- Pediatric Unit Sant'Andrea Hospital, NESMOS Department, Faculty of Medicine and Psychology, “Sapienza” University, Rome, Italy
Introduction
The worldwide Covid-19 outbreak has challenged our rules to manage pediatric patients with chronic respiratory diseases, particularly asthma. The spread of the novel coronavirus causing severe acute respiratory syndrome (SARS-Cov-2) constrained most countries to adopt drastic infection control strategies for health-care facilities (1, 2). Several Respiratory Societies have developed recommendations to protect patients and health-care staff in pulmonary function laboratories (3–6). These documents advise restriction of pulmonary function tests (PFTs) to those deemed essential, namely, spirometry and diffusion capacity measurements, in line with their clinical relevance and the epidemic phase. When testing is pertinent, infection prevention and control measures in the laboratory are required, including the disinfection of instruments, room cleaning, ventilation, and protective measures for patients and health personnel (3–6).
Notwithstanding the preceding measures, the risk of exposure to viral loads of SARS-Cov-2 following active respiratory maneuvers is not negligible. Consequently, all aerosol-generating procedures (AGPs) are discouraged, and no bronchial provocation tests are allowed.
Recommendations prevent spirometry in any child with suspected/confirmed Covid-19 (4, 6); on the other hand, the clinical picture of worsening asthma or an asthma exacerbation substantially overlaps with Covid-19 (7).
A recent consensus suggests screening patients for high-risk exposures, fever, and symptoms suggestive of COVID-19, ideally in two phases: within 3 days and upon arrival for medical visits when PFTs are due to be carried out. Alternatively, testing for SARS-CoV-2 patients within 72 h of their appointment (8). Patients reporting new symptoms upon arrival (even if previously tested negative for SARS-CoV-2) should be considered as suspected cases of COVID-19. In confirmed or suspected cases of COVID-19, resolution of symptoms and two negative tests for SARS-CoV-2 collected ≥24 h apart are required (6, 8). These patients could be rescheduled for PFTs after an interval without symptoms and fever since at least 10 days from their onset or, if asymptomatic, at least 10 days from their first positive test (8).
Execution of PFTs in patients coming from high prevalence settings [i.e., high-risk patients, require a negative pressure room (4, 8)]. The staff should wear an N95 mask, face shield, gown, and gloves; consumables must be managed within the risk area. Patients should wear a surgical mask between measures; both patients and staff should follow protocols on safe distance and hand washing. Metered dose inhalers (MDI) must replace nebulizers for assessing the bronchodilator response. Room and equipment disinfection, ventilation, and timing between patients are compulsory (4, 8).
Optional home spirometry can be useful for children needing close surveillance of pulmonary function (discussed in the last section).
Questions on the Need for Alternative Tests
While restrictions in the pulmonary function laboratory will change as the disease prevalence changes, several questions remain: shall we continue monitoring airway patency/responsiveness (i.e., bronchodilation with beta-agonists) with spirometry as the sole measurement tool? Could we offer alternative PFTs to asthmatic children? If so, what is the rationale for considering this alternative?
Small airways dysfunction in asthma is now widely recognized (9–11). Spirometric variables such as FEV1 are affected by flow resistance at the large airways. This fact may explain why spirometry poorly correlates with symptoms and why only markedly decreased FEV1 values (<60%) predict disease exacerbations (12). On the other hand, visual inspection of flow-volume curves and assessment of bronchodilation help clinical decisions (12, 13).
Spirometry is effort dependent and requires expertise (13). However, it is just the “forced” nature of spirometry that allows enhancing viral diffusion nearby from a potentially infected patient. The maneuver itself, which involves a maximum inspiration followed by an explosive and prolonged expiration, induces cough and the release of droplets in the environment (4). To note, young patients often require a high number of attempts to achieve a reliable flow-volume curve (13, 14).
Measurements of Respiratory Resistance
Alternative tests are already available in many pulmonary function laboratories. The forced oscillation technique (FOT) provides information on airway patency/responsiveness in terms of respiratory system impedance (Zrs) and its components, respiratory resistance (Rrs) and reactance (Xrs), during the patient's quiet breathing. Small oscillations are applied passively with a wave-emitting source (a loudspeaker) connected to the patient's mouth opening while cheeks are supported by the child or an operator. The pressure and flow relationship are then used to calculate Rrs, Xrs, the resonant frequency (Fres), and the area under the reactance curve (AX) (15). Waves can be delivered as a single frequency or multiple-single frequencies; another delivery method employs a train of pulses, the so-called impulse oscillometry (IOs) (15–17). Among the Zrs components, Xrs represents counteracting inertial and elastic forces of the respiratory system (chest wall, lung, airway tissues, and gas column moving inside). Both Rrs and Xrs are frequency-dependent; thus, frequencies >4 HZ can easily reach the peripheral airways whereas high frequencies (>20 HZ) reflect frictional forces of the proximal airways and surrounding tissues (15, 16). Frequencies between 4 and 10 Hz are retained clinically relevant for children (16). For these frequencies, the within-subject coefficient of variation in Rrs (CV = SD/mean × 100) varies between 6.2 and 8.0% for children aged 3–16 years (14). Both Rrs and Xrs measures are repeatable over 2 weeks (18). Day-to-day Rrs variability is higher in asthmatic children than in healthy controls; this variability is associated with disease severity and symptom control (19).
