision-making, and ultimately caregiver resilience in the midst of stressful workplace conditions (40). Dr. Parravinici said in regards to her comfort care team professionals, “We are friends, a tight knit group, and are not afraid to express concerns to each other. My friends care for my psychological needs. For instance, my nurse coordinator tells me things like ‘slow down,' ‘go home,' or ‘be realistic' when I need to hear it.”
A cohesive team is essential to the delivery of effective and beneficial palliative care in the perinatal/neonatal setting. Teams that have a well-defined program mission, vision, and goals that are fully embraced by each of the constituents are in an advantageous position to provide the necessary support for both individual and team resilience (11, 49). When the role of each team member is clearly delineated and in agreement with shared aspects of palliative care, the team as a whole benefits (11). Other aspects that can define the efficacy of a team include clear workload or productivity expectations, established lines of accountability, and a constructive evaluation process (49). Fostering respect and appreciation of the individual team members and the team as a whole requires evolving trust, open communication, prompt conflict resolution, and a shared movement toward common goals. Tempering factors that impair team function such as absenteeism, ongoing conflict, poor team structure, insufficient training, fear of conflict, and lack of commitment and accountability can help mitigate team erosion (49).
Studies have shown that caseloads perceived to be manageable by care providers often coincide with professional satisfaction and resilience. Keeton and colleagues [(50), p. 954] said that the “strongest single predictor of emotional resilience and personal accomplishment was control over schedule and hours worked.” Burnout and emotional exhaustion have been attributed to an increased workload (31, 51, 52). Specifically, palliative care providers reported more difficulty managing increasing caseloads because of the challenges in estimating the length of time needed for the provision of individual care plans, locating the family members involved in the care, and collaborating with the other team members (47, 53). In order to address issues related to absenteeism, employee retention, and burnout, healthcare institutions and legislative entities should carefully examine staffing polices and reimbursement guidelines (9).
Educational Strategies
Lack of education and training has frequently been cited as a barrier to the provision of consistent and comprehensive palliative and bereavement support in the neonatal setting (7, 54–57). Haug et al. (55) demonstrated, in a nationwide study, that fewer than a third of institutions offer any formal training for physicians or staff on perinatal palliative or comfort care. However, research has shown that professionals exhibit better emotional coping when they have been provided with education related to bereavement and end-of-life issues (56, 58–60). For example, a strong majority (91.8%) of neonatologists involved in that study indicated that increased education in perinatal palliative and end-of-life care would be beneficial (55). Elements of self-care activity, as well as the symptoms and risk factors for both burnout and compassion fatigue, should be included in the education for perinatal palliative care professionals (7, 61). An enhanced knowledge base can increase caregiver confidence when serving patients.
A commitment to continuous learning is key to providing the best possible care for patients (62). “Staff education should be provided during orientation and then periodically throughout the course of every year” [(7), p. S30]. Palliative and bereavement care training with a multifaceted approach improves caregiver communication and confidence. Allyson McCullough, Registered Nurse and Bereavement Care Coordinator at Bella Natural Women's Care & Family Medicine and former Bereavement Care Coordinator on an inpatient maternity ward, said, “As a new nurse, I was uncomfortable … and felt that I needed to fill the silence with saying the right thing.” She went on to explain that education and experience have improved her confidence in communicating with and comforting patients.
Wilkinson and Roberts (63) demonstrated that it is most beneficial to use a range of teaching methods to nurture effective communication techniques. Utilizing experts for on-site training to facilitate group analyses of case studies, role-playing exercises, and demonstrations is an effective means of teaching professional caregivers techniques that will improve their comfort level in delivering bad news and confidence in supporting the family. According to Sweeney et al. [(64), p. 14], role-play is particularly impactful, stating:
[It] led to increased understanding of and changes in attitudes toward key palliative care principles, interdisciplinary teamwork, and communication of bad news. There was evidence of increased self-awareness. Findings suggest that the interdisciplinary breaking bad news role-play was a [particularly] rich integrative learning experience valued by students.
Professional caregivers who communicate effectively with parents facing a life-threatening illness in a neonate have been shown to have more professional confidence and better patient rapport. Increasing self-awareness, practicing specific responses via role-play activities, improving eye contact and body language, and learning to mirror a patient's own language are key components of providing quality patient care. Boles [(65), p. 307] asserts that empathy, sensitivity, active listening, a calming presence, and advocacy are essential skills “all nurses and psychosocial staff are called to provide at various points in the patient and family's illness journey.” McCullough also said, “[it] is often not what you say, but [in] the things not said—the non-verbal communication [and] body language, sitting with the family, holding their hand, crying with them, sitting in silence, and meeting them where they are.” Caregivers can provide an environment conducive to emotional healing by acknowledging the individual's feelings, withholding judgmental comments, reassuring them that they are not alone, and essentially giving them permission to grieve.
Patients and families grappling with the life-limiting diagnosis of an unborn or newly born child often report feeling powerless and marginalized in their involvement of care for their child (18). The provision of practical applications to assist the family bonding with and memorializing their severely ill or deceased neonate can empower both the bereaved and the caregivers. Providing personalized care that is directed in part by the patient or parent also fosters relational efficacy and provider resilience (40). Côté-Arsenault (2) said, “Parents in [her] study chose to focus their love and attention on what they could do at the present moment and on memory making,” which included memorialization, photography, and comfort measures. Examples of patient-focused care include recognizing physical cues from the baby and asking the parent to assist in determining their child's needs such as holding, skin-to-skin time, breastfeeding, and assessing for comfort, hunger, thirst, and cold (19).
