- 1Department of Neurosurgery, Tangdu Hospital of the Fourth Military Medical University, Xi'an, China
- 2Department of Outpatient, The 316th Military Hospital of China, Beijing, China
- 3Department of Ultrasound, Xijing Hospital of the Fourth Military Medical University, Xi'an, China
Spontaneous extrusion of the distal catheter from the umbilicus following a ventriculoperitoneal shunt (VPS) for the treatment of hydrocephalus is an extremely rare complication. Here, we describe an 8-years-old boy who underwent a VPS for communicating hydrocephalus and thereafter the distal part of the catheter was extruded through the umbilicus. The extrusive part of the peritoneal catheter was successfully cut off with a laparoscope, keeping the remaining catheter in place and functional. The subsequent recovery process was uneventful. To the best of our knowledge, there have been no reports of using laparoscopy to cut the protruding part and replace the shunt end. By keeping the function of the original shunt pipe, this case report offers an innovative and informative approach to treating this complication.
Introduction
A ventriculoperitoneal shunt (VPS) is a common surgical intervention performed to treat different kinds of hydrocephalus in children and adults. However, postoperative complications such as infection, failure of a valve, catheter migration, obstruction of the shunt, and over-drainage are common (1). In contrast, extrusion of the peritoneal catheter from the umbilicus is rare. Here, we report such an unusual case.
Case Presentation
An 8-years-old boy presented at our unit with a visible catheter extrusion through the umbilicus 6 months after VPS. For his past medical history, a hemispherectomy for intractable epilepsy had been conducted 1 year earlier. A computed tomography (CT) scan of the head 5 months after the operation showed communicating hydrocephalus. Subsequently, the child underwent a right-sited medium-pressure VPS using the Codman Hakim programmable valve system (Codman, Johnson Company, Raynham, USA) to relieve the hydrocephalus. The length of the intraperitoneal catheter was about 50 cm, which was chosen taking into account that the patient's height will increase with normal growth and development. The shunt system has an antisiphon valve but no antibacterial activity. The child presented with a fever with a daily axillary temperature ranging from 38 to 39°C 1 week after the VPS. At the same time, he had abdominal symptoms such as pain and tension in the abdominal muscles. The plain abdominal radiography showed intestinal tympanites.
Culture of cerebrospinal fluid (CSF) extracted via lumbar puncture grew methicillin-resistant S. epidermidis, and blood culture grew S. simulans. Consequently, central nervous system infection and septicemia were definitely diagnosed based on the above results. Intravenous vancomycin was administered based on the drug sensitivity test. He was discharged from the hospital after successful recovery.
However, the umbilicus was red and swollen 6 months after VPS. The local skin ruptured, and yellow fluid was discharged from the fistula. The shunt catheter subsequently extruded through the fistula for about 25 cm length (Figure 1). Abdominal ultrasonography revealed that there was effusion under the umbilicus. Culture of the effusion via ultrasound-guided puncture grew methicillin-resistant S. epidermidis. Abdominal CT scan revealed that the effusion was encapsulated and localized around the umbilicus (Figure 2). The laboratory examinations of CSF and blood were normal. Most importantly, the patient's vital signs were stable.
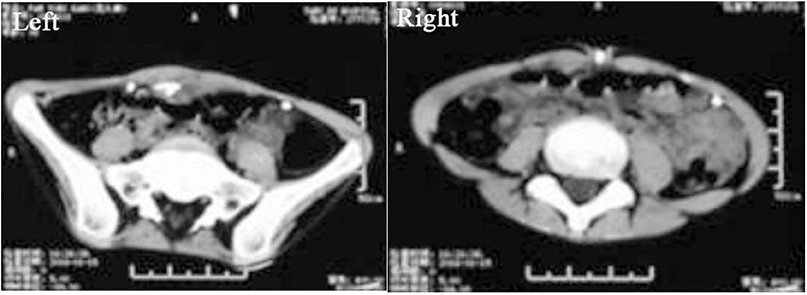
Figure 2. Abdominal axial CT (left) showing that there is fluid around the shunt at the superficial part of the abdomen around the umbilicus. CT (right) demonstrating that the shunt catheter was extruded through the umbilicus.