The clinical utility of FOT measurements for assessing airway obstruction and bronchial response to bronchodilators has been recently summarized (15, 16, 20). Differences between techniques and patients' selection criteria lead to contrasting results when airway patency of healthy and wheezy children is compared at baseline; instead, most studies agree in the ability of FOT for assessing changes in the airway caliber (Table 1). The entity of Zrs largely depends on standing height; thus, laboratories need to construct their reference values or to adopt those appropriated to their population (15). A decrease of at least −40% in Rrs and an increase of at least +50% in Xrs are considered thresholds for a bronchodilator response (15). Still, bronchodilator doses differ between studies (15, 20). Though several reference values have been provided for the different techniques, a call for standardization of these techniques is still evident (15–17, 20). The use of reference equations from studies whose population and devices most closely approximate the local situation has been recommended (15). In the absence of appropriated reference equations, the “personal best” measurement could be recorded as a reference point for the individual patient, to guide therapeutic decisions.
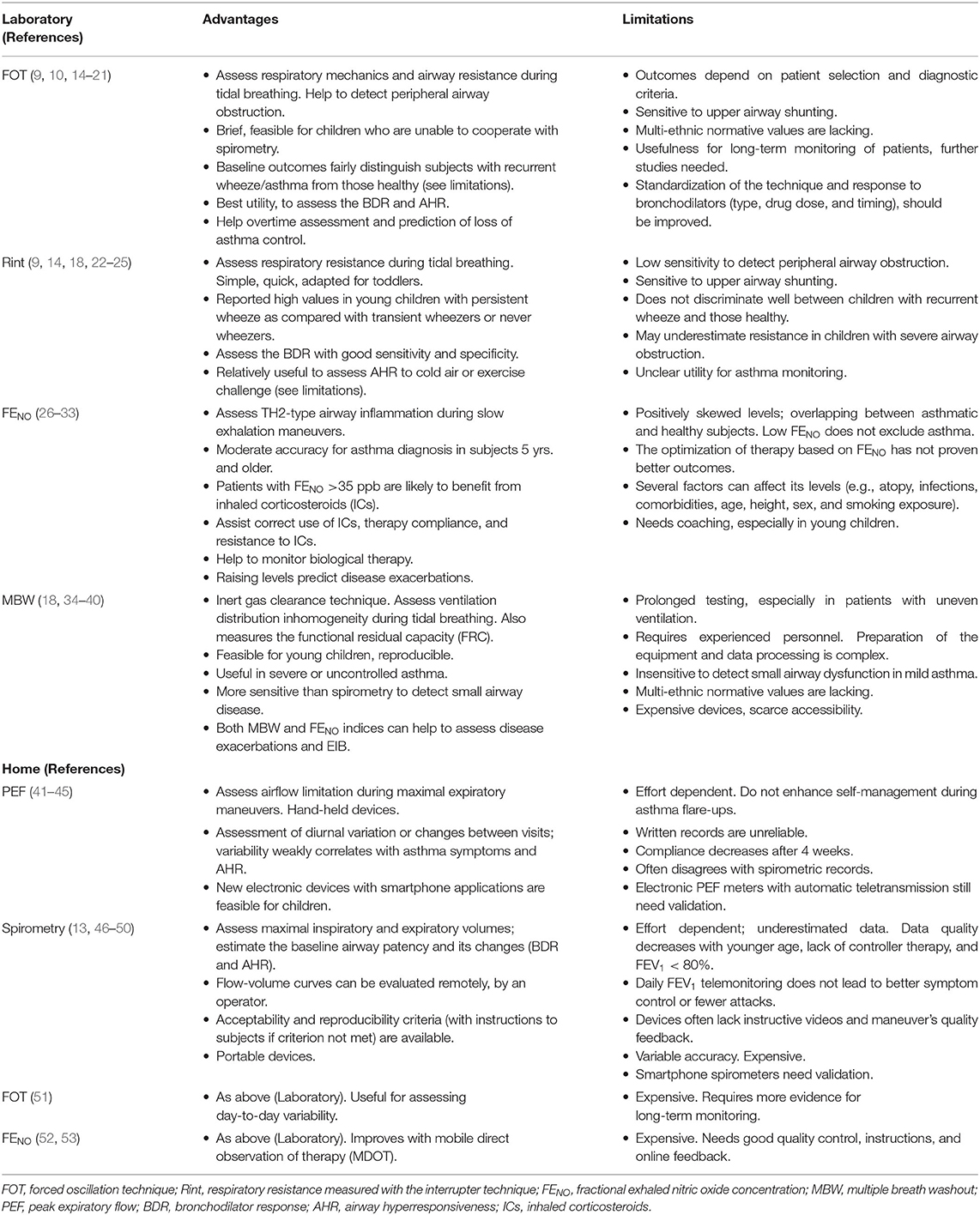
Table 1. Alternative pulmonary function tests (PFTs) for asthmatic children during the Covid-19 pandemic.