Formal and Informal Debriefing
Research indicates a beneficial advantage to members of a palliative team when they all participate as a group in scheduled discussions about the plan of care, appropriateness of the interventions, and the need for ongoing intensive support (39, 66, 67). Opportunities for formal debriefing should occur after every death and can be arranged to allow for reflection, quality improvement, shared narrative from the staff, and improved interdisciplinary cohesion (67). Many care teams have found that the utilization of a facilitator at these meetings can enhance the debriefing experience. For employers, it is important to note that stress management modalities and pre-incident education improve effective coping after encountering traumatic events (68).
Informal debriefing to a trusted colleague or mentor immediately or soon after a death or traumatic experience can also assist in mitigating the impact and facilitate personal emotional recovery (50, 69, 70). Also, small groups following a standardized debriefing process can help to ensure that all aspects of the incident were appropriately handled and allow for review from multiple perspectives (68). A nurse educator for the maternal ward at Flagstaff Medical Center reported, “I find that debriefing immediately after a case before going home helps me to relieve that pressure in my heart and in my mind.” She also reported that her employer had provided ample formal debriefing and mental health assistance, which she thought was indeed helpful for those caregivers needing more intense or prolonged assistance.
Care Delivery Models
An institution should consider the manner in which perinatal palliative care is integrated with each unit. Currently there are two palliative care models integrated into the healthcare system. One model comprises a core group of professionals who provide consultation and care for families meeting the criteria for palliative care. Another model of care educates and trains the entire staff to provide palliative care (71). Casarett et al. [(71), p. 653] found that “families reported better outcomes when the patient received care in a palliative unit than they did when the patient received a palliative care consultation.” A pattern of favorable outcomes can fuel compassion satisfaction and foster resilience in the care provider.
In 2002, Catlin and Carter (28) deciphered that those staff members willing to provide perinatal palliative care should be the ones primarily involved in its provision rather than it being required of all in a given unit. However, Mancini (67) countered that all staff members should receive the training to care for any patient they are presented with including those needing end-of-life care. The physicians and nurses I interviewed reported that they had colleagues who had expressed their discomfort with the provision of palliative and end-of-life support and avoided assignments requiring it. A neonatal nurse from Flagstaff, Arizona, said in an interview, “having dedicated members is a challenge because that's usually not the reason why nurses went into this specialty [maternal/child nursing] in the first place … [and] it takes a toll [on the nurse] emotionally, physically, and psychologically.” Her statements underscore the need for increased training in palliative and end-of-life care early on in each professional education track. Ongoing education provided to the entire staff about palliative and end-of-life care should train and equip all staff with basic communication modalities to be compassionate and comforting in their interactions with patients. In 2019, Wool and Catlin [(34), p. S28] reported that “an integrated system of care increases quality and safety and contributes to patient satisfaction. The goal for respectful caregiving throughout the entire hospital system is achievable.” Professionals should feel free to disclose moral distress and receive the debriefing, spiritual, and emotional support necessary for a manageable resolution and promotion of ongoing occupational resilience (67).
In 2018, U.S. reproductive grief care experts Michaelene Fredenburg and Katie Geppert provided training for all staff members of the Ukrainian L'Viv Children's Hospital Perinatal Unit. The nurses who organized the event indicated that a high incidence of neonatal death and the staff's lack of knowledge about reproductive grief were the galvanizing motivations. The entire unit participated in the training including physicians, nurses, medical assistants, and anesthesiologists as well as social workers and a hospital chaplain. Nurses attending to the NICU patients also listened to the presentation on headsets.
Participants were introduced to research and concepts related to the unique nature of reproductive loss (5), disenfranchised grief (6), and the tasks of grieving (72). Evidence-based grief care best practices were shared as well as basic self-care ideas. Frequent staff debriefings were also recommended. After an uncomfortable amount of silence during the time allotted for questions, one of the nurses ventured to admit, “Please don't interpret our silence as disagreement, it's just that we culturally haven't been allowed to discuss this topic. Thank you for giving us the words and for giving us permission to talk to each other and to the parents of our patients.” Concertedly affirmed by the rest of the staff with applause and inquiries, the medical director pledged to adopt the recommended reproductive grief care and self-care policies. Months later, the nurses who had organized the in-service confirmed enhanced patient care and improved staff morale after the training.
Self-Care Initiatives
Self-care is an imperative component to abating compassion fatigue (47, 73). One study reported that only 11% of the participating nurses and doctors practiced self-care [(74), p. 628]. Only 6% of that study's participants had an active self-care plan, and of those respondents “100% reported that they found the use of a self-care plan to be an effective self-care strategy” [(74), p. 627]. Koch and Jones [(30), p. 10] reported, “self-care is not only preventative for practitioners but can serve as a model for family caregivers about the critical importance of self-compassion and care.” Earnest intention to care for oneself can, in turn, result in an enhanced capacity for empathy and the service of others. Progressive resilience can be cultivated through a concerted and intentional effort to develop, implement, and fulfill a self-care plan.
The care provider should make an inventory of aspects of their personal and work practices that contribute to both distress and wellness (40, 46). The dimensions of holistic-wellness plans are multifactorial requiring attention to the mind, body, spirituality, and emotions (47, 75–77). Initially, a plan that includes pertinent goals and methods of accountability should be strategically developed. The anticipation of potential barriers can help the individual avoid being derailed from their pursuit (78). Diligent attention to potential subversions can foster timely attainment of the desired outcomes (79). Enlisting the assistance of a supportive person(s) to partner in the interventions and process of evaluating goals can improve accountability and overall beneficence (80). Care providers find that the creation of a written plan or contract for themselves is a motivating factor for their intended endeavor.