Based on these findings, we carried out the following treatments. First, the extrusive catheter was connected with a closed drainage bag for CSF collection. Secondly, according to the drug sensitivity test, vancomycin and cefoperazone sulbactam sodium were still used for 2 weeks to control local infection of the umbilicus. Thirdly, the fistula was washed with a disinfectant daily and drained smoothly. After a 2-weeks treatment, the patient showed no symptoms of infection or hydrocephalus. He was discharged with the extrusive catheter and followed up during dressing change at our outpatient clinic. Three months later, an abdominal CT revealed that the effusion had disappeared (Figure 3). Subsequently, the peritoneal catheter was revised via a laparoscopic procedure, but not totally replaced. During the operation, extensive adhesions of intra-abdominal organs, including the digestive tract, greater omentum, and peritoneum, were found. Connective tissue proliferation was also found to form a granular mass enclosing the fistula and catheter (Figure 4). Adhesiolysis was performed after laparoscopic exploration of the abdomen. Finally, the extrusive part of the shunt was cut off and the intra-abdominal part was repositioned on the diaphragm-facing surface of the liver after ensuring its patency, observing CSF dripping from its distal end (Figure 5). The child was discharged on the 7th day after surgery. The fistula of the umbilicus healed up. The plain abdominal radiograph and CT during the follow-up showed that the catheter was in place and well-functional.
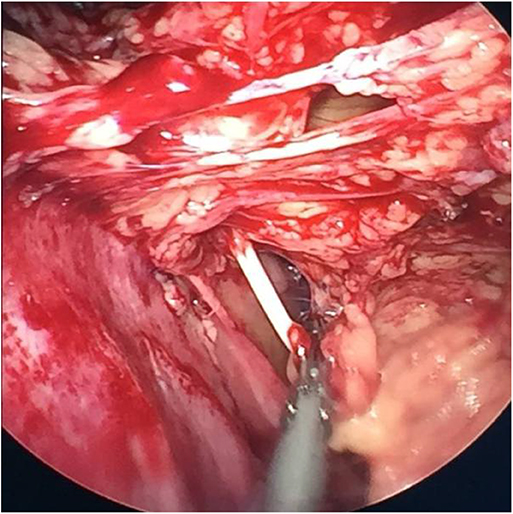
Figure 4. Extensive organ adhesions in the abdomen, including the digestive tract, greater omentum, and peritoneum, were visible.
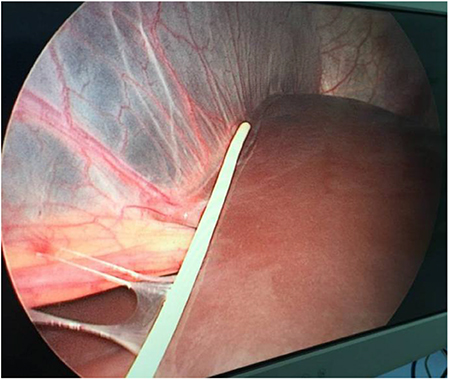
Figure 5. The extrusive part of the shunt was cut off, and the intra-abdominal part was repositioned on the diaphragm-facing surface of the liver using the laparoscope.
Discussion
VPS is the most common surgical therapy for the management of hydrocephalus of diverse etiologies. However, it has efficacy but does not guarantee absolute safety since complications are reported in some cases, especially the children, who survive long after VPS (2). A variety of abdominal complications have been reported with an acute abdomen, intestinal perforation, or obstruction, peritonitis, pseudocyst, and umbilical fistula (3–7). Here, we present a rare case that had the distal catheter extruded from the umbilicus after VPS. There were few previous reports of such a complication (8). The exact mechanism leading to this complication remains unknown.
A misbalance between the inflammatory reaction, either sterile or infectious, and body immunity is a possible reason (9).