A modified FOT method that measures the tidal volume dependence on airway resistance has been recently described (21). This method, based on the change of within-breath Rrs at zero flow (end-expiration vs. end-inspiration), improves the ability to detect acute airway obstruction in young children (21). Advantages of FOT over spirometry and other tests of airway resistance have been described recently (9). Yet, a systematic review could not disclose enough evidence to place FOT as an adjunct or as a substituent of spirometry (10). Despite the FOT gaining interest, the lack of familiarity with the technique, lack of equipment, and complexity of analysis still limit its wider adoption.
Estimates of airway resistance can be also obtained with the interrupter technique (Rint). The child is invited to sit with the neck in a neutral position, to wear a nose clip, and to breathe normally through a mouthpiece and microbial filter. An automated valve briefly occludes the airway opening at the end-expiratory phase, lasting 100 ms; the resultant pressure is divided by the flow immediately preceding the interruption to estimate airway resistance (14). As for the oscillometer, cheek support is required. The assumption is that alveolar and mouth pressure equilibrate after occlusion. This technique is simple, quick to perform, and suitable in younger children. Rint measurements mostly represent airway resistance but also a small resistance from lung tissues and chest wall (14). The within-subject variability in healthy children is close to 12% (14, 18). However, the wide between-subject CV in health leads to overlap values with those obtained in children with recurrent wheeze (18). Baseline Rint measurements have low sensitivity to detect bronchial obstruction but perform better for assessing bronchial response to bronchodilators (BDR) (14, 22, 23). A reliable BDR has been reported for a decrease in Rint ≥ 0.26 kPa L−1s from baseline or −1.25 Z-scores (22).
Measurements of respiratory resistance have a long history (14, 54); still, they must gain a wider consensus among general practitioners and pulmonologists. While airway resistance could be measured with body plethysmography, it has inconvenience in the pandemic context such as the need for thorough disinfection of the box and execution difficulties for younger children. Instead, oscillometry and Rint techniques are available with smaller devices and are simple to perform in the Lab. Another advantage of these procedures is that the operator can be placed behind the child during the breathing maneuvers and his participation to support the child's cheeks is required only for toddlers. Acquisition time is also reduced for these tests. For instance, during oscillometry, the minimal acquisition time for children under 12 years of age is 16 s (15). Both FOT and Rint devices are small and supplied with appropriated in-line antimicrobial filters. Some instruments (e.g., Resmon Pro Full) store outcomes automatically in a pen drive, so the operator can evaluate the results safely, outside the laboratory. The advantages and limitations of FOT and Rint are reported in Table 1.
Exhaled Nitric Oxide (NO)
The fractional concentration of exhaled nitric oxide (FENO) has been studied in the last decades for assessing asthmatic patients, including children; guidelines on standardized methods are still valid (26). This free radical is a helpful non-invasive biomarker of the atopic-eosinophilic (Th2-type) airway inflammation (26, 27). A robust model with FENO, together with blood eosinophil counts and other biomarkers of IL-13–driven gene expression (serum CCL17 and CCL26), has been recently developed; this model identifies Type 2-high asthma patients with positive and negative predictive values of 100 y and 87%, respectively (28).
The test requires a deep inspiration followed by a constant slow exhalation into the analyzer across an in-line microbial filter. A target expiratory flow rate of 50 ml/s, against an expiratory resistance between 5 and 20 cmH2O, is required to close the soft palate and to exclude contamination from nasal NO. Exhalations of at least 4 s can be sufficient to achieve a NO plateau. Schoolchildren usually can perform the classic maneuver; toddlers need audiovisual coaching and the use of dynamic flow restrictors to maintain a constant expiratory flow rate (26).