A cadre of wellness programs are often available at larger institutions. Kase et al. [(76), p. 3] found that only 60% of pediatric physicians had participated in those programs and their reasons for not partaking in them included “inconvenience of scheduling” (45.3%), time constraints (27.2%), the preference of participants to “handle things on my own” (34.1%), and the sentiment that partaking in the activity would not be helpful (21.9%). Studies have found that “one-size-fits-all” wellness programs offered by an institution might not effectively address specific needs of their employees and professional affiliates (76, 78, 79). Parravicini concurred, stating, “What people find to be helpful for self-care is a highly individual matter. Some prefer tennis, some skiing, some a walk in the park, others getting a beer.” Individualized discussions regarding the implementation of self-care strategies that include goals to be accomplished outside the work environment and continuing education can be integrated into occupational debriefing and evaluation conversations. Use of a self-administered assessment tool such as the Professional Quality of Life Assessment (43) or the Self-Care Assessment Worksheet (80) in planned intervals can assist in evaluating favorable progression toward the desired benefits (81).
A self-care plan would be ill equipped if it did not involve caring for personal losses. Caregivers cannot adequately assist others when they ignore their own bereavement, and they should not impose nor inject their personal grief experience into the care of others (82). James and Gilliand (82) observed that the palliative care provider can experience bereavement challenges when they encounter multiple meaningful losses in their domestic and occupational environments. They can find themselves overloaded emotionally and need more time to invest in adequate bereavement (82, 83). Obstacles to adequate grieving can occur when the nature of the loss is ambiguous. The absence of physical reminders, shared memories with others, and memorialization of the loss contribute to ambiguity and carrying out of the tasks associated with a typical grieving trajectory (5, 6, 72). When the grieving individual assimilates a healthier pattern of mourning losses through bereavement education and assistance “the knowledge and perspective gained from one's own growth following grief should serve as a quiet reservoir of strength” [(82), p. 461].
Cultural and Spiritual Humility
A humble approach to assess the particular relational, emotional, cultural, and spiritual needs of the patient and family receiving palliative care is essential. In the midst of the suffering inherent to neonatal end-of-life care, healthcare professionals can have a human but irrational tendency to deduce that their clients' anguish could have been avoided with more expert care (11). A reverent but curious approach with not only patients and their families but also with other consulting or attending providers can enhance open, nonjudgmental communication and collaboration (84). Physician and inspirational author Coulehan [(85), p. 206] wrote:
[An] operational definition of medical humility includes four distinct but closely related personal characteristics that are central to good doctoring: unpretentious openness, honest self-disclosure, avoidance of arrogance, and modulation of self-interest. Humility, like other virtues, is best taught by means of narrative and role modeling. We may rightly be proud of contemporary medical advances, while at the same time experiencing gratitude and humility as healers.
In addition, Sasagawa and Amieux [(86), p. 925], researchers of multidisciplinary care collaboration, found that “both quantitative and qualitative analyses revealed that humility was viewed as an important character trait for successful inter-professional collaboration.” Dr. Parravicini exemplified an unassuming approach to patient assessment when she said, “I have to look at each single patient, look to them to tell me through objective signs and cues what to do for them. It is a tremendous gift to learn from my little patients and from their parents.”
Culturally sensitive care is necessary for families enduring the loss of an infant. Caregivers need to be alert and respectful to their clients' cultural, racial, ethnic, spiritual, linguistic, educational, and geographical differences. Cultural competency is a process of gathering knowledge about particular cultural groups; cultural humility is a process of inquiry and interpersonal curiosity approached with openness toward another (87). The pervasive nature of multiculturalism in the United States has made basing cultural competency on knowledge alone increasingly challenging (88). Yancu and Farmer [(89), p. e1–e2] said:
In practice, cultural diversity is manifested in a broad range of ever-changing behaviors, beliefs, rituals, restrictions, traditions, norms, institutions, and relationships that form the basis of cultural knowledge. This makes cultural mastery something akin to trying to grab onto a cloud.
In response to the change, cultural humility is quickly becoming the preferred style to assessing and addressing the cultural needs of patients (90).
Cultural and spiritual humility are conducive to superlative interpersonal communication and relational efficacy contributing to provider compassion satisfaction (88). Nurse researcher Kalu (91) concluded that religious and spiritual beliefs can support and promote better coping for individuals experiencing a reproductive loss. In her study done in Africa, one woman said, “The midwife sat and listened to me. She was very knowledgeable, spiritual and caring. She asked me if I wanted to see the baby. I said yes and spent time with [her]. I have a good memory of [my baby]. That helped me to find ways to adjust and move on knowing that the baby will always be part of my family” [(91), p. 6]. The inference from this patient exemplifies how a provider's reserved but open communication style can support a patient's spiritual beliefs without imposing any religious maxims.
Awareness of one's personal cultural and spiritual values enhances the caregiver's ability to accommodate multicultural and multiracial differences in the patients they serve (90, 92). Appreciation and practice of one's spirituality can promote professional resilience (40, 47, 93, 94). Belcher and Griffiths [(95), p. 271] said that:
Personal spirituality and a knowledge base to support spiritual caregiving were significant factors in hospice nursing staff members' competence and confidence in providing this intimate level of care. Respondents related a commitment to, and the ability to achieve, a level of spiritual care that was highly consistent with the spiritual needs of patients: the need for meaning and purpose in life, the need to give love, the need to receive love, and the need for hope and creativity.