In our case, it was traced back to 1 week after VPS; the cultures of CSF and blood were positive for bacteria, which indicated systemic infection after VPS. Abdominal infection had led to severe peritonitis and abdominal adhesions, which were confirmed by laparoscope. The inflammation was gradually localized to the umbilicus after the infection had been controlled. The distal catheter migrated to the umbilicus under the impulse of intestinal peristalsis. Then, the tip of the shunt was enclosed and fixed under the umbilicus by the proliferation of the connective tissue in the process of eliminating the abdominal infection. Nevertheless, the compounded fluid of CSF and effusion was continually collected and invaded the umbilicus, which is the weakest part of the abdominal wall. A fistula ultimately formed through the umbilicus. Finally, the catheter extruded from the fistula.
There are two different opinions on the management of this complication, either a revision or a replacement of the abdominal catheter. Based on our experience, we suggest that the abdominal shunt should be revised. If this method fails, the shunt should be replaced. This is the only approach that guarantees optimal cost-effectiveness. The abdomen has a very strong capacity to defend against inflammation, and it is not necessary to excessively worry about this complication worsening if the vital signs are stable. Even antibiotics may not be necessary to prevent an infection except in the perioperative period. In addition, keeping the effusion draining smoothly is very important.
Teegala and Kota reported two cases of ventriculoperitoneal shunt herniation through the anus (10). Malnutrition and infection were analyzed as possible causes. In most cases, intestinal perforation is asymptomatic. In a few cases, complications such as intestinal obstruction, adhesion, and intussusception can occur, which need to be treated as soon as possible. Similar to this case, there was no sepsis after herniation of the shunt tube. In cases of no perforating peritonitis or no abdominal abscess, there is often simply herniation from the umbilicus without other complications, and there is no need for a formal laparotomy (11–13). The patient was followed up for 6 months without any symptoms or complications (follow-up results were not included).
In this case, the exposed part of the shunt was cut off and removed through laparoscope, and the rest of the distal end of the shunt was fixed on the diaphragm side of liver. According to a large number of previous clinical reports, adhesive peritonitis is the main cause of the complications of the abdominal end. For infectious complications, the previous treatment methods include antibiotics and the removal of the shunt. Many doctors prefer to replace a new shunt after the removal of the old one to avoid the aggravation of hydrocephalus, but this greatly increases the pain and economic burden of patients.
In this case, we first drained the distal end of the shunt tube externally and carried out anti-infective treatment at the same time. The re-operation of VPS was not chosen for the following reasons. First, the child had developed a shunt tube dependency. If the shunt tube is removed directly, a lateral ventricle puncture is required to relieve hydrocephalus. After the infection of abdominal cavity is improved, which may take a long time, the re-operation of VPS can be performed. This strategy increases the risk of surgery and the possibility of intracranial infection. Then, during the 3-months drainage period, the dressings were changed in the outpatient clinic, and the patient was carefully nursed at home but not in the hospital. Furthermore, in terms of economic cost, the cost of re-operation of VPS is about 50,000 RMB in China, while the cost of laparoscopic surgery is about 10,000 RMB.
For the use of laparoscopy, in addition to reducing the chance of infection, the abdominal end can be fixed on the diaphragmatic surface of the liver, far away from the greater omentum, so as to reduce the probability of recurrence of adhesive peritonitis. This is also the difference between the present case and the previous reports.
Conclusions
In summary, the extrusion of the abdominal shunt from an umbilical fistula is a serious complication because of abdominal infection, which is very rare. This report describes a pediatric case of an extrusion of the distal catheter from the umbilicus as a rare complication of VPS. This case report shares a relatively simple and effective therapeutic method, which is innovative and scientific to some extent. We hope to provide a simple and economic treatment option for neurosurgeons in the treatment of such complications.
For the use of laparoscopy, in addition to reducing the chance of infection, the abdominal end can be fixed on the diaphragmatic surface of the liver, far away from the greater omentum, so as to reduce the probability of recurrence of adhesive peritonitis.
Data Availability Statement
All datasets generated for this study are included in the article/supplementary material.
Ethics Statement
The studies involving human participants were reviewed and approved by Medical Ethics Committee of Tangdu Hospital, Fourth Military Medical University. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin. Written informed consent was obtained from the legal guardian for the publication of any potentially identifiable images or data included in this article. Informed consent was obtained from all individual participants included in the study.