FENO measurements help in asthma diagnosis if taken together with the clinical history; FENO also assists in evaluating the therapeutic response to oral or inhaled corticosteroids and predicts disease exacerbations after treatment withdrawal (29). Because FENO is a phenotype-linked biomarker, it is suited for monitoring children on biological therapy (30). A recent systematic review and meta-analysis support the diagnostic accuracy of FENO testing in pediatric asthma (31). Overall, FENO levels over 35 ppb in children indicate eosinophilic airway inflammation and changes below or above 20% between visits are consistent with either response to anti-inflammatory therapy or with a need for adjusting therapy, respectively (29).
Peripheral and proximal airway contributions of exhaled NO can be calculated from exhalations at several flow rates, using the two-compartment model (55). Their employ has been reported useful to distinguish disease patterns in asthmatic patients (32). However, most studies agree on the role of partitioned-NO airway parameters to assess exercise-induced bronchoconstriction (EIB), a hint of poor disease control (34, 56, 57). Recently, we found that increased concentrations of both alveolar NO (CaNO) and urinary adenosine predicted EIB in atopic asthmatic children (33). Because exercise bronchial challenge is an AGP, surrogates of EIB such as partitioned-NO parameters could replace the traditional challenge at this time.
An advantage of FENO testing is the low-target expiratory flow rate that needs only slow exhalation maneuvers. FENO analyzers are small; also, handheld devices help for daily home monitoring (Table 1).
Multiple Breath Washout (MBW)
Small airway dysfunction and ventilation heterogeneity are relevant in asthma (11, 18, 35–37). Uneven ventilation can be assessed through inert gas dilution during tidal breathing: washout of the resident nitrogen with 100% oxygen, or initial wash-in of an exogenous gas (e.g., sulfur hexafluoride, SF6), and washout thereafter. Initial and final tracer gas concentrations allow measuring the resting volume [i.e., the functional residual capacity (FRC)]. When the dilution process achieves 1/40th of the initial gas concentration, the “Lung clearance index” (LCI) is then calculated as the cumulative expired volume (CEV) during the procedure divided by the FRC:
LCI = CEV/FRC.
This index means how many “turnovers” are required to clear the subject's FRC and reflects the extent of its ventilation distribution inhomogeneity. Young children usually cooperate with the test; they need coaching to breath normally while seated, wearing a mouthpiece with in-line microbial filter. Gas leaks should be avoided during the process (11, 38).
There is a slight inverse relationship between LCI and age in schoolchildren. Reports on upper limits for normal LCI vary between 7.0 and 7.9 in subjects aged 6–18 years, depending on the technique (39). Children with severe asthma have elevated LCI values as compared to those with a mild-to-moderate disease or healthy controls. However, many patients with severe disease yield LCI values within the normal range (11, 36).
Presence of high LCI values in subjects whose FEV1 is normal suggests ongoing small airway dysfunction (37). A recent study shows that both LCI and FENO (but not FEV1) concordantly improved 4 weeks after a systemic steroid dose in children with severe therapy-resistant asthma (35).
Some devices can analyze the phase III of each tidal breath to estimate the conductive (Scond) and acinar (Sacin) contributions to inhomogeneity. Scond better correlates with LCI than Sacin (11, 37).
The clinical application of these indexes still needs to be established. See also in Table 1. Using the MBW technique during this pandemic requires caution. Tidal breathing PFTs generate small particles (≤0.5 μm) at the equipment inhalation port, even if at lower amounts than forced expiratory maneuvers (58). The main concerns with MBW testing are prolonged breathing (and room stay) and possible gas leaks. Requirements for testing high-risk patients (see Introduction) are advisable.
Home PFT Measurements
Several home PFTs have been developed with the aim to enhance patients' self-management (41, 47). Their use helps to overcome the infection control issues, as compared with laboratory tests. Most of these PFTs regard PEF and spirometry (13, 41–47, 51–53). Unsupervised measurements tend to be lower at home than in the laboratory, suggesting the need for patients' coaching (59, 60). Telemonitoring with visual coaching and automatic feedback for outcomes is promising, but its clinical utility remains unclear (13, 49). Daily home FEV1 telemonitoring did not reduce exacerbations in children with severe asthma (49). A recent Cochrane review found no additional benefits of telemonitoring for asthma control or exacerbations, over usual asthma care (50). Devices differ widely on their inclusion of instructive videos, graphical descriptions, and immediate feedback on the quality of the breathing maneuver (47) (Table 1).