Exploration of one's own cultural and spiritual background, particularly in aspects of family, childbearing, and grieving, can be a journey that enhances receptivity and caregiving satisfaction.
Research and Practice Implications
Larger scale qualitative studies would make a valuable contribution to explicit needs of perinatal palliative care providers particularly in the aspects of occupational misconceptions, moral distress, aspects of humility, and professional resiliency. Quantitative studies on the effectiveness of more widespread bereavement education on patient and professional satisfaction indicators throughout a hospital system could potentially help healthcare systems to mitigate caregiver burnout and turnover. Qualitative and quantitative studies utilized to explore the efficacy of team enhancing interventions and structured debriefing processes may also yield benefits for institutions.
Perinatal palliative care is greatly valued in the lives of those grappling with life-limiting neonatal conditions. Support for those gifted and compassionate professionals who provide the caregiving needs to be strategic and multifaceted. The onus to implement salient measures to cultivate resilience in the perinatal palliative caregiver should not be only upon the individuals themselves, but also upon prevailing regulatory governing bodies and healthcare institutions as well. The implementation of efficacious staffing, debriefing protocols, and ongoing bereavement and self-care education are also vital components to resiliency.
There is a societal trend to minimize the impact of death for those that occur within the perinatal period. It is often erroneously believed that suffering and grieving is obsolete because the unborn or newly born child has not lived long enough to establish themselves. The assumption and commentary that one can “just move on and try to have another one” is incredibly hurtful to those mourning the loss of their child. Perinatal palliative care providers support and become that benevolent community necessary for families to endure and mourn. Parravicini said (96) in an interview, “I'm most proud of the babies because they are so abandoned to our care. In fact, what is unique in our program is that we always put ourselves in the babies' shoes.” She incites a professional humility that can assist perinatal palliative care providers to flourish within the setting of illness and death. “In its relational aspect, humility includes reverence or awe for the grace and strength of patients and their care-givers, a sense that the care-provider is not self-sufficient but needs the care-receiver” [(97), p. 291].
Byock [(98), p. 10] was posed the question from a woman with a terminal diagnosis, “Do I need to die well?” He went on to clarify that by promoting palliative care he had “hoped to dispel the notion that life ends the moment you receive a lousy diagnosis” [(98), p. 11]. He also profoundly concluded that, “it is possible to feel well within oneself and right with the world, even as one dies” and “that therein lies the hope for us all.” [(98), p. 13] The profession of caregiving has traditionally been a trajectory of hope for the future that involves a relationship between the patient and provider. However, in palliative care the aim of care provision is not focused on curing the ailment but on bettering the course of the illness. Professional and personal strengths rise to accommodate the vulnerabilities inherent to perinatal palliative care, but that relational efficacy requires concerted fortification.
Author's Note
Professionals working in perinatal palliative care are at risk for burnout and compassion fatigue because of the emotional, collaborative, and ethical demands associated with the birth and death of infants with life-limiting illnesses. Consequently, healthcare institutions with perinatal palliative programs may be more vulnerable to poor retention, absenteeism, and waning quality of care. Medical professionals often report a lack of knowledge, inexperience in using effective communication skills (i.e., fear of saying the wrong thing), and emotional anguish concurrent with compassion fatigue as reasons for their emotionally avoidant or even irreverent behaviors in bereavement care delivery. Existential suffering and moral distress are common challenges inherent to the provision of care for life limiting neonatal conditions. There is an increased need for physician and interdisciplinary healthcare provider education, training, and ongoing support that promotes beneficial palliative care in the perinatal setting. Support should be to be strategic and multifaceted. The implementation of bereavement care training, effective communication modalities, and evidenced based practical applications are critical components for a thriving perinatal palliative care team. Authentic formal and informal debriefing, peer mentoring, adequate caseloads, robust provider self-care practices, cultural and spiritual humility can foster personal growth and vicarious resilience for perinatal palliative care professionals.
Author Contributions
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
Conflict of Interest
KG was employed by the company Life Perspectives. MF was president and CEO of the company Life Perspectives. PJ was employed by the company Life Perspectives and the University of Akron. KJ was employed by the company Life Perspectives.
References
1. Byock I. Dying Well: Peace and Possibilities at the End of Life. New York, NY: The Berkley Publishing Group. (1997).
2. Côté-Arsenault D, Krowchuk H, Hall WJ, Denney-Koelsch E. We want what's best for our baby: prenatal parenting of babies with lethal conditions. J Prenat Perinat Psychol Health. (2015) 29:157–76.
3. Jonas-Simpson C, Pilkington FB, MacDonald C, McMahon E. Nurses' experiences of grieving when there is a perinatal death. Sage Open. (2013) 3. doi: 10.1177/2158244013486116
4. Jaffe J, Diamond MO. Reproductive Trauma: Psychotherapy with Infertility and Pregnancy Loss Clients. Washington, DC: American Psychological Association. (2010).
5. Lang A, Fleiszer A, Huhammel F, Sword W, Gilbert K, Corsini-Munt S. Perinatal loss and parental grief: the challenge of ambiguity and disenfranchised grief. Omega. (2011) 63:183–96. doi: 10.2190/OM.63.2.e
6. Doka K editor. Disenfranchised Grief: New Directions, Challenges, and Strategies for Practice. Champaign, IL: Research Press (2002).