Author Contributions
YX and CW contributed conception and design of the study. ZR wrote the first draft of the manuscript. FH wrote sections of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Reddy GK, Bollam P, Caldito G. Long-term outcomes of ventriculoperitoneal shunt surgery in patients with hydrocephalus. World Neurosurg. (2014) 81:404–10. doi: 10.1016/j.wneu.2013.01.096
2. Bober J, Rochlin J, Marneni S. Ventriculoperitoneal shunt complications in children: an evidence-based approach to emergency department management. Pediatr Emerg Med Pract. (2016) 13:1–22.
3. Esposito C1, Colella G, Settimi A, Centonze A, Signorelli F, Ascione G, et al. One-trocar laparoscopy: a valid procedure to treat abdominal complications in children with peritoneal shunt for hydrocephalus. Surg Endosc. (2003) 17:828–30. doi: 10.1007/s00464-002-9063-8
4. Zhao R, Shi W, Yu J, Gao X, Li H. Complete intestinal obstruction and necrosis as a complication of a ventriculoperitoneal shunt in children: a report of 2 cases and systematic literature review. Medicine. (2015) 94:e1375–83. doi: 10.1097/MD.0000000000001375
5. Awori J, Wu CY, Maher CO. Malignant cause of ventriculoperitoneal shunt “pseudocyst”: a case report. Pediatr Neurosurg. (2015) 50:73–5. doi: 10.1159/000377731
6. Mohindra S, Singla N, Gupta R, Gupta SK. CSF fistula through the umbilicus following a shunt surgery: a case report and literature review. Pediatr Neurosurg. (2007) 43:396–8. doi: 10.1159/000106389
7. Wu Y, Green NL, Wrensch MR, Zhao S, Gupta N. Ventriculoperitoneal shunt complications in California: 1990 to 2000. Neurosurgery. (2007) 61:557–63. doi: 10.1227/01.NEU.0000290903.07943.AF
8. Wani AA, Ramzan A, Wani MA. Protrusion of a peritoneal catheter through the umblicus: an unusual complication of a ventriculoperitoneal shunt. Pediatr Surg Int. (2002) 18:171–2. doi: 10.1007/s003830100608
9. de Aquino HB, Carelli EF, Borges Neto AG, Pereira CU. Nonfunctional abdominal complications of the distal catheter on the treatment of hydrocephalus: an inflammatory hypothesis? Childs Nerv Syst. (2006) 22:1225–30. doi: 10.1007/s00381-005-0025-z
10. Teegala R, Kota LP. Unusual complications of ventriculo peritoneal shunt surgery. J Neurosci Rural Pract. (2012) 3:361–4. doi: 10.4103/0976-3147.102628
11. Sridhar K, Karmarkar V. Peroral extrusion of ventriculoperitoneal shunt: case report and review of literature. Neurol. (2009) 57:334–6. doi: 10.4103/0028-3886.53283
12. Yousfi MM, Jackson NS, Abbas M, Zimmerman RS, Fleischur RE. Bowel perforation complicating ventriculoperitoneal shunt: creport and review. Gastrointest Endosc. (2003) 58:144–8. doi: 10.1067/mge.2003.324
Keywords: hydrocephalus, ventriculoperitoneal shunt, complications, extrusion, umbilicus
Citation: Xia Y, He F, Ren Z and Wang C (2020) Extrusion of the Distal Catheter From the Umbilicus: A Case Report of a Rare Complication After Ventriculoperitoneal Shunt and Its Management. Front. Pediatr. 8:228. doi: 10.3389/fped.2020.00228
Received: 10 February 2020; Accepted: 15 April 2020;
Published: 27 May 2020.
Edited by:
Francesco Morini, Bambino Gesù Children Hospital (IRCCS), ItalyReviewed by:
Sanja Miodrag Sindjic Antunovic, University of Belgrade, SerbiaSherif Mohamed Shehata, Tanta University, Egypt
Copyright © 2020 Xia, He, Ren and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yi Xia, c2h5bG9ja194eUAxNjMuY29t; Chao Wang, NzYwNDI2MjhAcXEuY29t
 Yi Xia
Yi Xia Fang He2
Fang He2