Conclusion
The unpredictable duration of the Covid-19 pandemic imposes infection prevention and control measures in ambulatory settings with a pulmonary function. In keeping with these preventive actions, pulmonary function procedures offering quiet breathing or slow expiration are suitable for testing asthmatic children. Measurements of airway resistance (Oscillometry, Rint), and FENO, can help respiratory physicians to manage their patients until spirometry and bronchoprovocation tests can be resumed. The MBW test relies on the need to evaluate ventilation inhomogeneity in children with severe disease. Standardization of these PFTs and improvement of home telemonitoring are priorities, given this and other infectious community threats.
Author Contributions
MB and MV conceived and designed the text body. MB wrote the manuscript. ME, MM, and SM helped for searching the literature and reviewed critically the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. World Health Organization. Infection prevention and control during health care when COVID-19 is suspected: interim guidance, 19 March. (2020). World Health Organization. (2020). Available online at: https://apps.who.int/iris/handle/10665/331495 (accessed April 25, 2020).
2. CDC - Centers for Disease Control and Prevention. Outpatient and Ambulatory Care Settings: Responding to Community Transmission of COVID-19 in the United States. (2020). Available online at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/ambulatory-care-settings.html (accessed June 06, 2020).
3. McCormack MC, Kaminsky DA. 2020 members of the ATS Proficiency Standards for Pulmonary Function Testing Committee. Advice Regarding COVID 19 for Pulmonary Function Laboratories. (2020). Available online at: www.thoracic.org/professionals/clinical-resources/disease-relatedresources/pulmonary-function-laboratories.php (accessed May 31, 2020).
4. European Respiratory Society Groups 9.1 and 4.1. Recommendation from ERS Group 9.1 (Respiratory function technologists /Scientists). Lung function testing during COVID-19 pandemic and beyond. (2020). Available online at: https://ers.app.box.com/s/zs1uu88wy51monr0ewd990itoz4tsn2h (accessed May 31, 2020).
5. ARTP and British Thoracic Society. Respiratory Function Testing During Endemic COVID-19. Version 1.5. (2020). Available online at: https://www.artp.org.uk/COVID19 (accessed May 31, 2020).
6. Bignamini E, Cazzato S, Cutrera R, Ferrante G, La Grutta S, Licari A, et al. Italian pediatric respiratory society recommendations on pediatric pulmonary function testing during COVID-19 pandemic. Ital J Pediatr. (2020) 46:68. doi: 10.1186/s13052-020-00829-0
7. Abrams EM, Szefler SJ. Managing asthma during coronavirus disease-2019: an example for other chronic conditions in children and adolescents. J Pediatr. (2020) 222:221–6. doi: 10.1016/j.jpeds.2020.04.049
8. Wilson KC, Kaminsky DA, Michaud G, Sharma S, Nici L, Folz RJ, et al. Restoring pulmonary and sleep services as the COVID-19 pandemic lessens: from an association of pulmonary, critical care, and sleep division directors and American thoracic society-coordinated task force. Ann Am Thorac Soc. (2020). doi: 10.1513/AnnalsATS.202005-514ST. [Epub ahead of print].
9. Kaminski DA. What does airway resistance tell us about lung function? Respir Care. (2012) 57:85–96. doi: 10.4187/respcare.01411
10. Dos Santos K, Fausto LL, Camargos PAM, Kviecinski MR, da Silva J. Impulse oscillometry in the assessment of asthmatic children and adolescents: from a narrative to a systematic review. Paediatr Respir Rev. (2017) 23:61–7. doi: 10.1016/j.prrv.2016.09.002
11. Nuttall AGL, Velásquez W, Beardsmore CS, Gaillard EA. Lung clearance index: assessment and utility in children with asthma. Eur Respir Rev. (2019) 28:190046. doi: 10.1183/16000617.0046-2019
12. Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention, (2020). Available online at: www.ginasthma.org (accessed May 11, 2020).