7. Hall SL, Cross J, Selix NW, Patterson C, Segre L, Chuffo-Siewert R, et al. Recommendations for enhancing psychosocial support of NICU parents through staff education and support. J Perinatol. (2015) 35:S29–36. doi: 10.1038/jp.2015.147
8. Singer LT, Salvator A, Guo S, Collin M, Lilien L, Baley J. Maternal psychological distress and parenting stress after the birth of a very low-birth-weight infant. JAMA. (1999) 281:799–805. doi: 10.1001/jama.281.9.799
9. Kamal AH, Bull JH, Wolf SP, Swetz KM, Shanafelt TD, Ast K, et al. Prevalence and predictors of burnout among hospice and palliative care clinicians in the U.S. J Pain Symptom Manage. (2016) 51:690–6. doi: 10.1016/j.jpainsymman.2015.10.020
10. Sansó N, Galiana L, Oliver A, Pascual A, Sinclair S, Benito E. Palliative care professionals' inner life: exploring the relationships among awareness, self-care, and compassion satisfaction and fatigue, burnout, and coping with death. J Pain Symptom Manage. (2015) 50:200–7. doi: 10.1016/j.jpainsymman.2015.02.013
11. Cherny NI, Fallon MT, Kaasa S, Portenoy RK, Currow, et al. Oxford Textbook of Palliative Medicine. 5th Edn. New York, NY: Oxford University Press. (2015).
12. Carter BS. Pediatric palliative care in infants and neonates. Children (Basel). (2018) 5:21. doi: 10.3390/children5020021
13. Hoeldtke NJ, Calhoun BC. Perinatal hospice. Am J Obstetr Gynecol. (2001) 185:525–8. doi: 10.1067/mob.2001.116093
14. Perinatal palliative care: ACOG committee opinion number 786. Obstetr Gynecol. (2019) 134:e84–9. doi: 10.1097/AOG.0000000000003425
15. Arksey H, O′Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Meth. (2005) 8:19–32. doi: 10.1080/1364557032000119616
16. Taplak AS, Gurol A, Polat S. Nurses' perceptions of the palliative care need of neonates with multiple congenital anomalies. J Hos Pall Nurs. (2020) 22:137–44. doi: 10.1097/NJH.0000000000000628
17. Balaguer A, Martín-Ancel A, Ortigoza-Escobar D, Escribano J, Argemi J. The model of palliative care in the perinatal setting: a review of the literature. BMC Pediatr. (2012) 12:1–6. doi: 10.1186/1471-2431-12-25
18. Kenner C, Press J, Ryan D. Recommendations for palliative and bereavement care in the NICU: a family-centered integrative approach. J Perinatol. (2015) 35 (Suppl. 1):S19-S23. doi: 10.1038/jp.2015.145
19. Parravicini E, Daho' M, Foe G, Steinwurtzel R, Byrne M. Parental assessment of comfort in newborns affected by life-limiting conditions treated by a standardized neonatal comfort care program. J Perinatol. (2018) 38:142–7. doi: 10.1038/jp.2017.160
20. Côté-Arsenault D, Denney-Koelsch E. “My baby is a person”: parents' experiences with life-threatening fetal diagnosis. J Palliat Med. (2011) 14:1302–8. doi: 10.1089/jpm.2011.0165
21. Côté-Arsenault D, Denney-Koelsch E. “Have no regrets:” Parents' experiences and developmental tasks in pregnancy with a lethal fetal diagnosis. Soc Sci Med. (2016) 154:100–9. doi: 10.1016/j.socscimed.2016.02.033
22. Côté-Arsenault D, Donato K. Emotional cushioning in pregnancy after perinatal loss. J Reprod Infant Psychol. (2011) 29:81–92. doi: 10.1080/02646838.2010.513115
23. Hamric AB. A case study of moral distress. J Hosp Palliat Nur. (2014) 16:457–63. doi: 10.1097/NJH.0000000000000104
24. Klein SM. Moral distress in pediatric palliative care: a case study. J Pain Symptom Manage. (2009) 38:157–60. doi: 10.1016/j.jpainsymman.2009.04.014
25. Wool C. State of the science on perinatal palliative care. J Obstet Gynecol Neonatal Nurs. (2013) 42:372–E55. doi: 10.1111/1552-6909.12035
26. Chervenak F, McCullough LB. Responsibly counselling women about the clinical management of pregnancies complicated by severe fetal anomalies. J Med Ethics. (2012) 38:397–8. doi: 10.1136/medethics-2012-100491
27. Blakeley C, Smith DM, Johnstone ED, Wittkowski A. Parental decision-making following a prenatal diagnosis that is lethal, life-limiting, or has long term implications for the future child and family: a meta-synthesis of qualitative literature. BMC Med Ethics. (2019) 20:19. doi: 10.1186/s12910-019-0393-7
28. Catlin A, Carter B. Creation of a neonatal end-of-life palliative care protocol. J Perinatol. (2002) 22:184–95. doi: 10.1038/sj.jp.7210687
29. Garros D. Moral distress in the everyday life of an intensivist. Front Pediatr. (2016) 4:4. doi: 10.3389/fped.2016.00091
30. Koch KD, Jones BL. Support parent caregivers of children with life-limiting illness. Children (Basel). (2018) 5:85. doi: 10.3390/children5070085
31. McCloskey S, Taggart L. How much compassion have I left? an exploration of occupational stress among children's palliative care nurses. Int J Palliat Nurs. (2010) 16:233–40. doi: 10.12968/ijpn.2010.16.5.48144
32. Epstein EG, Hamric AB. Moral distress, moral residue, and the crescendo effect. J Clin Ethics. (2009) 20:330–42.
33. Grunauer M, Mikesell C. A review of the integrated model of care: an opportunity to respond to extensive palliative care needs in pediatric intensive care units in under-resourced settings. Front Pediatr. (2018) 6:9. doi: 10.3389/fped.2018.00003
34. Wool C, Catlin A. Perinatal bereavement and palliative care offered throughout the healthcare system. Ann Palliat Med. (2019) 8 (Suppl. 1):S22–9. doi: 10.21037/apm.2018.11.03
35. Profit J, Sharek PJ, Amspoker AB, Kowalkowski MA, Nisbet CC, Thomas EJ, et al. Burnout in the NICU setting and its relation to safety culture. BMJ Qual Saf. (2014) 23:806–13. doi: 10.1136/bmjqs-2014-002831
36. Figley C. Compassion Fatigue: Coping with Secondary Traumatic Stress Disorder in Those Who Treat the Traumatized. New York, NY: Brunner/Mazel. (1995).
37. Kamal A, Bull J, Wolf S, Samsa G, Ast K, Swetz KM, et al. Burnout among palliative care clinicians in the United States: results of a national survey. J Clin Oncol. (2014) 32 (Suppl. 35):e20530. doi: 10.1200/jco.2014.32.15_suppl.e20530
38. Barrett L, Yates P. Oncology/haematology nurses: a study of job satisfaction, burnout, and intention to leave specialty. Aust Heatlh Rev. (2002) 25:109–21. doi: 10.1071/AH020109
39. Weintraub AS, Geithner EM, Stroustrup A, Waldman ED. Compassion fatigue, burnout and compassion satisfaction in neonatologists in the US. J Perinatol. (2016) 36:1021–6. doi: 10.1038/jp.2016.121
40. Zwack J, Schweitzer J. If every fifth physician is affected by burnout, what about the other four? Resilience strategies of experienced physicians. Acad Med. (2013) 88:382–9. doi: 10.1097/ACM.0b013e318281696b
41. Hernández P, Gangsei D, Engstrom D. Vicarious resilience: a new concept in work with those who survive trauma. Fam Process. (2007) 46:229–41. doi: 10.1111/j.1545-5300.2007.00206.x
42. van Dernoot Lipsky L. Trauma Stewardship. San Fransisco, CA: Berrett-Koehler Publishers. Inc. (2009).
44. Mehta DH, Perez GK, Traeger L, Park ER, Goldmn RE, Haime, et al. Building resiliency in a palliative care team: a pilot study. J Pain Symptom Manage. (2016) 51:604–8. doi: 10.1016/j.jpainsymman.2015.10.013
45. Montgomery AJ. The inevitability of physician burnout: implications for interventions. Burnout Res. (2014) 1:50–6. doi: 10.1016/j.burn.2014.04.002
46. Epstein RM, Krasner MS. Physician resilience: what it means, why it matters, and how to promote it. Acad Med. (2013) 88:301–3. doi: 10.1097/ACM.0b013e318280cff0
47. Perez GK, Haime V, Jackson V, Chittenden E, Mehta DH, Park ER. Promoting resiliency among palliative care clinicians: stressors, coping strategies, and training needs. J Palliat Med. (2015) 18:332–7. doi: 10.1089/jpm.2014.0221
48. Hutti MH, Polvka B, White S, Hill J, Clark P, Cooke C, et al. Experiences of nurses who care for women after fetal loss. J Obstetr Gynecol Neonat Nurs. (2016) 45:17–27. doi: 10.1016/j.jogn.2015.10.010
49. Altilio T, Dahlin C, Tucker R, Remke SS, Weissman DE. Strategies for Maximizing the Health/Function of Palliative Care Teams: A Resource Monograph for the Center to Advance Palliative Care. New York, NY: Center to Advance Palliative Care (2019). Available online at: https://www.capc.org/documents/98/ (accessed on February 18, 2020).
50. Keeton K, Fenner DE, Johnson TR, Hayward RA. Predictors of physician career satisfaction, work-life balance, and burnout. Obstet Gynecol. (2007) 109:949–55. doi: 10.1097/01.AOG.0000258299.45979.37
51. Dev V, Fernando AT 3rd, Lim AG, Consedine NS. Does self-compassion mitigate the relationship between burnout and barriers to compassion? a cross-sectional quantitative study of 799 nurses. Int J Nurs Stud. (2018) 81:81–8. doi: 10.1016/j.ijnurstu.2018.02.003
52. Leiter MP, Maslach C. Six areas of worklife: a model of the organizational context of burnout. J Health Hum Serv Adm. (1999) 21:472–89.