13. Graham BL, Steenbruggen I, Miller MR, Barjaktarevic IZ, Cooper BG, Hall GL, et al. Standardization of Spirometry 2019 update. An official american thoracic society and european respiratory society technical statement. Am J Respir Crit Care Med. (2019) 200:e70–88. doi: 10.1164/rccm.201908-1590ST
14. Beydon N, Davis SD, Lombardi E, Allen JL, Arets HG, Aurora P, et al. An official American Thoracic Society/European Respiratory Society statement: pulmonary function testing in preschool children. Am J Respir Crit Care Med. (2007) 175:1304–45. doi: 10.1164/rccm.200605-642ST
15. King GG, Bates J, Berger KI, Calverley P, de Melo PL, Dellacà RL, et al. Technical standards for respiratory oscillometry. Eur Respir J. (2020) 55:1900753 doi: 10.1183/13993003.00753-2019
16. Skylogianni E, Douros K, Anthracopoulos MB, Fouzas S. The forced oscillation technique in paediatric respiratory practice. Paediatr Respir Rev. (2016) 18:46–51. doi: 10.1016/j.prrv.2015.11.001
17. Soares M, Richardson M, Thorpe J, Owers-Bradley J, Siddiqui S. Comparison of forced and impulse oscillometry measurements: a clinical population and printed airway model study. Sci Rep. (2019) 9:2130. doi: 10.1038/s41598-019-38513-x
18. Rosenfeld M, Allen J, Arets BH, Aurora P, Beydon N, Calogero C, et al. An official American Thoracic Society workshop report: optimal lung function tests for monitoring cystic fibrosis, bronchopulmonary dysplasia, and recurrent wheezing in children less than 6 years of age. Ann Am Thorac Soc. (2013) 10:S1–11. doi: 10.1513/AnnalsATS.201301-017ST
19. Robinson PD, Brown NJ, Turner M, Van Asperen P, Selvadurai H, King GG. Increased day-to-day variability of forced oscillatory resistance in poorly controlled or persistent pediatric asthma. Chest. (2014) 146:974–81. doi: 10.1378/chest.14-0288
20. Alblooshi A, Alkalbani A, Albadi G, Narchi H, Hall G. Is forced oscillation technique the next respiratory function test of choice in childhood asthma. World J Methodol. (2017) 7:129–38. doi: 10.5662/wjm.v7.i4.129
21. Czövek D, Shackleton C, Hantos Z, Taylor K, Kumar A, Chacko A, et al. Tidal changes in respiratory resistance are sensitive indicators of airway obstruction in children. Thorax. (2016) 71:907–15. doi: 10.1136/thoraxjnl-2015-208182
22. Mele L, Sly PD, Calogero C, Bernardini R, Novembre E, Azzari C, et al. Assessment and validation of bronchodilation using the interrupter technique in preschool children. Pediatr Pulmonol. (2010) 45:633–8. doi: 10.1002/ppul.21210
23. Beydon N, Mahut B, Maingot L, Guillo H, La Rocca MC, Medjahdi N, et al. Baseline and postbronchodilator interrupter resistance and spirometry in asthmatic children. Pediatr Pulmonol. (2012) 47:987–93. doi: 10.1002/ppul.22526
24. Delacourt C, Lorino H, Fuhrman C, Herve-Guillot M, Reinert P, Harf A, et al. Comparison of the forced oscillation technique and the interrupter technique for assessing airway obstruction and its reversibility in children. Am J Respir Crit Care Med. (2001) 164:965–72. doi: 10.1164/ajrccm.164.6.2010153
25. Caudri D, Wijga AH, Hoekstra MO, Kerkhof M, Koppelman GH, Brunekreef B, et al. Prediction of asthma in symptomatic preschool children using exhaled nitric oxide, Rint and specific IgE. Thorax. (2010) 65:801–7. doi: 10.1136/thx.2009.126912
26. American Thoracic Society, European Respiratory Society. ATS/ERS recommendations for standardized procedures for the online and offline measurement of exhaled lower respiratory nitric oxide and nasal nitric oxide, 2005. Am J Respir Crit Care Med. (2005). 171:912–30. doi: 10.1164/rccm.200406-710ST
27. Barreto M, Villa MP, Monti F, Bohmerova Z, Martella S, Montesano M et al. Additive effect of eosinophilia and atopy on exhaled nitric oxide levels in children with or without a history of respiratory symptoms. Pediatr Allergy Immunol. (2005) 16:52–8. doi: 10.1111/j.1399-3038.2005.00220.x
28. Silkoff PE, Laviolette M, Singh D, FitzGerald JM, Kelsen S, Backer V, et al. Identification of airway mucosal type 2 inflammation by using clinical biomarkers in asthmatic patients. J Allergy Clin Immunol. (2017) 140:710–9. doi: 10.1016/j.jaci.2016.11.038