53. Cortezzo DE, Bowers K, Meyer MC. Birth planning in uncertain or life-limiting fetal diagnoses: perspectives of physicians and parents. J of Pall Med. (2019) 22:1337–45. doi: 10.1089/jpm.2018.0596
54. Cortezzo DE, Sanders MR, Brownell EA, Moss K. End-of-life care in the neonatal intensive care unit: experiences of staff and parents. Am J Perinatol. (2015) 32:713–24. doi: 10.1055/s-0034-1395475
55. Haug S, Farooqi S, Wilson CG, Hopper A, Oei G, Carter B. Survey on neonatal end-of-life comfort care guidelines across America. J Pain Symptom Manage. (2018) 55:979–84.e2. doi: 10.1016/j.jpainsymman.2017.10.023
56. Hughes KH, Goodall UA. Perinatal bereavement care: are we meeting families' needs? Br J Midwif. (2013) 21:248–53. doi: 10.12968/bjom.2013.21.4.248
57. Wright V, Prasun MA, Hilgenberg C. Why is end-of-life care delivery sporadic? A quantitative look at the barriers to and facilitators of providing end-of-life care in the neonatal intensive care unit. Adv Neonatal Care. (2011) 11:29–36. doi: 10.1097/ANC.0b013e3182085642
58. Chan MF, Lou FL, Arthur DG, Cao FL, Wu LH, Li P, et al. Investigating factors associate to nurses' attitudes towards perinatal bereavement care. J Clin Nurs. (2008) 17:509–18. doi: 10.1111/j.1365-2702.2007.02007.x
59. Leinweber J, Rowe HJ. The costs of ‘being with the woman': secondary traumatic stress in midwifery. Midwifery. (2010) 26:76–87. doi: 10.1016/j.midw.2008.04.003
60. McCreight BS. Perinatal grief and emotional labour: a study of nurses' experiences in gynae wards. Int J Nurs Stud. (2005) 42:439–48. doi: 10.1016/j.ijnurstu.2004.07.004
61. Braithwaite M. Nurse burnout and stress in the NICU. Adv Neonatal Care. (2008) 8:343–7. doi: 10.1097/01.ANC.0000342767.17606.d1
62. Moore DE, Green JS, Gallis HA. Achieving desired results and improved outcomes: Integrating planning and assessment throughout learning activities. J Contin Educ Health Prof. (2009) 29:1–15. doi: 10.1002/chp.20001
63. Wilkinson S, Roberts A, Aldridge J. Nurse-patient communication in palliative care: an evaluation of a communication skills programme. Palliat Med. (1998) 12:13–22. doi: 10.1191/026921698675034697
64. Sweeney C, O'Sullivan E, McCarthy M. Keeping it real: exploring an interdisciplinary breaking bad news role-play as an integrative learning opportunity. J Scholarsh Teach Learn. (2015) 15:14–32. doi: 10.14434/josotl.v15i2.13262
65. Boles J. Bearing bad news: supporting patients and families through difficult conversations. Pediatr Nurs. (2015) 41:306–8.
66. Hazebroek FW, Smeets RM, Bos AP, Ouwens C, Tibboel D, Molenaar JC. Staff attitudes towards continuation of life-support in newborns with major congenital anomalies. Eur J Pediatr. (1996) 155:783–6. doi: 10.1007/BF02002907
67. Mancini A, Uthaya S, Beardsley C, Wood N, Modi D. Practical Guidance for The Management of Palliative Care on Neonatal Units. London: Chelsea and Westminster Hospital (2014).
68. Vaithilingam N, Jain S, Davies D. Clinical governance, helping the helpers: debriefing following an adverse incident. Obstatr Gynaecol. (2008) 10:251–6. doi: 10.1576/toag.10.4.251.27442
69. Mitchell AM, Sakraida TJ, Kameg K. Critical incident stress debriefing: implications for best practice. Disaster Manag Response. (2003) 1:46–51. doi: 10.1016/S1540-2487(03)00008-7
70. Pratt SD, Jachna BR. Care of the clinician after an adverse event. Int J Obstet Anesth. (2015) 24:54–63. doi: 10.1016/j.ijoa.2014.10.001
71. Casarett D, Johnson M, Smith D, Richardson D. The optimal delivery of palliative care: a national comparison of the outcomes of consultation teams vs inpatient units. Arch Intern Med. (2011) 171:649–55. doi: 10.1001/archinternmed.2011.87
72. Worden JW. Grief Counseling and Grief Therapy: A Handbook for the Mental Health Practitioner, 5th Edn. New York, NY: Springer Publishing Company. (2018).
73. Boyle DA. Countering compassion fatigue: a requisite nursing agenda. Online J Issues Nurs. (2011) 16:2. doi: 10.3912/OJIN.Vol16No01Man02
74. Mills J, Wand T, Fraser JA. Self-care in palliative care nursing and medical professionals: a cross-sectional survey. J Palliat Med. (2017) 20:625–30. doi: 10.1089/jpm.2016.0470
75. Jones SH. A delicate balance: self-care for the hospice professional. Aging Well. (2008) 1:38. Available online at: https://www.todaysgeriatricmedicine.com/archive/spring08p38.shtml
76. Kase SM, Gribben JL, Waldman ED, Weintraub AS. A pilot study exploring interventions for physician distress in pediatric subspecialists. Pediatr Res. (2020) 88:1–6. doi: 10.1038/s41390-020-0805-x
77. Sanchez-Reilly S, Morrison LJ, Carey E, Bernacki R, O'Neill L, Kapo J, et al. Caring for oneself to care for others: physicians and their self-care. J Support Oncol. (2013) 11:75–81. doi: 10.12788/j.suponc.0003
78. Back AL, Steinhauser KE, Kamal AH, Jackson VA. Building resilience for palliative care clinicians: an approach to burnout prevention based on individual skills and workplace factors. J Pain Symptom Manage. (2016) 52:284–91. doi: 10.1016/j.jpainsymman.2016.02.002
79. Mills J, Wand T, Fraser JA. Exploring the meaning and practice of self-care among palliative care nurses and doctors: a qualitative study. BMC Palliat Care. (2018) 17:63. doi: 10.1186/s12904-018-0318-0
80. Saakvitne KW, Pearlman LA, Staff of TSI/CAAP. Transforming the Pain: A Workbook on Vicarious Traumatization. New York, NY: Norton (1996).
81. Alkema K, Linton JM, Davies R. A study of the relationship between self-care, compassion satisfaction, compassion fatigue, and burnout among hospice professionals. J Soc Work End Life Palliat Care. (2008) 4:101–19. doi: 10.1080/15524250802353934
82. James RK, Gilliland BE. Crisis Intervention Strategies, 7th Edn. Belmont, CA: Brooks/Cole (2013).
83. Kilcullen M, Ireland S. Palliative care in the neonatal unit: neonatal nursing staff perceptions of facilitators and barriers in a regional tertiary nursery. BMC Palliat Care. (2017) 16:32. doi: 10.1186/s12904-017-0202-3
84. Back AL, Arnold RM, Baile WF, Fryer-Edwards KA, Alexander SC, Barley GE, et al. Efficacy of communication skills training for giving bad news and discussing transitions to palliative care. Arch Intern Med. (2007) 167:453–60. doi: 10.1001/archinte.167.5.453
85. Coulehan J. “A gentle and humane temper”: humility in medicine. Perspect Biol Med. (2011) 54:206–16. doi: 10.1353/pbm.2011.0017
86. Sasagawa M, Amieux PS. Dispositional humility of clinicians in an interprofessional primary care environment: a mixed methods study. J Multidiscip Healthc. (2019) 12:925–34. doi: 10.2147/JMDH.S226631
87. Hook JN, Davis DE, Owen J, Worthington Jr. EL, Utsey SO. Cultural humility: measuring openness to culturally diverse clients. J Counsel Psychol. (2013) 60:353–66. doi: 10.1037/a0032595
88. Hughes V, Delva S, Nkimeng M, Spaulding E, Turkson-Ocran R, Cudjoe J, et al. Not missing the opportunity: strategies to promote cultural humility among future nursing faculty. J Profession Nurs. (2020) 36:28–33. doi: 10.1016/j.profnurs.2019.06.005
89. Yancu CN, Farmer DF. Product or process: cultural competence or cultural humility? Palliat Med Hosp Care Open J. (2017) 3:e1–4. doi: 10.17140/PMHCOJ-3-e005
90. Waters A, Asbill L. Reflections on Cultural Humility: Given the Complexity of Multiculturalism, it Is Beneficial to Understand Cultural Competency as a Process Rather Than an End Product. American Psychological Association (2013). Available online at: https://www.apa.org/pi/families/resources/newsletter (accessed on February 19, 2020).
91. Kalu AF. Women's experiences of utilizing religious and spiritual beliefs as coping resources after miscarriage. Religions. (2019) 10:185. doi: 10.3390/rel10030185
92. Richardson P. Spirituality, religion and palliative care. Ann Palliat Med. (2014) 3:150–9. doi: 10.3978/j.issn.2224-5820.2014.07.05
93. Maytum JC, Heiman MB, Garwick AW. Compassion fatigue and burnout in nurses who work with children with chronic conditions and their families. J Pediatr Health Care. (2004) 18:171–9. doi: 10.1016/j.pedhc.2003.12.005
94. Forster E, Hafiz A. Paediatric death and dying: exploring coping strategies of health professionals and perceptions of support provision. Int J Palliat Nurs. (2015) 21:294–301. doi: 10.12968/ijpn.2015.21.6.294
95. Belcher A, Griffiths M. The spiritual care perspectives and practices of hospice nurses. J Hosp Palliat Nur. (2005) 7:271–79. doi: 10.1097/00129191-200509000-00014
96. Mariani L. Before death there is life. Communion and Liberation. (2019). Available online at: https://english.clonline.org/stories/encounters/2019/01/12/before-death-there-is-life
97. Lebacqz K. Humility in health care. J Med Philosophy. (1992) 17:291–307. doi: 10.1093/jmp/17.3.291
98. Byock I. Do I need to die well? sharing a personal growth experience. Touching lives. (2010) 2:10–3. Available online at: https://www.todaysgeratricmedicine.com/archive/spring08p38.shtml
Keywords: perinatal, palliative, compassion, burnout, ethical, self-care, grief, resiliency
Citation: Grauerholz KR, Fredenburg M, Jones PT and Jenkins KN (2020) Fostering Vicarious Resilience for Perinatal Palliative Care Professionals. Front. Pediatr. 8:572933. doi: 10.3389/fped.2020.572933
Received: 15 June 2020; Accepted: 26 August 2020;
Published: 08 October 2020.
Edited by:
Elvira Parravicini, Columbia University, United StatesReviewed by:
Rochelle Steinwurtzel, Columbia University, United StatesJohn Yohan Rhee, Massachusetts General Hospital and Harvard Medical School, United States
Copyright © 2020 Grauerholz, Fredenburg, Jones and Jenkins. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kathryn R. Grauerholz, a2F0aHJ5bkBsaWZlcGVyc3BlY3RpdmVzLmNvbQ==
 Kathryn R. Grauerholz
Kathryn R. Grauerholz Michaelene Fredenburg
Michaelene Fredenburg Premala Tara Jones
Premala Tara Jones Kristy N. Jenkins
Kristy N. Jenkins