29. Dweik RA, Boggs PB, Erzurum SC, Irvin CG, Leigh MW, Lundberg JO, et al. An official ATS clinical practice guideline: interpretation of exhaled nitric oxide levels (FeNO) for clinical applications. Am J Respir Crit Care Med. (2011) 184:602–15. doi: 10.1164/rccm.9120-11ST
30. Amat F, Labbé A. Biomarkers for severe allergic asthma in children: could they be useful to guide disease control and use of omalizumab? Expert Rev Respir Med. (2018) 12:475–82. doi: 10.1080/17476348.2018.1475233
31. Wang Z, Pianosi PT, Keogh KA, Zaiem F, Alsawas M, Alahdab F, et al. The diagnostic accuracy of fractional exhaled nitric oxide testing in asthma: a systematic review and meta-analyses. Mayo Clin Proc. (2018) 93:191–8. doi: 10.1016/j.mayocp.2017.11.012
32. Puckett JL, Taylor RWE, Leu S-Y, Guijon OL, Aledia AS, Galant SP, et al. Clinical patterns in asthma based on proximal and distal airway nitric oxide categories. Respir Res. (2010) 11:47. doi: 10.1186/1465-9921-11-47
33. Barreto M, Capi M, Lionetto L, Caiazzo I, Salerno G, Cardelli P, et al. Urinary and exhaled biomarkers of exercise-induced bronchoconstriction in atopic asthmatic children. Pediatr Pulmonol. (2019) 54:1447–56. doi: 10.1002/ppul.24419
34. Knihtilä H, Kotaniemi-Syrjänen A, Pelkonen AS, Mäkelä MJ, Malmberg LP. Small airway function in children with mild to moderate asthmatic symptoms. Ann Allergy Asthma Immunol. (2018) 121:451–57. doi: 10.1016/j.anai.2018.07.026
35. Irving S, Fleming L, Ahmad F, Biggart E, Bingham Y, Cook J, et al. Lung clearance index and steroid response in pediatric severe asthma. Pediatr Pulmonol. (2020) 55:890–8. doi: 10.1002/ppul.24675
36. Keen C, Olin AC, Wennergren G, Gustafsson P. Small airway function, exhaled NO and airway hyper-responsiveness in paediatric asthma. Respir Med. (2011) 105:1476–84. doi: 10.1016/j.rmed.2011.04.004
37. Macleod KA, Horsley AR, Bell NJ, Greening AP, Innes JA, Cunningham S. Ventilation heterogeneity in children with well-controlled asthma with normal spirometry indicates residual airways disease. Thorax. (2009) 64:33–7. doi: 10.1136/thx.2007.095018
38. Robinson PD, Latzin P, Verbanck S, Hall GL, Horsley A, Gappa M, et al. Consensus statement for inert gas washout measurement using multiple- and single- breath test. Eur Respir J. (2013) 41:507–22. doi: 10.1183/09031936.00069712
39. Anagnostopoulou P, Latzin P, Jensen R, Stahl M, Harper A, Yammine S, et al. Normative data for multiple breath washout outcomes in school-aged Caucasian children. Eur Respir J. (2020) 55:1901302. doi: 10.1183/13993003.01302-2019
40. Arianto L, Hallas H, Stokholm J, Bønnelykke K, Bisgaard H, Chawes BL. Multiple breath washout for diagnosing asthma and persistent wheeze in young children. Ann Am Thorac Soc. (2019) 16:599–605. doi: 10.1513/AnnalsATS.201807-503OC
41. Mikalsen IB, Nassehi D, Øymar K. Vortex whistle and smart phone application for peak flow recordings in asthmatic children: a feasibility study. Telemed J E Health. (2019) 25:1077–82. doi: 10.1089/tmj.2018.0270
42. Sly PD, Flack F. Is home monitoring of lung function worthwhile for children with asthma? Thorax. (2001) 56:164–5. doi: 10.1136/thorax.56.3.164
43. Wensley D, Silverman M. Peak flow monitoring for guided self-management in childhood asthma: a randomized controlled trial. Am J Respir Crit Care Med. (2004) 170:606–12. doi: 10.1164/rccm.200307-1025OC
44. Brand PL, Duiverman EJ, Postma DS, Waalkens HJ, Kerrebijn KF, van Essen-Zandvliet EE. Peak flow variation in childhood asthma: relationship to symptoms, atopy, airways obstruction and hyperresponsiveness. Dutch CNSLD study group. Eur Respir J. (1997) 10:1242–7. doi: 10.1183/09031936.97.10061242
45. Kamps AW, Roorda RJ, Brand PL. Peak flow diaries in childhood asthma are unreliable. Thorax. (2001) 56:180–2. doi: 10.1136/thorax.56.3.180
46. Mortimer KM, Fallot A, Balmes JR, Tager IB. Evaluating the use of a portable spirometer in a study of pediatric asthma. Chest. (2003) 123:1899–907. doi: 10.1378/chest.123.6.1899
47. Carpenter DM, Jurdi R, Roberts CA, Hernandez M, Horne R, Chan A. A review of portable electronic spirometers: implications for asthma self-management. Curr Allergy Asthma Rep. (2018) 18:53. doi: 10.1007/s11882-018-0809-3
48. Thompson R, Delfino RJ, Tjoa T, Nussbaum E, Cooper D. Evaluation of daily home spirometry for school children with asthma: new insights. Pediatr Pulmonol. (2006) 41:819–28. doi: 10.1002/ppul.20449
49. Deschildre A, Béghin L, Salleron J, Iliescu C, Thumerelle C, Santos C, et al. Home telemonitoring (forced expiratory volume in 1 s) in children with severe asthma does not reduce exacerbations. Eur Respir J. (2012) 39:290–6. doi: 10.1183/09031936.00185310
50. Kew KM, Cates CJ. Home telemonitoring and remote feedback between clinic visits for asthma. Cochrane Database Syst Rev. (2016) 2016:CD011714. doi: 10.1002/14651858.CD011714.pub2
51. Wong A, Hardaker K, Field P, Huvanandana J, King GG, Reddel H, et al. Home-based forced oscillation technique day-to-day variability in pediatric asthma. Am J Respir Crit Care Med. (2019) 199:1156–60. doi: 10.1164/rccm.201809-1659LE
52. van der Valk RJ, Baraldi E, Stern G, Frey U, de Jongste JC. Daily exhaled nitric oxide measurements and asthma exacerbations in children. Allergy. (2012) 67:265–71. doi: 10.1111/j.1398-9995.2011.02734.x
53. Shields MD, ALQahtani F, Rivey MP, McElnay JC. Mobile direct observation of therapy (MDOT) - a rapid systematic review and pilot study in children with asthma. PLoS ONE. (2018) 13:e0190031. doi: 10.1371/journal.pone.0190031
54. Dubois A, Brody A, Lewis D, Burgess BF. Oscillation mechanics of lungs and chest in man. J Appl Physiol. (1956) 8:587–94. doi: 10.1152/jappl.1956.8.6.587
55. Tsoukias NM, George SC. A two-compartment model of pulmonary nitric oxide exchange dynamics. J Appl Physiol. (1998) 85:653–66. doi: 10.1152/jappl.1998.85.2.653
56. Barreto M, Zambardi R, Villa MP. Exhaled nitric oxide and other exhaled biomarkers in bronchial challenge with exercise in asthmatic children: current knowledge. Paediatr Respir Rev. (2015) 16:68–74. doi: 10.1016/j.prrv.2013.11.006
57. Paraskakis E, Brindicci C, Fleming L, Krol R, Kharitonov SA, Wilson NM, et al. Measurement of bronchial and alveolar nitric oxide production in normal children and children with asthma. Am J Respir Crit Care Med. (2006) 174:260–7. doi: 10.1164/rccm.200506-962OC
58. Helgeson SA, Lim KG, Lee AS, Niven AS, Patel NM. Aerosol generation during spirometry. Ann Am Thorac Soc. (2020). doi: 10.1513/AnnalsATS.202005-569RL. [Epub ahead of print].
59. van Vliet D, van Horck M, van de Kant K, Vaassen S, Gulikers S, Winkens B, et al. Electronic monitoring of symptoms and lung function to assess asthma control in children. Ann Allergy Asthma Immunol. (2014) 113:257–62.e1. doi: 10.1016/j.anai.2014.05.015
Keywords: coronavirus disease (COVID-19), SARS-Cov-2, pulmonary function testing (pft), asthma, children, forced oscillation technique (FOT), interrupter resistance (Rint), exhaled nitric oxide (FeNO)
Citation: Barreto M, Evangelisti M, Montesano M, Martella S and Villa MP (2020) Pulmonary Function Testing in Asthmatic Children. Tests to Assess Outpatients During the Covid-19 Pandemic. Front. Pediatr. 8:571112. doi: 10.3389/fped.2020.571112
Received: 09 June 2020; Accepted: 22 September 2020;
Published: 17 November 2020.
Edited by:
Michael David Shields, Queen's University Belfast, United KingdomReviewed by:
Gary Martin Doherty, Royal Belfast Hospital for Sick Children, United KingdomNiamh Catherine Galway, Royal Belfast Hospital for Sick Children, United Kingdom
Louise Jane Fleming, Imperial College London, United Kingdom
Copyright © 2020 Barreto, Evangelisti, Montesano, Martella and Villa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mario Barreto, bWFyaW8uYmFycmV0b0B1bmlyb21hMS5pdA==
 Mario Barreto
Mario Barreto Melania Evangelisti
Melania Evangelisti Marilisa Montesano
Marilisa Montesano Susy Martella
Susy Martella Maria Pia Villa
Maria Pia Villa